Subcutaneous Semaglutide during Breastfeeding: Infant Safety Regarding Drug Transfer into Human Milk
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Acquisition, Dosing, and Reportable Info about Participating Women
2.2. Sample Preparation
2.3. Liquid Chromatography (LC)/Mass Spectrometry (MS)
2.4. Estimation of Relative Infant Dose (%)
3. Results
3.1. Mass Spectrometry of Semaglutide
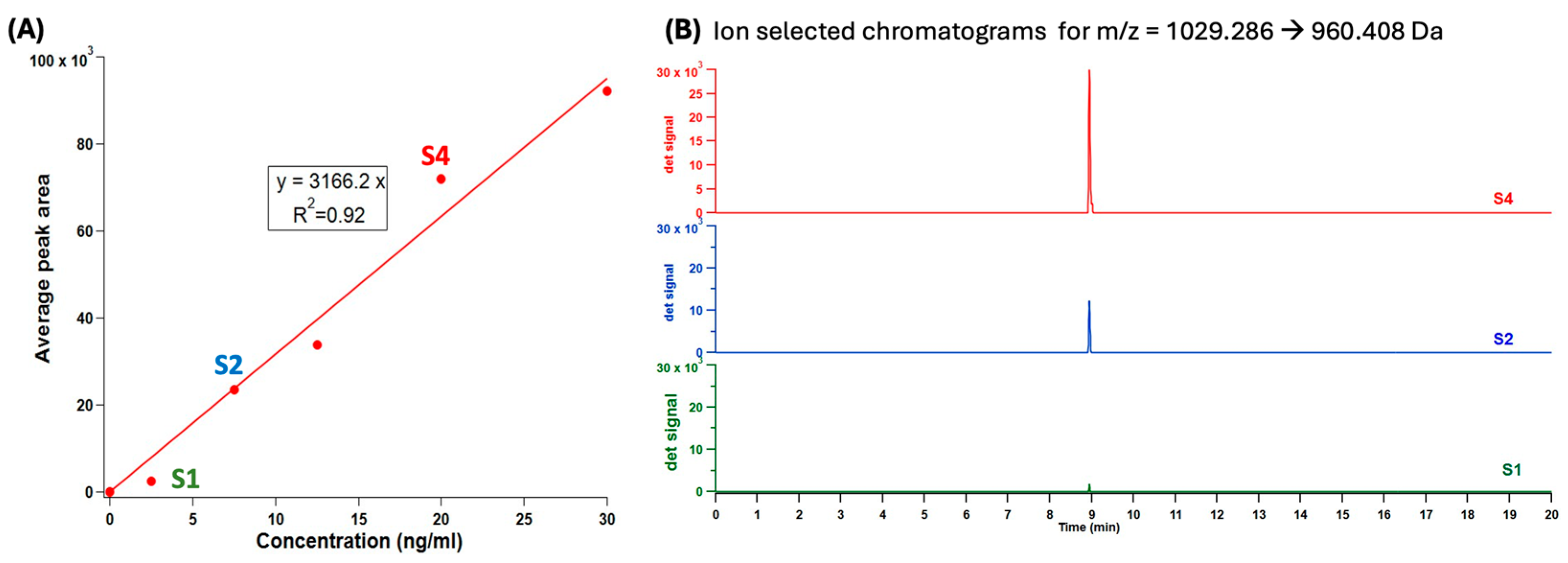
3.2. Chromatography and Figures of Merit
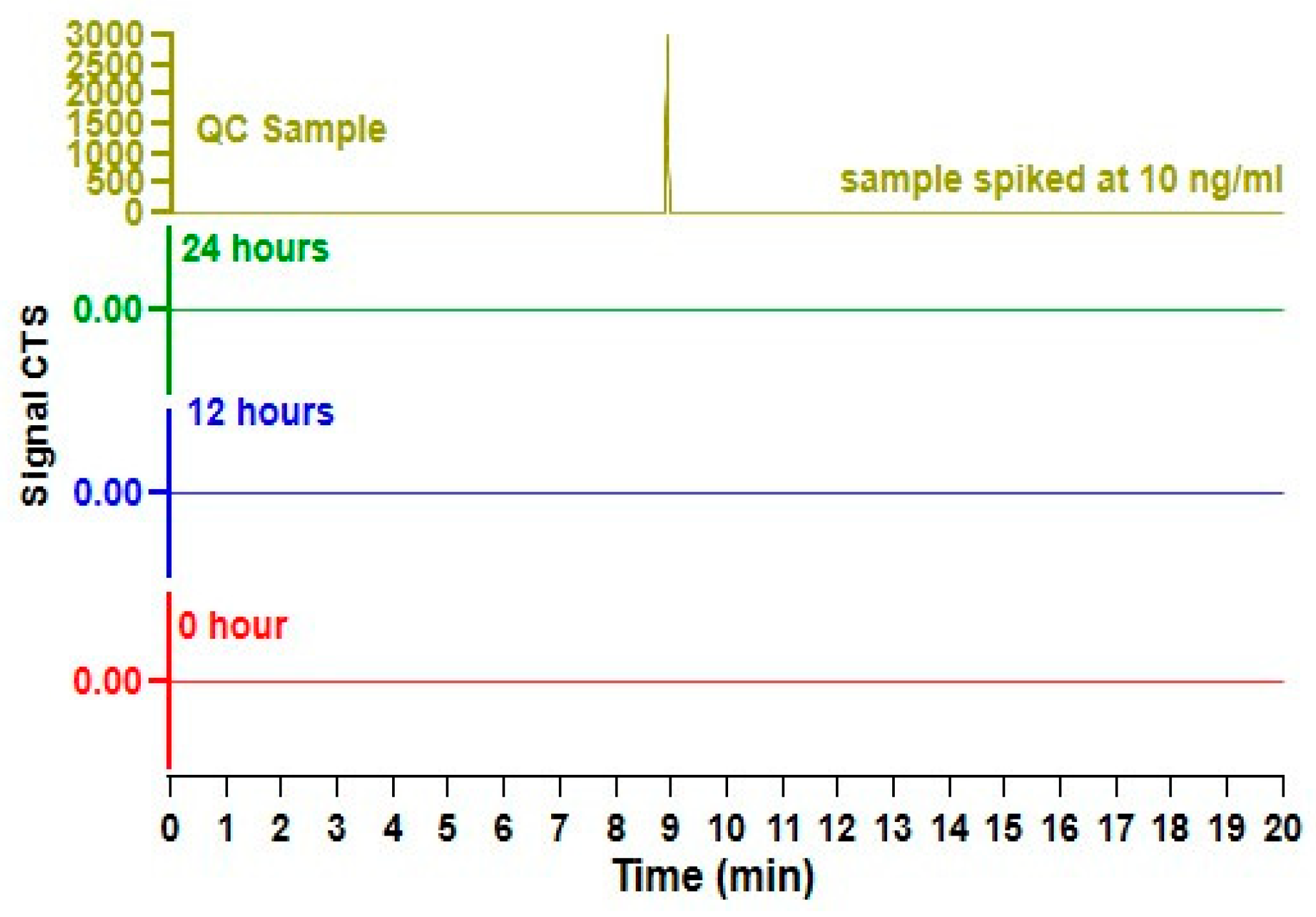
3.3. Analysis of Human Milk
3.4. Maternal and Infant Information
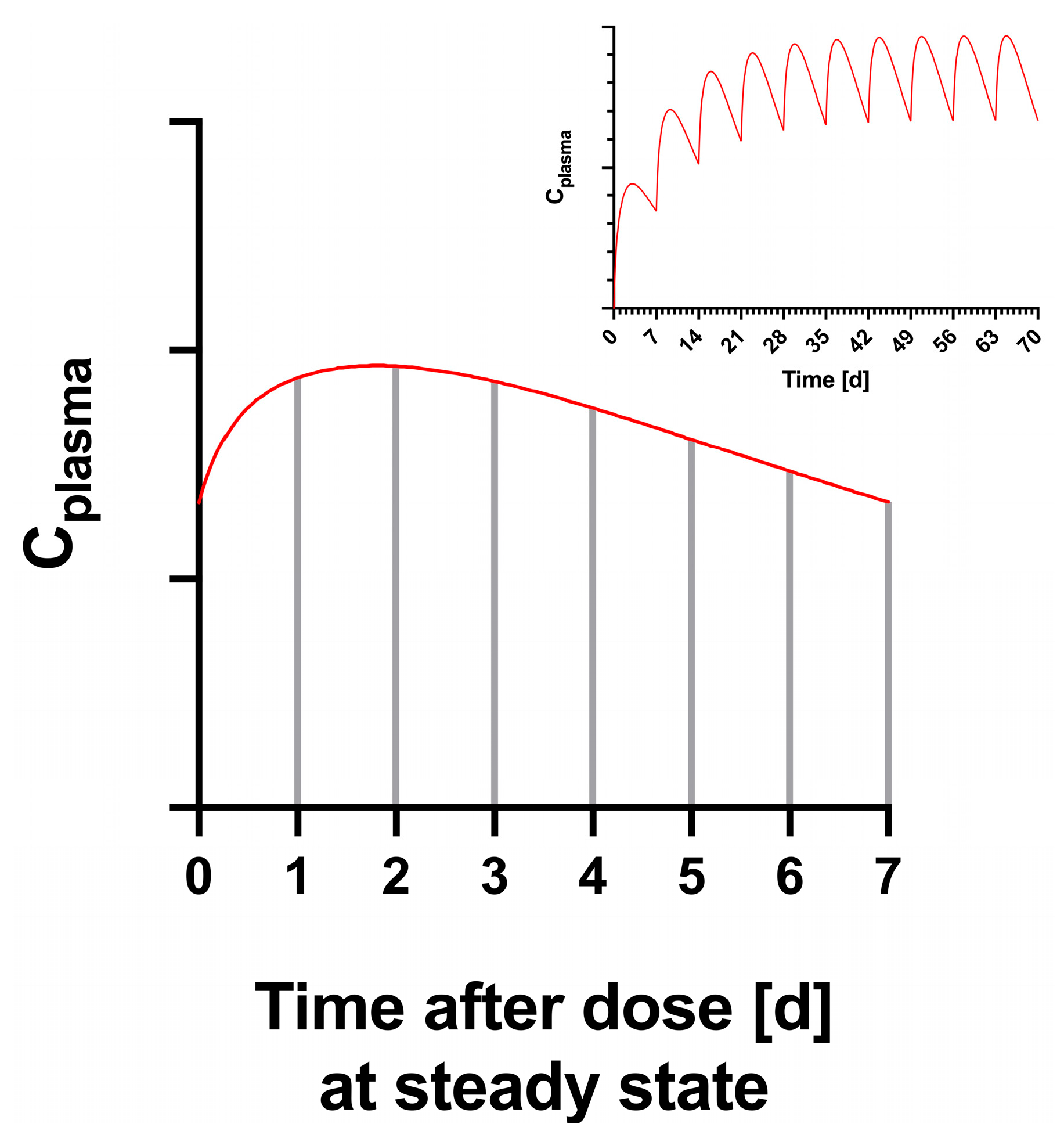
3.5. Pharmacokinetic Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lessen, R.; Kavanagh, K. Position of the Academy of Nutrition and Dietetics: Promoting and Supporting Breastfeeding. J. Acad. Nutr. Diet. 2015, 115, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.R.; Ling, P.R.; Blackburn, G.L. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients 2016, 8, 279. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US); Committee on Nutritional Status during Pregnancy and Lactation. Nutrition During Lactation; National Academies Press: Washington, DC, USA, 1991; Chapter 6. [Google Scholar]
- Savino, F.; Benetti, S.; Liguori, S.A.; Sorrenti, M.; Montezemolo, L.C.D. Advances on Human Milk Hormones and Protection against Obesity. Cell. Mol. Biol. 2013, 59, 89–98. [Google Scholar] [PubMed]
- Savino, F.; Liguori, S.A.; Fissore, M.F.; Oggero, R. Breast Milk Hormones and Their Protective Effect on Obesity. Int. J. Pediatr. Endocrinol. 2009, 2009, 327505. [Google Scholar] [CrossRef]
- Rooney, B.L.; Schauberger, C.W. Excess Pregnancy Weight Gain and Long-Term Obesity: One Decade Later. Obstet. Gynecol. 2002, 100, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.P.; Abrams, B.; Selvin, S. The Relative Importance of Gestational Gain and Maternal Characteristics Associated with the Risk of Becoming Overweight after Pregnancy. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1660–1668. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.Y.; Callaghan, W.M.; Bish, C.L.; D’Angelo, D. Gestational Weight Gain by Body Mass Index among US Women Delivering Live Births, 2004–2005: Fueling Future Obesity. Am. J. Obs. Gynecol. 2009, 200, 271.e1–271.e7. [Google Scholar] [CrossRef]
- Lim, S.; O’Reilly, S.; Behrens, H.; Skinner, T.; Ellis, I.; Dunbar, J.A. Effective Strategies for Weight Loss in Post-Partum Women: A Systematic Review and Meta-Analysis. Obes. Rev. 2015, 16, 972–987. [Google Scholar] [CrossRef]
- Lau, J.; Bloch, P.; Schäffer, L.; Pettersson, I.; Spetzler, J.; Kofoed, J.; Madsen, K.; Knudsen, L.B.; McGuire, J.; Steensgaard, D.B.; et al. Discovery of the Once-Weekly Glucagon-Like Peptide-1 (GLP-1) Analogue Semaglutide. J. Med. Chem. 2015, 58, 7370–7380. [Google Scholar] [CrossRef] [PubMed]
- Schueler, J.; Alexander, B.; Hart, A.M.; Austin, K.; Enette Larson-Meyer, D. Presence and Dynamics of Leptin, GLP-1, and PYY in Human Breast Milk at Early Postpartum. Obesity 2013, 21, 1451–1458. [Google Scholar] [CrossRef]
