Branched-Chain Amino Acids in Liver Diseases: Complexity and Controversy
Abstract
:1. Introduction
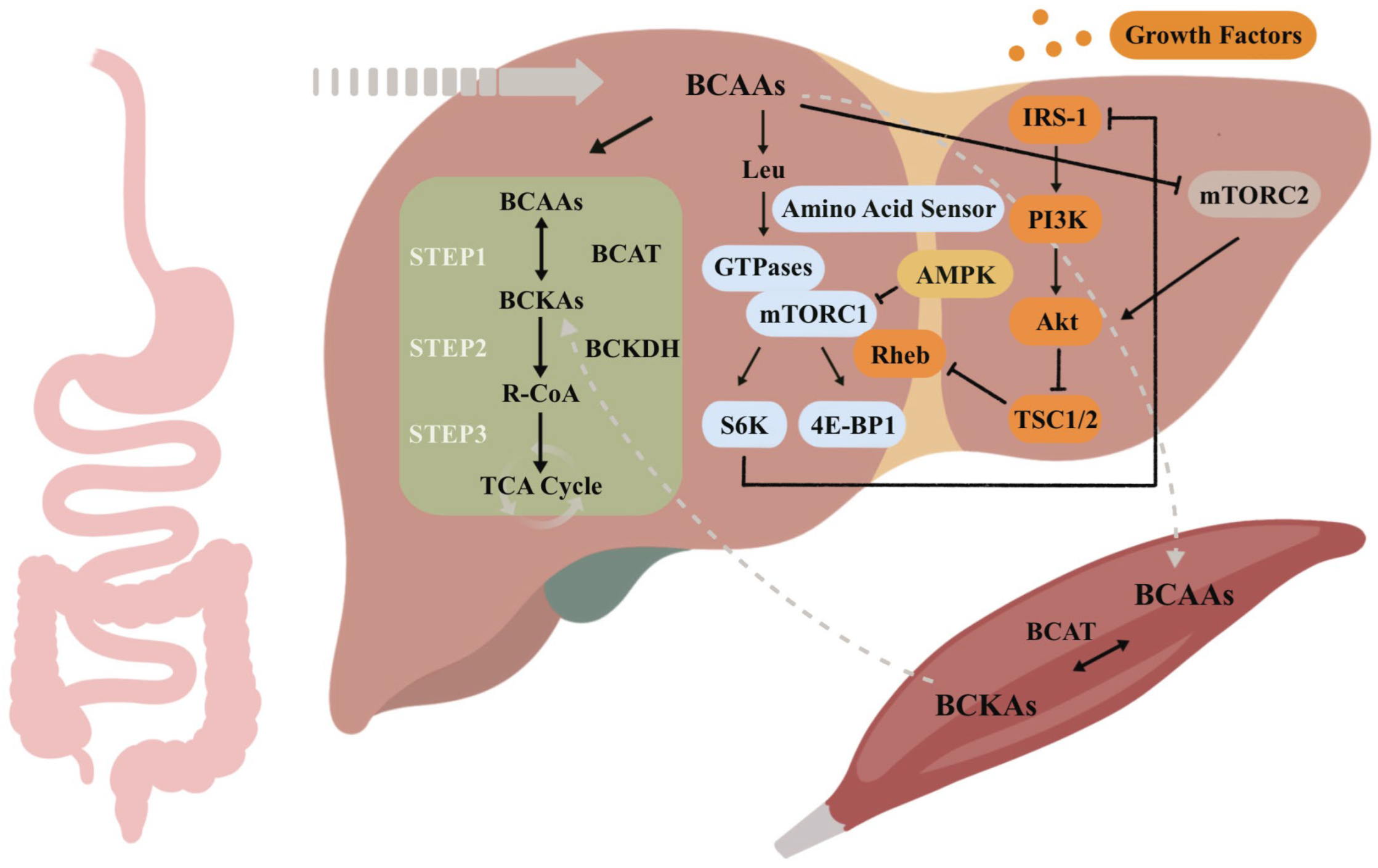
2. Metabolism and Signal Transduction in BCAAs in the Liver
3. Association of BCAAs with Liver Diseases
3.1. Non-Alcoholic Fatty Liver Disease
3.2. Hepatocellular Carcinoma
3.3. Cirrhosis
3.4. Hepatic Encephalopathy
3.5. Hepatitis C Virus Infection
3.6. Acute Liver Failure
4. Clinical Application of BCAAs in the Treatment of Liver Diseases
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wu, G. Amino Acids: Metabolism, Functions, and Nutrition. Amino Acids 2009, 37, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Neinast, M.; Murashige, D.; Arany, Z. Branched Chain Amino Acids. Annu. Rev. Physiol. 2019, 81, 139–164. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, R.L.; Chantranupong, L.; Saxton, R.A.; Shen, K.; Scaria, S.M.; Cantor, J.R.; Sabatini, D.M. Sestrin2 Is a Leucine Sensor for the mTORC1 Pathway. Science 2016, 351, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Neinast, M.D.; Jang, C.; Hui, S.; Murashige, D.S.; Chu, Q.; Morscher, R.J.; Li, X.; Zhan, L.; White, E.; Anthony, T.G.; et al. Quantitative Analysis of the Whole-Body Metabolic Fate of Branched-Chain Amino Acids. Cell Metab. 2019, 29, 417-429.e4. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.E.; Baldessarini, R.J. False Neurotransmitters and Hepatic Failure. Lancet 1971, 2, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Muto, Y.; Moriwaki, H.; Yamato, M. Effect of Long-Term Oral Supplementation with Branched-Chain Amino Acid Granules on the Prognosis of Liver Cirrhosis. Gastroenterol. Jpn. 1989, 24, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Soeters, P.B.; Fischer, J.E. Insulin, Glucagon, Aminoacid Imbalance, and Hepatic Encephalopathy. Lancet 1976, 2, 880–882. [Google Scholar] [CrossRef]
- Chashmniam, S.; Ghafourpour, M.; Farimani, A.R.; Gholami, A.; Ghoochani, B.F.N.M. Metabolomic Biomarkers in the Diagnosis of Non-Alcoholic Fatty Liver Disease. Hepat. Mon. 2019, 19, e92244. [Google Scholar] [CrossRef]
- Lischka, J.; Schanzer, A.; Hojreh, A.; Ba Ssalamah, A.; Item, C.B.; de Gier, C.; Walleczek, N.-K.; Metz, T.F.; Jakober, I.; Greber-Platzer, S.; et al. A Branched-Chain Amino Acid-Based Metabolic Score Can Predict Liver Fat in Children and Adolescents with Severe Obesity. Pediatr. Obes. 2021, 16, e12739. [Google Scholar] [CrossRef]
- Nezami Ranjbar, M.R.; Luo, Y.; Di Poto, C.; Varghese, R.S.; Ferrarini, A.; Zhang, C.; Sarhan, N.I.; Soliman, H.; Tadesse, M.G.; Ziada, D.H.; et al. GC-MS Based Plasma Metabolomics for Identification of Candidate Biomarkers for Hepatocellular Carcinoma in Egyptian Cohort. PLoS ONE 2015, 10, e0127299. [Google Scholar] [CrossRef] [PubMed]
- Park, J.G.; Tak, W.Y.; Park, S.Y.; Kweon, Y.O.; Chung, W.J.; Jang, B.K.; Bae, S.H.; Lee, H.J.; Jang, J.Y.; Suk, K.T.; et al. Effects of Branched-Chain Amino Acid (BCAA) Supplementation on the Progression of Advanced Liver Disease: A Korean Nationwide, Multicenter, Prospective, Observational, Cohort Study. Nutrients 2020, 12, 1429. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Chen, Y.; Wang, X.; Li, H.; Zhang, H.; Gong, J.; Shen, S.; Yin, W.; Hu, H. Efficacy and Safety of Oral Branched-Chain Amino Acid Supplementation in Patients Undergoing Interventions for Hepatocellular Carcinoma: A Meta-Analysis. Nutr. J. 2015, 14, 67. [Google Scholar] [CrossRef] [PubMed]
- Hayaishi, S.; Chung, H.; Kudo, M.; Ishikawa, E.; Takita, M.; Ueda, T.; Kitai, S.; Inoue, T.; Yada, N.; Hagiwara, S.; et al. Oral Branched-Chain Amino Acid Granules Reduce the Incidence of Hepatocellular Carcinoma and Improve Event-Free Survival in Patients with Liver Cirrhosis. Dig. Dis. 2011, 29, 326–332. [Google Scholar] [CrossRef]
- Brosnan, J.T.; Brosnan, M.E. Branched-Chain Amino Acids: Enzyme and Substrate Regulation. J. Nutr. 2006, 136, 207S–211S. [Google Scholar] [CrossRef] [PubMed]
- Suryawan, A.; Hawes, J.W.; Harris, R.A.; Shimomura, Y.; Jenkins, A.E.; Hutson, S.M. A Molecular Model of Human Branched-Chain Amino Acid Metabolism123. Am. J. Clin. Nutr. 1998, 68, 72–81. [Google Scholar] [CrossRef]
- Harper, A.E.; Miller, R.H.; Block, K.P. Branched-Chain Amino Acid Metabolism. Annu. Rev. Nutr. 1984, 4, 409–454. [Google Scholar] [CrossRef]
- Shin, A.C.; Fasshauer, M.; Filatova, N.; Grundell, L.A.; Zielinski, E.; Zhou, J.Y.; Scherer, T.; Lindtner, C.; White, P.J.; Lapworth, A.L.; et al. Brain Insulin Lowers Circulating Bcaa Levels by Inducing Hepatic Bcaa Catabolism. Cell Metab. 2014, 20, 898–909. [Google Scholar] [CrossRef]
- Everman, S.; Mandarino, L.J.; Carroll, C.C.; Katsanos, C.S. Effects of Acute Exposure to Increased Plasma Branched-Chain Amino Acid Concentrations on Insulin-Mediated Plasma Glucose Turnover in Healthy Young Subjects. PLoS ONE 2015, 10, e0120049. [Google Scholar] [CrossRef]
- Azuma, Y.; Maekawa, M.; Kuwabara, Y.; Nakajima, T.; Taniguchi, K.; Kanno, T. Determination of Branched-Chain Amino Acids and Tyrosine in Serum of Patients with Various Hepatic Diseases, and Its Clinical Usefulness. Clin. Chem. 1989, 35, 1399–1403. [Google Scholar] [CrossRef]
- Mino, M.; Sano, A.; Kakazu, E.; Matsubara, H.; Kakisaka, K.; Kogure, T.; Sekine, K.; Aoki, Y.; Imamura, M.; Matsuda, M.; et al. Differences in Branched-Chain Amino Acid to Tyrosine Ratio (BTR) among Etiologies of Chronic Liver Disease Progression Compared to Healthy Adults. J. Gastroenterol. 2024, 59, 483–493. [Google Scholar] [CrossRef]
- Shimobayashi, M.; Hall, M.N. Making New Contacts: The mTOR Network in Metabolism and Signalling Crosstalk. Nat. Rev. Mol. Cell Biol. 2014, 15, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Laplante, M.; Sabatini, D.M. mTOR Signaling in Growth Control and Disease. Cell 2012, 149, 274–293. [Google Scholar] [CrossRef] [PubMed]
- Sancak, Y.; Peterson, T.R.; Shaul, Y.D.; Lindquist, R.A.; Thoreen, C.C.; Bar-Peled, L.; Sabatini, D.M. The Rag GTPases Bind Raptor and Mediate Amino Acid Signaling to mTORC1. Science 2008, 320, 1496–1501. [Google Scholar] [CrossRef] [PubMed]
