Chrono-Nutrition and Cardiometabolic Health: An Overview of Epidemiological Evidence and Key Future Research Directions
Abstract
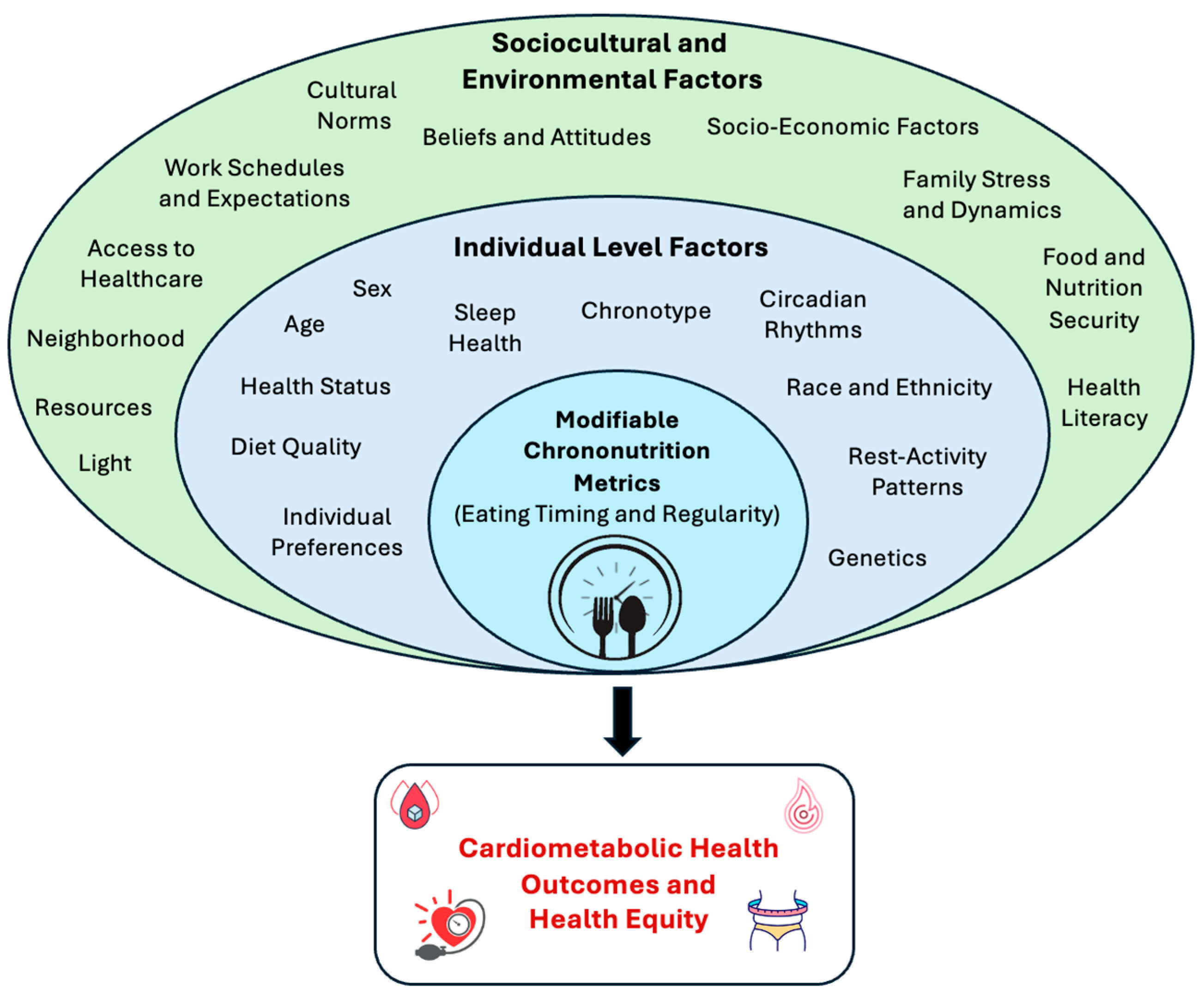
:1. Introduction
2. Eating Timing and Regularity Patterns in the US and Other Populations
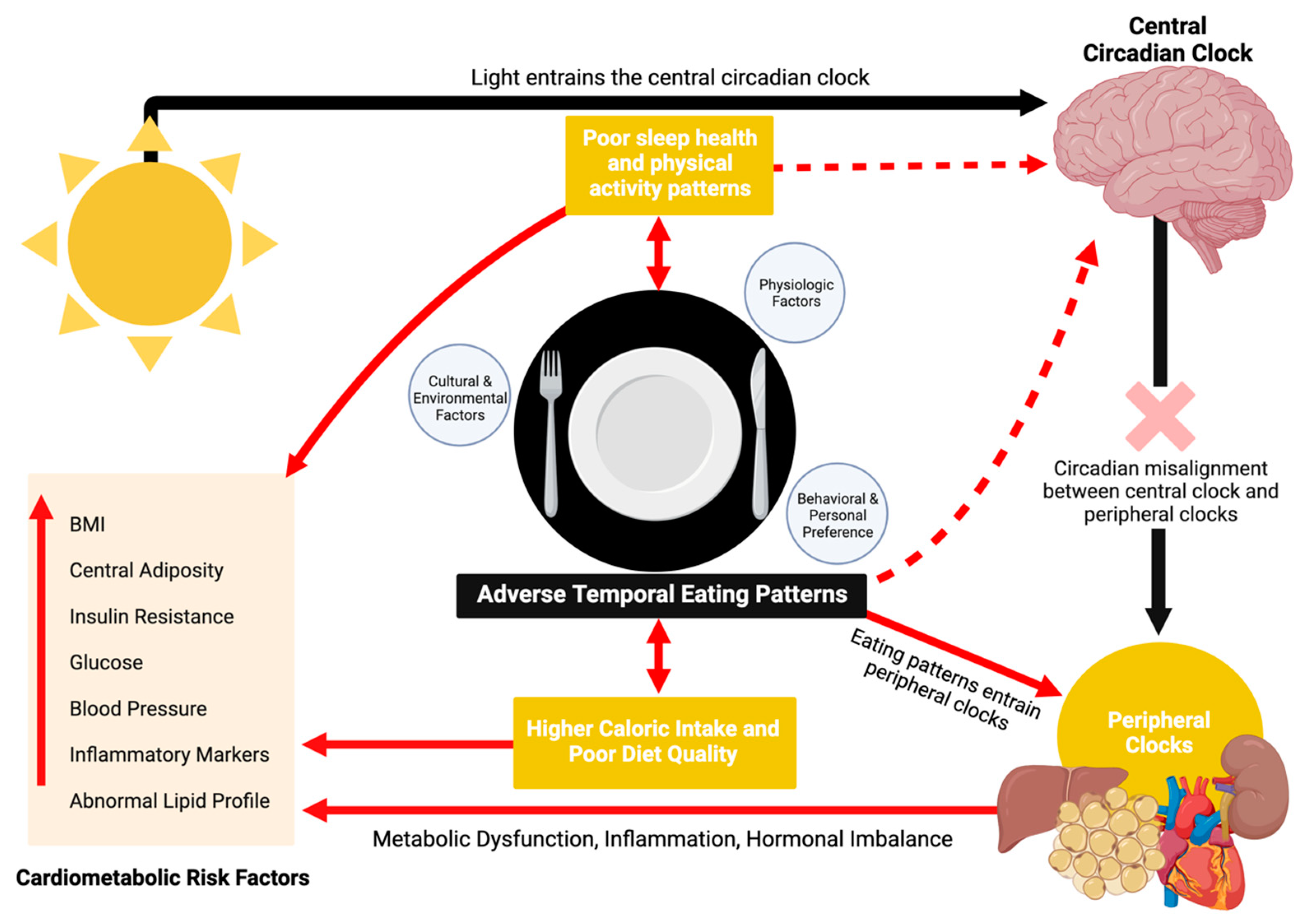
3. Overview of Mechanisms Linking Temporal Eating Patterns to Cardiometabolic Health
4. Summary of Observational Evidence
4.1. Breakfast Skipping and Timing of First Eating Occasion
4.2. Early Lunch vs. Late Lunch
4.3. Night Eating and Evening Caloric Intake
4.4. Eating Timing Variability and Eating Jetlag
5. Summary of Intervention Studies
5.1. Meal Skipping
5.2. Eating Timing
6. Research Gaps, Challenges, and Limitations
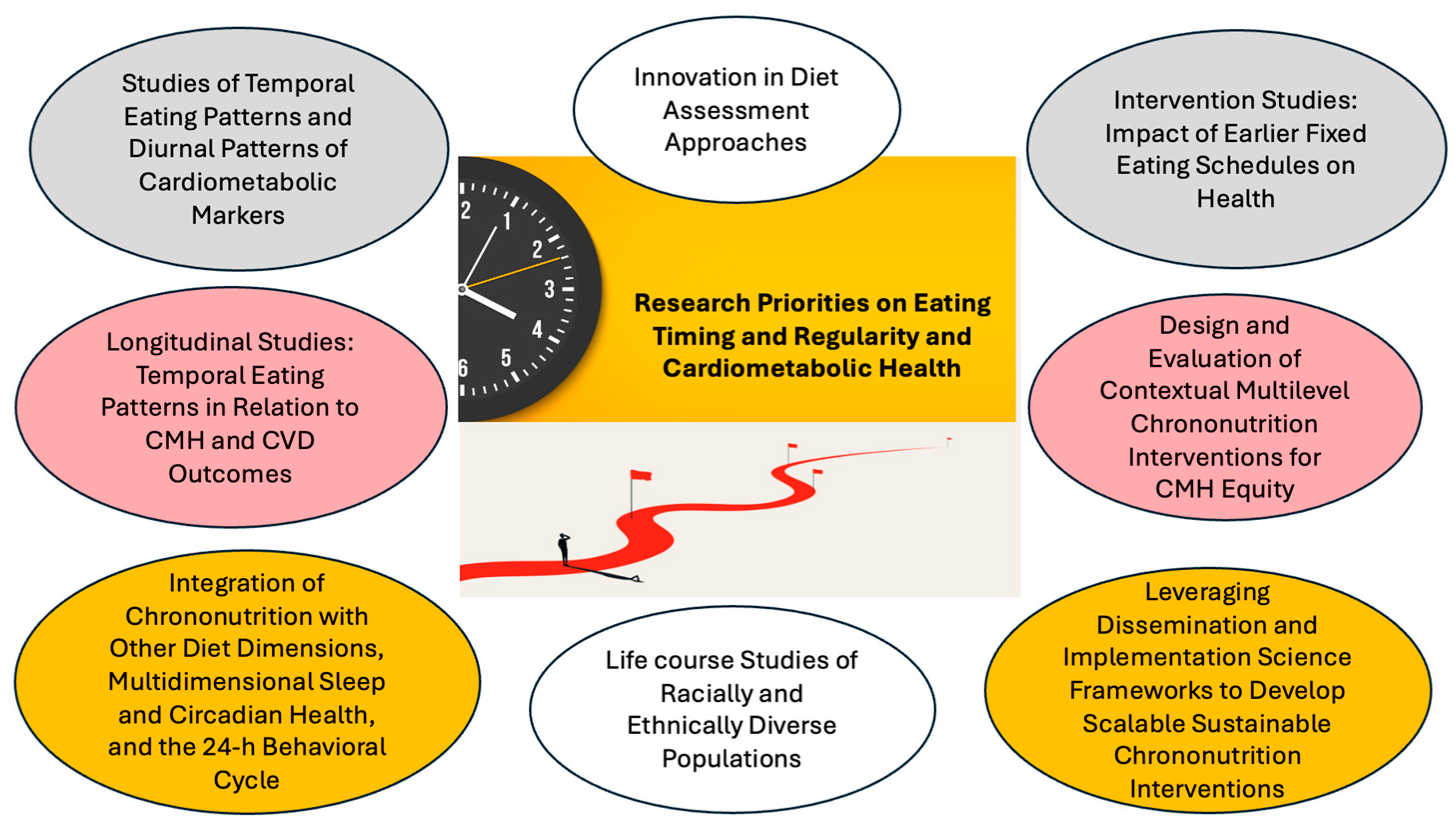
7. Research Priorities and Future Research Directions
8. Implications for Clinical Practice and Public Health Guidelines and Policy
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kessler, K.; Pivovarova-Ramich, O. Meal Timing, Aging, and Metabolic Health. Int. J. Mol. Sci. 2019, 20, 1911. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, A.; Bechtold, D.A.; Pot, G.K.; Johnston, J.D. Chrono-nutrition: From Molecular and Neuronal Mechanisms to Human Epidemiology and Timed Feeding Patterns. J. Neurochem. 2021, 157, 53–72. [Google Scholar] [CrossRef] [PubMed]
- Katsi, V.; Papakonstantinou, I.P.; Soulaidopoulos, S.; Katsiki, N.; Tsioufis, K. Chrononutrition in Cardiometabolic Health. J. Clin. Med. 2022, 11, 296. [Google Scholar] [CrossRef] [PubMed]
- Almoosawi, S.; Vingeliene, S.; Gachon, F.; Voortman, T.; Palla, L.; Johnston, J.D.; Van Dam, R.M.; Darimont, C.; Karagounis, L.G. Chronotype: Implications for Epidemiologic Studies on Chrono-Nutrition and Cardiometabolic Health. Adv. Nutr. 2019, 10, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Levin, S.; Barnard, N.D. Vegetarian Dietary Patterns and Cardiovascular Disease. Prog. Cardiovasc. Dis. 2018, 61, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Allen, N.B.; Anderson, C.A.M.; Black, T.; Brewer, L.C.; Foraker, R.E.; Grandner, M.A.; Lavretsky, H.; Perak, A.M.; Sharma, G.; et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation 2022, 146, 5. [Google Scholar] [CrossRef] [PubMed]
- Schuppelius, B.; Peters, B.; Ottawa, A.; Pivovarova-Ramich, O. Time Restricted Eating: A Dietary Strategy to Prevent and Treat Metabolic Disturbances. Front. Endocrinol. 2021, 12, 683140. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yi, P.; Liu, F. The Effect of Early Time-Restricted Eating vs Later Time-Restricted Eating on Weight Loss and Metabolic Health. J. Clin. Endocrinol. Metab. 2023, 108, 1824–1834. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Dietrich, M.; Brown, C.J.P.; Clark, C.A.; Block, G. The Effect of Breakfast Type on Total Daily Energy Intake and Body Mass Index: Results from the Third National Health and Nutrition Examination Survey (NHANES III). J. Am. Coll. Nutr. 2003, 22, 296–302. [Google Scholar] [CrossRef]
- Kant, A.K.; Graubard, B.I. 40-Year Trends in Meal and Snack Eating Behaviors of American Adults. J. Acad. Nutr. Diet. 2015, 115, 50–63. [Google Scholar] [CrossRef]
