Serum Levels of Hormones Regulating Appetite in Patients with Fetal Alcohol Spectrum Disorders
Abstract
:1. Introduction
2. Materials and Methods
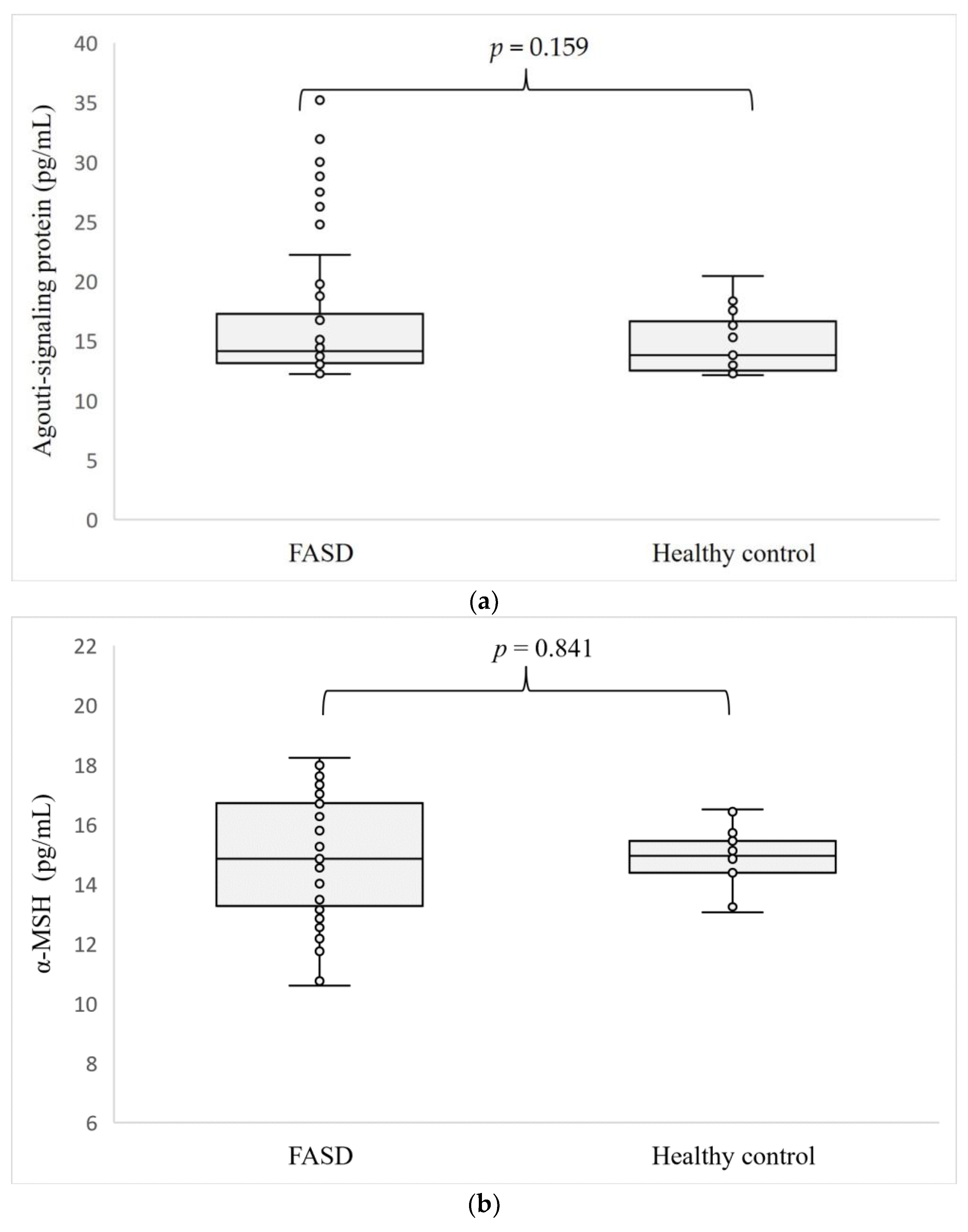
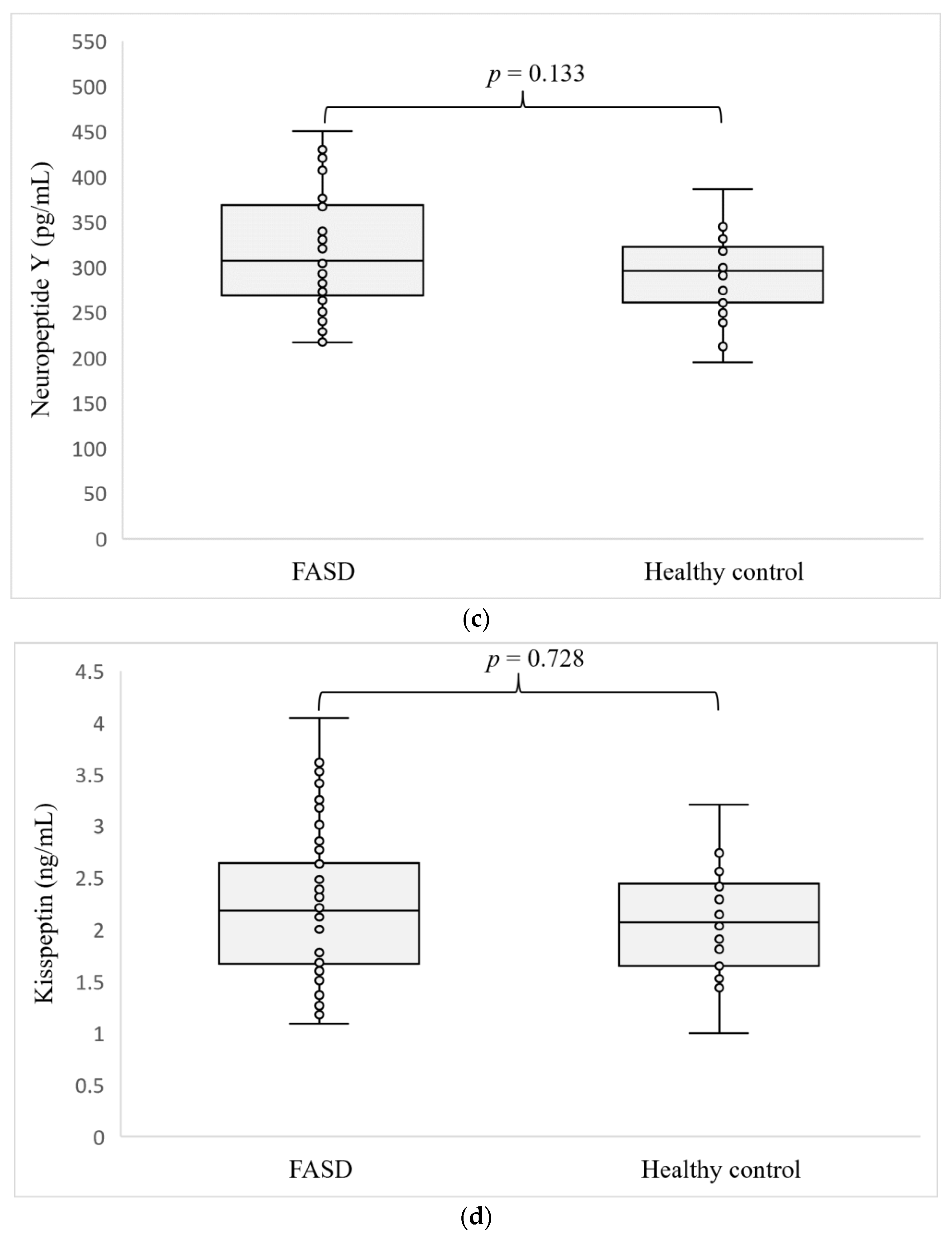
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jacobson, J.L.; Jacobson, S.W.; Sokol, R.J.; Martier, S.S.; Ager, J.W.; Kaplan-Estrin, M.G. Teratogenic Effects of Alcohol on Infant Development. Alcohol Clin. Exp. Res. 1993, 17, 174–183. [Google Scholar] [CrossRef]
- Jones, K.L. The Effects of Alcohol on Fetal Development. Birth Defects Res. Part C Embryo Today Rev. 2011, 93, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Dejong, K.; Olyaei, A.; Lo, J.O. Alcohol Use in Pregnancy. Clin. Obstet. Gynecol. 2019, 62, 142–155. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.; Probst, C.; Gmel, G.; Rehm, J.; Burd, L.; Popova, S. Global Prevalence of Fetal Alcohol Spectrum Disorder Among Children and Youth: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2017, 171, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.L.; Smith, D.W.; Ulleland, C.N.; Streissguth, P. Pattern of Malformation in Offspring of Chronic Alcoholic Mothers. Lancet Lond. Engl. 1973, 1, 1267–1271. [Google Scholar] [CrossRef]
- May, P.A.; Chambers, C.D.; Kalberg, W.O.; Zellner, J.; Feldman, H.; Buckley, D.; Kopald, D.; Hasken, J.M.; Xu, R.; Honerkamp-Smith, G.; et al. Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. JAMA 2018, 319, 474–482. [Google Scholar] [CrossRef] [PubMed]
- May, P.A.; Gossage, J.P.; Marais, A.-S.; Hendricks, L.S.; Snell, C.L.; Tabachnick, B.G.; Stellavato, C.; Buckley, D.G.; Brooke, L.E.; Viljoen, D.L. Maternal Risk Factors for Fetal Alcohol Syndrome and Partial Fetal Alcohol Syndrome in South Africa: A Third Study. Alcohol Clin. Exp. Res. 2008, 32, 738–753. [Google Scholar] [CrossRef]
- Chasnoff, I.J.; Wells, A.M.; King, L. Misdiagnosis and Missed Diagnoses in Foster and Adopted Children with Prenatal Alcohol Exposure. Pediatrics 2015, 135, 264–270. [Google Scholar] [CrossRef]
- Spohr, H.-L.; Steinhausen, H.-C. Fetal Alcohol Spectrum Disorders and Their Persisting Sequelae in Adult Life. Dtsch. Ärztebl. Int. 2008, 105, 693–698. [Google Scholar] [CrossRef]
- May, P.A.; Blankenship, J.; Marais, A.-S.; Gossage, J.P.; Kalberg, W.O.; Joubert, B.; Cloete, M.; Barnard, R.; De Vries, M.; Hasken, J.; et al. Maternal Alcohol Consumption Producing Fetal Alcohol Spectrum Disorders (FASD): Quantity, Frequency, and Timing of Drinking. Drug Alcohol Depend. 2013, 133, 502–512. [Google Scholar] [CrossRef]
- Oei, J.L. Alcohol Use in Pregnancy and Its Impact on the Mother and Child. Addiction 2020, 115, 2148–2163. [Google Scholar] [CrossRef]
- Hoyme, H.E.; Kalberg, W.O.; Elliott, A.J.; Blankenship, J.; Buckley, D.; Marais, A.-S.; Manning, M.A.; Robinson, L.K.; Adam, M.P.; Abdul-Rahman, O.; et al. Updated Clinical Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders. Pediatrics 2016, 138, e20154256. [Google Scholar] [CrossRef]
- Carter, R.C.; Jacobson, J.L.; Molteno, C.D.; Dodge, N.C.; Meintjes, E.M.; Jacobson, S.W. Fetal Alcohol Growth Restriction and Cognitive Impairment. Pediatrics 2016, 138, e20160775. [Google Scholar] [CrossRef]
- Amos-Kroohs, R.M.; Fink, B.A.; Smith, C.J.; Chin, L.; Van Calcar, S.C.; Wozniak, J.R.; Smith, S.M. Abnormal Eating Behaviors Are Common in Children with Fetal Alcohol Spectrum Disorder. J. Pediatr. 2016, 169, 194–200.e1. [Google Scholar] [CrossRef] [PubMed]
