Diet Quality and Resilience through Adulthood: A Cross-Sectional Analysis of the WELL for Life Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Measures
2.2.1. Main Outcome
2.2.2. Primary Exposure: Resilience
2.2.3. Covariates: Sociodemographics, Perceived Stress, Lifestyle (and BMI), and Mental Health
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kris-Etherton, P.M.; Petersen, K.S.; Velarde, G.; Barnard, N.D.; Miller, M.; Ros, E.; O’Keefe, J.H.; Williams, K., Sr.; Horn, L.V.; Na, M.; et al. Barriers, Opportunities, and Challenges in Addressing Disparities in Diet-Related Cardiovascular Disease in the United States. J. Am. Heart Assoc. 2020, 9, e014433. [Google Scholar] [CrossRef] [PubMed]
- Mohebi, R.; Chen, C.; Ibrahim, N.E.; McCarthy, C.P.; Gaggin, H.K.; Singer, D.E.; Hyle, E.P.; Wasfy, J.H.; Januzzi, J.L., Jr. Cardiovascular Disease Projections in the United States Based on the 2020 Census Estimates. J. Am. Coll. Cardiol. 2022, 80, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P. Sleep patterns, diet quality and energy balance. Physiol. Behav. 2014, 134, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Qiao, J.; Lin, X.; Wu, Y.; Huang, X.; Pan, X.; Xu, J.; Wu, J.; Ren, Y.; Shan, P.F. Global burden of non-communicable diseases attributable to dietary risks in 1990-2019. J. Hum. Nutr. Diet. 2022, 35, 202–213. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 2015, 132, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Zhong, V.W.; Ning, H.; Van Horn, L.; Carnethon, M.R.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Diet Quality and Long-Term Absolute Risks for Incident Cardiovascular Disease and Mortality. Am. J. Med. 2021, 134, 490–498 e424. [Google Scholar] [CrossRef]
- Micha, R.; Peñalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef]
- Liu, J.; Rehm, C.D.; Onopa, J.; Mozaffarian, D. Trends in diet quality among youth in the United States, 1999–2016. JAMA 2020, 323, 1161–1174. [Google Scholar] [CrossRef] [PubMed]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef] [PubMed]
- de Andrade, S.C.; Previdelli, A.N.; Cesar, C.L.G.; Marchioni, D.M.L.; Fisberg, R.M. Trends in diet quality among adolescents, adults and older adults: A population-based study. Prev. Med. Rep. 2016, 4, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Harshfield, E.L.; Pennells, L.; Schwartz, J.E.; Willeit, P.; Kaptoge, S.; Bell, S.; Shaffer, J.A.; Bolton, T.; Spackman, S.; Wassertheil-Smoller, S. Association between depressive symptoms and incident cardiovascular diseases. JAMA 2020, 324, 2396–2405. [Google Scholar] [CrossRef] [PubMed]
- Gooding, H.C.; Gidding, S.S.; Moran, A.E.; Redmond, N.; Allen, N.B.; Bacha, F.; Burns, T.L.; Catov, J.M.; Grandner, M.A.; Harris, K.M. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: Report from a National Heart, Lung, and Blood Institute Working Group. J. Am. Heart Assoc. 2020, 9, e016115. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef] [PubMed]
- Sominsky, L.; Spencer, S.J. Eating behavior and stress: A pathway to obesity. Front. Psychol. 2014, 5, 434. [Google Scholar] [CrossRef]
