Does Awareness of Malaysian Healthy Plate Associate with Adequate Fruit and Vegetable Intake among Malaysian Adults with Non-Communicable Diseases?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling
2.2. Ethical Consideration
2.3. Survey Materials and Data Collection
2.4. Study Variables
2.4.1. Independent Variable
2.4.2. Dependent Variable
2.4.3. Covariates
2.5. Statistical Analyses
3. Results
4. Discussion
5. Strengths, Limitations, and Future Works
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
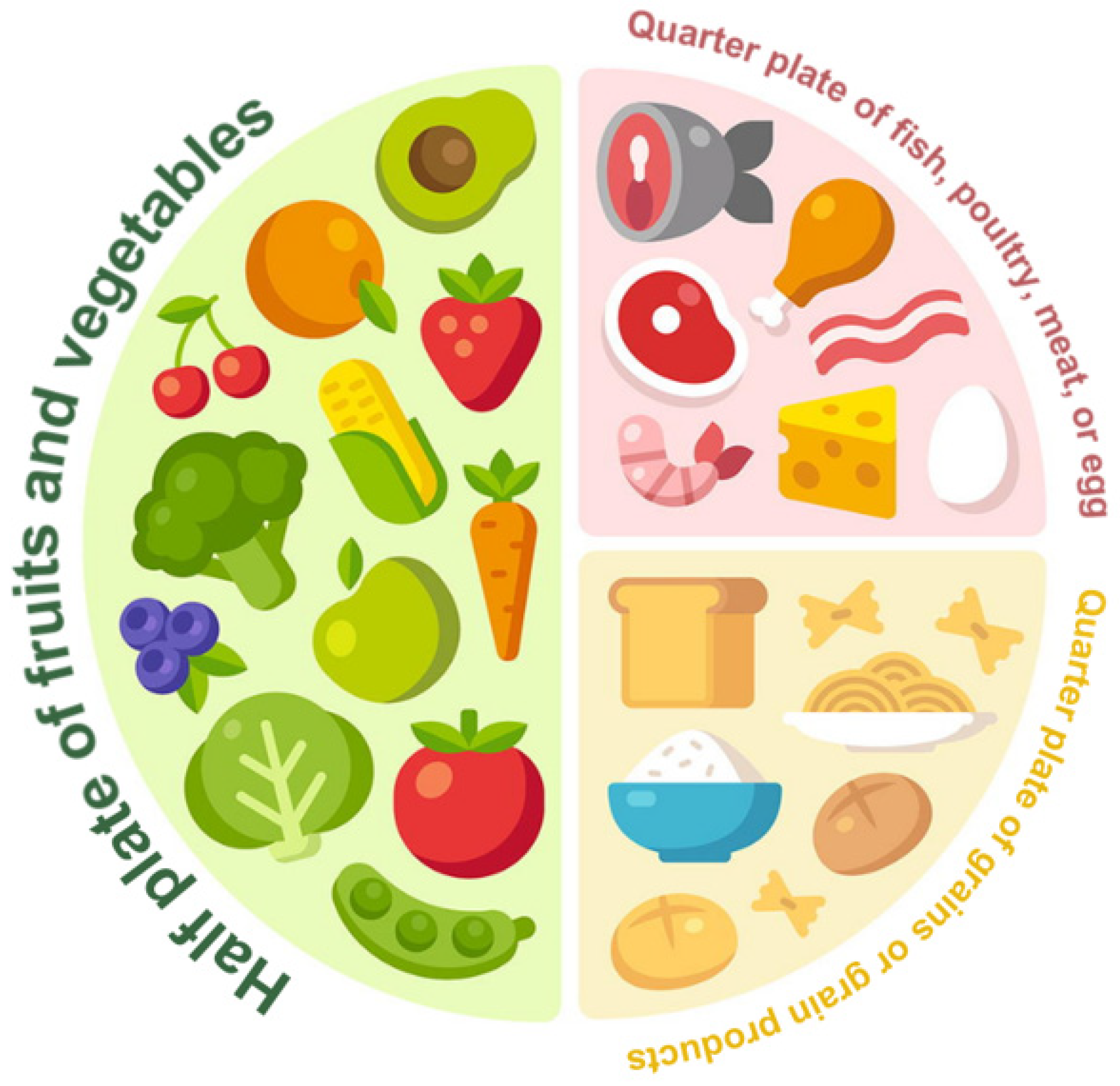
- Ministry of Health Malaysia: Panduan Pinggan Sihat Malaysia #Suku-Suku Separuh. 2016. Cawangan Penyakit Tidak Berjangkit Bahagian Kawalan Penyakit, Kementerian Kesihatan Malaysia. Putrajaya. Available online: https://www.moh.gov.my/index.php (accessed on 1 September 2023).
