Nutritional Management of Oncological Symptoms: A Comprehensive Review
Abstract
:1. Introduction
2. Material and Methods
2.1. Xerostomia
2.2. Stomatitis
2.3. Diarrhea
2.4. Constipation
2.5. Nausea and Vomiting
2.6. Dysphagia
2.7. Sub-Occlusion
2.8. Dysgeusia and Dysosmia
2.9. Anorexia
2.10. Cachexia
2.11. Tailored Recipes
- First, the oncologic and nutritional teams defined clinically relevant scenarios often encountered in the oncology setting;
- Second, the oncologic and nutritional teams performed a literature research for publications about nutritional management in that clinical scenario;
- Third, a synoptical table (Table 1) to translate in plain language the crucial features of the nutritional approach for that clinical scenario was created;
- Fourth, a chef and his team used that table to create a tailored recipe;
- Fifth, these recipes were analyzed and revised by nutritional team in order to check their appropriateness for clinical scenarios;
- Sixth, the recipes were modified accordingly to the revisions;
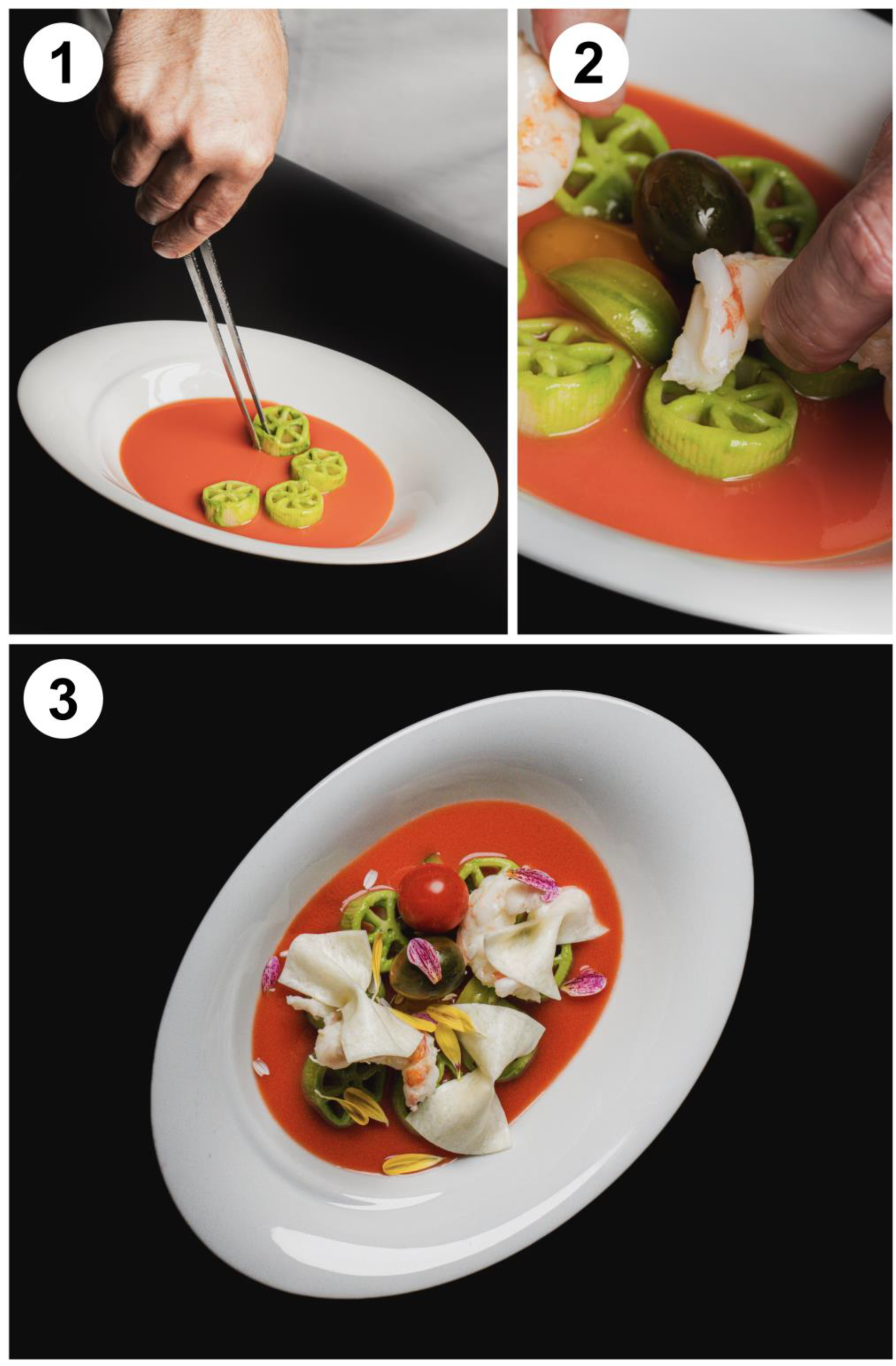
- Seventh, accepted recipes were implemented with a figure and detailed how-to instructions (Figure 3, Table 2, Supplementary File S1 for two additional recipes).
