Intakes of Lean Proteins and Processed Meats and Differences in Mental Health between Rural and Metro Adults 50 Years and Older
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Statistical Analyses
3. Results
3.1. Descriptive Statistics
3.2. Comparisons between Those Residing in Rural versus Metro Counties
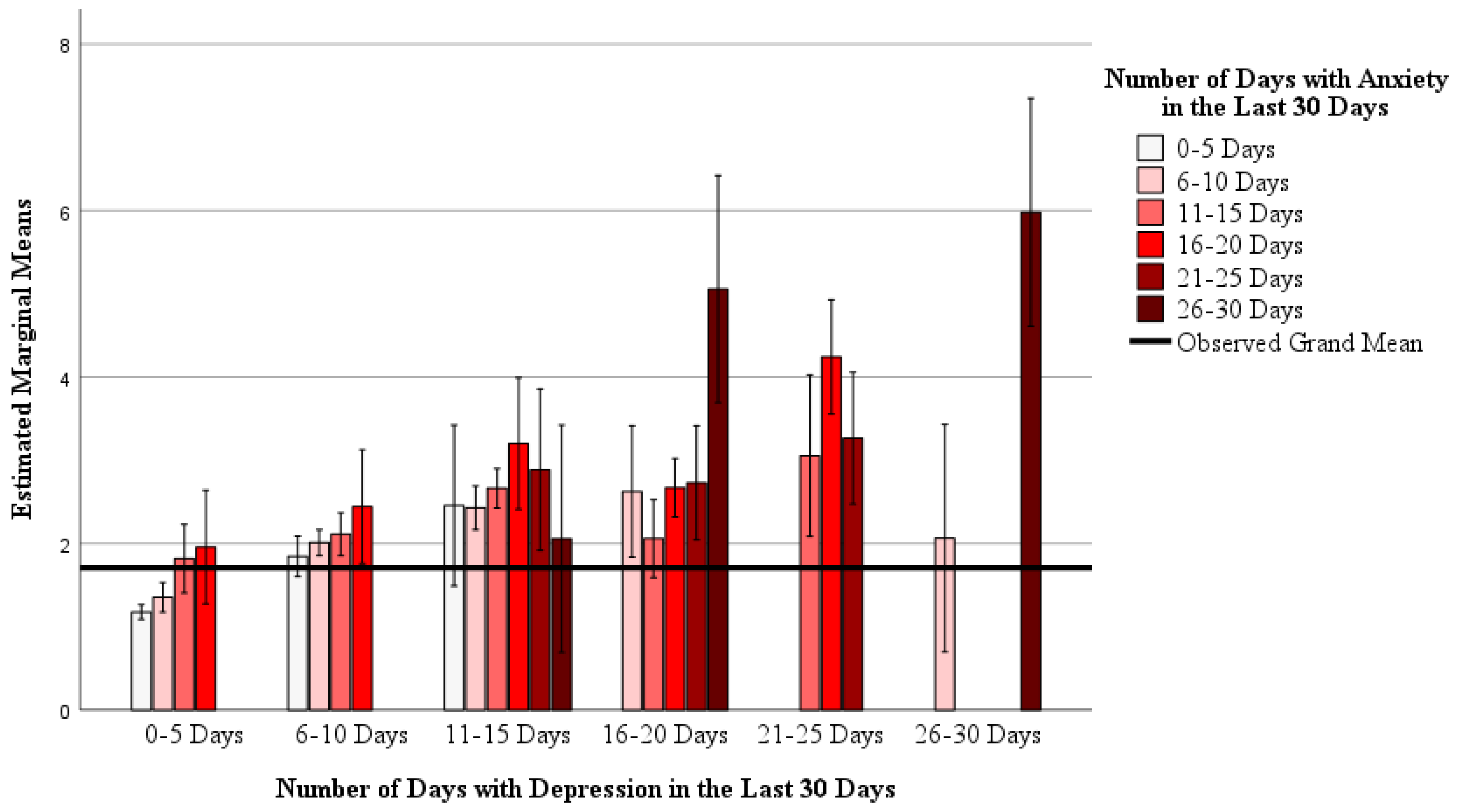
3.3. The Interaction between Days with Depression and Days with Anxiety on Mental Health Status
3.4. Associations between Dietary Intake with Depression or Anxiety
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, Y.; Je, Y.; Giovannucci, E.L. Association between Dietary Fat Intake and Mortality from All-Causes, Cardiovascular Disease, and Cancer: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Clin. Nutr. 2021, 40, 1060–1070. [Google Scholar] [CrossRef] [PubMed]
- Zhong, V.W.; Van Horn, L.; Greenland, P.; Carnethon, M.R.; Ning, H.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake with Incident Cardiovascular Disease and All-Cause Mortality. JAMA Intern. Med. 2020, 180, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.A.; Tayyiba, M.; Agarwal, A.; Mejia, S.B.; de Souza, R.J.; Wolever, T.M.S.; Leiter, L.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Sievenpiper, J.L. Relation of Total Sugars, Sucrose, Fructose, and Added Sugars With the Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Mayo Clin. Proc. 2019, 94, 2399–2414. [Google Scholar] [CrossRef]
- Atanasova, P.; Kusuma, D.; Pineda, E.; Frost, G.; Sassi, F.; Miraldo, M. The Impact of the Consumer and Neighbourhood Food Environment on Dietary Intake and Obesity-Related Outcomes: A Systematic Review of Causal Impact Studies. Soc. Sci. Med. 2022, 299, 114879. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Weis, K.E.; Schulz, M.; Tooze, J.A. Food Intake Patterns Associated With Incident Type 2 Diabetes. Diabetes Care 2009, 32, 263–268. [Google Scholar] [CrossRef]
- Tian, S.; Xu, Q.; Jiang, R.; Han, T.; Sun, C.; Na, L. Dietary Protein Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis of Cohort Studies. Nutrients 2017, 9, 982. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. Dietary Protein Quality Evaluation in Human Nutrition. Report of an FAO Expert Consultation; Food and Agriculture Organization of the United Nations: Rome, Italy, 2013; Volume 92, ISBN 9789251074176. [Google Scholar]
