Transcriptomics Reveals the Mechanism of Rosa roxburghii Tratt Ellagitannin in Improving Hepatic Lipid Metabolism Disorder in db/db Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Animal Feeding Methods
2.3. Effect of RTT Ellagitannin on Liver Lipid Levels in Mice
2.4. Pathological Analysis of Oil Red O
2.5. Transcriptome High-Throughput Sequencing
2.6. qRT-PCR Analysis
2.7. Western Blot Analysis
2.8. Data Analysis
3. Results
3.1. Effect of RTT Ellagitannin on Body Weight and FBG in Mice
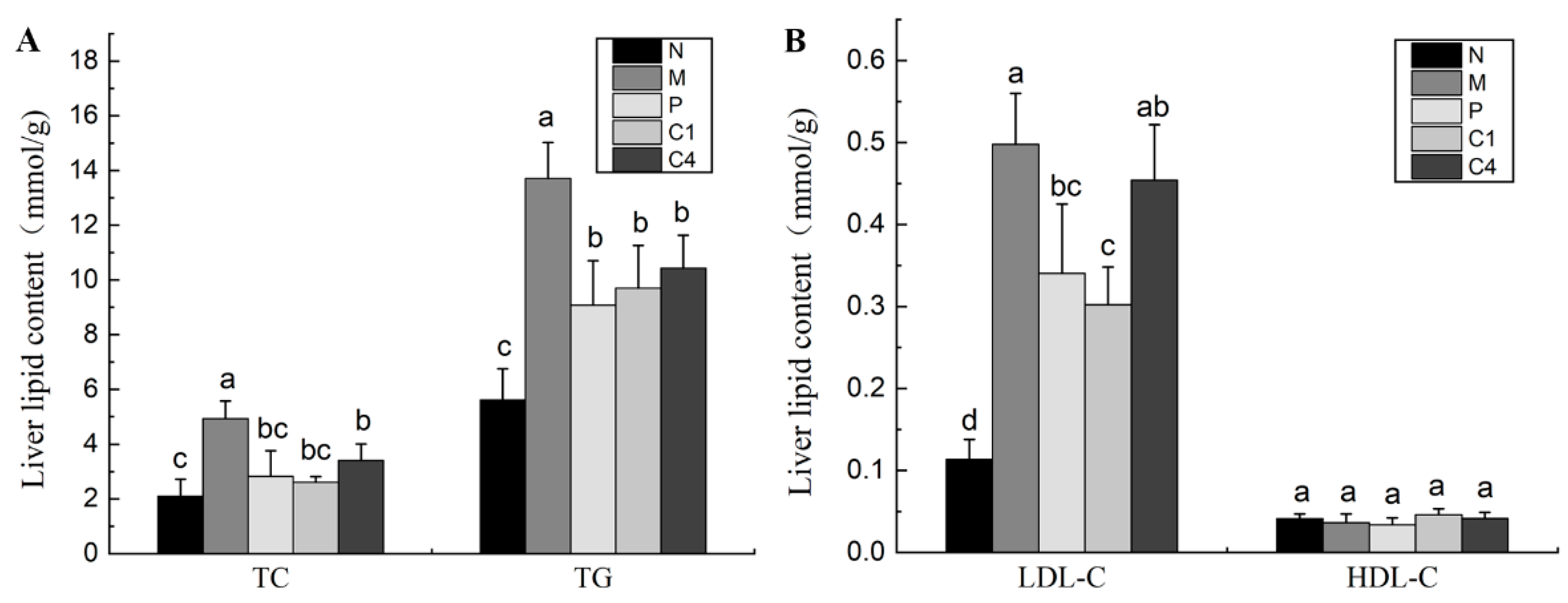
3.2. Effect of RTT Ellagitannin on Liver Lipid Contents in Mice
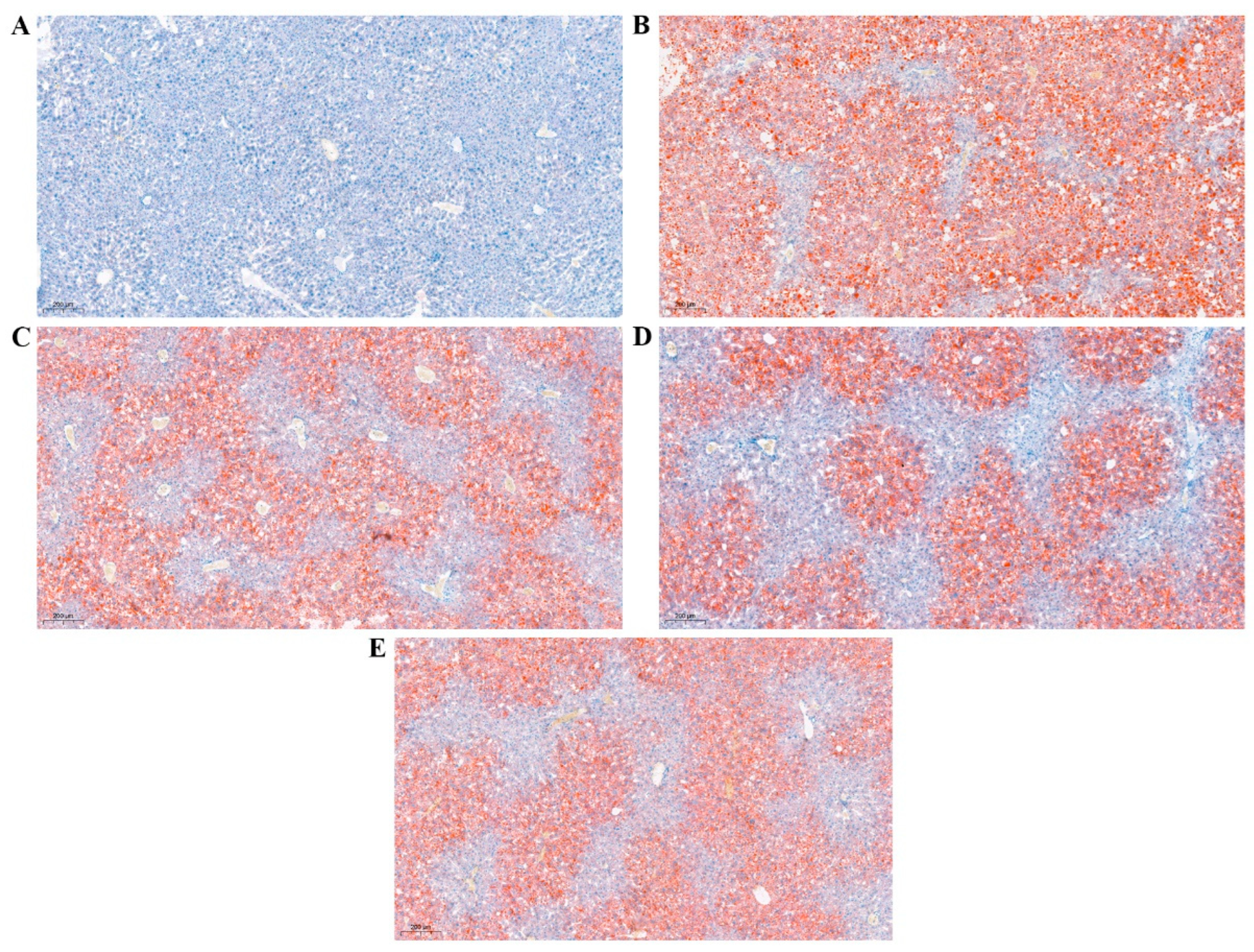
3.3. Oil Red O Staining
3.4. Sequencing QC Filtering Analysis
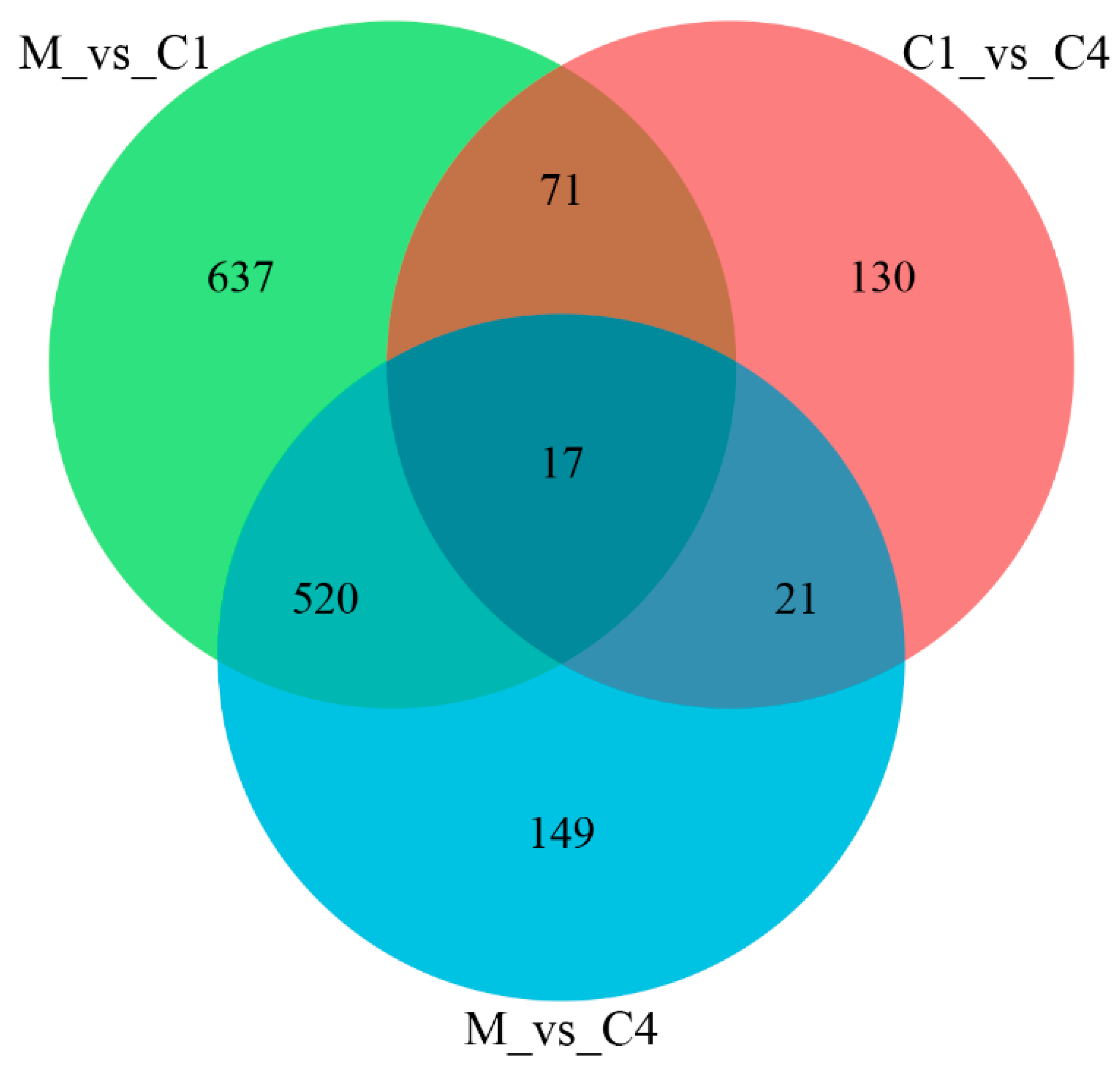
3.5. High-Throughput Sequencing Analysis
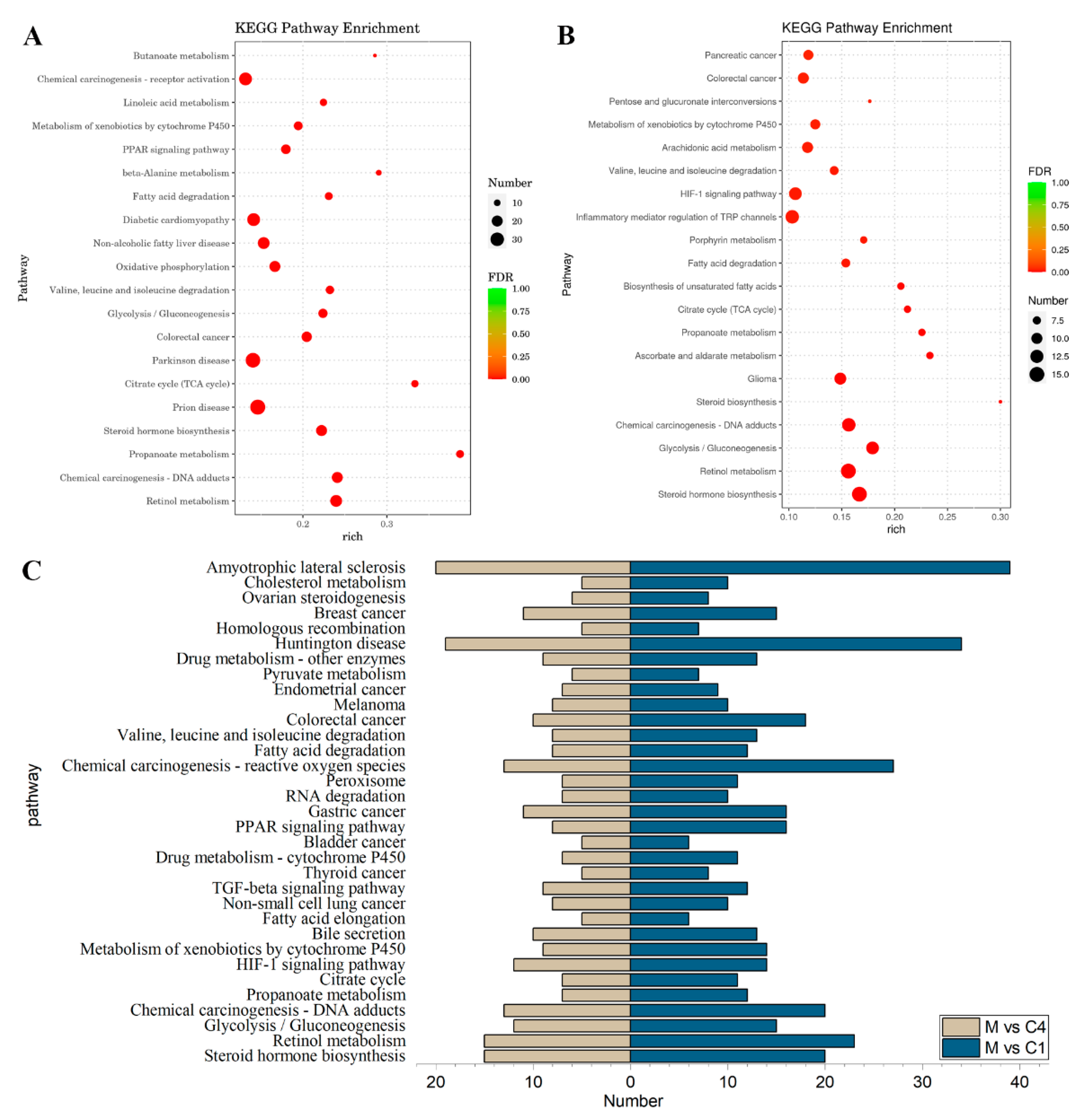
3.6. GO Term and KEGG Pathway Analysis of DEGs
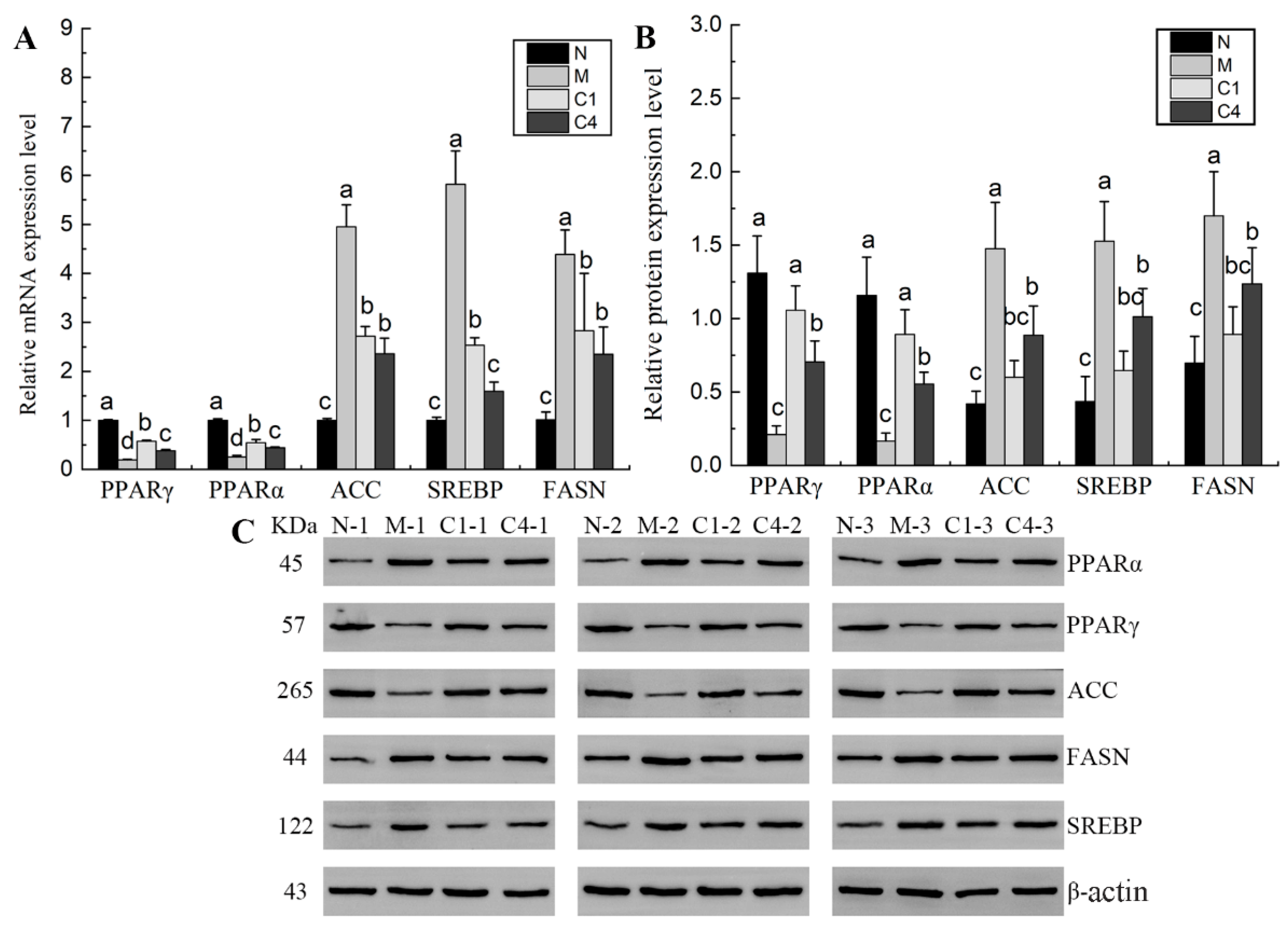
3.7. qRT-PCR and Western Blot Validation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chatterjee, S.; Khunti, K.; Davies, M.J. Type 2 diabetes. Lancet 2017, 389, 2239–2251. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.R.; Chen, H.H.; Nie, Q.X.; Huang, X.J.; Nie, S.P. Dendrobium officinale polysaccharide ameliorates the liver metabolism disorders of type II diabetic rats. Int. J. Biol. Macromol. 2020, 164, 1939–1948. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Nie, Q.X.; Hu, J.L.; Huang, X.J.; Zhang, K.; Pan, S.J.; Nie, S.P. Hypoglycemic and hypolipidemic effects of glucomannan extracted from Konjac on type 2 diabetic rats. J. Agric. Food Chem. 2019, 67, 5278–5288. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.Y.; Gao, K.; Liu, Y.C.; Mao, G.H.; Chen, K.; Qiu, X.C.; Zhao, T.; Yang, L.Q.; Feng, W.W.; Wu, X.Y. Transcriptome analysis revealed the mechanism of the metabolic toxicity and susceptibility of di-(2-ethylhexyl)phthalate on adolescent male ICR mice with type 2 diabetes mellitus. Arch. Toxicol. 2019, 93, 3183–3206. [Google Scholar] [CrossRef]
- Lu, M.; Zhang, H.S.; An, H.M. Chloroplast DNA-based genetic variation of Rosa roxburghii in Southwest China: Phylogeography and conservation implications. Hortic. Plant J. 2021, 7, 286–294. [Google Scholar] [CrossRef]
