Influence of the Results of Control of Intakes, Proteins and Anthropometry Nutritional Screening, Sarcopenia and Body Composition on the Clinical Evolution of Hospitalized Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Type of Study and Ethical Aspects
2.2. Inclusion and Exclusion Criteria
2.3. Collected and Analyzed Data
2.4. Statistical Analysis
3. Results
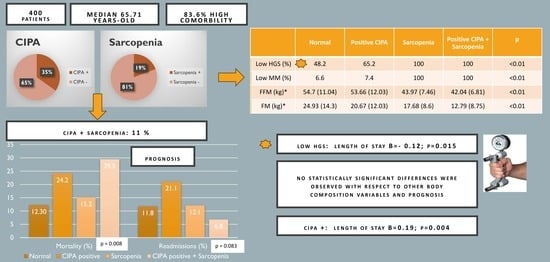
3.1. Characteristics of the Sample
3.2. Malnutrition and Sarcopenia Screening and Diagnosis
3.3. Association between Prognostic Clinical Outcomes and CIPA Results, Sarcopenia and Body Composition
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gomes, F.; Baumgartner, A.; Bounoure, L.; Bally, M.; Deutz, N.E.; Greenwald, J.L.; Stanga, Z.; Mueller, B.; Schuetz, P. Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: An Updated Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1915138. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Hernández, J.; Planas Vila, M.; León-Sanz, M.; García de Lorenzo, A.; Celaya-Pérez, S.; García-Lorda, P.; Araujo, K.; Sarto Guerri, B. Prevalence and costs of malnutrition in hospitalized patients; the PREDyCES Study. Nutr. Hosp. 2012, 27, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Zugasti-Murillo, A.; Petrina-Jáuregui, M.E.; Ripa-Ciáurriz, C.; Sánchez-Sánchez, R.; Villazón-González, F.; Faes, Á.G.D.; Fernández-López, C.; Calles-Romero, L.; Martín-Palmero, M.Á.; Riestra-Fernández, M.; et al. SeDREno study—Prevalence of hospital malnutrition according to GLIM criteria, ten years after the PREDyCES study. Nutr. Hosp. 2021, 38, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Mora Mendoza, A.; Suárez Llanos, J.P.; Sánchez Morales, A.; Lorenzo González, C.; Zambrano Huerta, Y.; Llorente Gómez de Segura, I. Validation of CIPA nutritional screening through prognostic clinical variables in hospitalized surgical patients. Endocrinol. Diabetes Nutr. 2020, 67, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Llanos, J.P.; Rosat-Rodrigo, A.; García-Niebla, J.; Vallejo-Torres, L.; Delgado-Brito, I.; García-Bello, M.A.; Pereyra-García-Castro, F.; Barrera-Gómez, M.A. Comparison of Clinical Outcomes in Surgical Patients Subjected to CIPA Nutrition Screening and Treatment versus Standard Care. Nutrients 2019, 11, 889. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Marra, M.; Sammarco, R.; De Lorenzo, A.; Iellamo, F.; Siervo, M.; Pietrobelli, A.; Donini, L.M.; Santarpia, L.; Cataldi, M.; Pasanisi, F.; et al. Assessment of Body Composition in Health and Disease Using Bioelectrical Impedance Analysis (BIA) and Dual Energy X-Ray Absorptiometry (DXA): A Critical Overview. Contrast Media Mol. Imaging 2019, 2019, 3548284. [Google Scholar] [CrossRef]
- Patil, B.R.; Patkar, D.P.; Mandlik, S.A.; Kuswarkar, M.M.; Jindal, G.D. Single prediction equation for bioelectrical impedance analysis in adults aged 22–59 years. J. Med. Eng. Technol. 2011, 35, 109–114. [Google Scholar] [CrossRef]
- Cereda, E.; Pedrazzoli, P.; Lobascio, F.; Masi, S.; Crotti, S.; Klersy, C.; Turri, A.; Stobäus, N.; Tank, M.; Franz, K.; et al. The prognostic impact of BIA-derived fat-free mass index in patients with cancer. Clin. Nutr. 2021, 40, 3901–3907. [Google Scholar] [CrossRef]
