Serum Fibroblast Growth Factor 21 Is Markedly Decreased following Exercise Training in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design and Population
2.2. Laboratory Methods
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Change in Serum FGF21 following Exercise Training
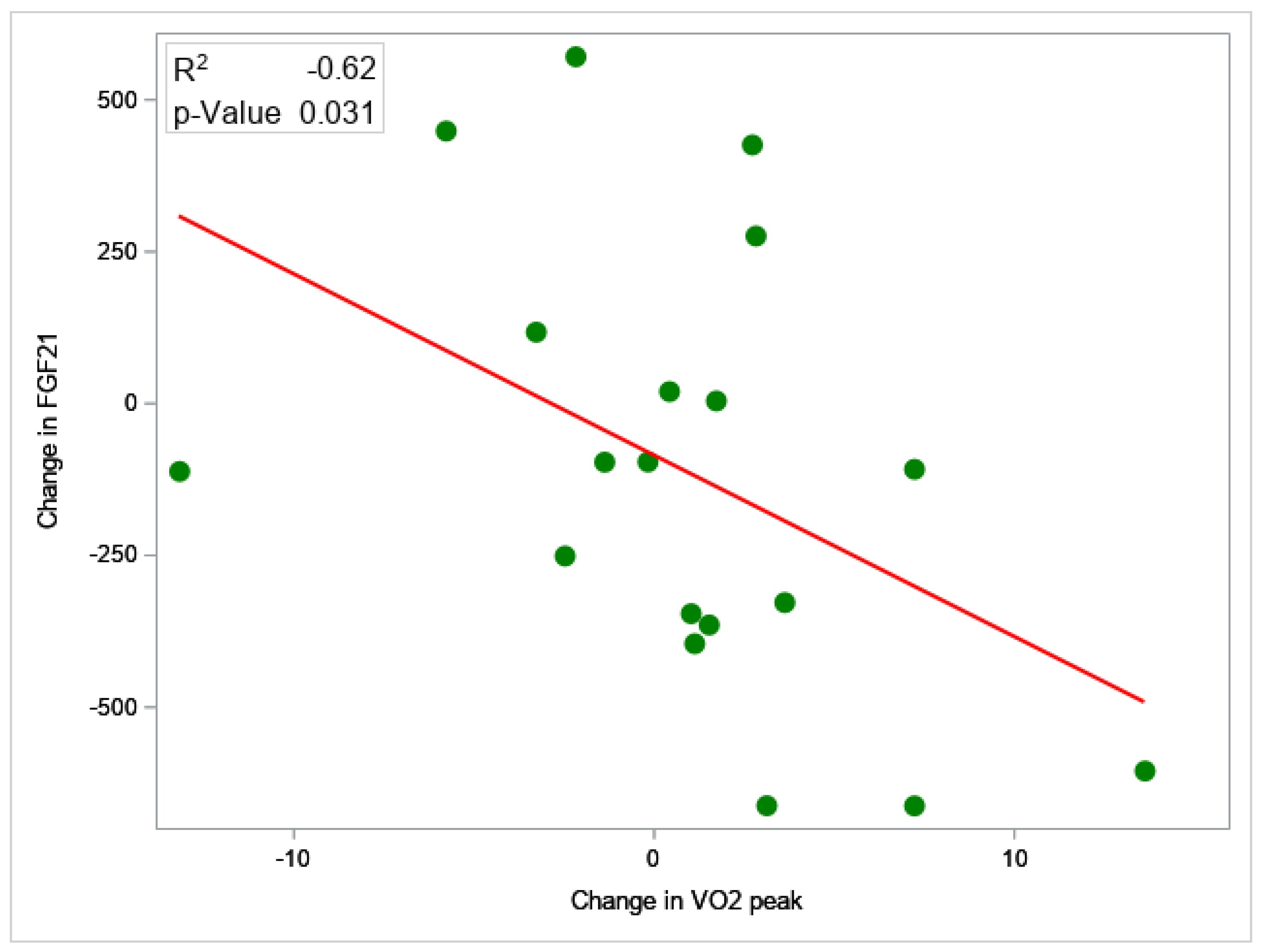
3.3. Change in Non-Invasive Tests for NASH
3.4. Change in Non-Hepatic Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Younossi, Z.M. Non-alcoholic fatty liver disease—A global public health perspective. J. Hepatol. 2019, 70, 531–544. [Google Scholar] [CrossRef]
- Simon, T.G.; Roelstraete, B.; Khalili, H.; Hagström, H.; Ludvigsson, J.F. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: Results from a nationwide cohort. Gut 2021, 70, 1375–1382. [Google Scholar] [CrossRef]
- Schneider, C.V.; Zandvakili, I.; Thaiss, C.A.; Schneider, K.M. Physical activity is associated with reduced risk of liver disease in the prospective UK Biobank cohort. JHEP Rep. Innov. Hepatol. 2021, 3, 100263. [Google Scholar] [CrossRef]
- Kim, D.; Murag, S.; Cholankeril, G.; Cheung, A.; Harrison, S.A.; Younossi, Z.M.; Ahmed, A. Physical Activity, Measured Objectively, Is Associated with Lower Mortality in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2021, 19, 1240–1247.e1245. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The Diagnosis and Management of Nonalcoholic Fatty Liver Disease: Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology 2017, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Lim, J.K.; Patton, H.; El-Serag, H.B. AGA Clinical Practice Update on Screening and Surveillance for Hepatocellular Carcinoma in Patients with Nonalcoholic Fatty Liver Disease: Expert Review. Gastroenterology 2020, 158, 1822–1830. [Google Scholar] [CrossRef] [PubMed]
- Stine, J.G.; Wentworth, B.J.; Zimmet, A.; Rinella, M.E.; Loomba, R.; Caldwell, S.H.; Argo, C.K. Systematic review with meta-analysis: Risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment. Pharmacol. Ther. 2018, 48, 696–703. [Google Scholar] [CrossRef]
- Thorp, A.; Stine, J.G. Exercise as Medicine: The Impact of Exercise Training on Nonalcoholic Fatty Liver Disease. Curr. Hepatol. Rep. 2020, 19, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Vilar-Gomez, E.; Martinez-Perez, Y.; Calzadilla-Bertot, L.; Torres-Gonzalez, A.; Gra-Oramas, B.; Gonzalez-Fabian, L.; Friedman, S.L.; Diago, M.; Romero-Gomez, M. Weight Loss through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology 2015, 149, 367–378.e365. [Google Scholar] [CrossRef] [PubMed]
- Cigrovski Berkovic, M.; Bilic-Curcic, I.; Mrzljak, A.; Cigrovski, V. NAFLD and Physical Exercise: Ready, Steady, Go! Front. Nutr. 2021, 8, 734859. [Google Scholar] [CrossRef] [PubMed]