- Kutsuma, A.; Nakajima, K.; Suwa, K. Potential Association between Breakfast Skipping and Concomitant Late-Night-Dinner Eating with Metabolic Syndrome and Proteinuria in the Japanese Population. Scientifica 2014, 2014, 253581. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.; Song, Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients 2019, 11, 2437. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Kim, A.-S.; Ko, H.-J.; Choi, H.-I.; Hong, H.-E. Association between Breakfast Skipping and the Metabolic Syndrome: The Korea National Health and Nutrition Examination Survey, 2017. Medicina 2020, 56, 396. [Google Scholar] [CrossRef] [PubMed]
- Barragán, R.; Fernández-Carrión, R.; Asensio-Márquez, E.M.; Ortega-Azorín, C.; Álvarez-Sala, A.; Pérez-Fidalgo, A.; Sorlí, J.V.; Portolés, O.; González-Monje, I.; St-Onge, M.P.; et al. Timing of Meals and Sleep in the Mediterranean Population: The Effect of Taste, Genetics, Environmental Determinants, and Interactions on Obesity Phenotypes. Nutrients 2023, 15, 708. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K. Eating Patterns of US Adults: Meals, Snacks, and Time of Eating. Physiol. Behav. 2018, 193, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Huseinovic, E.; Winkvist, A.; Slimani, N.; Park, M.; Freisling, H.; Boeing, H.; Buckland, G.; Schwingshackl, L.; Weiderpass, E.; Rostgaard-Hansen, A.; et al. Meal Patterns across Ten European Countries—Results from the European Prospective Investigation into Cancer and Nutrition (EPIC) Calibration Study. Public Health Nutr. 2016, 19, 2769–2780. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Gómez-Abellán, P.; Alburquerque-Béjar, J.J.; Lee, Y.-C.; Ordovás, J.M.; Scheer, F.A.J.L. Timing of Food Intake Predicts Weight Loss Effectiveness. Int. J. Obes. 2013, 37, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.J.; Baron, K.G.; Zee, P.C. Meal Timing Influences Daily Caloric Intake in Healthy Adults. Nutr. Res. 2014, 34, 930–935. [Google Scholar] [CrossRef]
- Gill, S.; Panda, S. A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans That Can Be Modulated for Health Benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Franko, D.L.; Thompson, D.; Affenito, S.; Kraemer, H.C. Night Eating: Prevalence and Demographic Correlates. Obesity 2006, 14, 139–147. [Google Scholar] [CrossRef]
- Zerón-Rugerio, M.; Hernáez, Á.; Porras-Loaiza, A.; Cambras, T.; Izquierdo-Pulido, M. Eating Jet Lag: A Marker of the Variability in Meal Timing and Its Association with Body Mass Index. Nutrients 2019, 11, 2980. [Google Scholar] [CrossRef]
- Makarem, N.; Sears, D.D.; St-Onge, M.; Zuraikat, F.M.; Gallo, L.C.; Talavera, G.A.; Castaneda, S.F.; Lai, Y.; Aggarwal, B. Variability in Daily Eating Patterns and Eating Jetlag Are Associated with Worsened Cardiometabolic Risk Profiles in the American Heart Association Go Red for Women Strategically Focused Research Network. J. Am. Heart Assoc. 2021, 10, e022024. [Google Scholar] [CrossRef]
- Dashti, H.S.; Scheer, F.A.J.L.; Saxena, R.; Garaulet, M. Timing of Food Intake: Identifying Contributing Factors to Design Effective Interventions. Adv. Nutr. 2019, 10, 606–620. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Rehm, C.D.; Vieux, F. Breakfast in the United States: Food and Nutrient Intakes in Relation to Diet Quality in National Health and Examination Survey 2011–2014. A Study from the International Breakfast Research Initiative. Nutrients 2018, 10, 1200. [Google Scholar] [CrossRef]