- Sampson, P.D.; Bookstein, F.L.; Barr, H.M.; Streissguth, A.P. Prenatal Alcohol Exposure, Birthweight, and Measures of Child Size from Birth to Age 14 Years. Am. J. Public Health 1994, 84, 1421–1428. [Google Scholar] [CrossRef]
- Carter, R.C.; Jacobson, J.L.; Sokol, R.J.; Avison, M.J.; Jacobson, S.W. Fetal Alcohol-Related Growth Restriction from Birth through Young Adulthood and Moderating Effects of Maternal Prepregnancy Weight. Alcohol Clin. Exp. Res. 2013, 37, 452–462. [Google Scholar] [CrossRef] [PubMed]
- Day, N.L.; Leech, S.L.; Richardson, G.A.; Cornelius, M.D.; Robles, N.; Larkby, C. Prenatal Alcohol Exposure Predicts Continued Deficits in Offspring Size at 14 Years of Age. Alcohol. Clin. Exp. Res. 2002, 26, 1584–1591. [Google Scholar] [CrossRef]
- Fuglestad, A.J.; Boys, C.J.; Chang, P.-N.; Miller, B.S.; Eckerle, J.K.; Deling, L.; Fink, B.A.; Hoecker, H.L.; Hickey, M.K.; Jimenez-Vega, J.M.; et al. Overweight and Obesity Among Children and Adolescents with Fetal Alcohol Spectrum Disorders. Alcohol Clin. Exp. Res. 2014, 38, 2502–2508. [Google Scholar] [CrossRef] [PubMed]
- Druce, M. The Regulation of Appetite. Arch. Dis. Child. 2005, 91, 183–187. [Google Scholar] [CrossRef]
- Wynne, K.; Stanley, S.; McGowan, B.; Bloom, S. Appetite Control. J. Endocrinol. 2005, 184, 291–318. [Google Scholar] [CrossRef]
- Okulicz-Kozaryn, K.; Maryniak, A.; Borkowska, M.; Śmigiel, R.; Dylag, K.A. Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals. Int. J. Environ. Res. Public. Health 2021, 18, 7526. [Google Scholar] [CrossRef] [PubMed]
- Astley, S.J. Validation of the Fetal Alcohol Spectrum Disorder (Fasd) 4-Digit Diagnostic Code. J. Popul. Ther. Clin. Pharmacol. 2013, 20, e416–e467. [Google Scholar]
- Cook, J.L.; Green, C.R.; Lilley, C.M.; Anderson, S.M.; Baldwin, M.E.; Chudley, A.E.; Conry, J.L.; LeBlanc, N.; Loock, C.A.; Lutke, J.; et al. Fetal Alcohol Spectrum Disorder: A Guideline for Diagnosis across the Lifespan. CMAJ 2016, 188, 191–197. [Google Scholar] [CrossRef]
- Bertrand, J.; Floyd, R.L.; Weber, M.K. Guidelines for Identifying and Referring Persons with Fetal Alcohol Syndrome. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2005, 54, 1–14. [Google Scholar]
- Podgórski, R.; Galiniak, S.; Mazur, A.; Domin, A. The Association of the Hypothalamic-Pituitary-Adrenal Axis with Appetite Regulation in Children with Fetal Alcohol Spectrum Disorders (FASDs). Nutrients 2023, 15, 1366. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw, S.L. Hypothalamic Proopiomelanocortin Processing and the Regulation of Energy Balance. Eur. J. Pharmacol. 2011, 660, 213–219. [Google Scholar] [CrossRef]
- Sohn, J.-W. Network of Hypothalamic Neurons That Control Appetite. BMB Rep. 2015, 48, 229–233. [Google Scholar] [CrossRef]
- Beck, B. Neuropeptides and Obesity. Nutrition 2000, 16, 916–923. [Google Scholar] [CrossRef]
- Iwasa, T.; Matsuzaki, T.; Kinouchi, R.; Gereltsetseg, G.; Murakami, M.; Nakazawa, H.; Yasui, T.; Irahara, M. Changes in the Responsiveness of Serum Leptin and Hypothalamic Neuropeptide Y mRNA Levels to Food Deprivation in Developing Rats. Int. J. Dev. Neurosci. 2011, 29, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.M.J.; Green, P.; Tapoulal, N.; Lewandowski, A.J.; Leeson, P.; Herring, N. The Role of Neuropeptide Y in Cardiovascular Health and Disease. Front. Physiol. 2018, 9, 1281. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Feder, A.; Wegener, G.; Bailey, C.; Saxena, S.; Charney, D.; Mathé, A.A. Central Functions of Neuropeptide Y in Mood and Anxiety Disorders. Expert Opin. Ther. Targets 2011, 15, 1317–1331. [Google Scholar] [CrossRef] [PubMed]
