Modelling Food Substitution Using the Ofcom Nutrient Profiling Model on Population Intakes from the Canadian Community Health Survey–Nutrition 2015
Abstract
:1. Introduction
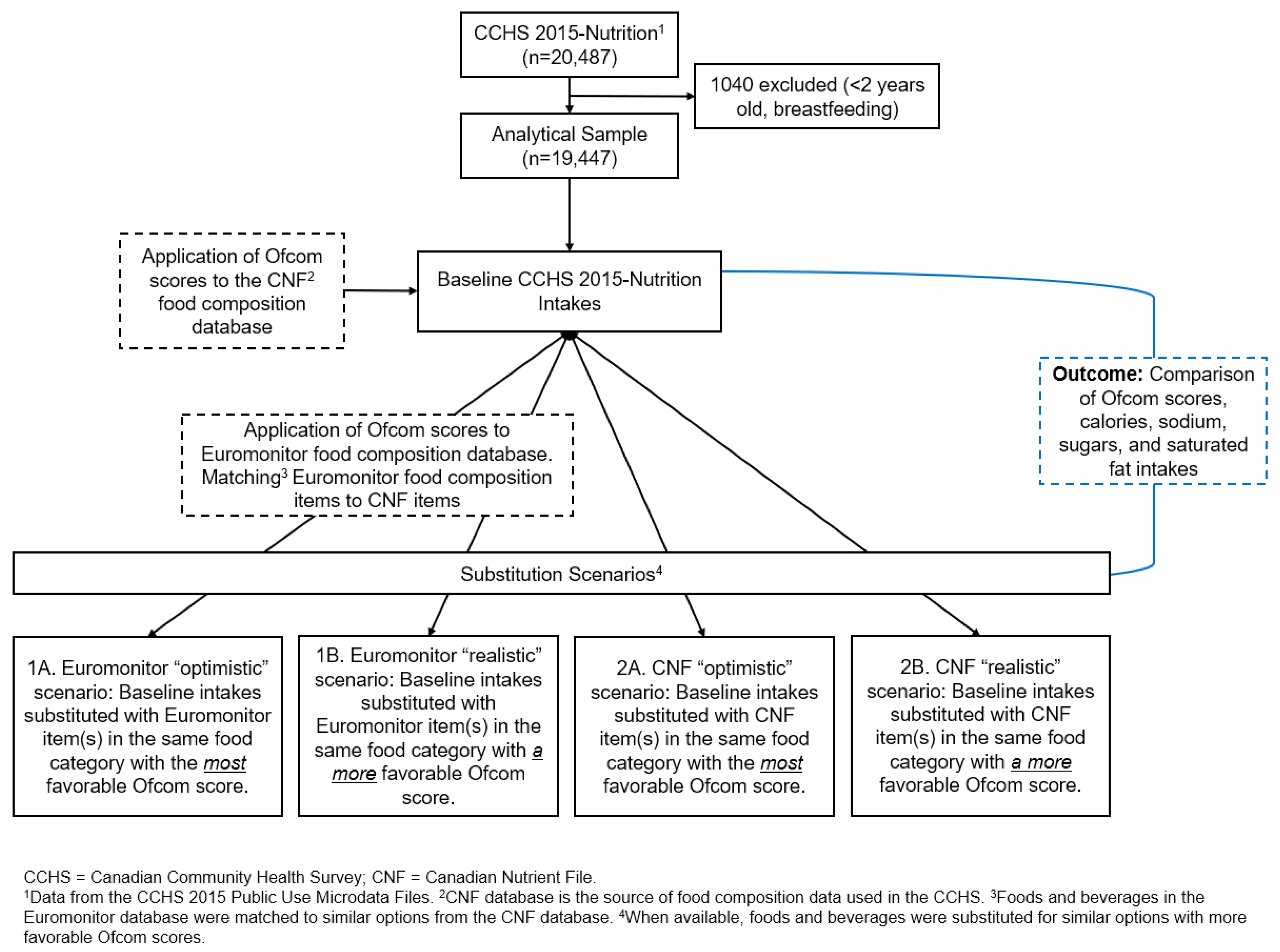
2. Materials and Methods
2.1. Databases Used
2.2. Calculation of Ofcom Scores
2.3. Substitution Scenarios
2.4. Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Diet Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Health Fact Sheet: Overweight and Obese Adults. 2018. Available online: https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00005-eng.htm (accessed on 22 April 2022).