- Koochakpoor, G.; Salari-Moghaddam, A.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Dietary Intake of Branched-Chain Amino Acids in Relation to Depression, Anxiety and Psychological Distress. Nutr. J. 2021, 20, 11. [Google Scholar] [CrossRef]
- Saghafian, F.; Hajishafiee, M.; Rouhani, P.; Saneei, P. Dietary Fiber Intake, Depression, and Anxiety: A Systematic Review and Meta-Analysis of Epidemiologic Studies. Nutr. Neurosci. 2023, 26, 108–126. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuizen, W.F.; Weenen, H.; Rigby, P.; Hetherington, M.M. Older Adults and Patients in Need of Nutritional Support: Review of Current Treatment Options and Factors Influencing Nutritional Intake. Clin. Nutr. 2010, 29, 160–169. [Google Scholar] [CrossRef]
- Carpenter, B.D.; Gatz, M.; Smyer, M.A. Mental Health and Aging in the 2020s. Am. Psychol. 2022, 77, 538–550. [Google Scholar] [CrossRef]
- Roberts, S.B.; Rosenberg, I. Nutrition and Aging: Changes in the Regulation of Energy Metabolism with Aging. Physiol. Rev. 2006, 86, 651–667. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Crimmins, E.M.; Kim, J.K.; Ailshire, J.A. Food and Nutrient Intake and Diet Quality among Older Americans. Public Health Nutr. 2021, 24, 1638–1647. [Google Scholar] [CrossRef] [PubMed]
- Beasley, J.M.; Firestone, M.J.; Popp, C.J.; Russo, R.; Yi, S.S. Age and Racial/Ethnic Differences in Dietary Sources of Protein, NHANES, 2011–2016. Front. Nutr. 2020, 7, 76. [Google Scholar] [CrossRef] [PubMed]
- Rohrmann, S.; Linseisen, J. Processed Meat: The Real Villain? Proc. Nutr. Soc. 2016, 75, 233–241. [Google Scholar] [CrossRef]
- Taylor, Z.B.; Stevenson, R.J.; Ehrenfeld, L.; Francis, H.M. The Impact of Saturated Fat, Added Sugar and Their Combination on Human Hippocampal Integrity and Function: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2021, 130, 91–106. [Google Scholar] [CrossRef]
- Qi, C.; Gou, R. Association of Dietary Saturated Fatty Acid Intake with Depression: Mediating Effects of the Dietary Inflammation Index. Front. Nutr. 2024, 11, 1396029. [Google Scholar] [CrossRef]
- Explore Census Data. Available online: https://data.census.gov/profile/North_Dakota?g=040XX00US38 (accessed on 5 August 2024).