- Yu, K.B.; Zhou, L.; Sun, Y.F.; Zeng, Z.C.; Chen, H.W.; Liu, J.P.; Zou, L.Q.; Liu, W. Anti-browning effect of Rosa roxburghii on apple juice and identification of polyphenol oxidase inhibitors. Food Chem. 2021, 359, 129855. [Google Scholar] [CrossRef]
- Xiang, Q.S.; Xiao, H.F.; Gao, S.B.; Wen, M.T.; Jia, G.L.; Ren, X.M.; Liu, X.B. In vitro antioxidant properties of Rosa roxburghii aqueous extracts. Aust. J. Crop Sci. 2012, 6, 854–860. [Google Scholar]
- Wang, L.T.; Lv, M.J.; An, J.Y.; Fan, X.H.; Dong, M.Z.; Zhang, S.D.; Wang, J.D.; Wang, Y.Q.; Cai, Z.H.; Fu, Y.J. Botanical characteristics, phytochemistry and related biological activities of Rosa roxburghii Tratt fruit, and its potential use in functional foods: A review. Food Funct. 2021, 12, 1432–1451. [Google Scholar] [CrossRef]
- Xu, P.; Liu, X.X.; Xiong, X.W.; Zhang, W.B.; Cai, X.H.; Qiu, P.Y.; Hao, M.H.; Wang, L.J.; Lu, D.D.; Zhang, X.H.; et al. Flavonoids of Rosa roxburghii Tratt exhibit anti-apoptosis properties by regulating PARP-1/AIF. J. Cell. Biochem. 2017, 118, 3943–3952. [Google Scholar] [CrossRef]
- Zhao, J.; Liu, J.J.; Wang, F.Q.; Wang, S.S.; Feng, H.; Xie, X.B.; Hao, F.L.; Zhang, L.Z.; Fang, C.B. Volatile constituents and ellagic acid formation in strawberry fruits of selected cultivars. Food Res. Int. 2020, 138, 109767. [Google Scholar] [CrossRef]
- Muthukumaran, S.; Tranchant, C.; Shi, J.; Ye, X.Q.; Xue, S.J. Ellagic acid in strawberry (Fragaria spp.): Biological, technological, stability, and human health aspects. Food Qual. Safety 2017, 1, 227–252. [Google Scholar] [CrossRef]
- Farbood, Y.; Rashno, M.; Ghaderi, S.; Khoshnam, S.E.; Sarkaki, A.; Rashidi, K.; Rashno, M.; Badavi, M. Ellagic acid protects against diabetes-associated behavioral deficits in rats: Possible involved mechanisms. Life Sci. 2019, 225, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Nankar, R.P.; Doble, M. Hybrid drug combination: Anti-diabetic treatment of type 2 diabetic Wistar rats with combination of ellagic acid and pioglitazone. Phytomedicine 2017, 37, 4–9. [Google Scholar] [CrossRef]
