Probiotic Supplementation Attenuates Chemotherapy-Induced Intestinal Mucositis in an Experimental Colorectal Cancer Liver Metastasis Rat Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experiment Design
2.3. Probiotics
2.4. Chemotherapy
2.5. Diarrhea Evaluation
2.6. Blood Tests
2.7. Immunohistochemical Staining
2.8. Intestine Crypt and Villi Length Analysis
2.9. Microbiome Analysis
2.10. Statistical Analysis
3. Results
3.1. Response to Chemotherapy
3.2. Diarrhea Assessment
3.3. Weight Change
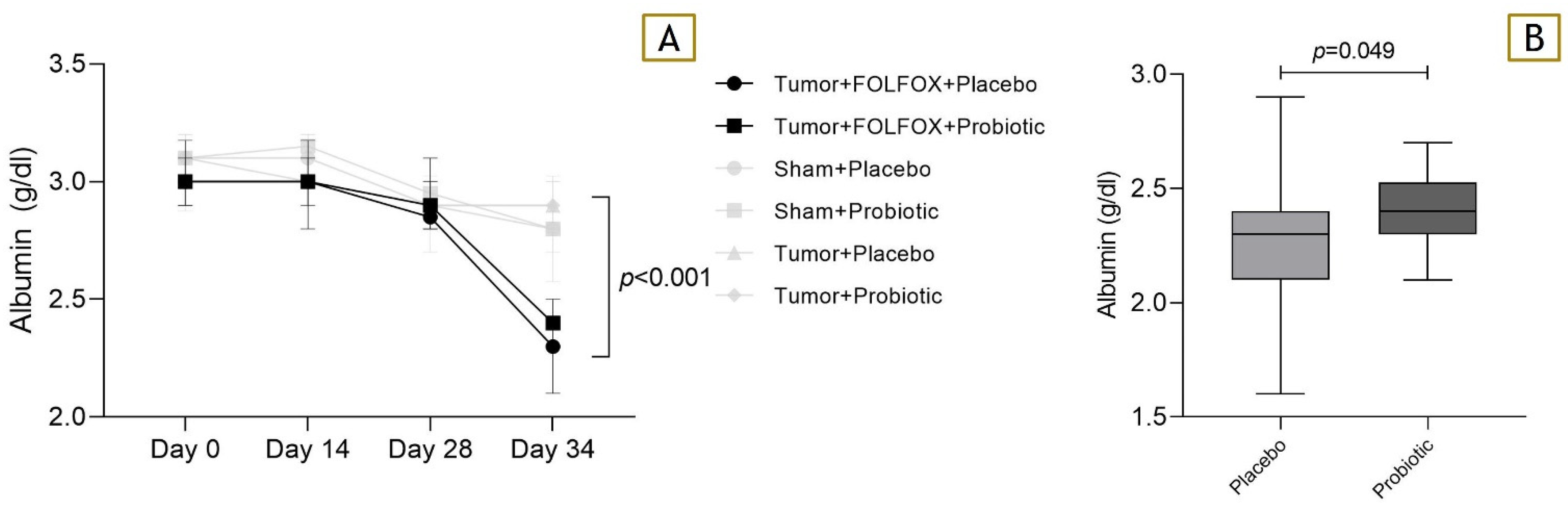
3.4. Blood Albumin Levels
3.5. Histopathological Examination
3.6. Associations between Adverse Effects and the Microbiome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Vogel, J.D.; Felder, S.I.; Bhama, A.R.; Hawkins, A.T.; Langenfeld, S.J.; Shaffer, V.O.; Thorsen, A.J.; Weiser, M.R.; Chang, G.J.; Lightner, A.L.; et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Colon Cancer. Dis. Colon Rectum 2022, 65, 148–177. [Google Scholar] [CrossRef] [PubMed]
- Villa, A.; Sonis, S.T. Mucositis: Pathobiology and Management. Curr. Opin. Oncol. 2015, 27, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Davila, M.; Bresalier, R.S. Gastrointestinal Complications of Oncologic Therapy. Nat. Rev. Gastroenterol. Hepatol. 2008, 5, 682–696. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, D.; Sjöblom, M.; Hellström, P.M.; Lennernäs, H. Chemotherapeutics-Induced Intestinal Mucositis: Pathophysiology and Potential Treatment Strategies. Front. Pharmacol. 2021, 12, 681417. [Google Scholar] [CrossRef] [PubMed]
- On behalf of The Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO); Bowen, J.; Al-Dasooqi, N.; Bossi, P.; Wardill, H.; Van Sebille, Y.; Al-Azri, A.; Bateman, E.; Correa, M.E.; Raber-Durlacher, J.; et al. The Pathogenesis of Mucositis: Updated Perspectives and Emerging Targets. Support. Care Cancer 2019, 27, 4023–4033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keefe, D.M.K.; Gibson, R.J.; Hauer-Jensen, M. Gastrointestinal Mucositis. Semin. Oncol. Nurs. 2004, 20, 38–47. [Google Scholar] [CrossRef]
- Miknevicius, P.; Zulpaite, R.; Leber, B.; Strupas, K.; Stiegler, P.; Schemmer, P. The Impact of Probiotics on Intestinal Mucositis during Chemotherapy for Colorectal Cancer: A Comprehensive Review of Animal Studies. Int. J. Mol. Sci. 2021, 22, 9347. [Google Scholar] [CrossRef]