- Schmeltzer, S.N.; Herman, J.P.; Sah, R. Neuropeptide Y (NPY) and Posttraumatic Stress Disorder (PTSD): A Translational Update. Exp. Neurol. 2016, 284, 196–210. [Google Scholar] [CrossRef]
- Thorsell, A.; Mathé, A.A. Neuropeptide Y in Alcohol Addiction and Affective Disorders. Front. Endocrinol. 2017, 8, 178. [Google Scholar] [CrossRef] [PubMed]
- Nyström, F.; Nilsson, P.; Olsson, A.G.; Karlberg, B.E.; Ohman, K.P. A Population Study of Plasma Neuropeptide Y: Correlations with Components of the Metabolic Syndrome. Blood Press. 1996, 5, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Gendall, K.A.; Kaye, W.H.; Altemus, M.; McConaha, C.W.; La Via, M.C. Leptin, Neuropeptide Y, and Peptide YY in Long-Term Recovered Eating Disorder Patients. Biol. Psychiatry 1999, 46, 292–299. [Google Scholar] [CrossRef]
- Sedlackova, D.; Kopeckova, J.; Papezova, H.; Hainer, V.; Kvasnickova, H.; Hill, M.; Nedvidkova, J. Comparison of a High-Carbohydrate and High-Protein Breakfast Effect on Plasma Ghrelin, Obestatin, NPY and PYY Levels in Women with Anorexia and Bulimia Nervosa. Nutr. Metab. 2012, 9, 52. [Google Scholar] [CrossRef]
- Baltazi, M.; Katsiki, N.; Savopoulos, C.; Iliadis, F.; Koliakos, G.; Hatzitolios, A.I. Plasma Neuropeptide Y (NPY) and Alpha-Melanocyte Stimulating Hormone (a-MSH) Levels in Patients with or without Hypertension and/or Obesity: A Pilot Study. Am. J. Cardiovasc. Dis. 2011, 1, 48–59. [Google Scholar]
- Baranowska, B.; Radzikowska, M.; Wasilewska-Dziubińska, E.; Kapliński, A.; Roguski, K.; Płonowski, A. Neuropeptide Y, Leptin, Galanin and Insulin in Women with Polycystic Ovary Syndrome. Gynecol. Endocrinol. Off. J. Int. Soc. Gynecol. Endocrinol. 1999, 13, 344–351. [Google Scholar] [CrossRef]
- Guevara, A.; Gates, H.; Urbina, B.; French, R. Developmental Ethanol Exposure Causes Reduced Feeding and Reveals a Critical Role for Neuropeptide F in Survival. Front. Physiol. 2018, 9, 237. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, T.; Matsuzaki, T.; Yano, K.; Tungalagsuvd, A.; Munkhzaya, M.; Mayila, Y.; Kuwahara, A.; Irahara, M. The Effects of Prenatal Undernutrition and a High-Fat Postnatal Diet on Central and Peripheral Orexigenic and Anorexigenic Factors in Female Rats. Endocr. J. 2017, 64, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Thangaratnarajah, C.; Dinger, K.; Vohlen, C.; Klaudt, C.; Nawabi, J.; Lopez Garcia, E.; Kwapiszewska, G.; Dobner, J.; Nüsken, K.D.; van Koningsbruggen-Rietschel, S.; et al. Novel Role of NPY in Neuroimmune Interaction and Lung Growth after Intrauterine Growth Restriction. Am. J. Physiol. Lung Cell. Mol. Physiol. 2017, 313, L491–L506. [Google Scholar] [CrossRef] [PubMed]
- Sebastiani, G.; Borrás-Novell, C.; Casanova, M.A.; Pascual Tutusaus, M.; Ferrero Martínez, S.; Gómez Roig, M.D.; García-Algar, O. The Effects of Alcohol and Drugs of Abuse on Maternal Nutritional Profile during Pregnancy. Nutrients 2018, 10, 1008. [Google Scholar] [CrossRef] [PubMed]
- Dinparastisaleh, R.; Mirsaeidi, M. Antifibrotic and Anti-Inflammatory Actions of α-Melanocytic Hormone: New Roles for an Old Player. Pharmaceuticals 2021, 14, 45. [Google Scholar] [CrossRef] [PubMed]