- Public Health Agency of Canada. Prevalence of Chronic Diseases among Canadian Adults. Available online: https://www.canada.ca/en/public-health/services/chronic-diseases/prevalence-canadian-adults-infographic-2019.html (accessed on 22 April 2022).
- Public Health Agency of Canada. Heart Disease in Canada: Highlights from the Canadian Chronic Disease Surveillance System. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/heart-disease-canada-fact-sheet.html (accessed on 22 April 2022).
- WHO/FAO Expert Consultation. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; World Health Organization: Geneva, Switzerland, 2003; pp. 1–149. [Google Scholar]
- Jessri, M.; Hennessey, D.; Eddeen, A.B.; Bennett, C.; Zhang, Z.; Yang, Q.; Sanmartin, C.; Manuel, D. Sodium, added sugar and saturated fat intake in relation to mortality and CVD events in adults: Canadian National Nutrition Survey linked with vital statistics and health administrative databases. Br. J. Nutr. 2023, 129, 1740–1750. [Google Scholar] [CrossRef] [PubMed]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; 9241549025; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Kris-Etherton, P.M.; Petersen, K.; Van Horn, L. Convincing evidence supports reducing saturated fat to decrease cardiovascular disease risk. BMJ Nutr. Prev. Health 2018, 1, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Martin, N.; Jimoh, O.F.; Kirk, C.; Foster, E.; Abdelhamid, A.S. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst. Rev. 2020, 5, CD011737. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.; Brassard, D.; Lemieux, S.; Lamarche, B. Consumption and sources of saturated fatty acids according to the 2019 Canada Food Guide: Data from the 2015 Canadian Community Health Survey. Nutrients 2019, 11, 1964. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Sodium Intakes of Canadians in 2017; Health Canada: Ottawa, ON, Canada, 2018.
- Liu, S.; Munasinghe, L.L.; Ohinmaa, A.; Veugelers, P.J. Added, free and total sugar content and consumption of foods and beverages in Canada. Health Rep. 2020, 31, 14–24. [Google Scholar]
- Hack, S.; Jessri, M.; L’Abbé, M.R. Evaluating Diet Quality of Canadian Adults Using Health Canada’s Surveillance Tool Tier System: Findings from the 2015 Canadian Community Health Survey-Nutrition. Nutrients 2020, 12, 1113. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Nishi, S.K.; L’Abbe, M.R. Assessing the nutritional quality of diets of Canadian children and adolescents using the 2014 Health Canada Surveillance Tool Tier System. BMC Public Health 2016, 16, 381. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Nishi, S.K.; L’Abbé, M.R. Assessing the Nutritional Quality of Diets of Canadian Adults Using the 2014 Health Canada Surveillance Tool Tier System. Nutrients 2015, 7, 10447–10468, Correction in Nutrients 2017, 9, 58. [Google Scholar] [CrossRef] [PubMed]
- Hack, S.; Jessri, M.; L’Abbé, M.R. Nutritional quality of the food choices of Canadian children. BMC Nutr. 2021, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Healthy Eating Strategy. Available online: https://www.canada.ca/en/health-canada/services/publications/food-nutrition/healthy-eating-strategy.html (accessed on 3 May 2022).
- Government of Canada. Canada’s Food Guide. Available online: https://food-guide.canada.ca/en/ (accessed on 26 April 2022).
- Government of Canada. Regulations Amending the Food and Drug Regulations (Nutrition Labelling, Other Labelling Provisions and Food Colours): Canada Gazette, Part II; Government of Canada: Ottawa, ON, Canada, 2016.
- Government of Canada. Voluntary Sodium Reduction Targets for Processed Foods 2020–2025; Government of Canada: Ottawa, ON, Canada, 2020.
- Government of Canada. Regulations Amending the Food and Drug Regulations (Nutrition Symbols, Other Labelling Provisions, Vitamin D and Hydrogenated Fats or Oils): SOR/2022-168; Government of Canada: Ottawa, ON, Canada, 2022.