- Ji, W.; Liu, X.L.; Liu, P.; He, Y.W.; Zhao, Y.X.; Zheng, K.; Cui, J.; Li, W. The efficacy of fat-free mass index and appendicular skeletal muscle mass index in cancer malnutrition: A propensity score match analysis. Front. Nutr. 2023, 10, 1172610. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Muscle strength: Clinical and prognostic value of hand-grip dynamometry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Torralvo, F.J.; Porras, N.; Abuín Fernández, J.; García Torres, F.; Tapia, M.J.; Lima, F.; Soriguer, F.; Gonzalo, M.; Martínez, G.R.; Olveira, G.; et al. Normative reference values for hand grip dynamometry in Spain. Association with lean mass. Nutr. Hosp. 2018, 35, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Jochem, C.; Leitzmann, M.; Volaklis, K.; Aune, D.; Strasser, B. Association Between Muscular Strength and Mortality in Clinical Populations: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2019, 20, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Lee, D.H.; Min, J.; Jeon, J.Y. Handgrip Strength as a Predictor of All-Cause Mortality in Patients With Chronic Kidney Disease Undergoing Dialysis: A Meta-Analysis of Prospective Cohort Studies. J. Ren. Nutr. 2019, 29, 471–479. [Google Scholar] [CrossRef]
- Mauricio, S.F.; Ribeiro, H.S.; Correia, M.I.T.D. Nutritional Status Parameters as Risk Factors for Mortality in Cancer Patients. Nutr. Cancer 2016, 68, 949–957. [Google Scholar] [CrossRef]
- Rossi, A.P.; Fantin, F.; Abete, P.; Bellelli, G.; Bo, M.; Cherubini, A.; Corica, F.; Di Bari, M.; Maggio, M.; Manca, G.M.; et al. Association between hospitalization-related outcomes, dynapenia and body mass index: The Glisten Study. Eur. J. Clin. Nutr. 2019, 73, 743–750. [Google Scholar] [CrossRef]
- Ballesteros-Pomar, M.D.; Gajete-Martín, L.M.; Pintor-De-la-maza, B.; González-Arnáiz, E.; González-Roza, L.; García-Pérez, M.P.; González-Alonso, V.; García-González, M.A.; de Prado-Espinosa, R.; Cuevas, M.J.; et al. Disease-Related Malnutrition and Sarcopenia Predict Worse Outcome in Medical Inpatients: A Cohort Study. Nutrients 2021, 13, 2937. [Google Scholar] [CrossRef]
- Cerri, A.P.; Bellelli, G.; Mazzone, A.; Pittella, F.; Landi, F.; Zambon, A.; Annoni, G. Sarcopenia and malnutrition in acutely ill hospitalized elderly: Prevalence and outcomes. Clin. Nutr. 2015, 34, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Llanos, J.P.; Benítez-Brito, N.; Vallejo-Torres, L.; Delgado-Brito, I.; Rosat-Rodrigo, A.; Hernández-Carballo, C.; Ramallo-Fariña, Y.; Pereyra-García-Castro, F.; Carlos-Romero, J.; Felipe-Pérez, N.; et al. Clinical and cost-effectiveness analysis of early detection of patients at nutrition risk during their hospital stay through the new screening method CIPA: A study protocol. BMC Health Serv. Res. 2017, 17, 292. [Google Scholar] [CrossRef]
- Sergi, G.; De Rui, M.; Veronese, N.; Bolzetta, F.; Berton, L.; Carraro, S.; Bano, G.; Coin, A.; Manzato, E.; Perissinotto, E. Assessing appendicular skeletal muscle mass with bioelectrical impedance analysis in free-living Caucasian older adults. Clin. Nutr. 2015, 34, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Genton, L.; Hans, D.; Pichard, C. Validation of a bioelectrical impedance analysis equation to predict appendicular skeletal muscle mass (ASMM). Clin. Nutr. 2003, 22, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Llanos, J.P.; Mora-Mendoza, A.; Benítez-Brito, N.; Pérez-Méndez, L.; Pereyra-García-Castro, F.; Oliva-García, J.G.; Palacio-Abizanda, J.E. Validity of the new nutrition screening tool Control of Food Intake, Protein, and Anthropometry (CIPA) in non-surgical inpatients. Arch. Med. Sci. 2018, 14, 1020–1024. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, P.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Tribolet, P.; Bregenzer, T.; Braun, N.; et al. Individualised nutritional support in medical inpatients at nutritional risk: A randomised clinical trial. Lancet 2019, 393, 2312–2321. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.; Schuetz, P.; Bounoure, L.; Austin, P.; Ballesteros-Pomar, M.; Cederholm, T.; Fletcher, J.; Laviano, A.; Norman, K.; Poulia, K.-A.; et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin. Nutr. 2018, 37, 336–353. [Google Scholar] [CrossRef] [PubMed]