2.12. Implications and Future Perspectives
3. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef]
- Mantzorou, M.; Koutelidakis, A.; Theocharis, S.; Giaginis, C. Clinical Value of Nutritional Status in Cancer: What is its Impact and how it Affects Disease Progression and Prognosis? Nutr. Cancer 2017, 69, 1151–1176. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-H.; Hoang, T.; Kim, J. Dietary Factors and Breast Cancer Prognosis among Breast Cancer Survivors: A Systematic Review and Meta-Analysis of Cohort Studies. Cancers 2021, 13, 5329. [Google Scholar] [CrossRef]
- Ravasco, P. Nutrition in Cancer Patients. J. Clin. Med. 2019, 8, 1211. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tang, T.; Pang, L.; Sharma, S.V.; Li, R.; Nyitray, A.G.; Edwards, B.J. Malnutrition and overall survival in older adults with cancer: A systematic review and meta-analysis. J. Geriatr. Oncol. 2019, 10, 874–883. [Google Scholar] [CrossRef]
- Millsop, J.W.; Wang, E.A.; Fazel, N. Etiology, evaluation, and management of xerostomia. Clin. Dermatol. 2017, 35, 468–476. [Google Scholar] [CrossRef]
- Tanasiewicz, M.; Hildebrandt, T.; Obersztyn, I. Xerostomia of various etiologies: A review of the literature. Adv. Clin. Exp. Med. 2016, 25, 199–206. [Google Scholar] [CrossRef]
- Villa, A.; Connell, C.; Abati, S. Diagnosis and management of xerostomia and hyposalivation. Ther. Clin. Risk Manag. 2014, 45, 45–51. [Google Scholar] [CrossRef]
- Han, P.; Suarez-Durall, P.; Mulligan, R. Dry mouth: A critical topic for older adult patients. J. Prosthodont. Res. 2015, 59, 6–19. [Google Scholar] [CrossRef]
- Baharvand, M.; Khodadoustan, A.; Mohammadi, M.; Mortazavi, H.; Movahhedian, A. Xerostomia due to systemic disease: A review of 20 conditions and mechanisms. Ann. Med. Health Sci. Res. 2014, 4, 503. [Google Scholar] [CrossRef]
- Holmes, S. Xerostomia: Aetiology and management in cancer patients. Support. Care Cancer 1998, 6, 348–355. [Google Scholar] [CrossRef]
- Davies, A.; Buchanan, A.; Todd, J.; Gregory, A.; Batsari, K.M. Oral symptoms in patients with advanced cancer: An observational study using a novel oral symptom assessment scale. Support. Care Cancer 2021, 29, 4357–4364. [Google Scholar] [CrossRef]
- Fischer, D.J.; Epstein, J.B.; Yao, Y.; Wilkie, D.J. Oral health conditions affect functional and social activities of terminally ill cancer patients. Support. Care Cancer 2014, 22, 803–810. [Google Scholar] [CrossRef]
- Bressan, V.; Stevanin, S.; Bianchi, M.; Aleo, G.; Bagnasco, A.; Sasso, L. The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: A systematic review. Cancer Treat. Rev. 2016, 45, 105–119. [Google Scholar] [CrossRef]
- Jensen, S.B.; Vissink, A.; Limesand, K.H.; Reyland, M.E. Salivary Gland Hypofunction and Xerostomia in Head and Neck Radiation Patients. J. Natl. Cancer Inst. Monogr. 2019, 2019, lgz016. [Google Scholar] [CrossRef]
- Jensen, S.B.; Mouridsen, H.T.; Reibel, J.; Brünner, N.; Nauntofte, B. Adjuvant chemotherapy in breast cancer patients induces temporary salivary gland hypofunction. Oral. Oncol. 2008, 44, 162–173. [Google Scholar] [CrossRef]
- Mercadante, V.; Jensen, S.B.; Smith, D.K.; Bohlke, K.; Bauman, J.; Brennan, M.T.; Coppes, R.P.; Jessen, N.; Malhotra, N.K.; Murphy, B.; et al. Salivary Gland Hypofunction and/or Xerostomia Induced by Nonsurgical Cancer Therapies: ISOO/MASCC/ASCO Guideline. J. Clin. Oncol. 2021, 39, 2825–2843. [Google Scholar] [CrossRef]
- Jones, J.A.; Chavarri-Guerra, Y.; Corrêa, L.B.C.; Dean, D.R.; Epstein, J.B.; Fregnani, E.R.; Lee, J.; Matsuda, Y.; Mercadante, V.; Monsen, R.E.; et al. MASCC/ISOO expert opinion on the management of oral problems in patients with advanced cancer. Support. Care Cancer 2022, 30, 8761–8773. [Google Scholar] [CrossRef]
- Chitapanarux, I.; Kamnerdsupaphon, P.; Tharavichitkul, E.; Sumitsawan, Y.; Sittitrai, P.; Pattarasakulchai, T.; Lorvidhaya, V.; Sukthomya, V.; Pukanhaphan, N.; Traisatit, P. Effect of oral pilocarpine on post-irradiation xerostomia in head and neck cancer patients: A single-center, single-blind clinical trial. J. Med. Assoc. Thai 2008, 91, 1410–1415. [Google Scholar]
- Furness, S.; Worthington, H.v.; Bryan, G.; Birchenough, S.; McMillan, R. Interventions for the management of dry mouth: Topical therapies. Cochrane Database Syst. Rev. 2011, 2011, CD008934. [Google Scholar] [CrossRef]
- Ni, X.; Tian, T.; Chen, D.; Liu, L.; Li, X.; Li, F.; Liang, F.; Zhao, L. Acupuncture for Radiation-Induced Xerostomia in Cancer Patients: A Systematic Review and Meta-Analysis. Integr. Cancer Ther. 2020, 19, 1534735420980825. [Google Scholar] [CrossRef]
- American Cancer Society; Besser, J.; Grant, B. What to Eat during Cancer Treatment, 2nd ed.; American Cancer Society: Chicago, IL, USA, 2018. [Google Scholar]
- Bozorgi, C.; Holleufer, C.; Wendin, K. Saliva Secretion and Swallowing—The Impact of Different Types of Food and Drink on Subsequent Intake. Nutrients 2020, 12, 256. [Google Scholar] [CrossRef]
- Sonis, S.T. The pathobiology of mucositis. Nat. Rev. Cancer 2004, 4, 277–284. [Google Scholar] [CrossRef]
- Pulito, C.; Cristaudo, A.; La Porta, C.; Zapperi, S.; Blandino, G.; Morrone, A.; Strano, S. Oral mucositis: The hidden side of cancer therapy. J. Exp. Clin. Cancer Res. 2020, 39, 210. [Google Scholar] [CrossRef]
- Rozza-de-Menezes, R.; Souza, P.H.C.; Westphalen, F.H.; Ignácio, S.A.; Moysés, S.T.; Sarmento, V.A. Behaviour and Prevention of 5’Fluorouracil and Doxorubicin-induced Oral Mucositis in Immunocompetent Patients with Solid Tumors: A Randomised Trial. Oral Health Prev. Dent. 2018, 16, 549–555. [Google Scholar] [CrossRef]