- National Coordinating Committee on Food and Nutrition. Malaysian Dietary Guidelines: Malaysian Dietary Guidelines; National Coordinating Committee on Food and Nutrition: Putrajaya, Malaysia, 2020.
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000.
- Mosher, A.L.; Piercy, K.L.; Webber, B.J.; Goodwin, S.K.; Casavale, K.O.; Olson, R.D. Dietary Guidelines for Americans: Implications for Primary Care Providers. Am. J. Lifestyle Med. 2016, 10, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-S.; Lay, S.; Yu, H.-N.; Shen, S.-R. Dietary Guidelines for Chinese Residents (2016): Comments and comparisons. J. Zhejiang Univ. B 2016, 17, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Yoshiike, N.; Hayashi, F.; Takemi, Y.; Mizoguchi, K.; Seino, F. A New Food Guide in Japan: The Japanese Food Guide Spinning Top. Nutr. Rev. 2008, 65, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Jayawardena, R.; Fernando, P.; Lokunarangoda, N.; Pathirana, A.K. Effects of the “plate model” as part of dietary intervention on modification of selected cardiometabolic risk factors in post-myocardial infarction patients: Study protocol for a randomized controlled trial. Trials 2017, 18, 314. [Google Scholar] [CrossRef] [PubMed]
- Trautwein, E.A.; McKay, S. The Role of Specific Components of a Plant-Based Diet in Management of Dyslipidemia and the Impact on Cardiovascular Risk. Nutrients 2020, 12, 2671. [Google Scholar] [CrossRef] [PubMed]
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014, 383, 1999–2007. [Google Scholar] [CrossRef] [PubMed]
- Castro, I.; Waclawovsky, G.; Marcadenti, A. Nutrition and Physical Activity on Hypertension: Implication of Current Evidence and Guidelines. Curr. Hypertens. Rev. 2015, 11, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.-S.; Sharp, S.J.; Imamura, F.; Chowdhury, R.; E Gundersen, T.; Steur, M.; Sluijs, I.; van der Schouw, Y.T.; Agudo, A.; Aune, D.; et al. Association of plasma biomarkers of fruit and vegetable intake with incident type 2 diabetes: EPIC-InterAct case-cohort study in eight European countries. BMJ 2020, 370, m2194. [Google Scholar] [CrossRef]
- Bertoia, M.L.; Mukamal, K.J.; Cahill, L.E.; Hou, T.; Ludwig, D.S.; Mozaffarian, D.; Willett, W.C.; Hu, F.B.; Rimm, E.B. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015, 12, e1001878. [Google Scholar] [CrossRef]
- Mohamad Hasnan, A.; Norsyamlina, C.A.R.; Cheong, S.M.; Ruhaya, S.; Munawara, P.; Wan Shakira, R.H.; Shubash, S.G.; Khairul Hasnan, A.; Noor Ani, A. Ever-never heard of ‘Malaysian Healthy Plate’: How many people know and practice this healthy eating concept? PLoS ONE 2023, 18, e0288325. [Google Scholar] [CrossRef]
- Institute for Public Health: Institute for Public Health (IPH), National Institutes of Health, Ministry of Health Malaysia. National Health and Morbidity Survey (NHMS) 2019: Vol. I: NCDs—Non-Communicable Diseases: Risk Factors and Other Health Problems; Institute for Public Health, National Institutes of Health, Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2020.
