Cardiovascular Health and Diet Quality among Vegetarians, Vegans and Omnivores: Insights from a Large Urban Population in Poland
Abstract
1. Introduction
2. Materials and Methods
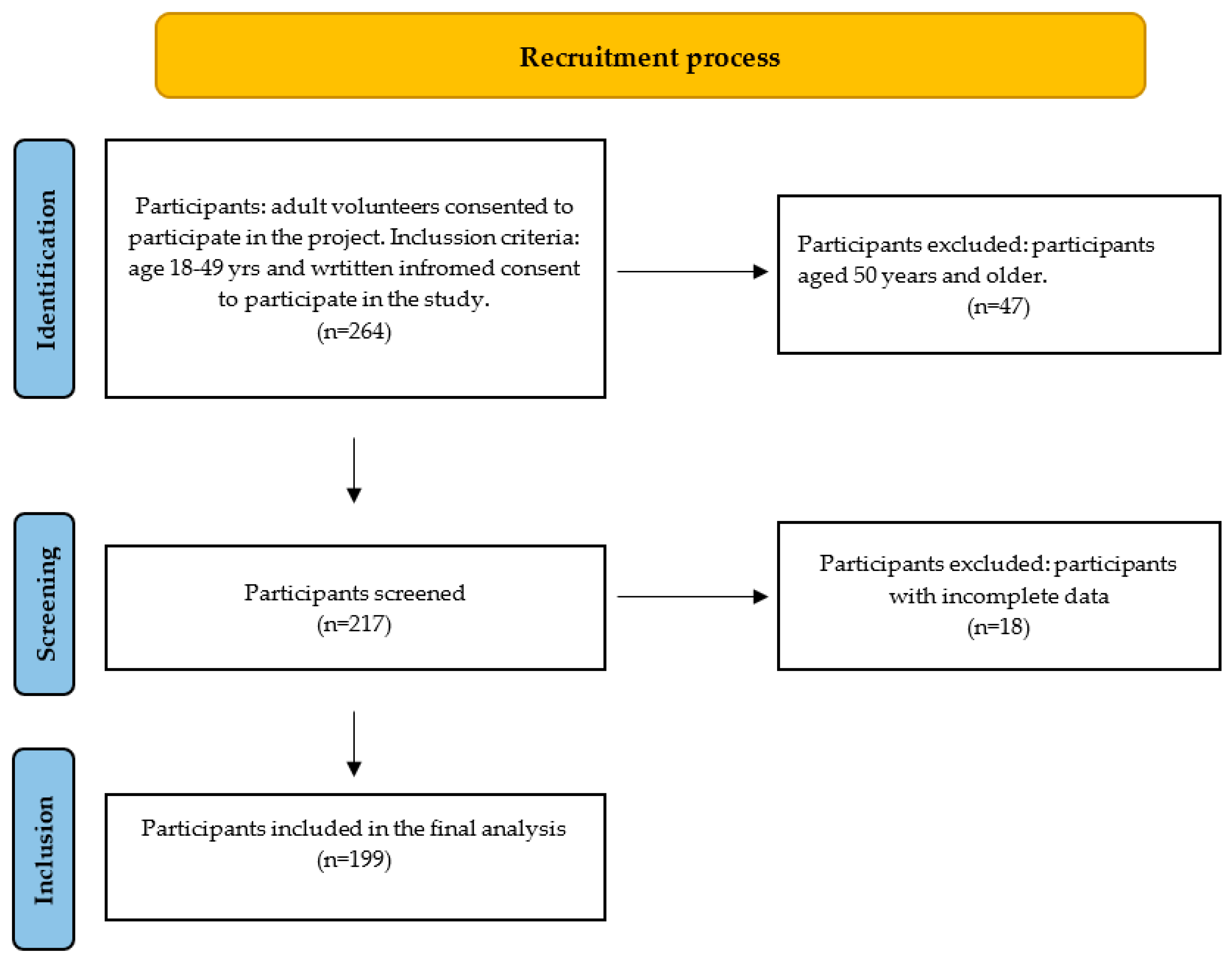
2.1. Study Population
2.2. Subjects
2.3. Protocol and Measures
2.4. Assessment of Dietary Patterns and Nutrition
2.5. Assessment of Cardiovascular Risk Factors
2.6. Statistical Analysis
3. Results
3.1. Baseline Data Analysis
3.2. Analysis of Nutrition Quality According to the Dietary Patterns
3.3. Adherence to the AHA Life’s Simple Seven Criteria According to the Dietary Patterns
3.4. Cardiovascular Characteristics According to the Dietary Patterns
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dinu, M.; Abbate, R.; Gensini, G.F.; Casini, A.; Sofi, F. Vegetarian, Vegan Diets and Multiple Health Outcomes: A Systematic Review with Meta-Analysis of Observational Studies. Crit. Rev. Food Sci. Nutr. 2017, 57, 3640–3649. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Islam, S.U.; Ahmed, M.B.; Ahsan, H.; Lee, Y.-S. Recent Molecular Mechanisms and Beneficial Effects of Phytochemicals and Plant-Based Whole Foods in Reducing LDL-C and Preventing Cardiovascular Disease. Antioxidants 2021, 10, 784. [Google Scholar] [CrossRef]
- Szczepańska, E.; Białek-Dratwa, A.; Janota, B.; Kowalski, O. Dietary Therapy in Prevention of Cardiovascular Disease (CVD)-Tradition or Modernity? A Review of the Latest Approaches to Nutrition in CVD. Nutrients 2022, 14, 2649. [Google Scholar] [CrossRef]
- World Health Organization; Food and Agriculture Organization of the United Nations. Sustainable Healthy Diets: Guiding Principles; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-151664-8. [Google Scholar]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Capodici, A.; Mocciaro, G.; Gori, D.; Landry, M.J.; Masini, A.; Sanmarchi, F.; Fiore, M.; Coa, A.A.; Castagna, G.; Gardner, C.D.; et al. Cardiovascular Health and Cancer Risk Associated with Plant Based Diets: An Umbrella Review. PLoS ONE 2024, 19, e0300711. [Google Scholar] [CrossRef]