- Wardill, H.R.; Sonis, S.T.; Blijlevens, N.M.A.; Van Sebille, Y.Z.A.; Ciorba, M.A.; Loeffen, E.A.H.; Cheng, K.K.F.; Bossi, P.; Porcello, L.; Castillo, D.A.; et al. Prediction of mucositis risk secondary to cancer therapy: A systematic review of current evidence and call to action. Support. Care Cancer 2020, 28, 5059–5073. [Google Scholar] [CrossRef]
- Watters, A.L.; Epstein, J.B.; Agulnik, M. Oral complications of targeted cancer therapies: A narrative literature review. Oral. Oncol. 2011, 47, 441–448. [Google Scholar] [CrossRef]
- Baselga, J.; Campone, M.; Piccart, M.; Burris, H.A., III; Rugo, H.S.; Sahmoud, T.; Noguchi, S.; Gnant, M.; Pritchard, K.I.; Lebrun, F.; et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N. Engl. J. Med. 2012, 366, 520–529. [Google Scholar] [CrossRef]
- Rugo, H.S.; Hortobagyi, G.N.; Yao, J.; Pavel, M.; Ravaud, A.; Franz, D.; Ringeisen, F.; Gallo, J.; Rouyrre, N.; Anak, O.; et al. Meta-analysis of stomatitis in clinical studies of everolimus: Incidence and relationship with efficacy. Ann. Oncol. 2016, 27, 519–525. [Google Scholar] [CrossRef]
- Barasch, A.; Peterson, D.E. Risk factors for ulcerative oral mucositis in cancer patients: Unanswered questions. Oral. Oncol. 2003, 39, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Mougeot, J.-L.C.; Stevens, C.B.; Morton, D.S.; Brennan, M.T.; Mougeot, F.B. Oral Microbiome and Cancer Therapy-Induced Oral Mucositis. J. Natl. Cancer Inst. Monogr. 2019, 2019, lgz002. [Google Scholar] [CrossRef]
- Bowen, J.; Al-Dasooqi, N.; Bossi, P.; Wardill, H.; van Sebille, Y.; Al-Azri, A.; Bateman, E.; Correa, M.E.; Raber-Durlacher, J.; Kandwal, A.; et al. The pathogenesis of mucositis: Updated perspectives and emerging targets. Support. Care Cancer 2019, 27, 4023–4033. [Google Scholar] [CrossRef]
- Fuchs, K.H.; DeMeester, T.R.; Otte, F.; Broderick, R.C.; Breithaupt, W.; Varga, G.; Musial, F. Severity of GERD and disease progression. Dis. Esophagus 2021, 34, doab006. [Google Scholar] [CrossRef]
- Eguchi, K.; Suzuki, M.; Ida, S.; Mori, K.; Imai, H.; Kudo, S.; Ando, K.; Higuchi, K.; Ebara, T. Association between Laryngopharyngeal Reflux and Radiation-induced Mucositis in Head and Neck Cancer. Anticancer Res. 2018, 38, 477–480. [Google Scholar] [CrossRef]
- Scully, C.; Sonis, S.; Diz, P.D. Oral mucositis. Oral. Dis. 2006, 12, 229–241. [Google Scholar] [CrossRef]
- Elting, L.S.; Cooksley, C.; Chambers, M.; Cantor, S.B.; Manzullo, E.; Rubenstein, E.B. The burdens of cancer therapy. Clinical and economic outcomes of chemotherapy-induced mucositis. Cancer 2003, 98, 1531–1539. [Google Scholar] [CrossRef]
- Elting, L.S.; Chang, Y.-C.; Parelkar, P.; Boers-Doets, C.B.; Michelet, M.; Hita, G.; Rouleau, T.; Cooksley, C.; Halm, J.; Vithala, M.; et al. Risk of oral and gastrointestinal mucosal injury among patients receiving selected targeted agents: A meta-analysis. Support. Care Cancer 2013, 21, 3243–3254. [Google Scholar] [CrossRef]
- Kumar, N.B. Nutritional Management of Cancer Treatment Effects; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar] [CrossRef]
- Ariyawardana, A.; Cheng, K.K.F.; Kandwal, A.; Tilly, V.; Al-Azri, A.R.; Galiti, D.; Chiang, K.; Vaddi, A.; Ranna, V.; Nicolatou-Galitis, O.; et al. Systematic review of anti-inflammatory agents for the management of oral mucositis in cancer patients and clinical practice guidelines. Support. Care Cancer 2019, 27, 3985–3995. [Google Scholar] [CrossRef] [PubMed]
- Elad, S.; Cheng, K.K.F.; Lalla, R.V.; Yarom, N.; Hong, C.; Logan, R.M.; Bowen, J.; Gibson, R.; Saunders, D.P.; Zadik, Y.; et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 2020, 126, 4423–4431. [Google Scholar] [CrossRef] [PubMed]
- Correa, M.E.P.; Cheng, K.K.F.; Chiang, K.; Kandwal, A.; Loprinzi, C.L.; Mori, T.; Potting, C.; Rouleau, T.; Toro, J.J.; Ranna, V.; et al. Systematic review of oral cryotherapy for the management of oral mucositis in cancer patients and clinical practice guidelines. Support. Care Cancer 2020, 28, 2449–2456. [Google Scholar] [CrossRef]
- Okada, N.; Hanafusa, T.; Abe, S.; Sato, C.; Nakamura, T.; Teraoka, K.; Abe, M.; Kawazoe, K.; Ishizawa, K. Evaluation of the risk factors associated with high-dose chemotherapy-induced dysgeusia in patients undergoing autologous hematopoietic stem cell transplantation: Possible usefulness of cryotherapy in dysgeusia prevention. Support. Care Cancer 2016, 24, 3979–3985. [Google Scholar] [CrossRef] [PubMed]
- Yarom, N.; Hovan, A.; Bossi, P.; Ariyawardana, A.; Jensen, S.B.; Gobbo, M.; Saca-Hazboun, H.; Kandwal, A.; Majorana, A.; Ottaviani, G.; et al. Systematic review of natural and miscellaneous agents for the management of oral mucositis in cancer patients and clinical practice guidelines-part 1: Vitamins, minerals, and nutritional supplements. Support. Care Cancer 2019, 27, 3997–4010. [Google Scholar] [CrossRef]
- Yarom, N.; Hovan, A.; Bossi, P.; Ariyawardana, A.; Jensen, S.B.; Gobbo, M.; Saca-Hazboun, H.; Kandwal, A.; Majorana, A.; Ottaviani, G.; et al. Systematic review of natural and miscellaneous agents, for the management of oral mucositis in cancer patients and clinical practice guidelines—Part 2: Honey, herbal compounds, saliva stimulants, probiotics, and miscellaneous agents. Support. Care Cancer 2020, 28, 2457–2472. [Google Scholar] [CrossRef] [PubMed]
