The Effects of Antioxidant Supplementation on the Pathologic Mechanisms of Metabolic Syndrome and Cardiovascular Disease Development
Abstract
:1. Introduction
2. Pathophysiological Mechanisms of Metabolic Syndrome
2.1. Obesity, Adipose Tissue Remodeling, and Dyslipidemia
2.2. Diabetes, Insulin Resistance, and Hyperglycemia
2.3. Hypertension
3. The Role of Metabolic Syndrome in the Development of CVDs
3.1. Obesity, Adipose Tissue Remodeling, and Dyslipidemia
3.2. Diabetes, Insulin Resistance, and Hyperglycemia
3.3. Hypertension
4. Oxidative Stress as a Strategic Mechanism Involved in the Pathophysiology of MetS
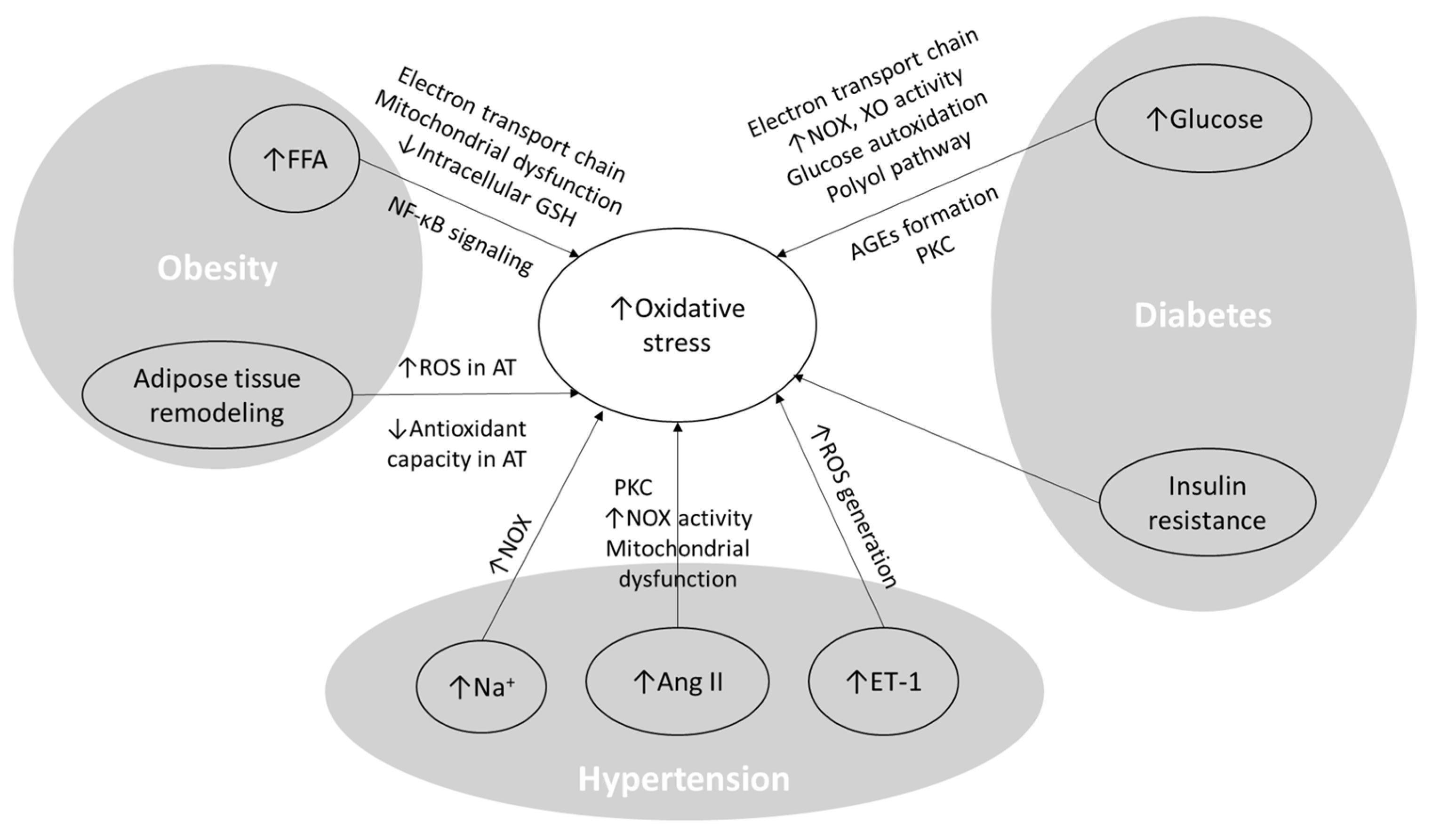
4.1. The Role of MetS Pathophysiological Components in Inducing Oxidative Stress
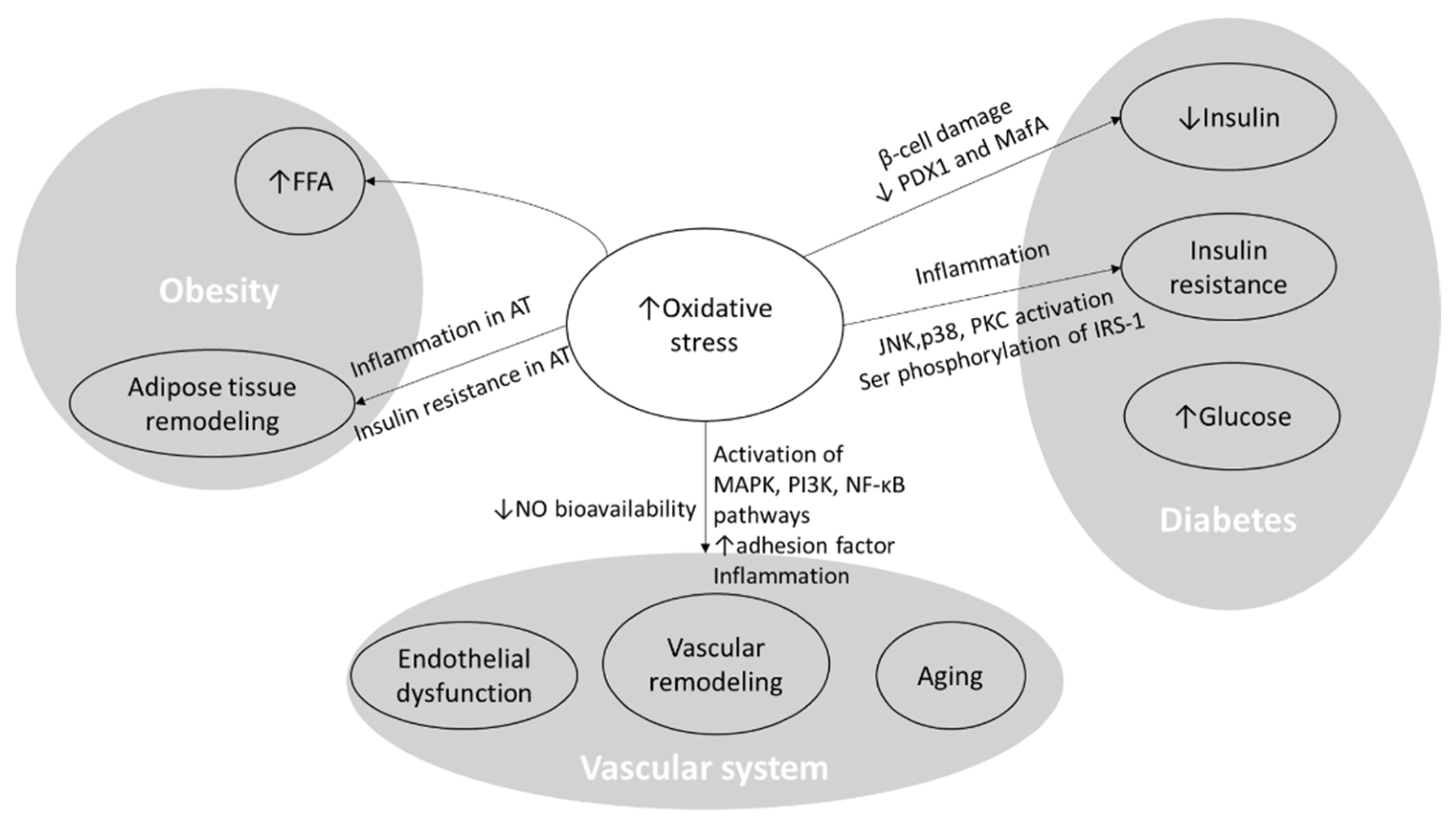
4.2. Effects of Oxidative Stress on the Pathophysiology of MetS and the Development of CVDs
5. Antioxidant Therapy for MetS Patients and Their Associated CVDs
5.1. Polyphenols
5.2. Flavonoids
5.3. Carotenoids
5.4. N-acetylcysteine
5.5. Melatonin
5.6. L-arginine
5.7. Vitamins C and E
5.8. Minerals
6. Epigenetic Role in MetS: A Bridge between Environment and MetS Pathophysiology
7. The Pathophysiological Network of Metabolic Syndrome and the Challenges in Its Management
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Dobrowolski, P.; Prejbisz, A.; Kurylowicz, A.; Baska, A.; Burchardt, P.; Chlebus, K.; Dzida, G.; Jankowski, P.; Jaroszewicz, J.; Jaworski, P.; et al. Metabolic syndrome a new definition and management guidelines. Arch. Med. Sci. 2022, 18, 1133–1156. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, S.M.; Shalaby, M.A.; El-shiekh, R.A.; El-banna, H.A.; Emam, S.R.; Bakr, A.F. Metabolic syndrome: Risk factors, diagnosis, pathogenesis, and management with natural approaches. Food Chem. Adv. 2023, 3, 100335. [Google Scholar] [CrossRef]
- Fahed, G.; Aoun, L.; Zerdan, M.B.; Allam, S.; Zerdan, M.B.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 38. [Google Scholar] [CrossRef]
- Regufe, V.M.G.; Pinto, C.M.C.B.; Perez, P.M.V.H.C. Metabolic syndrome in type 2 diabetic patients: A review of current evidence. Porto Biomed. J. 2020, 5, e101. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, K.A.; Luchian, I.; Goriuc, A.; Antoci, L.M.; Ciobanu, C.G.; Popescu, R.; Vlad, C.-E.; Blaj, M.; Foia, L.G. Mitochondrial Dysfunction, Oxidative Stress, and Therapeutic Strategies in Diabetes, Obesity, and Cardiovascular Disease. Antioxidants 2023, 12, 658. [Google Scholar] [CrossRef] [PubMed]