- Kuchta, A.; Lebiedzińska, A.; Fijałkowski, M.; Gałąska, R.; Kreft, E.; Totoń, M.; Czaja, K.; Kozłowska, A.; Ćwiklińska, A.; Kortas-Stempak, B.; et al. Impact of Plant-Based Diet on Lipid Risk Factors for Atherosclerosis. Cardiol. J. 2016, 23, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Bruns, A.; Greupner, T.; Nebl, J.; Hahn, A. Plant-Based Diets and Cardiovascular Risk Factors: A Comparison of Flexitarians, Vegans and Omnivores in a Cross-Sectional Study. BMC Nutr. 2024, 10, 29. [Google Scholar] [CrossRef]
- Feingold, K.R. The Effect of Diet on Cardiovascular Disease and Lipid and Lipoprotein Levels. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Dybvik, J.S.; Svendsen, M.; Aune, D. Vegetarian and Vegan Diets and the Risk of Cardiovascular Disease, Ischemic Heart Disease and Stroke: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Eur. J. Nutr. 2023, 62, 51–69. [Google Scholar] [CrossRef]
- Austin, G.; Ferguson, J.J.A.; Eslick, S.; Oldmeadow, C.; Wood, L.G.; Garg, M.L. Cardiovascular Disease Risk in Individuals Following Plant-Based Dietary Patterns Compared to Regular Meat-Eaters. Nutrients 2024, 16, 1063. [Google Scholar] [CrossRef]
- Kwaśniewska, M.; Pikala, M.; Grygorczuk, O.; Waśkiewicz, A.; Stepaniak, U.; Pająk, A.; Kozakiewicz, K.; Nadrowski, P.; Zdrojewski, T.; Puch-Walczak, A.; et al. Dietary Antioxidants, Quality of Nutrition and Cardiovascular Characteristics among Omnivores, Flexitarians and Vegetarians in Poland-The Results of Multicenter National Representative Survey WOBASZ. Antioxidants 2023, 12, 222. [Google Scholar] [CrossRef]
- Neufingerl, N.; Eilander, A. Nutrient Intake and Status in Adults Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients 2021, 14, 29. [Google Scholar] [CrossRef]
- Clem, J.; Barthel, B. A Look at Plant-Based Diets. Mo. Med. 2021, 118, 233–238. [Google Scholar]
- Vegetarian Resource Group. How Many Youth Are Vegetarians? How Many Kids Don’t Eat Meat? Veg. J. 2005, 26–27. [Google Scholar]
- Sebastiani, G.; Herranz Barbero, A.; Borrás-Novell, C.; Alsina Casanova, M.; Aldecoa-Bilbao, V.; Andreu-Fernández, V.; Pascual Tutusaus, M.; Ferrero Martínez, S.; Gómez Roig, M.D.; García-Algar, O. The Effects of Vegetarian and Vegan Diet during Pregnancy on the Health of Mothers and Offspring. Nutrients 2019, 11, 557. [Google Scholar] [CrossRef]
- Wilson, D. Revealed: Countries with the Most Vegetarians in the World. 2024. Available online: https://ceoworld.biz/2024/01/21/revealed-countries-with-the-most-vegetarians-in-the-world-2024/ (accessed on 18 June 2024).