- Johnson, D.A.; Cheng, P.; FarrHenderson, M.; Knutson, K. Understanding the Determinants of Circadian Health Disparities and Cardiovascular Disease. Chronobiol. Int. 2023, 40, 83–90. [Google Scholar] [CrossRef]
- Ansu Baidoo, V.Y.; Zee, P.C.; Knutson, K.L. Racial and Ethnic Differences in Eating Duration and Meal Timing: Findings from NHANES 2011–2018. Nutrients 2022, 14, 2428. [Google Scholar] [CrossRef]
- Schuler, B.R.; Bauer, K.W.; Lumeng, J.C.; Rosenblum, K.; Clark, M.; Miller, A.L. Poverty and Food Insecurity Predict Mealtime Structure: Mediating Pathways of Parent Disciplinary Practices and Depressive Symptoms. J. Child Fam. Stud. 2020, 29, 3169–3183. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Tan, Q.; Zhao, Y.; Zhao, J.; Zhang, Y.; Shi, D. Night Eating in Timing, Frequency, and Food Quality and Risks of All-Cause, Cancer, and Diabetes Mortality: Findings from National Health and Nutrition Examination Survey. Nutr. Diabetes 2024, 14, 5. [Google Scholar] [CrossRef]
- Lesani, A.; Barkhidarian, B.; Jafarzadeh, M.; Akbarzade, Z.; Djafarian, K.; Shab-Bidar, S. Time-Related Meal Patterns and Breakfast Quality in a Sample of Iranian Adults. BMC Nutr. 2023, 9, 13. [Google Scholar] [CrossRef] [PubMed]
- Vera, B.; Dashti, H.S.; Gómez-Abellán, P.; Hernández-Martínez, A.M.; Esteban, A.; Scheer, F.A.J.L.; Saxena, R.; Garaulet, M. Modifiable Lifestyle Behaviors, but Not a Genetic Risk Score, Associate with Metabolic Syndrome in Evening Chronotypes. Sci. Rep. 2018, 8, 945. [Google Scholar] [CrossRef]
- Garaulet, M.; Madrid, J.A. Chronobiological Aspects of Nutrition, Metabolic Syndrome and Obesity. Adv. Drug Deliv. Rev. 2010, 62, 967–978. [Google Scholar] [CrossRef] [PubMed]
- Makarem, N.; Zuraikat, F.M.; Caceres, B.; Sears, D.D.; St-Onge, M.-P.; Lai, Y.; Aggarwal, B. Variable Eating Patterns: A Potential Novel Risk Factor for Systemic Inflammation in Women. Ann. Behav. Med. 2023, 57, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Poggiogalle, E.; Jamshed, H.; Peterson, C.M. Circadian Regulation of Glucose, Lipid, and Energy Metabolism in Humans. Metabolism 2018, 84, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Ruddick-Collins, L.C.; Morgan, P.J.; Johnstone, A.M. Mealtime: A Circadian Disruptor and Determinant of Energy Balance? J. Neuroendocrinol. 2020, 32, e12886. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.A.J.L.; Hilton, M.F.; Mantzoros, C.S.; Shea, S.A. Adverse Metabolic and Cardiovascular Consequences of Circadian Misalignment. Proc. Natl. Acad. Sci. USA 2009, 106, 4453–4458. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Lopez-Minguez, J.; Dashti, H.S.; Vetter, C.; Hernández-Martínez, A.M.; Pérez-Ayala, M.; Baraza, J.C.; Wang, W.; Florez, J.C.; Scheer, F.A.J.L.; et al. Interplay of Dinner Timing and MTNR1B Type 2 Diabetes Risk Variant on Glucose Tolerance and Insulin Secretion: A Randomized Crossover Trial. Diabetes Care 2022, 45, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Colson, J.C.; Jin, C.; Becker, B.K.; Rhoads, M.K.; Pati, P.; Neder, T.H.; King, M.A.; Valcin, J.A.; Tao, B.; et al. Timing of Food Intake Drives the Circadian Rhythm of Blood Pressure. Function 2020, 2, zqaa034. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Purvis, T.E.; Hu, K.; Scheer, F.A.J.L. Circadian Misalignment Increases Cardiovascular Disease Risk Factors in Humans. Proc. Natl. Acad. Sci. USA 2016, 113, E1402–E1411. [Google Scholar] [CrossRef] [PubMed]