- Sharebiani, H.; Keramat, S.; Chavoshan, A.; Fazeli, B.; Stanek, A. The Influence of Antioxidants on Oxidative Stress-Induced Vascular Aging in Obesity. Antioxidants 2023, 12, 1295. [Google Scholar] [CrossRef] [PubMed]
- Masenga, S.K.; Kabwe, L.S.; Chakulya, M.; Kirabo, A. Mechanisms of Oxidative Stress in Metabolic Syndrome. Int. J. Mol. Sci. 2023, 24, 7898. [Google Scholar] [CrossRef] [PubMed]
- Panic, A.; Stanimirovic, J.; Sudar-Milovanovic, E.; Isenovic, E.R. Oxidative stress in obesity and insulin resistance. Explor. Med. 2022, 3, 58–70. [Google Scholar] [CrossRef]
- Han, T.S.; Lean, M.E. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc. Dis. 2016, 5, 204800401663337. [Google Scholar] [CrossRef]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’emidio, S.; Armeni, M.; Bravi, V.; Bendini, M.G.; Mazza, A. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens. Res. 2017, 40, 947–963. [Google Scholar] [CrossRef]
- Bagheri, S.; Zolghadri, S.; Stanek, A. Beneficial Effects of Anti-Inflammatory Diet in Modulating Gut Microbiota and Controlling Obesity. Nutrients 2022, 14, 3985. [Google Scholar] [CrossRef] [PubMed]
- Naing, Y.T.; Sun, L. The Role of Splicing Factors in Adipogenesis and Thermogenesis. Mol. Cells 2023, 46, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Brożyna-Tkaczyk, K.; Zolghadri, S.; Cholewka, A.; Myśliński, W. The Role of Intermittent Energy Restriction Diet on Metabolic Profile and Weight Loss among Obese Adults. Nutrients 2022, 14, 1509. [Google Scholar] [CrossRef] [PubMed]
- She, Y.; Mangat, R.; Tsai, S.; Proctor, S.D.; Richard, C. The Interplay of Obesity, Dyslipidemia and Immune Dysfunction: A Brief Overview on Pathophysiology, Animal Models, and Nutritional Modulation. Front. Nutr. 2022, 9, 840209. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.L.; Shi, Y.H.; Hao, G.; Li, W.; Le, G.W. Increasing oxidative stress with progressive hyperlipidemia in human: Relation between malondialdehyde and atherogenic index. J. Clin. Biochem. Nutr. 2008, 43, 154–158. [Google Scholar] [CrossRef]
- Tangvarasittichai, S. Oxidative stress, insulin resistance, dyslipidemia and type 2 diabetes mellitus. World J. Diabetes 2015, 6, 456. [Google Scholar] [CrossRef] [PubMed]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuñiga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 122. [Google Scholar] [CrossRef]
- Frazier-wood, A.C.; Wang, Z. 3/6/18-Technoscience-Metabolic Syndrome. In Metabolic Syndrome; Springer: Berlin/Heidelberg, Germany, 2016; pp. 447–459. Available online: http://link.springer.com/10.1007/978-3-319-11251-0 (accessed on 8 January 2016).