- Komunikat z Badań CBOS Warszawa, Sierpień 2014 “Zachowania Żywieniowe Polaków”; Centrum Badania Opinii Społecznej: 2024. Available online: https://www.cbos.pl/SPISKOM.POL/2014/K_115_14.PDF (accessed on 18 June 2024).
- Łączyński, A.; Bogumił, A.; Kursa, L.; Majcher, A.; Makowska, G.; Niszczota, S.; Rafa, W.; Wroblewska, A.; Wojciechowski, M.; Ziolkowska, E. Agriculture in 2019; Central Statistical Office, AgricultureDepartment: Warsaw, Poland, 2020; p. 67. [Google Scholar]
- Errata: Raport GUS—Przeciętne Spożycie Mięsa Na Osobę Spadło w Polsce o 2,24% w 2019 Roku. Available online: https://roslinniejemy.org/blog/gus-przecietne-spozycie-miesa-na-osobe-spadlo-w-polsce-o-20-w-2019-roku (accessed on 17 August 2024).
- IMAS International Żywność wegańska trafia już do ponad 1/3 Polaków 2021. Available online: https://imas.pl/blog/zywnosc-weganska-trafia-juz-do-ponad-1-3-polakow/ (accessed on 25 June 2024).
- Kukuła Healthy Food Podsumowuje 2021 Rok. Available online: https://www.isbtech.pl/2022/01/kukula-healthy-food-podsumowuje-2021-rok/ (accessed on 8 August 2024).
- Ambroziak, Ł.; Baszczak, Ł.; Kłosiewicz-Górecka, U.; Łukasik, K.; Maj, M.; Rybacki, J.; Szymańska, A.; Śliwowski, P. Tygodnik Gospodarczy PIE 2021. Available online: https://pie.net.pl/wp-content/uploads/2021/11/Tygodnik-Gospodarczy-PIE_44-2021.pdf (accessed on 25 June 2024).
- Satija, A.; Hu, F.B. Plant-Based Diets and Cardiovascular Health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef]
- Melina, V.; Craig, W.J.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef]
- Allès, B.; Baudry, J.; Méjean, C.; Touvier, M.; Péneau, S.; Hercberg, S.; Kesse-Guyot, E. Comparison of Sociodemographic and Nutritional Characteristics between Self-Reported Vegetarians, Vegans, and Meat-Eaters from the NutriNet-Santé Study. Nutrients 2017, 9, 1023. [Google Scholar] [CrossRef]
- Schüpbach, R.; Wegmüller, R.; Berguerand, C.; Bui, M.; Herter-Aeberli, I. Micronutrient Status and Intake in Omnivores, Vegetarians and Vegans in Switzerland. Eur. J. Nutr. 2017, 56, 283–293. [Google Scholar] [CrossRef]
- Bruns, A.; Nebl, J.; Jonas, W.; Hahn, A.; Schuchardt, J.P. Nutritional Status of Flexitarians Compared to Vegans and Omnivores—A Cross-Sectional Pilot Study. BMC Nutr. 2023, 9, 140. [Google Scholar] [CrossRef]
- Elorinne, A.-L.; Alfthan, G.; Erlund, I.; Kivimäki, H.; Paju, A.; Salminen, I.; Turpeinen, U.; Voutilainen, S.; Laakso, J. Food and Nutrient Intake and Nutritional Status of Finnish Vegans and Non-Vegetarians. PLoS ONE 2016, 11, e0148235. [Google Scholar] [CrossRef]
- Parker, H.W.; Vadiveloo, M.K. Diet Quality of Vegetarian Diets Compared with Nonvegetarian Diets: A Systematic Review. Nutr. Rev. 2019, 77, 144–160. [Google Scholar] [CrossRef] [PubMed]
- Deliens, T.; Mullie, P.; Clarys, P. Plant-Based Dietary Patterns in Flemish Adults: A 10-Year Trend Analysis. Eur. J. Nutr. 2022, 61, 561–565. [Google Scholar] [CrossRef]
- Gołębiowska, J.; Zimny-Zając, A.; Makuch, S.; Dróżdż, M.; Dudek, K.; Żórawska, J.; Mazur, G.; Agrawal, S. The Impact of Different Types of Diet on the Prevention of Diseases among Polish Inhabitants, Including COVID-19 Disease. Nutrients 2023, 15, 3947. [Google Scholar] [CrossRef]
- Grzelak, T.; Suliga, K.; Sperling, M.; Pelczyńska, M.; Czyżewska, K. Ocena Stosowania Suplementów Diety Wśród Kobiet Ciężarnych Lub Planujących Ciążę. Forum Zaburzeń Metab. 2016, 7, 8–15. [Google Scholar]