- Shelkar, G.P.; Kale, A.D.; Singh, U.; Singru, P.S.; Subhedar, N.K.; Kokare, D.M. Alpha-Melanocyte Stimulating Hormone Modulates Ethanol Self-Administration in Posterior Ventral Tegmental Area through Melanocortin-4 Receptors. Addict. Biol. 2015, 20, 302–315. [Google Scholar] [CrossRef]
- Kokare, D.M.; Kyzar, E.J.; Zhang, H.; Sakharkar, A.J.; Pandey, S.C. Adolescent Alcohol Exposure-Induced Changes in Alpha-Melanocyte Stimulating Hormone and Neuropeptide Y Pathways via Histone Acetylation in the Brain During Adulthood. Int. J. Neuropsychopharmacol. 2017, 20, 758–768. [Google Scholar] [CrossRef]
- Rainero, I.; De Gennaro, T.; Visentin, G.; Brunetti, E.; Cerrato, P.; Torre, E.; Portaleone, P.; Pinessi, L. Effects of Chronic Ethanol Treatment on Alpha-MSH Concentrations in Rat Brain and Pituitary. Neuropeptides 1990, 15, 139–141. [Google Scholar] [CrossRef]
- Katsuki, A.; Sumida, Y.; Murashima, S.; Furuta, M.; Araki-Sasaki, R.; Tsuchihashi, K.; Hori, Y.; Yano, Y.; Adachi, Y. Elevated Plasma Levels of Alpha-Melanocyte Stimulating Hormone (Alpha-MSH) Are Correlated with Insulin Resistance in Obese Men. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2000, 24, 1260–1264. [Google Scholar] [CrossRef]
- Hoggard, N.; Johnstone, A.M.; Faber, P.; Gibney, E.R.; Elia, M.; Lobley, G.; Rayner, V.; Horgan, G.; Hunter, L.; Bashir, S.; et al. Plasma Concentrations of α-MSH, AgRP and Leptin in Lean and Obese Men and Their Relationship to Differing States of Energy Balance Perturbation. Clin. Endocrinol. 2004, 61, 31–39. [Google Scholar] [CrossRef]
- Mao, Z.; Liu, G.; Chen, J.-J.; Liu, D.; Xu, M.-P.; Zhao, C.; Yang, H.-T.; Yue, Y.-B. Serum α-Melanocyte-Stimulating Hormone May Act as a Protective Biomarker for Non-Traumatic Osteonecrosis of the Femoral Head. Ann. Clin. Biochem. 2018, 55, 453–460. [Google Scholar] [CrossRef]
- Du, X.; Dong, B.; Li, C.; Zhang, F.; Ji, Y.; Zhang, J.; Yin, C. Dynamic Changes of α-Melanocyte-Stimulating Hormone Levels in the Serum of Patients with Craniocerebral Trauma. Exp. Ther. Med. 2017, 14, 2511–2516. [Google Scholar] [CrossRef]
- Donahoo, W.T.; Hernandez, T.L.; Costa, J.L.; Jensen, D.R.; Morris, A.M.; Brennan, M.B.; Hochgeschwender, U.; Eckel, R.H. Plasma α–Melanocyte-Stimulating Hormone: Sex Differences and Correlations with Obesity. Metabolism 2009, 58, 16–21. [Google Scholar] [CrossRef]
- Voisey, J.; van Daal, A. Agouti: From Mouse to Man, from Skin to Fat. Pigment Cell Res. 2002, 15, 10–18. [Google Scholar] [CrossRef]
- Page-Wilson, G.; Meece, K.; White, A.; Rosenbaum, M.; Leibel, R.L.; Smiley, R.; Wardlaw, S.L. Proopiomelanocortin, Agouti-Related Protein, and Leptin in Human Cerebrospinal Fluid: Correlations with Body Weight and Adiposity. Am. J. Physiol.-Endocrinol. Metab. 2015, 309, E458–E465. [Google Scholar] [CrossRef] [PubMed]
- Kempf, E.; Landgraf, K.; Stein, R.; Hanschkow, M.; Hilbert, A.; Abou Jamra, R.; Boczki, P.; Herberth, G.; Kühnapfel, A.; Tseng, Y.-H.; et al. Aberrant Expression of Agouti Signaling Protein (ASIP) as a Cause of Monogenic Severe Childhood Obesity. Nat. Metab. 2022, 4, 1697–1712. [Google Scholar] [CrossRef]
- Liu, Y.; Albrecht, E.; Schering, L.; Kuehn, C.; Yang, R.; Zhao, Z.; Maak, S. Agouti Signaling Protein and Its Receptors as Potential Molecular Markers for Intramuscular and Body Fat Deposition in Cattle. Front. Physiol. 2018, 9, 172. [Google Scholar] [CrossRef] [PubMed]