- Finch, L.E.; Tiongco-Hofschneider, L.; Tomiyama, A.J. Stress-induced eating dampens physiological and behavioral stress responses. In Nutrition in the Prevention and Treatment of Abdominal Obesity; Elsevier: Amsterdam, The Netherlands, 2019; pp. 175–187. [Google Scholar]
- Reichenberger, J.; Kuppens, P.; Liedlgruber, M.; Wilhelm, F.H.; Tiefengrabner, M.; Ginzinger, S.; Blechert, J. No haste, more taste: An EMA study of the effects of stress, negative and positive emotions on eating behavior. Biol. Psychol. 2018, 131, 54–62. [Google Scholar] [CrossRef]
- Lemos, T.C.; Coutinho, G.; Silva, L.A.; Stariolo, J.B.; Campagnoli, R.R.; Oliveira, L.; Pereira, M.G.; Mota, B.E.; Souza, G.G.; Canella, D.S. Ultra-Processed Foods Elicit Higher Approach Motivation Than Unprocessed and Minimally Processed Foods. Front. Public Health 2022, 10, 891546. [Google Scholar] [CrossRef]
- Campbell, N.; Browne, S.; Claudy, M.; Reilly, K.; Finucane, F.M. Ultra-Processed Food: The Tragedy of the Biological Commons. Int. J. Health Policy Manag. 2023, 12, 7557. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S.; Lancet, N.C.D.A.G. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- Vilaro, M.J.; Staub, D.; Xu, C.; Mathews, A.E. Theory-Based Interventions for Long-Term Adherence to Improvements in Diet Quality: An In-depth Review. Am. J. Lifestyle Med. 2016, 10, 369–376. [Google Scholar] [CrossRef]
- Rosenbaum, D.L.; White, K.S. The relation of anxiety, depression, and stress to binge eating behavior. J. Health Psychol. 2015, 20, 887–898. [Google Scholar] [CrossRef]
- Woods, N.F.; Rillamas-Sun, E.; Cochrane, B.B.; La Croix, A.Z.; Seeman, T.E.; Tindle, H.A.; Zaslavsky, O.; Bird, C.E.; Johnson, K.C.; Manson, J.E.; et al. Aging Well: Observations From the Women’s Health Initiative Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71 (Suppl. S1), S3–S12. [Google Scholar] [CrossRef] [PubMed]
- Krok-Schoen, J.L.; Naughton, M.J.; Felix, A.S.; Wiley Cené, C.; Springfield, S.; Yu, M.; McLaughlin, E.M.; Shadyab, A.H.; Nolan, T.S.; Kroenke, C.H. Resiliency among Women’s Health Initiative women aged 80 and older by race, ethnicity, and neighborhood socioeconomic status. J. Gerontol. Ser. B 2023, 78, 1445–1458. [Google Scholar] [CrossRef]
- Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Resilience and CVD-protective Health Behaviors in Older Women: Examining Racial and Ethnic Differences in a Cross-Sectional Analysis of the Women’s Health Initiative. Nutrients 2020, 12, 2107. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Pounis, G.; Persichillo, M.; Cerletti, C.; Donati, M.; De Gaetano, G.; Iacoviello, L. Mediterranean-type diet is associated with higher psychological resilience in a general adult population: Findings from the Moli-sani study. Eur. J. Clin. Nutr. 2018, 72, 154–160. [Google Scholar] [CrossRef]
- Robert, M.; Shankland, R.; Bellicha, A.; Kesse-Guyot, E.; Deschasaux-Tanguy, M.; Andreeva, V.A.; Srour, B.; Hercberg, S.; Touvier, M.; Leys, C. Associations between resilience and food intake are mediated by emotional eating in the NutriNet-Santé study. J. Nutr. 2022, 152, 1907–1915. [Google Scholar] [CrossRef]