- Sancak, Y.; Bar-Peled, L.; Zoncu, R.; Markhard, A.L.; Nada, S.; Sabatini, D.M. Ragulator-Rag Complex Targets mTORC1 to the Lysosomal Surface and Is Necessary for Its Activation by Amino Acids. Cell 2010, 141, 290–303. [Google Scholar] [CrossRef] [PubMed]
- Garami, A.; Zwartkruis, F.J.T.; Nobukuni, T.; Joaquin, M.; Roccio, M.; Stocker, H.; Kozma, S.C.; Hafen, E.; Bos, J.L.; Thomas, G. Insulin Activation of Rheb, a Mediator of mTOR/S6K/4E-BP Signaling, Is Inhibited by TSC1 and 2. Mol. Cell 2003, 11, 1457–1466. [Google Scholar] [CrossRef] [PubMed]
- Han, J.M.; Jeong, S.J.; Park, M.C.; Kim, G.; Kwon, N.H.; Kim, H.K.; Ha, S.H.; Ryu, S.H.; Kim, S. Leucyl-tRNA Synthetase Is an Intracellular Leucine Sensor for the mTORC1-Signaling Pathway. Cell 2012, 149, 410–424. [Google Scholar] [CrossRef] [PubMed]
- Bonfils, G.; Jaquenoud, M.; Bontron, S.; Ostrowicz, C.; Ungermann, C.; De Virgilio, C. Leucyl-tRNA Synthetase Controls TORC1 via the EGO Complex. Mol. Cell 2012, 46, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Yoon, M.S.; Son, K.; Arauz, E.; Han, J.M.; Kim, S.; Chen, J. Leucyl-tRNA Synthetase Activates Vps34 in Amino Acid-Sensing mTORC1 Signaling. Cell Rep. 2016, 16, 1510–1517. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.-X.; Xiong, Y.; Guan, K.-L. Nutrient Sensing, Metabolism, and Cell Growth Control. Mol. Cell 2013, 49, 379–387. [Google Scholar] [CrossRef]
- Hay, N.; Sonenberg, N. Upstream and Downstream of mTOR. Genes. Dev. 2004, 18, 1926–1945. [Google Scholar] [CrossRef] [PubMed]
- Inoki, K.; Li, Y.; Xu, T.; Guan, K.-L. Rheb GTpase Is a Direct Target of TSC2 GAP Activity and Regulates mTOR Signaling. Genes. Dev. 2003, 17, 1829–1834. [Google Scholar] [CrossRef] [PubMed]
- Alessi, D.R.; James, S.R.; Downes, C.P.; Holmes, A.B.; Gaffney, P.R.J.; Reese, C.B.; Cohen, P. Characterization of a 3-Phosphoinositide-Dependent Protein Kinase Which Phosphorylates and Activates Protein Kinase Bα. Curr. Biol. 1997, 7, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Alessi, D.R.; Andjelkovic, M.; Caudwell, B.; Cron, P.; Morrice, N.; Cohen, P.; Hemmings, B.A. Mechanism of Activation of Protein Kinase B by Insulin and IGF-1. EMBO J. 1996, 15, 6541–6551. [Google Scholar] [CrossRef] [PubMed]
- Inoki, K.; Li, Y.; Zhu, T.; Wu, J.; Guan, K.-L. TSC2 Is Phosphorylated and Inhibited by Akt and Suppresses mTOR Signalling. Nat. Cell Biol. 2002, 4, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Tzatsos, A.; Kandror, K.V. Nutrients Suppress Phosphatidylinositol 3-Kinase/Akt Signaling via Raptor-Dependent mTOR-Mediated Insulin Receptor Substrate 1 Phosphorylation. Mol. Cell Biol. 2006, 26, 63–76. [Google Scholar] [CrossRef] [PubMed]
- Um, S.H.; Frigerio, F.; Watanabe, M.; Picard, F.; Joaquin, M.; Sticker, M.; Fumagalli, S.; Allegrini, P.R.; Kozma, S.C.; Auwerx, J.; et al. Absence of S6K1 Protects against Age- and Diet-Induced Obesity While Enhancing Insulin Sensitivity. Nature 2004, 431, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, A.; Nishiyama, M.; Ishizaki, S. Branched-Chain Amino Acids Prevent Insulin-Induced Hepatic Tumor Cell Proliferation by Inducing Apoptosis through mTORC1 and mTORC2-Dependent Mechanisms. J. Cell. Physiol. 2012, 227, 2097–2105. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Sanyal, A.J. The Global NAFLD Epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A Multisociety Delphi Consensus Statement on New Fatty Liver Disease Nomenclature. J. Hepatol. 2023, 79, 1542–1556. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, E.H.; Flores-Guerrero, J.L.; Gruppen, E.G.; de Borst, M.H.; Wolak-Dinsmore, J.; Connelly, M.A.; Bakker, S.J.L.; Dullaart, R.P.F. Non-Alcoholic Fatty Liver Disease and Risk of Incident Type 2 Diabetes: Role of Circulating Branched-Chain Amino Acids. Nutrients 2019, 11, 705. [Google Scholar] [CrossRef] [PubMed]
- Newgard, C.B.; An, J.; Bain, J.R.; Muehlbauer, M.J.; Stevens, R.D.; Lien, L.F.; Haqq, A.M.; Shah, S.H.; Arlotto, M.; Slentz, C.A.; et al. A Branched-Chain Amino Acid-Related Metabolic Signature That Differentiates Obese and Lean Humans and Contributes to Insulin Resistance. Cell Metab. 2009, 9, 311–326. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Watkins, S.; Lorenzo, C.; Wagenknecht, L.; Il’yasova, D.; Chen, Y.-D.; Haffner, S.; Hanley, A. Branched-Chain Amino Acids and Insulin Metabolism: The Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 2016, 39, dc152284. [Google Scholar] [CrossRef] [PubMed]
- Sener, A.; Malaisse, W.J. The Stimulus-Secretion Coupling of Amino Acid-Induced Insulin Release: Insulinotropic Action of Branched-Chain Amino Acids at Physiological Concentrations of Glucose and Glutamine. Eur. J. Clin. Investig. 1981, 11, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Gaggini, M.; Carli, F.; Rosso, C.; Buzzigoli, E.; Marietti, M.; Della Latta, V.; Ciociaro, D.; Abate, M.L.; Gambino, R.; Cassader, M.; et al. Altered Amino Acid Concentrations in NAFLD: Impact of Obesity and Insulin Resistance. Hepatology 2018, 67, 145–158. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.; Wiklund, P.; Autio, R.; Borra, R.; Ojanen, X.; Xu, L.; Törmäkangas, T.; Alen, M. Adipose Tissue Dysfunction and Altered Systemic Amino Acid Metabolism Are Associated with Non-Alcoholic Fatty Liver Disease. PLoS ONE 2015, 10, e0138889. [Google Scholar] [CrossRef] [PubMed]
- Grzych, G.; Vonghia, L.; Bout, M.-A.; Weyler, J.; Verrijken, A.; Dirinck, E.; Chevalier Curt, M.J.; Van Gaal, L.; Paumelle, R.; Francque, S.; et al. Plasma BCAA Changes in Patients With NAFLD Are Sex Dependent. J. Clin. Endocrinol. Metab. 2020, 105, dgaa175. [Google Scholar] [CrossRef] [PubMed]
- Lagiou, P.; Kuper, H.; Stuver, S.O.; Tzonou, A.; Trichopoulos, D.; Adami, H.-O. Role of Diabetes Mellitus in the Etiology of Hepatocellular Carcinoma. JNCI J. Natl. Cancer Inst. 2000, 92, 1096–1099. [Google Scholar] [CrossRef] [PubMed]