- Galiniak, S.; Podgórski, R.; Rachel, M.; Mazur, A. Serum Levels of Hormones Regulating Appetite in Patients with Cystic Fibrosis − a Single-Center, Cross-Sectional Study. Front. Endocrinol. 2022, 13, 992667. [Google Scholar] [CrossRef]
- Han, S.-K.; Gottsch, M.L.; Lee, K.J.; Popa, S.M.; Smith, J.T.; Jakawich, S.K.; Clifton, D.K.; Steiner, R.A.; Herbison, A.E. Activation of Gonadotropin-Releasing Hormone Neurons by Kisspeptin as a Neuroendocrine Switch for the Onset of Puberty. J. Neurosci. 2005, 25, 11349–11356. [Google Scholar] [CrossRef]
- Zeydabadi Nejad, S.; Ramezani Tehrani, F.; Zadeh-Vakili, A. The Role of Kisspeptin in Female Reproduction. Int. J. Endocrinol. Metab. 2017, 15, e44337. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.J.; Anderson, G.M. Balancing Ovulation and Anovulation: Integration of the Reproductive and Energy Balance Axes by Neuropeptides. Hum. Reprod. Update 2012, 18, 313–332. [Google Scholar] [CrossRef]
- Pasquali, R.; Patton, L.; Gambineri, A. Obesity and Infertility. Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 482. [Google Scholar] [CrossRef]
- Yang, L.; Demetriou, L.; Wall, M.B.; Mills, E.G.; Wing, V.C.; Thurston, L.; Schaufelberger, C.N.; Owen, B.M.; Abbara, A.; Rabiner, E.A.; et al. The Effects of Kisspeptin on Brain Response to Food Images and Psychometric Parameters of Appetite in Healthy Men. J. Clin. Endocrinol. Metab. 2020, 106, 1837–1848. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.S.; Vu, J.P.; Oh, S.; Sanford, D.; Pisegna, J.R.; Germano, P. Intraperitoneal Treatment of Kisspeptin Suppresses Appetite and Energy Expenditure and Alters Gastrointestinal Hormones in Mice. Dig. Dis. Sci. 2020, 65, 2254–2263. [Google Scholar] [CrossRef] [PubMed]
- Luedde, M.; Spehlmann, M.E.; Hippe, H.-J.; Loosen, S.H.; Roy, S.; Vargas Cardenas, D.; Vucur, M.; Frey, N.; Koch, A.; Luedde, T.; et al. Serum Levels of Kisspeptin Are Elevated in Critically Ill Patients. PLoS ONE 2018, 13, e0206064. [Google Scholar] [CrossRef]
- Dudek, M.; Ziarniak, K.; Sliwowska, J.H. Kisspeptin and Metabolism: The Brain and Beyond. Front. Endocrinol. 2018, 9, 145. [Google Scholar] [CrossRef]
- Sitticharoon, C.; Mutirangura, P.; Chinachoti, T.; Iamaroon, A.; Triyasunant, N.; Churintaraphan, M.; Keadkraichaiwat, I.; Maikaew, P.; Sririwichitchai, R. Associations of Serum Kisspeptin Levels with Metabolic and Reproductive Parameters in Men. Peptides 2021, 135, 170433. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.J.; Li, S.J.; Pan, H.; Li, N.; Zhang, D.X.; Wang, L.J.; Yang, H.B.; Wu, Q.; Gong, F.Y. The Changes of Serum Leptin and Kisspeptin Levels in Chinese Children and Adolescents in Different Pubertal Stages. Int. J. Endocrinol. 2016, 2016, e6790794. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.L.; Lehman, M.N.; Smith, J.T.; Coolen, L.M.; de Oliveira, C.V.R.; Jafarzadehshirazi, M.R.; Pereira, A.; Iqbal, J.; Caraty, A.; Ciofi, P.; et al. Kisspeptin Neurons in the Arcuate Nucleus of the Ewe Express Both Dynorphin A and Neurokinin B. Endocrinology 2007, 148, 5752–5760. [Google Scholar] [CrossRef]
- Hrabovszky, E.; Ciofi, P.; Vida, B.; Horvath, M.C.; Keller, E.; Caraty, A.; Bloom, S.R.; Ghatei, M.A.; Dhillo, W.S.; Liposits, Z.; et al. The Kisspeptin System of the Human Hypothalamus: Sexual Dimorphism and Relationship with Gonadotropin-Releasing Hormone and Neurokinin B Neurons. Eur. J. Neurosci. 2010, 31, 1984–1998. [Google Scholar] [CrossRef]
