Nutrition and Food Literacy: Framing the Challenges to Health Communication
Abstract
:1. Introduction
2. Methods
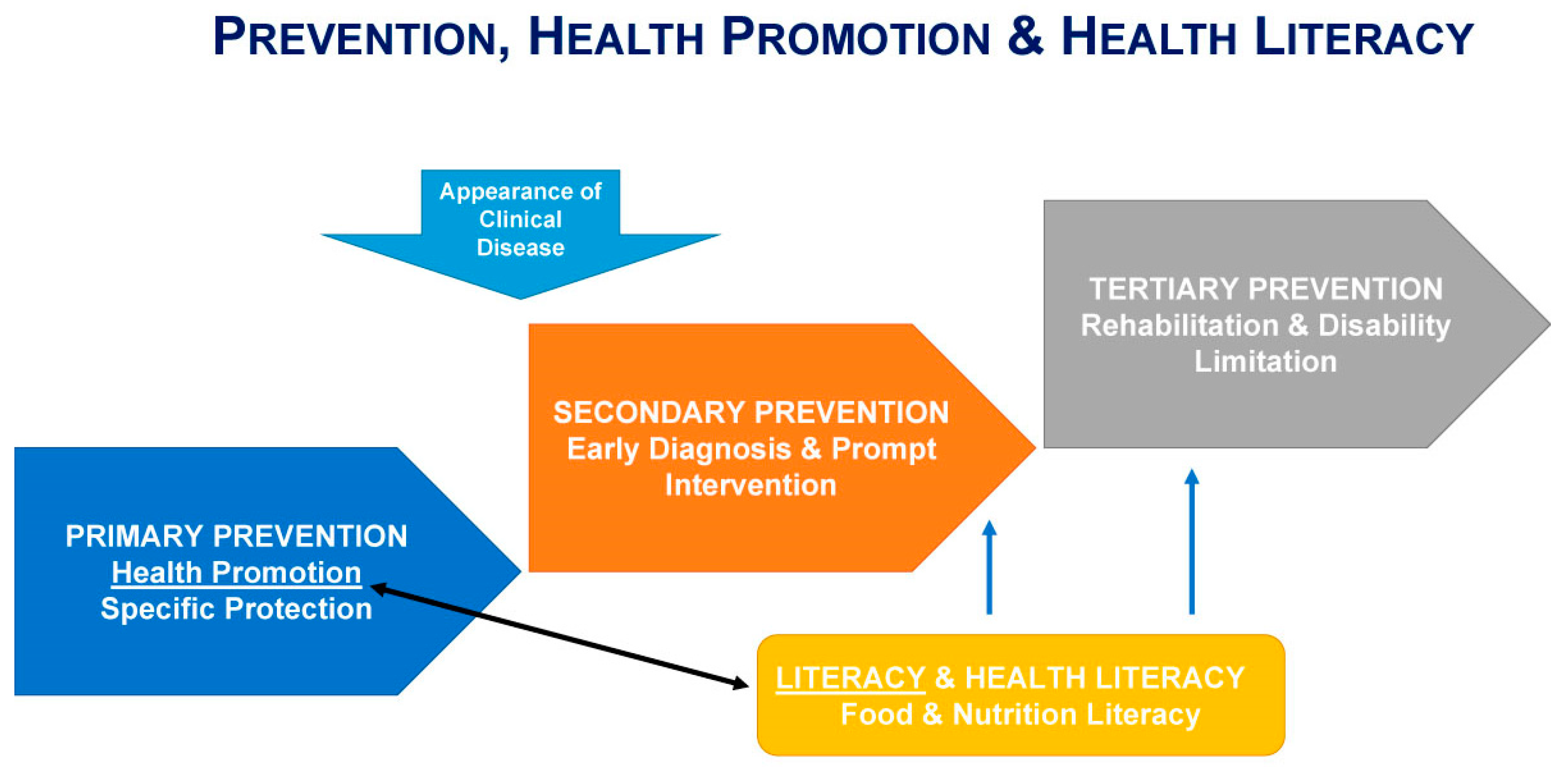
3. Health, Nutrition, and Food Literacy
4. The Emergence of Food Illiteracy as a Global Issue
5. Food Literacy Health Inequities
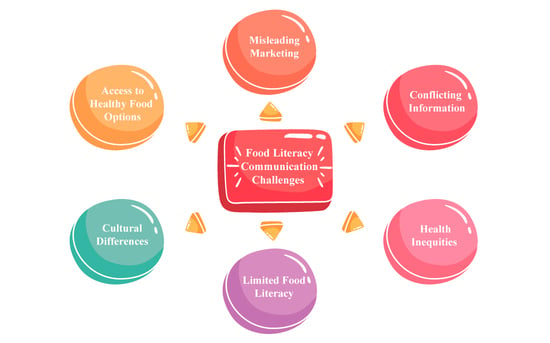
6. Food and Nutrition Disinformation: Challenges to Health Communication
6.1. Health Communication
6.2. Nutrition and Food Communication
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Silva, P.; Portillo, M.P.; Fernández-Quintela, A. Resveratrol and wine: An overview of thirty years in the digital news. Int. J. Environ. Res. Public Health 2022, 19, 15815. [Google Scholar] [CrossRef] [PubMed]
- Silva, P. Food and nutrition literacy: Exploring the divide between research and practice. Foods 2023, 12, 2751. [Google Scholar] [CrossRef] [PubMed]
- Deek, H.; Itani, L.; Davidson, P.M. Literacy critical to heart failure management: A scoping review. Heart Fail. Rev. 2021, 26, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Vaiciurgis, V.T.; Charlton, K.E.; Clancy, A.K.; Beck, E.J. Nutrition programmes for individuals living with disadvantage in supported residential settings: A scoping review. Public Health Nutr. 2022, 25, 2625–2636. [Google Scholar] [CrossRef] [PubMed]
- Hillier-Brown, F.C.; Summerbell, C.D.; Moore, H.J.; Routen, A.; Lake, A.A.; Adams, J.; White, M.; Araujo-Soares, V.; Abraham, C.; Adamson, A.J.; et al. The impact of interventions to promote healthier ready-to-eat meals (to eat in, to take away or to be delivered) sold by specific food outlets open to the general public: A systematic review. Obes. Rev. 2017, 18, 227–246. [Google Scholar] [CrossRef]
- Bojang, K.P.; Manchana, V. Nutrition and healthy aging: A review. Curr. Nutr. Rep. 2023, 12, 369–375. [Google Scholar] [CrossRef]
- Sullivan, A.D.; Gottschallpass, K.T. Food label nutrition literacy—Tool development and assessment. J. Can. Diet. Assoc. 1995, 56, 68–72. [Google Scholar]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Van Der Heide, I.; Wang, J.; Droomers, M.; Spreeuwenberg, P.; Rademakers, J.; Uiters, E. The relationship between health, education, and health literacy: Results from the Dutch Adult Literacy and Life Skills Survey. J. Health Commun. 2013, 18, 172–184. [Google Scholar] [CrossRef]
- Silk, K.J.; Sherry, J.; Winn, B.; Keesecker, N.; Horodynski, M.A.; Sayir, A. Increasing nutrition literacy: Testing the effectiveness of print, web site, and game modalities. J. Nutr. Educ. Behav. 2008, 40, 3–10. [Google Scholar] [CrossRef]
- Carbone, E.T.; Zoellner, J.M. Nutrition and health literacy: A systematic review to inform nutrition research and practice. J. Acad. Nutr. Diet. 2012, 112, 254–265. [Google Scholar] [CrossRef]
- Velardo, S. The nuances of health literacy, nutrition literacy, and food literacy. J. Nutr. Educ. Behav. 2015, 47, 385–389.e381. [Google Scholar] [CrossRef]
- Colatruglio, S.; Slater, J. Food Literacy: Bridging the Gap between Food, Nutrition and Well-Being. In Sustainable Well-Being: Concepts, Issues, and Educational Practices; Deer, F., Falkenberg, T., McMillan, B., Sims, L., Eds.; ESWB Press: Winnipeg, MB, Canada, 2014; pp. 37–55. [Google Scholar]
- Vidgen, H.A.; Gallegos, D. Defining food literacy and its components. Appetite 2014, 76, 50–59. [Google Scholar] [CrossRef]
- Truman, E.; Lane, D.; Elliott, C. Defining food literacy: A scoping review. Appetite 2017, 116, 365–371. [Google Scholar] [CrossRef]
- Cullen, T.; Hatch, J.; Martin, W.; Higgins, J.W.; Sheppard, R. Food literacy: Definition and framework for action. Can. J. Diet. Pract. Res. 2015, 76, 140–145. [Google Scholar] [CrossRef]
- Krause, C.; Sommerhalder, K.; Beer-Borst, S.; Abel, T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promot. Int. 2016, 33, 378–389. [Google Scholar] [CrossRef]
- Vidgen, H. (Ed.) A definition of food literacy and its components. In Food Literacy: Key Concepts for Health and Education, 1st ed.; Routledge: London, UK, 2016; pp. 35–65. [Google Scholar]
- Vettori, V.; Lorini, C.; Milani, C.; Bonaccorsi, G. Towards the implementation of a conceptual framework of food and nutrition literacy: Providing healthy eating for the population. Int. J. Environ. Res. Public Health 2019, 16, 5041. [Google Scholar] [CrossRef]
- Arena, R.; Lavie, C.J.; Hivert, M.F.; Williams, M.A.; Briggs, P.D.; Guazzi, M. Who will deliver comprehensive healthy lifestyle interventions to combat non-communicable disease? Introducing the healthy lifestyle practitioner discipline. Expert Rev. Cardiovasc. Ther. 2016, 14, 15–22. [Google Scholar] [CrossRef]
- Fitzgerald, N.; Morgan, K.T.; Slawson, D.L. Practice paper of the academy of nutrition and dietetics abstract: The role of nutrition in health promotion and chronic disease prevention. J. Acad. Nutr. Diet. 2013, 113, 983. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: Geneva, Switzerland, 2003; Volume 916.