- Larson-Meyer, D.E.; Schueler, J.; Kyle, E.; Austin, K.J.; Hart, A.M.; Alexander, B.M. Appetite-Regulating Hormones in Human Milk: A Plausible Biological Factor for Obesity Risk Reduction? J. Hum. Lact. 2021, 37, 603–614. [Google Scholar] [CrossRef]
- Andersen, A.; Knop, F.K.; Vilsbøll, T. A Pharmacological and Clinical Overview of Oral Semaglutide for the Treatment of Type 2 Diabetes. Drugs 2021, 81, 1003. [Google Scholar] [CrossRef]
- Aroda., V.R.; Blonde, L.; Pratley, R. A new era for oral peptides: SNAC and the development of oral semaglutide for the treatment of type 2 diabetes. Rev. Endocrine Metab. Dis. 2022, 23, 979–994. [Google Scholar] [CrossRef] [PubMed]
- RYBELSUS® Results | RYBELSUS® (Semaglutide) Tablets 7 Mg or 14 Mg. Available online: https://www.rybelsus.com/why-rybelsus/rybelsus-results.html?showisi=true&gclid=67a23ac255cf1aa9e0335e2d30475c23&gclsrc=3p.ds&&utm_source=bing&utm_medium=cpc&utm_term=rybelsus%20medication&utm_campaign=1_All_Shared_BR_Core_Brand_2021_Refresh&utm_content=-dc_pcrid_74286018910037_pkw_rybelsus%20medication_pmt_be_slid__&msclkid=67a23ac255cf1aa9e0335e2d30475c23 (accessed on 8 May 2024).
