Beneficial Effect of Dietary Approaches to Stop Hypertension Diet Combined with Regular Physical Activity on Fat Mass and Anthropometric and Metabolic Parameters in People with Overweight and Obesity
Abstract
1. Introduction
2. Materials and Methods
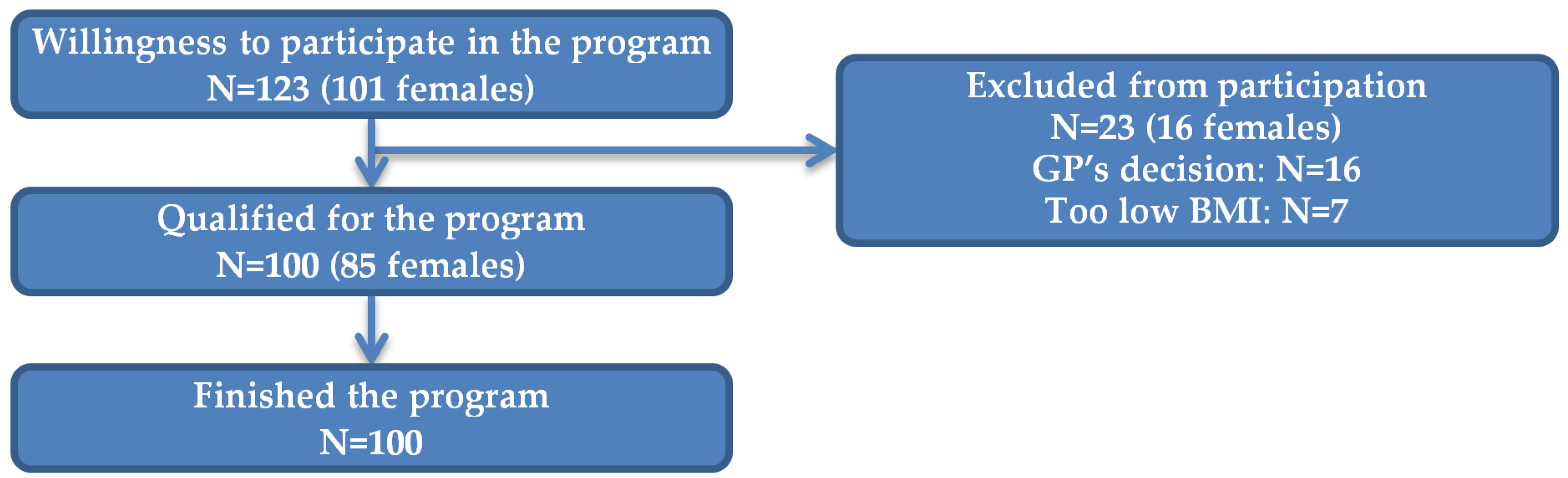
2.1. Study Population
2.2. Assessments
2.3. Intervention
2.3.1. Diet
2.3.2. Physical Activity
2.4. Statistical Analysis
3. Results
3.1. Whole Group
3.2. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 April 2024).
- Narodowy Fundusz Zdrowia (NFZ) [National Health Fund]. NFZ o zdrowiu. Otyłość i jej konsekwencje. Available online: https://ezdrowie.gov.pl/portal/home/badania-i-dane/zdrowe-dane/raporty/otylosc (accessed on 3 August 2024).