- Shimada, M.; Hashimoto, E.; Taniai, M.; Hasegawa, K.; Okuda, H.; Hayashi, N.; Takasaki, K.; Ludwig, J. Hepatocellular Carcinoma in Patients with Non-Alcoholic Steatohepatitis. J. Hepatol. 2002, 37, 154–160. [Google Scholar] [CrossRef]
- El-serag, H.B.; Tran, T.; Everhart, J.E. Diabetes Increases the Risk of Chronic Liver Disease and Hepatocellular Carcinoma. Gastroenterology 2004, 126, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Ti, H.; Jc, W.; Wy, L.; Yh, H.; Pc, L.; Jh, C.; Fy, C.; Sd, L. Differential Mechanism and Prognostic Impact of Diabetes Mellitus on Patients with Hepatocellular Carcinoma Undergoing Surgical and Nonsurgical Treatment. Am. J. Gastroenterol. 2004, 99, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Miuma, S.; Ichikawa, T.; Taura, N.; Shibata, H.; Takeshita, S.; Akiyama, M.; Motoyoshi, Y.; Ozawa, E.; Fujimoto, M.; Kawashimo, H.; et al. The Level of Fasting Serum Insulin, but Not Adiponectin, Is Associated with the Prognosis of Early Stage Hepatocellular Carcinoma. Oncol. Rep. 2009, 22, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Inoue, S.; Saito, T.; Kiso, S.; Ito, N.; Tamura, S.; Watanabe, H.; Takeda, H.; Misawa, H.; Togashi, H.; et al. Augmentation Effect of Postprandial Hyperinsulinaemia on Growth of Human Hepatocellular Carcinoma. Gut 2002, 51, 100. [Google Scholar] [CrossRef] [PubMed]
- Muto, Y.; Sato, S.; Watanabe, A.; Moriwaki, H.; Suzuki, K.; Kato, A.; Kato, M.; Nakamura, T.; Higuchi, K.; Nishiguchi, S.; et al. Overweight and Obesity Increase the Risk for Liver Cancer in Patients with Liver Cirrhosis and Long-Term Oral Supplementation with Branched-Chain Amino Acid Granules Inhibits Liver Carcinogenesis in Heavier Patients with Liver Cirrhosis. Hepatol. Res. Off. J. Jpn. Soc. Hepatol. 2006, 35, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Yoshiji, H.; Noguchi, R.; Kitade, M.; Kaji, K.; Ikenaka, Y.; Namisaki, T.; Yoshii, J.; Yanase, K.; Yamazaki, M.; Tsujimoto, T.; et al. Branched-Chain Amino Acids Suppress Insulin-Resistance-Based Hepatocarcinogenesis in Obese Diabetic Rats. J. Gastroenterol. 2009, 44, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Miuma, S.; Ichikawa, T.; Arima, K.; Takeshita, S.; Muraoka, T.; Matsuzaki, T.; Ootani, M.; Shibata, H.; Akiyama, M.; Ozawa, E.; et al. Branched-Chain Amino Acid Deficiency Stabilizes Insulin-Induced Vascular Endothelial Growth Factor mRNA in Hepatocellular Carcinoma Cells. J. Cell Biochem. 2012, 113, 3113–3121. [Google Scholar] [CrossRef] [PubMed]
- Nishitani, S.; Horie, M.; Ishizaki, S.; Yano, H. Branched Chain Amino Acid Suppresses Hepatocellular Cancer Stem Cells through the Activation of Mammalian Target of Rapamycin. PLoS ONE 2013, 8, e82346. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kato, M.; Marui, K.; Murakami, T.; Onishi, K.; Adachi, T.; Matsuoka, J.; Ueki, H.; Yoshino, T.; Tsuruta, M.; et al. Easy Clinical Predictor for Low BCAA to Tyrosine Ratio in Chronic Liver Disease Patients with Hepatocellular Carcinoma: Usefulness of ALBI Score as Nutritional Prognostic Marker. Cancer Med. 2021, 10, 3584–3592. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, S.E.; Abdel-Samiee, M.; El-Said, H.; Youssef, M.I.; ElZohry, H.A.; Abdelsameea, E.; Moaz, I.; Abdelwahab, S.F.; Elaskary, S.A.; Zaher, E.M.; et al. Evaluation of Amino Acids Profile as Non-Invasive Biomarkers of Hepatocellular Carcinoma in Egyptians. Trop. Med. Infect. Dis. 2022, 7, 437. [Google Scholar] [CrossRef] [PubMed]
- Buchard, B.; Teilhet, C.; Abeywickrama Samarakoon, N.; Massoulier, S.; Joubert-Zakeyh, J.; Blouin, C.; Reynes, C.; Sabatier, R.; Biesse-Martin, A.-S.; Vasson, M.-P.; et al. Two Metabolomics Phenotypes of Human Hepatocellular Carcinoma in Non-Alcoholic Fatty Liver Disease According to Fibrosis Severity. Metabolites 2021, 11, 54. [Google Scholar] [CrossRef] [PubMed]
- Ericksen, R.E.; Lim, S.L.; McDonnell, E.; Shuen, W.H.; Vadiveloo, M.; White, P.J.; Ding, Z.; Kwok, R.; Lee, P.; Radda, G.K.; et al. Loss of BCAA Catabolism during Carcinogenesis Enhances mTORC1 Activity and Promotes Tumor Development and Progression. Cell Metab. 2019, 29, 1151-1165.e6. [Google Scholar] [CrossRef] [PubMed]
- Higashi, T.; Hayashi, H.; Kaida, T.; Arima, K.; Takeyama, H.; Taki, K.; Izumi, D.; Tokunaga, R.; Kosumi, K.; Nakagawa, S.; et al. Prognostic Impact of Visceral Fat Amount and Branched-Chain Amino Acids (BCAA) in Hepatocellular Carcinoma. Ann. Surg. Oncol. 2015, 22 (Suppl. 3), S1041–S1047. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M.Y.; Milsom, J.P.; Sherlock, S. Plasma Ratio of Valine, Leucine and Isoleucine to Phenylalanine and Tyrosine in Liver Disease. Gut 1978, 19, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- Tajika, M.; Kato, M.; Mohri, H.; Miwa, Y.; Kato, T.; Ohnishi, H.; Moriwaki, H. Prognostic Value of Energy Metabolism in Patients with Viral Liver Cirrhosis. Nutrition 2002, 18, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Yamato, M.; Muto, Y.; Yoshida, T.; Kato, M.; Moriwaki, H. Clearance Rate of Plasma Branched-Chain Amino Acids Correlates Significantly with Blood Ammonia Level in Patients with Liver Cirrhosis. Int. Hepatol. Commun. 1995, 3, 91–96. [Google Scholar] [CrossRef]
- Kato, M.; Miwa, Y.; Tajika, M.; Hiraoka, T.; Muto, Y.; Moriwaki, H. Preferential Use of Branched-Chain Amino Acids as an Energy Substrate in Patients with Liver Cirrhosis. Intern. Med. 1998, 37, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Grattagliano, I.; Russmann, S.; Diogo, C.; Bonfrate, L.; Oliveira, P.; Wang, D.; Portincasa, P. Mitochondria in Chronic Liver Disease. Curr. Drug Targets 2011, 12, 879–893. [Google Scholar] [CrossRef] [PubMed]
- James, J.H. Branched Chain Amino Acids in Heptatic Encephalopathy. Am. J. Surg. 2002, 183, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.E.; Rosen, H.M.; Ebeid, A.M.; James, J.H.; Keane, J.M.; Soeters, P.B. The Effect of Normalization of Plasma Amino Acids on Hepatic Encephalopathy in Man. Surgery 1976, 80, 77–91. [Google Scholar] [PubMed]