- Stine, J.G.; Schreibman, I.R.; Faust, A.J.; Dahmus, J.; Stern, B.; Soriano, C.; Rivas, G.; Hummer, B.; Kimball, S.R.; Geyer, N.R.; et al. NASHFit: A randomized controlled trial of an exercise training program to reduce clotting risk in patients with NASH. Hepatology 2022, 76, 172–185. [Google Scholar] [CrossRef]
- Tezze, C.; Romanello, V.; Sandri, M. FGF21 as Modulator of Metabolism in Health and Disease. Front. Physiol. 2019, 10. eCollection 2019. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xu, Y.; Hu, Y.; Wang, G. The role of fibroblast growth factor 21 in the pathogenesis of non-alcoholic fatty liver disease and implications for therapy. Metabolism 2015, 64, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Falamarzi, K.; Malekpour, M.; Tafti, M.F.; Azarpira, N.; Behboodi, M.; Zarei, M. The role of FGF21 and its analogs on liver associated diseases. Front. Med. 2022, 9, 967375. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.; Charles, E.D.; Neuschwander-Tetri, B.A.; Loomba, R.; Harrison, S.A.; Abdelmalek, M.F.; Lawitz, E.J.; Halegoua-DeMarzio, D.; Kundu, S.; Noviello, S.; et al. Pegbelfermin (BMS-986036), a PEGylated fibroblast growth factor 21 analogue, in patients with non-alcoholic steatohepatitis: A randomised, double-blind, placebo-controlled, phase 2a trial. Lancet 2019, 392, 2705–2717. [Google Scholar] [CrossRef] [PubMed]
- Abdelmalek, M.F.; Charles, E.D.; Sanyal, A.J.; Harrison, S.A.; Neuschwander-Tetri, B.A.; Goodman, Z.; Ehman, R.A.; Karsdal, M.; Nakajima, A.; Du, S.; et al. The FALCON program: Two phase 2b randomized, double-blind, placebo-controlled studies to assess the efficacy and safety of pegbelfermin in the treatment of patients with nonalcoholic steatohepatitis and bridging fibrosis or compensated cirrhosis. Contemp. Clin. Trials 2021, 104, 106335. [Google Scholar] [CrossRef]
- Harrison, S.A.; Ruane, P.J.; Freilich, B.L.; Neff, G.; Patil, R.; Behling, C.A.; Hu, C.; Fong, E.; de Temple, B.; Tillman, E.J.; et al. Efruxifermin in non-alcoholic steatohepatitis: A randomized, double-blind, placebo-controlled, phase 2a trial. Nat. Med. 2021, 27, 1262–1271. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, S.H.; Min, Y.K.; Yang, H.M.; Lee, J.B.; Lee, M.S. Acute exercise induces FGF21 expression in mice and in healthy humans. PloS ONE 2013, 8, e63517. [Google Scholar] [CrossRef]
- Gao, Y.; Zhang, W.; Zeng, L.-Q.; Bai, H.; Li, J.; Zhou, J.; Zhou, G.-Y.; Fang, C.-W.; Wang, F.; Qin, X.-J. Exercise and dietary intervention ameliorate high-fat diet-induced NAFLD and liver aging by inducing lipophagy. Redox Biol. 2020, 36, 101635. [Google Scholar] [CrossRef]
