Time-Dependent Effect of Eggshell Membrane on Monosodium-Iodoacetate-Induced Osteoarthritis: Early-Stage Inflammation Control and Late-Stage Cartilage Protection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of ESM
2.2. Animals and Ethics Statement
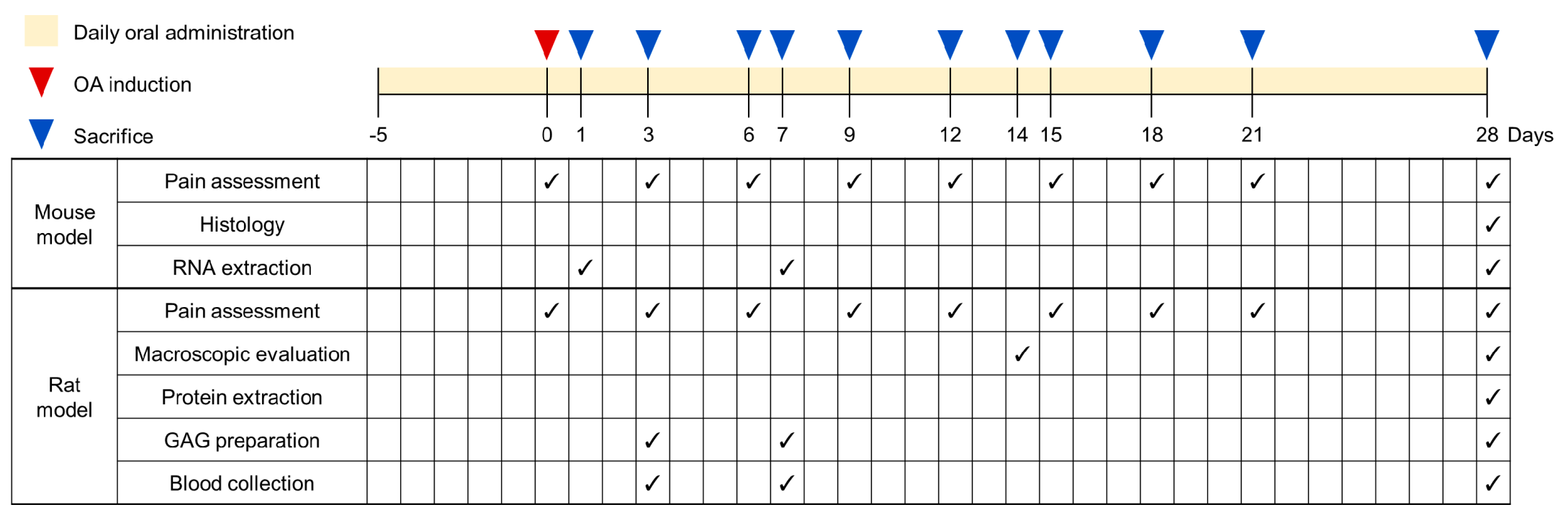
2.3. Experimental Design and Administration
2.4. MIA-Induced OA Animal Modelling
2.5. Pain Assessment (Weight-Bearing Test)
2.6. Macroscopic Observation (Gross Pathology)
2.7. Histological Analysis
2.8. Immunohistochemistry
2.9. Real-Time PCR Analysis
2.10. Western Blot Analysis
2.11. Glycosaminoglycan (GAG) Assay
2.12. Enzyme-Linked Immunosorbent Assay (ELISA)
2.13. Statistical Analysis
3. Results
3.1. ESM Exerted Pain-Alleviating Effects in MIA-Induced OA
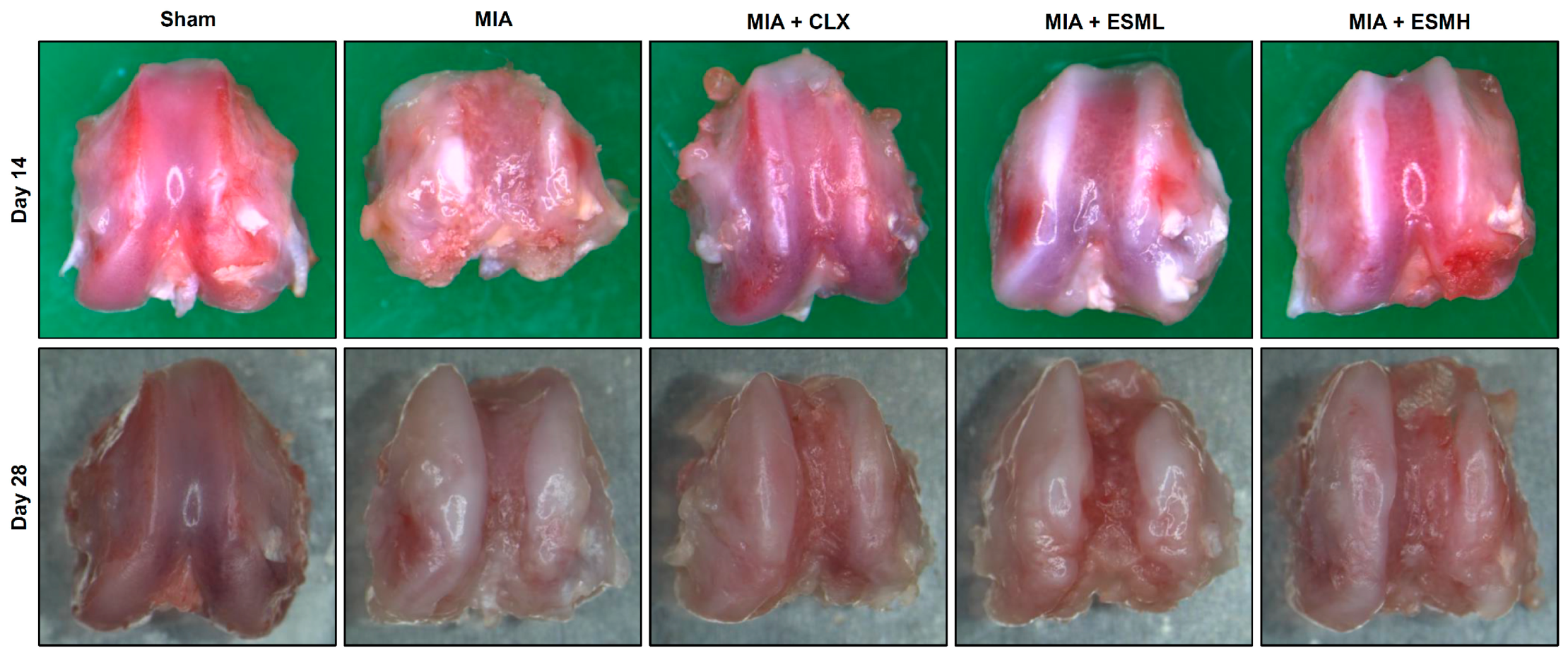
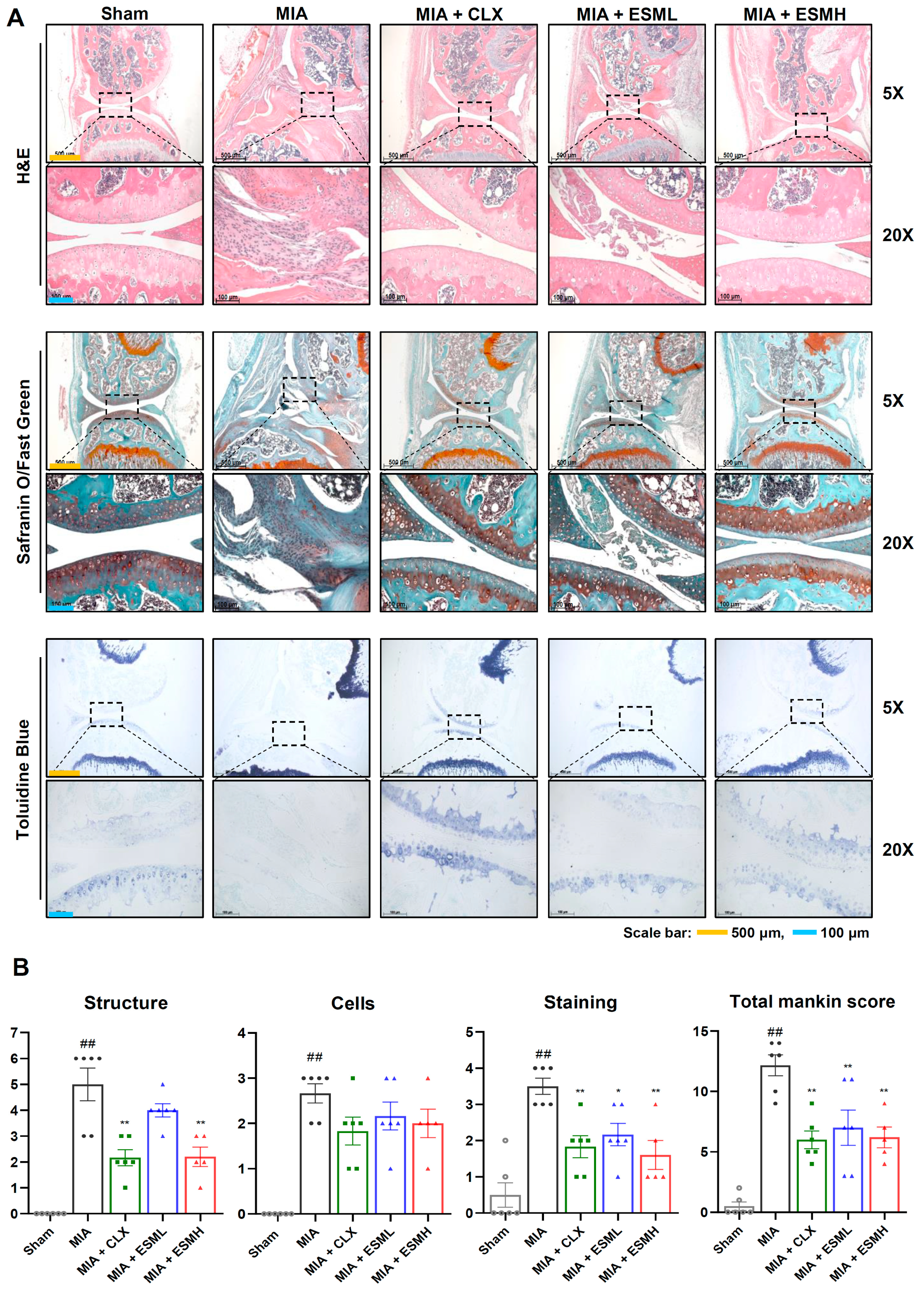
3.2. ESM Protects Articular Cartilage in MIA-Induced OA
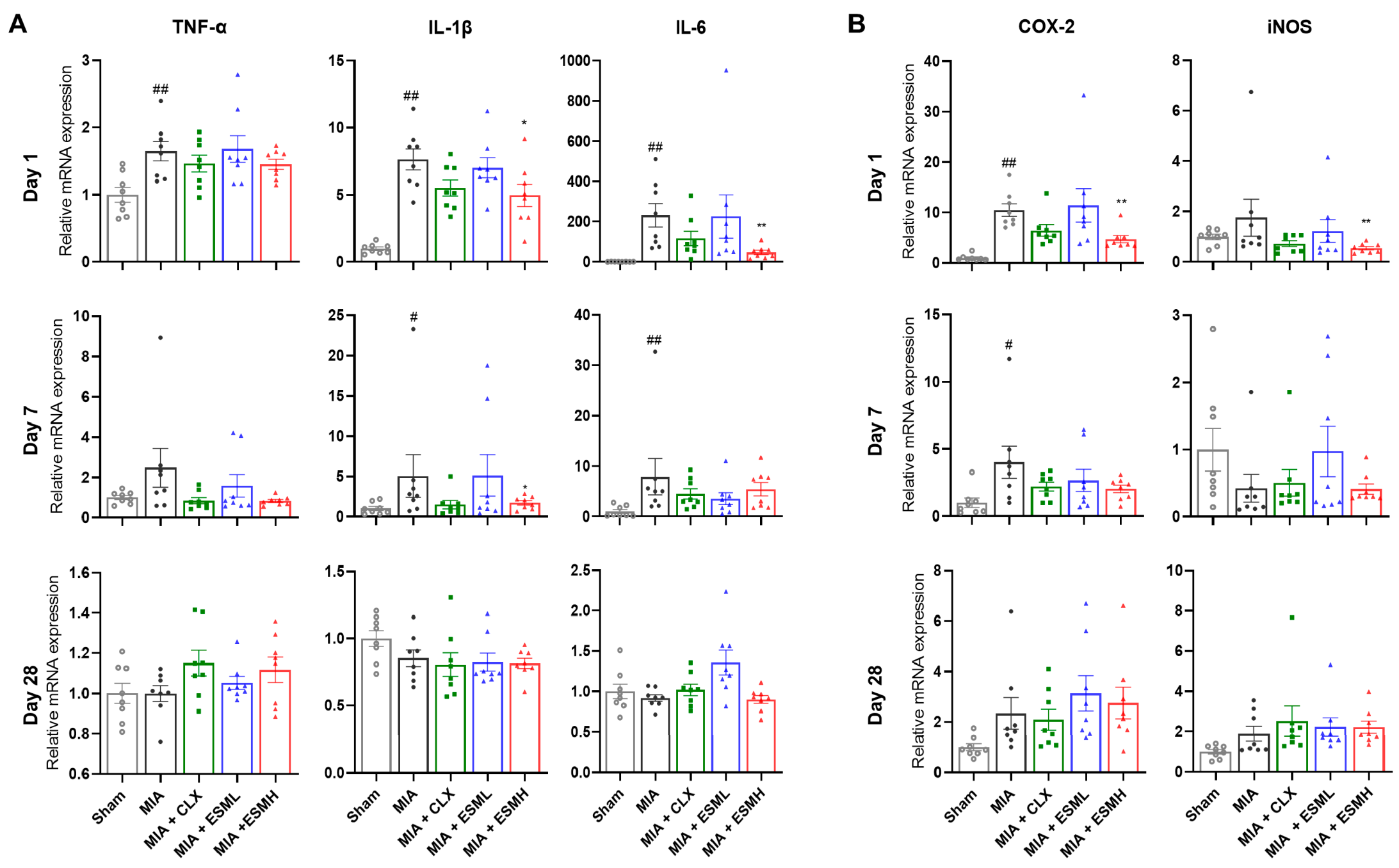
3.3. ESM Suppresses Early Inflammatory Responses in MIA-Induced OA
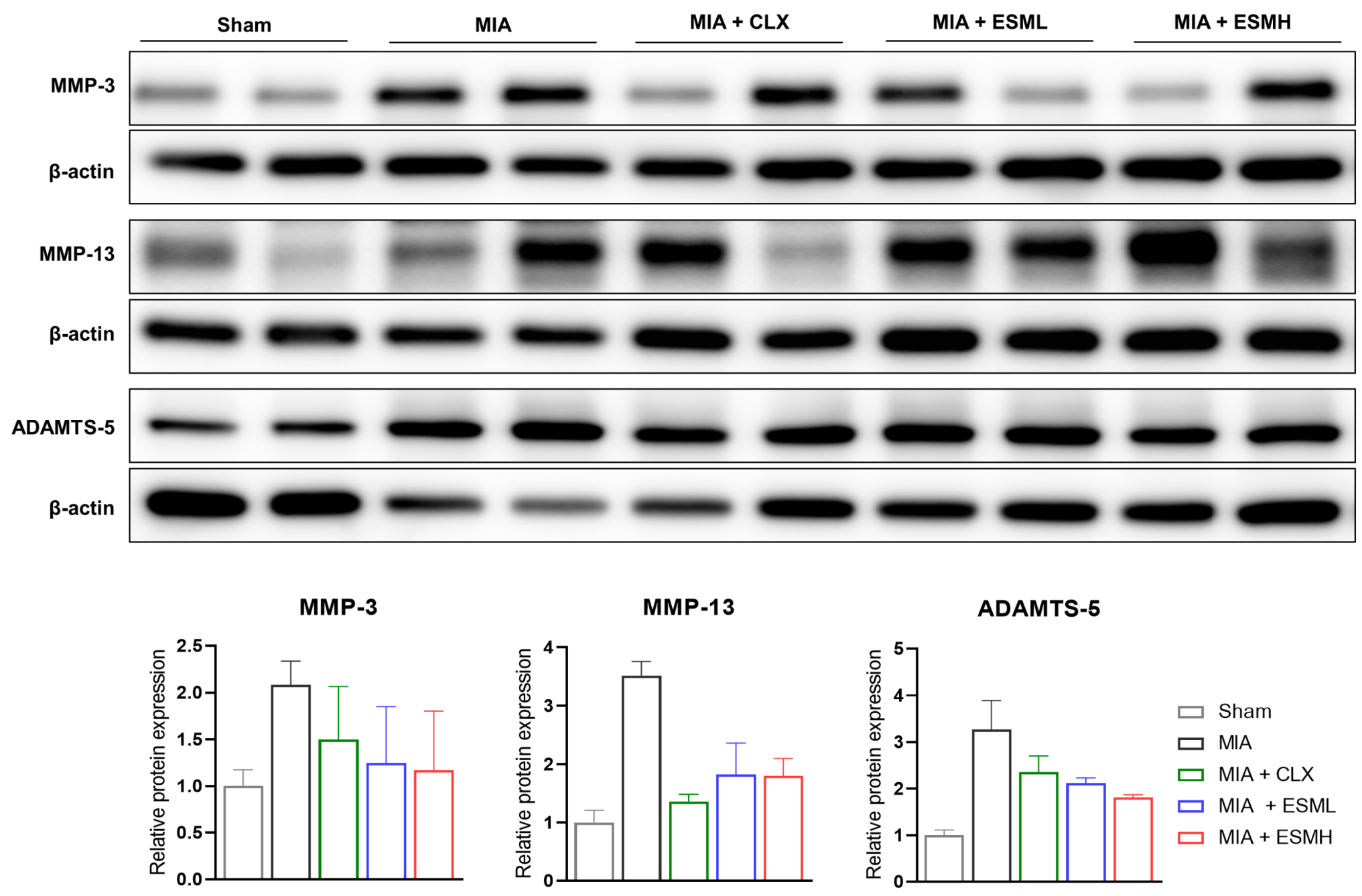
3.4. ESM Inhibits the Expression of Cartilage-Degrading Enzymes in the Late Stage of MIA-Induced OA
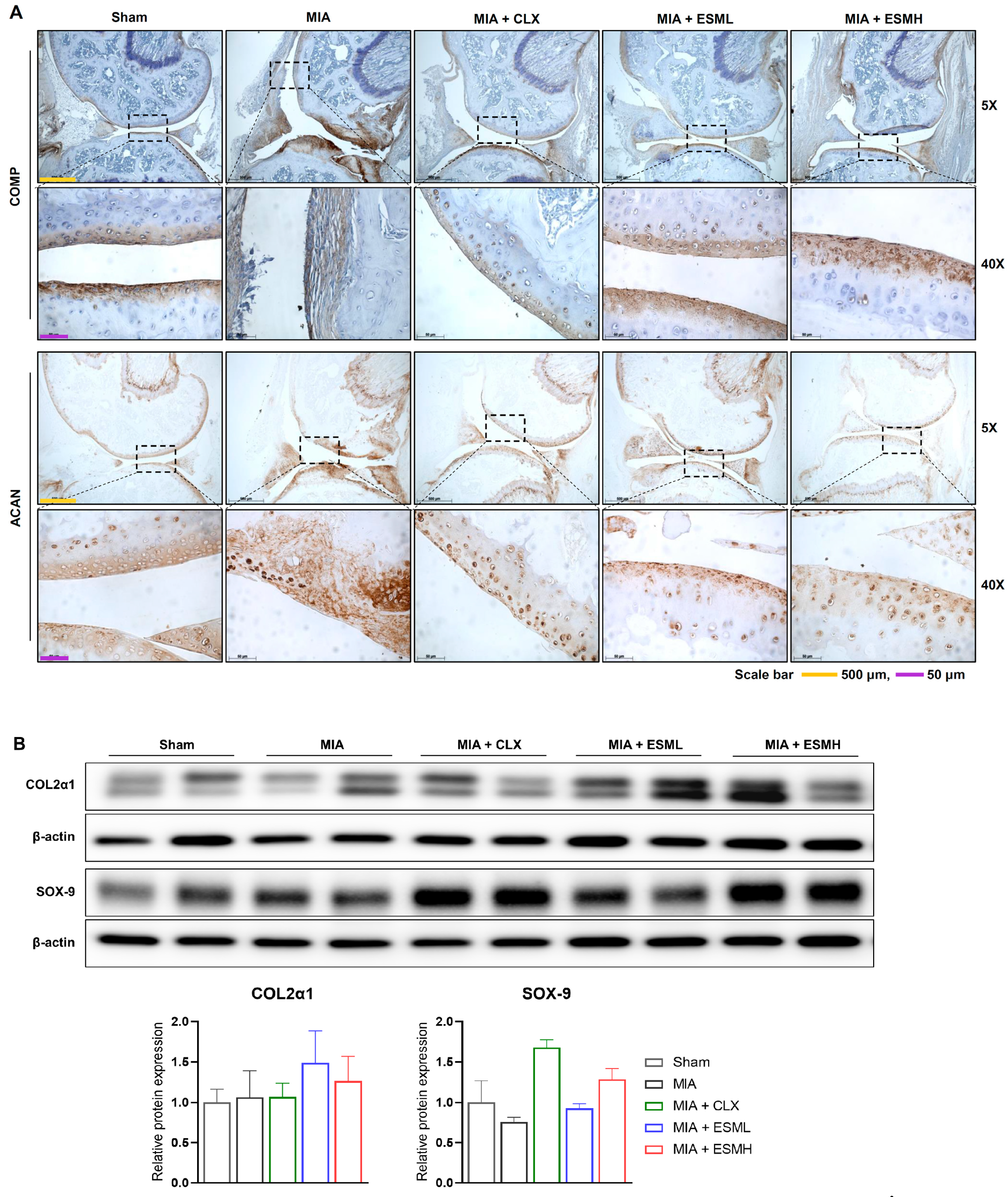
3.5. ESM Promotes Cartilage Repair in the Late Stage of MIA-Induced OA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Samuels, J.; Krasnokutsky, S.; Abramson, S.B. A tale of three tissues. Bull. NYU Hosp. 2008, 66, 244–250. [Google Scholar]
- Loeser, R.F.; Goldring, S.R.; Scanzello, C.R.; Goldring, M.B. Osteoarthritis: A disease of the joint as an organ. Arthritis Rheum. 2012, 64, 1697. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Liu, Q.; Yin, H.; Wang, K.; Diao, N.; Zhang, Y.; Lin, J.; Guo, A. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: Findings from the Global Burden of Disease Study 2019. Arthritis Rheumatol. 2022, 74, 1172–1183. [Google Scholar] [CrossRef] [PubMed]