- Kakazu, E.; Kanno, N.; Ueno, Y.; Shimosegawa, T. Extracellular Branched-Chain Amino Acids, Especially Valine, Regulate Maturation and Function of Monocyte-Derived Dendritic Cells. J. Immunol. 2007, 179, 7137–7146. [Google Scholar] [CrossRef] [PubMed]
- Kakazu, E.; Ueno, Y.; Kondo, Y.; Fukushima, K.; Shiina, M.; Inoue, J.; Tamai, K.; Ninomiya, M.; Shimosegawa, T. Branched Chain Amino Acids Enhance the Maturation and Function of Myeloid Dendritic Cells Ex Vivo in Patients with Advanced Cirrhosis. Hepatology 2009, 50, 1936–1945. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Torimura, T.; Takata, A.; Satomi, S.; Sata, M. Valine, a Branched-Chain Amino Acid, Reduced HCV Viral Load and Led to Eradication of HCV by Interferon Therapy in a Decompensated Cirrhotic Patient. Case Rep. Gastroenterol. 2012, 6, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Ishida, H.; Kato, T.; Takehana, K.; Tatsumi, T.; Hosui, A.; Nawa, T.; Kodama, T.; Shimizu, S.; Hikita, H.; Hiramatsu, N.; et al. Valine, the Branched-Chain Amino Acid, Suppresses Hepatitis C Virus RNA Replication but Promotes Infectious Particle Formation. Biochem. Biophys. Res. Commun. 2013, 437, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Honda, M.; Takehana, K.; Sakai, A.; Tagata, Y.; Shirasaki, T.; Nishitani, S.; Muramatsu, T.; Yamashita, T.; Nakamoto, Y.; Mizukoshi, E.; et al. Malnutrition Impairs Interferon Signaling through mTOR and FoxO Pathways in Patients with Chronic Hepatitis C. Gastroenterology 2011, 141, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Nagao, Y.; Kawaguchi, T.; Ide, T.; Sata, M. Effect of Branched-Chain Amino Acid-Enriched Nutritional Supplementation on Interferon Therapy in Japanese Patients with Chronic Hepatitis C Virus Infection: A Retrospective Study. Virol. J. 2012, 9, 282. [Google Scholar] [CrossRef] [PubMed]
- Honda, T.; Fukuda, Y.; Nakano, I.; Katano, Y.; Goto, H.; Nagasaki, M.; Sato, Y.; Murakami, T.; Shimomura, Y. Effects of Liver Failure on Branched-Chain Alpha-Keto Acid Dehydrogenase Complex in Rat Liver and Muscle: Comparison between Acute and Chronic Liver Failure. J. Hepatol. 2004, 40, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, T.; Yokoyama, Y.; Kokuryo, T.; Nagino, M. Protective Effects of Branched-Chain Amino Acids on Hepatic Ischemia-Reperfusion-Induced Liver Injury in Rats: A Direct Attenuation of Kupffer Cell Activation. Am. J. Physiol.-Gastrointest. Liver Physiol. 2013, 304, G346–G355. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, G.; Adachi, N.; Liu, K.; Motoki, A.; Mitsuyo, T.; Nagaro, T.; Arai, T. Recovery of Brain Dopamine Metabolism by Branched-Chain Amino Acids in Rats with Acute Hepatic Failure. J. Neurosurg. Anesthesiol. 2007, 19, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Kuwahata, M.; Kuramoto, Y.; Tomoe, Y.; Sugata, E.; Segawa, H.; Ito, M.; Oka, T.; Miyamoto, K. Posttranscriptional Regulation of Albumin Gene Expression by Branched-Chain Amino Acids in Rats with Acute Liver Injury. Biochim. Et Biophys. Acta (BBA)—Mol. Basis Dis. 2004, 1739, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Rigotti, P.; Peters, J.C.; Tranberg, K.-G.; Fischer, J.E. Effects of Amino Acid Infusions on Liver Regeneration after Partial Hepatectomy in the Rat. JPEN. J. Parenter. Enter. Nutr. 1986, 10, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Holecek, M.; Simek, J.; Kruf, M.; Zadák, Z. Effect of Branched Chain Amino Acids on Liver Regeneration after Partial Hepatectomy. Physiol. Bohemoslov. 1985, 34, 359–366. [Google Scholar] [PubMed]
- Holecek, M.; Simek, J.; Palicka, V.; Zadák, Z. Effect of Glucose and Branched Chain Amino Acid (BCAA) Infusion on Onset of Liver Regeneration and Plasma Amino Acid Pattern in Partially Hepatectomized Rats. J. Hepatol. 1991, 13, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Okita, M.; Watanabe, A.; Nagashima, H. Nutritional Treatment of Liver Cirrhosis by Branched-Chain Amino Acid-Enriched Nutrient Mixture. J. Nutr. Sci. Vitaminol. 1985, 31, 291–303. [Google Scholar] [CrossRef] [PubMed]
- American Association for the Study of Liver Diseases; European Association for the Study of the Liver. Hepatic Encephalopathy in Chronic Liver Disease: 2014 Practice Guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J. Hepatol. 2014, 61, 642–659. [Google Scholar] [CrossRef] [PubMed]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN Guideline on Clinical Nutrition in Liver Disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, S.; Ichikawa, T.; Nakao, K.; Miyaaki, H.; Shibata, H.; Matsuzaki, T.; Muraoka, T.; Honda, T.; Otani, M.; Akiyama, M.; et al. A Snack Enriched with Oral Branched-Chain Amino Acids Prevents a Fall in Albumin in Patients with Liver Cirrhosis Undergoing Chemoembolization for Hepatocellular Carcinoma. Nutr. Res. 2009, 29, 89–93. [Google Scholar] [CrossRef] [PubMed]
- San-in Group of Liver Surgery. Long-Term Oral Administration of Branched Chain Amino Acids after Curative Resection of Hepatocellular Carcinoma: A Prospective Randomized Trial. The San-in Group of Liver Surgery. Br. J. Surg. 1997, 84, 1525–1531. [Google Scholar] [CrossRef]
- Poon, R.T.-P.; Yu, W.-C.; Fan, S.-T.; Wong, J. Long-Term Oral Branched Chain Amino Acids in Patients Undergoing Chemoembolization for Hepatocellular Carcinoma: A Randomized Trial. Aliment. Pharmacol. Ther. 2004, 19, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Togo, S.; Tanaka, K.; Morioka, D.; Sugita, M.; Ueda, M.; Miura, Y.; Kubota, T.; Nagano, Y.; Matsuo, K.; Endo, I.; et al. Usefulness of Granular BCAA after Hepatectomy for Liver Cancer Complicated with Liver Cirrhosis. Nutrition 2005, 21, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, Y.; Hiroshima, Y.; Matsuo, K.; Kawaguchi, D.; Murakami, T.; Yabushita, Y.; Endo, I.; Taguri, M.; Koda, K.; Tanaka, K. A Randomized Clinical Trial of Preoperative Administration of Branched-Chain Amino Acids to Prevent Postoperative Ascites in Patients with Liver Resection for Hepatocellular Carcinoma. Ann. Surg. Oncol. 2016, 23, 3727–3735. [Google Scholar] [CrossRef] [PubMed]