- Taniguchi, H.; Tanisawa, K.; Sun, X.; Kubo, T.; Higuchi, M. Endurance Exercise Reduces Hepatic Fat Content and Serum Fibroblast Growth Factor 21 Levels in Elderly Men. J. Clin. Endocrinol. Metab. 2016, 101, 191–198. [Google Scholar] [CrossRef]
- Takahashi, A.; Abe, K.; Fujita, M.; Hayashi, M.; Okai, K.; Ohira, H. Simple resistance exercise decreases cytokeratin 18 and fibroblast growth factor 21 levels in patients with nonalcoholic fatty liver disease: A retrospective clinical study. Medicine 2020, 99, e20399. [Google Scholar] [CrossRef] [PubMed]
- Tas, E.; Bai, S.; Ou, X.; Mercer, K.; Lin, H.; Mansfield, K.; Buchmann, R.; Diaz, E.C.; Oden, J.; Børsheim, E.; et al. Fibroblast. Growth Factor-21 to Adiponectin Ratio: A Potential Biomarker to Monitor Liver Fat in Children with Obesity. Front. Endocrinol. 2020, 11, 654. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Liu, L.; Wei, Y.; Fang, C.; Zhou, F.; Chen, J.; Han, Q.; Huang, M.; Tan, X.; Liu, Q.; et al. Exercise ameliorates the FGF21-adiponectin axis impairment in diet-induced obese mice. Endocr. Connect. 2019, 8, 596–604. [Google Scholar] [CrossRef] [PubMed]
- Stine, J.G.; Schreibman, I.; Navabi, S.; Kang, M.; Dahmus, J.; Soriano, C.; Rivas, G.; Hummer, B.; Beyer, M.; Tressler, H.; et al. Nonalcoholic steatohepatitis Fitness Intervention in Thrombosis (NASHFit): Study protocol for a randomized controlled trial of a supervised aerobic exercise program to reduce elevated clotting risk in patients with NASH. Contemp. Clin. Trials Commun. 2020, 18, 100560. [Google Scholar] [CrossRef] [PubMed]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Stine, J.G.; Munaganuru, N.; Barnard, A.; Wang, J.L.; Kaulback, K.; Argo, C.K.; Singh, S.; Fowler, K.J.; Sirlin, C.B.; Loomba, R. Change in MRI-PDFF and Histologic Response in Patients with Nonalcoholic Steatohepatitis: A Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2021, 19, 2274–2283.e2275. [Google Scholar] [CrossRef]
- Tamaki, N.; Munaganuru, N.; Jung, J.; Yonan, A.Q.; Loomba, R.R.; Bettencourt, R.; Ajmera, V.; Valasek, M.A.; Behling, C.; Sirlin, C.B.; et al. Clinical utility of 30% relative decline in MRI-PDFF in predicting fibrosis regression in non-alcoholic fatty liver disease. Gut 2022, 71, 983–990. [Google Scholar] [CrossRef]
- Loomba, R.; Sanyal, A.J.; Kowdley, K.V.; Terrault, N.; Chalasani, N.P.; Abdelmalek, M.F.; McCullough, A.J.; Shringarpure, R.; Ferguson, B.; Lee, L.; et al. Factors Associated with Histologic Response in Adult Patients with Nonalcoholic Steatohepatitis. Gastroenterology 2019, 156, 88–95.e85. [Google Scholar] [CrossRef]
- Fon Tacer, K.; Bookout, A.L.; Ding, X.; Kurosu, H.; John, G.B.; Wang, L.; Goetz, R.; Mohammadi, M.; Kuroso, M.; Mangelsdorf, D.J.; et al. Research resource: Comprehensive expression atlas of the fibroblast growth factor system in adult mouse. Mol. Endocrinol. 2010, 24, 2050–2064. [Google Scholar] [CrossRef] [PubMed]