- Voss, M.L.; Currie, C.L. Sleep Quality and the Importance Women Place on Healthy Eating Interact to Influence Psychological Resilience. Am. J. Health Behav. 2022, 46, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Whatnall, M.C.; Patterson, A.J.; Siew, Y.Y.; Kay-Lambkin, F.; Hutchesson, M.J. Are psychological distress and resilience associated with dietary intake among Australian university students? Int. J. Environ. Res. Public Health 2019, 16, 4099. [Google Scholar] [CrossRef] [PubMed]
- Sinska, B.; Jaworski, M.; Panczyk, M.; Traczyk, I.; Kucharska, A. The Role of Resilience and Basic Hope in the Adherence to Dietary Recommendations in the Polish Population during the COVID-19 Pandemic. Nutrients 2021, 13, 2108. [Google Scholar] [CrossRef] [PubMed]
- Lutz, L.J.; Gaffney-Stomberg, E.; Williams, K.W.; McGraw, S.M.; Niro, P.J.; Karl, J.P.; Cable, S.J.; Cropper, T.L.; McClung, J.P. Adherence to the dietary guidelines for Americans is associated with psychological resilience in young adults: A cross-sectional study. J. Acad. Nutr. Diet. 2017, 117, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions. Int. J. Environ. Res. Public Health 2022, 19, 7089. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, U.M. The positive plasticity of adult development: Potential for the 21st century. Am. Psychol. 2020, 75, 540–553. [Google Scholar] [CrossRef]
- Greve, W.; Staudinger, U.M. Resilience in later adulthood and old age: Resources and potentials for successful aging. In Developmental Psychopathology: Volume Three: Risk, Disorder, and Adaptation; Wiley: Hoboken, NJ, USA, 2015; pp. 796–840. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef] [PubMed]
- Leppin, A.L.; Gionfriddo, M.R.; Sood, A.; Montori, V.M.; Erwin, P.J.; Zeballos-Palacios, C.; Bora, P.R.; Dulohery, M.M.; Brito, J.P.; Boehmer, K.R.; et al. The efficacy of resilience training programs: A systematic review protocol. Syst. Rev. 2014, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, M.A.; Brown, S.A.; Dubois, S.K.; Harrison, L., Jr.; Lehrer, H.M.; Jaggars, S.S. A resilience intervention in African-American adults with type 2 diabetes. Am. J. Health Behav. 2015, 39, 507–518. [Google Scholar] [CrossRef]
- Steinhardt, M.A.; Mamerow, M.M.; Brown, S.A.; Jolly, C.A. A resilience intervention in African American adults with type 2 diabetes: A pilot study of efficacy. Diabetes Educ. 2009, 35, 274–284. [Google Scholar] [CrossRef]
- Heaney, C.A.; Avery, E.C.; Rich, T.; Ahuja, N.J.; Winter, S.J. Stanford WELL for life: Learning what it means to be well. Am. J. Health Promot. 2017, 31, 449–450. [Google Scholar]
- Chrisinger, B.W.; Gustafson, J.A.; King, A.C.; Winter, S.J. Understanding Where We Are Well: Neighborhood-Level Social and Environmental Correlates of Well-Being in the Stanford Well for Life Study. Int. J. Environ. Res. Public Health 2019, 16, 1786. [Google Scholar] [CrossRef] [PubMed]
- Rich, T.; Chrisinger, B.W.; Kaimal, R.; Winter, S.J.; Hedlin, H.; Min, Y.; Zhao, X.; Zhu, S.; You, S.-L.; Sun, C.-A. Contemplative practices behavior is positively associated with well-being in three global Multi-Regional Stanford WELL for Life Cohorts. Int. J. Environ. Res. Public Health 2022, 19, 13485. [Google Scholar] [CrossRef] [PubMed]