- Morihara, D.; Iwata, K.; Hanano, T.; Kunimoto, H.; Kuno, S.; Fukunaga, A.; Yotsumoto, K.; Takata, K.; Tanaka, T.; Sakurai, K.; et al. Late-Evening Snack with Branched-Chain Amino Acids Improves Liver Function after Radiofrequency Ablation for Hepatocellular Carcinoma. Hepatol. Res. 2012, 42, 658–667. [Google Scholar] [CrossRef] [PubMed]
- Yoshiji, H.; Noguchi, R.; Namisaki, T.; Moriya, K.; Kitade, M.; Aihara, Y.; Douhara, A.; Yamao, J.; Fujimoto, M.; Toyohara, M.; et al. Branched-Chain Amino Acids Suppress the Cumulative Recurrence of Hepatocellular Carcinoma under Conditions of Insulin-Resistance. Oncol. Rep. 2013, 30, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Meng, W.C.; Leung, K.L.; Ho, R.L.; Leung, T.W.; Lau, W.Y. Prospective Randomized Control Study on the Effect of Branched-Chain Amino Acids in Patients with Liver Resection for Hepatocellular Carcinoma. Aust. N. Z. J. Surg. 1999, 69, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, H.; Ushio, A.; Miyamoto, Y.; Sawara, K.; Oikawa, K.; Kasai, K.; Endo, R.; Takikawa, Y.; Kato, A.; Suzuki, K. Effects of Branched-Chain Amino Acid-Enriched Nutrient for Patients with Hepatocellular Carcinoma Following Radiofrequency Ablation: A One-Year Prospective Trial. J. Gastroenterol. Hepatol. 2010, 25, 1550–1555. [Google Scholar] [CrossRef] [PubMed]
- Okabayashi, T.; Iyoki, M.; Sugimoto, T.; Kobayashi, M.; Hanazaki, K. Oral Supplementation with Carbohydrate- and Branched-Chain Amino Acid-Enriched Nutrients Improves Postoperative Quality of Life in Patients Undergoing Hepatic Resection. Amino Acids 2011, 40, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, K.; Okabayashi, T.; Maeda, H.; Namikawa, T.; Iiyama, T.; Sugimoto, T.; Kobayashi, M.; Mimura, T.; Hanazaki, K. Oral Supplementation of Branched-Chain Amino Acids Reduces Early Recurrence after Hepatic Resection in Patients with Hepatocellular Carcinoma: A Prospective Study. Surg. Today 2013, 43, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Nojiri, S.; Fujiwara, K.; Shinkai, N.; Iio, E.; Joh, T. Effects of Branched-Chain Amino Acid Supplementation after Radiofrequency Ablation for Hepatocellular Carcinoma: A Randomized Trial. Nutrition 2017, 33, 20–27. [Google Scholar] [CrossRef]
- Hachiya, H.; Aoki, T.; Iso, Y.; Shimizu, T.; Tago, K.; Park, K.H.; Sakuraoka, Y.; Shiraki, T.; Mori, S.; Kubota, K. Effects of Branched-Chain Amino Acids on Postoperative Tumor Recurrence in Patients Undergoing Curative Resection for Hepatocellular Carcinoma: A Randomized Clinical Trial. J. Hepatobiliary Pancreat. Sci. 2020, 27, 819–829. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.J.; Seong, J.; Bae, J.I.; You, S.H.; Rhee, Y.; Lee, J.H. Effect of Oral Supplementation with Branched-Chain Amino Acid (BCAA) during Radiotherapy in Patients with Hepatocellular Carcinoma: A Double-Blind Randomized Study. Cancer Res. Treat. 2011, 43, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Yoshiji, H.; Noguchi, R.; Ikenaka, Y.; Kaji, K.; Aihara, Y.; Yamazaki, M.; Yamao, J.; Toyohara, M.; Mitoro, A.; Sawai, M.; et al. Combination of Branched-Chain Amino Acids and Angiotensin-Converting Enzyme Inhibitor Suppresses the Cumulative Recurrence of Hepatocellular Carcinoma: A Randomized Control Trial. Oncol. Rep. 2011, 26, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Tada, T.; Kumada, T.; Toyoda, H.; Yasuda, S.; Koyabu, T.; Nakashima, M. Impact of Branched-Chain Amino Acid Granule Therapy in Patients with Hepatocellular Carcinoma Who Have Normal Albumin Levels and Low Branched-Chain Amino Acid to Tyrosine Ratios. Nutr. Cancer 2019, 71, 1132–1141. [Google Scholar] [CrossRef] [PubMed]
- Harima, Y.; Yamasaki, T.; Hamabe, S.; Saeki, I.; Okita, K.; Terai, S.; Sakaida, I. Effect of a Late Evening Snack Using Branched-Chain Amino Acid-Enriched Nutrients in Patients Undergoing Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma. Hepatol. Res. 2010, 40, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Nishiguchi, S.; Habu, D. Effect of Oral Supplementation with Branched-Chain Amino Acid Granules in the Early Stage of Cirrhosis. Hepatol. Res. 2004, 30S, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Muto, Y.; Sato, S.; Watanabe, A.; Moriwaki, H.; Suzuki, K.; Kato, A.; Kato, M.; Nakamura, T.; Higuchi, K.; Nishiguchi, S.; et al. Effects of Oral Branched-Chain Amino Acid Granules on Event-Free Survival in Patients with Liver Cirrhosis. Clin. Gastroenterol. Hepatol. 2005, 3, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Watanabe, A.; Muto, Y.; Suzuki, K.; Kato, A.; Moriwaki, H.; Kato, M.; Nakamura, T. LIV-EN Study Group Clinical Comparison of Branched-Chain Amino Acid (l-Leucine, l-Isoleucine, l-Valine) Granules and Oral Nutrition for Hepatic Insufficiency in Patients with Decompensated Liver Cirrhosis (LIV-EN Study). Hepatol. Res. 2005, 31, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Nakaya, Y.; Okita, K.; Suzuki, K.; Moriwaki, H.; Kato, A.; Miwa, Y.; Shiraishi, K.; Okuda, H.; Onji, M.; Kanazawa, H.; et al. BCAA-Enriched Snack Improves Nutritional State of Cirrhosis. Nutrition 2007, 23, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Habu, D.; Nishiguchi, S.; Nakatani, S.; Lee, C.; Enomoto, M.; Tamori, A.; Takeda, T.; Ohfuji, S.; Fukushima, W.; Tanaka, T.; et al. Comparison of the Effect of BCAA Granules on between Decompensated and Compensated Cirrhosis. Hepatogastroenterology 2009, 56, 1719–1723. [Google Scholar] [PubMed]