- Marinac, C.R.; Sears, D.D.; Natarajan, L.; Gallo, L.C.; Breen, C.I.; Patterson, R.E. Frequency and Circadian Timing of Eating May Influence Biomarkers of Inflammation and Insulin Resistance Associated with Breast Cancer Risk. PLoS ONE 2015, 10, e0136240. [Google Scholar] [CrossRef]
- Vujović, N.; Piron, M.J.; Qian, J.; Chellappa, S.L.; Nedeltcheva, A.; Barr, D.; Heng, S.W.; Kerlin, K.; Srivastav, S.; Wang, W.; et al. Late Isocaloric Eating Increases Hunger, Decreases Energy Expenditure, and Modifies Metabolic Pathways in Adults with Overweight and Obesity. Cell Metab. 2022, 34, 1486–1498.e7. [Google Scholar] [CrossRef]
- Garaulet, M.; Gómez-Abellán, P. Timing of Food Intake and Obesity: A Novel Association. Physiol. Behav. 2014, 134, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, J.L.; Musaad, S.M.; Holscher, H.D. Time of Day and Eating Behaviors Are Associated with the Composition and Function of the Human Gastrointestinal Microbiota. Am. J. Clin. Nutr. 2017, 106, 1220–1231. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Wainstein, J.; Landau, Z.; Raz, I.; Ahren, B.; Chapnik, N.; Ganz, T.; Menaged, M.; Barnea, M.; Bar-Dayan, Y.; et al. Influences of Breakfast on Clock Gene Expression and Postprandial Glycemia in Healthy Individuals and Individuals with Diabetes: A Randomized Clinical Trial. Diabetes Care 2017, 40, 1573–1579. [Google Scholar] [CrossRef] [PubMed]
- Collado, M.C.; Engen, P.A.; Bandín, C.; Cabrera-Rubio, R.; Voigt, R.M.; Green, S.J.; Naqib, A.; Keshavarzian, A.; Scheer, F.A.J.L.; Garaulet, M. Timing of Food Intake Impacts Daily Rhythms of Human Salivary Microbiota: A Randomized, Crossover Study. FASEB J. 2018, 32, 2060–2072. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Corbalán-Tutau, M.D.; Madrid, J.A.; Baraza, J.C.; Parnell, L.D.; Lee, Y.-C.; Ordovas, J.M. PERIOD2 Variants Are Associated with Abdominal Obesity, Psycho-Behavioral Factors, and Attrition in the Dietary Treatment of Obesity. J. Am. Diet. Assoc. 2010, 110, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Minguez, J.; Dashti, H.S.; Madrid-Valero, J.J.; Madrid, J.A.; Saxena, R.; Scheer, F.A.J.L.; Ordoñana, J.R.; Garaulet, M. Heritability of the Timing of Food Intake. Clin. Nutr. 2019, 38, 767–773. [Google Scholar] [CrossRef] [PubMed]
- De Castro, J.M. Heritability of Diurnal Changes in Food Intake in Free-Living Humans. Nutrition 2001, 17, 713–720. [Google Scholar] [CrossRef]
- Wilson, J.E.; Blizzard, L.; Gall, S.L.; Magnussen, C.G.; Oddy, W.H.; Dwyer, T.; Sanderson, K.; Venn, A.J.; Smith, K.J. An Eating Pattern Characterised by Skipped or Delayed Breakfast Is Associated with Mood Disorders among an Australian Adult Cohort. Psychol. Med. 2020, 50, 2711–2721. [Google Scholar] [CrossRef] [PubMed]
- Tahara, Y.; Makino, S.; Suiko, T.; Nagamori, Y.; Iwai, T.; Aono, M.; Shibata, S. Association between Irregular Meal Timing and the Mental Health of Japanese Workers. Nutrients 2021, 13, 2775. [Google Scholar] [CrossRef]
- Chang, Z.-S.; Boolani, A.; Conroy, D.A.; Dunietz, T.; Jansen, E.C. Skipping Breakfast and Mood: The Role of Sleep. Nutr. Health 2021, 27, 373–379. [Google Scholar] [CrossRef]
- Walker, W.H.; Walton, J.C.; DeVries, A.C.; Nelson, R.J. Circadian Rhythm Disruption and Mental Health. Transl. Psychiatry 2020, 10, 28. [Google Scholar] [CrossRef]