- Buckley, S.T.; Bækdal, T.A.; Vegge, A.; Maarbjerg, S.J.; Pyke, C.; Ahnfelt-Rønne, J.; Madsen, K.G.; Schéele, S.G.; Alanentalo, T.; Kirk, R.K.; et al. Transcellular Stomach Absorption of a Derivatized Glucagon-like Peptide-1 Receptor Agonist. Sci. Transl. Med. 2018, 10, 7047. [Google Scholar] [CrossRef] [PubMed]
- Overgaard, R.V.; Hertz, C.L.; Ingwersen, S.H.; Navarria, A.; Drucker, D.J. Levels of Circulating Semaglutide Determine Reductions in HbA1c and Body Weight in People with Type 2 Diabetes. Cell Rep. Med. 2021, 2, 100387. [Google Scholar] [CrossRef] [PubMed]
- Weight-Loss Prescription Medication | Wegovy® (Semaglutide) Injection 2.4 Mg. Available online: https://www.wegovy.com/?showisi=true&gclid=b6c49bddc4191d8b1e28ff32567cdc9d&gclsrc=3p.ds&&utm_source=bing&utm_medium=cpc&utm_term=wegovy&utm_campaign=1_All_Shared_BR_Wegovy_Core&utm_content=_-mkwid-s_dc-pcrid--pkw-wegovy-pmt-e-&msclkid=b6c49bddc4191d8b1e28ff32567cdc9d (accessed on 8 May 2024).
- Novo Nordisk’s Blockbuster Ozempic Sales to Surge by 23% in 2023, Forecasts GlobalData—GlobalData. Available online: https://www.globaldata.com/media/pharma/novo-nordisks-blockbuster-ozempic-sales-surge-23-2023-forecasts-globaldata/ (accessed on 22 July 2024).
- Fighting Misinformation on Weight Loss Drugs and the Affect on Breastfeeding Moms | Springer Publishing. Available online: https://www.springerpub.com/blog/fighting-misinformation-on-weight-loss-drugs-the-affect-on-breastfeeding-moms/ (accessed on 8 May 2024).
- Blundell, J.; Finlayson, G.; Axelsen, M.; Flint, A.; Gibbons, C.; Kvist, T.; Hjerpsted, J.B. Effects of Once-Weekly Semaglutide on Appetite, Energy Intake, Control of Eating, Food Preference and Body Weight in Subjects with Obesity. Diabetes Obes. Metab. 2017, 19, 1242–1251. [Google Scholar] [CrossRef]
- Gabery, S.; Salinas, C.G.; Paulsen, S.J.; Ahnfelt-Rønne, J.; Alanentalo, T.; Baquero, A.F.; Buckley, S.T.; Farkas, E.; Fekete, C.; Frederiksen, K.S.; et al. Semaglutide Lowers Body Weight in Rodents via Distributed Neural Pathways. JCI Insight 2021, 5, e133429. [Google Scholar] [CrossRef] [PubMed]
- Verdich, C.; Toubro, S.; Buemann, B.; Lysgård Madsen, J.; Juul Holst, J.; Astrup, A. The Role of Postprandial Releases of Insulin and Incretin Hormones in Meal-Induced Satiety—Effect of Obesity and Weight Reduction. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 1206–1214. [Google Scholar] [CrossRef]
- Peterson, A.C.; Russell, J.D.; Bailey, D.J.; Westphall, M.S.; Coon, J.J. Parallel Reaction Monitoring for High Resolution and High Mass Accuracy Quantitative, Targeted Proteomics. Mol. Cell. Proteom. 2012, 11, 1475–1488. [Google Scholar] [CrossRef]
- Doerr, A. Targeting with PRM. Nat. Methods 2012, 9, 950. [Google Scholar] [CrossRef]
- Verstegen, R.H.J.; Anderson, P.O.; Ito, S. Infant Drug Exposure via Breast Milk. Br. J. Clin. Pharmacol. 2022, 88, 4311–4327. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.O.; Sauberan, J.B. Modeling Drug Passage into Human Milk. Clin. Pharmacol. Ther. 2016, 100, 42–52. [Google Scholar] [CrossRef]