- Santos-Silva, A.R.; Rosa, G.B.; Eduardo, C.P.; Dias, R.B.; Brandao, T.B. Increased risk for radiation-related caries in cancer patients using topical honey for the prevention of oral mucositis. Int. J. Oral. Maxillofac. Surg. 2011, 40, 1335–1336. [Google Scholar] [CrossRef]
- Chen, Q.-Y.; Kim, S.; Lee, B.; Jeong, G.; Lee, D.H.; Keum, N.; Manson, J.E.; Giovannucci, E.L. Post-Diagnosis Vitamin D Supplement Use and Survival among Cancer Patients: A Meta-Analysis. Nutrients 2022, 14, 3418. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef]
- Lappe, J.; Watson, P.; Travers-Gustafson, D.; Recker, R.; Garland, C.; Gorham, E.; Baggerly, K.; McDonnell, S.L. Effect of Vitamin D and Calcium Supplementation on Cancer Incidence in Older Women. JAMA 2017, 317, 1234. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 2019, 380, 33–44. [Google Scholar] [CrossRef]
- Vaughan-Shaw, P.G.; Buijs, L.F.; Blackmur, J.P.; Theodoratou, E.; Zgaga, L.; Din, F.V.N.; Farrington, S.M.; Dunlop, M.G. The effect of vitamin D supplementation on survival in patients with colorectal cancer: Systematic review and meta-analysis of randomised controlled trials. Br. J. Cancer 2020, 123, 1705–1712. [Google Scholar] [CrossRef]
- Kanno, K.; Akutsu, T.; Ohdaira, H.; Suzuki, Y.; Urashima, M. Effect of Vitamin D Supplements on Relapse or Death in a p53-Immunoreactive Subgroup with Digestive Tract Cancer. JAMA Netw. Open 2023, 6, e2328886. [Google Scholar] [CrossRef] [PubMed]
- Chandler, P.D.; Chen, W.Y.; Ajala, O.N.; Hazra, A.; Cook, N.; Bubes, V.; Lee, I.-M.; Giovannucci, E.L.; Willett, W.; Buring, J.E.; et al. Effect of Vitamin D3 Supplements on Development of Advanced Cancer. JAMA Netw. Open 2020, 3, e2025850. [Google Scholar] [CrossRef]
- Ng, K.; Nimeiri, H.S.; McCleary, N.J.; Abrams, T.A.; Yurgelun, M.B.; Cleary, J.M.; Rubinson, D.A.; Schrag, D.; Miksad, R.; Bullock, A.J.; et al. Effect of High-Dose vs Standard-Dose Vitamin D3 Supplementation on Progression-Free Survival among Patients with Advanced or Metastatic Colorectal Cancer. JAMA 2019, 321, 1370. [Google Scholar] [CrossRef]
- Urashima, M.; Ohdaira, H.; Akutsu, T.; Okada, S.; Yoshida, M.; Kitajima, M.; Suzuki, Y. Effect of Vitamin D Supplementation on Relapse-Free Survival among Patients with Digestive Tract Cancers. JAMA 2019, 321, 1361. [Google Scholar] [CrossRef]
- Barkokebas, A.; Silva, I.H.M.; de Andrade, S.C.; Carvalho, A.A.T.; Gueiros, L.A.M.; Paiva, S.M.; Leão, J.C. Impact of oral mucositis on oral-health-related quality of life of patients diagnosed with cancer. J. Oral. Pathol. Med. 2015, 44, 746–751. [Google Scholar] [CrossRef]
- Hong, C.H.L.; Gueiros, L.A.; Fulton, J.S.; Cheng, K.K.F.; Kandwal, A.; Galiti, D.; Fall-Dickson, J.M.; Johansen, J.; Ameringer, S.; Kataoka, T.; et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support. Care Cancer 2019, 27, 3949–3967. [Google Scholar] [CrossRef] [PubMed]
- Longo, D.; Fauci, A.; Kasper, D.; Hauser, S.; Jameson, J.; Loscalzo, J. Harrison’s Principles of Internal Medicine, 21st ed.; McGraw-Hill Education: New York, NY, USA, 2022; Volume 1. [Google Scholar]
- Forde, C. Systemic anti-cancer therapy-induced diarrhoea. Br. J. Hosp. Med. 2017, 78, C135–C139. [Google Scholar] [CrossRef] [PubMed]
- McQuade, R.M.; Stojanovska, V.; Abalo, R.; Bornstein, J.C.; Nurgali, K. Chemotherapy-Induced Constipation and Diarrhea: Pathophysiology, Current and Emerging Treatments. Front. Pharmacol. 2016, 7, 414. [Google Scholar] [CrossRef]
- Maroun, J.A.; Anthony, L.B.; Blais, N.; Burkes, R.; Dowden, S.D.; Dranitsaris, G.; Samson, B.; Shah, A.; Thirlwell, M.P.; Vincent, M.D.; et al. Prevention and management of chemotherapy-induced diarrhea in patients with colorectal cancer: A consensus statement by the Canadian Working Group on Chemotherapy-Induced Diarrhea. Curr. Oncol. 2007, 14, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Riddle, M.S.; DuPont, H.L.; Connor, B.A. ACG Clinical Guideline: Diagnosis, Treatment, and Prevention of Acute Diarrheal Infections in Adults. Am. J. Gastroenterol. 2016, 111, 602–622. [Google Scholar] [CrossRef]
- Wright, E.M.; Loo, D.D. Coupling between Na+, sugar, and water transport across the intestine. Ann. N. Y. Acad. Sci. 2000, 915, 54–66. [Google Scholar] [CrossRef]
- Gill, S.K.; Rossi, M.; Bajka, B.; Whelan, K. Dietary fibre in gastrointestinal health and disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Yang, J. Effect of dietary fiber on constipation: A meta analysis. World J. Gastroenterol. 2012, 18, 7378. [Google Scholar] [CrossRef] [PubMed]
- Benson, A.B.; Ajani, J.A.; Catalano, R.B.; Engelking, C.; Kornblau, S.M.; Martenson, J.A.; McCallum, R.; Mitchell, E.P.; O’Dorisio, T.M.; Vokes, E.E.; et al. Recommended Guidelines for the Treatment of Cancer Treatment-Induced Diarrhea. J. Clin. Oncol. 2004, 22, 2918–2926. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, N.K.; Suppiah, S.; Veettil, S.K.; Ching, S.M.; Lee, K.W.; Menon, R.K.; Soo, M.J.; Deuraseh, I.; Hoo, F.K.; Sivaratnam, D. The Effects of Probiotic Supplementation on the Incidence of Diarrhea in Cancer Patients Receiving Radiation Therapy: A Systematic Review with Meta-Analysis and Trial Sequential Analysis of Randomized Controlled Trials. Nutrients 2019, 11, 2886. [Google Scholar] [CrossRef] [PubMed]
- Goodman, C.; Keating, G.; Georgousopoulou, E.; Hespe, C.; Levett, K. Probiotics for the prevention of antibiotic-associated diarrhoea: A systematic review and meta-analysis. BMJ Open 2021, 11, e043054. [Google Scholar] [CrossRef]