- Bond, J.-A.P.D.; Smith, J.T. Kisspeptin and Energy Balance in Reproduction. Reproduction 2014, 147, R53–R63. [Google Scholar] [CrossRef]
- Demirbilek, H.; Gonc, E.N.; Ozon, A.; Alikasifoglu, A.; Kandemir, N. Evaluation of Serum Kisspeptin Levels in Girls in the Diagnosis of Central Precocious Puberty and in the Assessment of Pubertal Suppression. J. Pediatr. Endocrinol. Metab. JPEM 2012, 25, 313–316. [Google Scholar] [CrossRef]
- Li, M.; Chen, Y.; Liao, B.; Tang, J.; Zhong, J.; Lan, D. The Role of Kisspeptin and MKRN3 in the Diagnosis of Central Precocious Puberty in Girls. Endocr. Connect. 2021, 10, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Akison, L.K.; Moritz, K.M.; Reid, N. Adverse Reproductive Outcomes Associated with Fetal Alcohol Exposure: A Systematic Review. Reprod. Camb. Engl. 2019, 157, 329–343. [Google Scholar] [CrossRef]
- Sliwowska, J.H.; Comeau, W.L.; Bodnar, T.S.; Ellis, L.; Weinberg, J. Prenatal Alcohol Exposure and Pair Feeding Differentially Impact Puberty and Reproductive Development in Female Rats: Role of the Kisspeptin System. Alcohol. Clin. Exp. Res. 2016, 40, 2368–2376. [Google Scholar] [CrossRef] [PubMed]
- Sliwowska, J.H.; Bodnar, T.S.; Weinberg, J. Prenatal Alcohol Exposure Alters Response of Kisspeptin-Ir Neurons to Estradiol and Progesterone in Adult Female Rats. Alcohol. Clin. Exp. Res. 2014, 38, 2780–2789. [Google Scholar] [CrossRef]
- Lee, E.B.; Dilower, I.; Marsh, C.A.; Wolfe, M.W.; Masumi, S.; Upadhyaya, S.; Rumi, M.A.K. Sexual Dimorphism in Kisspeptin Signaling. Cells 2022, 11, 1146. [Google Scholar] [CrossRef]
- De Freitas, R.S.; França, T.F.A.; Pompeia, S. Sex-Specific Association between Urinary Kisspeptin and Pubertal Development. Endocr. Connect. 2022, 11, e220165. [Google Scholar] [CrossRef] [PubMed]
- Jayasena, C.N.; Nijher, G.M.; Narayanaswamy, S.; Silva, A.D.; Abbara, A.; Ghatei, M.A.; Bloom, S.R.; Bridges, N.; Dhillo, W.S. Age-Dependent Elevations in Plasma Kisspeptin Are Observed in Boys and Girls When Compared with Adults. Ann. Clin. Biochem. 2014, 51, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Roth, C.L.; Enriori, P.J.; Gebhardt, U.; Hinney, A.; Müller, H.L.; Hebebrand, J.; Reinehr, T.; Cowley, M.A. Changes of Peripheral α-Melanocyte–Stimulating Hormone in Childhood Obesity. Metab.—Clin. Exp. 2010, 59, 186–194. [Google Scholar] [CrossRef]
- Dâmaso, A.R.; de Piano, A.; Campos, R.M.d.S.; Corgosinho, F.C.; Siegfried, W.; Caranti, D.A.; Masquio, D.C.L.; Carnier, J.; Sanches, P.; Leão da Silva, P.; et al. Multidisciplinary Approach to the Treatment of Obese Adolescents: Effects on Cardiovascular Risk Factors, Inflammatory Profile, and Neuroendocrine Regulation of Energy Balance. Int. J. Endocrinol. 2013, 2013, 541032. [Google Scholar] [CrossRef]
- Katsuki, A.; Sumida, Y.; Gabazza, E.C.; Murashima, S.; Tanaka, T.; Furuta, M.; Araki-Sasaki, R.; Hori, Y.; Nakatani, K.; Yano, Y.; et al. Plasma Levels of Agouti-Related Protein Are Increased in Obese Men. J. Clin. Endocrinol. Metab. 2001, 86, 1921–1924. [Google Scholar] [CrossRef]
- Chen, H.; Hansen, M.J.; Jones, J.E.; Vlahos, R.; Bozinovski, S.; Anderson, G.P.; Morris, M.J. Cigarette Smoke Exposure Reprograms the Hypothalamic Neuropeptide Y Axis to Promote Weight Loss. Am. J. Respir. Crit. Care Med. 2006, 173, 1248–1254. [Google Scholar] [CrossRef]