- Marciniak, S.; Lange, E.; Laskowski, W. Assessment of the Knowledge of Nutritional Recommendations and Way of Nutrition in Vegetarians and Vegans. Rocz. Panstw. Zakl. Hig. 2021, 72, 381–391. [Google Scholar] [CrossRef]
- Skorek, P.; Glibowski, P.; Banach, K. Nutrition of Vegetarians in Poland—A Review of Research. Rocz. Panstw. Zakl. Hig. 2019, 70, 217–223. [Google Scholar] [CrossRef]
- Czapla, M.; Juárez-Vela, R.; Rozensztrauch, A.; Karniej, P.; Uchmanowicz, I.; Santolalla-Arnedo, I.; Baska, A. Psychometric Properties and Cultural Adaptation of the Polish Version of the Healthy Lifestyle and Personal Control Questionnaire (HLPCQ). Int. J. Environ. Res. Public Health 2021, 18, 9190. [Google Scholar] [CrossRef]
- Mirosław, J.; Ewa, R.; Katarzyna, S.; Jadwiga, C. Normy Żywienia Dla Populacji Polski i Ich Zastosowanie; Narodowy Instytut Zdrowia Publicznego—Państwowy Zakład Higieny: Warszawa, Poland, 2020; ISBN 978-83-65870-28-5. [Google Scholar]
- Mohajan, D.; Mohajan, H.K. Body Mass Index (BMI) Is a Popular Anthropometric Tool to Measure Obesity Among Adults. J. Innov. Med. Res. 2023, 2, 25–33. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction: The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Myers, C.A.; Martin, C.K.; Newton, R.L.; Apolzan, J.W.; Arnold, C.L.; Davis, T.C.; Price-Haywood, E.G.; Katzmarzyk, P.T. Cardiovascular Health, Adiposity, and Food Insecurity in an Underserved Population. Nutrients 2019, 11, 1376. [Google Scholar] [CrossRef]
- Rocha, J.P.; Laster, J.; Parag, B.; Shah, N.U. Multiple Health Benefits and Minimal Risks Associated with Vegetarian Diets. Curr. Nutr. Rep. 2019, 8, 374–381. [Google Scholar] [CrossRef]
- Oussalah, A.; Levy, J.; Berthezène, C.; Alpers, D.H.; Guéant, J.-L. Health Outcomes Associated with Vegetarian Diets: An Umbrella Review of Systematic Reviews and Meta-Analyses. Clin. Nutr. Edinb. Scotl. 2020, 39, 3283–3307. [Google Scholar] [CrossRef]
- Jedut, P.; Glibowski, P.; Skrzypek, M. Comparison of the Health Status of Vegetarians and Omnivores Based on Biochemical Blood Tests, Body Composition Analysis and Quality of Nutrition. Nutrients 2023, 15, 3038. [Google Scholar] [CrossRef]
- Storz, M.A.; Müller, A.; Niederreiter, L.; Zimmermann-Klemd, A.M.; Suarez-Alvarez, M.; Kowarschik, S.; Strittmatter, M.; Schlachter, E.; Pasluosta, C.; Huber, R.; et al. A Cross-Sectional Study of Nutritional Status in Healthy, Young, Physically-Active German Omnivores, Vegetarians and Vegans Reveals Adequate Vitamin B12 Status in Supplemented Vegans. Ann. Med. 2023, 55, 2269969. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of Nutritional Quality of the Vegan, Vegetarian, Semi-Vegetarian, Pesco-Vegetarian and Omnivorous Diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef] [PubMed]
- Dawczynski, C.; Weidauer, T.; Richert, C.; Schlattmann, P.; Dawczynski, K.; Kiehntopf, M. Nutrient Intake and Nutrition Status in Vegetarians and Vegans in Comparison to Omnivores—The Nutritional Evaluation (NuEva) Study. Front. Nutr. 2022, 9, 819106. [Google Scholar] [CrossRef]
- Xie, L.; Wang, B.; Cui, X.; Tang, Q.; Cai, W.; Shen, X. Young Adult Vegetarians in Shanghai Have Comparable Bone Health to Omnivores despite Lower Serum 25(OH) Vitamin D in Vegans: A Cross-Sectional Study. Asia Pac. J. Clin. Nutr. 2019, 28, 383–388. [Google Scholar] [CrossRef]