- Cecchi, F.; Mannoni, A.; Molino-Lova, R.; Ceppatelli, S.; Benvenuti, E.; Bandinelli, S.; Lauretani, F.; Macchi, C.; Ferrucci, L. Epidemiology of hip and knee pain in a community based sample of Italian persons aged 65 and older. Osteoarthr. Cartil. 2008, 16, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Dominick, K.L.; Ahern, F.M.; Gold, C.H.; Heller, D.A. Health-related quality of life among older adults with arthritis. Health Qual. Life Outcomes 2004, 2, 5. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Zhang, Z.; Sheng, P.; Mobasheri, A. The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res. Rev. 2021, 66, 101249. [Google Scholar] [CrossRef] [PubMed]
- Buckwalter, J.; Mankin, H. Articular cartilage: Part I. J. Bone Jt. Surg. 1997, 79, 600. [Google Scholar] [CrossRef]
- Bhosale, A.M.; Richardson, J.B. Articular cartilage: Structure, injuries and review of management. Br. Med. Bull. 2008, 87, 77–95. [Google Scholar] [CrossRef] [PubMed]
- Eyre, D.R. Collagens and cartilage matrix homeostasis. Clin. Orthop. Relat. Res. 2004, 427, S118–S122. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.K.; Goodship, A.E. Tendon and ligament physiology: Responses to exercise and training. In Equine Exercise Physiology, the Science of Exercise in the Athletic Horse; Hinchcliff, K.W., Geor, R.J., Kanep, A.J., Eds.; Elsevier Ltd.: London, UK, 2008; pp. 106–131. [Google Scholar]
- Park, P.W. Proteoglycans. In Encyclopedia of Cell Biology (Second Edition); Bradshaw, R.A., Hart, G.W., Stahl, P.D., Eds.; Academic Press: Oxford, UK, 2023; pp. 335–344. [Google Scholar] [CrossRef]
- Goldring, M.B. The role of the chondrocyte in osteoarthritis. Arthritis Rheum. 2000, 43, 1916–1926. [Google Scholar] [CrossRef] [PubMed]