- CPG Secretariat. Clinical Practice Guidelines. Management of Type 2 Diabetes Mellitus, 6th ed.; CPG Secretariat: Putrajaya, Malaysia, 2020.
- CPG Secretariat. Clinical Practice Guidelines. Management of Hypertension, 5th ed.; CPG Secretariat: Putrajaya, Malaysia, 2018.
- Malaysia Health Technology Assessment Section (MaHTAS). Clinical Practice Guidelines. Management of Obesity, 2nd ed.; Malaysia Health Technology Assessment Section: Putrajaya, Malaysia, 2023. [Google Scholar]
- World Health Organization Western Pacific Region. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; World Health Organization: Geneva, Switzerland, 2000.
- R Development Core Team: R: A Language and Environment for Statistical Computing. 2009. Available online: https://www.R-project.org (accessed on 1 September 2023).
- Rahim, N.C.A.; Ahmad, M.H.; Man, C.S.; Zainuddin, A.A.; Hasani, W.S.R.; Ganapathy, S.S.; Ahmad, N.A. Factors Influencing the Levels of Awareness on Malaysian Healthy Plate Concept among Rural Adults in Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 6257. [Google Scholar] [CrossRef] [PubMed]
- Noh, S.N.M.; Jawahir, S.; Tan, Y.R.; Ab Rahim, I.; Tan, E.H. The Health-Seeking Behavior among Malaysian Adults in Urban and Rural Areas Who Reported Sickness: Findings from the National Health and Morbidity Survey (NHMS) 2019. Int. J. Environ. Res. Public Health 2022, 19, 3193. [Google Scholar] [CrossRef]
- Al-Salmi, N.; Cook, P.; D’souza, M.S. Diet Adherence among Adults with Type 2 Diabetes Mellitus: A Concept Analysis. Oman Med. J. 2022, 37, e361. [Google Scholar] [CrossRef] [PubMed]
- Appannah, G.; Murray, K.; Trapp, G.; Dymock, M.; Oddy, W.H.; Ambrosini, G.L. Dietary pattern trajectories across adolescence and early adulthood and their associations with childhood and parental factors. Am. J. Clin. Nutr. 2021, 113, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Chong, M.F.-F. Dietary trajectories through the life course: Opportunities and challenges. Br. J. Nutr. 2022, 128, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Ishak, S.I.Z.S.; Chin, Y.S.; Taib, M.N.M.; Chan, Y.M.; Shariff, Z.M. Effectiveness of a school-based intervention on knowledge, attitude and practice on healthy lifestyle and body composition in Malaysian adolescents. BMC Pediatr. 2020, 20, 122. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, H.; Wang, Z.; Huang, F.; Zhang, X.; Du, W.; Su, C.; Ouyang, Y.; Li, L.; Bai, J.; et al. Trajectories of Dietary Patterns and Their Associations with Overweight/Obesity among Chinese Adults: China Health and Nutrition Survey 1991–2018. Nutrients 2021, 13, 2835. [Google Scholar] [CrossRef]
- Kaikkonen, J.E.; Mikkilä, V.; Magnussen, C.G.; Juonala, M.; Viikari, J.S.A.; Raitakari, O.T. Does childhood nutrition influence adult cardiovascular disease risk?—Insights from the Young Finns Study. Ann. Med. 2013, 45, 120–128. [Google Scholar] [CrossRef]