- Atıcı, S.; Soysal, A.; Karadeniz Cerit, K.; Yılmaz, Ş.; Aksu, B.; Kıyan, G.; Bakır, M. Catheter-related Saccharomyces cerevisiae Fungemia Following Saccharomyces boulardii Probiotic Treatment: In a child in intensive care unit and review of the literature. Med. Mycol. Case Rep. 2017, 15, 33–35. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xia, S.; Jiang, X.; Feng, C.; Gong, S.; Ma, J.; Fang, Z.; Yin, J.; Yin, Y. Gut Microbiota and Diarrhea: An Updated Review. Front. Cell Infect. Microbiol. 2021, 11, 625210. [Google Scholar] [CrossRef]
- Österlund, P.; Ruotsalainen, T.; Peuhkuri, K.; Korpela, R.; Ollus, A.; Ikonen, M.; Joensuu, H.; Elomaa, I. Lactose intolerance associated with adjuvant 5-fluorouracil-based chemotherapy for colorectal cancer. Clin. Gastroenterol. Hepatol. 2004, 2, 696–703. [Google Scholar] [CrossRef]
- Sharma, A.; Rao, S.S.C.; Kearns, K.; Orleck, K.D.; Waldman, S.A. Review article: Diagnosis, management and patient perspectives of the spectrum of constipation disorders. Aliment. Pharmacol. Ther. 2021, 53, 1250–1267. [Google Scholar] [CrossRef]
- Serra, J.; Mascort-Roca, J.; Marzo-Castillejo, M.; Aros, S.D.; Santos, J.F.; Rubio, E.R.D.; Manrique, F.M. Clinical practice guidelines for the management of constipation in adults. Part 1: Definition, aetiology and clinical manifestations. Gastroenterol. Hepatol. 2017, 40, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Rao, S. Constipation: Pathophysiology and Current Therapeutic Approaches. Handb. Exp. Pharmacol. 2017, 239, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Viscusi, E.R. Clinical Overview and Considerations for the Management of Opioid-induced Constipation in Patients with Chronic Noncancer Pain. Clin. J. Pain. 2019, 35, 174–188. [Google Scholar] [CrossRef]
- Twycross, R.; Sykes, N.; Mihalyo, M.; Wilcock, A. Stimulant Laxatives and Opioid-Induced Constipation. J. Pain. Symptom Manage 2012, 43, 306–313. [Google Scholar] [CrossRef]
- Lacy, B.E.; Schey, R.; Shiff, S.J.; Lavins, B.J.; Fox, S.M.; Jia, X.D.; Blakesley, R.E.; Hao, X.; Cronin, J.A.; Currie, M.G.; et al. Linaclotide in Chronic Idiopathic Constipation Patients with Moderate to Severe Abdominal Bloating: A Randomized, Controlled Trial. PLoS ONE 2015, 10, e0134349. [Google Scholar] [CrossRef] [PubMed]
- Quigley, E.M.M.; Vandeplassche, L.; Kerstens, R.; Ausma, J. Clinical trial: The efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation—A 12-week, randomized, double-blind, placebo-controlled study. Aliment. Pharmacol. Ther. 2009, 29, 315–328. [Google Scholar] [CrossRef]
- Tuteja, A.K.; Rao, S.S.C. Lubiprostone for constipation and irritable bowel syndrome with constipation. Expert. Rev. Gastroenterol. Hepatol. 2008, 2, 727–733. [Google Scholar] [CrossRef]
- Davies, A.; Leach, C.; Caponero, R.; Dickman, A.; Fuchs, D.; Paice, J.; Emmanuel, A. MASCC recommendations on the management of constipation in patients with advanced cancer. Support. Care Cancer 2020, 28, 23–33. [Google Scholar] [CrossRef]
- Bellini, M.; Tonarelli, S.; Barracca, F.; Rettura, F.; Pancetti, A.; Ceccarelli, L.; Ricchiuti, A.; Costa, F.; de Bortoli, N.; Marchi, S.; et al. Chronic Constipation: Is a Nutritional Approach Reasonable? Nutrients 2021, 13, 3386. [Google Scholar] [CrossRef]
- Wickham, R.J. Managing Constipation in Adults With Cancer. J. Adv. Pract. Oncol. 2017, 8, 149–161. [Google Scholar]
- Ang, S.K.; Shoemaker, L.K.; Davis, M.P. Nausea and vomiting in advanced cancer. Am. J. Hosp. Palliat. Care 2010, 27, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Horn, C.C. Why is the neurobiology of nausea and vomiting so important? Appetite 2008, 50, 430–434. [Google Scholar] [CrossRef]
- D’arienzo, A.; Verrazzo, A.; Pagliuca, M.; Napolitano, F.; Parola, S.; Viggiani, M.; Caputo, R.; Puglisi, F.; Giuliano, M.; Del Mastro, L.; et al. Toxicity profile of antibody-drug conjugates in breast cancer: Practical considerations. EClinicalMedicine 2023, 62, 102113. [Google Scholar] [CrossRef] [PubMed]
- Bianchini, G.; Arpino, G.; Biganzoli, L.; Lonardi, S.; Puglisi, F.; Santini, D.; Lambertini, M.; Pappagallo, G. Emetogenicity of Antibody-Drug Conjugates (ADCs) in Solid Tumors with a Focus on Trastuzumab Deruxtecan: Insights from an Italian Expert Panel. Cancers 2022, 14, 1022. [Google Scholar] [CrossRef]
- Navari, R.M. Nausea and Vomiting in Advanced Cancer. Curr. Treat. Options Oncol. 2020, 21, 14. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, L.L.; Roscoe, J.A.; Olver, I.; Aapro, M.; Molassiotis, A. 2016 updated MASCC/ESMO consensus recommendations: Anticipatory nausea and vomiting in children and adults receiving chemotherapy. Support Care Cancer 2017, 25, 317–321. [Google Scholar] [CrossRef]
- Hesketh, P.J.; Kris, M.G.; Basch, E.; Bohlke, K.; Barbour, S.Y.; Clark-Snow, R.A.; Danso, M.A.; Dennis, K.; Dupuis, L.L.; Dusetzina, S.B.; et al. Antiemetics: ASCO Guideline Update. J. Clin. Oncol. 2020, 38, 2782–2797. [Google Scholar] [CrossRef]
- Davis, M.; Hui, D.; Davies, A.; Ripamonti, C.; Capela, A.; DeFeo, G.; Del Fabbro, E.; Bruera, E. MASCC antiemetics in advanced cancer updated guideline. Support. Care Cancer 2021, 29, 8097–8107. [Google Scholar] [CrossRef]
- Herrstedt, J.; Roila, F.; Warr, D.; Celio, L.; Navari, R.M.; Hesketh, P.J.; Chan, A.; Aapro, M.S. 2016 Updated MASCC/ESMO Consensus Recommendations: Prevention of Nausea and Vomiting Following High Emetic Risk Chemotherapy. Support Care Cancer 2017, 25, 277–288. [Google Scholar] [CrossRef]