- Baker, P.; Machado, P.; Santos, T.; Sievert, K.; Backholer, K.; Hadjikakou, M.; Russell, C.; Huse, O.; Bell, C.; Scrinis, G.; et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes. Rev. 2020, 21, e13126. [Google Scholar] [CrossRef]
- Elinder, L.S. Obesity, hunger, and agriculture: The damaging role of subsidies. Br. Med. J. 2005, 331, 1333–1336. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Dixon, J.; Omwega, A.M.; Friel, S.; Burns, C.; Donati, K.; Carlisle, R. The health equity dimensions of urban food systems. J. Urban Health 2007, 84, 118–129. [Google Scholar] [CrossRef]
- Vidgen, H. Food Literacy: Key Concepts for Health and Education; Routledge: London, UK, 2016. [Google Scholar]
- Lancet, T. Why is health literacy failing so many? Lancet 2022, 400, 1655. [Google Scholar] [CrossRef]
- Craig, W.J.; Mangels, A.R. Position of the American Dietetic Association: Vegetarian diets. J. Am. Diet. Assoc. 2009, 109, 1266. [Google Scholar] [CrossRef]
- Larson, N.; Laska, M.N.; Neumark-Sztainer, D. Food insecurity, diet quality, home food availability, and health risk behaviors among emerging adults: Findings from the EAT 2010–2018 study. Am. J. Public Health 2020, 110, 1422–1428. [Google Scholar] [CrossRef]
- Luta, X.; Hayoz, S.; Gréa Krause, C.; Sommerhalder, K.; Roos, E.; Strazzullo, P.; Beer-Borst, S. The relationship of health/food literacy and salt awareness to daily sodium and potassium intake among a workplace population in Switzerland. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 270–277. [Google Scholar] [CrossRef]
- Sami, W.; Ansari, T.; Butt, N.S.; Ab Hamid, M.R. Effect of diet on type 2 diabetes mellitus: A review. Int. J. Health Sci. 2017, 11, 65. [Google Scholar]
- Cecchini, M.; Sassi, F.; Lauer, J.A.; Lee, Y.Y.; Guajardo-Barron, V.; Chisholm, D. Tackling of unhealthy diets, physical inactivity, and obesity: Health effects and cost-effectiveness. Lancet 2010, 376, 1775–1784. [Google Scholar] [CrossRef]
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef]
- Mak, T.N. Public policy and older people’s diets. In Food for the Aging Population; Elsevier: Amsterdam, The Netherlands, 2017; pp. 257–268. [Google Scholar]
- Vaitkeviciute, R.; Ball, L.E.; Harris, N. The relationship between food literacy and dietary intake in adolescents: A systematic review. Public Health Nutr. 2015, 18, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Somerville, L.H.; Jones, R.M.; Casey, B.J. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cogn. 2010, 72, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Wills, W.; Backett-Milburn, K.; Roberts, M.-L.; Lawton, J. The framing of social class distinctions through family food and eating practices. Sociol. Rev. 2011, 59, 725–740. [Google Scholar] [CrossRef]
- Fairbrother, H.; Curtis, P.; Goyder, E. Where are the schools? Children, families and food practices. Health Place 2016, 40, 51–57. [Google Scholar] [CrossRef]
- Rose, K.; O’Malley, C.; Eskandari, F.; Lake, A.A.; Brown, L.; Ells, L.J. The impact of, and views on, school food intervention and policy in young people aged 11–18 years in Europe: A mixed methods systematic review. Obes. Rev. 2021, 22, e13186. [Google Scholar] [CrossRef]
- Gustavsson, J.; Cederberg, C.; Sonesson, U.; van Otterdijk, R.; Meybeck, A. Global Food Losses and Food Waste; FAO: Rome, Italy, 2011. [Google Scholar]
- Lins, M.; Zandonadi, R.P.; Strasburg, V.J.; Nakano, E.Y.; Botelho, R.B.A.; Raposo, A.; Ginani, V.C. Eco-Inefficiency Formula: A method to verify the cost of the economic, environmental, and social impact of waste in food services. Foods 2021, 10, 1369. [Google Scholar] [CrossRef]
- Aydin, A.E.; Yildirim, P. Understanding food waste behavior: The role of morals, habits and knowledge. J. Clean. Prod. 2021, 280, 124250. [Google Scholar] [CrossRef]
- Mora, M.; Romeo-Arroyo, E.; Toran-Pereg, P.; Chaya, C.; Vazquez-Araujo, L. Sustainable and health claims vs sensory properties: Consumers’ opinions and choices using a vegetable dip as example product. Food Res. Int. 2020, 137, 109521. [Google Scholar] [CrossRef]
- Heller, M.C.; Keoleian, G.A. Greenhouse gas emission estimates of u.s. dietary choices and food loss. J. Ind. Ecol. 2015, 19, 391–401. [Google Scholar] [CrossRef]
- Walia, B.; Sanders, S. Curbing food waste: A review of recent policy and action in the USA. Renew. Agric. Food Syst. 2017, 34, 169–177. [Google Scholar] [CrossRef]
- Brennan, L.; Langley, S.; Verghese, K.; Lockrey, S.; Ryder, M.; Francis, C.; Phan-Le, N.T.; Hill, A. The role of packaging in fighting food waste: A systematised review of consumer perceptions of packaging. J. Clean. Prod. 2021, 281, 125276. [Google Scholar] [CrossRef]
- Parmar, A. Optimizing agricultural practices. In Saving Food; Academic Press: Cambridge, MA, USA, 2019; pp. 89–116. [Google Scholar] [CrossRef]
- Amouzandeh, C.; Fingland, D.; Vidgen, H.A. A scoping review of the validity, reliability and conceptual alignment of food literacy measures for adults. Nutrients 2019, 11, 801. [Google Scholar] [CrossRef] [PubMed]
- Durmus, H.; Gökler, M.E.; Havlioglu, S. Reliability and validity of the Turkish version of the short food literacy questionnaire among university students. Prog. Nutr. 2019, 21, 333–338. [Google Scholar] [CrossRef]
- Luque, B.; Villaécija, J.; Ramallo, A.; de Matos, M.G.; Castillo-Mayén, R.; Cuadrado, E.; Tabernero, C. Spanish validation of the Self-Perceived Food Literacy Scale: A five-factor model proposition. Nutrients 2022, 14, 2902. [Google Scholar] [CrossRef]
- Poelman, M.P.; Dijkstra, S.C.; Sponselee, H.; Kamphuis, C.B.M.; Battjes-Fries, M.C.E.; Gillebaart, M.; Seidell, J.C. Towards the measurement of food literacy with respect to healthy eating: The development and validation of the self perceived food literacy scale among an adult sample in the Netherlands. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 54. [Google Scholar] [CrossRef]
- Selçuk, K.T.; Çevik, C.; Baydur, H.; Meseri, R. Validity and reliability of the Turkish version of the Self-perceived Food Literacy Scale. Prog. Nutr. 2020, 22, 671–677. [Google Scholar] [CrossRef]
- Zeminian, L.B.; Corona, L.P.; Batista, I.D.N.; Da Silva, M.C.; Da Cunha, D.T. Translation, adaptation, and validity of the Short Food Literacy Questionnaire for Brazil. Foods 2022, 11, 3968. [Google Scholar] [CrossRef]
- Zwierczyk, U.; Kobryn, M.; Duplaga, M. Validation of the Short Food Literacy Questionnaire in the representative sample of polish internet users. Int. J. Environ. Res. Public Health 2022, 19, 9710. [Google Scholar] [CrossRef]
- Krause, C.; Beer-Borst, S.; Sommerhalder, K.; Hayoz, S.; Abel, T. A Short Food Literacy Questionnaire (SFLQ) for adults: Findings from a Swiss validation study. Appetite 2018, 120, 275–280. [Google Scholar] [CrossRef]
- Sponselee, H.C.S.; Kroeze, W.; Poelman, M.P.; Renders, C.M.; Ball, K.; Steenhuis, I.H.M. Food and health promotion literacy among employees with a low and medium level of education in the Netherlands. BMC Public Health 2021, 21, 1273. [Google Scholar] [CrossRef] [PubMed]
- Trieste, L.; Bazzani, A.; Amato, A.; Faraguna, U.; Turchetti, G. Food literacy and food choice—A survey-based psychometric profiling of consumer behaviour. Br. Food J. 2021, 123, 124–141. [Google Scholar] [CrossRef]