- Kobayashi, M.; Ikeda, K.; Arase, Y.; Suzuki, Y.; Suzuki, F.; Akuta, N.; Hosaka, T.; Murashima, N.; Saitoh, S.; Someya, T.; et al. Inhibitory Effect of Branched-Chain Amino Acid Granules on Progression of Compensated Liver Cirrhosis Due to Hepatitis C Virus. J. Gastroenterol. 2008, 43, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Marchesini, G.; Bianchi, G.; Merli, M.; Amodio, P.; Panella, C.; Loguercio, C.; Rossi Fanelli, F.; Abbiati, R. Nutritional Supplementation with Branched-Chain Amino Acids in Advanced Cirrhosis: A Double-Blind, Randomized Trial. Gastroenterology 2003, 124, 1792–1801. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, E.; Habu, D.; Morikawa, H.; Enomoto, M.; Kawabe, J.; Tamori, A.; Sakaguchi, H.; Saeki, S.; Kawada, N.; Shiomi, S. A Randomized Pilot Trial of Oral Branched-Chain Amino Acids in Early Cirrhosis: Validation Using Prognostic Markers for Pre-Liver Transplant Status. Liver Transpl. 2009, 15, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Paski, S.C.; Dodge, J.; Bambha, K.; Biggins, S.W.; Ioannou, G.N. Effect of Dietary Branched Chain Amino Acids on Liver Related Mortality: Results from a Large Cohort of North American Patients with Advanced HCV Infection. PLoS ONE 2023, 18, e0284739. [Google Scholar] [CrossRef] [PubMed]
- Les, I.; Doval, E.; García-Martínez, R.; Planas, M.; Cárdenas, G.; Gómez, P.; Flavià, M.; Jacas, C.; Mínguez, B.; Vergara, M.; et al. Effects of Branched-Chain Amino Acids Supplementation in Patients with Cirrhosis and a Previous Episode of Hepatic Encephalopathy: A Randomized Study. Am. J. Gastroenterol. 2011, 106, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Hidaka, H.; Nakazawa, T.; Kutsukake, S.; Yamazaki, Y.; Aoki, I.; Nakano, S.; Asaba, N.; Minamino, T.; Takada, J.; Tanaka, Y.; et al. The Efficacy of Nocturnal Administration of Branched-Chain Amino Acid Granules to Improve Quality of Life in Patients with Cirrhosis. J. Gastroenterol. 2013, 48, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Conde, M.; Llop, E.; Gómez-Pimpollo, L.; Fernández Carrillo, C.; Rodríguez, L.; Van Den Brule, E.; Perelló, C.; López-Gómez, M.; Abad, J.; Martínez-Porras, J.L.; et al. Adding Branched-Chain Amino Acids to an Enhanced Standard-of-Care Treatment Improves Muscle Mass of Cirrhotic Patients With Sarcopenia: A Placebo-Controlled Trial. Am. J. Gastroenterol. 2021, 116, 2241–2249. [Google Scholar] [CrossRef] [PubMed]
- Singh Tejavath, A.; Mathur, A.; Nathiya, D.; Singh, P.; Raj, P.; Suman, S.; Mundada, P.R.; Atif, S.; Rai, R.R.; Tomar, B.S. Impact of Branched Chain Amino Acid on Muscle Mass, Muscle Strength, Physical Performance, Combined Survival, and Maintenance of Liver Function Changes in Laboratory and Prognostic Markers on Sarcopenic Patients With Liver Cirrhosis (BCAAS Study): A Randomized Clinical Trial. Front. Nutr. 2021, 8, 715795. [Google Scholar] [CrossRef] [PubMed]
- Siramolpiwat, S.; Limthanetkul, N.; Pornthisarn, B.; Vilaichone, R.-K.; Chonprasertsuk, S.; Bhanthumkomol, P.; Nunanan, P.; Issariyakulkarn, N. Branched-Chain Amino Acids Supplementation Improves Liver Frailty Index in Frail Compensated Cirrhotic Patients: A Randomized Controlled Trial. BMC Gastroenterol. 2023, 23, 154. [Google Scholar] [CrossRef] [PubMed]
- Sobhy, E.; Kamal, M.M.; Saad, Y.; Saleh, D.A.; Elgohary, R.; Hassan, M.S. Effect of Branched-Chain Amino Acid Supplementation and Exercise on Quadriceps Muscle Quantity and Quality in Patients with Cirrhosis as Assessed by Ultrasonography: A Randomized Controlled Trial. Clin. Nutr. ESPEN 2024, 61, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Tsien, C.; Davuluri, G.; Singh, D.; Allawy, A.; Ten Have, G.A.M.; Thapaliya, S.; Schulze, J.M.; Barnes, D.; McCullough, A.J.; Engelen, M.P.K.J.; et al. Metabolic and Molecular Responses to Leucine-Enriched Branched Chain Amino Acid Supplementation in the Skeletal Muscle of Alcoholic Cirrhosis. Hepatology 2015, 61, 2018–2029. [Google Scholar] [CrossRef] [PubMed]
- Mohta, S.; Anand, A.; Sharma, S.; Qamar, S.; Agarwal, S.; Gunjan, D.; Singh, N.; Madhusudhan, K.S.; Pandey, R.M.; Saraya, A. Randomised Clinical Trial: Effect of Adding Branched Chain Amino Acids to Exercise and Standard-of-Care on Muscle Mass in Cirrhotic Patients with Sarcopenia. Hepatol. Int. 2022, 16, 680–690. [Google Scholar] [CrossRef] [PubMed]
- Hey, P.; Hoermann, R.; Sinclair, M.; Chapman, B.; Testro, A.; Apostolov, R.; Angus, P.; Gow, P. Branched-Chain Amino Acid Supplementation Does Not Improve Measures of Sarcopenia in Cirrhosis: Results of a Randomised Controlled Trial. Aliment. Pharmacol. Ther. 2024, 59, 941–952. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, M.; Takeda, K.; Sakamoto, K.; Ohata, M.; Toda, G. Effect of Oral Branched Chain Amino Acid Supplementation in the Late Evening on the Nutritional State of Patients with Liver Cirrhosis. Hepatol. Res. 2001, 21, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, H.; Miwa, Y.; Ida, E.; Kuriyama, S.; Toda, K.; Shimomura, Y.; Sugiyama, A.; Sugihara, J.; Tomita, E.; Moriwaki, H. Nocturnal Branched-Chain Amino Acid Administration Improves Protein Metabolism in Patients with Liver Cirrhosis: Comparison with Daytime Administration. J. Parenter. Enter. Nutr. 2003, 27, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, M.; Sakaida, I.; Okamoto, M.; Okita, K. The Effect of a Late Evening Snack in Patients with Liver Cirrhosis. Hepatol. Res. 2005, 31, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Korenaga, K.; Korenaga, M.; Uchida, K.; Yamasaki, T.; Sakaida, I. Effects of a Late Evening Snack Combined with Alpha-Glucosidase Inhibitor on Liver Cirrhosis. Hepatol. Res. 2008, 38, 1087–1097. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, T.; Naota, T.; Miyaaki, H.; Miuma, S.; Isomoto, H.; Takeshima, F.; Nakao, K. Effect of an Oral Branched Chain Amino Acid-Enriched Snack in Cirrhotic Patients with Sleep Disturbance. Hepatol. Res. 2010, 40, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Koreeda, C.; Seki, T.; Okazaki, K.; Ha-Kawa, S.K.; Sawada, S. Effects of Late Evening Snack Including Branched-Chain Amino Acid on the Function of Hepatic Parenchymal Cells in Patients with Liver Cirrhosis. Hepatol. Res. 2011, 41, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Maki, H.; Yamanaka-Okumura, H.; Katayama, T.; Ozawa, Y.; Hosoda, A.; Kurata, N.; Amemiya, F. Late Evening Snacks with Branched-Chain Amino Acids Improve the Fischer Ratio with Patients Liver Cirrhosis at Fasting in the next Morning. Clin. Nutr. ESPEN 2019, 30, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, K.; Namisaki, T.; Mashitani, T.; Kaji, K.; Ozaki, K.; Saikawa, S.; Sato, S.; Inoue, T.; Sawada, Y.; Kitagawa, K.; et al. Late-Evening Snack with Branched-Chain Amino Acid-Enriched Nutrients Does Not Always Inhibit Overt Diabetes in Patients with Cirrhosis: A Pilot Study. Nutrients 2019, 11, 2140. [Google Scholar] [CrossRef] [PubMed]