- Badman, M.K.; Pissios, P.; Kennedy, A.R.; Koukos, G.; Flier, J.S.; Maratos-Flier, E. Hepatic fibroblast growth factor 21 is regulated by PPARalpha and is a key mediator of hepatic lipid metabolism in ketotic states. Cell Metab. 2007, 5, 426–437. [Google Scholar] [CrossRef]
- Samson, S.L.; Sathyanarayana, P.; Jogi, M.; Gonzalez, E.V.; Gutierrez, A.; Krishnamurthy, R.; Muthupillai, R.; Chan, L.; Bajaj, M. Exenatide decreases hepatic fibroblast growth factor 21 resistance in non-alcoholic fatty liver disease in a mouse model of obesity and in a randomised controlled trial. Diabetologia 2011, 54, 3093–3100. [Google Scholar] [CrossRef]
- Cho, J.; Lee, I.; Kim, D.; Koh, Y.; Kong, J.; Lee, S.; Kang, H. Effect of aerobic exercise training on non-alcoholic fatty liver disease induced by a high fat diet in C57BL/6 mice. J. Exerc. Nutr. Biochem. 2014, 18, 339–346. [Google Scholar] [CrossRef]
- Dahmus, J.; Hummer, B.; Rivas, G.; Schmitz, K.; Caldwell, S.H.; Argo, C.K.; Schreibman, I.; Stine, J.G. Patients with Nonalcoholic Steatohepatitis and Advanced Liver Disease Have the Lowest Cardiorespiratory Fitness. Dig. Dis. Sci. 2023. Epub Jan 2024. [Google Scholar] [CrossRef]
- Krasnoff, J.B.; Painter, P.L.; Wallace, J.P.; Bass, N.M.; Merriman, R.B. Health-related fitness and physical activity in patients with nonalcoholic fatty liver disease. Hepatology 2008, 47, 1158–1166. [Google Scholar] [CrossRef]
- Williams, P.T. Physical fitness and activity as separate heart disease risk factors: A meta-analysis. Med. Sci. Sport. Exerc. 2001, 33, 754–761. [Google Scholar] [CrossRef]
- Croci, I.; Coombes, J.S.; Bucher Sandbakk, S.; Keating, S.E.; Nauman, J.; Macdonald, G.A.; Wisloff, U. Non-alcoholic fatty liver disease: Prevalence and all-cause mortality according to sedentary behaviour and cardiorespiratory fitness. The HUNT Study. Prog. Cardiovasc. Dis. 2019, 62, 127–134. [Google Scholar] [CrossRef]
- Taniguchi, H.; Tanisawa, K.; Sun, X.; Cao, Z.B.; Oshima, S.; Ise, R.; Sakamoto, S.; Higuchi, M. Cardiorespiratory fitness and visceral fat are key determinants of serum fibroblast growth factor 21 concentration in Japanese men. J. Clin. Endocrinol. Metab. 2014, 99, E1877–E1884. [Google Scholar] [CrossRef] [PubMed]
- Lakhani, I.; Gong, M.; Wong, W.T.; Bazoukis, G.; Lampropoulos, K.; Wong, S.H.; Wu, W.K.K.; Wong, M.C.S.; Ong, K.L.; Liu, T.; et al. Fibroblast growth factor 21 in cardio-metabolic disorders: A systematic review and meta-analysis. Metabolism 2018, 83, 11–17. [Google Scholar] [CrossRef]
- Baker, C.J.; Martinez-Huenchullan, S.F.; D’Souza, M.; Xu, Y.; Li, M.; Bi, Y.; Johnson, N.A.; Twigg, S.M. Effect of exercise on hepatic steatosis: Are benefits seen without dietary intervention? A systematic review and meta-analysis. J. Diabetes 2021, 13, 63–77. [Google Scholar] [CrossRef]