- Wassink, A.M.J.; Olijhoek, J.K.; Visseren, F.L.J. The metabolic syndrome: Metabolic changes with vascular consequences. Eur. J. Clin. Investig. 2007, 37, 8–17. [Google Scholar] [CrossRef]
- Silveira Rossi, J.L.; Barbalho, S.M.; Reverete de Araujo, R.; Bechara, M.D.; Sloan, K.P.; Sloan, L.A. Metabolic syndrome and cardiovascular diseases: Going beyond traditional risk factors. Diabetes Metab. Res. Rev. 2022, 38, e3502. [Google Scholar] [CrossRef]
- Boarescu, P.M.; Boarescu, I.; Pop, R.M.; Roşan, Ş.H.; Bocșan, I.C.; Rus, V.; Mada, R.O.; Popa, I.D.; Neagu, N.; Bulboacă, A.E.; et al. Evaluation of Oxidative Stress Biomarkers, Pro-Inflammatory Cytokines, and Histological Changes in Experimental Hypertension, Dyslipidemia, and Type 1 Diabetes Mellitus. Int. J. Mol. Sci. 2022, 23, 1438. [Google Scholar] [CrossRef]
- Soleimani, M.; Barone, S.; Luo, H.; Zahedi, K. Pathogenesis of Hypertension in Metabolic Syndrome: The Role of Fructose and Salt. Int. J. Mol. Sci. 2023, 24, 4294. [Google Scholar] [CrossRef] [PubMed]
- Shariq, O.A.; Mckenzie, T.J. Obesity-related hypertension: A review of pathophysiology, management, and the role of metabolic surgery. Gland. Surg. 2020, 9, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Kwaifa, I.K.; Bahari, H.; Yong, Y.K.; Noor, S.M. Endothelial dysfunction in obesity-induced inflammation: Molecular mechanisms and clinical implications. Biomolecules 2020, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Mendizábal, Y.; Llorens, S.; Nava, E. Hypertension in metabolic syndrome: Vascular pathophysiology. Int. J. Hypertens. 2013, 2013, 230868. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Brożyna-Tkaczyk, K.; Myśliński, W. The role of obesity-induced perivascular adipose tissue (Pvat) dysfunction in vascular homeostasis. Nutrients 2021, 13, 3843. [Google Scholar] [CrossRef] [PubMed]
- Jakubiak, G.K.; Cieślar, G.; Stanek, A. Nitrotyrosine Nitrated Lipoproteins Cardiovascular Dysfunction in Patients with Type 2 Diabetes: What Do We, K.n.o.w.What Remains to Be Explained? Antioxidants 2022, 11, 856. [Google Scholar] [CrossRef] [PubMed]
- Clyne, A.M. Endothelial response to glucose: Dysfunction, metabolism, and transport. Biochem. Soc. Trans. 2021, 49, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Yanai, H.; Tomono, Y.; Ito, K.; Furutani, N.; Yoshida, H.; Tada, N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr. J. 2008, 7, 10. [Google Scholar] [CrossRef]
- Humar, R.; Resink, T.; Battegay, E.J. Vascular remodeling in hypertension. Hypertens. Princ. Pract. 2005, 85–98. [Google Scholar] [CrossRef]
- Martinez-Quinones, P.; McCarthy, C.G.; Watts, S.W.; Klee, N.S.; Komic, A.; Calmasini, F.B.; Priviero, F.; Warner, A.; Chenghao, Y.; Wenceslau, C.F. Hypertension induced morphological and physiological changes in cells of the arterial wall. Am. J. Hypertens. 2018, 31, 1067–1078. [Google Scholar] [CrossRef]
- Dorresteijn, J.A.N.; Van Der Graaf, Y.; Spiering, W.; Grobbee, D.E.; Bots, M.L.; Visseren, F.L.J. Relation between blood pressure and vascular events and mortality in patients with manifest vascular disease: J-curve revisited. Hypertension 2012, 59, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Fudim, M.; Jones, W.S. New curveball for hypertension guidelines? Blood pressure targets in peripheral artery disease. Circulation 2018, 138, 1815–1818. [Google Scholar] [CrossRef] [PubMed]
- Vrsalovic, M. Blood pressure goals in hypertensive patients with peripheral arterial disease. Eur. Hear. J.—Qual. Care Clin. Outcomes 2019, 5, 183. [Google Scholar] [CrossRef] [PubMed]
- Vona, R.; Gambardella, L.; Cittadini, C.; Straface, E. Review Article Biomarkers of Oxidative Stress in Metabolic Syndrome and Associated Diseases. Oxidative Med. Cell. Longev. 2019, 2019, 8267234. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Motz, E. Is Oxidative Stress the Pathogenic Mechanism Underlying Insulin Resistance, Diabetes, and Cardiovascular Disease? The Common Soil Hypothesis Revisited. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Zanetti, M.; Cappellari, G.G.; Semolic, A.; Boschelle, M.; Codarin, E. Fatty acids acutely enhance insulin-induced oxidative stress and cause insulin resistance by increasing mitochondrial reactive oxygen species (ROS) generation and nuclear factor-κB inhibitor (IκB)-nuclear factor-κB (NFκB) activation in rat muscle, in the absence of mitochondrial dysfunction. Diabetologia 2012, 55, 773–782. [Google Scholar] [PubMed]
- Newsholme, P.; Keane, K.N.; Carlessi, R.; Cruzat, V. Oxidative stress pathways in pancreatic β-cells and insulin-sensitive cells and tissues: Importance to cell metabolism, function, and dysfunction. Am. J. Physiol.—Cell Physiol. 2019, 317, C420–C433. [Google Scholar] [CrossRef] [PubMed]
- Panov, A.V.; Darenskaya, M.A.; Dikalov, S.I.; Kolesnikov, S.I. Metabolic Syndrome as the First Stage of Eldership; the Beginning of Real Aging. In Update in Geriatrics; Amornyotin, S., Ed.; IntechOpen: Rijeka, Croatia, 2021. [Google Scholar] [CrossRef]
- Krieger-Brauer, H.I.; Medda, P.K.; Kather, H. Insulin-induced activation of NADPH-dependent H2O2 generation in human adipocyte plasma membranes is mediated by Gα(i2). J. Biol. Chem. 1997, 272, 10135–10143. [Google Scholar] [CrossRef] [PubMed]
- Aggeli, I.K.; Theofilatos, D.; Beis, I.; Gaitanaki, C. Insulin-induced oxidative stress up-regulates heme oxygenase-1 via diverse signaling cascades in the C2 skeletal myoblast cell line. Endocrinology 2011, 152, 1274–1283. [Google Scholar] [CrossRef]
- Hernandez-Hernandez, M.E.; Torres-Rasgado, E.; Pulido-Perez, P.; Nicolás-Toledo, L.; Martínez-Gómez, M.; Rodríguez-Antolín, J.; Pérez-Fuentes, R.; Romero, J.R. Disordered Glucose Levels Are Associated with Xanthine Oxidase Activity in Overweight Type 2 Diabetic Women. Int. J. Mol. Sci. 2022, 23, 11177. [Google Scholar] [CrossRef]
- Higashi, Y. Roles of Oxidative Stress and Inflammation in Vascular Endothelial Dysfunction-Related Disease. Antioxidants 2022, 11, 1958. [Google Scholar] [CrossRef]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid Peroxidation: Production, Metabolism, and Signaling Mechanisms of Malondialdehyde and 4-Hydroxy-2-Nonenal. Oxid. Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef]