- Arcaya, M.C.; Arcaya, A.L.; Subramanian, S.V. Inequalities in health: Definitions, concepts, and theories. Glob. Health Action 2015, 8, 27106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Inequities and Their Causes. Available online: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed on 23 January 2023).
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P.; on behalf of the Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Hargrove, T.W. Intersecting social inequalities and body mass index trajectories from adolescence to early adulthood. J. Health Soc. Behav. 2018, 59, 56–73. [Google Scholar] [CrossRef]
- Marquez, F.D.; Risica, P.M.; Mathis, K.J.; Sullivan, A.; Gobin, A.P.; Tyrka, A.R. Do measures of healthy eating differ in survivors of early adversity? Appetite 2021, 162, 105180. [Google Scholar] [CrossRef]
- Butcher, L.M.; Platts, J.R.; Le, N.; McIntosh, M.M.; Celenza, C.A.; Foulkes-Taylor, F. Can addressing food literacy across the life cycle improve the health of vulnerable populations? A case study approach. Health Promot. J. Aust. 2021, 32, 5–16. [Google Scholar] [CrossRef]
- Forray, A.I.; Coman, M.A.; Cherecheș, R.M.; Borzan, C.M. Exploring the impact of sociodemographic characteristics and health literacy on adherence to dietary recommendations and food literacy. Nutrients 2023, 15, 2853. [Google Scholar] [CrossRef]
- Kim, P.J. Social determinants of health inequities in indigenous canadians through a life course approach to colonialism and the residential school system. Health Equity 2019, 3, 378–381. [Google Scholar] [CrossRef]
- Abbatangelo-Gray, J.; Byrd-Bredbenner, C.; Austin, S.B. Health and nutrient content claims in food advertisements on hispanic and mainstream prime-time television. J. Nutr. Educ. Behav. 2008, 40, 348–354. [Google Scholar] [CrossRef]
- Fleming-Milici, F.; Harris, J.L.; Sarda, V.; Schwartz, M.B. Amount of Hispanic youth exposure to food and beverage advertising on spanish- and english-language television. JAMA Pediatr. 2013, 167, 723. [Google Scholar] [CrossRef] [PubMed]
- Herrera, A.L.; Pasch, K.E. Targeting Hispanic adolescents with outdoor food & beverage advertising around schools. Ethn. Health 2018, 23, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Rowe, S.; Alexander, N. Fake nutrition/health news, part 3: How (and why) did we get here? Nutr. Today 2019, 54, 170–173. [Google Scholar] [CrossRef]
- Demestichas, K.; Remoundou, K.; Adamopoulou, E. Food for thought: Fighting fake news and online disinformation. IT Prof. 2020, 22, 28–34. [Google Scholar] [CrossRef]
- Rowe, S.; Alexander, N. Fighting nutrition and health misinformation: Enlisting the public’s help. Nutr. Today 2022, 57, 34–37. [Google Scholar] [CrossRef]
- Benn, Y.; Webb, T.L.; Chang, B.P.I.; Reidy, J. What information do consumers consider, and how do they look for it, when shopping for groceries online? Appetite 2015, 89, 265–273. [Google Scholar] [CrossRef]
- Supthanasup, A.; Banwell, C.; Kelly, M.; Yiengprugsawan, V.S.; Davis, J.L. Child feeding practices and concerns: Thematic content analysis of Thai virtual communities. Matern. Child Nutr. 2021, 17, e13095. [Google Scholar] [CrossRef]
- Moorman, E.L.; Warnick, J.L.; Acharya, R.; Janicke, D.M. The use of internet sources for nutritional information is linked to weight perception and disordered eating in young adolescents. Appetite 2020, 154, 104782. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, J. Consumer health information seeking in social media: A literature review. Health Inf. Libr. J. 2017, 34, 268–283. [Google Scholar] [CrossRef]
- Rounsefell, K.; Gibson, S.; McLean, S.; Blair, M.; Molenaar, A.; Brennan, L.; Truby, H.; McCaffrey, T.A. Social media, body image and food choices in healthy young adults: A mixed methods systematic review. Nutr. Diet. 2020, 77, 19–40. [Google Scholar] [CrossRef]
- Steele, S.; Sarcevic, L.; Ruskin, G.; Stuckler, D. Confronting potential food industry ‘front groups’: Case study of the international food information Council’s nutrition communications using the UCSF food industry documents archive. Glob. Health 2022, 18, 16. [Google Scholar] [CrossRef] [PubMed]
- Taillie, L.S.; Ng, S.W.; Xue, Y.; Busey, E.; Harding, M. No fat, no sugar, no salt… no problem? Prevalence of “low-content” nutrient claims and their associations with the nutritional profile of food and beverage purchases in the United States. J. Acad. Nutr. Diet. 2017, 117, 1366–1374.e1366. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, Y.; Gwizdka, J.; Trace, C.B. Consumer evaluation of the quality of online health information: Systematic literature review of relevant criteria and indicators. J. Med. Internet Res. 2019, 21, e12522. [Google Scholar] [CrossRef] [PubMed]
- Klinker, C.D.; Aaby, A.; Ringgaard, L.W.; Hjort, A.V.; Hawkins, M.; Maindal, H.T. Health literacy is associated with health behaviors in students from vocational education and training schools: A Danish population-based survey. Int. J. Environ. Res. Public Health 2020, 17, 671. [Google Scholar] [CrossRef]
- Ramírez, A.S.; Carmona, K. Beyond fatalism: Information overload as a mechanism to understand health disparities. Soc. Sci. Med. 2018, 219, 11–18. [Google Scholar] [CrossRef]
- Tartaglia, J.; McIntosh, M.; Jancey, J.; Scott, J.; Begley, A. Exploring feeding practices and food literacy in parents with young children from disadvantaged areas. Int. J. Environ. Res. Public Health 2021, 18, 1496. [Google Scholar] [CrossRef]
- Rogers, E.M. The field of health communication today: An up-to-date report. J. Health Commun. 1996, 1, 15–23. [Google Scholar] [CrossRef]
- Ratzan, S.C.; Payne, J.G.; Bishop, C. The status and scope of health communication. J. Health Commun. 1996, 1, 25–41. [Google Scholar] [CrossRef]
- Kreps, G.L.; Bonaguro, E.W.; Query, J.L. The history and development of the field of health communication. In Health Communication Research: Guide to Developments and Directions; Duffy, B.K., Jackson, L.D., Eds.; Greenwood Press: Westport, CT, USA, 1998; pp. 1–15. [Google Scholar]
- Thomas, R.K. Health communication. In Traditional Approaches to Health Communication; Springer: New York, NY, USA, 2006; pp. 1–212. [Google Scholar]
- Zoller, H.; Dutta, M.J. Emerging Perspectives in Health Communication: Meaning, Culture, and Power; Routledge: London, UK, 2009. [Google Scholar]
- Liu, S.; Chen, G.-M. Communicating health: People, culture and context. China Media Res. 2010, 6, 1–2. [Google Scholar]
- Schiavo, R. Health Communication: From Theory to Practice; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 217. [Google Scholar]
- Sturm, R.; An, R. Obesity and economic environments. CA Cancer J. Clin. 2014, 64, 337–350. [Google Scholar] [CrossRef]
- Desbouys, L.; Mejean, C.; De Henauw, S.; Castetbon, K. Socio-economic and cultural disparities in diet among adolescents and young adults: A systematic review. Public Health Nutr. 2020, 23, 843–860. [Google Scholar] [CrossRef]
- Andersson, C.; Vasan, R.S. Epidemiology of cardiovascular disease in young individuals. Nat. Rev. Cardiol. 2018, 15, 230–240. [Google Scholar] [CrossRef]
- Lascar, N.; Brown, J.; Pattison, H.; Barnett, A.H.; Bailey, C.J.; Bellary, S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018, 6, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Kawabe, H.; Azegami, T.; Takeda, A.; Kanda, T.; Saito, I.; Saruta, T.; Hirose, H. Features of and preventive measures against hypertension in the young. Hypertens. Res. Nat. 2019, 42, 935–948. [Google Scholar] [CrossRef]