- Qian, J.; Vujovic, N.; Nguyen, H.; Rahman, N.; Heng, S.W.; Amira, S.; Scheer, F.A.J.L.; Chellappa, S.L. Daytime Eating Prevents Mood Vulnerability in Night Work. Proc. Natl. Acad. Sci. USA 2022, 119, e2206348119. [Google Scholar] [CrossRef]
- Pot, G.K. Sleep and Dietary Habits in the Urban Environment: The Role of Chrono-Nutrition. Proc. Nutr. Soc. 2018, 77, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Garrido, A.L.F.; Duarte, A.D.S.; Santana, P.T.; Rodrigues, G.H.; Pellegrino, P.; Nogueira, L.F.R.; Cipolla-Neto, J.; Moreno, C.R.D.C.; Marqueze, E.C. Eating Habits, Sleep, and a Proxy for Circadian Disruption Are Correlated with Dyslipidemia in Overweight Night Workers. Nutrition 2021, 83, 111084. [Google Scholar] [CrossRef]
- Chowdhury, E.A.; Richardson, J.D.; Holman, G.D.; Tsintzas, K.; Thompson, D.; Betts, J.A. The Causal Role of Breakfast in Energy Balance and Health: A Randomized Controlled Trial in Obese Adults. Am. J. Clin. Nutr. 2016, 103, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Roshanmehr, F.; Hayashi, K.; Tahara, Y.; Suiko, T.; Nagamori, Y.; Iwai, T.; Shibata, S. Association between Breakfast Meal Categories and Timing of Physical Activity of Japanese Workers. Foods 2022, 11, 2609. [Google Scholar] [CrossRef]
- Katagiri, R.; Asakura, K.; Kobayashi, S.; Suga, H.; Sasaki, S.; the Three-generation Study of Women on Diets and Health Study Group. Low Intake of Vegetables, High Intake of Confectionary, and Unhealthy Eating Habits Are Associated with Poor Sleep Quality among Middle-aged Female Japanese Workers. J. Occup. Health 2014, 56, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, E.; Kim, M.; Kim, W.G.; Yoon, J. Nutritional Aspects of Night Eating and Its Association with Weight Status among Korean Adolescents. Nutr. Res. Pract. 2016, 10, 448. [Google Scholar] [CrossRef] [PubMed]
- Cahill, L.E.; Chiuve, S.E.; Mekary, R.A.; Jensen, M.K.; Flint, A.J.; Hu, F.B.; Rimm, E.B. Prospective Study of Breakfast Eating and Incident Coronary Heart Disease in a Cohort of Male US Health Professionals. Circulation 2013, 128, 337–343. [Google Scholar] [CrossRef]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef]
- Deshmukh-Taskar, P.; Nicklas, T.A.; Radcliffe, J.D.; O’Neil, C.E.; Liu, Y. The Relationship of Breakfast Skipping and Type of Breakfast Consumed with Overweight/Obesity, Abdominal Obesity, Other Cardiometabolic Risk Factors and the Metabolic Syndrome in Young Adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr. 2013, 16, 2073–2082. [Google Scholar] [CrossRef] [PubMed]
- Witbracht, M.; Keim, N.L.; Forester, S.; Widaman, A.; Laugero, K. Female Breakfast Skippers Display a Disrupted Cortisol Rhythm and Elevated Blood Pressure. Physiol. Behav. 2015, 140, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Lloren, J.I.; Mashchak, A.; Hill, M.; Fraser, G.E. Meal Frequency and Timing Are Associated with Changes in Body Mass Index in Adventist Health Study 2. J. Nutr. 2017, 147, 1722–1728. [Google Scholar] [CrossRef] [PubMed]
- Min, C.; Noh, H.; Kang, Y.-S.; Sim, H.J.; Baik, H.W.; Song, W.O.; Yoon, J.; Park, Y.-H.; Joung, H. Skipping Breakfast Is Associated with Diet Quality and Metabolic Syndrome Risk Factors of Adults. Nutr. Res. Pract. 2011, 5, 455. [Google Scholar] [CrossRef] [PubMed]
- Makarem, N.; Sears, D.D.; St-Onge, M.-P.; Zuraikat, F.M.; Gallo, L.C.; Talavera, G.A.; Castaneda, S.F.; Lai, Y.; Mi, J.; Aggarwal, B. Habitual Nightly Fasting Duration, Eating Timing, and Eating Frequency Are Associated with Cardiometabolic Risk in Women. Nutrients 2020, 12, 3043. [Google Scholar] [CrossRef] [PubMed]