- Neefjes, M.; van Caam, A.P.; van der Kraan, P.M. Transcription factors in cartilage homeostasis and osteoarthritis. Biology 2020, 9, 290. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.-P.; Martel-Pelletier, J.; Rannou, F.; Cooper, C. Efficacy and safety of oral NSAIDs and analgesics in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Proc. Semin. Arthritis Rheum. 2016, 45, S22–S27. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, P.; Bhojani, K.; Joshi, V. NSAIDs and kidney. J. Assoc. Physicians India JAPI 2004, 52, 371. [Google Scholar]
- Henrotin, Y.; Mobasheri, A. Natural products for promoting joint health and managing osteoarthritis. Curr. Rheumatol. Rep. 2018, 20, 72. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.-H.; Lee, H.J.; Lee, C.J.; Park, J.-S. Natural products as sources of novel drug candidates for the pharmacological management of osteoarthritis: A narrative review. Biomol. Ther. 2019, 27, 503. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.A.; Suso, H.-P.; Hincke, M.T. In-depth comparative analysis of the chicken eggshell membrane proteome. J. Proteom. 2017, 155, 49–62. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio, C.; Arena, S.; Scaloni, A.; Guerrier, L.; Boschetti, E.; Mendieta, M.E.; Citterio, A.; Righetti, P.G. Exploring the chicken egg white proteome with combinatorial peptide ligand libraries. J. Proteome Res. 2008, 7, 3461–3474. [Google Scholar] [CrossRef] [PubMed]
- Leach Jr, R.M. Biochemistry of the organic matrix of the eggshell. Poult. Sci. 1982, 61, 2040–2047. [Google Scholar] [CrossRef]
- Shi, Y.; Zhou, K.; Li, D.; Guyonnet, V.; Hincke, M.T.; Mine, Y. Avian eggshell membrane as a novel biomaterial: A review. Foods 2021, 10, 2178. [Google Scholar] [CrossRef] [PubMed]
- Kulshreshtha, G.; Ahmed, T.A.; Wu, L.; Diep, T.; Hincke, M.T. A novel eco-friendly green approach to produce particalized eggshell membrane (PEM) for skin health applications. Biomater. Sci. 2020, 8, 5346–5361. [Google Scholar] [CrossRef] [PubMed]