- Lu, W.; Li, X.; Luo, Y. FGF21 in obesity and cancer: New insights. Cancer Lett. 2021, 499, 5–13. [Google Scholar] [CrossRef] [PubMed]
- DiJoseph, K.; Thorp, A.; Harrington, A.; Schmitz, K.H.; Chinchilli, V.M.; Stine, J.G. Physical Activity and Risk of Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Dig. Dis. Sci. 2023, 68, 1051–1059. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.C.; Lee, I.M.; Weiderpass, E.; Campbell, P.T.; Sampson, J.N.; Kitahara, C.M.; Keadle, S.K.; Arem, H.; Berrington de Gonzalez, A.; Hartge, P.; et al. Association of Leisure-Time Physical Activity with Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern. Med. 2016, 176, 816–825. [Google Scholar] [CrossRef] [PubMed]

| KERRYPNX | Standard Clinical Care (n = 8) | Exercise (n = 12) |
|---|---|---|
| Demographics | ||
| Age, yrs | 44.9 (36.8, 55.0) | 53.9 (45.7, 63.6) |
| Female sex, n (%) | 3 (38) | 8 (67) |
| BMI, kg/m2 | 34.2 (29.9, 39.1) | 32.8 (29.7, 36.2) |
| Body weight, kg | 106.4 (89.1, 127.2) | 95.5 (87.4, 104.3) |
| Metabolic risk | ||
| Comorbidities, n (%) | ||
| Diabetes | 3 (38) | 5 (42) |
| Hyperlipidemia | 5 (63) | 7 (58) |
| Hypertension | 5 (63) | 12 (100) |
| Hemoglobin A1c, % | 6.1 (5.3, 7.0) | 6.4 (5.6, 7.4) |
| Glucose (fasting), mg/dL | 128.4 (97.1, 169.7) | 136.3 (115.2, 161.3) |
| HOMA-IR | 7.7 (4.0, 15.0) | 13.3 (9.2, 19.2) |
| VO2peak, mL/kg/min | 24.0 (19.8, 29.1) | 19.3 (15.8, 23.6) |
| Body fat, % | 39.1 (30.8, 49.7) | 42.3 (37.7, 47.5) |
| NASH phenotyping | ||
| Medications, n (%) | ||
| Vitamin E | 2 (25) | 3 (25) |
| GLP-1 agonist | 0 (0) | 1 (8) |
| Non-invasive tests | ||
| FIB-4 | 1.07 (0.47, 2.40) | 1.15 (0.85, 1.57) |
| NFS, Median (IQR) | −1.75 (2.74) | −1.51 (1.25) |
| Serum biomarkers | ||
| Adiponectin, ng/mL | 3272 (2211, 4843) | 3449 (2947, 4036) |
| CK-18, IU/L | 85.7 (31.1, 236.4) | 231.5 (76.3, 702.1) |
| FGF-21, ng/dL | 372.4 (246.8, 561.8) | 520.7 (346.1, 783.3) |
| PAI-1, ng/mL | 206.0 (120.1, 353.5) | 165.8 (124.0, 221.7) |
| Imaging biomarkers | ||
| Liver fat (MRI-PDFF), % | 19.0 (11.8, 30.6) | 20.5 (17.4, 24.2) |
| NAS | 5.0 (4.5, 5.4) | 5.1 (4.5, 5.7) |
| Steatosis | 2.3 (2.0, 2.7) | 2.5 (2.0, 3.0) |
| Lobular inflammation, Median (IQR) | 1.0 (1.0) | 1.3 (0.7) |
| Hepatocyte ballooning | 1.2 (0.9, 1.5) | 1.2 (1.0, 1.5) |
| Fibrosis stage, n (%) | ||
| 0/1 | 4 (50) | 7 (58) |
| 2 | 3 (38) | 2 (17) |
| 3 | 0 (0) | 3 (25) |
| 4 | 1 (12) | 0 (0) |
| Standard Clinical Care (n = 8) | Exercise (n = 12) | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Post | Within Group p-Value | Baseline | Post | Within Group p-Value | Between Group p-Value | |