- Gantner, L.A.; Olson, C.M.; Frongillo, E.A.; Wells, N.M. Prevalence of Nontraditional Food Stores and Distance to Healthy Foods in a Rural Food Environment. J. Hunger Environ. Nutr. 2011, 6, 279–293. [Google Scholar] [CrossRef]
- Lacko, A.; Ng, S.W.; Popkin, B. Urban vs. Rural Socioeconomic Differences in the Nutritional Quality of Household Packaged Food Purchases by Store Type. Int. J. Environ. Res. Public Health 2020, 17, 7637. [Google Scholar] [CrossRef]
- Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) Rural Health Information Hub. Available online: https://www.ruralhealthinfo.org/ (accessed on 10 July 2023).
- Nourish | NDSU Agriculture. Available online: https://www.ndsu.edu/agriculture/extension/programs/nourish (accessed on 5 August 2024).
- Centers for Disease Control. Behavioral Risk Factor Surveillance System Questionnaires. Available online: https://www.cdc.gov/brfss/questionnaires/index.htm (accessed on 31 May 2022).
- National Cancer Institute Division of Cancer Control & Population Sciences. Dietary Screener Questionnaire in the National Health Interview Survey Cancer Control Supplement 2015; National Cancer Institute Division of Cancer Control & Population Sciences: Rockville, MD, USA, 2016. Available online: https://epi.grants.cancer.gov/nhis/2015-screener/ (accessed on 31 May 2022).
- Data Access-Urban Rural Classification Scheme for Counties. Available online: https://www.cdc.gov/nchs/data_access/urban_rural.htm#2013_Urban-Rural_Classification_Scheme_for_Counties (accessed on 14 August 2024).
- Morales, D.A.; Barksdale, C.L.; Beckel-Mitchener, A.C. A Call to Action to Address Rural Mental Health Disparities. J. Clin. Transl. Sci. 2020, 4, 463–467. [Google Scholar] [CrossRef]
- Edwards, A.M.; Hung, R.; Levin, J.B.; Forthun, L.; Sajatovic, M.; McVoy, M. Health Disparities among Rural Individuals with Mental Health Conditions: A Systematic Literature Review. J. Rural Ment. Health 2023, 47, 163–178. [Google Scholar] [CrossRef]
- Haytowitz, D.B.; Ahuja, J.K.C.; Wu, X.; Somanchi, M.; Nickle, M.; Nguyen, Q.A.; Roseland, J.M.; Williams, J.R.; Patterson, K.Y.; Li, Y.; et al. USDA National Nutrient Database for Standard Reference, Legacy Release | Ag Data Commons; Nutrient Data Laboratory, Beltsville Human Nutrition Research Center, Agricultural Research Service, United States Department of Agriculture: Beltsville, MD, USA, 2019; Dataset. [Google Scholar] [CrossRef]
- Ferraris, C.; Scarlett, C.J.; Bucher, T.; Beckett, E.L. Liking of Salt Is Associated with Depression, Anxiety, and Stress. Chem Senses 2023, 48, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cold Food Storage Chart | FoodSafety.Gov. Available online: https://www.foodsafety.gov/food-safety-charts/cold-food-storage-charts (accessed on 7 August 2024).