- Brandes, R.P.; Fleming, I.; Busse, R. Endothelial aging. Cardiovasc. Res. 2005, 66, 286–294. [Google Scholar] [CrossRef]
- Litvinova, L.; Atochin, D.N.; Fattakhov, N.; Vasilenko, M.; Zatolokin, P.; Kirienkova, E. Nitric oxide and mitochondria in metabolic syndrome. Front. Physiol. 2015, 6, 20. [Google Scholar] [CrossRef]
- Newsholme, P.; Cruzat, V.F.; Keane, K.N.; Carlessi, R.; De Bittencourt, P.I.H. Molecular mechanisms of ROS production and oxidative stress in diabetes. Biochem. J. 2016, 473, 4527–4550. [Google Scholar] [CrossRef]
- Eguchi, N.; Vaziri, N.D.; Dafoe, D.C.; Ichii, H. The role of oxidative stress in pancreatic β cell dysfunction in diabetes. Int. J. Mol. Sci. 2021, 22, 1509. [Google Scholar] [CrossRef]
- Martindale, J.L.; Holbrook, N.J. Cellular Response to Oxidative Stress: Signaling for Suicide and Survival. J. Cell. Physiol. 2002, 192, 1–15. [Google Scholar] [CrossRef]
- Bloom, S.I.; Liu, Y.; Tucker, J.R.; Islam, M.T.; Machin, D.R.; Abdeahad, H.; Thomas, T.G.; Bramwell, R.C.; Lesniewski, L.A.; Donato, A.J. Endothelial cell telomere dysfunction induces senescence and results in vascular and metabolic impairments. Aging Cell 2023, 22, e13875. [Google Scholar] [CrossRef]
- Jia, G.; Aroor, A.R.; Jia, C.; Sowers, J.R. Endothelial cell senescence in aging-related vascular dysfunction. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- Singh, U.; Devaraj, S.; Jialal, I. Vitamin E, oxidative stress, and inflammation. Annu. Rev. Nutr. 2005, 25, 151–174. [Google Scholar] [CrossRef] [PubMed]
- Gregório, B.M.; De Souza, D.B.; de Morais Nascimento, F.A.; Pereira, L.M.; Fernandes-Santos, C. The potential role of antioxidants in metabolic syndrome. Curr. Pharm. Des. 2016, 22, 859–869. Available online: http://www.eurekaselect.com/openurl/content.php?genre=article&issn=1381-6128&volume=22&issue=7&spage=859 (accessed on 27 January 2016). [CrossRef]
- Bilbis, L.S.; Muhammad, S.A.; Saidu, Y. The Potentials Of Antioxidant Micronutrients In The Management Of Metabolic Syndrome. J. Antioxid. Act. 2014, 1, 1–21. [Google Scholar] [CrossRef]
- Bhatti, M.I.; Bano, R.; Memon, F.R.; Shah, M.; Memon, R.A.; Memon, A.R. Effects of Vitamin E in the Management of Dyslipidemia in Combination with Statin Therapy. Pakistan J. Med. Health Sci. 2022, 16, 58–60. [Google Scholar] [CrossRef]
- Manning, P.J.; Sutherland, W.H.F.; Walker, R.J.; Williams, S.M.; de Jong, S.A.; Ryalls, A.R.; Berry, E.A. Effect of High-Dose Vitamin E on Insulin Resistance and Associated Parameters in Overweight Subjects. Diabetes Care 2004, 27, 2166–2171. [Google Scholar] [CrossRef]
- Asbaghi, O.; Nazarian, B.; Yousefi, M.; Anjom-Shoae, J.; Rasekhi, H.; Sadeghi, O. Effect of vitamin E intake on glycemic control and insulin resistance in diabetic patients: An updated systematic review and meta-analysis of randomized controlled trials. Nutr. J. 2023, 22, 10. [Google Scholar] [CrossRef]
- Gęgotek, A.; Skrzydlewska, E. Antioxidative and Anti-Inflammatory Activity of Ascorbic Acid. Antioxidants 2022, 11, 1993. [Google Scholar] [CrossRef]
- Wang, D.; Yang, X.; Chen, Y.; Gong, K.; Yu, M.; Gao, Y.; Wu, X.; Hu, H.; Liao, C.; Han, J.; et al. Ascorbic acid enhances low-density lipoprotein receptor expression by suppressing proprotein convertase subtilisin/kexin 9 expression. J. Biol. Chem. 2020, 295, 15870–15882. [Google Scholar] [CrossRef]
- Santosh, H.N.; David, C.M. Role of ascorbic acid in diabetes mellitus: A comprehensive review. J. Med. Radiol. Pathol. Surg. 2017, 4, 1–3. [Google Scholar] [CrossRef]
- Roohani, N.; Hurrell, R.; Kelishadi, R.; Schulin, R. Zinc and its importance for human health: An integrative review. J. Res. Med. Sci. 2013, 18, 144–157. [Google Scholar] [PubMed]
- Morelli, M.B.; Gambardella, J.; Castellanos, V.; Trimarco, V.; Santulli, G. Vitamin C and cardiovascular disease: An update. Antioxidants 2020, 9, 1227. [Google Scholar] [CrossRef] [PubMed]
- Ruz, M.; Carrasco, F.; Rojas, P.; Basfi-fer, K.; Hernández, M.C.; Pérez, A. Nutritional Effects of Zinc on Metabolic Syndrome and Type 2 Diabetes: Mechanisms and Main Findings in Human Studies. Biol. Trace Elem. Res. 2019, 188, 177–188. [Google Scholar] [CrossRef]
- Rashid, S.K.; Alhosin, M. The role of zinc deficiency in endothelial dysfunction. Eur. J. Cell Sci. 2019, 25, 22–25. [Google Scholar] [CrossRef]
- Jarosz, M.; Olbert, M.; Wyszogrodzka, G.; Młyniec, K.; Librowski, T. Antioxidant and anti-inflammatory effects of zinc. Zinc-dependent NF-κB signaling. Inflammopharmacology 2017, 25, 11–24. [Google Scholar] [CrossRef]
- Abdollahi, S.; Toupchian, O.; Jayedi, A.; Meyre, D.; Tam, V.; Soltani, S. Zinc Supplementation and Body Weight: A Systematic Review and Dose-Response Meta-analysis of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 398–411. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Mofrad, M.D.; do Nascimento, I.J.B.; Milajerdi, A.; Mokhtari, T.; Esmaillzadeh, A. The effect of zinc supplementation on blood pressure: A systematic review and dose–response meta-analysis of randomized-controlled trials. Eur. J. Nutr. 2020, 59, 1815–1827. [Google Scholar] [CrossRef]
- Shi, Y.; Zou, Y.; Shen, Z.; Xiong, Y.; Zhang, W.; Liu, C.; Chen, S. Trace elements, PPARs, and metabolic syndrome. Int. J. Mol. Sci. 2020, 21, 2612. [Google Scholar] [CrossRef]
- Bo, S.; Durazzo, M.; Gambino, R.; Berutti, C.; Milanesio, N.; Caropreso, A.; Gentile, L.; Cassader, M.; Cavallo-Perin, P.; Pagano, G. Associations of dietary and serum copper with inflammation, oxidative stress, and metabolic variables in adults. J. Nutr. 2008, 138, 305–310. [Google Scholar] [CrossRef]
- Wen, H.; Niu, X.; Hu, L.; Sun, N.; Zhao, R.; Wang, Q.; Li, Y. Dietary copper intake and risk of myocardial infarction in US adults: A propensity score-matched analysis. Front. Cardiovasc. Med. 2022, 9, 942000. [Google Scholar] [CrossRef]
- Rayman, M.P. Selenium and human health. Lancet 2012, 379, 1256–1268. [Google Scholar] [CrossRef] [PubMed]