- Ciorba, M.A.; Hallemeier, C.L.; Stenson, W.F.; Parikh, P.J. Probiotics to Prevent Gastrointestinal Toxicity from Cancer Therapy: An Interpretive Review and Call to Action. Curr. Opin. Support. Palliat. Care 2015, 9, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, B.; Delgado, S.; Blanco-Míguez, A.; Lourenço, A.; Gueimonde, M.; Margolles, A. Probiotics, Gut Microbiota, and Their Influence on Host Health and Disease. Mol. Nutr. Food Res. 2017, 61, 1600240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, C.-W.; Lee, H.-C.; Li, L.-H.; Chiang Chiau, J.-S.; Wang, T.-E.; Chuang, W.-H.; Chen, M.-J.; Wang, H.-Y.; Shih, S.-C.; Liu, C.-Y.; et al. Fecal Microbiota Transplantation Prevents Intestinal Injury, Upregulation of Toll-Like Receptors, and 5-Fluorouracil/Oxaliplatin-Induced Toxicity in Colorectal Cancer. Int. J. Mol. Sci. 2020, 21, 386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mi, H.; Dong, Y.; Zhang, B.; Wang, H.; Peter, C.C.K.; Gao, P.; Fu, H.; Gao, Y. Bifidobacterium Infantis Ameliorates Chemotherapy-Induced Intestinal Mucositis Via Regulating T Cell Immunity in Colorectal Cancer Rats. Cell. Physiol. Biochem. 2017, 42, 2330–2341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kvietkauskas, M.; Zitkute, V.; Leber, B.; Strupas, K.; Stiegler, P.; Schemmer, P. Dietary Melatonin and Glycine Decrease Tumor Growth through Antiangiogenic Activity in Experimental Colorectal Liver Metastasis. Nutrients 2021, 13, 2035. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Jacob, S. A Simple Practice Guide for Dose Conversion between Animals and Human. J. Basic Clin. Pharma. 2016, 7, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, R.J.; Bowen, J.M.; Inglis, M.R.; Cummins, A.G.; Keefe, D.M. Irinotecan Causes Severe Small Intestinal Damage, as Well as Colonic Damage, in the Rat with Implanted Breast Cancer. J. Gastroenterol. Hepatol. 2003, 18, 1095–1100. [Google Scholar] [CrossRef]
- Bankhead, P.; Loughrey, M.B.; Fernández, J.A.; Dombrowski, Y.; McArt, D.G.; Dunne, P.D.; McQuaid, S.; Gray, R.T.; Murray, L.J.; Coleman, H.G.; et al. QuPath: Open Source Software for Digital Pathology Image Analysis. Sci. Rep. 2017, 7, 16878. [Google Scholar] [CrossRef] [Green Version]
- Adelman, D.C.; Murray, J.; Wu, T.-T.; Mäki, M.; Green, P.H.; Kelly, C.P. Measuring Change In Small Intestinal Histology In Patients With Celiac Disease. Am. J. Gastroenterol. 2018, 113, 339–347. [Google Scholar] [CrossRef]
- Klymiuk, I.; Bambach, I.; Patra, V.; Trajanoski, S.; Wolf, P. 16S Based Microbiome Analysis from Healthy Subjects’ Skin Swabs Stored for Different Storage Periods Reveal Phylum to Genus Level Changes. Front. Microbiol. 2016, 7, 2012. [Google Scholar] [CrossRef]
- Kienesberger, B.; Obermüller, B.; Singer, G.; Mittl, B.; Grabherr, R.; Mayrhofer, S.; Heinl, S.; Stadlbauer, V.; Horvath, A.; Miekisch, W.; et al. (S)-Reutericyclin: Susceptibility Testing and In Vivo Effect on Murine Fecal Microbiome and Volatile Organic Compounds. Int. J. Mol. Sci. 2021, 22, 6424. [Google Scholar] [CrossRef]