- Głąbska, D.; Guzek, D.; Groele, B.; Gutkowska, K. Fruit and Vegetable Intake and Mental Health in Adults: A Systematic Review. Nutrients 2020, 12, 115. [Google Scholar] [CrossRef] [PubMed]
- Aucoin, M.; LaChance, L.; Naidoo, U.; Remy, D.; Shekdar, T.; Sayar, N.; Cardozo, V.; Rawana, T.; Chan, I.; Cooley, K. Diet and Anxiety: A Scoping Review. Nutrients 2021, 13, 4418. [Google Scholar] [CrossRef]
- Robb, C.E.; de Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H.; et al. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef]
- Holmes, B.A.; Roberts, C.L.; Nelson, M. How Access, Isolation and Other Factors May Influence Food Consumption and Nutrient Intake in Materially Deprived Older Men in the UK. Nutr. Bull. 2008, 33, 212–220. [Google Scholar] [CrossRef]
- Hughes, G.; Bennett, K.M.; Hetherington, M.M. Old and Alone: Barriers to Healthy Eating in Older Men Living on Their Own. Appetite 2004, 43, 269–276. [Google Scholar] [CrossRef]
- Whitelock, E.; Ensaff, H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients 2018, 10, 413. [Google Scholar] [CrossRef]
- Prentice, R.L.; Mossavar-Rahmani, Y.; Huang, Y.; Van Horn, L.; Beresford, S.A.A.; Caan, B.; Tinker, L.; Schoeller, D.; Bingham, S.; Eaton, C.B.; et al. Evaluation and Comparison of Food Records, Recalls, and Frequencies for Energy and Protein Assessment by Using Recovery Biomarkers. Am. J. Epidemiol. 2011, 174, 591–603. [Google Scholar] [CrossRef] [PubMed]
- Pachana, N.A.; Byrne, G.J.; Siddle, H.; Koloski, N.; Harley, E.; Arnold, E. Development and Validation of the Geriatric Anxiety Inventory. Int. Psychogeriatr. 2007, 19, 103–114. [Google Scholar] [CrossRef]
- Saracino, R.M.; Cham, H.; Rosenfeld, B.; Nelson, C.J. Confirmatory Factor Analysis of the Center for Epidemiologic Studies Depression Scale in Oncology With Examination of Invariance Between Younger and Older Patients. Eur. J. Psychol. Assess. 2020, 36, 229–236. [Google Scholar] [CrossRef]
- Aiyegbusi, O.L.; Roydhouse, J.; Rivera, S.C.; Kamudoni, P.; Schache, P.; Wilson, R.; Stephens, R.; Calvert, M. Key Considerations to Reduce or Address Respondent Burden in Patient-Reported Outcome (PRO) Data Collection. Nat. Commun. 2022, 13, 6026. [Google Scholar] [CrossRef] [PubMed]

| Age | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 50–55 Years | 56–61 Years | 62–64 Years | 65–70 Years | ≥71 Years | Missing or Prefer Not to Answer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 165 (32.7%) | 151 (30.0%) | 103 (20.4%) | 53 (10.5%) | 31 (6.2%) | 1 (0.2%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 32 (24.1%) | 34 (25.6%) | 18 (13.5%) | 21 (15.8%) | 28 (21.1%) | 0 (0.0%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sex | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Female | Male | Other | Missing or Prefer Not to Answer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 265 (52.6%) | 232 (46.0%) | 6 (1.2%) | 1 (0.2%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 82 (61.7%) | 50 (37.6%) | 0 (0.0%) | 1 (0.8%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Race and Ethnicity | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| African American | American Indian/Alaska Native | Asian American/Pacific Islander | Hispanic | Non-Hispanic White | Other | Missing or Prefer Not to Answer | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 48 (9.5%) | 15 (3.0%) | 21 (4.2%) | 25 (5.0%) | 385 (76.4%) | 10 (2.0%) | 0 (0.0%) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 1 (0.8%) | 2 (1.5%) | 2 (1.5%) | 5 (3.8%) | 133 (88.0%) | 6 (4.5%) | 0 (0.0%) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Education | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Did Not Finish High School | High School Graduate | Some College | Associate’s Degree | Bachelor’s Degree | Some Graduate School | Post-Graduate Degree | Missing or Prefer Not to Answer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 13 (2.6%) | 76 (15.1%) | 123 (24.4%) | 101 (20.0%) | 140 (27.8%) | 26 (5.2%) | 25 (5.0%) | 0 (0.0%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 1 (0.8%) | 0 (7.5%) | 24 (18.0%) | 21 (15.8%) | 46 (34.6%) | 7 (5.3%) | 24 (18.0%) | 0 (0.0%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Household Income | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| USD 0–24,999 | USD 25,000–49,999 | USD 50,000–74,999 | USD 75,000–99,999 | USD 100,000–149,999 | ≥USD 150,000 | Missing or Prefer Not to Answer | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 18 (3.6%) | 70 (13.9%) | 113 (22.4%) | 154 (30.6%) | 78 (15.5%) | 43 (8.5%) | 28 (5.6%) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 6 (4.5%) | 19 (14.3%) | 27 (20.3%) | 34 (25.6%) | 25 (18.8%) | 10 (7.5%) | 12 (9.0%) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cohabitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Lives Alone | Lives with a Spouse or Partner | Lives with Other Persons | Missing or Prefer Not to Answer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rural | 105 (20.8%) | 384 (76.2%) | 15 (3.0%) | 0 (0.0%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Metro | 35 (26.3%) | 95 (71.4%) | 3 (2.3%) | 0 (0.0%) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Regarding Your MENTAL Health (Stress, Depression, Emotions, etc.) in the Past 30 Days, How Many Days Would You Consider Your Mental Health “Not Good?” | |||||||
|---|---|---|---|---|---|---|---|
| 0–5 Days | 6–10 Days | 11–15 Days | 16–20 Days | 21–25 Days | 26–30 Days | Missing or Prefer Not to Answer | |
| Rural | 292 (57.9%) | 111 (22.0%) | 71 (14.1%) | 19 (3.8%) | 11 (2.2%) | 0 (0.0%) | 0 (0.0%) |
| Metro | 78 (58.6%) | 24 (18.0%) | 24 (18.0%) | 4 (3.8%) | 1 (0.8%) | 1 (0.8%) | 0 (0.0%) |
| Regarding Your MENTAL Health, in the Past 30 Days, How Many Days Were You Unable to Perform Your Usual, Daily Activities (Self-Care, Work, Recreation, etc.)? | |||||||
| 0–5 Days | 6–10 Days | 11–15 Days | 16–20 Days | 21–25 Days | 26–30 Days | Missing or Prefer Not to Answer | |