- Mohammadifard, N.; Humphries, K.H.; Gotay, C.; Mena-Sánchez, G.; Salas-Salvadó, J.; Esmaillzadeh, A.; Ignaszewski, A.; Sarrafzadegan, N. Trace minerals intake: Risks and benefits for cardiovascular health. Crit. Rev. Food Sci. Nutr. 2019, 59, 1334–1346. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Tan, H.Y.; Li, S.; Xu, Y.; Guo, W.; Feng, Y. Supplementation of micronutrient selenium in metabolic diseases: Its role as an antioxidant. Oxid. Med. Cell. Longev. 2017, 2017, 7478523. [Google Scholar] [CrossRef] [PubMed]
- Koziróg, M.; Poliwczak, A.R.; Duchnowicz, P.; Koter-Michalak, M.; Sikora, J.; Broncel, M. Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J. Pineal Res. 2011, 50, 261–266. [Google Scholar] [CrossRef]
- Meng, X.; Li, Y.; Li, S.; Zhou, Y.; Gan, R.Y.; Xu, D.P.; Li, H.B. Dietary sources and bioactivities of melatonin. Nutrients 2017, 9, 367. [Google Scholar] [CrossRef] [PubMed]
- Imenshahidi, M.; Karimi, G.; Hosseinzadeh, H. Effects of melatonin on cardiovascular risk factors and metabolic syndrome: A comprehensive review. Naunyn Schmiedebergs Arch. Pharmacol. 2020, 393, 521–536. [Google Scholar] [CrossRef] [PubMed]
- Otamas, A.; Grant, P.J.; Ajjan, R.A. Diabetes and atherothrombosis: The circadian rhythm and role of melatonin in vascular protection. Diabetes Vasc. Dis. Res. 2020, 17, 1479164120920582. [Google Scholar] [CrossRef] [PubMed]
- Hnia, K.; Gayraud, J.; Hugon, G.; Ramonatxo, M.; De La Porte, S.; Matecki, S.; Mornet, D. L-arginine decreases inflammation and modulates the nuclear factor-κB/matrix metalloproteinase cascade in Mdx muscle fibers. Am. J. Pathol. 2008, 172, 1509–1519. [Google Scholar] [CrossRef] [PubMed]
- Bogdanski, P.; Suliburska, J.; Grabanska, K.; Musialik, K.; Cieslewicz, A.; Skoluda, A.; Jablecka, A. Effect of 3-month L-arginine supplementation on insulin resistance and tumor necrosis factor activity in patients with visceral obesity. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 816–823. [Google Scholar]
- Szlas, A.; Kurek, J.M.; Krejpcio, Z. The Potential of L-Arginine in Prevention and Treatment of Disturbed Carbohydrate and Lipid Metabolism. Nutrients 2022, 14, 961. [Google Scholar] [CrossRef]
- Hosseini, A.; Razavi, B.M.; Banach, M.; Hosseinzadeh, H. Quercetin and metabolic syndrome: A review. Phyther. Res. 2021, 35, 5352–5364. [Google Scholar] [CrossRef]
- Gouveia, H.J.C.B.; Urquiza-Martínez, M.V.; Manhães-de-Castro, R.; Costa-de-Santana, B.J.R.; Villarreal, J.P.; Mercado-Camargo, R.; Torner, L.; Aquino, J.d.S.; Toscano, A.E.; Guzmán-Quevedo, O. Effects of the Treatment with Flavonoids on Metabolic Syndrome Components in Humans: A Systematic Review Focusing on Mechanisms of Action. Int. J. Mol. Sci. 2022, 23, 8344. [Google Scholar] [CrossRef]
- Noreddin, A. Readings in Advanced Pharmacokinetics—Theory, Methods and Applications; IntechOpen: London, UK, 2012. [Google Scholar]
- Abdel-Daim, M.M.; El-Tawil, O.S.; Bungau, S.G.; Atanasov, A.G. Applications of Antioxidants in Metabolic Disorders and Degenerative Diseases: Mechanistic Approach. Oxid. Med. Cell. Longev. 2019, 2019, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Galleano, M.; Calabro, V.; Prince, P.D.; Litterio, M.C.; Piotrkowski, B.; Vazquez-Prieto, M.A.; Miatello, R.M.; Oteiza, P.I.; Fraga, C.G. Flavonoids and metabolic syndrome. Ann. N. Y. Acad. Sci. 2012, 1259, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Li, X.; Zhu, C.; Sun, J.; Tian, L.; Chen, W.; Bai, W. The target cells of anthocyanins in metabolic syndrome. Crit. Rev. Food Sci. Nutr. 2019, 59, 921–946. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.L.; Hsu, C.N. Metabolic Syndrome Programming and Reprogramming: Mechanistic Aspects of Oxidative Stress. Antioxidants 2022, 11, 2108. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liao, B.; Wang, C.; Zhong, O.; Lei, X.; Yang, Y. Effects of Antioxidant Supplementation on Metabolic Disorders in Obese Patients from Randomized Clinical Controls: A Meta-Analysis and Systematic Review. Oxid. Med. Cell. Longev. 2022, 2022, 7255413. [Google Scholar] [CrossRef] [PubMed]
- Ghadimi, D.; Hemmati, M.; Karimi, N.; Khadive, T. Soy isoflavone genistein is a potential agent for metabolic syndrome treatment: A narrative review. J. Adv. Med. Biomed. Res. 2020, 28, 64–75. [Google Scholar] [CrossRef]
- Syndrome, M. Potential Effects of Soy Isoflavones on the Prevention of Metabolic Syndrome. Molecules 2021, 26, 5863. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Ito, Y.; Inoue, T.; Hamajima, N. Inverse association of serum carotenoids with prevalence of metabolic syndrome among Japanese. Clin. Nutr. 2011, 30, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Chen, X.; Jha, K.; Beydoun, H.A.; Zonderman, A.B.; Canas, J.A. Carotenoids, vitamin A, and their association with the metabolic syndrome: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.P.M.; Souza, A.C.R.; Vasconcelos, A.R.; Prado, P.S.; Name, J.J. Antioxidant and anti-inflammatory mechanisms of action of astaxanthin in cardiovascular diseases (Review). Int. J. Mol. Med. 2021, 47, 37–48. [Google Scholar] [CrossRef]
- Bremer, A.A. Resveratrol use in metabolic syndrome. Metab. Syndr. Relat. Disord. 2014, 12, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Ostadmohammadi, V.; Raygan, F.; Sharif, M.R.; Sahebkar, A. The effects of N-acetylcysteine administration on metabolic status and serum adiponectin levels in patients with metabolic syndrome: A randomized, double-blind, placebo-controlled trial. J. Funct. Foods 2022, 99, 105299. [Google Scholar] [CrossRef]
- Brnoliakova, Z.; Knezl, V.; Sotnikova, R.; Gasparova, Z. Metabolic Syndrome in Hypertriglyceridemic Rats: Effects of Antioxidants. Physiol. Res. 2023, 72, S31–S35. [Google Scholar] [CrossRef] [PubMed]
- Rani, M.; Aggarwal, R.; Vohra, K. Effect of N-Acetylcysteine on Metabolic Profile in Metabolic Syndrome Patients. Metab. Syndr. Relat. Disord. 2020, 18, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.A.; Franco, F.N.; Caldeira, C.A.; de Araújo, G.R.; Vieira, A.; Chaves, M.M.; Lara, R.C. Antioxidant effect of Resveratrol: Change in MAPK cell signaling pathway during the aging process. Arch. Gerontol. Geriatr. 2021, 92, 104266. [Google Scholar] [CrossRef] [PubMed]