- Eng, C.W.; Lim, S.C.; Ngongo, C.; Sham, Z.H.; Kataria, I.; Chandran, A.; Mustapha, F.I. Dietary practices, food purchasing, and perceptions about healthy food availability and affordability: A cross-sectional study of low-income Malaysian adults. BMC Public Health 2022, 22, 192. [Google Scholar] [CrossRef]
- Pestoni, G.; Krieger, J.-P.; Sych, J.M.; Faeh, D.; Rohrmann, S. Cultural Differences in Diet and Determinants of Diet Quality in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2019, 11, 126. [Google Scholar] [CrossRef]
- Ashari, L.S.; Rashid, A.A.A.; Shahril, M.R.; Lee, Y.Y.; Kueh, Y.C.; Hakim, B.N.A.; Shafiee, N.H.; Ali, R.A.R.; Mohamed, H.J.J. Exploring the norms of eating-out practice among adults in Malaysia. Mal. J. Nutr. 2022, 28, 031–041. [Google Scholar] [CrossRef]
- Von Goh, E.; Azam-Ali, S.; McCullough, F.; Mitra, S.R. The nutrition transition in Malaysia; key drivers and recommendations for improved health outcomes. BMC Nutr. 2020, 6, 32. [Google Scholar] [CrossRef]
- Lachat, C.; Nago, E.; Verstraeten, R.; Roberfroid, D.; Van Camp, J.; Kolsteren, P. Eating out of home and its association with dietary intake: A systematic review of the evidence. Obes. Rev. 2012, 13, 329–346. [Google Scholar] [CrossRef]
- Gesteiro, E.; García-Carro, A.; Aparicio-Ugarriza, R.; González-Gross, M. Eating out of Home: Influence on Nutrition, Health, and Policies: A Scoping Review. Nutrients 2022, 14, 1265. [Google Scholar] [CrossRef] [PubMed]
- Seguin, R.A.; Aggarwal, A.; Vermeylen, F.; Drewnowski, A. Consumption Frequency of Foods Away from Home Linked with Higher Body Mass Index and Lower Fruit and Vegetable Intake among Adults: A Cross-Sectional Study. J. Environ. Public Health 2016, 2016, 3074241. [Google Scholar] [CrossRef] [PubMed]
- Alnasser, A. The palm or the plate? An assessment of dietary guideline promotion, awareness, and preferences among Saudis: Cross-sectional survey. BMC Public Health 2023, 23, 1984. [Google Scholar] [CrossRef]
- Lim, R.B.T.; Wee, W.K.; For, W.C.; Ananthanarayanan, J.A.; Soh, Y.H.; Goh, L.M.L.; Tham, D.K.T.; Wong, M.L. Correlates, Facilitators and Barriers of Healthy Eating Among Primary Care Patients with Prediabetes in Singapore—A Mixed Methods Approach. Nutrients 2019, 11, 1014. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Halvorsen, R.E.; Elvestad, M.; Molin, M.; Aune, D. Fruit and vegetable consumption and the risk of type 2 diabetes: A systematic review and dose–response meta-analysis of prospective studies. BMJ Nutr. Prev. Health 2021, 4, 519–531. [Google Scholar] [CrossRef]
- Aaseth, J.; Ellefsen, S.; Alehagen, U.; Sundfør, T.M.; Alexander, J. Diets and drugs for weight loss and health in obesity—An update. Biomed. Pharmacother. 2021, 140, 111789. [Google Scholar] [CrossRef]