| Clinical Decision Aids | |||||||
| NFS, Median (IQR) | −1.75 (2.74) | −1.42 (2.60) | 0.653 | −1.51 (1.25) | −1.69 (1.30) | 0.679 | 0.431 |
| FIB-4 | 1.07 (0.48, 2.40) | 1.02 (0.47, 2.20) | 0.671 | 1.15 (0.85, 1.57) | 1.03 (0.76, 1.40) | 0.077 | 0.777 |
| Serum Biomarkers | |||||||
| Adiponectin, ng/mL | 3271 (2210, 4843) | 3141 (2101, 4698) | 0.468 | 3448 (2947, 4035) | 3530 (3060, 4071) | 0.652 | 0.440 |
| CK18, IU/L | 85.7 (31.1, 236.4) | 85.8 (16.1, 458.1) | 0.998 | 231.5 (76.3, 702.1) | 177.0 (56.7, 552.6) | 0.034 | 0.062 |
| FGF21, ng/mL | 372 (247, 562) | 390 (190, 802) | 0.670 | 521 (346, 783) | 277 (153, 501) | 0.044 | 0.037 |
| FGF21/Adiponectin | 0.11 (0.06, 0.19) | 0.13 (0.07, 0.27) | 0.602 | 0.15 (0.09, 0.24) | 0.07 (0.04, 0.15) | 0.049 | 0.099 |
| PAI-1, ng/mL | 206 (120, 353) | 279 (187, 415) | 0.061 | 166 (124, 221) | 130 (101, 168) | 0.160 | 0.020 |
| ≥17 IU/L reduction in ALT, n (%) | 1 (13) | 7 (58) | <0.001 | ||||
| Imaging biomarkers | |||||||
| MRI-PDFF liver fat, % | 19.0 (11.8, 30.6) | 18.8 (10.2, 34.7) | 0.934 | 19.0 (11.8, 30.6) | 18.8 (10.2, 34.7) | 0.018 | 0.011 |
| ≥30% relative reduction in MRI-PDFF, n (%) | 1 (13) | 4 (33) | 0.008 | ||||
| Standard Clinical Care (n = 8) | Exercise (n = 12) | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Post | Within Group p-Value | Baseline | Post | Within Group p-Value | Between Group p-Value | |
| Anthropometry and Body composition | |||||||
| BMI, kg/m2 | 34.2 (29.9, 39.1) | 34.6 (30.3, 39.5) | 0.173 | 32.8 (29.7, 36.2) | 32.2 (29.2, 35.4) | 0.267 | 0.155 |
| Body weight, kg | 106.6 (89.1, 127.2) | 107.9 (90.1, 129.3) | 0.069 | 95.5 (87.4, 104.3) | 93.4 (85.8, 101.8) | 0.099 | 0.030 |
| Waist circumference, in | 45.5 (41.6, 49.9) | 46.1 (42.3, 49.9) | 0.385 | 43.8 (41.6, 46.1) | 43.1 (40.9, 45.4) | 0.230 | 0.135 |
| Hip circumference, in | 45.3 (40.7, 50.5) | 46.3 (41.6, 51.6) | 0.001 | 44.9 (42.4, 47.5) | 43.6 (40.5, 47.5) | 0.243 | 0.026 |
| VAT, lbs. | 6.5 (4.7, 8.9) | 6.8 (4.7, 9.7) | 0.795 | 5.5 (4.7, 6.4) | 5.1 (4.3, 5.9) | 0.016 | 0.122 |
| Fat free (muscle) mass, lbs. | 117.2 (88.8, 154.7) | 122.1 (88.7, 154.7) | 0.294 | 106.6 (87.1, 130.4) | 106.5 (87.1, 130.3) | 0.913 | 0.611 |
| Body fat, % | 39.1 (30.8, 49.7) | 37.1 (28.7, 48.1) | 0.259 | 42.3 (37.7, 47.5) | 41.4 (36.5, 46.8) | 0.040 | 0.254 |
| Liver volume, cc | 2480 (2028, 3031) | 2543 (2116, 3055) | 0.289 | 2305 (2022, 2627) | 2118 (1861, 2410) | 0.020 | 0.024 |
| Cardiorespiratory fitness | |||||||
| Resting VO2, L/min | 3.4 (2.7, 4.2) | 3.5 (3.0, 4.0) | 0.432 | 3.5 (2.7, 4.5) | 4.0 (3.3, 4.8) | 0.378 | 0.573 |
| VO2peak, mL/kg/min | 24.0 (19.8, 29.1) | 22.5 (20.0, 25.4) | 0.381 | 19.3 (15.8, 23.6) | 22.6 (20.0, 25.5) | 0.076 | 0.057 |
| Biochemistry | |||||||