- Hou, C.Y.; Tain, Y.L.; Yu, H.R.; Huang, L.T. The effects of resveratrol in the treatment of metabolic syndrome. Int. J. Mol. Sci. 2019, 20, 535. [Google Scholar] [CrossRef]
- Andrade, J.M.O.; Frade, A.C.M.; Guimarães, J.B.; Freitas, K.M.; Lopes, M.T.P.; Guimarães, A.L.S.; de Paula, A.M.B.; Coimbra, C.C.; Santos, S.H.S. Resveratrol increases brown adipose tissue thermogenesis markers by increasing SIRT1 and energy expenditure and decreasing fat accumulation in adipose tissue of mice fed a standard diet. Eur. J. Nutr. 2014, 53, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Kim, O.Y.; Chung, J.Y.; Song, J. Effect of resveratrol on adipokines and myokines involved in fat browning: Perspectives in healthy weight against obesity. Pharmacol. Res. 2019, 148, 104411. [Google Scholar] [CrossRef]
- Wang, G.; Wang, Y.; Yao, L.; Gu, W.; Zhao, S.; Shen, Z.; Lin, Z.; Liu, W.; Yan, T. Pharmacological Activity of Quercetin: An Updated Review. Evid.-Based Complement. Altern. Med. 2022, 2022, 3997190. [Google Scholar] [CrossRef] [PubMed]
- Pei, Y.; Parks, J.S.; Kang, H.W. Quercetin alleviates high-fat diet-induced inflammation in brown adipose tissue. J. Funct. Foods 2021, 85, 104614. [Google Scholar] [CrossRef]
- Kábelová, A.; Malínská, H.; Marková, I.; Hűttl, M.; Chylíková, B.; Šeda, O. Quercetin supplementation alters adipose tissue and hepatic transcriptomes and ameliorates adiposity, dyslipidemia, and glucose intolerance in adult male rats. Front. Nutr. 2022, 9, 952065. [Google Scholar] [CrossRef] [PubMed]
- Hurrle, S.; Hsu, W.H. The etiology of oxidative stress in insulin resistance. Biomed. J. 2017, 40, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Yahya, A.Z.; Taqa, G.A.; Alkataan, M.A. Evaluation of the Effects of N-Acetylcysteine on Serum Glucose, Lipid Profile, and Body Weight in Rats With Fructose-Induced Metabolic Syndrome. Mil. Med. Sci. Lett. 2023, 92, 194–207. [Google Scholar] [CrossRef]
- Gori, T. Exogenous no therapy for the treatment and prevention of atherosclerosis. Int. J. Mol. Sci. 2020, 21, 2703. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Ng, C.; He, J.; Yang, M.; Luo, X.; Herbert, T.P.; Whitehead, J.P. Vitamin C protects against hypoxia, inflammation, and ER stress in primary human preadipocytes and adipocytes. Mol. Cell. Endocrinol. 2022, 556, 111740. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.K.; Chin, K.Y.; Ima-Nirwana, S. Vitamin C: A review on its role in the management of metabolic syndrome. Int. J. Med. Sci. 2020, 17, 1625–1638. [Google Scholar] [CrossRef]
- Mumtaz, S.; Ali, S.; Tahir, H.M.; Kazmi, S.A.R.; Shakir, H.A.; Mughal, T.A.; Mumtaz, S.; Summer, M.; Farooq, M.A. Aging and its treatment with vitamin C: A comprehensive mechanistic review. Mol. Biol. Rep. 2021, 48, 8141–8153. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Hosseini-Esfahani, F.; Esfandiar, Z.; Hosseinpour-Niazi, S.; Azizi, F. Associations between dietary antioxidant intakes and cardiovascular disease. Sci. Rep. 2022, 12, 1504. [Google Scholar] [CrossRef]
- Miao, X.; Sun, W.; Fu, Y.; Miao, L.; Cai, L. Zinc homeostasis in the metabolic syndrome and diabetes. Front. Med. China 2013, 7, 31–52. [Google Scholar] [CrossRef]
- Gembillo, G.; Labbozzetta, V.; Giuffrida, A.E.; Peritore, L.; Calabrese, V.; Spinella, C.; Stancanelli, M.R.; Spallino, E.; Visconti, L.; Santoro, D. Potential Role of Copper in Diabetes and Diabetic Kidney Disease. Metabolites 2023, 13, 17. [Google Scholar] [CrossRef]
- Carson, C.; Lawson, H.A. Epigenetics of metabolic syndrome. Physiol. Genom. 2018, 50, 947–955. [Google Scholar] [CrossRef]
- Wu, Y.L.; Lin, Z.J.; Li, C.C.; Lin, X.; Shan, S.K.; Guo, B.; Zheng, M.H.; Li, F.; Yuan, L.Q.; Li, Z.H. Epigenetic regulation in metabolic diseases: Mechanisms and advances in clinical study. Signal Transduct. Target Ther. 2023, 8, 98. [Google Scholar] [CrossRef] [PubMed]
- Nuotio, M.L.; Pervjakova, N.; Joensuu, A.; Karhunen, V.; Hiekkalinna, T.; Milani, L.; Kettunen, J.; Järvelin, M.-R.; Jousilahti, P.; Metspalu, A.; et al. An epigenome-wide association study of metabolic syndrome and its components. Sci. Rep. 2020, 10, 20567. [Google Scholar] [CrossRef] [PubMed]
- Ramzan, F.; Vickers, M.H.; Mithen, R.F. Epigenetics, microrna and metabolic syndrome: A comprehensive review. Int. J. Mol. Sci. 2021, 22, 5047. [Google Scholar] [CrossRef] [PubMed]
- Beetch, M.; Harandi-Zadeh, S.; Shen, K.; Lubecka, K.; Kitts, D.D.; O’Hagan, H.M.; Stefanska, B. Dietary antioxidants remodel DNA methylation patterns in chronic disease. Br. J. Pharmacol. 2020, 177, 1382–1408. [Google Scholar] [CrossRef] [PubMed]
- Çakır, I.; Hadley, C.K.; Pan, P.L.; Bagchi, R.A.; Ghamari-Langroudi, M.; Porter, D.T.; Wang, Q.; Litt, M.J.; Jana, S.; Hagen, S.; et al. Histone deacetylase 6 inhibition restores leptin sensitivity and reduces obesity. In Nature Metabolism; Springer: New York, NY, USA, 2022; Volume 4, pp. 44–59. [Google Scholar]
- Yoon, G.E.; Jung, J.K.; Lee, Y.H.; Jang, B.C.; In Kim, J. Histone deacetylase inhibitor CG200745 ameliorates high-fat diet-induced hypertension via inhibition of angiotensin II production. Naunyn Schmiedebergs Arch. Pharmacol. 2020, 393, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Pedro Ferreira, J.; Pitt, B.; Zannad, F. Histone deacetylase inhibitors for cardiovascular conditions and healthy longevity. Lancet Health Longev. 2021, 2, e371–e379. [Google Scholar] [CrossRef] [PubMed]
- Kee, H.J.; Kim, I.; Jeong, M.H. Zinc-dependent histone deacetylases: Potential therapeutic targets for arterial hypertension. Biochem. Pharmacol. 2022, 202, 115111. [Google Scholar] [CrossRef] [PubMed]
- Ullah, H.; De Filippis, A.; Santarcangelo, C.; Daglia, M. Epigenetic regulation by polyphenols in diabetes and related complications. Med. J. Nutr. Metab. 2020, 13, 289–310. [Google Scholar] [CrossRef]
- Číž, M.; Dvořáková, A.; Skočková, V.; Kubala, L. The role of dietary phenolic compounds in epigenetic modulation involved in inflammatory processes. Antioxidants 2020, 9, 691. [Google Scholar] [CrossRef]