- García-Maldonado, E.; Gallego-Narbón, A.; Zapatera, B.; Alcorta, A.; Martínez-Suárez, M.; Vaquero, M.P. Bone Remodelling, Vitamin D Status, and Lifestyle Factors in Spanish Vegans, Lacto-Ovo Vegetarians, and Omnivores. Nutrients 2024, 16, 448. [Google Scholar] [CrossRef]
- Fu, L.; Zhang, G.; Qian, S.; Zhang, Q.; Tan, M. Associations between Dietary Fiber Intake and Cardiovascular Risk Factors: An Umbrella Review of Meta-Analyses of Randomized Controlled Trials. Front. Nutr. 2022, 9, 972399. [Google Scholar] [CrossRef]
- Waddell, I.S.; Orfila, C. Dietary Fiber in the Prevention of Obesity and Obesity-Related Chronic Diseases: From Epidemiological Evidence to Potential Molecular Mechanisms. Crit. Rev. Food Sci. Nutr. 2023, 63, 8752–8767. [Google Scholar] [CrossRef] [PubMed]
- Nowicki, G.J.; Ślusarska, B.; Piasecka, H.; Bartoszek, A.; Kocka, K.; Deluga, A. The Status of Cardiovascular Health in Rural and Urban Areas of Janów Lubelski District in Eastern Poland: A Population-Based Study. Int. J. Environ. Res. Public Health 2018, 15, 2388. [Google Scholar] [CrossRef]
- Vaidean, G.; Manczuk, M.; Michos, E. Ideal Cardiovascular Health and Women’s Health Characteristics in Middle Aged Women Free of Diagnosed Cardiovascular Disease. The Polish Norwegian Study. Eur. Heart J. 2022, 43, ehac544.2512. [Google Scholar] [CrossRef]
- Egan, B.M.; Li, J.; Sutherland, S.E.; Jones, D.W.; Ferdinand, K.C.; Hong, Y.; Sanchez, E. Sociodemographic Determinants of Life’s Simple 7: Implications for Achieving Cardiovascular Health and Health Equity Goals. Ethn. Dis. 2020, 30, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, M.M.; Mohebi, R.; Hosseini, F.; Lotfaliany, M.; Azizi, F.; Saadat, N.; Hadaegh, F. Distribution of Ideal Cardiovascular Health in a Community-Based Cohort of Middle East Population. Ann. Saudi Med. 2014, 34, 134–142. [Google Scholar] [CrossRef]
- Chavoshi, V.; Barzin, M.; Ebadinejad, A.; Dehghan, P.; Momeni Moghaddam, A.; Mahdavi, M.; Hadaegh, F.; Niroomand, M.; Valizadeh, M.; Azizi, F.; et al. Association of Ideal Cardiovascular Health with Carotid Intima-Media Thickness (cIMT) in a Young Adult Population. Sci. Rep. 2022, 12, 10056. [Google Scholar] [CrossRef]
- McKenzie, J.A.; Younger, N.O.; Tulloch-Reid, M.K.; Govia, I.; Bennett, N.R.; McFarlane, S.; Walters, R.; Francis, D.K.; Webster-Kerr, K.; Grant, A.; et al. Ideal Cardiovascular Health in Urban Jamaica: Prevalence Estimates and Relationship to Community Property Value, Household Assets and Educational Attainment: A Cross-Sectional Study. BMJ Open 2020, 10, e040664. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Yao, B.; Yu, Z.; Xu, J.; Wu, J.; Ma, Y.; Zheng, L.; Sun, Z. Prevalence of Ideal Cardiovascular Health and Its Relationship with Relative Handgrip Strength in Rural Northeast China. Front. Cardiovasc. Med. 2023, 10, 1124757. [Google Scholar] [CrossRef]
- Wu, X.; Liu, X.; Luo, Z.; Niu, M.; He, Y.; Hou, J.; Mao, Z.; Huo, W.; Li, L.; Wang, C. Gender-Specific Prevalence and Influencing Factors of Ideal Cardiovascular Health in Chinese Rural Population: The Henan Rural Cohort Study 2020. Available online: https://www.researchsquare.com/article/rs-32403/v1 (accessed on 18 August 2024).