- Ahad, A.; Ganai, A.A.; Mujeeb, M.; Siddiqui, W.A. Ellagic acid, an NF-kB inhibitor, ameliorates renal function in experimental diabetic nephropathy. Chem. Biol. Interact. 2014, 219, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Bodis, K.; Roden, M. Energy metabolism of white adipose tissue and insulin resistance in humans. Eur. J. Clin. Investig. 2018, 48, e13017. [Google Scholar] [CrossRef]
- Chen, C.; Tan, S.; Ren, T.; Wang, H.; Dai, X.; Wang, H. Polyphenol from Rosaroxburghii Tratt fruit ameliorates the symptoms of diabetes by activating the P13K/AKT insulin pathway in db/db mice. Foods 2022, 11, 636. [Google Scholar] [CrossRef]
- Zhang, C.J.; Zhu, N.; Li, H.F.; Gong, Y.Z.; Gu, J.; Shi, Y.N.; Liao, D.F.; Wang, W.; Dai, A.G.; Qin, L. New dawn for cancer cell death: Emerging role of lipid metabolism. Mol. Metab. 2022, 63, 101529. [Google Scholar] [CrossRef]
- Shetty, S.S.; Kumari, S. Fatty acids and their role in type-2 diabetes. Exp. Ther. Med. 2021, 22, 706. [Google Scholar] [CrossRef]
- Li, N.; Qiu, Y.M.; Wu, Y.P.; Zhang, M.; Lai, Z.Z.; Wang, Q.; Du, Y.Y.; Guo, L.; Liu, S.; Li, Z.L. Association of serum total fatty acids with type 2 diabetes. Clin. Chim. Acta 2020, 500, 59–68. [Google Scholar] [CrossRef]
- Menendez, J.A.; Lupu, R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat. Rev. Cancer 2007, 7, 763–777. [Google Scholar] [CrossRef]
- Allred, J.B.; Reilly, K.E. Short-term regulation of acetyl CoA carboxylase in tissues of higher animals. Prog. Lipid Res. 1996, 35, 371–385. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Hu, J.J.; Sheng, L.; Yuan, M.; Wu, Y.; Chen, L.; Zheng, G.H.; Qiu, Z.P. Metformin delays AKT/c-Met-driven hepatocarcinogenesis by regulating signaling pathways for de novo lipogenesis and ATP generation. Toxicol. Appl. Pharmacol. 2019, 365, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Salles, J.; Sargueil, F.; Knoll-Gellida, A.; Witters, L.A.; Cassagne, C.; Garbay, B. Acetyl-CoA carboxylase and SREBP expression during peripheral nervous system myelination. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids 2003, 1631, 229–238. [Google Scholar] [CrossRef]
- Kuriyama, H.; Liang, G.; Engelking, L.J.; Horton, J.D.; Goldstein, J.L.; Brown, M.S. Compensatory increase in fatty acid synthesis in adipose tissue of mice with conditional deficiency of SCAP in liver. Cell Metab. 2005, 1, 41–51. [Google Scholar] [CrossRef]