- Rogers, H.L.; Hernando, S.P.; Fernández, S.N.; Sanchez, A.; Martos, C.; Moreno, M.; Grandes, G. Barriers and facilitators in the implementation of an evidence-based health promotion intervention in a primary care setting: A qualitative study. J. Heal. Organ. Manag. 2021, 35, 349–367. [Google Scholar] [CrossRef] [PubMed]



| Characteristic | Estimated Population | Count (n) | % | 95% CI 1 |
|---|---|---|---|---|
| Sociodemographic | ||||
| Gender | ||||
| Male | 9,430,670 | 4427 | 50.2 | 49.0–51.4 |
| Female | 9,367,092 | 5333 | 49.8 | 48.6–51.0 |
| Age group (years old) | ||||
| 18–39 | 9,828,210 | 3894 | 52.3 | 50.7–53.8 |
| 40–59 | 5,900,808 | 3465 | 31.4 | 30.0–32.9 |
| ≥60 | 3,068,744 | 2401 | 16.3 | 15.1–17.6 |
| Ethnicity | ||||
| Malay | 10,656,046 | 6655 | 56.7 | 52.4–60.9 |
| Chinese | 4,510,234 | 1315 | 24.0 | 20.1–28.3 |
| Indian | 1,174,130 | 639 | 6.2 | 5.0–7.8 |
| Others | 2,457,353 | 1151 | 13.1 | 11.0–15.4 |
| Residential area | ||||
| Urban | 14,753,184 | 5908 | 78.5 | 77.0–79.9 |
| Rural | 4,044,578 | 3852 | 21.5 | 20.1–23.0 |
| Marital status | ||||
| Single | 5,455,290 | 2071 | 29.0 | 27.3–30.8 |
| Married | 11,950,450 | 6619 | 63.6 | 61.6–65.5 |
| Widow/Widower/Divorcee | 1,392,022 | 1070 | 7.4 | 6.7–8.2 |
| Education level | ||||
| No formal education | 713,115 | 530 | 3.8 | 3.2–4.4 |
| Primary education | 3,111,533 | 2113 | 16.6 | 15.4–17.8 |
| Secondary education | 12,901,427 | 6218 | 68.6 | 67.0–70.3 |
| Tertiary education | 2,058,279 | 891 | 11.0 | 9.7–12.4 |
| Occupation status | ||||
| Employed | 11,618,678 | 5464 | 61.8 | 60.1–63.5 |
| Unemployed | 7,177,953 | 4295 | 38.2 | 36.5–39.9 |
| Monthly household income | ||||
| Bottom 40% | 11,117,530 | 6193 | 62.9 | 60.1–65.7 |
| Middle 40% | 4,842,580 | 2190 | 27.5 | 25.0–29.9 |
| Top 20% | 1,701,166 | 765 | 9.6 | 8.0–11.5 |
| Lifestyle | ||||
| Smoking | ||||
| Ever-smoker | 4,839,808 | 2340 | 25.7 | 24.3–27.3 |
| Never-smoker | 13,957,953 | 7420 | 74.3 | 72.7–75.7 |
| Characteristic | Estimated Population | Count (n) | Not Aware (n = 7201) | Aware (n = 2295) | p-Value | ||
|---|---|---|---|---|---|---|---|
| Prevalence (%) | 95% CI 1 | Prevalence (%) | 95% CI 1 | ||||
| Sociodemographic | |||||||
| Gender | <0.001 | ||||||
| Male | 9,430,670 | 4427 | 84.5 | 82.7–86.1 | 15.5 | 13.9–17.3 | |
| Female | 9,367,092 | 5333 | 69.5 | 67.2–71.7 | 30.5 | 28.3–32.8 | |
| Age group (years old) | <0.001 | ||||||
| 18–39 | 9,828,210 | 3894 | 73.8 | 71.4–76.0 | 26.2 | 24.0–28.6 | |
| 40–59 | 5,900,808 | 3465 | 76.7 | 74.3–78.9 | 23.3 | 21.1–25.7 | |
| ≥60 | 3,068,744 | 2401 | 88.2 | 85.9–90.1 | 11.8 | 9.9–14.1 | |
| Ethnicity | <0.001 | ||||||
| Malay | 10,656,046 | 6655 | 73.7 | 71.8–75.6 | 26.3 | 24.4–28.2 | |
| Chinese | 4,510,234 | 1315 | 82.2 | 78.3–85.5 | 17.8 | 14.5–21.7 | |