- Vuong, T.T.; Rønning, S.B.; Suso, H.-P.; Schmidt, R.; Prydz, K.; Lundström, M.; Moen, A.; Pedersen, M.E. The extracellular matrix of eggshell displays anti-inflammatory activities through NF-κB in LPS-triggered human immune cells. J. Inflamm. Res. 2017, 10, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Kovacs-Nolan, J.; Jiang, B.; Tsao, R.; Mine, Y. Antioxidant activity of enzymatic hydrolysates from eggshell membrane proteins and its protective capacity in human intestinal epithelial Caco-2 cells. J. Funct. Foods 2014, 10, 35–45. [Google Scholar] [CrossRef]
- Shi, Y.; Kovacs-Nolan, J.; Jiang, B.; Tsao, R.; Mine, Y. Peptides derived from eggshell membrane improve antioxidant enzyme activity and glutathione synthesis against oxidative damage in Caco-2 cells. J. Funct. Foods 2014, 11, 571–580. [Google Scholar] [CrossRef]
- Jung, J.Y.; Yun, H.-C.; Kim, T.-M.; Joo, J.W.; Song, I.S.; Rah, Y.C.; Chang, J.; Im, G.J.; Choi, J. Analysis of effect of eggshell membrane patching for moderate-to-large traumatic tympanic membrane perforation. J. Audiol. Otol. 2017, 21, 39. [Google Scholar] [CrossRef] [PubMed]
- Ramli, N.S.; Jia, H.; Sekine, A.; Lyu, W.; Furukawa, K.; Saito, K.; Hasebe, Y.; Kato, H. Eggshell membrane powder lowers plasma triglyceride and liver total cholesterol by modulating gut microbiota and accelerating lipid metabolism in high-fat diet-fed mice. Food Sci. Nutr. 2020, 8, 2512–2523. [Google Scholar] [CrossRef] [PubMed]
- Vuong, T.T.; Rønning, S.B.; Ahmed, T.A.; Brathagen, K.; Høst, V.; Hincke, M.T.; Suso, H.-P.; Pedersen, M.E. Processed eggshell membrane powder regulates cellular functions and increase MMP-activity important in early wound healing processes. PLoS ONE 2018, 13, e0201975. [Google Scholar] [CrossRef] [PubMed]