- Athanikar, J.N.; Sanchez, H.B.; Osborne, T.F. Promoter selective transcriptional synergy mediated by sterol regulatory element binding protein and Sp1: A critical role for the Btd domain of Sp1. Mol. Cell. Biol. 1997, 17, 5193–5200. [Google Scholar] [CrossRef] [PubMed]
- Fortis-Barrera, M.D.L.Á.; Alarcón-Aguilar, F.J.; Becerril-García, A.; Flores-Sáenz, J.L.E.; Almanza-Pérez, J.C.; García-Lorenzana, M.; Lazzarini-Lechuga, R.C.; Román-Ramos, R.; Blancas-Flores, G. Mechanism of the hypoglycemic activity and hepatoprotective effect of the aqueous extract of Cecropia obtusifolia Bertol. J. Med. Food 2020, 23, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Figueroa, S.; Ramirez-Espinosa, J.J.; Estrada-Soto, S.; Almanza-Perez, J.C.; Roman-Ramos, R.; Alarcon-Aguilar, F.J.; Hernandez-Rosado, J.V.; Moreno-Diaz, H.; Diaz-Coutino, D.; Navarrete-Vazquez, G. Discovery of thiazolidine-2,4-dione/biphenylcarbonitrile hybrid as dual PPAR α/γ modulator with antidiabetic effect: In vitro, in silico and in vivo approaches. Chem. Biol. Drug Des. 2013, 81, 474–483. [Google Scholar] [CrossRef]
- Su, H.M.; Bao, T.; Xie, L.H.; Xu, Y.; Chen, W. Transcriptome profiling reveals the antihyperglycemic mechanism of pelargonidin-3-O-glucoside extracted from wild raspberry. J. Funct. Foods 2020, 64, 103657. [Google Scholar] [CrossRef]
- Suckling, K.E.; Stange, E.F. Role of acyl-CoA: Cholesterol acyltransferase in cellular cholesterol metabolism. J. Lipid Res. 1985, 26, 647–671. [Google Scholar] [CrossRef]
- Gilep, A.A.; Sushko, T.A.; Usanov, S.A. At the crossroads of steroid hormone biosynthesis: The role, substrate specificity and evolutionary development of CYP17. Biochim. Biophys. Acta (BBA) Proteins Proteom. 2011, 1814, 200–209. [Google Scholar] [CrossRef]
- Vijayan, M.M.; Raptis, S.; Sathiyaa, R. Cortisol treatment affects glucocorticoid receptor and glucocorticoid-responsive genes in the liver of rainbow trout. Gen. Comp. Endocrinol. 2003, 132, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.C.; Du, F.K.; Li, Y.; Nie, Z.J.; Xu, P. Integrated application of transcriptomics and metabolomics yields insights into population-asynchronous ovary development in Coilia Nasus. Sci. Rep. 2016, 6, 31835. [Google Scholar] [CrossRef] [PubMed]