- Larsen, E.R.; Damkier, P.; Pedersen, L.H.; Fenger-Gron, J.; Mikkelsen, R.L.; Nielsen, R.E.; Linde, V.J.; Knudsen, H.E.D.; Skaarup, L.; Videbech, P. Use of Psychotropic Drugs during Pregnancy and Breast-Feeding. Acta Psychiatr. Scand. 2015, 132, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Bennett, P.N.; Jensen, A.A. Drugs and Human Lactation: A Comprehensive Guide to the Content and Consequences of Drugs, Micronutrients, Radiopharmaceuticals, and Environmental and Occupational Chemicals in Human Milk; Elsevier: Amsterdam, The Netherlands, 1996; p. 712. [Google Scholar]
- Clinical Lactation Studies: Considerations for Study Design | FDA. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-lactation-studies-considerations-study-design (accessed on 14 August 2024).
- Ozempic Product Information. Available online: https://www.novo-pi.com/ozempic.pdf#guide (accessed on 22 July 2024).
- Rybelsus Product Guide. Available online: https://www.novo-pi.com/rybelsus.pdf#guide (accessed on 22 July 2024).
- Overgaard, R.V.; Delff, P.H.; Petri, K.C.C.; Anderson, T.W.; Flint, A.; Ingwersen, S.H. Population Pharmacokinetics of Semaglutide for Type 2 Diabetes. Diabetes Ther. 2019, 10, 649–662. [Google Scholar] [CrossRef] [PubMed]
- Jensen, L.; Helleberg, H.; Roffel, A.; van Lier, J.J.; Bjørnsdottir, I.; Pedersen, P.J.; Rowe, E.; Derving Karsbøl, J.; Pedersen, M.L. Absorption, Metabolism and Excretion of the GLP-1 Analogue Semaglutide in Humans and Nonclinical Species. Eur. J. Pharm. Sci. 2017, 104, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Kapitza, C.; Nosek, L.; Jensen, L.; Hartvig, H.; Jensen, C.B.; Flint, A. Semaglutide, a Once-Weekly Human GLP-1 Analog, Does Not Reduce the Bioavailability of the Combined Oral Contraceptive, Ethinylestradiol/Levonorgestrel. J. Clin. Pharmacol. 2015, 55, 497–504. [Google Scholar] [CrossRef]
- Marbury, T.C.; Flint, A.; Jacobsen, J.B.; Derving Karsbøl, J.; Lasseter, K. Pharmacokinetics and Tolerability of a Single Dose of Semaglutide, a Human Glucagon-Like Peptide-1 Analog, in Subjects With and Without Renal Impairment. Clin. Pharmacokinet. 2017, 56, 1381–1390. [Google Scholar] [CrossRef]
- Overgaard, R.V.; Navarria, A.; Ingwersen, S.H.; Bækdal, T.A.; Kildemoes, R.J. Clinical Pharmacokinetics of Oral Semaglutide: Analyses of Data from Clinical Pharmacology Trials. Clin. Pharmacokinet. 2021, 60, 1335–1348. [Google Scholar] [CrossRef]
- Jensen, L.; Kupcova, V.; Arold, G.; Pettersson, J.; Hjerpsted, J.B. Pharmacokinetics and Tolerability of Semaglutide in People with Hepatic Impairment. Diabetes Obes. Metab. 2018, 20, 998–1005. [Google Scholar] [CrossRef]
- Bækdal, T.A.; Thomsen, M.; Kupčová, V.; Hansen, C.W.; Anderson, T.W. Pharmacokinetics, Safety, and Tolerability of Oral Semaglutide in Subjects with Hepatic Impairment. J. Clin. Pharmacol. 2018, 58, 1314–1323. [Google Scholar] [CrossRef]