- Roila, F.; Warr, D.; Hesketh, P.J.; Gralla, R.; Herrstedt, J.; Jordan, K.; Aapro, M.; Ballatori, E.; Rapoport, B. 2016 updated MASCC/ESMO consensus recommendations: Prevention of nausea and vomiting following moderately emetogenic chemotherapy. Support Care Cancer 2017, 25, 289–294. [Google Scholar] [CrossRef]
- Navari, R.M.; Aapro, M. Antiemetic Prophylaxis for Chemotherapy-Induced Nausea and Vomiting. N. Engl. J. Med. 2016, 374, 1356–1367. [Google Scholar] [CrossRef]
- Olver, I.; Ruhlmann, C.H.; Jahn, F.; Schwartzberg, L.; Rapoport, B.; Rittenberg, C.N.; Clark-Snow, R. 2016 Updated MASCC/ESMO Consensus Recommendations: Controlling nausea and vomiting with chemotherapy of low or minimal emetic potential. Support Care Cancer 2017, 25, 297–301. [Google Scholar] [CrossRef]
- Dibble, S.; Luce, J.; Cooper, B.; Israel, J.; Cohen, M.; Nussey, B.; Rugo, H. Acupressure for chemotherapy-induced nausea and vomiting: A randomized clinical trial. Oncol. Nurs. Forum 2007, 34, 813–820. [Google Scholar] [CrossRef]
- Molassiotis, A.; Helin, A.M.; Dabbour, R.; Hummerston, S. The effects of P6 acupressure in the prophylaxis of chemotherapy-related nausea and vomiting in breast cancer patients. Complement. Ther. Med. 2007, 15, 3–12. [Google Scholar] [CrossRef]
- Crichton, M.; Marshall, S.; Marx, W.; McCarthy, A.L.; Isenring, E. Efficacy of Ginger (Zingiber officinale) in Ameliorating Chemotherapy-Induced Nausea and Vomiting and Chemotherapy-Related Outcomes: A Systematic Review Update and Meta-Analysis. J. Acad. Nutr. Diet. 2019, 119, 2055–2068. [Google Scholar] [CrossRef]
- Smith, L.A.; Azariah, F.; Lavender, V.T.C.; Stoner, N.S.; Bettiol, S. Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst. Rev. 2015, 2015, CD009464. [Google Scholar] [CrossRef]
- Sanaati, F.; Najafi, S.; Kashaninia, Z.; Sadeghi, M. Effect of Ginger and Chamomile on Nausea and Vomiting Caused by Chemotherapy in Iranian Women with Breast Cancer. Asian Pac. J. Cancer Prev. 2016, 17, 4125–4129. [Google Scholar]
- Efe Ertürk, N.; Taşcı, S. The Effects of Peppermint Oil on Nausea, Vomiting and Retching in Cancer Patients Undergoing Chemotherapy: An Open Label Quasi–Randomized Controlled Pilot Study. Complement. Ther. Med. 2021, 56, 102587. [Google Scholar] [CrossRef]
- Abdolhosseini, S.; Hashem Dabaghian, F.; Mehrabani, M.; Mokaberinejad, R. A Review of Herbal Medicines for Nausea and Vomiting of Pregnancy in Traditional Persian Medicine. Galen. Med. J. 2017, 6, 281–290. [Google Scholar] [CrossRef]
- Marx, W.; Kiss, N.; McCarthy, A.L.; McKavanagh, D.; Isenring, L. Chemotherapy-Induced Nausea and Vomiting: A Narrative Review to Inform Dietetics Practice. J. Acad. Nutr. Diet. 2016, 116, 819–827. [Google Scholar] [CrossRef]
- Levine, M.E.; Gillis, M.G.; Koch, S.Y.; Voss, A.C.; Stern, R.M.; Koch, K.L. Protein and ginger for the treatment of chemotherapy-induced delayed nausea. J. Altern. Complement. Med. 2008, 14, 545–551. [Google Scholar] [CrossRef]
- Wickham, R.J. Revisiting the physiology of nausea and vomiting-challenging the paradigm. Support. Care Cancer 2020, 28, 13–21. [Google Scholar] [CrossRef]
- Kulbersh, B.D.; Rosenthal, E.L.; McGrew, B.M.; Duncan, R.D.; McColloch, N.L.; Carroll, W.R.; Magnuson, J.S. Pretreatment, Preoperative Swallowing Exercises May Improve Dysphagia Quality of Life. Laryngoscope 2006, 116, 883–886. [Google Scholar] [CrossRef]
- Tuca, A.; Guell, E.; Martinez-Losada, E.; Codorniu, N. Malignant bowel obstruction in advanced cancer patients: Epidemiology, management, and factors influencing spontaneous resolution. Cancer Manag. Res. 2012, 2012, 159–169. [Google Scholar] [CrossRef]
- Ripamonti, C.; Twycross, R.; Baines, M.; Bozzetti, F.; Capri, S.; De Conno, F.; Gemlo, B.; Hunt, T.M.; Hans, -B.K.; Mercadante, S.; et al. Clinical-practice recommendations for the management of bowel obstruction in patients with end-stage cancer. Support. Care Cancer 2001, 9, 223–233. [Google Scholar] [CrossRef]
- World Health Organization. Cancer Pain Relief: With a Guide to Opioid Availability, 2nd ed.; World Health Organization: Geneve, Switzerland, 1996. [Google Scholar]
- Madariaga, A.; Lau, J.; Ghoshal, A.; Dzierżanowski, T.; Larkin, P.; Sobocki, J.; Dickman, A.; Furness, K.; Fazelzad, R.; Crawford, G.B.; et al. MASCC multidisciplinary evidence-based recommendations for the management of malignant bowel obstruction in advanced cancer. Support. Care Cancer 2022, 30, 4711–4728. [Google Scholar] [CrossRef]
- Epstein, J.B.; Villines, D.; Epstein, G.L.; Smutzer, G. Oral examination findings, taste and smell testing during and following head and neck cancer therapy. Support. Care Cancer 2020, 28, 4305–4311. [Google Scholar] [CrossRef]
- Boesveldt, S.; Postma, E.M.; Boak, D.; Welge-Luessen, A.; Schöpf, V.; Mainland, J.D.; Martens, J.; Ngai, J.; Duffy, V.B. Anosmia-A Clinical Review. Chem. Senses 2017, 42, 513–523. [Google Scholar] [CrossRef]
- Bromley, S.M. Smell and taste disorders: A primary care approach. Am. Fam. Phys. 2000, 61, 427–436, 438. [Google Scholar]
- Comeau, T.B.; Epstein, J.B.; Migas, C. Taste and smell dysfunction in patients receiving chemotherapy: A review of current knowledge. Support. Care Cancer 2001, 9, 575–580. [Google Scholar] [CrossRef]