- Browning, J.D.; Horton, J.D. Molecular mediators of hepatic steatosis and liver injury. J. Clin. Investig. 2004, 114, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Feng, M.J.; Li, Z.R.; Zhou, M.S.; Xu, L.N.; Pan, K.; Wang, S.X.; Su, W.; Zhang, W.Z. ETV5 regulates hepatic fatty acid metabolism through PPAR signaling pathway. Diabetes 2021, 70, 214–226. [Google Scholar] [CrossRef] [PubMed]
- Ravnskjaer, K.; Boergesen, M.; Rubi, B.; Larsen, J.K.; Nielsen, T.; Fridriksson, J.; Maechler, P.; Mandrup, S. Peroxisome proliferator-activated receptor α (PPARα) potentiates, whereas PPARγ attenuates, glucose-stimulated insulin secretion in pancreatic beta-cells. Endocrinology 2005, 146, 3266–3276. [Google Scholar] [CrossRef]
- Huang, Z.P.; He, W.; Zhou, X.Y.; Nicholson, A.C.; Gotto Jr, A.M.; Hajjar, D.P. Activation of PPARα and PPARγ induce expression of the hepatic LDL receptor. FASEB J. 2007, 21, A1137. [Google Scholar] [CrossRef]
- Takei, K.; Han, S.I.; Murayama, Y.; Satoh, A.; Oikawa, F.; Ohno, H.; Osaki, Y.; Matsuzaka, T.; Sekiya, M.; Iwasaki, H.; et al. Selective peroxisome proliferator-activated receptor-alpha modulator K-877 efficiently activates the peroxisome proliferator-activated receptor-α pathway and improves lipid metabolism in mice. J. Diabetes Investig. 2017, 8, 446–452. [Google Scholar] [CrossRef]
- Kersten, S. Integrated physiology and systems biology of PPARα. Mol. Metab. 2014, 3, 354–371. [Google Scholar] [CrossRef]
- Bernal-Mizrachi, C.; Weng, S.; Feng, C.; Finck, B.N.; Knutsen, R.H.; Leone, T.C.; Coleman, T.; Mecham, R.P.; Kelly, D.P.; Semenkovich, C.F. Dexamethasone induction of hypertension and diabetes is PPAR-α dependent in LDL receptor-null mice. Nat. Med. 2003, 9, 1069–1075. [Google Scholar] [CrossRef]
- Li, S.; Huang, Q.; Zhang, L.; Qiao, X.; Zhang, Y.; Tang, F.; Li, Z. Effect of CAPE-pNO2 against type 2 diabetes mellitus via the AMPK/GLUT4/GSK3β/PPARα pathway in HFD/STZ-induced diabetic mice. Eur. J. Pharmacol. 2019, 853, 1–10. [Google Scholar] [CrossRef]
- Han, K.L.; Choi, J.S.; Lee, J.Y.; Song, J.; Joe, M.K.; Jung, M.H.; Hwang, J.K. Therapeutic potential of peroxisome proliferators-activated receptor-α/γ dual agonist with alleviation of endoplasmic reticulum stress for the treatment of diabetes. Diabetes 2008, 57, 737–745. [Google Scholar] [CrossRef]