- Motta, A.C.S.V.; Bousquet-Santos, K.; Motoki, I.H.L.; Andrade, J.M.D.L. Prevalence of Ideal Cardiovascular Health in the Brazilian Adult Population—National Health Survey 2019. Epidemiol. E Serv. Saude Rev. Sist. Unico Saude Bras. 2023, 32, e2022669. [Google Scholar] [CrossRef]
- Benziger, C.P.; Zavala-Loayza, J.A.; Bernabe-Ortiz, A.; Gilman, R.H.; Checkley, W.; Smeeth, L.; Malaga, G.; Miranda, J.J. CRONICAS Cohort Study group Low Prevalence of Ideal Cardiovascular Health in Peru. Heart Br. Card. Soc. 2018, 104, 1251–1256. [Google Scholar] [CrossRef]
- Appleby, P.N.; Key, T.J. The Long-Term Health of Vegetarians and Vegans. Proc. Nutr. Soc. 2016, 75, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, S.; Beeson, W.L.; Shavlik, D.J.; Siapco, G.; Jaceldo-Siegl, K.; Fraser, G.; Knutsen, S.F. Association between Vegetarian Diets and Cardiovascular Risk Factors in Non-Hispanic White Participants of the Adventist Health Study-2. J. Nutr. Sci. 2019, 8, e6. [Google Scholar] [CrossRef]
- Gan, Z.H.; Cheong, H.C.; Tu, Y.-K.; Kuo, P.-H. Association between Plant-Based Dietary Patterns and Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3952. [Google Scholar] [CrossRef] [PubMed]
- Kharaty, S.; Harrington, J.M.; Millar, S.R.; Perry, I.J.; Phillips, C.M. Plant-Based Dietary Indices and Biomarkers of Chronic Low-Grade Inflammation: A Cross-Sectional Analysis of Adults in Ireland. Eur. J. Nutr. 2023, 62, 3397–3410. [Google Scholar] [CrossRef] [PubMed]
- Craddock, J.C.; Neale, E.P.; Peoples, G.E.; Probst, Y.C. Vegetarian-Based Dietary Patterns and Their Relation with Inflammatory and Immune Biomarkers: A Systematic Review and Meta-Analysis. Adv. Nutr. Bethesda Md 2019, 10, 433–451. [Google Scholar] [CrossRef]
- Barnard, N.D.; Goldman, D.M.; Loomis, J.F.; Kahleova, H.; Levin, S.M.; Neabore, S.; Batts, T.C. Plant-Based Diets for Cardiovascular Safety and Performance in Endurance Sports. Nutrients 2019, 11, 130. [Google Scholar] [CrossRef]
- Escalante-Araiza, F.; Rivera-Monroy, G.; Loza-López, C.E.; Gutiérrez-Salmeán, G. The Effect of Plant-Based Diets on Meta-Inflammation and Associated Cardiometabolic Disorders: A Review. Nutr. Rev. 2022, 80, 2017–2028. [Google Scholar] [CrossRef]
- Najjar, R.S.; Moore, C.E.; Montgomery, B.D. Consumption of a Defined, Plant-based Diet Reduces Lipoprotein(a), Inflammation, and Other Atherogenic Lipoproteins and Particles within 4 Weeks. Clin. Cardiol. 2018, 41, 1062–1068. [Google Scholar] [CrossRef]
- Kahleova, H.; Petersen, K.F.; Shulman, G.I.; Alwarith, J.; Rembert, E.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. Effect of a Low-Fat Vegan Diet on Body Weight, Insulin Sensitivity, Postprandial Metabolism, and Intramyocellular and Hepatocellular Lipid Levels in Overweight Adults: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2025454. [Google Scholar] [CrossRef]
- Haghighatdoost, F.; Bellissimo, N.; Totosy De Zepetnek, J.O.; Rouhani, M.H. Association of Vegetarian Diet with Inflammatory Biomarkers: A Systematic Review and Meta-Analysis of Observational Studies. Public Health Nutr. 2017, 20, 2713–2721. [Google Scholar] [CrossRef]