| ALT, IU/L | 51.6 (40.0, 66.6) | 50.7 (20.0, 25.4) | 0.318 | 56.8 (46.8, 68.9) | 43.8 (35.7, 53.7) | 0.009 | 0.259 |
| AST, IU/L | 39.4 (27.2, 57.1) | 33.4 (25.0, 44.7) | 0.388 | 38.9 (32.1, 47.1) | 30.6 (25.4, 36.8) | 0.004 | 0.859 |
| Glucose (fasting), mg/dL | 128.3 (97.1, 169.7) | 139.1 (93.0, 207.9) | 0.386 | 136.3 (115.2, 161.3) | 117.4 (100.2, 137.7) | 0.074 | 0.030 |
| Hemoglobin A1c, % | 6.1 (5.3, 7.7) | 6.4 (5.4, 7.7) | 0.056 | 6.4 (5.6, 7.4) | 6.1 (5.5,6.6) | 0.028 | 0.006 |
| HOMA-IR | 7.7 (4.0, 15.0) | 7.7 (3.2, 18.7) | 0.880 | 13.3 (9.2, 19.2) | 7.9 (4.8, 13.2) | 0.080 | 0.168 |
| Insulin, IU/mL | 24.4 (15.4, 38.8) | 22.5 (10.9, 46.2) | 0.447 | 39.5 (28.0, 55.7) | 27.4 (15.9, 47.0) | 0.152 | 0.351 |
| Lipids | |||||||
| Total cholesterol, mg/dL | 199.5 (169.5, 234.7) | 182.5 (160.7, 207.3) | 0.358 | 183.1 (157.8, 212.4) | 183.4 (160.2, 210.0) | 0.969 | 0.410 |
| LDL, mg/dL | 114.9 (82.2, 160.5) | 104.3 (72.9, 149.4) | 0.510 | 102.8 (82.4, 128.4) | 101.9 (83.0, 125.0) | 0.906 | 0.583 |
| HDL, mg/dL | 41.5 (32.3, 53.4) | 37.9 (28.0, 51.4) | 0.352 | 41.7 (36.1, 48.1) | 43.7 (39.2, 48.6) | 0.221 | 0.152 |
| Triglyceride, mg/dL | 207.5 (144.1, 298.7) | 210.2 (134.1, 329.5) | 0.974 | 172.3 (137.3, 216.4) | 168.8 (130.4, 218.5) | 0.781 | 0.309 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stine, J.G.; Welles, J.E.; Keating, S.; Hussaini, Z.; Soriano, C.; Heinle, J.W.; Geyer, N.; Chinchilli, V.M.; Loomba, R.; Kimball, S.R. Serum Fibroblast Growth Factor 21 Is Markedly Decreased following Exercise Training in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis. Nutrients 2023, 15, 1481. https://doi.org/10.3390/nu15061481
Stine JG, Welles JE, Keating S, Hussaini Z, Soriano C, Heinle JW, Geyer N, Chinchilli VM, Loomba R, Kimball SR. Serum Fibroblast Growth Factor 21 Is Markedly Decreased following Exercise Training in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis. Nutrients. 2023; 15(6):1481. https://doi.org/10.3390/nu15061481
Chicago/Turabian StyleStine, Jonathan G., Jaclyn E. Welles, Shelley Keating, Zeba Hussaini, Christopher Soriano, J. Wes Heinle, Nathaniel Geyer, Vernon M. Chinchilli, Rohit Loomba, and Scot R. Kimball. 2023. "Serum Fibroblast Growth Factor 21 Is Markedly Decreased following Exercise Training in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis" Nutrients 15, no. 6: 1481. https://doi.org/10.3390/nu15061481
APA StyleStine, J. G., Welles, J. E., Keating, S., Hussaini, Z., Soriano, C., Heinle, J. W., Geyer, N., Chinchilli, V. M., Loomba, R., & Kimball, S. R. (2023). Serum Fibroblast Growth Factor 21 Is Markedly Decreased following Exercise Training in Patients with Biopsy-Proven Nonalcoholic Steatohepatitis. Nutrients, 15(6), 1481. https://doi.org/10.3390/nu15061481