- Ripamonti, C.; Zecca, E.; Brunelli, C.; Fulfaro, F.; Villa, S.; Balzarini, A.; Bombardieri, E.; De Conno, F. A randomized, controlled clinical trial to evaluate the effects of zinc sulfate on cancer patients with taste alterations caused by head and neck irradiation. Cancer 1998, 82, 1938–1945. [Google Scholar] [CrossRef]
- Windfuhr, J.P.; Sack, F.; Sesterhenn, A.M.; Landis, B.N.; Chen, Y.-S. Post-tonsillectomy taste disorders. Eur. Arch. Otorhinolaryngol. 2010, 267, 289–293. [Google Scholar] [CrossRef]
- de Las Peñas, R.; Majem, M.; Perez-Altozano, J.; Virizuela, J.A.; Cancer, E.; Diz, P.; Donnay, O.; Hurtado, A.; Jimenez-Fonseca, P.; Ocon, M.J. SEOM clinical guidelines on nutrition in cancer patients (2018). Clin. Transl. Oncol. 2019, 21, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Copland, L.; Liedman, B.; Rothenberg, E.; Bosaeus, I. Effects of nutritional support long time after total gastrectomy. Clin. Nutr. 2007, 26, 605–613. [Google Scholar] [CrossRef]
- Ockenga, J.; Valentini, L. Review article: Anorexia and cachexia in gastrointestinal cancer. Aliment. Pharmacol. Ther. 2005, 22, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Arias, F.; Manterola, A.; Domínguez, M.A.; Martínez, E.; Villafranca, E.; Romero, P.; Vera, R. Acute dysphagia of oncological origin. Therapeutic management. An. Sist. Sanit. Navar. 2004, 27 (Suppl. S3), 109–115. [Google Scholar]
- Schwartz, M.W.; Dallman, M.F.; Woods, S.C. Hypothalamic response to starvation: Implications for the study of wasting disorders. Am. J. Physiol. 1995, 269, R949–R957. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, W.; Bała, M.; Jaeschke, R.; Krzakowski, M. Effects of megestrol acetate in patients with cancer anorexia-cachexia syndrome—A systematic review and meta-analysis. Pol. Arch. Med. Wewn. 2008, 118, 636–644. [Google Scholar] [CrossRef]
- Ruiz Garcia, V.; López-Briz, E.; Carbonell Sanchis, R.; Gonzalvez Perales, J.L.; Bort-Marti, S. Megestrol acetate for treatment of anorexia-cachexia syndrome. Cochrane Database Syst. Rev. 2013, 2013, CD004310. [Google Scholar] [CrossRef]
- Gullett, N.P.; Mazurak, V.C.; Hebbar, G.; Ziegler, T.R. Nutritional Interventions for Cancer-Induced Cachexia. Curr. Probl. Cancer 2011, 35, 58–90. [Google Scholar] [CrossRef]
- Navari, R.M.; Brenner, M.C. Treatment of cancer-related anorexia with olanzapine and megestrol acetate: A randomized trial. Support. Care Cancer 2010, 18, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, K.-P.; Zhang, X.; Tang, M.; Song, C.-H.; Cong, M.-H.; Guo, Z.-Q.; Ding, J.-S.; Braga, M.; Cederholm, T.; et al. Scored-GLIM as an effective tool to assess nutrition status and predict survival in patients with cancer. Clin. Nutr. 2021, 40, 4225–4233. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tang, M.; Zhang, Q.; Zhang, K.-P.; Guo, Z.-Q.; Xu, H.-X.; Yuan, K.-T.; Yu, M.; Braga, M.; Cederholm, T.; et al. The GLIM criteria as an effective tool for nutrition assessment and survival prediction in older adult cancer patients. Clin. Nutr. 2021, 40, 1224–1232. [Google Scholar] [CrossRef]
- Inui, A. Cancer anorexia-cachexia syndrome: Current issues in research and management. CA Cancer J. Clin. 2002, 52, 72–91. [Google Scholar] [CrossRef]
- van de Worp, W.R.P.H.; Schols, A.M.W.J.; Theys, J.; van Helvoort, A.; Langen, R.C.J. Nutritional Interventions in Cancer Cachexia: Evidence and Perspectives from Experimental Models. Front. Nutr. 2020, 7, 601329. [Google Scholar] [CrossRef] [PubMed]
- Bargetzi, L.; Brack, C.; Herrmann, J.; Bargetzi, A.; Hersberger, L.; Bargetzi, M.; Kaegi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; et al. Nutritional support during the hospital stay reduces mortality in patients with different types of cancers: Secondary analysis of a prospective randomized trial. Ann. Oncol. 2021, 32, 1025–1033. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Rubio-Zarapuz, A.; Martínez-Guardado, I.; Navarro-Jiménez, E.; Tornero-Aguilera, J.F. Nutritional and Exercise Interventions in Cancer-Related Cachexia: An Extensive Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 4604. [Google Scholar] [CrossRef]
- Tanaka, K.; Nakamura, S.; Narimatsu, H. Nutritional Approach to Cancer Cachexia: A Proposal for Dietitians. Nutrients 2022, 14, 345. [Google Scholar] [CrossRef]
- Navarro, D.A.; Boaz, M.; Krause, I.; Elis, A.; Chernov, K.; Giabra, M.; Levy, M.; Giboreau, A.; Kosak, S.; Mouhieddine, M.; et al. Improved meal presentation increases food intake and decreases readmission rate in hospitalized patients. Clin. Nutr. 2016, 35, 1153–1158. [Google Scholar] [CrossRef]
- Mullins, V.A.; Bresette, W.; Johnstone, L.; Hallmark, B.; Chilton, F.H. Genomics in Personalized Nutrition: Can You “Eat for Your Genes”? Nutrients 2020, 12, 3118. [Google Scholar] [CrossRef]
- Robinson, K.; Rozga, M.; Braakhuis, A.; Ellis, A.; Monnard, C.R.; Sinley, R.; Wanner, A.; Vargas, A.J. Effect of Incorporating Genetic Testing Results into Nutrition Counseling and Care on Dietary Intake: An Evidence Analysis Center Systematic Review-Part I. J. Acad. Nutr. Diet. 2021, 121, 553–581.e3. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Qu, Y.; Zhang, L.; Zhang, W.; Yan, P.; Yang, C.; Zhang, M.; Bai, Y.; Tang, M.; Wang, Y.; et al. Epidemiological and genetic evidence for the relationship between ABO blood group and human cancer. Int. J. Cancer 2023, 153, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, H.; Hajian, S.; Fadavi, E.; Sabour, S.; Baharvand, M.; Bakhtiari, S. ABO blood groups in oral cancer: A first case-control study in a defined group of Iranian patients. Asian Pac. J. Cancer Prev. 2014, 15, 1415–1418. [Google Scholar] [CrossRef]