- Ohto-Fujita, E.; Shimizu, M.; Sano, S.; Kurimoto, M.; Yamazawa, K.; Atomi, T.; Sakurai, T.; Murakami, Y.; Takami, T.; Murakami, T. Solubilized eggshell membrane supplies a type III collagen-rich elastic dermal papilla. Cell Tissue Res. 2019, 376, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Benson, K.F.; Ruff, K.J.; Jensen, G.S. Effects of natural eggshell membrane (NEM) on cytokine production in cultures of peripheral blood mononuclear cells: Increased suppression of tumor necrosis factor-α levels after in vitro digestion. J. Med. Food 2012, 15, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Ruff, K.J.; Morrison, D.; Duncan, S.A.; Back, M.; Aydogan, C.; Theodosakis, J. Beneficial effects of natural eggshell membrane versus placebo in exercise-induced joint pain, stiffness, and cartilage turnover in healthy, postmenopausal women. Clin. Interv. Aging 2018, 13, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Kiers, J.L.; Bult, J.H.F. Mildly processed natural eggshell membrane alleviates joint pain associated with osteoarthritis of the knee: A randomized double-blind placebo-controlled study. J. Med. Food 2021, 24, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Gil-Quintana, E.; Fenaux, M.; Nuez, M.; Molero, A.; Aguirre, A. Short-Term Effects of Ovomet®, Eggshell Membrane, in Joint Pain: A Double-Blind and Placebo Study. J. Osteopor. Phys. Act. 2018, 6, 1. [Google Scholar]
- Blasco, J.; Aguirre, A.; Gil-Quintana, E.; Fenaux, M. The effect of daily administration of 300 mg of Ovomet® for treatment of arthritis in elderly patients. Int. J. Clin. Rheumatol 2016, 11, 077–081. [Google Scholar]
- Aguirre, A.; Quintana, E.; Fenaux, M.; Erdozain, S.; Nuez, M. Effects of 50 Days Eggshell Membrane Ovomet® Supplementation on Biomechanics Parameters and Subjective Pain Perception Among Crossfit Athletes. A Preliminary Study. J. Trauma Treat. 2017, 6, 2. [Google Scholar] [CrossRef]