- Lee, T.S.; Park, E.J.; Choi, M.; Oh, H.S.; An, Y.; Kim, T.; Kim, T.H.; Shin, B.S.; Shin, S. Novel LC-MS/MS Analysis of the GLP-1 Analog Semaglutide with Its Application to Pharmacokinetics and Brain Distribution Studies in Rats. J. Chromatogr. B 2023, 1221, 123688. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.C.; Lucy, C.A. Quantitative Chemical Analysis, 10th ed.; Macmillan: New York, NY, USA, 2020; ISBN 9781319274016. [Google Scholar]
- Bartick, M.C.; Schwarz, E.B.; Green, B.D.; Jegier, B.J.; Reinhold, A.G.; Colaizy, T.T.; Bogen, D.L.; Schaefer, A.J.; Stuebe, A.M. Suboptimal Breastfeeding in the United States: Maternal and Pediatric Health Outcomes and Costs. Matern. Child Nutr. 2017, 13, e12366. [Google Scholar] [CrossRef] [PubMed]
- Fda Rybelsus (Semaglutide). Available online: https://www.fda.gov/RegulatoryInformation/Guidances/default.htm (accessed on 18 July 2024).
- Sahin, L. PRGLAC Overview: History & Current Status. In Proceedings of the Inaugural Stakeholder Meeting for the Prioritization of Therapeutic Research Needs for Pregnant, Postpartum and Lactating Persons, Bethesda, MD, USA, 9 July 2024. [Google Scholar]
- Bertrand, K.; Kelly, A.; Chambers, C.D. The Prevalence of Nonserious Events in a Cohort of Breastfed Infants. Breastfeed Med. 2023, 18, 43–47. [Google Scholar] [CrossRef]
- Heryl, C.; Ovelady, A.L.; Arner, I.E.G.; Erri, K.; Oreno, L.M.; Ohn, J.; Illiams, P.W. The Effect of Weight Loss in Overweight, Lactating Women on the Growth of Their Infants. N. Engl. J. Med. 2000, 342, 449–453. [Google Scholar] [CrossRef]
- Dror, D.K.; Allen, L.H. Overview of Nutrients in Human Milk. Adv. Nutr. 2018, 9, 278S–294S. [Google Scholar] [CrossRef]
- Holst, J.J. The Physiology of Glucagon-like Peptide 1. Physiol. Rev. 2007, 87, 1409–1439. [Google Scholar] [CrossRef] [PubMed]

| Participant | SubQ Dose (mg/Week) | Semaglutide (0 h) | Semaglutide (12 h) | Semaglutide (24 h) |
|---|---|---|---|---|
| 1 | 0.5 | n.d. | n.d. | n.d. |
| 2 | 0.5 | n.d. | n.d. | n.d. |
| 3 | 0.25 | n.d. | n.d. | n.d. |
| 4 | 0.5 | n.d. | n.d. | n.d. |
| 5 | 0.25 | n.d. | n.d. | n.d. |
| 6 | 1 | n.d. | n.d. | n.d. |
| 7 | 0.5 | n.d. | n.d. | n.d. |
| 8 * | 1 | n.d. | n.d. | n.d. |
| Participant | Self-Reported Race | Weight (kg) | Dose Per Week | Maternal History | Maternal Meds | Infant History | Infant Age | Infant Diet | Infant Growth | Infant Milestones | Duration Infant Exposed to Milk with Semaglutide | Potentially Related Infant Adverse Events |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | white/caucasian | 107 | 0.5 | asthma, epilepsy, migraines, pcos, reynaud’s | prenatal, vitamin d, omega 3 fish oil, | dairy intolerance, poor growth until dairy removed from diet | 12–23 months | breastmilk, water, solid foods (never formula) | average weight, height head circumference | right on track | 4+ weeks | none |
| 2 | black & white | 98 | 0.5 | asthma, anxiety, depression GERD, gestational diabetes, PCOS | prenantal | none | 7 to 11 months | breastmilk, water, solid foods (never formula) | average weight, height head circumference | right on track | 4+ weeks | none |