| Rural | 345 (68.5%) | 85 (16.9%) | 41 (8.1%) | 22 (4.4%) | 8 (1.6%) | 3 (0.6%) | 0 (0.0%) |
| Metro | 107 (80.5%) | 17 (12.8%) | 4 (3.0%) | 3 (2.3%) | 0 (0.0%) | 2 (1.5%) | 0 (0.0%) |
| In the Past 30 Days, for How Many Days Have you Felt SAD, BLUE, or DEPRESSED? | |||||||
| 0–5 Days | 6–10 Days | 11–15 Days | 16–20 Days | 21–25 Days | 26–30 Days | Missing or Prefer Not to Answer | |
| Rural | 286 (56.7%) | 119 (23.6%) | 61 (12.1%) | 30 (6.0%) | 7 (1.4%) | 1 (0.2%) | 0 (0.0%) |
| Metro | 83 (62.4%) | 27 (20.3%) | 16 (12.0%) | 4 (3.0%) | 2 (1.5%) | 1 (0.8%) | 0 (0.0%) |
| In the Past 30 Days, for How Many Days Have You Felt WORRIED, TENSE, or ANXIOUS? | |||||||
| 0–5 Days | 6–10 Days | 11–15 Days | 16–20 Days | 21–25 Days | 26–30 Days | Missing or Prefer Not to Answer | |
| Rural | 246 (48.8%) | 146 (29.0%) | 76 (15.1%) | 28 (5.6%) | 7 (1.4%) | 1 (0.2%) | 0 (0.0%) |
| Metro | 77 (57.9%) | 30 (22.6%) | 16 (12.0%) | 4 (3.0%) | 3 (2.3%) | 3 (2.3%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes a Source of Lean Protein (Lean Meat, Poultry, Fish and Other Seafood, Eggs, Dairy, Soy and Other Beans, and Other Substitutes)? | ||||||||
|---|---|---|---|---|---|---|---|---|
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 1 (0.2%) | 7 (1.4%) | 5 (1.0%) | 44 (8.7%) | 158 (31.3%) | 166 (32.9%) | 123 (24.4%) | 0 (0.0%) |
| Metro | 1 (0.8%) | 1 (0.8%) | 4 (3.0%) | 6 (4.5%) | 41 (30.8%) | 36 (27.1%) | 44 (33.1%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes a Processed Meat (Bacon, Sausage, Cold Cuts, Deli Meats, etc.)? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 4 (0.8%) | 35 (6.9%) | 55 (10.9%) | 112 (22.2%) | 139 (27.6%) | 115 (22.8%) | 44 (8.7%) | 0 (0.0%) |
| Metro | 4 (3.0%) | 12 (9.0%) | 25 (18.8%) | 23 (17.3%) | 44 (33.1%) | 20 (15.0%) | 5 (3.8%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes a Fruit? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 2 (0.4%) | 15 (3.0%) | 34 (6.7%) | 36 (7.1%) | 115 (22.8%) | 190 (37.7%) | 112 (22.2%) | 0 (0.0%) |
| Metro | 2 (1.5%) | 5 (3.8%) | 3 (2.3%) | 8 (6.0%) | 29 (21.8%) | 46 (34.6%) | 40 (30.1%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes a Vegetable? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 2 (0.4%) | 7 (1.4%) | 13 (2.6%) | 45 (8.9%) | 101 (20.0%) | 175 (34.7%) | 161 (31.9%) | 0 (0.0%) |
| Metro | 1 (0.8%) | 2 (1.5%) | 5 (3.8%) | 3 (2.3%) | 29 (21.8%) | 44 (33.1%) | 49 (36.8%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes a Leafy, Green Vegetable (Spinach, Kale, Lettuce, etc.)? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 3 (0.6%) | 12 (2.4%) | 29 (5.8%) | 50 (9.9%) | 149 (29.6%) | 166 (32.9%) | 95 (18.8%) | 0 (0.0%) |
| Metro | 3 (2.3%) | 4 (3.0%) | 6 (4.5%) | 9 (6.8%) | 52 (39.1%) | 37 (27.8%) | 2 (16.5%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes Nuts and Seeds? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two Or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 3 (0.6%) | 32 (6.3%) | 51 (10.1%) | 119 (23.6%) | 147 (29.2%) | 118 (23.4%) | 34 (6.7%) | 0 (0.0%) |
