Assessment of Vascular Function in Response to High-Fat and Low-Fat Ground Beef Consumption in Men
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. General Procedures
2.3. Sources of Ground Beef and Food Logs
2.4. Carotid–Femoral Pulse Wave Velocity
2.5. Flow-Mediated Dilation
2.6. Body Composition
2.7. Submaximal Oxygen Consumption
2.8. Statistical Analysis
3. Results
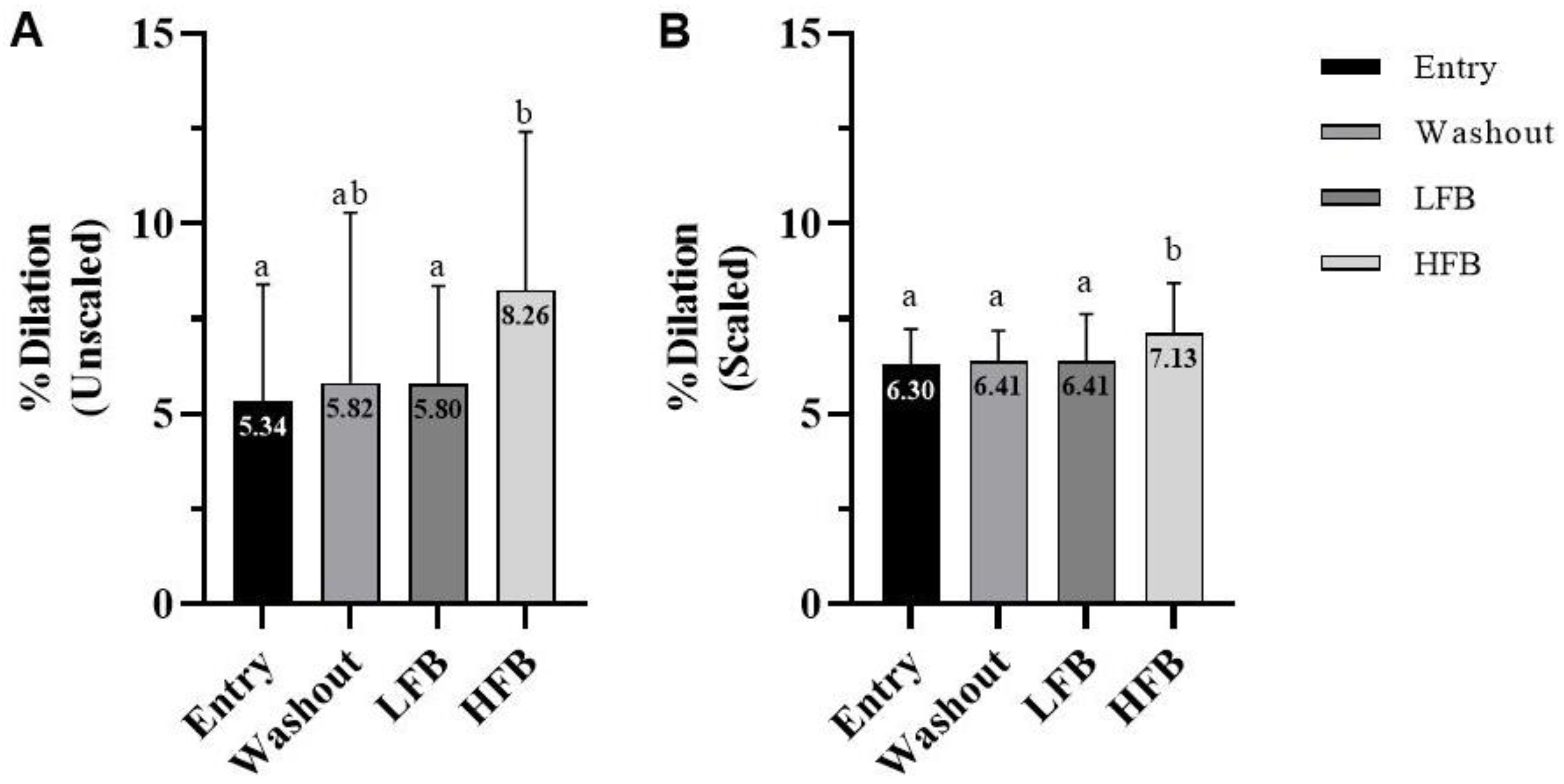
3.1. Flow-Mediated Dilation
3.2. Pulse Wave Velocity
3.3. Resting Blood Pressure
3.4. Dietary Analysis
3.5. Aerobic Fitness and Energy Expenditure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics—2016 Update. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.; Zimmet, P.; Shaw, J. The Metabolic Syndrome—A New Worldwide Definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.B.; Lunt, D.K.; Smith, D.R.; Walzem, R.L. Producing High-Oleic Acid Beef and the Impact of Ground Beef Consumption on Risk Factors for Cardiovascular Disease: A Review. Meat Sci. 2020, 163, 108076. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lin, X.; Ouyang, Y.Y.; Liu, J.; Zhao, G.; Pan, A.; Hu, F.B. Red and Processed Meat Consumption and Mortality: Dose–Response Meta-Analysis of Prospective Cohort Studies. Public Health Nutr. 2016, 19, 893–905. [Google Scholar] [CrossRef] [Green Version]
- Micha, R.; Michas, G.; Mozaffarian, D. Unprocessed Red and Processed Meats and Risk of Coronary Artery Disease and Type 2 Diabetes—An Updated Review of the Evidence. Curr. Atheroscler. Rep. 2012, 14, 515–524. [Google Scholar] [CrossRef] [Green Version]
- Al-Shaar, L.; Satija, A.; Wang, D.D.; Rimm, E.B.; Smith-Warner, S.A.; Stampfer, M.J.; Hu, F.B.; Willett, W.C. Red Meat Intake and Risk of Coronary Heart Disease among US Men: Prospective Cohort Study. BMJ 2020, 371, m4141. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, Y.; Satija, A.; Pan, A.; Sotos-Prieto, M.; Rimm, E.; Willett, W.C.; Hu, F.B. Association of Changes in Red Meat Consumption with Total and Cause Specific Mortality among US Women and Men: Two Prospective Cohort Studies. BMJ 2019, 365, l2110. [Google Scholar] [CrossRef] [Green Version]
- Bronzato, S.; Durante, A. A Contemporary Review of the Relationship between Red Meat Consumption and Cardiovascular Risk. Int. J. Prev. Med. 2017, 8, 40. [Google Scholar] [CrossRef]
- Lescinsky, H.; Afshin, A.; Ashbaugh, C.; Bisignano, C.; Brauer, M.; Ferrara, G.; Hay, S.I.; He, J.; Iannucci, V.; Marczak, L.B.; et al. Health Effects Associated with Consumption of Unprocessed Red Meat: A Burden of Proof Study. Nat. Med. 2022, 28, 2075–2082. [Google Scholar] [CrossRef]