- Springfield, S.; Cunanan, K.; Heaney, C.; Peng, K.; Gardner, C. The WELL diet score correlates with the alternative healthy eating index-2010. Food Sci. Nutr. 2020, 8, 2710–2718. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Mealy, R.; Saldanha, I.J.; Loucks, E.B.; Needham, B.L.; Sims, M.; Fava, J.L.; Dulin, A.J.; Howe, C.J. Multilevel resilience resources and cardiovascular disease in the United States: A systematic review and meta-analysis. Health Psychol. 2022, 41, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Love, M.F.; Wood, G.L.; Wardell, D.W.; Beauchamp, J.E.S. Resilience and associated psychological, social/cultural, behavioural, and biological factors in patients with cardiovascular disease: A systematic review. Eur. J. Cardiovasc. Nurs. 2021, 20, 604–617. [Google Scholar] [CrossRef]
- Wood, D.; Crapnell, T.; Lau, L.; Bennett, A.; Lotstein, D.; Ferris, M.; Kuo, A. Emerging adulthood as a critical stage in the life course. In Handbook of Life Course Health Development; Springer: Berlin/Heidelberg, Germany, 2018; pp. 123–143. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Wethington, E.; Glanz, K.; Schwartz, M.D. Stress, coping, and health behavior. Health Behav. Theory Res. Pract. 2015, 223, 242. [Google Scholar] [CrossRef]
- Rand, K.; Vallis, M.; Aston, M.; Price, S.; Piccinini-Vallis, H.; Rehman, L.; Kirk, S.F. “It is not the diet; it is the mental part we need help with.” A multilevel analysis of psychological, emotional, and social well-being in obesity. Int. J. Qual. Stud. Health Well-Being 2017, 12, 1306421. [Google Scholar] [CrossRef]
- Berding, K.; Vlckova, K.; Marx, W.; Schellekens, H.; Stanton, C.; Clarke, G.; Jacka, F.; Dinan, T.G.; Cryan, J.F. Diet and the Microbiota-Gut-Brain Axis: Sowing the Seeds of Good Mental Health. Adv. Nutr. 2021, 12, 1239–1285. [Google Scholar] [CrossRef]
- Barber, T.M.; Valsamakis, G.; Mastorakos, G.; Hanson, P.; Kyrou, I.; Randeva, H.S.; Weickert, M.O. Dietary Influences on the Microbiota-Gut-Brain Axis. Int. J. Mol. Sci. 2021, 22, 3502. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, G.; Ferri, A.; Clarke, G.; Cryan, J.F. Diet and the microbiota–gut–brain-axis: A primer for clinical nutrition. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, A.; Feig, E.H.; Harnedy, L.E.; Huffman, J.C.; Park, E.R.; Thorndike, A.N.; Kim, S.; Millstein, R.A. The role of positive psychological constructs in diet and eating behavior among people with metabolic syndrome: A qualitative study. Health Psychol. Open 2022, 9, 20551029211055264. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Ruhm, C.J.; Puac-Polanco, V.; Hwang, I.H.; Lee, S.; Petukhova, M.V.; Sampson, N.A.; Ziobrowski, H.N.; Zaslavsky, A.M.; Zubizarreta, J.R. Estimated prevalence of and factors associated with clinically significant anxiety and depression among US adults during the first year of the COVID-19 pandemic. JAMA Netw. Open 2022, 5, e2217223. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, R.D.; Dierker, L.C.; Wu, M.; Galea, S.; Hoven, C.W.; Weinberger, A.H. Trends in US depression prevalence from 2015 to 2020: The widening treatment gap. Am. J. Prev. Med. 2022, 63, 726–733. [Google Scholar] [CrossRef] [PubMed]