- Government of Canada. Policy Update on Restricting Food Advertising Primarily Directed at Children: Overview. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating-strategy/policy-update-restricting-food-advertising-primarily-directed-children.html (accessed on 9 April 2024).
- Labonte, M.E.; Poon, T.; Gladanac, B.; Ahmed, M.; Franco-Arellano, B.; Rayner, M.; L’Abbe, M.R. Nutrient Profile Models with Applications in Government-Led Nutrition Policies Aimed at Health Promotion and Noncommunicable Disease Prevention: A Systematic Review. Adv. Nutr. 2018, 9, 741–788. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, U.; Charles, V.R.; Vlassopoulos, A.; Masset, G.; Spieldenner, J. Nutrient profiling for product reformulation: Public health impact and benefits for the consumer. Proc. Nutr. Soc. 2017, 76, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.; Rito, A.I.; Matias, F.N.; Assunção, R.; Castanheira, I.; Loureiro, I. Nutrient profile models a useful tool to facilitate healthier food choices: A comprehensive review. Trends Food Sci. Technol. 2021, 110, 120–131. [Google Scholar] [CrossRef]
- UK Department of Health. Nutrient Profiling Technical Guidance; UK Department of Health: London, UK, 2011.
- Julia, C.; Ducrot, P.; Lassale, C.; Fezeu, L.; Mejean, C.; Peneau, S.; Touvier, M.; Hercberg, S.; Kesse-Guyot, E. Prospective associations between a dietary index based on the British Food Standard Agency nutrient profiling system and 13-year weight gain in the SU. VI. MAX cohort. Prev. Med. 2015, 81, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Julia, C.; Fézeu, L.K.; Ducrot, P.; Méjean, C.; Péneau, S.; Touvier, M.; Hercberg, S.; Kesse-Guyot, E. The nutrient profile of foods consumed using the British Food Standards Agency nutrient profiling system is associated with metabolic syndrome in the SU. VI. MAX cohort. J. Nutr. 2015, 145, 2355–2361. [Google Scholar] [CrossRef] [PubMed]
- Adriouch, S.; Julia, C.; Kesse-Guyot, E.; Méjean, C.; Ducrot, P.; Péneau, S.; Donnenfeld, M.; Deschasaux, M.; Menai, M.; Hercberg, S. Prospective association between a dietary quality index based on a nutrient profiling system and cardiovascular disease risk. Eur. J. Prev. Cardiol. 2016, 23, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Donnenfeld, M.; Julia, C.; Kesse-Guyot, E.; Méjean, C.; Ducrot, P.; Péneau, S.; Deschasaux, M.; Latino-Martel, P.; Fezeu, L.; Hercberg, S. Prospective association between cancer risk and an individual dietary index based on the British Food Standards Agency Nutrient Profiling System. Br. J. Nutr. 2015, 114, 1702–1710. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Reference Guide to Understanding and Using the Data—2015 Canadian Community Health Survey—Nutrition. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/reference-guide-understanding-using-data-2015.html (accessed on 3 May 2022).
- Health Canada. Canadian Nutrient File (CNF). Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/nutrient-data/canadian-nutrient-file-2015-download-files.html (accessed on 3 May 2022).
- Euromonitor International. Food and Nutrition Industry Analysis & Market Research Reporting Posts. Available online: https://www.euromonitor.com/insights/food-and-nutrition (accessed on 25 June 2022).