- Grier, S.; Bryant, C.A. Social marketing in public health. Annu. Rev. Public Health 2005, 26, 319–339. [Google Scholar] [CrossRef] [PubMed]
- Kotler, P.; Zaltman, G. Social marketing: An approach to planned social change. J. Mark. Res. 1971, 35, 3–12. [Google Scholar] [CrossRef]
- Andreasen, A.R. Social marketing—Its definition and domain. J. Public Policy Mark. 1994, 13, 108–114. [Google Scholar] [CrossRef]
- Stead, M.; Gordon, R.; Angus, K.; McDermott, L. A systematic review of social marketing effectiveness. Health Educ. 2007, 107, 126–191. [Google Scholar] [CrossRef]
- Aschemann-Witzel, J.; Perez-Cueto, F.J.; Niedzwiedzka, B.; Verbeke, W.; Bech-Larsen, T. Lessons for public health campaigns from analysing commercial food marketing success factors: A case study. BMC Public Health 2012, 12, 139. [Google Scholar] [CrossRef]
- Freeland-Graves, J.H.; Nitzke, S.; Academy of Nutrition and Dietetics. Position of the academy of nutrition and dietetics: Total diet approach to healthy eating. J. Acad. Nutr. Diet. 2013, 113, 307–317. [Google Scholar] [CrossRef]
- Herrick, C. Risky bodies: Public health, social marketing and the governance of obesity. Geoforum 2007, 38, 90–102. [Google Scholar] [CrossRef]
- Stead, M.; Arnott, L.; Dempsey, E. Healthy heroes, magic meals, and a visiting alien. Soc. Mark. Q. 2013, 19, 26–39. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Food Literacy: How Do Communications and Marketing Impact Consumer Knowledge, Skills, and Behavior? Workshop Summary; National Academies Press: Washington, DC, USA, 2016.
- Ginani, V.C.; Saccol, A.L.d.F.; Zandonadi, R.P. What, how, and where to eat is more than an individual choice: New ways to achieve healthy eating. Front. Sustain. Food Syst. 2022, 6, 1048719. [Google Scholar] [CrossRef]
- Lin, T.; Nan, X. A scoping review of emerging COVID-19 health communication research in communication and media journals. Health Commun. 2022, 38, 2570–2581. [Google Scholar] [CrossRef] [PubMed]
- Mytton, O.T.; Clarke, D.; Rayner, M. Taxing unhealthy food and drinks to improve health. Br. Med. J. (Online) 2012, 344, e2931. [Google Scholar] [CrossRef] [PubMed]
- Sacks, G.; Veerman, J.L.; Moodie, M.; Swinburn, B. Traffic-light nutrition labelling and junk-food tax: A modelled comparison of cost-effectiveness for obesity prevention. Int. J. Obes. 2011, 35, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Sacks, G.; Kwon, J.; Backholer, K. Do taxes on unhealthy foods and beverages influence food purchases? Curr. Nutr. Rep. 2021, 10, 179–187. [Google Scholar] [CrossRef]
- Thow, A.M.; Downs, S.; Jan, S. A systematic review of the effectiveness of food taxes and subsidies to improve diets: Understanding the recent evidence. Nutr. Rev. 2014, 72, 551–565. [Google Scholar] [CrossRef]
- Dodd, R.; Santos, J.A.; Tan, M.; Campbell, N.R.C.; Ni Mhurchu, C.; Cobb, L.; Jacobson, M.F.; He, F.J.; Trieu, K.; Osornprasop, S.; et al. Effectiveness and feasibility of taxing salt and foods high in sodium: A systematic review of the evidence. Adv. Nutr. 2020, 11, 1616–1630. [Google Scholar] [CrossRef]
- Nakhimovsky, S.S.; Feigl, A.B.; Avila, C.; O’Sullivan, G.; Macgregor-Skinner, E.; Spranca, M. Taxes on sugar-sweetened beverages to reduce overweight and obesity in middle-income countries: A systematic review. PLoS ONE 2016, 11, e0163358. [Google Scholar] [CrossRef]
- Silver, L.D.; Ng, S.W.; Ryan-Ibarra, S.; Taillie, L.S.; Induni, M.; Miles, D.R.; Poti, J.M.; Popkin, B.M. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: A before-and-after study. PLoS Med. 2017, 14, e1002283. [Google Scholar] [CrossRef] [PubMed]
- Nnoaham, K.E.; Sacks, G.; Rayner, M.; Mytton, O.; Gray, A. Modelling income group differences in the health and economic impacts of targeted food taxes and subsidies. Int. J. Epidemiol. 2009, 38, 1324–1333. [Google Scholar] [CrossRef] [PubMed]
- Gosliner, W.; Brown, D.M.; Sun, B.C.; Woodward-Lopez, G.; Crawford, P.B. Availability, quality and price of produce in low-income neighbourhood food stores in California raise equity issues. Public Health Nutr. 2018, 21, 1639–1648. [Google Scholar] [CrossRef] [PubMed]
- Lowery, B.; Sloane, D.; Payán, D.; Illum, J.; Lewis, L. Do farmers’ markets increase access to healthy foods for all communities? Comparing markets in 24 neighborhoods in Los Angeles. J. Am. Plan. Assoc. 2016, 82, 252–266. [Google Scholar] [CrossRef]
- Silva, B.; Lima, J.P.M.; Baltazar, A.L.; Pinto, E.; Fialho, S. Perception of Portuguese consumers regarding food labeling. Nutrients 2022, 14, 2944. [Google Scholar] [CrossRef] [PubMed]
- Watson, W.L.; Chapman, K.; King, L.; Kelly, B.; Hughes, C.; Louie, J.C.Y.; Crawford, J.; Gill, T.P. How well do Australian shoppers understand energy terms on food labels? Public Health Nutr. 2013, 16, 409–417. [Google Scholar] [CrossRef]
- Sacco, J.E.; Sumanac, D.; Tarasuk, V. Front-of-package references to fiber on foods in Canadian supermarkets highlight the need for increased nutrition knowledge among consumers. J. Nutr. Educ. Behav. 2013, 45, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.M.S.; Applegate, E.; Beckett, L.A.; Wilson, M.D.; Gibson, T.N. Age differences in the use of serving size information on food labels: Numeracy or attention? Public Health Nutr. 2017, 20, 786–796. [Google Scholar] [CrossRef]
- Bhawra, J.; Kirkpatrick, S.I.; Hall, M.G.; Vanderlee, L.; Thrasher, J.F.; Hammond, D. Correlates of self-reported and functional understanding of nutrition labels across 5 countries in the 2018 international food policy study. J. Nutr. 2022, 152, 13S–24S. [Google Scholar] [CrossRef]
- Moorman, C. The effects of stimulus and consumer characteristics on the utilization of nutrition information. J. Consum. Res. 1990, 17, 362. [Google Scholar] [CrossRef]
- Sinclair, S.; Hammond, D.; Goodman, S. Sociodemographic differences in the comprehension of nutritional labels on food products. J. Nutr. Educ. Behav. 2013, 45, 767–772. [Google Scholar] [CrossRef]
- Wang, G.; Fletcher, S.M.; Carley, D.H. Consumer utilization of food labeling as a source of nutrition information. J. Consum. Aff. 1995, 29, 368–380. [Google Scholar] [CrossRef]
- Raffoul, A.; Gibbons, B.; Boluk, K.; Neiterman, E.; Hammond, D.; Kirkpatrick, S.I. “Maybe a little bit of guilt isn’t so bad for the overall health of an individual”: A mixed-methods exploration of young adults’ experiences with calorie labelling. BMC Public Health 2022, 22, 938. [Google Scholar] [CrossRef] [PubMed]
- Blitstein, J.L.; Evans, W.D. Use of nutrition facts panels among adults who make household food purchasing decisions. J. Nutr. Educ. Behav. 2006, 38, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Nayga, R.M.; Lipinski, D.; Savur, N. Consumers’ Use of nutritional labels while food shopping and at home. J. Consum. Aff. 1998, 32, 106–120. [Google Scholar] [CrossRef]
- Nayga, R.M. Nutrition knowledge, gender, and food label use. J. Consum. Aff. 2000, 34, 97–112. [Google Scholar] [CrossRef]
- Feick, L.F.; Herrmann, R.O.; Warland, R.H. Search for nutrition information: A probit analysis of the use of different information sources. J. Consum. Aff. 1986, 20, 173–192. [Google Scholar] [CrossRef]
- Viswanathan, M.; Hastak, M.; Gau, R. Understanding and facilitating the usage of nutritional labels by low-literate consumers. J. Public Policy Mark. 2009, 28, 135–145. [Google Scholar] [CrossRef]