| Indian | 1,174,130 | 639 | 77.0 | 71.4–81.7 | 23.0 | 18.3–28.6 | |
| Others | 2,457,353 | 1151 | 81.9 | 78.2–85.1 | 18.1 | 14.9–21.8 | |
| Residential area | <0.001 | ||||||
| Urban | 14,753,184 | 5908 | 75.9 | 73.9–77.8 | 24.1 | 22.2–26.1 | |
| Rural | 4,044,578 | 3852 | 81.1 | 78.8–83.2 | 18.9 | 16.8–21.2 | |
| Marital status | <0.001 | ||||||
| Single | 5,455,290 | 2071 | 79.4 | 76.7–81.8 | 20.6 | 18.2–23.3 | |
| Married | 11,950,450 | 6619 | 75.1 | 73.1–76.9 | 24.9 | 23.1–26.9 | |
| Widow/Widower/Divorcee | 1,392,022 | 1070 | 84.9 | 81.6–87.8 | 15.1 | 12.2–18.4 | |
| Education level | <0.001 | ||||||
| No formal education | 713,115 | 530 | 93.8 | 89.7–96.3 | 6.2 | 3.7–10.3 | |
| Primary education | 3,111,533 | 2113 | 88.7 | 86.2–90.8 | 11.3 | 9.2–13.8 | |
| Secondary education | 12,901,427 | 6218 | 76.4 | 74.5–78.2 | 23.6 | 21.8–25.5 | |
| Tertiary education | 2,058,279 | 891 | 57.7 | 52.4–62.7 | 42.3 | 37.3–47.6 | |
| Occupation status | 0.01 | ||||||
| Employed | 11,618,678 | 5464 | 75.7 | 73.6–77.6 | 24.3 | 22.4–26.4 | |
| Unemployed | 7,177,953 | 4295 | 79.2 | 76.9–81.3 | 20.8 | 18.7–23.1 | |
| Monthly household income | <0.001 | ||||||
| Bottom 40% | 11,117,530 | 6193 | 79.0 | 77.2–80.7 | 21.0 | 19.3–22.8 | |
| Middle 40% | 4,842,580 | 2190 | 75.0 | 71.6–78.1 | 25.0 | 21.9–28.4 | |
| Top 20% | 1,701,166 | 765 | 68.9 | 63.6–73.8 | 31.1 | 26.2–36.4 | |
| Lifestyle | |||||||
| Smoking | <0.001 | ||||||
| Ever-smoker | 4,839,808 | 2340 | 85.0 | 82.4–87.2 | 15.0 | 12.8–17.6 | |
| Never-smoker | 13,957,953 | 7420 | 74.2 | 72.3–76.1 | 25.8 | 23.9–27.7 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, L.K.; Chua, E.H.; Mohd Ghazali, S.; Cheah, Y.K.; Jayaraj, V.J.; Kee, C.C. Does Awareness of Malaysian Healthy Plate Associate with Adequate Fruit and Vegetable Intake among Malaysian Adults with Non-Communicable Diseases? Nutrients 2023, 15, 5043. https://doi.org/10.3390/nu15245043
Tan LK, Chua EH, Mohd Ghazali S, Cheah YK, Jayaraj VJ, Kee CC. Does Awareness of Malaysian Healthy Plate Associate with Adequate Fruit and Vegetable Intake among Malaysian Adults with Non-Communicable Diseases? Nutrients. 2023; 15(24):5043. https://doi.org/10.3390/nu15245043
Chicago/Turabian StyleTan, Lay Kim, En Hong Chua, Sumarni Mohd Ghazali, Yong Kang Cheah, Vivek Jason Jayaraj, and Chee Cheong Kee. 2023. "Does Awareness of Malaysian Healthy Plate Associate with Adequate Fruit and Vegetable Intake among Malaysian Adults with Non-Communicable Diseases?" Nutrients 15, no. 24: 5043. https://doi.org/10.3390/nu15245043
APA StyleTan, L. K., Chua, E. H., Mohd Ghazali, S., Cheah, Y. K., Jayaraj, V. J., & Kee, C. C. (2023). Does Awareness of Malaysian Healthy Plate Associate with Adequate Fruit and Vegetable Intake among Malaysian Adults with Non-Communicable Diseases? Nutrients, 15(24), 5043. https://doi.org/10.3390/nu15245043