- Menzel, J.; Jabakhanji, A.; Biemann, R.; Mai, K.; Abraham, K.; Weikert, C. Systematic Review and Meta-Analysis of the Associations of Vegan and Vegetarian Diets with Inflammatory Biomarkers. Sci. Rep. 2020, 10, 21736. [Google Scholar] [CrossRef]
- Sutliffe, J.T.; Wilson, L.D.; de Heer, H.D.; Foster, R.L.; Carnot, M.J. C-Reactive Protein Response to a Vegan Lifestyle Intervention. Complement. Ther. Med. 2015, 23, 32–37. [Google Scholar] [CrossRef]
- Shah, B.; Newman, J.D.; Woolf, K.; Ganguzza, L.; Guo, Y.; Allen, N.; Zhong, J.; Fisher, E.A.; Slater, J. Anti-Inflammatory Effects of a Vegan Diet Versus the American Heart Association-Recommended Diet in Coronary Artery Disease Trial. J. Am. Heart Assoc. 2018, 7, e011367. [Google Scholar] [CrossRef]
- Kwaśniewska, M.; Pikala, M.; Aranowska, A.; Bielecki, W.; Kozakiewicz, K.; Pająk, A.; Tykarski, A.; Zdrojewski, T.; Nadrowski, P.; Piwoński, J.; et al. Ten-Year Changes in Adherence to a Healthy Lifestyle: The Results of the WOBASZ Surveys. Pol. Arch. Intern. Med. 2021, 131, 136–144. [Google Scholar] [CrossRef]
- Waśkiewicz, A.; Szcześniewska, D.; Szostak-Węgierek, D.; Kwaśniewska, M.; Pająk, A.; Stepaniak, U.; Kozakiewicz, K.; Tykarski, A.; Zdrojewski, T.; Zujko, M.E.; et al. Are Dietary Habits of the Polish Population Consistent with the Recommendations for Prevention of Cardiovascular Disease?—WOBASZ II Project. Kardiol. Pol. 2016, 74, 969–977. [Google Scholar] [CrossRef]
- Śliż, D.; Jodczyk, A.M.; Łakoma, K.; Kucharska, A.; Panczyk, M.; Rostkowska, O.M.; Turlej, K.; Młynarska, A.; Drożdż, J.; Jarzębska-Wódka, M.; et al. Examining the Nutrition of Cardiological Patients in Hospitals: Evaluating the Discrepancy between Received Diets and Reference Diet Based on ESC 2021 Guidelines—Hospital Diet Medical Investigation) (HDMI) Study. Nutrients 2023, 15, 4606. [Google Scholar] [CrossRef]
- Raczkiewicz, D.; Owoc, J.; Krakowiak, J.; Rzemek, C.; Owoc, A.; Bojar, I. Patient Safety Culture in Polish Primary Healthcare Centers. Int. J. Qual. Health Care 2019, 31, G60–G66. [Google Scholar] [CrossRef]
- Albert, S.L.; Massar, R.E.; Kwok, L.; Correa, L.; Polito-Moller, K.; Joshi, S.; Shah, S.; McMacken, M. Pilot Plant-Based Lifestyle Medicine Program in an Urban Public Healthcare System: Evaluating Demand and Implementation. Am. J. Lifestyle Med. 2024, 18, 403–419. [Google Scholar] [CrossRef]
- Massar, R.E.; McMacken, M.; Kwok, L.; Joshi, S.; Shah, S.; Boas, R.; Ortiz, R.; Correa, L.; Polito-Moller, K.; Albert, S.L. Patient-Reported Outcomes from a Pilot Plant-Based Lifestyle Medicine Program in a Safety-Net Setting. Nutrients 2023, 15, 2857. [Google Scholar] [CrossRef]
- Baska, A.; Kurpas, D.; Kenkre, J.; Vidal-Alaball, J.; Petrazzuoli, F.; Dolan, M.; Śliż, D.; Robins, J. Social Prescribing and Lifestyle Medicine—A Remedy to Chronic Health Problems? Int. J. Environ. Res. Public Health 2021, 18, 10096. [Google Scholar] [CrossRef]
| Vegans n = 50 | Vegetarians n = 101 | Omnivores n = 48 | |
|---|---|---|---|
| Age, years (mean ± SD) | 33.3 ± 8.5 | 32.9 ± 11.5 | 35.4 ± 685 |
| Marital status, f (%) | |||
| Single | 35/50 (70.0) | 69/101 (68.3) | 21/48 (43.8) |
| Married/partnership | 13/50 (26.0) | 29/101 (28.7) | 20/48 (41.6) |
| Divorced | 1/50 (2.0) | 3/101 (3.0) | 5/48 (10.4) |