- Perkisas, S.; Bastijns, S.; Baudry, S.; Bauer, J.; Beaudart, C.; Beckwée, D.; Cruz-Jentoft, A.; Gasowski, J.; Hobbelen, H.; Jager-Wittenaar, H.; et al. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur. Geriatr. Med. 2021, 12, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Kaegi-Braun, N.; Tribolet, P.; Baumgartner, A.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Hoess, C.; et al. Value of handgrip strength to predict clinical outcomes and therapeutic response in malnourished medical inpatients: Secondary analysis of a randomized controlled trial. Am. J. Clin. Nutr. 2021, 114, 731–740. [Google Scholar] [CrossRef] [PubMed]
- García-Almeida, J.M.; García-García, C.; Ballesteros-Pomar, M.D.; Olveira, G.; Lopez-Gomez, J.J.; Bellido, V.; Lesmes, I.B.; Burgos, R.; Sanz-Paris, A.; Matia-Martin, P.; et al. Expert Consensus on Morphofunctional Assessment in Disease-Related Malnutrition. Grade Review and Delphi Study. Nutrients 2023, 15, 612. [Google Scholar] [CrossRef]
- Westbury, L.D.; Beaudart, C.; Bruyère, O.; Cauley, J.A.; Cawthon, P.; Cruz-Jentoft, A.J.; Curtis, E.M.; Ensrud, K.; Fielding, R.A.; Johansson, H.; et al. Recent sarcopenia definitions-prevalence, agreement and mortality associations among men: Findings from population-based cohorts. J. Cachexia Sarcopenia Muscle 2023, 14, 565–575. [Google Scholar] [CrossRef]
- Roberti, E.; Merlano, M.; Ravanelli, M.; Alberti, A.; Esposito, A.; Gili, R.; Spinazzé, S.; Baré, C.; Jocollé, G.; Benasso, M.; et al. Muscle quality and not quantity as a predictor of survival in head and neck squamous cell carcinoma. Oral. Oncol. 2023, 145, 106540. [Google Scholar] [CrossRef]
- Aleixo, G.F.P.; Valente, S.A.; Wei, W.; Moore, H.C.F. Association of body composition and surgical outcomes in patients with early-stage breast cancer. Breast Cancer Res. Treat. 2023, 202, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Sheean, P.; Gonzalez, M.C.; Prado, C.M.; McKeever, L.; Hall, A.M.; Braunschweig, C.A. American Society for Parenteral and Enteral Nutrition Clinical Guidelines: The Validity of Body Composition Assessment in Clinical Populations. JPEN J. Parenter. Enteral Nutr. 2020, 44, 12–43. [Google Scholar] [CrossRef] [PubMed]

| n = 400 Mean (SD) | |
|---|---|
| Age (years) | 65.71 (27.23) |
| Sex (% men) | 51.5 |
| CCI | 7.63 (5.33) |
| BMI (kg/m2) | 27.23 (6.39) |
| HGS (kg) | 19.17 (10.64) |
| ASMI (kg/m2) | 7.36 (1.68) |
| FFM (kg) | 52.22 (11.58) |
| FM (kg) | 21.98 (13.45) |
| Albumin (g/dL) | 3.54 (0.62) |
| Normal | Positive CIPA | Sarcopenia | Positive CIPA + Sarcopenia | p | |
|---|---|---|---|---|---|
| n (%) | 228 (57) | 139 (34.8) | 77 (19.3) | 44 (11) | - |
| Age (years) * | 63.45 (14.51) | 65.77 (15.51) | 74.3 (10.85) | 70.84 (12.89) | <0.01 |
| Sex (% men) | 50.99 | 45.3 | 57.9 | 63.6 | 0.204 |
| BMI (kg/m2) * | 29.12 (6.03) | 27.41 (6.06) | 23.06 (3.03) | 20.12 (4.09) | <0.01 |
| Admission service (% surgical) | 29.4 | 27.4 | 27.3 | 18.2 | 0.508 |
| CCI * | 6.93 (5.07) | 8.42 (5.66) | 8.28 (5.04) | 9.02 (5.68) | 0.023 |
| Albumin < 3 g/dL (%) | 3.81 (0.45) | 3.03 (0.63) | 3.57 (0.44) | 3.19 (0.58) | <0.01 |