- Quintana Pacheco, D.A.; Sookthai, D.; Wittenbecher, C.; Graf, M.E.; Schübel, R.; Johnson, T.; Katzke, V.; Jakszyn, P.; Kaaks, R.; Kühn, T. Red Meat Consumption and Risk of Cardiovascular Diseases—Is Increased Iron Load a Possible Link? Am. J. Clin. Nutr. 2018, 107, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Zeraatkar, D.; Han, M.A.; Guyatt, G.H.; Vernooij, R.W.M.; El Dib, R.; Cheung, K.; Milio, K.; Zworth, M.; Bartoszko, J.J.; Valli, C.; et al. Red and Processed Meat Consumption and Risk for All-Cause Mortality and Cardiometabolic Outcomes. Ann. Intern. Med. 2019, 171, 703–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vernooij, R.W.M.; Zeraatkar, D.; Han, M.A.; El Dib, R.; Zworth, M.; Milio, K.; Sit, D.; Lee, Y.; Gomaa, H.; Valli, C.; et al. Patterns of Red and Processed Meat Consumption and Risk for Cardiometabolic and Cancer Outcomes. Ann. Intern. Med. 2019, 171, 732–741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sitia, S.; Tomasoni, L.; Atzeni, F.; Ambrosio, G.; Cordiano, C.; Catapano, A.; Tramontana, S.; Perticone, F.; Naccarato, P.; Camici, P.; et al. From Endothelial Dysfunction to Atherosclerosis. Autoimmun. Rev. 2010, 9, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, D.H.J.; Black, M.A.; Pyke, K.E.; Padilla, J.; Atkinson, G.; Harris, R.A.; Parker, B.; Widlansky, M.E.; Tschakovsky, M.E.; Green, D.J. Assessment of Flow-Mediated Dilation in Humans: A Methodological and Physiological Guideline. Am. J. Physiol.-Heart Circ. Physiol. 2011, 300, H2–H12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chrysant, S.G. Noninvasive Vascular Function Tests for the Future Prediction of Primary Cardiovascular Diseases. Hosp. Pract. 2020, 48, 113–118. [Google Scholar] [CrossRef]
- Nabel, E.G.; Selwyn, A.P.; Ganz, P. Large Coronary Arteries in Humans Are Responsive to Changing Blood Flow: An Endothelium-Dependent Mechanism That Fails in Patients with Atherosclerosis. J. Am. Coll. Cardiol. 1990, 16, 349–356. [Google Scholar] [CrossRef] [Green Version]
- Heiss, C.; Rodriguez-Mateos, A.; Bapir, M.; Skene, S.S.; Sies, H.; Kelm, M. Flow-Mediated Dilation Reference Values for Evaluation of Endothelial Function and Cardiovascular Health. Cardiovasc. Res. 2022, cvac095. [Google Scholar] [CrossRef] [PubMed]