- Carew, A.S.; Mekary, R.A.; Kirkland, S.; Theou, O.; Siddiqi, F.; Urquhart, R.; George, M.; Blanchard, C.; Biggs, M.L.; Djoussé, L.; et al. Prospective Study of Breakfast Frequency and Timing and the Risk of Incident Type 2 Diabetes in Community-Dwelling Older Adults: The Cardiovascular Health Study. Am. J. Clin. Nutr. 2022, 116, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Palomar-Cros, A.; Andreeva, V.A.; Fezeu, L.K.; Julia, C.; Bellicha, A.; Kesse-Guyot, E.; Hercberg, S.; Romaguera, D.; Kogevinas, M.; Touvier, M.; et al. Dietary Circadian Rhythms and Cardiovascular Disease Risk in the Prospective NutriNet-Santé Cohort. Nat. Commun. 2023, 14, 7899. [Google Scholar] [CrossRef] [PubMed]
- Van Cauter, E.; Leproult, R.; Kupfer, D.J. Effects of Gender and Age on the Levels and Circadian Rhythmicity of Plasma Cortisol. J. Clin. Endocrinol. Metab. 1996, 81, 2468–2473. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.; Silver, R. Sex Differences in Circadian Timing Systems: Implications for Disease. Front. Neuroendocrinol. 2014, 35, 111–139. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, N.C.; Chrousos, G.P. Sex Differences in Circadian Endocrine Rhythms: Clinical Implications. Eur. J. Neurosci. 2020, 52, 2575–2585. [Google Scholar] [CrossRef]
- Xiao, Q.; Garaulet, M.; Scheer, F.A.J.L. Meal Timing and Obesity: Interactions with Macronutrient Intake and Chronotype. Int. J. Obes. 2019, 43, 1701–1711. [Google Scholar] [CrossRef]
- Dhurandhar, E.J.; Dawson, J.; Alcorn, A.; Larsen, L.H.; Thomas, E.A.; Cardel, M.; Bourland, A.C.; Astrup, A.; St-Onge, M.-P.; Hill, J.O.; et al. The Effectiveness of Breakfast Recommendations on Weight Loss: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 100, 507–513. [Google Scholar] [CrossRef]
- Betts, J.A.; Richardson, J.D.; Chowdhury, E.A.; Holman, G.D.; Tsintzas, K.; Thompson, D. The Causal Role of Breakfast in Energy Balance and Health: A Randomized Controlled Trial in Lean Adults. Am. J. Clin. Nutr. 2014, 100, 539–547. [Google Scholar] [CrossRef]
- Nas, A.; Mirza, N.; Hägele, F.; Kahlhöfer, J.; Keller, J.; Rising, R.; Kufer, T.A.; Bosy-Westphal, A. Impact of Breakfast Skipping Compared with Dinner Skipping on Regulation of Energy Balance and Metabolic Risk. Am. J. Clin. Nutr. 2017, 105, 1351–1361. [Google Scholar] [CrossRef]
- Ogata, H.; Kayaba, M.; Tanaka, Y.; Yajima, K.; Iwayama, K.; Ando, A.; Park, I.; Kiyono, K.; Omi, N.; Satoh, M.; et al. Effect of Skipping Breakfast for 6 Days on Energy Metabolism and Diurnal Rhythm of Blood Glucose in Young Healthy Japanese Males. Am. J. Clin. Nutr. 2019, 110, 41–52. [Google Scholar] [CrossRef]
- Geliebter, A.; Astbury, N.M.; Aviram-Friedman, R.; Yahav, E.; Hashim, S. Skipping Breakfast Leads to Weight Loss but Also Elevated Cholesterol Compared with Consuming Daily Breakfasts of Oat Porridge or Frosted Cornflakes in Overweight Individuals: A Randomised Controlled Trial. J. Nutr. Sci. 2014, 3, e56. [Google Scholar] [CrossRef] [PubMed]