- SAMHSA. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health; HHS Publication No. PEP21-07-01-003, NSDUH Series H-56; SAMHSA: Rockville, MD, USA, 2021. [Google Scholar]
- Yap, M.C.; Wu, F.; Huang, X.; Tang, L.; Su, K.; Tong, X.; Kwok, S.C.; Wu, C.; Wang, S.; He, Z. Association between individual resilience and depression or anxiety among general adult population during COVID-19: A systematic review. J. Public Health 2023, 45, fdad144. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Sznajder, K.; Cheng, D.; Wang, S.; Cui, C.; Yang, X. Coping styles for mediating the effect of resilience on depression among medical students in web-based classes during the COVID-19 pandemic: Cross-sectional questionnaire study. J. Med. Internet Res. 2021, 23, e25259. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Zhao, Y.Y.; Wang, J.; Sun, Y.H. Academic burnout and depression of Chinese medical students in the pre-clinical years: The buffering hypothesis of resilience and social support. Psychol. Health Med. 2020, 25, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.; Dong, X.; Zhao, J. Effects of Envy on Depression: The Mediating Roles of Psychological Resilience and Social Support. Psychiatry Investig. 2020, 17, 547–555. [Google Scholar] [CrossRef]
- Höltge, J.; Theron, L.; Ungar, M. A multisystemic perspective on the temporal interplay between adolescent depression and resilience-supporting individual and social resources. J. Affect. Disord. 2022, 297, 225–232. [Google Scholar] [CrossRef]
- de Vera García, M.; Gambarte, M. Resilience as a protective factor of chronic stress in teachers. Eur. J. Investig. Health Psychol. Educ. 2019, 9, 159–175. [Google Scholar] [CrossRef]
- Lee, J.-K.; Choi, H.-G.; Kim, J.-Y.; Nam, J.; Kang, H.-T.; Koh, S.-B.; Oh, S.-S. Self-resilience as a protective factor against development of post-traumatic stress disorder symptoms in police officers. Ann. Occup. Environ. Med. 2016, 28, 58. [Google Scholar] [CrossRef]
- Lehrer, H.M.; Steinhardt, M.A.; Dubois, S.K.; Laudenslager, M.L. Perceived stress, psychological resilience, hair cortisol concentration, and metabolic syndrome severity: A moderated mediation model. Psychoneuroendocrinology 2020, 113, 104510. [Google Scholar] [CrossRef]
- Sharpley, C.F.; Christie, D.R.; Bitsika, V.; Andronicos, N.M.; Agnew, L.L.; McMillan, M.E. Does psychological resilience buffer against the link between the 5-HTTLPR polymorphism and depression following stress. Physiol. Behav. 2017, 180, 53–59. [Google Scholar] [CrossRef]
- Breslow, A.S.; Brewster, M.E.; Velez, B.L.; Wong, S.; Geiger, E.; Soderstrom, B. Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 253. [Google Scholar] [CrossRef]
- Perna, L.; Mielck, A.; Lacruz, M.E.; Emeny, R.T.; Holle, R.; Breitfelder, A.; Ladwig, K.H. Socioeconomic position, resilience, and health behaviour among elderly people. Int. J. Public Health 2012, 57, 341–349. [Google Scholar] [CrossRef]