- Hewlings, S.; Kalman, D.; Schneider, L.V. A randomized, double-blind, placebo-controlled, prospective clinical trial evaluating water-soluble chicken eggshell membrane for improvement in joint health in adults with knee osteoarthritis. J. Med. Food 2019, 22, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Pillai, M.M.; Gopinathan, J.; Senthil Kumar, R.; Sathish Kumar, G.; Shanthakumari, S.; Sahanand, K.S.; Bhattacharyya, A.; Selvakumar, R. Tissue engineering of human knee meniscus using functionalized and reinforced silk-polyvinyl alcohol composite three-dimensional scaffolds: Understanding the in vitro and in vivo behavior. J. Biomed. Mater. Res. Part A 2018, 106, 1722–1731. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.B.; Jacob, S. A simple practice guide for dose conversion between animals and human. J. Basic Clin. Pharm. 2016, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Pitcher, T.; Sousa-Valente, J.; Malcangio, M. The monoiodoacetate model of osteoarthritis pain in the mouse. J. Vis. Exp. 2016, 111, 53746. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Yan, L.; Yan, B.; Zhou, L.; Tong, P.; Shan, L. Osteoarthritis pain model induced by intra-articular injection of mono-iodoacetate in rats. J. Vis. Exp. 2020, 159, e60649. [Google Scholar] [CrossRef] [PubMed]
- Marker, C.L.; Pomonis, J.D. The monosodium iodoacetate model of osteoarthritis pain in the rat. In Pain Research: Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2012; pp. 239–248. [Google Scholar]
- Morais, S.V.d.; Czeczko, N.G.; Malafaia, O.; Ribas Filho, J.M.; Garcia, J.B.S.; Miguel, M.T.; Zini, C.; Massignan, A.G. Osteoarthritis model induced by intra-articular monosodium iodoacetate in rats knee. Acta Cir. Bras. 2016, 31, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Mankin, H.J.; Dorfman, H.; Lippiello, L.; Zarins, A. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips: II. Correlation of morphology with biochemical and metabolic data. J. Bone Jt. Surg. JBJS 1971, 53, 523–537. [Google Scholar] [CrossRef]