- De Lorenzo, A.; Romano, L.; Di Renzo, L.; Di Lorenzo, N.; Cenname, G.; Gualtieri, P. Obesity: A Preventable, Treatable, but Relapsing Disease. Nutrition 2019, 71, 110615. [Google Scholar] [CrossRef] [PubMed]
- Bodai, B.I.; Nakata, T.E.; Wong, W.T.; Clark, D.R.; Lawenda, S.; Tsou, C.; Liu, R.; Shiue, L.; Cooper, N.R.; Rehbein, M.; et al. Lifestyle Medicine: A brief review of its dramatic impact on health and survival. Perm. J. 2018, 22, 17–025. [Google Scholar] [CrossRef] [PubMed]
- Renehan, A.G.; Tyson, M.; Egger, M.; Heller, R.F.; Zwahlen, M. Body-Mass Index and Incidence of Cancer: A Systematic Review and Meta-Analysis of Prospective Observational Studies. Lancet 2008, 371, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’Emidio, S.; Armeni, M.; Bravi, V.; Bendini, M.G.; Mazza, A. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens Res. 2017, 40, 947–963. [Google Scholar] [CrossRef] [PubMed]
- Natsis, M.; Antza, C.; Doundoulakis, I.; Stabouli, S.; Kotsis, V. Hypertension in Obesity: Novel Insights. Curr. Hypertens. Rev. 2020, 16, 30–36. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Dereziński, T.; Zozulińska-Ziółkiewicz, D.; Uruska, A.; Dąbrowski, M. Anthropometric, Metabolic and Clinical Factors Associated with Diabetes and Prediabetes Prevalence in Women Aged 65–74 Living in Central Poland. Clin. Diabetol. 2019, 8, 238–247. [Google Scholar] [CrossRef]
- Araszkiewicz, A.; Bandurska-Stankiewicz, E.; Borys, S.; Broncel, M.; Budzyński, A.; Cyganek, K.; Cypryk, K.; Cyranka, K.; Czupryniak, L.; Dzida, G.; et al. Standards of Care in Diabetes. The Position of Diabetes Poland—2024. Curr. Top. Diabetes 2023, 4, 1–348. [Google Scholar] [CrossRef]
- Xiao, C.; Graf, S. Overweight, Poor Diet and Physical Activity: Analysis of Trends and Patterns. In The Heavy Burden of Obesity: The Economics of Prevention; OECD Publishing: Paris, UK, 2019. [Google Scholar] [CrossRef]
- Hassapidou, M.; Vlassopoulos, A.; Kalliostra, M.; Govers, E.; Mulrooney, H.; Ells, L.; Salas, X.R.; Muscogiuri, G.; Darleska, T.H.; Busetto, L.; et al. European Association for the Study of Obesity Position Statement on Medical Nutrition Therapy for the Management of Overweight and Obesity in Adults Developed in Collaboration with the European Federation of the Associations of Dietitians. Obes. Facts 2023, 16, 11–18. [Google Scholar] [CrossRef]
- Soltani, S.; Shirani, F.; Chitsazi, M.J.; Salehi-Abargouei, A. The Effect of Dietary Approaches to Stop Hypertension (DASH) Diet on Weight and Body Composition in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Obes. Rev. 2016, 17, 442–454. [Google Scholar] [CrossRef]
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2015, 113, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Higuera-Hernández, M.F.; Reyes-Cuapio, E.; Gutiérrez-Mendoza, M.; Rocha, N.B.; Veras, A.B.; Budde, H.; Jesse, J.; Zaldívar-Rae, J.; Blanco-Centurión, C.; Machado, S.; et al. Fighting Obesity: Non-Pharmacological Interventions. Clin. Nutr. ESPEN 2018, 25, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, J.A.; Babyak, M.A.; Hinderliter, A.; Watkins, L.L.; Craighead, L.; Lin, P.H.; Caccia, C.; Johnson, J.; Waugh, R.; Sherwood, A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE study. Arch. Intern. Med. 2010, 170, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, J.A.; Babyak, M.A.; Sherwood, A.; Craighead, L.; Lin, P.H.; Johnson, J.; Watkins, L.L.; Wang, J.T.; Kuhn, C.; Feinglos, M.; et al. Effects of the dietary approaches to stop hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension 2010, 55, 1199–1205. [Google Scholar] [CrossRef] [PubMed]