| Metro | 3 (2.3%) | 14 (10.5%) | 9 (6.8%) | 23 (17.3%) | 34 (25.6%) | 35 (26.3%) | 15 (11.3%) | 0 (0.0%) |
| How Often Do You Eat a Meal or Snack That Includes Beans (Kidney Beans, Chickpeas, Lentils, etc.)? | ||||||||
| Never | Rarely | Less Than Once per Week | About Once per Week | Every Two or Three Days | Once per Day | More Than Once per Day | Missing or Prefer Not to Answer | |
| Rural | 11 (2.2%) | 35 (6.9%) | 79 (15.7%) | 117 (23.2%) | 167 (33.1%) | 74 (14.7%) | 21 (4.2%) | 0 (0.0%) |
| Metro | 4 (3.0%) | 22 (16.5%) | 21 (15.8%) | 33 (24.8%) | 35 (26.3%) | 17 (12.8%) | 1 (0.8%) | 0 (0.0%) |
| Variable | Location | Median or Percentage | Interquartile Range (Min, Max) | Χ2 or U a (p) |
|---|---|---|---|---|
| Age (Ordinal) | Rural | 2.00 | 1.00–3.00 (1, 5) | 7.099 (p = 0.008) |
| Metro | 3.00 | 2.00–3.00 (1, 5) | ||
| Sex (Categorical) | Rural | 46.0% Male | - | −1.806 (p = 0.071) |
| Metro | 37.6% Male | - | ||
| Race and Ethnicity (Categorical) | Rural | 76.4% non-Hispanic white | - | 3.458 (p < 0.001) |
| Metro | 88.0% non-Hispanic white | - | ||
| Education (Ordinal) | Rural | 4.00 | 3.00–5.00 (1, 7) | 16.457 (p < 0.001) |
| Metro | 5.00 | 3.00–5.00 (1, 7) | ||
| Household Income (Ordinal) | Rural | 4.00 | 3.00–5.00 (1, 6) | 0.446 (p = 0.504) |
| Metro | 4.00 | 3.00–5.00 (1, 6) | ||
| Cohabitation (Categorical) | Rural | 20.8% Live alone | - | 1.357 (p = 0.175) |
| Metro | 26.3% Live alone | - | ||
| Number of “Not Good” Mental Health Days in the Last 30 Days (Ordinal) | Rural | 1.00 | 1.00–2.00 (1, 6) | 0.002 (p = 0.961) |
| Metro | 1.00 | 1.00–2.00 (1, 6) | ||
| Number of Days Unable to Perform Activities due to Poor Mental Health (Ordinal) | Rural | 1.00 | 1.00–2.00 (1, 6) | 6.781 (p = 0.009) |
| Metro | 1.00 | 1.00–1.00 (1, 6) | ||
| Number of Days with Depressive Symptoms in the Last 30 Days (Ordinal) | Rural | 1.00 | 1.00–2.00 (1, 6) | 1.161 (p = 0.281) |
| Metro | 1.00 | 1.00–2.00 (1, 6) | ||
| Number of Days with Anxiety Symptoms in the Last 30 Days (Ordinal) | Rural | 2.00 | 1.00–2.00 (1, 6) | 3.121 (p = 0.077) |
| Metro | 1.00 | 1.00–2.00 (1, 6) | ||
| Lean Protein Intake (Ordinal) | Rural | 6.00 | 5.00–6.00 (1, 7) | 3.660 (p = 0.056) |
| Metro | 6.00 | 5.00–7.00 (1, 7) | ||
| Processed Meat Intake (Ordinal) | Rural | 5.00 | 4.00–6.00 (1, 7) | 7.719 (p = 0.005) |
| Metro | 5.00 | 3.00–5.00 (1, 7) | ||
| Fruit Intake (Ordinal) | Rural | 6.00 | 5.00–6.00 (1, 7) | 3.153 (p = 0.076) |
| Metro | 6.00 | 5.00–7.00 (1, 7) | ||
| Vegetable Intake (Ordinal) | Rural | 6.00 | 5.00–7.00 (1, 7) | 0.931 (p = 0.335) |
| Metro | 6.00 | 5.00–7.00 (1, 7) | ||
| Leafy Green Intake (Ordinal) | Rural | 6.00 | 5.00–6.00 (1, 7) | 0.236 (p = 0.627) |
| Metro | 5.00 | 5.00–6.00 (1, 7) | ||
| Nuts and Seeds Intake (Ordinal) | Rural | 5.00 | 4.00–6.00 (1, 7) | 2.354 (p = 0.125) |
| Metro | 5.00 | 4.00–6.00 (1, 7) | ||
| Beans Intake (Ordinal) | Rural | 5.00 | 4.00–5.00 (1, 7) | 5.723 (p = 0.017) |