- Sellam, J.; Berenbaum, F. The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat. Rev. Rheumatol. 2010, 6, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Požgan, U.; Caglič, D.; Rozman, B.; Nagase, H.; Turk, V.; Turk, B. Expression and activity profiling of selected cysteine cathepsins and matrix metalloproteinases in synovial fluids from patients with rheumatoid arthritis and osteoarthritis. Biol. Chem. 2010, 391, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Pritzker, K.P.; Gay, S.; Jimenez, S.; Ostergaard, K.; Pelletier, J.-P.; Revell, P.; Salter, D.; Van den Berg, W. Osteoarthritis cartilage histopathology: Grading and staging. Osteoarthr. Cartil. 2006, 14, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Sim, B.Y.; Bak, J.W.; Lee, H.J.; Jun, J.; Choi, H.J.; Kwon, C.J.; Kim, H.Y.; Ruff, K.J.; Brandt, K.; Kim, D.H. Effects of natural eggshell membrane (NEM) on monosodium iodoacetate-induced arthritis in rats. J. Nutr. Health 2015, 48, 310–318. [Google Scholar] [CrossRef]
- Zhu, L.; Ma, M.; Ahn, D.U.; Guyonnet, V.; Wang, L.; Zheng, Y.; He, Q.; Xiong, H.; Huang, X. Hatched Eggshell Membrane Can Be a Novel Source of Antioxidant Hydrolysates to Protect against H2O2-Induced Oxidative Stress in Human Chondrocytes. Antioxidants 2022, 11, 2428. [Google Scholar] [CrossRef] [PubMed]
- Oesser, S.; Seifert, J. Stimulation of type II collagen biosynthesis and secretion in bovine chondrocytes cultured with degraded collagen. Cell Tissue Res. 2003, 311, 393–399. [Google Scholar] [CrossRef] [PubMed]

| Species | Groups | Substance | Dose (mg/kg/day) | Volume (mL) |
|---|---|---|---|---|
| Mouse | Sham | Saline Saline | - | 0.1 0.1 |
| MIA | - | |||
| CLX | CLX | 20 | 0.1 | |
| ESML | ESM | 60 | 0.1 | |
| ESMH | ESM | 120 | 0.1 | |
| Rat | Sham | Saline | - | 1 |
| MIA | Saline | - | 1 | |
| CLX | CLX | 10 | 1 | |
| ESML | ESM | 30 | 1 | |
| ESMH | ESM | 60 | 1 |
| Gene | Forward/Reverse | Sequence (5′→3′) |