- Gross, B.; Pawlak, M.; Lefebvre, P.; Staels, B. PPARs in obesity-induced T2DM, dyslipidaemia and NAFLD. Nat. Rev. Endocrinol. 2017, 13, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Sydow, K.; Mondon, C.E.; Schrader, J.; Konishi, H.; Cooke, J.P. Dimethylarginine dimethylaminohydrolase overexpression enhances insulin sensitivity. Arterioscl. Throm. Vas. Biol. 2008, 28, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Cassader, M. Recent insights into hepatic lipid metabolism in non-alcoholic fatty liver disease (NAFLD). Prog. Lipid Res. 2009, 48, 1–26. [Google Scholar] [CrossRef]
- Konings, E.; Corpeleijn, E.; Bouwman, F.G.; Mariman, E.C.; Blaak, E.E. Expression of genes involved in lipid metabolism in men with impaired glucose tolerance: Impact of insulin stimulation and weight loss. J. Nutrigenet. Nutrigenom. 2010, 3, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Frederico, M.J.; Vitto, M.F.; Cesconetto, P.A.; Engelmann, J.; De Souza, D.R.; Luz, G.; Pinho, R.A.; Ropelle, E.R.; Cintra, D.E.; De Souza, C.T. Short-term inhibition of SREBP-1c expression reverses diet-induced non-alcoholic fatty liver disease in mice. Scand. J. Gastroenterol. 2011, 46, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Munoz, G.; Ovilo, C.; Noguera, J.L.; Sanchez, A.; Rodriguez, C.; Silio, L. Assignment of the fatty acid synthase (FASN) gene to pig chromosome 12 by physical and linkage mapping. Anim. Genet. 2003, 34, 234–235. [Google Scholar] [CrossRef] [PubMed]
- Mehmood, A.; Zhao, L.; Wang, Y.; Pan, F.; Hao, S.; Zhang, H.; Iftikhar, A.; Usman, M. Dietary anthocyanins as potential natural modulators for the prevention and treatment of non-alcoholic fatty liver disease: A comprehensive review. Food Res. Int. 2021, 142, 110180. [Google Scholar] [CrossRef]
- Ho, C.K.; Gao, Y.; Zheng, D.N.; Liu, Y.J.; Shan, S.Z.; Fang, B.; Zhao, Y.X.; Song, D.Z.; Zhang, Y.F.; Li, Q.F. Alisol A attenuates high-fat-diet-induced obesity and metabolic disorders via the AMPK/ACC/SREBP-1c pathway. J. Cell. Mol. Med. 2019, 23, 5108–5118. [Google Scholar] [CrossRef]