| Metro | 4.00 | 3.00–5.00 (1, 7) |
| Dietary Intake Variable | Univariate (n = 637) | Partially Adjusted Model Including Demographic Covariates (n = 589) a | Fully Adjusted Model Including Dietary Covariates (n = 589) b | |||
|---|---|---|---|---|---|---|
| β ± S.E. c | p | β ± S.E. | p | β ± S.E. | p | |
| Lean protein intake | −0.189 ± 0.036 | <0.001 | −0.146 ± 0.037 | <0.001 | −0.117 ± 0.040 | 0.004 |
| Processed meat intake | 0.043 ± 0.028 | 0.133 | −0.010 ± 0.030 | 0.741 | 0.016 ± 0.032 | 0.614 |
| Fruit intake | −0.139 ± 0.030 | <0.001 | −0.093 ± 0.032 | 0.004 | −0.096 ± 0.038 | 0.011 |
| Vegetable intake | −0.120 ± 0.036 | <0.001 | −0.055 ± 0.035 | 0.115 | −0.027 ± 0.044 | 0.536 |
| Leafy green intake | 0.021 ± 0.031 | =0.512 | 0.039 ± 0.033 | 0.232 | 0.078 ± 0.041 | 0.059 |
| Nut and seed intake | −0.021 ± 0.029 | =0.512 | −0.022 ± 0.030 | 0.461 | −0.003 ± 0.035 | 0.925 |
| Bean intake | 0.058 ± 0.029 | <0.001 | 0.003 ± 0.031 | 0.920 | 0.014 ± 0.037 | 0.712 |
| Dietary Intake Variable | Univariate (n = 637) | Partially Adjusted Model Including Demographic Covariates (n = 589) a | Fully Adjusted Model Including Dietary Covariates (n = 589) b | |||
|---|---|---|---|---|---|---|
| β ± S.E. c | p | β ± S.E. | p | β ± S.E. | p | |
| Lean protein intake | −0.145 ± 0.037 | <0.001 | −0.108 ± 0.037 | 0.004 | −0.086 ± 0.040 | 0.031 |
| Processed meat intake | 0.086 ± 0.029 | 0.003 | 0.044 ± 0.30 | 0.146 | 0.089 ± 0.040 | 0.005 |
| Fruit intake | −0.157 ± 0.031 | <0.001 | −0.105 ± 0.032 | 0.001 | −0.095 ± 0.038 | 0.012 |
| Vegetable intake | −0.138 ± 0.034 | <0.001 | −0.089 ± 0.035 | 0.011 | −0.051 ± 0.044 | 0.242 |
| Leafy green intake | −0.012 ± 0.032 | 0.712 | −0.006 ± 0.033 | 0.853 | 0.068 ± 0.041 | 0.103 |
| Nut and seed intake | −0.028 ± 0.30 | 0.356 | −0.022 ± 0.30 | 0.452 | 0.032 ± 0.035 | 0.929 |
| Bean intake | −0.003 ± 0.030 | 0.916 | −0.070 ± 0.031 | 0.025 | −0.092 ± 0.037 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnson, N.R.; Stastny, S.N.; Garden-Robinson, J. Intakes of Lean Proteins and Processed Meats and Differences in Mental Health between Rural and Metro Adults 50 Years and Older. Nutrients 2024, 16, 3056. https://doi.org/10.3390/nu16183056
Johnson NR, Stastny SN, Garden-Robinson J. Intakes of Lean Proteins and Processed Meats and Differences in Mental Health between Rural and Metro Adults 50 Years and Older. Nutrients. 2024; 16(18):3056. https://doi.org/10.3390/nu16183056
Chicago/Turabian StyleJohnson, Nathaniel R., Sherri N. Stastny, and Julie Garden-Robinson. 2024. "Intakes of Lean Proteins and Processed Meats and Differences in Mental Health between Rural and Metro Adults 50 Years and Older" Nutrients 16, no. 18: 3056. https://doi.org/10.3390/nu16183056
APA StyleJohnson, N. R., Stastny, S. N., & Garden-Robinson, J. (2024). Intakes of Lean Proteins and Processed Meats and Differences in Mental Health between Rural and Metro Adults 50 Years and Older. Nutrients, 16(18), 3056. https://doi.org/10.3390/nu16183056