- Sonis, S.T. Mucositis: The Impact, Biology and Therapeutic Opportunities of Oral Mucositis. Oral Oncol. 2009, 45, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-W.; Liu, C.-Y.; Lee, H.-C.; Huang, Y.-H.; Li, L.-H.; Chiau, J.-S.C.; Wang, T.-E.; Chu, C.-H.; Shih, S.-C.; Tsai, T.-H.; et al. Lactobacillus Casei Variety Rhamnosus Probiotic Preventively Attenuates 5-Fluorouracil/Oxaliplatin-Induced Intestinal Injury in a Syngeneic Colorectal Cancer Model. Front. Microbiol. 2018, 9, 983. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Gao, J.; Qian, L.; Gao, J.; Zhu, S.; Wu, M.; Zhang, Y.; Guan, W.; Ye, H.; Yu, Y.; et al. Exogenous IL-1Ra Attenuates Intestinal Mucositis Induced by Oxaliplatin and 5-Fluorouracil through Suppression of P53-Dependent Apoptosis. Anti Cancer Drugs 2015, 26, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Carnie, L.; Abraham, M.; McNamara, M.G.; Hubner, R.A.; Valle, J.W.; Lamarca, A. Impact on Prognosis of Early Weight Loss during Palliative Chemotherapy in Patients Diagnosed with Advanced Pancreatic Cancer. Pancreatology 2020, 20, 1682–1688. [Google Scholar] [CrossRef]
- Justino, P.F.C.; Melo, L.F.M.; Nogueira, A.F.; Morais, C.M.; Mendes, W.O.; Franco, A.X.; Souza, E.P.; Ribeiro, R.A.; Souza, M.H.L.P.; Soares, P.M.G. Regulatory Role of Lactobacillus Acidophilus on Inflammation and Gastric Dysmotility in Intestinal Mucositis Induced by 5-Fluorouracil in Mice. Cancer Chemother. Pharmacol. 2015, 75, 559–567. [Google Scholar] [CrossRef]
- Kato, S.; Hamouda, N.; Kano, Y.; Oikawa, Y.; Tanaka, Y.; Matsumoto, K.; Amagase, K.; Shimakawa, M. Probiotic Bifidobacterium Bifidum G9-1 Attenuates 5-Fluorouracil-Induced Intestinal Mucositis in Mice via Suppression of Dysbiosis-Related Secondary Inflammatory Responses. Clin. Exp. Pharmacol. Physiol. 2017, 44, 1017–1025. [Google Scholar] [CrossRef]
- Bowen, J.M.; Stringer, A.M.; Gibson, R.J.; Yeoh, A.S.; Hannam, S.; Keefe, D.M. VSL#3 Probiotic Treatment Reduces Chemotherapy-Induced Diarrhoea and Weight Loss. Cancer Biol. Ther. 2007, 6, 1445–1450. [Google Scholar] [CrossRef]
- Lheureux, S.; Clarisse, B.; Launay-Vacher, V.; Gunzer, K.; Delcambre-Lair, C.; Bouhier-Leporrier, K.; Kaluzinski, L.; Maron, D.; Ngo, M.-D.; Grossi, S.; et al. Evaluation of Current Practice: Management of Chemotherapy-Related Toxicities. Anti-Cancer Drugs 2011, 22, 919–925. [Google Scholar] [CrossRef]
- Yokota, T.; Ando, N.; Igaki, H.; Shinoda, M.; Kato, K.; Mizusawa, J.; Katayama, H.; Nakamura, K.; Fukuda, H.; Kitagawa, Y. Prognostic Factors in Patients Receiving Neoadjuvant 5-Fluorouracil plus Cisplatin for Advanced Esophageal Cancer (JCOG9907). Oncology 2015, 89, 143–151. [Google Scholar] [CrossRef]