- Farshchi, H.R.; Taylor, M.A.; Macdonald, I.A. Deleterious Effects of Omitting Breakfast on Insulin Sensitivity and Fasting Lipid Profiles in Healthy Lean Women1–3. Am. J. Clin. Nutr. 2005, 81, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Wainstein, J.; Ahren, B.; Landau, Z.; Bar-Dayan, Y.; Froy, O. Fasting Until Noon Triggers Increased Postprandial Hyperglycemia and Impaired Insulin Response After Lunch and Dinner in Individuals with Type 2 Diabetes: A Randomized Clinical Trial. Diabetes Care 2015, 38, 1820–1826. [Google Scholar] [CrossRef] [PubMed]
- Young, I.E.; Poobalan, A.; Steinbeck, K.; O’Connor, H.T.; Parker, H.M. Distribution of Energy Intake across the Day and Weight Loss: A Systematic Review and Meta-analysis. Obes. Rev. 2023, 24, e13537. [Google Scholar] [CrossRef]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. High Caloric Intake at Breakfast vs. Dinner Differentially Influences Weight Loss of Overweight and Obese Women: Effect of High-Calorie Breakfast vs. Dinner. Obesity 2013, 21, 2504–2512. [Google Scholar] [CrossRef]
- Jakubowicz, D.; Barnea, M.; Wainstein, J.; Froy, O. Effects of Caloric Intake Timing on Insulin Resistance and Hyperandrogenism in Lean Women with Polycystic Ovary Syndrome. Clin. Sci. 2013, 125, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Bandín, C.; Scheer, F.A.J.L.; Luque, A.J.; Ávila-Gandía, V.; Zamora, S.; Madrid, J.A.; Gómez-Abellán, P.; Garaulet, M. Meal Timing Affects Glucose Tolerance, Substrate Oxidation and Circadian-Related Variables: A Randomized, Crossover Trial. Int. J. Obes. 2015, 39, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, Y.; Hata, S.; Sone, Y. Effects of a Late Supper on Digestion and the Absorption of Dietary Carbohydrates in the Following Morning. J. Physiol. Anthropol. 2013, 32, 9. [Google Scholar] [CrossRef] [PubMed]
- Shams-White, M.M.; O’Connor, L.E.; O’Connor, S.G.; Herrick, K.A. Development of the Sleep Module for the Automated Self-Administered 24-Hour (ASA24) Dietary Assessment Tool: New Research Opportunities. J. Acad. Nutr. Diet. 2022, 122, 2017–2022. [Google Scholar] [CrossRef]
- Phoi, Y.Y.; Bonham, M.P.; Rogers, M.; Dorrian, J.; Coates, A.M. Content Validation of a Chrononutrition Questionnaire for the General and Shift Work Populations: A Delphi Study. Nutrients 2021, 13, 4087. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Mattis, J.; Sehgal, A. Circadian Rhythms, Sleep, and Disorders of Aging. Trends Endocrinol. Metab. 2016, 27, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Cornelissen, G.; Otsuka, K. Chronobiology of Aging: A Mini-Review. Gerontology 2017, 63, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short Sleep Duration and Dietary Intake: Epidemiologic Evidence, Mechanisms, and Health Implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Kingsbury, J.H.; Buxton, O.M.; Emmons, K.M.; Redline, S. Sleep and Its Relationship to Racial and Ethnic Disparities in Cardiovascular Disease. Curr. Cardiovasc. Risk Rep. 2013, 7, 387–394. [Google Scholar] [CrossRef]
- Makarem, N.; St-Onge, M.-P.; Liao, M.; Lloyd-Jones, D.M.; Aggarwal, B. Association of Sleep Characteristics with Cardiovascular Health among Women and Differences by Race/Ethnicity and Menopausal Status: Findings from the American Heart Association Go Red for Women Strategically Focused Research Network. Sleep Health 2019, 5, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Hale, L.; Troxel, W.; Buysse, D.J. Sleep Health: An Opportunity for Public Health to Address Health Equity. Annu. Rev. Public Health 2020, 41, 81–99. [Google Scholar] [CrossRef] [PubMed]