- Maruhashi, T.; Kajikawa, M.; Kishimoto, S.; Hashimoto, H.; Takaeko, Y.; Yamaji, T.; Harada, T.; Han, Y.; Aibara, Y.; Mohamad Yusoff, F.; et al. Diagnostic Criteria of Flow-Mediated Vasodilation for Normal Endothelial Function and Nitroglycerin-Induced Vasodilation for Normal Vascular Smooth Muscle Function of the Brachial Artery. J. Am. Heart Assoc. 2020, 9, e013915. [Google Scholar] [CrossRef]
- Mitchell, G.F.; Hwang, S.-J.; Vasan, R.S.; Larson, M.G.; Pencina, M.J.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J. Arterial Stiffness and Cardiovascular Events. Circulation 2010, 121, 505–511. [Google Scholar] [CrossRef] [Green Version]
- Nichols, W.W. Clinical Measurement of Arterial Stiffness Obtained from Noninvasive Pressure Waveforms. Am. J. Hypertens. 2005, 18, 3S–10S. [Google Scholar] [CrossRef]
- Mattace-Raso, F.U.S.; van der Cammen, T.J.M.; Hofman, A.; van Popele, N.M.; Bos, M.L.; Schalekamp, M.A.D.H.; Asmar, R.; Reneman, R.S.; Hoeks, A.P.G.; Breteler, M.M.B.; et al. Arterial Stiffness and Risk of Coronary Heart Disease and Stroke. Circulation 2006, 113, 657–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Rose, N.M.; Bots, M.L.; Siebelink, E.; Schouten, E.; Katan, M.B. Flow-Mediated Vasodilation Is Not Impaired When HDL-Cholesterol Is Lowered by Substituting Carbohydrates for Monounsaturated Fat. Br. J. Nutr. 2001, 86, 181–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Roos, N.M.; Bots, M.L.; Katan, M.B. Replacement of Dietary Saturated Fatty Acids by Trans Fatty Acids Lowers Serum HDL Cholesterol and Impairs Endothelial Function in Healthy Men and Women. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 1233–1237. [Google Scholar] [CrossRef] [Green Version]
- Sanders, T.; Lewis, F.; Frost, G.; Goff, L.; Chowienczyk, P. Impact of the Amount and Type of Fat and Carbohydrate on Vascular Function in the RISCK Study. Proc. Nutr. Soc. 2008, 67, E315. [Google Scholar] [CrossRef] [Green Version]
- Keogh, J.B.; Grieger, J.A.; Noakes, M.; Clifton, P.M. Flow-Mediated Dilatation Is Impaired by a High–Saturated Fat Diet but Not by a High-Carbohydrate Diet. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1274–1279. [Google Scholar] [CrossRef] [Green Version]
- Gokce, N.; Holbrook, M.; Duffy, S.J.; Demissie, S.; Cupples, L.A.; Biegelsen, E.; Keaney, J.F.; Loscalzo, J.; Vita, J.A. Effects of Race and Hypertension on Flow-Mediated and Nitroglycerin-Mediated Dilation of the Brachial Artery. Hypertension 2001, 38, 1349–1354. [Google Scholar] [CrossRef] [Green Version]
- Ghiadoni, L.; Taddei, S.; Virdis, A. Hypertension and Endothelial Dysfunction: Therapeutic Approach. Curr. Vasc. Pharmacol. 2012, 10, 42–60. [Google Scholar] [CrossRef] [PubMed]