- Vehreschild, M.J.G.T.; Vehreschild, J.J.; Hübel, K.; Hentrich, M.; Schmidt-Hieber, M.; Christopeit, M.; Maschmeyer, G.; Schalk, E.; Cornely, O.A.; Neumann, S. Diagnosis and Management of Gastrointestinal Complications in Adult Cancer Patients: Evidence-Based Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann. Oncol. 2013, 24, 1189–1202. [Google Scholar] [CrossRef]
- Lu, K.; Dong, S.; Wu, X.; Jin, R.; Chen, H. Probiotics in Cancer. Front. Oncol. 2021, 11, 638148. [Google Scholar] [CrossRef]
- Cheng, W.Y.; Wu, C.-Y.; Yu, J. The Role of Gut Microbiota in Cancer Treatment: Friend or Foe? Gut 2020, 69, 1867–1876. [Google Scholar] [CrossRef]
- Jakubauskas, M.; Jakubauskiene, L.; Leber, B.; Horvath, A.; Strupas, K.; Stiegler, P.; Schemmer, P. Probiotic Supplementation Suppresses Tumor Growth in an Experimental Colorectal Cancer Liver Metastasis Model. Int. J. Mol. Sci. 2022, 23, 7674. [Google Scholar] [CrossRef] [PubMed]
- Yeung, C.-Y.; Chan, W.-T.; Jiang, C.-B.; Cheng, M.-L.; Liu, C.-Y.; Chang, S.-W.; Chiang Chiau, J.-S.; Lee, H.-C. Amelioration of Chemotherapy-Induced Intestinal Mucositis by Orally Administered Probiotics in a Mouse Model. PLoS ONE 2015, 10, e0138746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, J.M.; Gibson, R.J.; Cummins, A.G.; Keefe, D.M.K. Intestinal Mucositis: The Role of the Bcl-2 Family, P53 and Caspases in Chemotherapy-Induced Damage. Support. Care Cancer 2006, 14, 713–731. [Google Scholar] [CrossRef] [PubMed]
- van Vliet, M.J.; Harmsen, H.J.M.; de Bont, E.S.J.M.; Tissing, W.J.E. The Role of Intestinal Microbiota in the Development and Severity of Chemotherapy-Induced Mucositis. PLoS Pathog. 2010, 6, e1000879. [Google Scholar] [CrossRef] [Green Version]
- Montassier, E.; Batard, E.; Massart, S.; Gastinne, T.; Carton, T.; Caillon, J.; Le Fresne, S.; Caroff, N.; Hardouin, J.B.; Moreau, P.; et al. 16S RRNA Gene Pyrosequencing Reveals Shift in Patient Faecal Microbiota During High-Dose Chemotherapy as Conditioning Regimen for Bone Marrow Transplantation. Microb. Ecol. 2014, 67, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Stringer, A.M.; Al-Dasooqi, N.; Bowen, J.M.; Tan, T.H.; Radzuan, M.; Logan, R.M.; Mayo, B.; Keefe, D.M.K.; Gibson, R.J. Biomarkers of Chemotherapy-Induced Diarrhoea: A Clinical Study of Intestinal Microbiome Alterations, Inflammation and Circulating Matrix Metalloproteinases. Support. Care Cancer 2013, 21, 1843–1852. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.B.; Dieleman, L.A.; Ketabi, A.; Bibova, I.; Sawyer, M.B.; Xue, H.; Field, C.J.; Baracos, V.E.; Gänzle, M.G. Irinotecan (CPT-11) Chemotherapy Alters Intestinal Microbiota in Tumour Bearing Rats. PLoS ONE 2012, 7, e39764. [Google Scholar] [CrossRef]