- Keramat, S.; Sharebiani, H.; Patel, M.; Fazeli, B.; Stanek, A. The Potential Role of Antioxidants in the Treatment of Peripheral Arterial Disease: A Systematic Review. Antioxidants 2022, 11, 2126. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, G.F.S.; Silva, G.D.B.; Pavan, A.R.; Chiba, D.E.; Chin, C.M.; Dos Santos, J.L. Epigenetic regulatory mechanisms induced by resveratrol. Nutrients 2017, 9, 1201. [Google Scholar] [CrossRef] [PubMed]

| Case Report | Cross Sectional Study | RCT 1 | Meta-Analysis and Systematic Review |
|---|---|---|---|
| 13 | 7 | 6 | 8 |
| Antioxidants | Sources | Functions | |||||
|---|---|---|---|---|---|---|---|
| Antioxidant Function | Anti-Inflammatory Role | Obesity, Dyslipidemia, Adipose Tissue Remodeling | Hyperglycemia, Insulin Resistance, Hyperinsulinemia | Hypertension | Endothelial Dysfunction | ||
| Vitamin E | Vegetable oils, safflower seed oil, soy oil, palm oil [52] | Scavenging free radicals [53] ↑ NO bioavailability ↓ NOX activity [54] Inhibition of lipid peroxidation [54] | ↓ CRP level ↓ Pro-inflammatory cytokines (IL-1 and 6, TNF) ↓ PGE2 synthesis ↓ Chemokine IL-8, PAI-1 levels [52] | Inhibition of cholesterol synthesis ↓ LDL oxidation [55] | Improving insulin sensitivity ↓ Plasma glucose [56] ↓ HbA1c [57] | ↓ Blood pressure | ↓ Monocyte adhesion to endothelium ↓ E-selectin, ICAM-1, and VCAM-1 ↓ Platelet aggregation [52] ↓ Risk of CVD morbidity and mortality [54] protecting endothelial cells from chromatin damage protecting endothelial cells from telomere shortening [6] |
| Vitamin C | Cherries, wild rose, blackcurrant, guava, peppers, brussels, broccoli, grapefruit, pomelo, lemon, orange, lime [58] | ↓ ROS production ↑ NO bioavailability [54] ↓ XO activity ↓ NOX activity ↑ SOD activity ↑ GPx activity ↑ GR activity ↑ TrxR activity Preventing lipid peroxidation [58] | ↓ IL-2,6,12, IFN-γ Activation of Nrf2 Suppressing NF-κB, TNF-α pathway ↓ CRP [58] | ↑ HDL ↓ Cholesterol, LDL and TG [59] | ↓ Plasma insulin ↓ Plasma TGL ↓ HbA1c ↓ FBS [60] | ↓ Systolic blood pressure [61] | ↓ Endothelial dysfunction [62] ↓ Risk of CVD morbidity and mortality [54] |
| Zinc | Milk, cheese, red meat, or liver [61] | ↑ CuZn-SOD activity [63] ↑ eNOS expression levels ↑ NO availability [64] | Suppression of the NF-B pathway ↑ PPAR-α expression [65] | ↑ Leptin synthesis Improve leptin sensitivity [66] | ↓ Glucagon secretion ↓ Insulin resistance ↑ Insulin sensitivity ↑ GLUT4 Translocation [63] | ↓ Systolic blood pressure [67] | Prevention of endothelial dysfunction [64] |
| Copper | Milk, meat, seafood, vegetables, fruits [68] | Scavenging free radicals ↑ CuZn-SOD activity [69] | Activation of PPAR-α signaling [68] | ↓ Total cholesterol ↓ LDL [69] | ↓ Plasma glucose [69] ↓ Intramuscular fat accretion [68] | ↓ Diastolic blood pressure [69] | Benefited the fibers of the blood vessel wall by maintaining its toughness and suppleness [70] |
| Selenium | Fish, such as tuna and mackerel, animal foods, cereals, plant sources, such as garlic, onions, and broccoli [71] | ↑ NO bioavailability ↓ Lipid peroxidation ↑ Antioxidant capacity in liver and kidney [72] ↑ GSH in the RBCs and liver ↑ Antioxidant enzyme activities (↑ GPx activity) [73] ↓ MDA [74] | ↓ TNF-α, IL-1β, PGE2 [68] ↓ Leukocyte and neutrophil count in circulation ↓ CRP, IL-6 ↓ MDA Inhibition of NF-B [74] | ↓ Leptin resistance Improving hyperlipidemia [73] ↑ HDL ↓ LDL ↓ TG ↓ Ratio of total cholesterol to HDL cholesterol [71] | ↓ Blood glucose ↓ Diabetes prevalence [71] ↑ Insulin secretion ↓ Insulin resistance [73] | High levels of selenium: ↑ incidence of hypertension | Inhibition of platelet aggregation [72] |
| Melatonin | Eggs and fish, nuts, some cereals, germinated legumes or seeds, mushrooms [75] | Scavenging of free radicals ↓ Lipid peroxidation ↑ NO synthesis ↓ MDA Activation of SOD, CAT, and GR [74] Activation of SIRT1/Nrf2 signaling pathway ↓ Oxidative stress damage [75] | Down-regulation of chemokine expression Inhibition of the NF-κB phosphorylation of PI3K/Akt, p38, ERK, JNK and MAPK [75] ↓ NOX ↓ Pro-inflammatory mediators (COX-2, TNF-α, iNOS) [76] | ↓ LDL ↑ HDL [74] ↓ Leptin resistance [77] ↓ Total cholesterol, TG, and ox-LDL ↓ Body weight ↓ Intra-abdominal visceral fat deposition [76] | Improvement in insulin resistance ↓ Hyperinsulinemia ↓ Hyperglycemia ↓ HbA1c ↓ Incidence of T2D [77] | ↓ Blood pressure [74] | Prevention of endothelial dysfunction [76] ↓ E-selectin, ICAM-1, and VCAM-1 [76] Inhibition of platelet aggregation Alteration of levels/activity of proteins involved in the coagulation cascade [77] |
| L-arginine | Seafood, watermelon juice, nuts, seeds, algae, meats, rice protein concentrate, and soy protein isolate [78] | ↑ ↓ ROS production ↑ SOD activity ↓ Lipid peroxidation [79] NO bioavailability ↓ MDA [80] | ↓ TNF-α, IL-1β, and IL-6 secretion [78] | ↓ Total cholesterol, LDL and TG ↑ HDL ↑ Adiponectin ↓ Body fat ↓ FFA ↓ Leptin [80] | ↓ Risk of diabetes ↑ Insulin secretion ↓ Blood glucose ↑ Insulin sensitivity [80] | ↓ Blood pressure [80] | Improvement in endothelial function [80] |
| Quercetin (Flavonol) | Citrus fruits, apples, grapes, dark cherries and dark berries, onions, parsley and sage, tea, olive oil, red wine [53], mangoes, buckwheat, plums, and tomatoes [6] | ROS scavenger Inhibition of lipid peroxidation Inhibition of ROS production up-regulating the expression of SOD, CAT, and GSH ↑ TAC and GPX ↓ MDA Prevention of ROS production by inhibition of NOX2 Cu2+ and Fe2+ chelation [6] | Inhibition of neutrophil infiltration Inhibition of NLRP3 pathways Inhibition of NF-κB pathways Inhibition of ROS/AMPK pathways ↓ IL-6 and TNFα [6] | ↓ Inflammation in BAT Promoting thermogenesis and browning of WAT [6] ↓ Ox-LDL ↓ Body weight [53] ↓ TG ↓ Cholesterol ↑ Adiponectin ↓ Leptin ↑ HDL [81] ↓ Waist circumference [82] | ↓ Blood glucose ↓ Insulin resistance ↑ Insulin ↓ HbA1c [81] ↑ β-cell number [82] | ↓ Systolic blood pressure [53] | Removal of endothelial cells aging Vasodilatory effect due to up-regulation of eNOS Anti-atherosclerosis effects Reduction in CVD [6] |