- Lucero, J.E.; Emerson, A.D.; Bowser, T.; Koch, B. Mental health risk among members of the millennial population cohort: A concern for public health. Am. J. Health Promot. 2021, 35, 266–270. [Google Scholar] [CrossRef]
- Bankole, E.; Harris, N.; Rutherford, S.; Wiseman, N. A systematic review of the adolescent-directed marketing strategies of transnational fast food companies in low-and middle-income countries. Obes. Sci. Pract. 2023, 9, 670–680. [Google Scholar] [CrossRef]
- Truman, E.; Elliott, C. Identifying food marketing to teenagers: A scoping review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 67. [Google Scholar] [CrossRef]
- Ares, G.; Antúnez, L.; Alcaire, F.; Natero, V.; Otterbring, T. Is this advertisement designed to appeal to you? Adolescents’ views about Instagram advertisements promoting ultra-processed products. Public Health Nutr. 2024, 27, e96. [Google Scholar] [CrossRef]
- Mialon, M. An overview of the commercial determinants of health. Glob. Health 2020, 16, 74. [Google Scholar] [CrossRef]
- Szakos, D.; Ózsvári, L.; Kasza, G. Perception of older adults about health-related functionality of foods compared with other age groups. Sustainability 2020, 12, 2748. [Google Scholar] [CrossRef]
- Ye, Y.-C.; Wu, C.-H.; Huang, T.-Y.; Yang, C.-T. The difference between the Connor–Davidson Resilience Scale and the Brief Resilience Scale when assessing resilience: Confirmatory factor analysis and predictive effects. Glob. Ment. Health 2022, 9, 339–346. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Smith, B.W.; deCruz-Dixon, N.; Schodt, K.; Torres, F. Brief resilience scale (BRS). In Handbook of Assessment in Mindfulness Research; Springer: Berlin/Heidelberg, Germany, 2023; pp. 1–19. [Google Scholar]
- Onvani, S.; Haghighatdoost, F.; Surkan, P.; Larijani, B.; Azadbakht, L. Adherence to the Healthy Eating Index and Alternative Healthy Eating Index dietary patterns and mortality from all causes, cardiovascular disease and cancer: A meta-analysis of observational studies. J. Hum. Nutr. Diet. 2017, 30, 216–226. [Google Scholar] [CrossRef]
- Hu, E.A.; Steffen, L.M.; Coresh, J.; Appel, L.J.; Rebholz, C.M. Adherence to the Healthy Eating Index-2015 and Other Dietary Patterns May Reduce Risk of Cardiovascular Disease, Cardiovascular Mortality, and All-Cause Mortality. J. Nutr. 2020, 150, 312–321. [Google Scholar] [CrossRef]
- Bureau, U.C. 2020 Census Illuminates Racial and Ethnic Composition of the Country; US Government Printing Office: Washington, DC, USA, 2020. [Google Scholar]
- McElrath, K.; Martin, M. Bachelor’s Degree Attainment in the United States: 2005 to 2019; American Community Survey Briefs, ACSBR-009; US Census Bureau: Suitland, MD, USA, 2021. [Google Scholar]
- Handy, A.; Mangal, R.; Stead, T.S.; Coffee, R.L., Jr.; Ganti, L. Prevalence and Impact of Diagnosed and Undiagnosed Depression in the United States. Cureus 2022, 14, e28011. [Google Scholar] [CrossRef]