| Low HGS (%) | 48.2 | 65.2 | 100 | 100 | <0.01 |
| Low muscle mass (%) | 6.6 | 7.4 | 100 | 100 | <0.01 |
| FFM (kg) * | 54.7 (11.04) | 53.66 (12.03) | 43.97 (7.46) | 42.04 (6.81) | <0.01 |
| FM (kg) * | 24.93 (14.3) | 20.67 (12.03) | 17.68 (8.6) | 12.79 (8.75) | <0.01 |
| No Readmissions | Readmissions | p | No Mortality | Mortality | p | |
|---|---|---|---|---|---|---|
| BMI (kg/m2) | 27.27 (6.58) | 26.98 (5.03) | 0.755 | 27.2 (6.43) | 26.33 (6.18) | 0.202 |
| HGS (kg) | 19.23 (10.94) | 18.74 (8.47) | 0.757 | 19.54 (10.71) | 17.37 (10.19) | 0.132 |
| ASMI (kg/m2) | 7.32 (1.7) | 7.67 (1.5) | 0.150 | 7.38 (1.69) | 7.28 (1.63) | 0.654 |
| FFM (kg) | 51.97 (11.75) | 53.84 (10.47) | 0.270 | 52.34 (11.57) | 51.67 (11.75) | 0.663 |
| FM (kg) | 22.38 (13.76) | 19.49 (11.02) | 0.143 | 22.38 (13.77) | 20.09 (11.67) | 0.197 |
| Mortality (<6 Months) | Readmissions (<30 Days) | Length of Stay (Log-Transformed) | ||||
|---|---|---|---|---|---|---|
| ORa (IC 95%) | p | ORa (IC 95%) | p | Ba (IC 95%) | p | |
| Normal | Ref | Ref | Ref | |||
| Positive CIPA | 1.99 (1.02–3.91) | 0.043 | 1.86 (0.94–3.65) | 0.073 | 0.19 (0.01;0.38) | 0.040 |
| Sarcopenia | 1.01 (0.33–3.08) | 0.9 | 1.16 (0.35–3.79) | 0.805 | 0.21 (−0.08;0.49) | 0.159 |
| Positive CIPA + Sarcopenia | 2.10 (0.90–4.92) | 0.088 | 0.43 (0.12–1.58) | 0.205 | 0.19 (−0.05;0.45) | 0.126 |
| BMI | 0.98 (0.94–1.03) | 0.466 | 0.99 (0.95–1.04) | 0.901 | −0.01 (−0.02;0.003) | 0.130 |
| HGS | 0.97 (0.93–1.01) | 0.097 | 0.98 (0.94–1.02) | 0.372 | −0.012 (−0.02;−0.002) | 0.015 |
| ASMI | 0.94 (0.78–1.13) | 0.510 | 1.10 (0.92–1.31) | 0.295 | 0.009 (−0.04;−0.057) | 0.727 |
| FFM | 0.97 (0.95–1.01) | 0.115 | 1.00 (0.97–1.04) | 0.798 | −0.005 (−0.01;0.003) | 0.208 |
| FM | 0.99 (0.97–1.01) | 0.483 | 0.98 (0.96–1.01) | 0.141 | −0.004 (−0.01;0.01) | 0.126 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Márquez Mesa, E.; Suárez Llanos, J.P.; Afonso Martín, P.M.; Negrín, C.B.; García Ascanio, M.; González González, S.; Llorente Gómez de Segura, I. Influence of the Results of Control of Intakes, Proteins and Anthropometry Nutritional Screening, Sarcopenia and Body Composition on the Clinical Evolution of Hospitalized Patients. Nutrients 2024, 16, 14. https://doi.org/10.3390/nu16010014
Márquez Mesa E, Suárez Llanos JP, Afonso Martín PM, Negrín CB, García Ascanio M, González González S, Llorente Gómez de Segura I. Influence of the Results of Control of Intakes, Proteins and Anthropometry Nutritional Screening, Sarcopenia and Body Composition on the Clinical Evolution of Hospitalized Patients. Nutrients. 2024; 16(1):14. https://doi.org/10.3390/nu16010014
Chicago/Turabian StyleMárquez Mesa, Elena, José Pablo Suárez Llanos, Patricia Mercedes Afonso Martín, Carla Brito Negrín, María García Ascanio, Samuel González González, and Ignacio Llorente Gómez de Segura. 2024. "Influence of the Results of Control of Intakes, Proteins and Anthropometry Nutritional Screening, Sarcopenia and Body Composition on the Clinical Evolution of Hospitalized Patients" Nutrients 16, no. 1: 14. https://doi.org/10.3390/nu16010014
APA StyleMárquez Mesa, E., Suárez Llanos, J. P., Afonso Martín, P. M., Negrín, C. B., García Ascanio, M., González González, S., & Llorente Gómez de Segura, I. (2024). Influence of the Results of Control of Intakes, Proteins and Anthropometry Nutritional Screening, Sarcopenia and Body Composition on the Clinical Evolution of Hospitalized Patients. Nutrients, 16(1), 14. https://doi.org/10.3390/nu16010014