- Grubb, M.; Vogl, C.R. Understanding food literacy in urban gardeners: A case study of the Twin Cities, Minnesota. Sustainability 2019, 11, 3617. [Google Scholar] [CrossRef]
- Alpaugh, M.; Pope, L.; Trubek, A.; Skelly, J.; Harvey, J. Cooking as a health behavior: Examining the role of cooking classes in a weight loss intervention. Nutrients 2020, 12, 3669. [Google Scholar] [CrossRef]
- Brown, B.J.; Hermann, J.R. Cooking classes increase fruit and vegetable intake and food safety behaviors in youth and adults. J. Nutr. Educ. Behav. 2005, 37, 104–105. [Google Scholar] [CrossRef] [PubMed]
- Cunningham-Sabo, L.; Lohse, B. Cooking with kids. Positively affects fourth graders’ vegetable preferences and attitudes and self-efficacy for food and cooking. Child. Obes. 2013, 9, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Hersch, D.; Perdue, L.; Ambroz, T.; Boucher, J.L. The Impact of cooking classes on food-related preferences, attitudes, and behaviors of school-aged children: A systematic review of the evidence, 2003–2014. Prev. Chronic Dis. 2014, 11, E193. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, J.A.; Frattaroli, S.; Bleich, S.N.; Smith, K.C.; Teret, S.P. Perspectives on learning to cook and public support for cooking education policies in the United States: A mixed methods study. Appetite 2017, 108, 226–237. [Google Scholar] [CrossRef]
- Youssef, J.; Mora, M.; Maiz, E.; Spence, C. Sensory exploration of vegetables combined with a cookery class increases willingness to choose/eat plant-based food and drink. Int. J. Gastron. Food Sci. 2022, 28, 100515. [Google Scholar] [CrossRef]
- Truss, A.; Marshall, R.; Blair-Stevens, C. A History of Social Marketing. In Social Marketing and Public Health: Theory and Practice; French, J., Blair-Stevens, C., McVey, D., Merritt, R., Eds.; Oxford University Press: Oxford, UK, 2009; pp. 19–28. Available online: https://academic.oup.com/book/38700/chapter-abstract/336375979?redirectedFrom=fulltext (accessed on 23 January 2023).
- Carins, J.E.; Rundle-Thiele, S.R. Eating for the better: A social marketing review (2000–2012). Public Health Nutr. 2014, 17, 1628–1639. [Google Scholar] [CrossRef]
- Samuels, S.E. Project LEAN: A national campaign to reduce dietary fat consumption. Am. J. Health Promot. 1990, 4, 435–440. [Google Scholar] [CrossRef]
- Samuels, S.E. Project LEAN—Lessons learned from a national social marketing campaign. Public Health Rep. 1993, 108, 45–53. [Google Scholar]
- Foerster, S.B.; Kizer, K.W.; DiSogra, L.K.; Bal, D.G.; Krieg, B.F.; Bunch, K.L. California’s “5 a Day—For Better Health!” campaign: An innovative population-based effort to effect large-scale dietary change. Am. J. Prev. Med. 1995, 11, 124–131. [Google Scholar] [CrossRef]
- Shive, S.E.; Morris, M.N. Evaluation of the energize your life! Social marketing campaign pilot study to increase fruit intake among community college students. J. Am. Coll. Health 2006, 55, 33–39. [Google Scholar] [CrossRef]
- Beaudoin, C.E.; Fernandez, C.; Wall, J.L.; Farley, T.A. Promoting healthy eating and physical activity short-term effects of a mass media campaign. Am. J. Prev. Med. 2007, 32, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Buller, M.K.; Kane, I.L.; Dunn, A.L.; Edwards, E.J.; Buller, D.B.; Liu, X. Marketing fruit and vegetable intake with interactive games on the internet. Soc. Mark. Q. 2009, 15, 136–154. [Google Scholar] [CrossRef]
- Hofer, R.; Wilkin, M.K.; Mayers, E.; Wolford, B.K.; Butler, B.; Beavers, B.; Zubieta, A.C. Development and evaluation of a research-driven health communication campaign to increase fruit and vegetable consumption among SNAP-eligible Ohio adults. Soc. Mark. Q. 2021, 27, 267–283. [Google Scholar] [CrossRef]
- Boles, M.; Adams, A.; Gredler, A.; Manhas, S. Ability of a mass media campaign to influence knowledge, attitudes, and behaviors about sugary drinks and obesity. Prev. Med. 2014, 67 (Suppl. S1), S40–S45. [Google Scholar] [CrossRef] [PubMed]
- Jeong, M.; Gilmore, J.S.; Bleakley, A.; Jordan, A. Local news media framing of obesity in the context of a sugar-sweetened beverage reduction media campaign. J. Nutr. Educ. Behav. 2014, 46, 583–588. [Google Scholar] [CrossRef]
- Bleakley, A.; Jordan, A.; Mallya, G.; Hennessy, M.; Piotrowski, J.T. Do you know what your kids are drinking? Evaluation of a media campaign to reduce consumption of sugar-sweetened beverages. Am. J. Health Promot. 2018, 32, 1409–1416. [Google Scholar] [CrossRef]
- George, K.S.; Roberts, C.B.; Beasley, S.; Fox, M.; Rashied-Henry, K.; Brooklyn partnership to drive down, d. our health is in our hands: A social marketing campaign to combat obesity and diabetes. Am. J. Health Promot. 2016, 30, 283–286. [Google Scholar] [CrossRef]
- Klassen, A.C.; Sood, S.; Summers, A.; Perera, U.; Shuster, M.; Lopez, J.P.; McCord, A.; Stokes, J.; White, J.; Wagner, A. From salt to stroke—Evaluation of a media campaign for sodium reduction in Philadelphia. Front. Public Health 2021, 8, 619261. [Google Scholar] [CrossRef]
- Reckinger, R.; Regnier, F. Diet and public health campaigns: Implementation and appropriation of nutritional recommendations in France and Luxembourg. Appetite 2017, 112, 249–259. [Google Scholar] [CrossRef]
- Nosi, C.; D’Agostino, A.; Pratesi, C.A.; Barbarossa, C. Evaluating a social marketing campaign on healthy nutrition and lifestyle among primary-school children: A mixed-method research design. Eval. Program Plan. 2021, 89, 101965. [Google Scholar] [CrossRef]
- Graça, P.; Gregório, M.J.; Freitas, M.d.G. A decade of food and nutrition policy in Portugal (2010–2020). Port. J. Public Health 2020, 38, 1–25. [Google Scholar] [CrossRef]
- Gregório, M.J.; Afonso Henriques, A.D.; da Graça Freitas, M.; Mestre, R.; Teixeira, D.; Salvador, C.; Graça, P. Programa Nacional Para a Promoção da Alimentação Saudável 2022–2030; Direção-Geral da Saúde: Lisboa, Portugal, 2023. [Google Scholar]
- Buller, D.B.; Woodall, W.G.; Zimmerman, D.E.; Slater, M.D.; Heimendinger, J.; Waters, E.; Hines, J.M.; Starling, R.; Hau, B.; Burris-Woodall, P.; et al. Randomized trial on the “5 a Day, the Rio Grande Way” website, A Web-based program to improve fruit and vegetable consumption in rural communities. J. Health Commun. 2008, 13, 230–249. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, N.L.; Saperstein, S.L.; Desmond, S.M.; Gold, R.S.; Billing, A.S.; Tian, J. Rural eHealth nutrition education for limited-income families: An iterative and user-centered design approach. J. Med. Internet Res. 2009, 11, e21. [Google Scholar] [CrossRef] [PubMed]
- Livingood, W.C.; Monticalvo, D.; Bernhardt, J.M.; Wells, K.T.; Harris, T.; Kee, K.; Hayes, J.; George, D.; Woodhouse, L.D. Engaging adolescents through participatory and qualitative research methods to develop a digital communication intervention to reduce adolescent obesity. Health Educ. Behav. 2017, 44, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; Caperchione, C.M.; Ellison, M.; George, E.S.; Maeder, A.; Kolt, G.S.; Duncan, M.J.; Karunanithi, M.; Noakes, M.; Hooker, C.; et al. What kinds of website and mobile phone–Delivered physical activity and nutrition interventions do middle-aged men want? J. Health Commun. 2013, 18, 1070–1083. [Google Scholar] [CrossRef]