- Beevers, G.; Lip, G.Y.H.; O’Brien, E. The Pathophysiology of Hypertension. BMJ 2001, 322, 912–916. [Google Scholar] [CrossRef]
- Ashton, E.L.; Pomeroy, S.; Foster, J.E.; Kaye, R.S.; Nestel, P.J.; Ball, M. Diet High in Monounsaturated Fat Does Not Have a Different Effect on Arterial Elasticity than a Low Fat, High Carbohydrate Diet. J. Am. Diet. Assoc. 2000, 100, 537–542. [Google Scholar] [CrossRef]
- Rasmussen, B.M.; Vessby, B.; Uusitupa, B.; Berglund, L.; Pederson, E.; Riccardi, G.; Rivellese, A.A.; Tapsell, L.; Hermansen, K. Effects of Dietary Saturated, Monounsaturated, and N−3 Fatty Acids on Blood Pressure in Healthy Subjects. Am. J. Clin. Nutr. 2006, 83, 221–226. [Google Scholar] [CrossRef] [Green Version]
- Lytle, J.R.; Price, T.; Crouse, S.F.; Smith, D.R.; Walzem, R.L.; Smith, S.B. Consuming High-Fat and Low-Fat Ground Beef Depresses High-Density and Low-Density Lipoprotein Cholesterol Concentrations, and Reduces Small, Dense Low-Density Lipoprotein Particle Abundance. Nutrients 2023, 15, 337. [Google Scholar] [CrossRef]
- Gilmore, L.A.; Walzem, R.L.; Crouse, S.F.; Smith, D.R.; Adams, T.H.; Vaidyanathan, V.; Cao, X.; Smith, S.B. Consumption of High-Oleic Acid Ground Beef Increases HDL-Cholesterol Concentration but Both High- and Low-Oleic Acid Ground Beef Decrease HDL Particle Diameter in Normocholesterolemic Men. J. Nutr. 2011, 141, 1188–1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuentes, F.; López-Miranda, J.; Sánchez, E.; Sánchez, F.; Paez, J.; Paz-Rojas, E.; Marín, C.; Gómez, P.; Jimenez-Perepérez, J.; Ordovás, J.M.; et al. Mediterranean and Low-Fat Diets Improve Endothelial Function in Hypercholesterolemic Men. Ann. Intern. Med. 2001, 134, 1115–1119. [Google Scholar] [CrossRef]
- Choi, S.H.; Gharahmany, G.; Walzem, R.L.; Meade, T.H.; Smith, S.B. Ground Beef High in Total Fat and Saturated Fatty Acids Decreases X Receptor Signaling Targets in Peripheral Blood Mononuclear Cells of Men and Women. Lipids 2018, 53, 279–290. [Google Scholar] [CrossRef]
- Blackmon, T.; Miller, R.K.; Kerth, C.; Smith, S.B. Ground Beef Patties Prepared from Brisket, Flank and Plate Have Unique Fatty Acid and Sensory Characteristics. Meat Sci. 2015, 103, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Adams, T.H.; Walzem, R.L.; Smith, D.R.; Tseng, S.; Smith, S.B. Hamburger High in Total, Saturated and Trans-Fatty Acids Decreases HDL Cholesterol and LDL Particle Diameter, and Increases TAG, in Mildly Hypercholesterolaemic Men. Br. J. Nutr. 2010, 103, 