| Year | Hepatocellular Carcinoma | Duration | Study Design | Sample Size | Interventions | Frequency | Major Outcome | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1997 | after curative resection | 3 years | RCT | 150 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily for at least 1 year | bid | • improved clinical features and laboratory data without increasing the rate of tumor recurrence | [86] |
| 1999 | after hepatic resection | 1 year | RCT | 44 | 150 g Aminoleban® EN (contains 16.5 g BCAAs) daily for 12 weeks | tid | • a shorter hospital stay • quicker improvement of liver function | [92] |
| 2004 | undergoing chemoembolization | 1 year | RCT | 84 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily | bid | • increased serum albumin level • reduced the morbidity • improve QOL | [87] |
| 2005 | complicated with cirrhosis after hepatectomy | 1 year | RCT | 43 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • maintained a higher serum albumin level • decreased liver fibrosis | [88] |
| 2009 | complicated with cirrhosis undergoing chemoembolization | 2 weeks | RCT | 56 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) daily | qd | • prevented suppression of liver function by TACE | [85] |
| 2010 | complicated with cirrhosis, underwent RFA (HCV) | 1 year | 49 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily | bid | • improved both nutritional state and QOL | [93] | |
| 2010 | undergoing HAIC | 5 weeks | RCT | 23 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) at 22:00 | qd | • improved energy metabolism and glucose tolerance | [101] |
| 2010 | undergoing radiotherapy | 6 weeks | RCT | 50 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily during radiotherapy | tid | • improved biochemical profiles | [98] |
| 2010 | after hepatic resection | 26 weeks | RCT | 96 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily | bid | • improved postoperative QOL over the long term | [94] |
| 2011 | underwent RFA | 4 years | RCT | 110 | ACEI (perindopril; 4 mg/day) or BCAA granules (Livact; 12 g/day) or ACEI + BCAA | • ACEI + BCAA markedly inhibited the cumulative recurrence of HCC under IR conditions • neither single treatment exerted a significant inhibition | [99] | |
| 2012 | complicated with cirrhosis, underwent RFA | 3 months | RCT | 30 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) daily after breakfast or at 22:00 | qd | • improved liver functioning and Child–Pugh score | [90] |
| 2012 | after hepatic resection | 26 weeks | RCT | 56 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • reduced early recurrence | [95] |
| 2013 | underwent local curative therapy (IR) | 60 months | RCT | 93 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • BCAAs functioned via coordinated effects of anti-angiogenesis and IR improvement | [91] |
| 2016 | undergoing major liver resection | 13 months | RCT | 77 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily for 1 month before liver resection and 1 year after | tid | • preoperative administration of BCAA did not significantly improve the prevention of refractory ascites • prevented ascites, pleural effusion, or both • improved the metabolism of albumin | [89] |
| 2017 | underwent RFA | 5 years | RCT | 51 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily | bid | • relieved mental stress • reduced the risks of intrahepatic recurrence and complications | [96] |
| 2019 | (normal albumin levels and low BTRs) | 10 years | 78 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • improved both overall survival and disease-specific survival | [100] | |
| 2020 | after curative resection | 4 years | RCT | 156 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • did not reduce the risk of recurrence • was beneficial for patients who were younger and had mildly impaired glucose tolerance | [97] |
| Year | Cirrhosis | Duration | Study Design | Sample Size | Interventions | Frequency | Major Outcome | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1985 | cirrhosis | 6 weeks | SAT | 10 | 150 g SF-1008C (contains 18.45 g BCAAs) daily for 2 weeks | tid | • no deleterious effects on nitrogen metabolism • useful for the improvement of plasma amino acid imbalance and PEM | [82] |
| 2001 | cirrhosis | 28 days | SAT | 14 | 100 g Aminoleban® (contains 11 g BCAAs) daily at 8:30 and 19:00 or at 8:30 and 22:30 | bid | • late-evening BCAA supplementation was more helpful in improving protein catabolism and lipolysis | [120] |
| 2003 | compensated | 3 weeks and 3 months | crossover study and RCT | 24 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily 4g after each meal (at 8:30 AM, 12:30 PM, and 6:30 PM), or 4 g at 8:30 AM and 8 g at 11 PM | bid or tid | • nocturnal BCAA administration improved serum albumin levels, whereas daytime administration did not | [121] |
| 2003 | advanced | 15 months | RCT | 174 | 14.4 g BCAAs daily for 1 year | tid | • prevented progressive hepatic failure • improved surrogate markers and perceived health status | [108] |
| 2004 | early-stage (HCV) | 2 years | RCT | 65 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • maintained serum albumin • improved prognosis and maintained QOL | [102] |