| Flavones | Dried oregano, dried parsley [53] | ↑ Activation of PPARs ↓ MCP-1 ↓ TNF-α ↓ INF-γ ↓ IL-1β ↓ IL-6 [83] | ↑ Adiponectin ↓ Body weight ↓ TG ↓ Cholesterol ↓ LDL ↓ V-LDL ↓ Apo-B [83] | ↑ Glucose tolerance glycemic control improvement ↓ Insulin resistance Regulation of GLUT4 expression [83] | Blockage of macrophage foam cell formation [83] | ||
| Flavanones | Grapefruit juice and cooked tomato [53] | Stimulation of the antioxidant defense system and apoptosis [84] ↑ Antioxidant Capacity [82] | ↓ CRP ↓ TNF-α ↓ IL-6 [82] | ↓ LDL ↑ HDL ↓ TG ↓ Cholesterol ↓ ApoB ↑ Adiponectin [82] | ↑ Insulin sensitivity ↑ Insulin signaling [53] ↓ Blood glucose ↓ Insulin resistance ↓ C-peptide ↓ Glucose intolerance ↓ HbA1c ↑ GLUT4 [82] | ↓ Blood pressure [82] | ↑ Endothelium-dependent vasodilation ↑ NO production ↓ IL-6 ↓ E-selectin ↓ P-selectin ↓ VCAM-1 ↓ ICAM-1 [82] |
| Catechins (Flavanol) | Brewed green tea, black tea, blueberries, fava beans, cocoa, and dark chocolate [53] | ↓ ROS formation and NOX activity ↑Phosphorylation of eNOS and ↑ NOS production using the PI3k-dependent pathway ↑ GSH [53] ↑ NO and consequently decrease in formation of reactive oxygen and nitrogen species [24] | Inhibition TNF-α- mediated NF-κB, and MAPKs activation [85] | ↓ Body weight ↓ BMI ↓ Cholesterol ↓ LDL ↓ TG [53] | ↓ Blood glucose ↓ Glucose intolerance ↑ Insulin sensitivity [53] | ↓ Blood pressure [53] | ↓ Endothelial dysfunction [53] |
| Anthocyanins | Blueberries, strawberries, pomegranates, wine, asparagus, elderberry juice concentrate [53] | Inhibition of lipid peroxidation [21] Suppressing protein levels of NOX1 and NOX4 Up-regulating Nrf2 [86] ↓MDA [85] | ↓ CRP ↓ IL-1β [82] Up-regulation of the PPARα ↓ Serum leptin and resistin ↓ TNF-α ↓ IL-6 ↓ IL-12 Suppressing iNOS and COX-2 Inhibition of signaling pathway of MAPK and NF-κB [86] ↓ MCP-1 [87] | ↓ BMI ↓ Body weight [88] ↓ ApoB [82] ↑ HDL ↓ LDL ↓ Cholesterol ↓ TG ↓ Hypertrophy of the adipocytes in epididymal WAT [86] | ↓ Insulin resistance GLUT4 and GLUT1, and thereby Improvement in insulin sensitivity | ↓ Systolic blood pressure [53] | ↑ Von Willebrand factor ↓ Endothelial dysfunction ↓ P-selectin [82] Inhibition of ICAM-1 and VCAM-1 ↑ eNOS expression and NO release [87] |
| Genistein (Isoflavones) | Soy and fava beans, green bean, kudzu root, and alfalfa sprouts [53] | Preventing phosphorylation of JNK Activation of Akt /ERK 1,2 pathway [89] ↑ eNOS activity and blocking NADPH-stimulated ROS production Suppression of superoxide production and NOX4 expression ↓ MDA [90] | ↓ CRP [53] ↓ TNF-α [82] Activation of PPARs and AMPK ↓ IL-6 [89] | ↓ TG ↓ Cholesterol ↓ Visfatin ↓ LDL and ox-LDL ↑ HDL ↑ Adiponectin [53] ↑ β-oxidation of FA ↓ Lipogenesis Preventing de-novo lipid synthesis [89] Promotion of browning of white adipocytes [90] | ↓ Insulin resistance [82] ↑ Proliferation of βcells [89] ↓ HbA1c ↓ Blood glucose [90] | ↓ Blood pressure [53] | ↓ Circulating ICAM ↓ Endothelial dysfunction [53] ↓ ET-1 NO production via PKA/eNOS/NO signaling ↑ Expression of E-selectin, P-selectin, MCP-1, and IL-8 [90] |
| Carotenoids | Fruits (tangerines, cantaloupes, papayas, and oranges) and vegetables (carrot, pumpkin, spinach, sweet potato, tomato, broccoli, and green peas) [53] | ↓ Production of free radicals [91] Serve as precursors for retinol (vitamin A), retinaldehyde, and retinoic acid, among other substances; retinoid conversion products that play important roles as transcriptional regulators in the visual cycle and gene regulation link [92] | Down-regulation of NF-κB and MAPK signaling pathways, Reducing the release of pro-inflammatory cytokines [93] | ↑ Adiponectin ↓ Body weight ↓ Visceral fat ↓ Lipid storage ↓ LDL [53] ↓ TG ↑ HDL [91] Reversing cholesterol transport by HDL [93] | ↑ Insulin sensitivity ↓ Insulin resistance [53] ↓ Blood glucose [91] | ↓ Blood pressure [53] | ↓ Endothelial dysfunction ↓ PAI-1 [53] Delay the progression of cardiovascular diseases ↑ NO bioavailability ↓ Accumulation of cholesterol in foam cells and the formation of atherosclerotic plaques [93] |
| Resveratrol | Grapes, apples, blueberries, plums, wine, peanuts [6], and dark chocolate [53] | ↓ H2O2 production ↑ Level of regulatory T cells ↓ ROS by inhibiting the MAPK pathways [6] | Inhibition of PKA and Akt/PKB pathway [6] | Acting as a WAT remodeling to BAT ↓ Accumulation of glycerol in adipose tissue Promoting thermogenesis by activation of SIRT1 and suppressing white adipogenesis [6] | ↑ Insulin production ↓ Insulin resistance [87] ↓ Blood glucose [94] | ↓ Blood pressure ↑ Na+ excretion (renal) [53] | ↑ NO production Up-regulation of eNOS expression Suppressing the synthesis of ET-1 [6] |
| N-acetylcysteine | Allium plant [87] | ↑ Endogenous concentrations of total glutathione Scavenging free radicals Suppressing ROS generation [95] ↑ Intracellular cysteine levels Replenishing systemic pools of (LMW) thiols and reduced protein sulfhydryl groups, which are implicated in the regulation of the redox stats [96] | ↓ CRP [97] Blocking NF-κB Inhibition of the release of IL-1, IL-6, and TNF [96] ↓ Gene expression of pro-inflammatory cytokines [33] | ↓ TG ↑ HDL [97] ↓ Cholesterol ↓ LDL ↓ VLDL Preventing lipid accumulation in BAT [96] | ↑ Insulin secretion [96] ↓ Blood glucose ↓ Insulin resistance [95] | ↓ Blood pressure [87] | ↑ NO [97] Stabilizing the production of atherosclerotic plaque [96] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharebiani, H.; Mokaram, M.; Mirghani, M.; Fazeli, B.; Stanek, A. The Effects of Antioxidant Supplementation on the Pathologic Mechanisms of Metabolic Syndrome and Cardiovascular Disease Development. Nutrients 2024, 16, 1641. https://doi.org/10.3390/nu16111641
Sharebiani H, Mokaram M, Mirghani M, Fazeli B, Stanek A. The Effects of Antioxidant Supplementation on the Pathologic Mechanisms of Metabolic Syndrome and Cardiovascular Disease Development. Nutrients. 2024; 16(11):1641. https://doi.org/10.3390/nu16111641
Chicago/Turabian StyleSharebiani, Hiva, Mina Mokaram, Melika Mirghani, Bahare Fazeli, and Agata Stanek. 2024. "The Effects of Antioxidant Supplementation on the Pathologic Mechanisms of Metabolic Syndrome and Cardiovascular Disease Development" Nutrients 16, no. 11: 1641. https://doi.org/10.3390/nu16111641