- Gilbert, S.Z.; Morrison, C.L.; Chen, Q.J.; Punian, J.; Bernstein, J.T.; Jessri, M. Algorithm-based mapping of products in a branded Canadian food and beverage database to their equivalents in Health Canada’s Canadian Nutrient File. Front. Nutr. 2023, 9, 1013516. [Google Scholar] [CrossRef]
- Juraschek, S.P.; Miller, E.R.; Weaver, C.M.; Appel, L.J. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J. Am. Coll. Cardiol. 2017, 70, 2841–2848. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. NEJM 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Emrich, T.E.; Qi, Y.; Lou, W.Y.; L’Abbe, M.R. Traffic-light labels could reduce population intakes of calories, total fat, saturated fat, and sodium. PLoS ONE 2017, 12, e0171188. [Google Scholar] [CrossRef]
- Young, L.; Swinburn, B. Impact of the Pick the Tick food information programme on the salt content of food in New Zealand. Health Promot Int. 2002, 17, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Dhar, T.; Baylis, K. Fast-food consumption and the ban on advertising targeting children: The Quebec experience. J. Mark. Res. 2011, 48, 799–813. [Google Scholar] [CrossRef]
- Kaur, A.; Scarborough, P.; Rayner, M. Regulating health and nutrition claims in the UK using a nutrient profile model: An explorative modelled health impact assessment. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 18. [Google Scholar] [CrossRef] [PubMed]
- Roodenburg, A.J.; van Ballegooijen, A.J.; Dötsch-Klerk, M.; van der Voet, H.; Seidell, J.C. Modelling of usual nutrient intakes: Potential impact of the choices programme on nutrient intakes in young Dutch adults. PLoS ONE 2013, 8, e72378. [Google Scholar] [CrossRef] [PubMed]
- Balcombe, K.; Fraser, I.; Di Falco, S. Traffic lights and food choice: A choice experiment examining the relationship between nutritional food labels and price. Food Policy 2010, 35, 211–220. [Google Scholar] [CrossRef]
- Leger. Consumer Research on Front of Package Nutrition Labelling: Report; Leger: Montreal, QC, Canada, 2018. [Google Scholar]
- Feteira-Santos, R.; Fernandes, J.; Virgolino, A.; Alarcão, V.; Sena, C.; Vieira, C.P.; Gregório, M.J.; Nogueira, P.; Costa, A.; Graça, P. Effectiveness of interpretive front-of-pack nutritional labelling schemes on the promotion of healthier food choices: A systematic review. JBI Evid. Synth. 2020, 18, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Thomson, R.K.; McLean, R.M.; Ning, S.X.; Mainvil, L.A. Tick front-of-pack label has a positive nutritional impact on foods sold in New Zealand. Public Health Nutr. 2016, 19, 2949–2958. [Google Scholar] [CrossRef]
- Nilson, E.A.; Spaniol, A.M.; Gonçalves, V.S.; Moura, I.; Silva, S.A.; L’Abbé, M.; Jaime, P.C. Sodium reduction in processed foods in Brazil: Analysis of food categories and voluntary targets from 2011 to 2017. Nutrients 2017, 9, 742. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Eyles, H.; Choi, Y.-H. Effects of a voluntary front-of-pack nutrition labelling system on packaged food reformulation: The health star rating system in New Zealand. Nutrients 2017, 9, 918. [Google Scholar] [CrossRef] [PubMed]
- Shangguan, S.; Afshin, A.; Shulkin, M.; Ma, W.; Marsden, D.; Smith, J.; Saheb-Kashaf, M.; Shi, P.; Micha, R.; Imamura, F. A meta-analysis of food labeling effects on consumer diet behaviors and industry practices. Am. J. Prev. Med. 2019, 56, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Ogundijo, D.A.; Tas, A.A.; Onarinde, B.A. Factors influencing the perception and decision-making process of consumers on the choice of healthier foods in the United Kingdom: A systematic review using narrative synthesis. Int. J. Food Sci. 2022, 57, 881–897. [Google Scholar] [CrossRef]
- United States Department of Agriculture (USDA) Agricultural Research Service. APMN—USDA Automated Multiple-Pass Method. Available online: http://www.ars.usda.gov/Services/docs.htm?docid=7710 (accessed on 8 May 2023).