- Johnson, A.J.; McCloyn, K.; Sims, M. Discrimination, High-Effort Coping, and Cardiovascular Risk Profiles in the Jackson Heart Study: A Latent Profile Analysis. J. Racial Ethn. Health Disparities 2022, 9, 1464–1473. [Google Scholar] [CrossRef]
- Islam, S.J.; Kim, J.H.; Topel, M.; Liu, C.; Ko, Y.A.; Mujahid, M.S.; Sims, M.; Mubasher, M.; Ejaz, K.; Morgan-Billingslea, J. Cardiovascular risk and resilience among Black adults: Rationale and design of the MECA Study. J. Am. Heart Assoc. 2020, 9, e015247. [Google Scholar] [CrossRef]
- McKay, S.; Skues, J.L.; Williams, B.J. Does the Brief Resilience Scale actually measure resilience and succumbing? Comparing artefactual and substantive models. Adv. Ment. Health 2021, 19, 192–201. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernàndez, G.; Fiebach, C.J.; Galatzer-Levy, I. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef] [PubMed]
| Participant Characteristics | All Ages | Early Young | Late Young | Middle | Late | |
|---|---|---|---|---|---|---|
| (18–50+) N = 6171 | (18–24) N = 1585 | (25–34) N = 1485 | (35–49) N = 1470 | 50+ N = 1631 | ||
| Main outcome and primary exposure | WELL Diet Score, mean (SD) Range 0–120; higher score indicates higher diet quality | 70.2 (19.3) | 58.7 (18.0) | 68.3 (17.8) | 73.5 (17.6) | 80.2 (17.2) |
| Resilience, mean (SD) Range 0–10; higher score indicates more resilience | 6.7 (1.7) | 6.4 (1.7) | 6.7 (1.8) | 6.8 (1.7) | 7 (1.7) | |
| Sociodemographic | Age, mean (SD) | 38.8 (16.8) | 20.7 (2.1) | 29.3 (2.8) | 41.8 (4.7) | 62.4 (8.4) |
| Gender, n (%) (n = 6148) | ||||||
| Male | 1668 (27.1) | 554 (35.1) | 365 (24.6) | 311 (21.2) | 438 (27) | |
| Female | 4407 (71.7) | 999 (63.2) | 1094 (73.9) | 1137 (77.7) | 1177 (72.5) | |
| Transgender and genderqueer | 73 (1.2) | 27 (1.7) | 22 (1.5) | 16 (1.1) | 8 (0.5) | |
| Race/ethnicity, n (%) (n = 6120) | ||||||
| White/Caucasian | 3727 (60.9) | 939 (59.5) | 792 (53.6) | 814 (55.8) | 1182 (73.6) | |
| Hispanic | 664 (10.8) | 203 (12.9) | 211 (14.3) | 167 (11.4) | 83 (5.2) | |
| Black/African American | 268 (4.4) | 103 (6.5) | 49 (3.3) | 60 (4.1) | 56 (3.5) | |
| Asian | 1523 (24.9) | 369 (23.4) | 449 (30.4) | 424 (29.0) | 281 (17.5) | |
| Other | 165 (2.7) | 52 (3.3) | 45 (3.0) | 39 (2.7) | 29 (1.8) | |
| Marital status, n (%) (n = 6146) | ||||||
| Married | 2558 (41.6) | 60 (3.8) | 496 (33.6) | 954 (65.2) | 1048 (64.6) | |
| Living with partner | 564 (9.2) | 122 (7.7) | 263 (17.8) | 106 (7.2) | 73 (4.5) | |
| Single | 2487 (40.5) | 1388 (87.7) | 677 (45.8) | 254 (17.4) | 168 (10.4) | |
| Other | 537 (8.7) | 13 (0.8) | 42 (2.8) | 149 (10.2) | 333 (20.5) | |
| Education, n (%) (n = 6135) | ||||||
| HS or below | 759 (12.4) | 595 (37.6) | 72 (4.9) | 40 (2.7) | 52 (3.2) | |
| Some college | 1139 (18.6) | 527 (33.3) | 178 (12.0) | 200 (13.7) | 234 (14.5) | |
| College graduate | 2030 (33.1) | 381 (24.1) | 654 (44.2) | 459 (31.5) | 536 (33.2) | |
| Graduate | 2207 (36) | 79 (5) | 576 (38.9) | 758 (52) | 794 (49.1) | |
| Perceived stress | Stress, mean (SD) (n = 6160) Range 0–10; higher score indicates greater stress | 5.9 (1.7) | 5.5 (1.7) | 5.8 (1.6) | 5.9 (1.7) | 6.5 (1.7) |