- Percoco, V.M. Food logging and blogging toward healthier nutrition: Bringing the curriculum out of the classroom and into the 21st century. Pedagog. Health Promot. 2017, 3, 77–81. [Google Scholar] [CrossRef]
- Cairns, G.; Angus, K.; Hastings, G.; Caraher, M. Systematic reviews of the evidence on the nature, extent and effects of food marketing to children. A retrospective summary. Appetite 2013, 62, 209–215. [Google Scholar] [CrossRef]
- Rowbotham, S.; Astell-Burt, T.; Barakat, T.; Hawe, P. 30+ years of media analysis of relevance to chronic disease: A scoping review. BMC Public Health 2020, 20, 364. [Google Scholar] [CrossRef]
- Burke-Garcia, A.; Kreps, G.L.; Wright, K.B. Perceptions about disseminating health information among mommy bloggers: Quantitative study. JMIR Res. Protoc. 2018, 20, e116. [Google Scholar] [CrossRef]
- Plaisime, M.; Robertson-James, C.; Mejia, L.; Núñez, A.; Wolf, J.; Reels, S. Social media and teens: A needs assessment exploring the potential role of social media in promoting health. Soc. Media Soc. 2020, 6, 205630511988602. [Google Scholar] [CrossRef]
- Loss, J.; Von Uslar, C. How German health insurance providers use social online networks to promote healthy lifestyles: A content analysis of Facebook® accounts. BMC Med. Inform. Decis. Mak. 2021, 21, 64. [Google Scholar] [CrossRef]
- Tobey, L.N.; Manore, M.M. Social media and nutrition education: The food hero experience. J. Nutr. Educ. Behav. 2014, 46, 128–133. [Google Scholar] [CrossRef]
- Barklamb, A.M.; Molenaar, A.; Brennan, L.; Evans, S.; Choong, J.; Herron, E.; Reid, M.; McCaffrey, T.A. Learning the language of social media: A comparison of engagement metrics and social media strategies used by food and nutrition-related social media accounts. Nutrients 2020, 12, 2839. [Google Scholar] [CrossRef]
- Meitz, T.G.K.; Ort, A.; Kalch, A.; Zipfel, S.; Zurstiege, G. Source does matter: Contextual effects on online media-embedded health campaigns against childhood obesity. Comput. Hum. Behav. 2016, 60, 565–574. [Google Scholar] [CrossRef]
- Jenkins, E.L.; Ilicic, J.; Molenaar, A.; Chin, S.; McCaffrey, T.A. Strategies to improve health communication: Can health professionals be heroes? Nutrients 2020, 12, 1861. [Google Scholar] [CrossRef] [PubMed]
- Lynn, T.; Rosati, P.; Santos, G.L.; Endo, P.T. Sorting the healthy diet signal from the social media expert noise: Preliminary evidence from the healthy diet discourse on twitter. Int. J. Environ. Res. Public Health 2020, 17, 8557. [Google Scholar] [CrossRef] [PubMed]
- Atehortua, N.A.; Patino, S. COVID-19, a tale of two pandemics: Novel coronavirus and fake news messaging. Health Promot. Int. 2021, 36, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Sbardelotto, J.; Martins, B.B.; Buss, C. Use of social networks in the context of the dietitian’s practice in Brazil and changes during the COVID-19 pandemic: Exploratory study. JMIR Form. Res. 2022, 6, e31533. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.; Nagavally, S.; Wagner, N.; Walker, R.; Segon, Y.; Segon, A. Creating a culture of quality: Our experience with providing feedback to frontline hospitalists. Br. Med. J. Open Qual. 2021, 10, e001141. [Google Scholar] [CrossRef] [PubMed]
- McDonald, K.M.; Bryce, C.L.; Graber, M.L. The patient is in: Patient involvement strategies for diagnostic error mitigation. Br. Med. J. Qual. Saf. 2013, 22, ii33–ii39. [Google Scholar] [CrossRef]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect. 2018, 21, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Zegers, M.; Veenstra, G.L.; Gerritsen, G.; Verhage, R.; Van Der Hoeven, H.J.G.; Welker, G.A. Perceived burden due to registrations for quality monitoring and improvement in hospitals: A mixed methods study. Int. J. Health Policy Manag. 2020, 11, 183. [Google Scholar] [CrossRef] [PubMed]
- Britto, M.T.; Fuller, S.C.; Kaplan, H.C.; Kotagal, U.; Lannon, C.; Margolis, P.A.; Muething, S.E.; Schoettker, P.J.; Seid, M. Using a network organisational architecture to support the development of Learning Healthcare Systems. Br. Med. J. Qual. Saf. 2018, 27, 937–946. [Google Scholar] [CrossRef] [PubMed]
| Nutrition Literacy Definition | Reference |
| “Nutritional literacy, as a specific form of health literacy, requires both general literacy and computational skill. It is not surprising to find that higher levels of nutrition knowledge have been associated with nutrition label use.” | Blitstein, J.L.; Evans, W.D. Use of Nutrition Facts Panels among Adults Who Make Household Food Purchasing Decisions. Journal of Nutrition Education and Behavior 2006, 38, 360–364, doi:10.1016/j.jneb.2006.02.009. (p. 1) |
| “Adequate health literacy and nutrition literacy require an individual not only to read well, but also to understand health and nutrition concepts and to have basic quantitative skills (defined as numeracy: the ability to use and understand numbers in daily life, including the ability to read and interpret nutrition information. People without these skills may have difficulty understanding concepts of healthful diets, reading nutrition information, and measuring a portion size.” | Neuhauser, L.; Rothschild, R.; Rodríguez, F.M. MyPyramid.gov: Assessment of Literacy, Cultural and Linguistic Factors in the USDA Food Pyramid Web Site. Journal of Nutrition Education and Behavior 2007, 39, 219–225, doi:10.1016/j.jneb.2007.03.005. (p. 220) |
| “Nutrition literacy can be defined similarly to health literacy as the degree to which individuals can obtain, process, and understand the basic health (nutrition) information and services they need to make appropriate health (nutrition) decisions, with the qualification that the definition is nutrition-specific.” | Silk, K.J.; Sherry, J.; Winn, B.; Keesecker, N.; Horodynski, M.A.; Sayir, A. Increasing Nutrition Literacy: Testing the Effectiveness of Print, Web site, and Game Modalities. Journal of Nutrition Education and Behavior 2008, 40, 3–10, doi:10.1016/j.jneb.2007.08.012. (p. 4) |
| “Nutrition literacy may be defined as the degree to which people have the capacity to obtain, process, and understand basic nutrition information.” | Zoellner, J.; Connell, C.; Bounds, W.; Crook, L.; Yadrick, K. Nutrition literacy status and preferred nutrition communication channels among adults in the lower Mississippi Delta. Preventing Chronic Disease 2009, 6, doi:19755004. (p. 2) |
| “In other words, at what point is this client no longer dependent on expert knowledge? When do his or her food choices reflect what is right for him or her 80% to 90% of the time? That is when the person achieves nutrition literacy. Fortunately, the term can and should be individualized according to the goals set at the beginning of the relationship. When that individual says, “I can do this on my own”, the dietetics practitioner will have succeeded.” | Escott-Stump, S.A. Our nutrition literacy challenge: Making the 2010 dietary guidelines relevant for consumers. Journal of the American Dietetic Association 2011, 111, 979, doi:10.1016/j.jada.2011.05.024. (p. 979) |
| “…‘nutrition literacy’ can mean the extent to which people access, understand and use nutrition information. In this context, consumers’ nutrition literacy is critical in their interpretation of noninterpretative front-of-pack food labelling and menu labelling.” | Watson, W.L.; Chapman, K.; King, L.; Kelly, B.; Hughes, C.; Yu Louie, J.C.; Crawford, J.; Gill, T.P. How well do Australian shoppers understand energy terms on food labels? Public Health Nutrition 2013, 16, 409–417, doi:10.1017/s1368980012000900. (p. 410) |