- Edwards, K.M.; Wilson, K.L.; Sadja, J.; Ziegler, M.G.; Mills, P.J. Effects on blood pressure and autonomic nervous system function of a 12-week exercise or exercise plus DASH-diet intervention in individuals with elevated blood pressure. Acta. Physiol. 2011, 203, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Paula, T.P.; Viana, L.V.; Neto, A.T.; Leitão, C.B.; Gross, J.L.; Azevedo, M.J. Effects of the DASH Diet and Walking on Blood Pressure in Patients With Type 2 Diabetes and Uncontrolled Hypertension: A Randomized Controlled Trial. J. Clin. Hypertens. 2015, 17, 895–901. [Google Scholar] [CrossRef] [PubMed]
- L P de Oliveira, V.; de Freitas, M.M.; P de Paula, T.; Gubert, M.L.; Miller, M.E.P.; Schuchmann, R.A.; Souza, K.L.A.; Viana, L.V. DASH diet vs. DASH diet plus physical activity in older patients with type 2 diabetes and high blood pressure: A randomized clinical trial. Nutr. Health 2024, 30, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef]
- Lohman, T.G.; Roche, A.F.; Martorell, R. (Eds.) Anthropometric Standardization Reference Manual: Abridged Edition; Human Kinetics Books: Champaign, IL, USA, 1991. [Google Scholar] [CrossRef]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral Adiposity Index: A Reliable Indicator of Visceral Fat Function Associated with Cardiometabolic Risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef]
- Lin, P.H.; Proschan, M.A.; Bray, G.A.; Fernandez, C.P.; Hoben, K.; Most-Windhauser, M.; Karanja, N.; Obarzanek, E. DASH Collaborative Research Group. Estimation of energy requirements in a controlled feeding trial. Am. J. Clin. Nutr. 2003, 77, 639–645. [Google Scholar] [CrossRef]
- Westerterp, K.R. Physical activity and physical activity induced energy expenditure in humans: Measurement. determinants. and effects. Front Physiol. 2013, 4, 90. [Google Scholar] [CrossRef] [PubMed]
- Mann, T.; Lamberts, R.P.; Lambert, M.I. Methods of prescribing relative exercise intensity: Physiological and practical considerations. Sports Med. 2013, 43, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Sheng, G.; Qiu, J.; Kuang, M.; Peng, N.; Xie, G.; Chen, Y.; Zhang, S.; Zou, Y. Assessing Temporal Differences of Baseline Body Mass Index, Waist Circumference, and Waist-Height Ratio in Predicting Future Diabetes. Front. Endocrinol. 2023, 13, 1020253. [Google Scholar] [CrossRef] [PubMed]
- Dereziński, T.; Zozulińska-Ziółkiewicz, D.; Uruska, A.; Dąbrowski, M. Abdominal aorta diameter as a novel marker of diabetes incidence risk in elderly women. Sci. Rep. 2020, 10, 13734. [Google Scholar] [CrossRef]
- Tewari, A.; Kumar, G.; Maheshwari, A.; Tewari, V.; Tewari, J. Comparative Evaluation of Waist-To-Height Ratio and BMI in Predicting Adverse Cardiovascular Outcome in People with Diabetes: A Systematic Review. Cureus 2023, 15, e38801. [Google Scholar] [CrossRef]