91–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilmore, L.A.; Crouse, S.F.; Carbuhn, A.; Klooster, J.; Calles, J.A.E.; Meade, T.; Smith, S.B. Exercise Attenuates the Increase in Plasma Monounsaturated Fatty Acids and High-Density Lipoprotein Cholesterol but Not High-Density Lipoprotein 2b Cholesterol Caused by High-Oleic Ground Beef in Women. Nutr. Res. 2013, 33, 1003–1011. [Google Scholar] [CrossRef]
- Van Bortel, L.M.; Laurent, S.; Boutouyrie, P.; Chowienczyk, P.; Cruickshank, J.K.; De Backer, T.; Filipovsky, J.; Huybrechts, S.; Mattace-Raso, F.U.S.; Protogerou, A.D.; et al. Expert Consensus Document on the Measurement of Aortic Stiffness in Daily Practice Using Carotid-Femoral Pulse Wave Velocity. J. Hypertens. 2012, 30, 445–448. [Google Scholar] [CrossRef] [Green Version]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard, H.M.; Herrington, D.; et al. Guidelines for the Ultrasound Assessment of Endothelial-Dependent Flow-Mediated Vasodilation of the Brachial Artery. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Greene, N.P.; Martin, S.E.; Crouse, S.F. Acute Exercise and Training Alter Blood Lipid and Lipoprotein Profiles Differently in Overweight and Obese Men and Women. Obesity 2012, 20, 1618–1627. [Google Scholar] [CrossRef]
- Crouse, S.F.; Green, J.S.; Meade, T.H.; Smith, D.R.; Smith, S.B. Exercise Raises High-Density Lipoprotein Cholesterol in Men after Consumption of Ground Beef with a High but Not Low Monounsaturated Fatty Acid–Saturated Fatty Acid Ratio. Nutr. Res. 2016, 36, 974–981. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-Predicted Maximal Heart Rate Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [Green Version]
- Bruce, R.A.; Kusumi, F.; Hosmer, D. Maximal Oxygen Intake and Nomographic Assessment of Functional Aerobic Impairment in Cardiovascular Disease. Am. Heart J. 1973, 85, 546–562. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.; Askew, W.; Bennett, D.; Mihalopoulos, J.; Anantharaman, S.; Fjeldstad, A.S.; Rule, D.C.; Nanjee, N.M.; Harris, R.A.; Richardson, R.S. Bison Meat Has a Lower Atherogenic Risk than Beef in Healthy Men. Nutr. Res. 2013, 33, 293–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosendorff, C. Effects of LDL Cholesterol on Vascular Function. J. Hum. Hypertens. 2002, 16, S26–S28. [Google Scholar] [CrossRef] [Green Version]