- Semple, R.K.; Sleigh, A.; Murgatroyd, P.R.; Adams, C.A.; Bluck, L.; Jackson, S.; Vottero, A.; Kanabar, D.; Charlton-Menys, V.; Durrington, P.; et al. Postreceptor insulin resistance contributes to human dyslipidemia and hepatic steatosis. J. Clin. Investig. 2009, 119, 315–322. [Google Scholar] [CrossRef]
- Zhang, Z.; Liang, X.; Tong, L.; Lv, Y.; Yi, H.; Gong, P.; Tian, X.; Cui, Q.; Liu, T.; Zhang, L. Effect of Inonotus obliquus (Fr.) Pilat extract on the regulation of glycolipid metabolism via PI3K/Akt and AMPK/ACC pathways in mice. J. Ethnopharmacol. 2021, 273, 113963. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Balsa-Canto, E.; Cicin-Sain, D.; Hoermann, A.; Janssens, H.; Banga, J.R.; Jaeger, J. Reverse-engineering post-transcriptional regulation of gap genes in Drosophila melanogaster. PLoS Comput. Biol. 2013, 9, e1003281. [Google Scholar] [CrossRef] [PubMed]
- Surkova, S.; Sokolkova, A.; Kozlov, K.; Nuzhdin, S.V.; Samsonova, M. Quantitative analysis reveals genotype- and domain- specific differences between mRNA and protein expression of segmentation genes in Drosophila. Dev. Biol. 2019, 448, 48–58. [Google Scholar] [CrossRef] [PubMed]

| Gene Names | Forward Primer (5′-3′) | Reverse Primer (5′-3′) |
|---|---|---|
| PPARα | AATGAACGTGCAATCCGATTTG | ACTCCACATTTGCGTAATTGTTG |
| PPARγ | GGAAGACCACTCGCATTCCTT | GTAATCAGCAACCATTGGGTCA |
| ACC | AATGAACGTGCAATCCGATTTG | ACTCCACATTTGCGTAATTGTTG |
| FASN | AGGTGGTGATAGCCGGTATGT | TGGGTAATCCATAGAGCCCAG |
| SREBP | CTTTGGCCTCGCTTTTCGG | TGGGTCCAATTAGAGCCATCTC |
| β-Actin | GTGCTATGTTGCTCTAGACTTCG | ATGCCACAGGATTCCATACC |
| Time (Week) | Body Weight (g) * | ||||
|---|---|---|---|---|---|
| N | M | P | C1 | C4 | |
| 1 | 20.18 ± 1.08 b | 33.11 ± 0.13 a | 33.81 ± 1.01 a | 33.41 ± 0.56 a | 33.27 ± 0.96 a |
| 2 | 21.76 ± 0.54 c | 42.09 ± 0.92 a | 40.67 ± 0.95 ab | 39.53 ± 1.05 b | 39.36 ± 1.10 b |
| 3 | 21.56 ± 2.00 c | 45.10 ± 0.60 a | 41.28 ± 1.44 b | 41.88 ± 0.97 b | 42.65 ± 0.94 ab |
| 4 | 23.31 ± 1.42 c | 47.61 ± 0.70 a | 43.43 ± 0.81 b | 43.81 ± 1.01 b | 45.24 ± 0.70 b |
| 5 | 23.30 ± 1.18 c | 49.86 ± 1.46 a | 46.42 ± 1.14 b | 46.39 ± 0.69 b | 48.45 ± 0.93 ab |
| 6 | 24.37 ± 1.06 c | 53.31 ± 1.44 a | 49.23 ± 0.83 c | 48.25 ± 0.96 c | 52.58 ± 1.30 b |