- Badali, T.; Arefhosseini, S.; Rooholahzadegan, F.; Tutunchi, H.; Ebrahimi-Mameghani, M. The effect of DASH diet on atherogenic indices, pro-oxidant-antioxidant balance, and liver steatosis in obese adults with non-alcoholic fatty liver disease: A double-blind controlled randomized clinical trial. Health Promot. Perspect 2023, 13, 77–87. [Google Scholar] [CrossRef]
- Kjeldsen, E.W.; Thomassen, J.Q.; Frikke-Schmidt, R. HDL Cholesterol Concentrations and Risk of Atherosclerotic Cardiovascular Disease—Insights from Randomized Clinical Trials and Human Genetics. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2022, 1867, 159063. [Google Scholar] [CrossRef]
- Feng, J.; Huang, Y.; Wang, H.; Wang, C.; Xu, H.; Ke, P.; He, Y.; Tian, Q.; Cao, S.; Lu, Z. Association between Adherence to the Dietary Approaches to Stop Hypertension Diet and Serum Uric Acid. Sci. Rep. 2023, 13, 6347. [Google Scholar] [CrossRef]
- Gohari, S.; Ghobadi, S.; Jafari, A.; Ahangar, H.; Gohari, S.; Mahjani, M. The Effect of Dietary Approaches to Stop Hypertension and Ketogenic Diets Intervention on Serum Uric Acid Concentration: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sci. Rep. 2023, 13, 10492. [Google Scholar] [CrossRef]
- Wang, L.; Cong, H.; Zhang, J.; Hu, Y.; Wei, A.; Zhang, Y.; Yang, H.; Ren, L.; Qi, W.; Li, W. Predictive Value of the Triglyceride to High-Density Lipoprotein Cholesterol Ratio for All-Cause Mortality and Cardiovascular Death in Diabetic Patients with Coronary Artery Disease Treated With Statins. Front. Cardiovasc. Med. 2021, 8, 718604. [Google Scholar] [CrossRef] [PubMed]
- Kosmas, C.E.; Rodriguez Polanco, S.; Bousvarou, M.D.; Papakonstantinou, E.J.; Peña Genao, E.; Guzman, E.; Kostara, C.E. The Triglyceride/High-Density Lipoprotein Cholesterol (TG/HDL-C) Ratio as a Risk Marker for Metabolic Syndrome and Cardiovascular Disease. Diagnostics 2023, 13, 929. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Tan, Z.; Huang, Y.; Zhao, H.; Liu, M.; Yu, P.; Ma, J.; Zhao, Y.; Zhu, W.; Wang, J. Relationship between the Triglyceride-Glucose Index and Risk of Cardiovascular Diseases and Mortality in the General Population: A Systematic Review and Meta-Analysis. Cardiovasc. Diabetol. 2022, 21, 124. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Shi, J.; Guan, B.; Peng, S.; Wu, X.; Lu, X.; Zhou, J.; Man, J.; Hiu, Y.; Satti, D.I.; et al. Triglyceride-Glucose Index and the Risk of Heart Failure: Evidence from Two Large Cohorts and a Mendelian Randomization Analysis. Cardiovasc. Diabetol. 2022, 21, 229. [Google Scholar] [CrossRef] [PubMed]
- Dereziński, T.; Zozulińska-Ziółkiewicz, D.; Uruska, A.; Dąbrowski, M. Visceral adiposity index as a useful tool for the assessment of cardiometabolic disease risk in women aged 65 to 74. Diabetes Metab. Res. Rev. 2018, 34, e3052. [Google Scholar] [CrossRef]
- Tamosiunas, A.; Luksiene, D.; Kranciukaite-Butylkiniene, D.; Radisauskas, R.; Sopagiene, D.; Bobak, M. Predictive importance of the visceral adiposity index and atherogenic index of plasma of all-cause and cardiovascular disease mortality in middle-aged and elderly Lithuanian population. Front. Public Health 2023, 11, 1150563. [Google Scholar] [CrossRef]
| Parameter | Women, n = 85 | Men, n = 15 | p Value |
|---|---|---|---|