| “Functional nutrition literacy refers to proficiency in applying basic literacy skills, such as reading and understanding food labelling and grasping the essence of nutrition information guidelines. Interactive nutrition literacy comprises more advanced literacy skills, such as the cognitive and interpersonal communication skills needed to interact appropriately with nutrition counsellors, as well as interest in seeking and applying adequate nutrition information for the purpose of improving one’s nutritional status and behaviour. Critical nutrition literacy refers to being proficient in critically analyzing nutrition information and advice, as well as having the will to participate in actions to address nutritional barriers in personal, social, and global perspectives. CNL is part of scientific literacy– ‘the capacity to use scientific knowledge, to identify questions and to draw evidence-based conclusions’ i.e., proficiency in describing, explaining and predicting scientific phenomena, and understanding the processes of scientific inquiries as well as the premises of scientific evidence and conclusion.” | Guttersrud, O.; Dalane, J.O.; Pettersen, S. Improving measurement in nutrition literacy research using Rasch modelling: Examining construct validity of stage-specific ‘critical nutrition literacy’ scales. Public Health Nutrition 2014, 17, 877–883, doi:10.1017/S1368980013000530. (p. 887) |
| “Nutrition literacy focuses mainly on abilities to understand nutrition information, which can be seen as a prerequisite for a wider range of skills described under the term food literacy. Thus, nutrition literacy can be seen a subset of food literacy.” | Krause, C.; Sommerhalder, K.; Beer-Borst, S.; Abel, T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promotion International 2016, 33, 378–389, doi:10.1093/heapro/daw084. (p. 387) |
| Food Literacy Definition | Reference |
| “We defined food literacy as the capacity of an individual to obtain, interpret and understand basic food and nutrition information and services and the competence to use that information and services in ways that are health-enhancing. This definition was derived from the accepted definition of health literacy…” | Kolasa, K.M.; Peery, A.; Harris, N.G.; Shovelin, K. Food Literacy Partners Program: A Strategy To Increase Community Food Literacy. Topics in Clinical Nutrition 2001, 16, 1–10. (p. 5) |
| “…food literacy as more than knowledge; it also involves the motivation to apply nutrition information to food choices. Whereas food knowledge is the possession of food-related information, food literacy entails both understanding nutrition information and acting on that knowledge in ways consistent with promoting nutrition goals and “food well-being”.” | Block, L.G.; Grier, S.A.; Childers, T.L.; Davis, B.; Ebert, J.E.J.; Kumanyika, S.; Laczniak, R.N.; Machin, J.E.; Motley, C.M.; Peracchio, L.; et al. From nutrients to nurturance: A conceptual introduction to food well-being. Journal of Public Policy and Marketing 2011, 30, 5–13, doi:10.1509/jppm.30.1.5. (p. 7) |
| “…expands traditional measures of nutrition knowledge to include not only what people know about food but their ability to use that information to facilitate higher levels of food well-being. Food literacy ranges from declarative types of knowledge (e.g., knowing what asparagus is and what types of the nutrients asparagus might provide) to procedural knowledge (e.g., how to cook this vegetable).” | Bublitz, M.G.; Peracchio, L.A.; Andreasen, A.R.; Kees, J.; Kidwell, B.; Miller, E.G.; Motley, C.M.; Peter, P.C.; Rajagopal, P.; Scott, M.L. The quest for eating right: Advancing food well-being. Journal of Research for Consumers 2011, 1. (pp. 3–4) |
| “Food literacy was seen mainly as an individual’s ability to read, understand, and act upon labels on fresh, frozen, canned, frozen, processed, and takeout food.” | Fordyce-Voorham, S. Identification of essential food skills for skill-based healthful eating programs in secondary schools. J Nutr Educ Behav 2011, 43, 116–122, doi:10.1016/j.jneb.2009.12.002. (p. 119) |
| “I take the inspiration for food literacy from the notions of ‘health literacy’ in public health literature. The concept was born out of public health policy’s endeavor to educate people to seek healthier lifestyles and adhere to prescribed advice and was used to explain ‘the relationship between the patient literacy levels and their ability to comply with prescribed therapeutic regimens’.” | Kimura, A.H. Food education as food literacy: Privatized and gendered food knowledge in contemporary Japan. Agriculture and Human Values 2011, 28, 465–482, doi:10.1007/s10460-010-9286-6. (p. 479) |
| “Food literacy is the ‘capacity of an individual to obtain, interpret and understand basic food and nutrition information and services as well as the competence to use that information and available services that are health enhancing.’” | Pendergast, D.; Garvis, S.; Kanasa, H. Insight from the Public on Home Economics and Formal Food Literacy. Family and Consumer Sciences Research Journal 2011, 39, 415–430, doi:10.1111/j.1552-3934.2011.02079.x. (p. 418) |
| “…the relative ability to basically understand the nature of food and how it is important to you, and how able you are to gain information about food, process it, analyze it and act upon it.” | Vidgen, H.A.; Gallegos, D. What is food literacy and does it influence what we eat: a study of Australian food experts. 2011. (p. ii) |
| “… a complex, interrelated, person-centred set of skills that are necessary to provide and prepare safe, nutritious, and culturally-acceptable meals for all members of one’s household.” | Thomas, H.M.; Irwin, J.D. Cook It Up! A community-based cooking program for at-risk youth: Overview of a food literacy intervention. BMC Research Notes 2011, 4, 495, doi:10.1186/1756-0500-4-495. (p. 6) |
| “A collection of inter-related knowledge, skills and behaviours required to plan, manage, select, prepare and eat foods to meet needs and determine food intake. Food literacy is the scaffolding that empowers individuals, households, communities or nations to protect diet quality through change and support dietary resilience over time.” | Vidgen, H.A.; Gallegos, D. Defining food literacy, its components, development and relationship to food intake: A case study of young people and disadvantage. 2012. (p. vii) |
| “…the capacity of an individual to obtain, process and understand basic food information about food and nutrition as well as the competence to use that information in order to make appropriate health decisions.” | Murimi, M.W. Healthy literacy, nutrition education, and food literacy. Journal of Nutrition Education and Behavior 2013, 45, 195, doi:10.1016/j.jneb.2013.03.014. (p. 195) |
| “…focuses on food and nutrition information to help individuals make appropriate eating decisions.” | Rawl, R.; Kolasa, K.M.; Lee, J.; Whetstone, L.M. A Learn and Serve Nutrition Program: The Food Literacy Partners Program. Journal of Nutrition Education and Behavior 2008, 40, 49–51, doi:10.1016/j.jneb.2007.04.372. (p. 49) |