| 7 | 24.54 ± 0.89 e | 55.56 ± 0.90 a | 51.52 ± 1.01 c | 49.30 ± 0.95 d | 53.38 ± 0.89 b |
| 8 | 24.43 ± 0.71 c | 55.51 ± 0.62 a | 51.44 ± 1.34 b | 50.64 ± 1.14 b | 52.63 ± 1.23 b |
| Time (Week) | FBG (mmol/L) * | ||||
|---|---|---|---|---|---|
| N | M | P | C1 | C4 | |
| 0 | 4.58 ± 1.16 b | 9.84 ± 2.67 a | 9.05 ± 1.43 a | 9.45 ± 1.09 a | 9.64 ± 0.91 a |
| 4 | 5.37 ± 0.66 c | 20.14 ± 4.92 ab | 23.13 ± 7.40 a | 12.87 ± 0.31 bc | 14.57 ± 3.13 b |
| 8 | 5.38 ± 0.92 c | 21.77 ± 4.06 a | 14.93 ± 3.84 b | 10.39 ± 0.73 bc | 11.73 ± 1.91 b |
| Sample | Reads No. | Bases (bp) | Q30 (bp) | N (%) | Q20 (%) * | Q30 (%) * |
|---|---|---|---|---|---|---|
| M_1 | 49989464 | 7498419600 | 6995602942 | 0.000356 | 97.36 | 93.29 |
| M_2 | 54246640 | 8136996000 | 7628038842 | 0.000342 | 97.58 | 93.74 |
| M_3 | 45603244 | 6840486600 | 6382261682 | 0.000341 | 97.37 | 93.3 |
| C1_1 | 52733304 | 7909995600 | 7408232317 | 0.000355 | 97.55 | 93.65 |
| C1_2 | 51074184 | 7661127600 | 7183401187 | 0.00036 | 97.6 | 93.76 |
| C1_3 | 43787058 | 6568058700 | 5993737424 | 0.000129 | 96.73 | 91.25 |
| C4_1 | 44626308 | 6693946200 | 6266481249 | 0.000357 | 97.47 | 93.61 |
| C4_2 | 45570930 | 6835639500 | 6405171513 | 0.000356 | 97.54 | 93.7 |
| C4_3 | 56577088 | 8486563200 | 7934581869 | 0.000347 | 97.47 | 93.49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, Y.; Tan, S.; Ren, T.; Yu, L.; Li, P.; Xie, G.; Chen, C.; Yuan, M.; Xu, Q.; Chen, Z. Transcriptomics Reveals the Mechanism of Rosa roxburghii Tratt Ellagitannin in Improving Hepatic Lipid Metabolism Disorder in db/db Mice. Nutrients 2023, 15, 4187. https://doi.org/10.3390/nu15194187
Tan Y, Tan S, Ren T, Yu L, Li P, Xie G, Chen C, Yuan M, Xu Q, Chen Z. Transcriptomics Reveals the Mechanism of Rosa roxburghii Tratt Ellagitannin in Improving Hepatic Lipid Metabolism Disorder in db/db Mice. Nutrients. 2023; 15(19):4187. https://doi.org/10.3390/nu15194187
Chicago/Turabian StyleTan, Yunyun, Shuming Tan, Tingyuan Ren, Lu Yu, Pei Li, Guofang Xie, Chao Chen, Meng Yuan, Qing Xu, and Zhen Chen. 2023. "Transcriptomics Reveals the Mechanism of Rosa roxburghii Tratt Ellagitannin in Improving Hepatic Lipid Metabolism Disorder in db/db Mice" Nutrients 15, no. 19: 4187. https://doi.org/10.3390/nu15194187