| Age range (years), n (%): <45 45–54 ≥55 | 32 (37.6%) 22 (25.9%) 31 (36.5%) | 7 (46.7%) 4 (26.7%) 4 (26.7%) | 0.705 |
| BMI category, n (%): Normal weight/overweight Obesity I grade Obesity II and III grade | 23 (27.1%) 37 (43.5%) 25 (29.4%) | 6 (40.0%) 9 (60.0%) | 0.022 |
| Hypertension, n (%): Yes No | 41 (48.2%) 44 (51.8%) | 9 (60.0%) 6 (40.0%) | 0.575 |
| Glucose metabolism, n (%) Diabetes Prediabetes Normoglycemia | 12 (14.1%) 9 (10.6%) 64 (75.3%) | 2 (13.3%) 6 (40.0%) 7 (46.7%) | 0.012 |
| Parameter | Baseline Mean ± SD or n (%) | End of Study Mean ± SD or n (%) | Difference Mean ± SD | p Value |
|---|---|---|---|---|
| Weight (kg) | 92.2 ± 16.8 | 86.5 ± 15.8 | −5.6 ± 4.0 | <0.001 |
| BMI (kg/m2) | 33.7 ± 4.9 | 31.7 ± 4.6 | −2.1 ± 1.4 | <0.001 |
| Obesity II and III grade, n (%) Obesity I grade, n (%) Overweight, n (%) Normal weight, n (%) | 34 (34%) 43 (43%) 22 (22%) 1 (1%) | 19 (19%) 36 (36%) 39 (39%) 5 (5%) | - | 0.004 * |
| Waist (cm) | 102.6 ± 13.8 | 97.0 ± 13.6 | −5.6 ± 3.7 | <0.001 |
| WHtR | 0.62 ± 0.08 | 0.59 ± 0.08 | −0.03 ± 0.02 | <0.001 |
| Hip (cm) | 115.5 ± 9.1 | 110.1 ± 8.9 | −5.4 ± 3.9 | <0.001 |
| WHR | 0.89 ± 0.09 | 0.88 ± 0.10 | −0.01 ± 0.04 | 0.033† |
| Fat mass (%) | 40.0 ± 6.9 | 36.6 ± 7.1 | −3.5 ± 2.8 | <0.001 |
| Total cholesterol (mmol/L) | 5.37 ± 1.29 | 4.89 ± 0.89 | −0.49 ± 0.74 | <0.001 |
| Triglycerides (mmol/L) | 1.42 ± 0.58 | 1.24 ± 0.52 | −0.18 ± 0.48 | <0.001 |
| HDL cholesterol (mmol/L) | 1.49 ± 0.40 | 1.41 ± 0.34 | −0.08 ± 0.23 | 0.002 |
| LDL cholesterol (mmol/L) | 3.27 ± 0.98 | 2.90 ± 0.83 | −0.36 ± 0.68 | <0.001 |
| Glucose (mmol/L) | 5.37 ± 0.95 | 5.33 ± 0.92 | −0.04 ± 0.73 | 0.466 |
| Uric acid (μmol/L) | 316.0 ± 78.0 | 300.0 ± 73.3 | −16.0 ± 41.6 | <0.001 |
| TG/HDL-C ratio | 2.48 ± 1.59 | 2.21 ± 1.26 | −0.27 ± 1.04 | 0.030† |
| TyG index | 4.66 ± 0.22 | 4.59 ± 0.22 | −0.07 ± 0.16 | <0.001 |
| VAI | 4.35 ± 2.52 | 3.82 ± 1.88 | −0.53 ± 1.78 | 0.010 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soroń-Lisik, M.; Więch, P.; Dąbrowski, M. Beneficial Effect of Dietary Approaches to Stop Hypertension Diet Combined with Regular Physical Activity on Fat Mass and Anthropometric and Metabolic Parameters in People with Overweight and Obesity. Nutrients 2024, 16, 3187. https://doi.org/10.3390/nu16183187
Soroń-Lisik M, Więch P, Dąbrowski M. Beneficial Effect of Dietary Approaches to Stop Hypertension Diet Combined with Regular Physical Activity on Fat Mass and Anthropometric and Metabolic Parameters in People with Overweight and Obesity. Nutrients. 2024; 16(18):3187. https://doi.org/10.3390/nu16183187
Chicago/Turabian StyleSoroń-Lisik, Małgorzata, Paweł Więch, and Mariusz Dąbrowski. 2024. "Beneficial Effect of Dietary Approaches to Stop Hypertension Diet Combined with Regular Physical Activity on Fat Mass and Anthropometric and Metabolic Parameters in People with Overweight and Obesity" Nutrients 16, no. 18: 3187. https://doi.org/10.3390/nu16183187
APA StyleSoroń-Lisik, M., Więch, P., & Dąbrowski, M. (2024). Beneficial Effect of Dietary Approaches to Stop Hypertension Diet Combined with Regular Physical Activity on Fat Mass and Anthropometric and Metabolic Parameters in People with Overweight and Obesity. Nutrients, 16(18), 3187. https://doi.org/10.3390/nu16183187