- Kosmas, C.E.; Christodoulidis, G.; Cheng, J.; Lerakis, S.; Vittorio, T.J. High-Density Lipoprotein Functionality in Coronary Artery Disease. Am. J. Med. Sci. 2014, 347, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Wood, R.; Tseng, S.; Smith, S.B. Increased Beef Consumption Increases Apolipoprotein A-I but Not Serum Cholesterol of Mildly Hypercholesterolemia Men with Different Levels of Habitual Beef Intake. Exp. Biol. Med. 2002, 227, 266–275. [Google Scholar] [CrossRef]
- Rasmussen, O.W.; Thomsen, C.; Hansen, K.W.; Vesterlund, M.; Winther, E.; Hermansen, K. Effects on Blood Pressure, Glucose, and Lipid Levels of High-Monounsaturated Fat Diet Compared with a High-Carbohydrate Diet in NIDDM Subjects. Diabetes Care 1993, 16, 1565–1571. [Google Scholar] [CrossRef]
- Williams, P.T.; Fortmann, S.P.; Terry, R.B.; Garay, S.C.; Vranizan, K.M.; Ellsworth, N.; Wood, P.D. Associations of Dietary Fat, Regional Adiposity, and Blood Pressure in Men. JAMA 1987, 257, 3251–3256. [Google Scholar] [CrossRef]
- Rubba, P.; Mancini, M.; Fidanza, F.; Gautiero, G.; Salo, M.; Nikkari, T.; Elton, R.; Oliver, M.F. Adipose Tissue Fatty Acids and Blood Pressure in Middle-Aged Men from Southern Italy. Int. J. Epidemiol. 1987, 16, 528–531. [Google Scholar] [CrossRef]
- McKnight, J.R.; Satterfield, M.C.; Jobgen, W.S.; Smith, S.B.; Spencer, T.E.; Meininger, C.J.; McNeal, C.J.; Wu, G. Beneficial Effects of L-Arginine on Reducing Obesity: Potential Mechanisms and Important Implications for Human Health. Amino Acids 2010, 39, 349–357. [Google Scholar] [CrossRef]
- Wu, G.; Cross, H.R.; Gehring, K.B.; Savell, J.W.; Arnold, A.N.; McNeill, S.H. Composition of Free and Peptide-Bound Amino Acids in Beef Chuck, Loin, and Round Cuts1,2. J. Anim. Sci. 2016, 94, 2603–2613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clevidence, B.; Fong, A.; Todd, K.; Brinkley, L.; Heiser, C.; Swain, J.; Rasmussen, H.; Tsay, R.; Oexmann, M.; Salbe, A. Planning Diet Studies. In Well-Controlled Diet Studies in Humans; Dennis, B.H., Ershow, A.G., Obarzanek, E., Clevidence, B.A., Eds.; The American Dietetic Association: Chicago, IL, USA, 1997; pp. 144–145. [Google Scholar]
- Bots, S.H.; Peters, S.A.E.; Woodward, M. Sex Differences in Coronary Heart Disease and Stroke Mortality: A Global Assessment of the Effect of Ageing between 1980 and 2010. BMJ Glob. Health 2017, 2, e000298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Prediction of Future Cardiovascular Outcomes by Flow-Mediated Vasodilatation of Brachial Artery: A Meta-Analysis. Int. J. Cardiovasc. Imaging 2010, 26, 631–640. [Google Scholar] [CrossRef] [PubMed]


| Entry (n = 23) | |
|---|---|
| Age (years) | 39.9 ± 10.8 |
| Height (cm) | 177.5 ± 6.7 |
| Body weight (kg) | 97.3 ± 25.0 |