- Chen, H.; Hansen, M.J.; Jones, J.E.; Vlahos, R.; Bozinovski, S.; Anderson, G.P.; Morris, M.J. Regulation of Hypothalamic NPY by Diet and Smoking. Peptides 2007, 28, 384–389. [Google Scholar] [CrossRef]
- Pain, S.; Brot, S.; Gaillard, A. Neuroprotective Effects of Neuropeptide Y against Neurodegenerative Disease. Curr. Neuropharmacol. 2022, 20, 1717–1725. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.K.; Szczepanik, M.; Trypuć, M.; Pogorzelski, A.; Bobkowski, W.; Grytczuk, M.; Minarowska, A.; Wójciak, R.; Walkowiak, J. Circulating Brain-Derived Neurotrophic Factor, Leptin, Neuropeptide Y, and Their Clinical Correlates in Cystic Fibrosis: A Cross-Sectional Study. Arch. Med. Sci. AMS 2020, 16, 1049–1056. [Google Scholar] [CrossRef]
- Huang, Q.; Liao, J.; Liu, Y.; Liang, H.; Ma, P.; Pan, J. Plasma Neuropeptide Y Levels in Chinese Patients with Primary Insomnia. Sleep Breath. 2015, 19, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Rhie, Y.J.; Lee, K.H.; Eun, S.H.; Choi, B.M.; Chae, H.W.; Kwon, A.R.; Lee, W.J.; Kim, J.H.; Kim, H.-S. Serum Kisspeptin Levels in Korean Girls with Central Precocious Puberty. J. Korean Med. Sci. 2011, 26, 927–931. [Google Scholar] [CrossRef]
- Mancini, A.; Currò, D.; Cipolla, C.; Barini, A.; Bruno, C.; Vergani, E.; Di Segni, C.; Guidi, F.; Nicolotti, N.; Silvestrini, A.; et al. Evaluation of Kisspeptin Levels in Prepubertal Obese and Overweight Children: Sexual Dimorphism and Modulation of Antioxidant Levels. Eur. Rev. 2021, 25, 941–949. [Google Scholar]
| FASD | Healthy Controls | p Value | ||
|---|---|---|---|---|
| Sex (F/M) | 29/28 | 7/16 | ||
| Age (years) | Mean ± SD | 8.01 ± 3.95 | 7.45 ± 5.12 | 0.526 |
| range | 1.83–16.5 | 0.42–17 | ||
| BMI percentile | Mean ± SD | 32.29 ± 31.79 | 60.71 ± 27.03 | 0.037 |
| range | 0.1–99.9 | 12–99 | ||
| Clinical laboratory markers | ||||
| Cholesterol (mg/dL) Norm < 190 | Median | 158 | 155 | 0.929 |
| Range | 76–244 | 126–191 | ||
| LDL (mg/dL) Norm < 135 | Median | 90.5 | 95 | 0.848 |
| Range | 31–163 | 72–104 | ||
| HDL (mg/dL) Norm > 40 | Median | 53 | 53 | 0.948 |
| Range | 24–108 | 42–59 | ||
| Triglycerides (mg/dL) Norm < 150 | Median | 67 | 65 | 0.828 |
| Range | 30–241 | 38–141 | ||
| Glucose (mg/dL) Norm (70–99) | Median | 85.5 | 87 | 0.829 |
| Range | 72–99 | 6–94 | ||
| Insulin (mIU/mL) Norm < 15 | Median | 5.03 | 2.05 | 0.156 |
| Range | 1.41–16.46 | 1.0–9.03 | ||
| HbA1c (%) Normal range (4–6) | Median | 5.38 | 5.41 | 0.801 |
| Range | 4.81–5.86 | 5.26–5.55 | ||
| HOMA-IR Norm < 2.5 | Median | 1.05 | 0.78 | 0.223 |
| Range | 0.27–3.62 | 0.21–2.03 | ||
| FAS | ND-PAE | p Value | ||
|---|---|---|---|---|
| Sex (F/M) | 14/12 | 15/16 | ||
| Age (years) | Mean ± SD | 7.91 ± 4.77 | 8.13 ± 3.32 | 0.843 |
| range | 0.42–16 | 2.08–13.5 | ||
| BMI percentile | Mean ± SD | 22.12 ± 27.51 | 42.04 ± 33.02 | 0.02 |
| range | 0.1–78 | 0.1–99.9 | ||
| Clinical Laboratory Markers | ||||
| Cholesterol (mg/dL) Norm < 190 | Median | 154. | 161 | 0.110 |
| Range | 76–238 | 114–244 | ||
| LDL (mg/dL) Norm < 135 | Median | 86 | 75 | 0.365 |
| Range | 31–143 | 114–244 | ||
| HDL (mg/dL) Norm > 40 | Median | 49.5 | 53 | 0.382 |
| Range | 33–80 | 24–108 | ||
| Triglycerides (mg/dL) Norm < 150 | Median | 64 | 75 | 0.607 |
| Range | 30–229 | 34–241 | ||