- Verma, P.; Kumar, A.; Dixit, S.; Mohan, K.; Gupta, N.; Mandal, G. Assessment of Relationship of ABO Blood Groups in Oral Cancer Patients—A Retrospective Study. Ann. Maxillofac. Surg. 2021, 11, 80–85. [Google Scholar] [CrossRef]
- Garutti, M.; Foffano, L.; Mazzeo, R.; Michelotti, A.; Da Ros, L.; Viel, A.; Miolo, G.; Zambelli, A.; Puglisi, F. Hereditary Cancer Syndromes: A Comprehensive Review with a Visual Tool. Genes 2023, 14, 1025. [Google Scholar] [CrossRef]


| Xerostomia | Stomatitis | Diarrhea | Nausea/Vomiting | Dysphagia (Mechanical) | Dysphagia (Neurological) | Sub-Occlusion | Dysgeusia and Dysosmia | Anorexia | Cachexia | |
|---|---|---|---|---|---|---|---|---|---|---|
| Texture (IDDSI scale) | 0–5 | 0–4 | Any | Any | 0–4 | 3–5 | 0–4 | Any | Any | Any |
| Multiple textures | Any | Any | Any | Any | Avoid | Any | Any | Any | Any | Any |
| Temperature | Any | Low | Normal | Low | Any | Any | Any | Any to warm/hot | Any | Any |
| Sourness | Mild to high | Very low | Normal to low | Low | Any | Any | Any | Any | Any | Any |
| Sapidity | Any | Low to very low | Normal to low | Normal to low | Any | Any | Normal | Normal to very low | Any | Any |
| Spiciness | Any | Avoid | Low | Low | Any | Any | Normal to low | Normal to very high | Normal to very high | Normal to very high |
| Hydration | High | High | Low | Normal | High | High | High | Any | Any | Any |
| Fattiness | Normal | Normal | Low | Low to very low | High to very high | Normal | Any | High | High to very high | High to very high |
| Amount of fiber | Any | Any | Low to very low | Low | Avoid | Normal to avoid | Avoid | Any | Normal to low | Normal to low |
| Leading nutritional points | Proper oral hygiene Introducing different flavors Avoiding sour foods Acupuncture during and after radiation for H&N | Saline and sodium bicarbonate mouthwashes Oral cryotherapy Preferring soft or semisolid, mild-textured foods Opting for cool or room-temperature foods | Abundant oral liquids with solutions rich in electrolytes and glucose Probiotics supplementation Small and fractioned meals rich in soluble fibers Avoiding foods and beverages with high osmolarity, caffeine and theine | Eating small and frequent meals Having light snacks between meals Introducing ginger, chamomile, peppermint and cardamom Reducing liquid intake during meals Avoiding spicy, fatty, salty food and strong flavors Preferring bland foods, soft fruits or vegetables | Preferring more liquid forms of foods Reducing fiber content | Consuming small, fractionated semi-solid meals and thick liquids Prioritizing hard texture and fatty food Avoiding sticky or bulky foods, mixed textures | Consuming smaller meal portions Opting for a diet lower in fiber and softer-textured foods Selecting refined grains Avoiding foods with high fiber content, skins of fruits and vegetables | Preparing toppings or dressings Marinating meat or fish before cooking, or grilling them with acid products Opting for cold or lukewarm dishes Seasoning meat or fish with herbs and spices like rosemary, bay leaf, parsley, thyme, or Jamaica pepper Avoiding warm meals | Using toppings, contrasting colors, and serving small portions Opting for small, frequent meals, especially well-cooked and energy-rich foods, particularly in the morning Including high-calorie and high-protein foods in the diet (homemade smoothies, juices and cream soups) | Endorsing high-energy and high-protein foods with delicate aromas and flavors Preferring a homogeneous and creamy texture and a soft consistency Protein 1.5 g/day per kilogram of BW Opting for boiled, cooked, or grilled Adding fruit jams and honey to yogurt or salads and pairing aged cheese with soup |
| Fiori sulle farfalle (Flowers on butterflies) Preparation and servings for two people For the tomato soup: Ingredients:
For the cold pesto pasta: Ingredients:
For the mozzarella butterflies: Ingredients:
For the steamed langoustines: Ingredients:
Plating
| |
| Calories, Kcal | 484 |
| Proteins, g | 21 |
| Fats, g | 31 |
| Saturated fatty acids, g | 8 |
| Monounsaturated fatty acids, g | 18 |
| Polyunsaturated fatty acids, g | 3 |
| Carbohydrates, g | 31 |
| Sugars, g | 7 |
| Fiber, g | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garutti, M.; Noto, C.; Pastò, B.; Cucciniello, L.; Alajmo, M.; Casirati, A.; Pedrazzoli, P.; Caccialanza, R.; Puglisi, F. Nutritional Management of Oncological Symptoms: A Comprehensive Review. Nutrients 2023, 15, 5068. https://doi.org/10.3390/nu15245068
Garutti M, Noto C, Pastò B, Cucciniello L, Alajmo M, Casirati A, Pedrazzoli P, Caccialanza R, Puglisi F. Nutritional Management of Oncological Symptoms: A Comprehensive Review. Nutrients. 2023; 15(24):5068. https://doi.org/10.3390/nu15245068
Chicago/Turabian StyleGarutti, Mattia, Claudia Noto, Brenno Pastò, Linda Cucciniello, Massimiliano Alajmo, Amanda Casirati, Paolo Pedrazzoli, Riccardo Caccialanza, and Fabio Puglisi. 2023. "Nutritional Management of Oncological Symptoms: A Comprehensive Review" Nutrients 15, no. 24: 5068. https://doi.org/10.3390/nu15245068
APA StyleGarutti, M., Noto, C., Pastò, B., Cucciniello, L., Alajmo, M., Casirati, A., Pedrazzoli, P., Caccialanza, R., & Puglisi, F. (2023). Nutritional Management of Oncological Symptoms: A Comprehensive Review. Nutrients, 15(24), 5068. https://doi.org/10.3390/nu15245068