| BMI (kg/m2) | 31.2 ± 9.0 |
| Lean mass (kg) | 64.5 ± 9.5 |
| Fat mass (kg) | 30.6 ± 19.1 |
| Body fat (%) | 29.9 ± 10.4 |
| Android fat (%) | 35.8 ± 14.1 |
| Gynoid fat (%) | 31.0 ± 9.8 |
| VO2max (mL/kg/min) | 37.9 ± 7.6 |
| Entry | Washout | LFB | HFB | |
|---|---|---|---|---|
| Baseline diameter (mm) | 4.45 ± 0.54 | 4.47 ± 0.60 | 4.48 ± 0.54 | 4.45 ± 0.61 |
| Peak diameter (mm) | 4.68 ± 0.57 | 4.73 ± 0.67 | 4.74 ± 0.58 | 4.81 ± 0.63 |
| Time to peak dilation (s) | 35.1 ± 20.4 | 32.3 ± 19.7 | 35.1 ± 22.5 | 28.4 ± 17.1 |
| Entry | Washout | LFB | HFB | |
|---|---|---|---|---|
| EN (kcal/day) | 2071 ± 491 a | 1966 ± 399 a | 1887 ± 401 a | 2071 ± 487 a |
| % EN CHO | 41.3 ± 8.6 a | 41.2 ± 7.4 ab | 40.3 ± 8.2 ab | 38.3 ± 8.8 b |
| % EN Protein | 18.6 ± 3.5 a | 18.9 ± 4.7 a | 22.0 ± 4.8 b | 18.4 ± 5.8 a |
| % EN Fat | 38.6 ± 6.0 a | 37.4 ± 6.6 a | 36.8 ± 6.6 a | 42.2 ± 8.7 b |
| Cholesterol (mg/d) | 437.2 ± 304.8 a | 330.4 ± 179.9 a | 344.8 ± 196.7 a | 321.7 ± 170.0 a |
| Protein (g/d) | 96.2 ± 28.5 a | 91.2 ± 22.8 a | 103.9 ± 32.5 a | 95.2 ± 38.2 a |
| CHO (g/d) | 212.5 ± 63.9 a | 202.4 ± 53.3 a | 188.7 ± 48.8 a | 197.5 ± 64.0 a |
| Fat (g/d) | 90.0 ± 28.0 a | 82.2 ± 24.6 a | 76.9 ± 19.1 a | 97.1 ± 30.8 b |
| SFAs (g/d) | 29.8 ± 9.5 a | 27.9 ± 8.8 a | 26.9 ± 8.5 a | 34.1 ± 13.0 b |
| MUFAs (g/d) | 15.7 ± 8.5 a | 15.3 ± 8.2 a | 15.7 ± 7.3 a | 22.9 ± 11.2 b |
| PUFAs (g/d) | 8.3 ± 4.3 a | 8.2 ± 4.2 a | 7.8 ± 4.9 a | 7.9 ± 3.6 a |
| TFAs (g/d) | 0.8 ± 0.8 a | 0.5 ± 0.5 a | 0.3 ± 0.4 a | 0.6 ± 0.8 a |
| n-6 fatty acids (g/d) | 6.2 ± 4.0 a | 5.7 ± 3.4 a | 5.4 ± 4.7 a | 5.1 ± 2.7 a |
| n-3 fatty acids (g/d) | 0.7 ± 0.7 a | 0.7 ± 0.5 a | 0.7 ± 0.6 a | 0.5 ± 0.3 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lytle, J.R.; Stanelle, S.T.; Martin, S.E.; Smith, S.B.; Smith, D.R.; Crouse, S.F. Assessment of Vascular Function in Response to High-Fat and Low-Fat Ground Beef Consumption in Men. Nutrients 2023, 15, 1410. https://doi.org/10.3390/nu15061410
Lytle JR, Stanelle ST, Martin SE, Smith SB, Smith DR, Crouse SF. Assessment of Vascular Function in Response to High-Fat and Low-Fat Ground Beef Consumption in Men. Nutrients. 2023; 15(6):1410. https://doi.org/10.3390/nu15061410
Chicago/Turabian StyleLytle, Jason R., Sean T. Stanelle, Steven E. Martin, Stephen B. Smith, Dana R. Smith, and Stephen F. Crouse. 2023. "Assessment of Vascular Function in Response to High-Fat and Low-Fat Ground Beef Consumption in Men" Nutrients 15, no. 6: 1410. https://doi.org/10.3390/nu15061410