| Lifestyle and BMI | Physical activity, mean (SD) (n = 6085) Range 0–10; higher score indicates more physical activity | 5 (2.9) | 4.8 (3.1) | 5.1 (2.9) | 4.9 (2.9) | 5.3 (2.7) |
| Smoking status, n (%) (n = 6151) | ||||||
| Never | 5100 (82.9) | 1445 (91.3) | 1303 (88.0) | 1169 (79.7) | 1183 (72.9) | |
| Former | 830 (13.5) | 69 (4.4) | 118 (8.0) | 237 (16.2) | 406 (25.0) | |
| Current | 221 (3.6) | 68 (4.3) | 60 (4.1) | 60 (4.1) | 33 (2.0) | |
| BMI, mean (SD) (n = 6008) | 25.2 (5.7) | 24.1 (5.1) | 24.9 (6.4) | 25.8 (5.8) | 25.9 (5.5) | |
| Self-reported history of hypertension, n (%) (n = 6025) | 784 (13.0) | 65 (4.3) | 87 (6.0) | 148 (10.2) | 484 (30.0) | |
| Mental health | Positive affect, mean (SD) (n = 6159) Range 0–10; higher score indicates more positive emotions | 6.8 (1.7) | 6.6 (1.7) | 6.7 (1.6) | 6.8 (1.7) | 7.0 (1.7) |
| Self-reported history of depression, n (%) (n = 5948) | 1447 (24.3) | 362 (24.5) | 340 (23.8) | 342 (23.6) | 403 (25.3) | |
| Negative affect, mean (SD) (n = 6160) Range 0–10; higher score indicates fewer negative emotions (reversed-scored) | 5.1 (1.8) | 4.6 (1.8) | 5.0 (1.7) | 5.2 (1.8) | 5.7 (1.7) | |
| Overall WELL Score (well-being), mean (SD) (n = 5918) Range 0–100; greater score indicates better overall well-being | 66.2 (12.6) | 62.6 (12.5) | 65.2 (12.1) | 66.8 (12.0) | 70.2 (12.4) | |
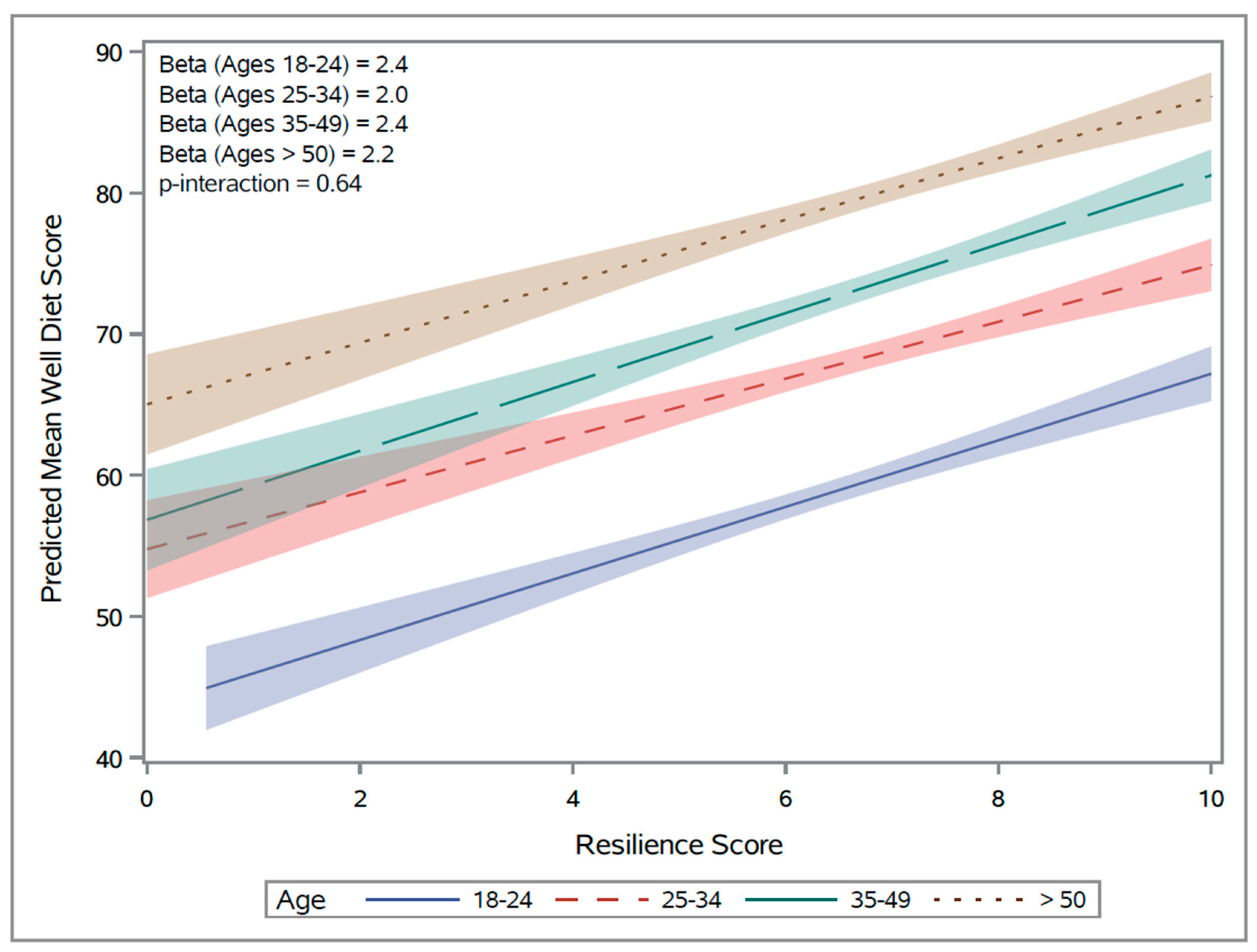
| Age-Adjusted | Early Young Ages 18–24 | Late Young Ages 25–34 | Middle Ages 35–49 | Late Ages ≥ 50 | p-Value for Interaction | |
|---|---|---|---|---|---|---|
| Crude | 2.3 ± 0.1 ** | 2.4 ± 0.3 ** | 2.0 ± 0.3 ** | 2.4 ± 0.3 ** | 2.2 ± 0.2 ** | 0.64 |
| Model 1 | 2.1 ± 0.1 ** | 2.0 ± 0.2 ** | 1.9 ± 0.3 ** | 2.2 ± 0.3 ** | 1.9 ± 0.2 ** | 0.65 |
| Model 2 | 1.5 ± 0.1 ** | 1.5 ± 0.3 ** | 1.1 ± 0.3 ** | 1.4 ± 0.3 ** | 1.5 ± 0.3 ** | 0.60 |
| Model 3 | 1.3 ± 0.1 ** | 1.2 ± 0.3 ** | 1.3 ± 0.3 ** | 1.1 ± 0.3 ** | 1.3 ± 0.3 ** | 0.26 |
| Model 4 | 1.2 ± 0.2 ** | 1.1 ± 0.3 ** | 1.2 ± 0.3 ** | 0.9 ± 0.3 * | 1.0 ± 0.3 * | 0.34 |
| Beta ± Standard Error | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Springfield-Trice, S.; Joyce, C.; Wu, Y.-H.; Hsing, A.W.; Cunanan, K.; Gardner, C. Diet Quality and Resilience through Adulthood: A Cross-Sectional Analysis of the WELL for Life Study. Nutrients 2024, 16, 1724. https://doi.org/10.3390/nu16111724
Springfield-Trice S, Joyce C, Wu Y-H, Hsing AW, Cunanan K, Gardner C. Diet Quality and Resilience through Adulthood: A Cross-Sectional Analysis of the WELL for Life Study. Nutrients. 2024; 16(11):1724. https://doi.org/10.3390/nu16111724
Chicago/Turabian StyleSpringfield-Trice, Sparkle, Cara Joyce, Yi-Hsuan Wu, Ann W. Hsing, Kristen Cunanan, and Christopher Gardner. 2024. "Diet Quality and Resilience through Adulthood: A Cross-Sectional Analysis of the WELL for Life Study" Nutrients 16, no. 11: 1724. https://doi.org/10.3390/nu16111724
APA StyleSpringfield-Trice, S., Joyce, C., Wu, Y.-H., Hsing, A. W., Cunanan, K., & Gardner, C. (2024). Diet Quality and Resilience through Adulthood: A Cross-Sectional Analysis of the WELL for Life Study. Nutrients, 16(11), 1724. https://doi.org/10.3390/nu16111724