- Tumilowicz, A.; Ruel, M.T.; Pelto, G.; Pelletier, D.; Monterrosa, E.C.; Lapping, K.; Kraemer, K.; De Regil, L.M.; Bergeron, G.; Arabi, M.; et al. Implementation Science in Nutrition: Concepts and Frameworks for an Emerging Field of Science and Practice. Curr. Dev. Nutr. 2019, 3, nzy080. [Google Scholar] [CrossRef] [PubMed]
- The US Burden of Disease Collaborators; Mokdad, A.H.; Ballestros, K.; Echko, M.; Glenn, S.; Olsen, H.E.; Mullany, E.; Lee, A.; Khan, A.R.; Ahmadi, A.; et al. The State of US Health, 1990–2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA 2018, 319, 1444. [Google Scholar] [CrossRef]
| Chrono-Nutrition Metrics | Key Findings | Research Limitations and Future Directions |
|---|---|---|
| Breakfast Consumption | Breakfast skipping generally associated with higher risk of coronary heart disease, type 2 diabetes (higher glucose, insulin, and insulin resistance), hypertension, obesity (higher BMI and central adiposity), and hypercholesterolemia (higher total and LDL cholesterol levels and decreased HDL-cholesterol levels) [59,60,61,62,63]. Mixed evidence on weight, ranging from no impact of breakfast skipping on weight [55,72,73] to breakfast skipping leading to weight gain [75,76] or loss [78]. Breakfast skipping had an adverse effect on glycemic markers and insulin resistance [64,74,78]. | Observational data limitations:
|
| Timing of Breakfast or First Eating Occasion | Morning eating is associated with lower odds of metabolic syndrome, while later timing of first eating occasion is linked to poorer overall cardiovascular health, central adiposity, higher blood pressure, and poorer glycemic control [8,12,65,79]. Earlier timing of meals associated with lower CVD risk, particularly among women [65,67,80,81]. | |
| Timing of Lunch | Earlier timing of lunch linked to greater weight loss, better glycemic control, and lower insulin resistance [17,82]. | |
| Timing of Dinner or Last Eating Occasion and Extent of Evening Caloric Intake | Later eating timing and greater caloric intake in the evening linked to higher cardiovascular disease risk, metabolic syndrome, systemic inflammation, poorer glycemic control, and higher blood pressure [59,67,71,83]. | |
| Eating Regularity and Eating Jetlag | Increased day-to-day variability and weekday–weekend differences in timing of the first eating occasion, span of the daily eating period, and evening caloric intake is associated with higher BMI, waist circumference, blood pressure, and HbA1c [21,22]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raji, O.E.; Kyeremah, E.B.; Sears, D.D.; St-Onge, M.-P.; Makarem, N. Chrono-Nutrition and Cardiometabolic Health: An Overview of Epidemiological Evidence and Key Future Research Directions. Nutrients 2024, 16, 2332. https://doi.org/10.3390/nu16142332
Raji OE, Kyeremah EB, Sears DD, St-Onge M-P, Makarem N. Chrono-Nutrition and Cardiometabolic Health: An Overview of Epidemiological Evidence and Key Future Research Directions. Nutrients. 2024; 16(14):2332. https://doi.org/10.3390/nu16142332
Chicago/Turabian StyleRaji, Oluwatimilehin E., Esther B. Kyeremah, Dorothy D. Sears, Marie-Pierre St-Onge, and Nour Makarem. 2024. "Chrono-Nutrition and Cardiometabolic Health: An Overview of Epidemiological Evidence and Key Future Research Directions" Nutrients 16, no. 14: 2332. https://doi.org/10.3390/nu16142332