| 2005 | cirrhosis | 7 days | RCT | 26 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) daily at 22:00 or 100 g Aminoleban® EN (contains 11 g BCAAs) daily at 22:00 and in the daytime | bid or tid | • LESs alone improved the energy malnutrition state and glucose intolerance to the same extent as LESs combined with divided meals | [122] |
| 2005 | decompensated | 2 years | RCT | 646 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • improved event-free survival, serum albumin concentration, and QOL | [103] |
| 2005 | decompensated (HE, hypoalbuminemia) | 6 months | RCT | 281 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) or 100 g Aminoleban® EN (contains 12.5 g BCAAs) daily | bid or tid | • adequate BCAAs alone improved serum albumin profiles to a similar extent as the oral nutritional supplementation | [104] |
| 2006 | decompensated (hypoalbuminemia) | 2 years | RCT | 622 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • the risk for liver cancer was significantly reduced in the BCAA group with a BMI of 25 or higher and with an AFP level of 20 ng/mL or higher | [53] |
| 2007 | advanced (HCV) | 3 months | RCT | 48 | 6.075 g of BCAAs daily | once a day before bedtime | • long-term oral supplementation of BCAA as LESs could better improve serum albumin levels and energy metabolism compared to regular food | [105] |
| 2008 | cirrhosis | 3 months | SAT | 11 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) + 0.2 mg voglibose daily | qd | • the combination of α-glucosidase inhibitors with BCAA-enriched LESs showed potential for improving glucose tolerance and energy metabolism | [123] |
| 2008 | compensated (HCV) | 3.5 years | RCT | 40 | 12 g BCAAs daily for 168 weeks | tid | • BCAA may inhibit hepatic carcinogenesis in patients with compensated cirrhosis with a serum albumin level of <4.0 g/dL | [107] |
| 2009 | early stage | 6 years | RCT | 56 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily for at least 1 year | tid | • early interventional oral BCAAs might prolong the liver transplant waiting period by preserving hepatic reserve in cirrhosis | [109] |
| 2009 | decompensated and compensated (HCV) | 2 years | RCT | 65 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | tid | • if cirrhotic patients were in the compensated stage at the entrybut with lower BTR, as for decompensated cirrhosis, oral BCAA supplementation might be effective in maintaining serum albumin levels for 2 years | [106] |
| 2010 | (a previous episode of HE) | 8 weeks | RCT | 21 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) at 22:00 | qd | • beneficial for patients with sleep disturbance | [124] |
| 2011 | cirrhosis | 6 months | SAT | 17 | 100 g Aminoleban® EN (contains 11 g BCAAs) daily at 22:00 and in the daytime | bid | • BCAA-enriched LESs could improve protein malnutrition and improve hepatic parenchymal cell mass in the early stages of cirrhosis | [125] |
| 2011 | (a previous episode of HE) | 14 months | RCT | 116 | 100 g BCAAs daily for 56 weeks | bid | • did not decrease the recurrence of HE • improved minimal HE and muscle mass | [111] |
| 2013 | compensated | 3 months | RCT | 37 | 14.22 g LIVACT® Granules (contains 12 g BCAAs) daily | bid or tid | • nocturnal administration reduced the occurrence of muscle cramps in the leg but did not improve the patients’ QOL | [112] |
| 2015 | (alcoholic) | 14 | a single oral BCAA mixture enriched with leucine (BCAA/Leu) (7.5 g L-Leu, 3.75 g L-Ile, 3.75 g L-Val) | • impaired mTOR1 signaling and increased autophagy in skeletal muscle was acutely reversed | [117] | |||
| 2019 | cirrhosis | 1 month | RCT | 10 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) as LESs or 9.48 g LIVACT® Granules (contains 8 g BCAAs) + 50 g Aminoleban® EN (contains 5.5 g BCAAs) intraday or 9.48 g LIVACT® Granules (contains 8 g BCAAs) intraday + 50 g Aminoleban® EN (contains 5.5 g BCAAs) as LES | qd or tid | • increasing the fasting Fischer’s ratio required not only an increase in the intake of BCAAs, but also BCAA-enriched LES | [126] |
| 2019 | compensated (hypoalbuminemia) | 15 days | 13 | 50 g Aminoleban® EN (contains 5.5 g BCAAs) as LES | qd | • may worsen glucose homeostasis in obese and IR cirrhosis patients | [127] | |
| 2021 | (sarcopenia) | 3 months | RCT | 32 | 5.24 g BCAAs daily | qd | • improved muscle mass | [113] |
| 2021 | (sarcopenia) | 6 months | RCT | 106 | 7.2 g BCAAs daily | qd | • improved sarcopenia and prognostic markers | [114] |
| 2022 | (sarcopenia) | 6 months | RCT | 60 | 12 g BCAAs daily | bid | • did not improve muscle mass | [118] |
| 2023 | compensated (frailty) | 4 months | RCT | 54 | 100 g Aminoleban® (contains 11 g BCAAs) daily | bid | • improved frailty • improved muscle mass and physical domain of QOL | [115] |
| 2023 | (HCV) | retrospective cohort study | 656 | • BCAA intake was not associated with liver-related outcomes in HCV-infected patients with advanced fibrosis or compensated cirrhosis | [110] | |||
| 2024 | (sarcopenia) | 12 months | RCT | 150 | 21.2 g BCAAs daily | bid or tid | • did not improve measures of muscle strength, mass, or performance or physical frailty | [119] |
| 2024 | cirrhosis | 28 days | RCT | 220 | 10 g BCAAs daily or programmed exercise or 10 g BCAAs daily and programmed exercise | qd | • improved quadriceps muscle quantity and quality | [116] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Zhan, L.; Zhang, L.; Shi, Q.; Li, L. Branched-Chain Amino Acids in Liver Diseases: Complexity and Controversy. Nutrients 2024, 16, 1875. https://doi.org/10.3390/nu16121875
Zhang Y, Zhan L, Zhang L, Shi Q, Li L. Branched-Chain Amino Acids in Liver Diseases: Complexity and Controversy. Nutrients. 2024; 16(12):1875. https://doi.org/10.3390/nu16121875
Chicago/Turabian StyleZhang, Yaqi, Luqi Zhan, Lingjian Zhang, Qingmiao Shi, and Lanjuan Li. 2024. "Branched-Chain Amino Acids in Liver Diseases: Complexity and Controversy" Nutrients 16, no. 12: 1875. https://doi.org/10.3390/nu16121875