|---|---|---|
| TNF-α | Forward | AGGGTCTGGGCCATAGAACT |
| Reverse | CCACCACGCTCTTCTGTCTA | |
| IL-1β | Forward | CTCGCAGCAGCACATCAACAAG |
| Reverse | CCACGGGAAAGACACAGGTAGC | |
| IL-6 | Forward | ACAAAGCCAGAGTCCTTCAGAGAG |
| Reverse | TTGGATGGTCTTGGTCCTTAGCC | |
| COX-2 | Forward | TGAGCAACTATTCCAAACCAGC |
| Reverse | GCACGTAGTCTTCGATCACTATC | |
| iNOS | Forward | GAGACAGGGAAGTCTGAAGCAC |
| Reverse | CCAGCAGTAGTTGCTCCTCTTC | |
| β-actin | Forward | AGCCATGTACGTAGCCATCC |
| Reverse | CTCTCAGCTGTGGTGGTGAA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, M.; Park, C.; Son, Y.B.; Jo, S.E.; Jeon, S.H.; Kim, Y.J.; Han, S.B.; Hong, J.T.; Son, D.J. Time-Dependent Effect of Eggshell Membrane on Monosodium-Iodoacetate-Induced Osteoarthritis: Early-Stage Inflammation Control and Late-Stage Cartilage Protection. Nutrients 2024, 16, 1885. https://doi.org/10.3390/nu16121885
Yu M, Park C, Son YB, Jo SE, Jeon SH, Kim YJ, Han SB, Hong JT, Son DJ. Time-Dependent Effect of Eggshell Membrane on Monosodium-Iodoacetate-Induced Osteoarthritis: Early-Stage Inflammation Control and Late-Stage Cartilage Protection. Nutrients. 2024; 16(12):1885. https://doi.org/10.3390/nu16121885
Chicago/Turabian StyleYu, Min, Cheoljin Park, Young Bae Son, So Eun Jo, Seong Hee Jeon, Ye Jin Kim, Sang Bae Han, Jin Tae Hong, and Dong Ju Son. 2024. "Time-Dependent Effect of Eggshell Membrane on Monosodium-Iodoacetate-Induced Osteoarthritis: Early-Stage Inflammation Control and Late-Stage Cartilage Protection" Nutrients 16, no. 12: 1885. https://doi.org/10.3390/nu16121885
APA StyleYu, M., Park, C., Son, Y. B., Jo, S. E., Jeon, S. H., Kim, Y. J., Han, S. B., Hong, J. T., & Son, D. J. (2024). Time-Dependent Effect of Eggshell Membrane on Monosodium-Iodoacetate-Induced Osteoarthritis: Early-Stage Inflammation Control and Late-Stage Cartilage Protection. Nutrients, 16(12), 1885. https://doi.org/10.3390/nu16121885