- Xie, J.; Li, L.-F.; Dai, T.-Y.; Qi, X.; Wang, Y.; Zheng, T.-Z.; Gao, X.-Y.; Zhang, Y.-J.; Ai, Y.; Ma, L.; et al. Short-Chain Fatty Acids Produced by Ruminococcaceae Mediate α-Linolenic Acid Promote Intestinal Stem Cells Proliferation. Mol. Nutr. Food Res. 2022, 66, e2100408. [Google Scholar] [CrossRef]
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermúdez-Humarán, L.G.; Gratadoux, J.-J.; Blugeon, S.; Bridonneau, C.; Furet, J.-P.; Corthier, G.; et al. Faecalibacterium Prausnitzii Is an Anti-Inflammatory Commensal Bacterium Identified by Gut Microbiota Analysis of Crohn Disease Patients. Proc. Natl. Acad. Sci. USA 2008, 105, 16731–16736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, C.; Jiang, C.; Li, W.; Wei, J.; Hong, H.; Li, J.; Feng, L.; Wei, H.; Xin, H.; Chen, T. A Phase II Randomized Clinical Trial and Mechanistic Studies Using Improved Probiotics to Prevent Oral Mucositis Induced by Concurrent Radiotherapy and Chemotherapy in Nasopharyngeal Carcinoma. Front. Immunol. 2021, 12, 618150. [Google Scholar] [CrossRef] [PubMed]
- Schellekens, H.; Torres-Fuentes, C.; van de Wouw, M.; Long-Smith, C.M.; Mitchell, A.; Strain, C.; Berding, K.; Bastiaanssen, T.F.S.; Rea, K.; Golubeva, A.V.; et al. Bifidobacterium Longum Counters the Effects of Obesity: Partial Successful Translation from Rodent to Human. EBioMedicine 2021, 63, 103176. [Google Scholar] [CrossRef] [PubMed]







| CONTROL Tumor (−)/CTx (−) | Non FOLFOX Tumor (+)/CTx (−) | FOLFOX Tumor (+)/CTx (+) | ||||
|---|---|---|---|---|---|---|
| Gavage | Placebo | Probiotics | Placebo | Probiotics | Placebo | Probiotics |
| Start (n) | 10 | 10 | 15 | 15 | 20 | 20 |
| End (n) | 10 | 10 | 15 | 15 | 20 | 19 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakubauskas, M.; Jakubauskiene, L.; Leber, B.; Horvath, A.; Strupas, K.; Stiegler, P.; Schemmer, P. Probiotic Supplementation Attenuates Chemotherapy-Induced Intestinal Mucositis in an Experimental Colorectal Cancer Liver Metastasis Rat Model. Nutrients 2023, 15, 1117. https://doi.org/10.3390/nu15051117
Jakubauskas M, Jakubauskiene L, Leber B, Horvath A, Strupas K, Stiegler P, Schemmer P. Probiotic Supplementation Attenuates Chemotherapy-Induced Intestinal Mucositis in an Experimental Colorectal Cancer Liver Metastasis Rat Model. Nutrients. 2023; 15(5):1117. https://doi.org/10.3390/nu15051117
Chicago/Turabian StyleJakubauskas, Matas, Lina Jakubauskiene, Bettina Leber, Angela Horvath, Kestutis Strupas, Philipp Stiegler, and Peter Schemmer. 2023. "Probiotic Supplementation Attenuates Chemotherapy-Induced Intestinal Mucositis in an Experimental Colorectal Cancer Liver Metastasis Rat Model" Nutrients 15, no. 5: 1117. https://doi.org/10.3390/nu15051117