| “…a set of skills and attributes that help people sustain the daily preparation of healthy, tasty, affordable meals for themselves and their families. Food literacy builds resilience, because it includes food skills (techniques, knowledge and planning ability), the confidence to improvise and problem-solve, and the ability to access and share information. Food literacy is made possible through external support with healthy food access and living conditions, broad learning opportunities, and positive socio-cultural environments.” | Desjardins, E. Making Something out of Nothing: Food Literacy Among Youth, Young Pregnant Women and Young Parents Who are at Risk for Poor Health. A Locally Driven Collaborative Project. 2013. At: http://www.osnpph.on.ca/upload/membership/document/foodliteracy-study.ldcpontario.final.dec2013.pdf (accessed on 23 January 2023) (p. 70) |
| “Food literacy can be defined as an individual’s food related knowledge, attitudes, and skills. This broad definition of food literacy incorporates household perception, assessment, and management of the risks associated with their food choices. Individuals’ food literacy level influences their food-related decisions, which ultimately impact their diet and health as well as the environment.” | Howard, A.; Brichta, J. What’s to Eat?: Improving Food Literacy in Canada. 2013. (p. 2) |
| “Food literacy is the ability to “read the world” in terms of food, thereby recreating it and remaking ourselves. It involves a full-cycle understanding of food—where it is grown, how it is produced, who benefits and who loses when it is purchased, who can access it (and who can’t), and where it goes when we are finished with it. It includes an appreciation of the cultural significance of food, the capacity to prepare healthy meals and make healthy decisions, and the recognition of the environmental, social, economic, cultural, and political implications of those decisions.” | Sumner, J. Food literacy and adult education: Learning to read the world by eating. Canadian Journal for the Study of Adult Education 2013, 25, 79–92. (p. 86) |
| “Functional food literacy: basic communication of credible, evidence-based food and nutrition information, involving accessing, understanding and evaluating information. Interactive food literacy: development of personal skills regarding food and nutrition issues, involving decision making, goal setting and practices to enhance nutritional health and well-being Critical food literacy: respecting different cultural, family and religious beliefs in respect to food and nutrition (including nutritional health), understanding the wider context of food production and nutritional health, and advocating for personal, family and community changes that enhance nutritional health.” | Slater, J. Is cooking dead? The state of Home Economics Food and Nutrition education in a Canadian province. International Journal of Consumer Studies 2013, 37, 617–624, doi:10.1111/ijcs.12042. (p. 623) |
| “Food literacy is the scaffolding that empowers individuals, households, communities or nations to protect diet quality through change and strengthen dietary resilience over time. It is composed of a collection of inter-related knowledge, skills and behaviours required to plan, manage, select, prepare and eat food to meet needs and determine intake.” | Vidgen, H.A.; Gallegos, D. Defining food literacy and its components. Appetite 2014, 76, 50–59, doi:10.1016/j.appet.2014.01.010. (p. 54) |
| “Food literacy is the ability of an individual to understand food in a way that they develop a positive relationship with it, including food skills and practices across the lifespan in order to navigate, engage, and participate within a complex food system. It’s the ability to make decisions to support the achievement of personal health and a sustainable food system considering environmental, social, economic, cultural, and political components.” | Cullen, T.; Hatch, J.; Martin, W.; Higgins, J.W.; Sheppard, R. Food literacy: Definition and framework for action. Canadian Journal of Dietetic Practice and Research 2015, 76, 140–145, doi:10.3148/cjdpr-2015-010. (p. 143) |
| “We suggest using the term food literacy instead of nutrition literacy to describe the wide range of skills needed for a healthy and responsible nutrition behaviour. When measuring food literacy, we suggest the following core abilities and skills be taken into account: reading, understanding, and judging the quality of information; gathering and exchanging knowledge related to food and nutrition themes; practical skills like shopping and preparing food; and critically reflecting on factors that influence personal choices about food, and understanding the impact of those choices on society.” | Krause, C.; Sommerhalder, K.; Beer-Borst, S.; Abel, T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promotion International 2016, 33, 378–389, doi:10.1093/heapro/daw084. (p. 387) |
| “‘food literacy’ encompasses a more holistic approach to describe the practicalities needed to meet nutrition recommendations: plan, management, selection, preparation, and consumption.” | Garcia, A.L.; Reardon, R.; McDonald, M.; Vargas-Garcia, E.J. Community Interventions to Improve Cooking Skills and Their Effects on Confidence and Eating Behaviour. Current Nutrition Reports 2016, 5, 315–322, doi:10.1007/s13668-016-0185-3. (p. 316) |
| “…food literacy is a complex phenomenon made up of multiple attributes, including those that are both intrinsic and extrinsic. By conceptualizing these attributes, the results of the present scoping review provide the foundation for the development of a measurement tool that can support monitoring and the evaluation of interventions to support food literacy.” | Perry, E.A.; Thomas, H.; Samra, H.R.; Edmonstone, S.; Davidson, L.; Faulkner, A.; Petermann, L.; Manafò, E.; Kirkpatrick, S.I. Identifying attributes of food literacy: A scoping review. Public Health Nutrition 2017, 20, 2406–2415, doi:10.1017/S1368980017001276. (p. 2413) |
| “Food Literacy (FL) is the combination of knowledge, skills, and behaviours required to plan, select, manage, prepare, and consume foods that meet nutritional recommendations. Understood to be an important component of healthy living, FL is associated with confidence, autonomy, and empowerment towards food.” | Bomfim, M.C.C.; Wallace, J.R. Pirate bri’s grocery adventure: Teaching food literacy through shopping. In Proceedings of the Conference on Human Factors in Computing Systems—Proceedings, 2018., (p. 2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, P.; Araújo, R.; Lopes, F.; Ray, S. Nutrition and Food Literacy: Framing the Challenges to Health Communication. Nutrients 2023, 15, 4708. https://doi.org/10.3390/nu15224708
Silva P, Araújo R, Lopes F, Ray S. Nutrition and Food Literacy: Framing the Challenges to Health Communication. Nutrients. 2023; 15(22):4708. https://doi.org/10.3390/nu15224708
Chicago/Turabian StyleSilva, Paula, Rita Araújo, Felisbela Lopes, and Sumantra Ray. 2023. "Nutrition and Food Literacy: Framing the Challenges to Health Communication" Nutrients 15, no. 22: 4708. https://doi.org/10.3390/nu15224708
APA StyleSilva, P., Araújo, R., Lopes, F., & Ray, S. (2023). Nutrition and Food Literacy: Framing the Challenges to Health Communication. Nutrients, 15(22), 4708. https://doi.org/10.3390/nu15224708