| Glucose (mg/dL) Norm (70–99) | Median | 82 | 87 | 0.211 |
| Range | 72–99 | 74–99 | ||
| Insulin (mIU/mL) Norm < 15 mIU/ml | Median | 5.1 | 4.22 | 0.623 |
| Range | 1.41–16.46 | 1.56–13.97 | ||
| HbA1c (%) Normal range (4–6) | Median | 5.24 | 5.45 | 0.039 |
| Range | 4.81–5.86 | 4.89–5.85 | ||
| HOMA-IR Norm < 2.5 | Median | 1.07 | 1.29 | 0.79 |
| Range | 0.27–3.62 | 0.31–3.53 | ||
| FAS | ND-PAE | p Value | ||
|---|---|---|---|---|
| Agouti-signaling protein (pg/mL) | Median | 14.02 | 14.59 | 0.59 |
| Range | 12.22–35.18 | 12.18–32.28 | ||
| Neuropeptide Y (pg/mL) | Median | 316.22 | 303.82 | 0.278 |
| Range | 216.75–429.7 | 217.4–430.3 | ||
| α-MSH (pg/ml) | Median | 15.44 | 13.65 | 0.071 |
| Range | 12.16–18.23 | 10.59–17.99 | ||
| KISS1 (ng/mL) | Median | 2.03 | 2.16 | 0.585 |
| Range | 1.18–4.04 | 1.09–3.65 |
| Hormone | FASD | |||
|---|---|---|---|---|
| Female | Male | p Value | ||
| Agouti-signaling protein (pg/mL) | Median | 13.86 | 14.27 | 0.856 |
| Range | 12.22–32.28 | 12.18–35.18 | ||
| Neuropeptide Y (pg/mL) | Median | 306.9 | 307.25 | 0.596 |
| Range | 217.4–429.7 | 216.75–450.4 | ||
| α-MSH (pg/mL) | Median | 15.43 | 14.27 | 0.173 |
| Range | 11.85–18.23 | 10.59–17.99 | ||
| KISS1 (ng/mL) | Median | 7.3 | 9.8 | 0.169 |
| Range | 3.5–18.9 | 5–26 | ||
| Age | BMI per | Cortisol | ACTH | Ch | LDL | HDL | TGL | Glu | Ins | HOMA-IR | HbA1c | KISS1 | ASP | NPY | α-MSH | POMC | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| KISS1 | R | −0.119 | 0.244 | −0.008 | 0.095 | 0.115 | 0.066 | −0.025 | 0.151 | −0.151 | 0.04 | 0.049 | 0.064 | 0.046 | 0.042 | −0.065 | 0.121 | |
| p | 0.359 | 0.065 | 0.952 | 0.583 | 0.376 | 0.613 | 0.849 | 0.246 | 0.257 | 0.772 | 0.723 | 0.644 | 0.722 | 0.748 | 0.618 | 0.348 | ||
| Agouti- signaling protein | R | 0.434 | 0.228 | 0.015 | 0.380 | 0.211 | 0.163 | 0.094 | 0.097 | 0.149 | 0.233 | 0.250 | 0.218 | 0.046 | −0.164 | −0.316 | 0.691 | |
| p | <0.001 | 0.086 | 0.913 | 0.022 | 0.103 | 0.209 | 0.47 | 0.459 | 0.264 | 0.089 | 0.068 | 0.113 | 0.722 | 0.203 | 0.013 | <0.001 | ||
| Neuropeptide Y | R | −0.109 | −0.163 | 0.036 | 0.092 | −0.011 | −0.045 | −0.078 | 0.006 | −0.23 | −0.137 | −0.152 | −0.356 | 0.042 | −0.164 | 0.025 | −0.145 | |
| p | 0.397 | 0.220 | 0.787 | 0.593 | 0.931 | 0.733 | 0.548 | 0.966 | 0.082 | 0.323 | 0.273 | 0.008 | 0.748 | 0.203 | 0.846 | 0.26 | ||
| α-MSH | R | −0.323 | −0.288 | 0.096 | −0.134 | −0.202 | −0.111 | −0.17 | −0.035 | −0.213 | −0.12 | −0.150 | −0.302 | −0.065 | −0.316 | 0.025 | −0.171 | |
| p | 0.011 | 0.030 | 0.475 | 0.442 | 0.123 | 0.4 | 0.195 | 0.802 | 0.111 | 0.392 | 0.284 | 0.033 | 0.618 | 0.013 | 0.846 | 0.187 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Podgórski, R.; Galiniak, S.; Mazur, A.; Podgórska, D.; Domin, A. Serum Levels of Hormones Regulating Appetite in Patients with Fetal Alcohol Spectrum Disorders. Nutrients 2023, 15, 4215. https://doi.org/10.3390/nu15194215
Podgórski R, Galiniak S, Mazur A, Podgórska D, Domin A. Serum Levels of Hormones Regulating Appetite in Patients with Fetal Alcohol Spectrum Disorders. Nutrients. 2023; 15(19):4215. https://doi.org/10.3390/nu15194215
Chicago/Turabian StylePodgórski, Rafał, Sabina Galiniak, Artur Mazur, Dominika Podgórska, and Agnieszka Domin. 2023. "Serum Levels of Hormones Regulating Appetite in Patients with Fetal Alcohol Spectrum Disorders" Nutrients 15, no. 19: 4215. https://doi.org/10.3390/nu15194215