| Dietary Ofcom Score | Daily Calories, kcal | Daily Saturated Fat, g | Daily Sodium, mg | Daily Total Sugars, g | |
|---|---|---|---|---|---|
| Baseline data | 5.2 ± 0.1 [5.0, 5.5] | 1805.6 ± 12.5 [1781.1, 1830.1] | 22.8 ± 0.4 [22.1, 23.6] | 2710.5 ± 30.7 [2650.2, 2770.7] | 90.8 ± 0.9 [89.1, 92.5] |
| Euromonitor “Optimistic” Scenario 1A 1 | 4.9 ± 0.1 [4.7, 5.2] * | 1741.7 ± 11.7 [1718.7, 1764.8] * | 21.4 ± 0.4 [20.6, 22.2] * | 2542.0 ± 31.8 [2479.5, 2604.5] * | 82.6 ± 0.8 [81.1, 84.1] * |
| Euromonitor “Realistic” Scenario 1B 2 | 5.0 ± 0.1 [4.7, 5.2] * | 1747.0 ± 11.8 [1723.9, 1770.2] * | 21.5 ± 0.4 [20.7, 22.3] * | 2543.0 ± 32.2 [2479.8, 2606.3] * | 83.8 ± 0.7 [82.3, 85.2] * |
| CNF “Optimistic” Scenario 2A 3 | −0.9 ± 0.1 [−1.1, −0.8] * | 1703.8 ± 16.1 [1672.1, 1735.5] * | 12.8 ± 0.3 [12.2, 13.4] * | 909.3 ± 8.9 [891.8, 926.7] * | 58.1 ± 0.9 [56.4, 59.8] * |
| CNF “Realistic” Scenario 2B 4 | 3.7 ± 0.1 [3.5, 3.9] * | 2838.6 ± 33.7 [2772.4, 2904.9] * | 19.7 ± 0.5 [18.7, 20.6] * | 2330.7 ± 39.4 [2253.4, 2408.1] * | 85.9 ± 0.8 [84.4, 87.4] * |
| Dietary Ofcom Score | Daily Calories, kcal | Daily Saturated Fat, g | Daily Sodium, mg | Daily Total Sugars, g | |
|---|---|---|---|---|---|
| Baseline data | 10.4 ± 0.2 [10.0, 10.8] | 351.7 ± 5.8 [340.2, 363.1] | 4.9 ± 0.1 [4.7, 5.1] | 573.8 ± 8.9 [556.4, 591.2] | 18.1 ± 0.5 [17.0, 19.1] |
| Euromonitor “Optimistic” Scenario 1A 1 | 6.2 ± 0.2 [5.9, 6.6] * | 317.7 ± 6.5 [304.9, 330.5] * | 3.7 ± 0.1 [3.5, 4.0] * | 428.5 ± 6.8 [415.1, 441.8] * | 9.5 ± 0.4 [8.7, 10.4] * |
| Euromonitor “Realistic” Scenario 1B 2 | 6.8 ± 0.2 [6.3, 7.2] * | 323.7 ± 6.2 [311.5, 335.9] * | 3.8 ± 0.1 [3.6, 4.1] * | 429.6 ± 7.0 [416.0, 443.3] * | 10.9 ± 0.3 [10.2, 11.6] * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Q.; Gillis, M.; Bernstein, J.T.; Jacobs, A.; Morrison, C.L.; Jessri, M. Modelling Food Substitution Using the Ofcom Nutrient Profiling Model on Population Intakes from the Canadian Community Health Survey–Nutrition 2015. Nutrients 2024, 16, 1874. https://doi.org/10.3390/nu16121874
Chen Q, Gillis M, Bernstein JT, Jacobs A, Morrison CL, Jessri M. Modelling Food Substitution Using the Ofcom Nutrient Profiling Model on Population Intakes from the Canadian Community Health Survey–Nutrition 2015. Nutrients. 2024; 16(12):1874. https://doi.org/10.3390/nu16121874
Chicago/Turabian StyleChen, Qiuyu (Julia), Misa Gillis, Jodi T. Bernstein, Adelia Jacobs, Conor L. Morrison, and Mahsa Jessri. 2024. "Modelling Food Substitution Using the Ofcom Nutrient Profiling Model on Population Intakes from the Canadian Community Health Survey–Nutrition 2015" Nutrients 16, no. 12: 1874. https://doi.org/10.3390/nu16121874
APA StyleChen, Q., Gillis, M., Bernstein, J. T., Jacobs, A., Morrison, C. L., & Jessri, M. (2024). Modelling Food Substitution Using the Ofcom Nutrient Profiling Model on Population Intakes from the Canadian Community Health Survey–Nutrition 2015. Nutrients, 16(12), 1874. https://doi.org/10.3390/nu16121874