| 3 | white | 79 | 0.25 | anemia, anxiety | none | dairy intolerance, frequent ear infection | 7 to 11 months | breastmilk and some solid food (never forumla) | average weight and height, head circumference above average | surpassing expectations | 4+ weeks | none |
| 4 | biracial (black/white) | 112 | 0.5 | infertility, PCOS | none | none | 4 to 6 months | breastmilk and some rice cereal (never foruma, never solids) | average weight, height, and head circumference | right on track | 9 weeks, interrupted | none |
| 5 | not reported | 95 | 0.25 | anxiety, asthma, depression, IBS | cetirizine, fluoxetine, buproprion, linaclotide, naltrexone | none | 7 to 11 months | breastmilk, water, solid foods (never formula) | average weight, height, and head circumference | right on track | 3+ weeks | none |
| 6 | white, non hispanic | 97 | 1 | migraines | none | none | 12–23 months | breastmilk, water, juice, solid foods (never formula) | average weight, height, and head circumference | surpassing expectations | 3+ weeks | possible diarrhea, possible decreased appetite (transient, resolved) |
| 7 | Black/African decent | 83 | 0.5 | anemia, anxiety, depression, high blood pressure, high cholesterol | Bupropion, desvenlafaxine, metformin | none | 4 to 6 months | breastmilk every day, solid foods and formula on some days | average weight and height, head circumference well above average | right on track | 4+ weeks | none |
| 8 * | Mixed (Korean & White) | 72 | 1 | anxiety, depression, gestational diabetes, high cholesterol, PCOS | amphetamine salts, zolpidem, sertraline, alcaftadine eyedrops | none | 12–23 months | breastmilk, formula, water, solid food every day | average weight, height, and head circumference | right on track | 6+ weeks | none |
| Parameter | Mean Value |
|---|---|
| Maternal Weight (kg) | 93 |
| Dose (mg/week) | 0.56 |
| Cavg | n.d. |
| Cmax | n.d. |
| Tmax | unknown |
| LLOQ (ng/mL) | 5.7 |
| RIDF (%) | <1.12 |
| RIDFP (%) | <1.26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diab, H.; Fuquay, T.; Datta, P.; Bickel, U.; Thompson, J.; Krutsch, K. Subcutaneous Semaglutide during Breastfeeding: Infant Safety Regarding Drug Transfer into Human Milk. Nutrients 2024, 16, 2886. https://doi.org/10.3390/nu16172886
Diab H, Fuquay T, Datta P, Bickel U, Thompson J, Krutsch K. Subcutaneous Semaglutide during Breastfeeding: Infant Safety Regarding Drug Transfer into Human Milk. Nutrients. 2024; 16(17):2886. https://doi.org/10.3390/nu16172886
Chicago/Turabian StyleDiab, Hanin, Taylor Fuquay, Palika Datta, Ulrich Bickel, Jonathan Thompson, and Kaytlin Krutsch. 2024. "Subcutaneous Semaglutide during Breastfeeding: Infant Safety Regarding Drug Transfer into Human Milk" Nutrients 16, no. 17: 2886. https://doi.org/10.3390/nu16172886
APA StyleDiab, H., Fuquay, T., Datta, P., Bickel, U., Thompson, J., & Krutsch, K. (2024). Subcutaneous Semaglutide during Breastfeeding: Infant Safety Regarding Drug Transfer into Human Milk. Nutrients, 16(17), 2886. https://doi.org/10.3390/nu16172886