| Widowed | 1/50 (2.0) | 0/101 (0.0) | 1/48 (2.1) |
| Educational level, f (%) | |||
| Primary | 1/50 (2.0) | 0/101 (0.0) | 4/48 (8.3) |
| Secondary | 4/50 (8.0) | 19/101 (18.8) | 12/48 (25) |
| University | 45/50 (90.0) | 82/101 (81.2) | 31/48 (64.6) |
| Vegans n = 50 | Vegetarians n = 101 | Omnivores n = 48 | |
|---|---|---|---|
| Energy, kcal | 1693.9 (1678.9; 1958.4) | 1679.4(1622.4; 1846.5) | 1597.7 (1523.7; 1850.6) |
| Total protein, g | 54.4 (54.7; 70.9) | 67.7 ± 25.5 1 | 77.1 ± 27 1,b |
| Proteins (%) | 13.8 | 15.6 | 18.3 |
| Carbohydrates, g | 256.1 (234.3; 284.5) a | 223.1(220.4; 255.5) | 198.7 (187.2; 234.3) b,c |
| Carbohydrates (%) | 57.1 | 54.8 | 50.1 |
| Total fat, g | 63.7 ± 24.2 1 | 57.7 (56.9; 66.9) | 61.1 ± 24.8 1 |
| Fat (%) | 31.6 | 32.1 | 32.5 |
| SFA, g | 8.5 (8.8; 14.4) a | 13.3 (14.1; 18.5) | 9.2 (8.4; 14.2) b,c |
| MUFA, g | 20 (18.1; 25.8) | 21.4 (20.4; 24.8) | 8.5 (9.5; 17.2) b,c |
| PUFA, g | 14.7 (14.2; 19.7) a | 12 (11.9; 14.7) | 4.9 (5.3; 9) b,c |
| Cholesterol, mg | 9.3 (3.2; 18.9) a | 86.6 (108.6; 168.8) | 64.5 (67.8; 148.8) b,c |
| Fibre, g | 29.2 (27.8; 36.6) a | 23 (23.1; 27.1) | 16 (13.7; 20.1) b,c |
| Vegans | Vegetarians | Omnivores | |
|---|---|---|---|
| Potassium, mg | 3054.8 (2815.8; 3846.2) | 2907.7 (2825.8; 3355.5) | 1508.0 (1455.0; 2435.2) b,c |
| Sodium, mg | 1928.0 (1630.6; 2397) a | 2345.1 (2103.0; 2619.9) | 872.2 (1163.9; 2034.9) b,c |
| Phosphorus, mg | 1068.3 (919.6; 1272) | 1772.0 ± 500.4 1 | 598.6 (526.4; 864.4) b,c |
| Magnesium, mg | 413.1 ± 208.6 1 | 343.1 ± 140.8 1 | 167.6 (157.9; 241.3) b,c |
| Iron, mg | 15.0 | 12.2 (10.8; 17.8) | 7.8 (7.0; 10.7) b,c |
| Calcium, mg | 563.0 (521; 735.6) a | 723.6 (702.6; 894) | 508.0 (464.7; 727.8) c |
| Zinc, mg | 8.9 ± 4.6 1 | 8.7 ± 3.5 1 | 4.4 (4.0; 6.3) b,c |
| Copper, mg | 2.1 (1.7; 2.4) a | 1.5 (1.5; 1.8) | 0.8 (0.7; 1.1) b,c |
| Manganese, mg | 7.6 (6.5; 9.7) a | 4.8 (5.0; 6.5) | 2.2 (2.6; 6.1) b,c |
| Vitamin A, µg | 704.5 (612.3; 971.5) | 706.3 (687.8; 906.0) | 223.0 (267.9; 549) b,c |
| Vitamin C, mg | 114.1 (108.5; 155.4) | 107.5 (112.4; 148.6) | 40.4 (51.0; 99.6) b,c |
| Vitamin E, mg | 10.4 (10.1; 15.1) | 11.0 (10.4; 12.6) | 2.5 (3.9; 8.1) b.c |
| Vitamin D, µg | 30.9 (30.3; 63.4) | 32.6 (39.5; 60) | 14.0 (18.4; 58.1) c |
| Vitamin B1, mg | 1.1 (1.0; 1.4) a | 0.9 (0.9; 1.4) | 0.8 (0.7; 1.0) b,c |
| Vitamin B2, mg | 1.0 (0.9; 1.2) a | 1.3 (1.3; 1.5) | 0.7 (0.7; 1.0) b,c |
| Niacin, mg | 11.9 (10.4; 15.7) | 10.1 (9.8; 13.2) | 6.7 (7.0; 12.3) b,c |
| Vitamin B6, mg | 1.6 (1.5; 2) | 1.5 ± 0.6 1 | 0.9 (0.8; 1.2) b,c |
| Folate, µg | 331.2 (256.7; 392.8) | 324.0 (299.1; 364.9) | 100.5 (132.6; 247.8) b,c |
| Vitamin B12, µg | 0.2 (1.2; 1.8) a | 1.5 (1.6; 2.2) | 0.7 (1.1; 1.7) b |
| Recommended Daily Intake (Males/Females) | Vegans | Vegetarians | Omnivores | |
|---|---|---|---|---|
| N (%) | ||||
| Potassium, mg | ≥4700 | 9 (18.0) | 12 (11.9) | 2 (4.2) c |
| Calcium, mg | 19–50 years ≥ 800; above 50 years ≥ 1000 | 15 (30.0) | 42 (41.6) | 14 (29.2) |
| Phosphorus, mg | ≥700 | 36 (72.0) | 81 (80.2) b | 18 (37.5) c |
| Magnesium, mg | ≥350/265 | 34 (68.0) | 66 (65.4) b | 12 (25.0) c |
| Iron, mg | ≥18/10 | 28 (56.0) | 52 (51.5) b | 11 (22.9) c |
| Zinc, mg | ≥11/8 | 24 (48.0) | 36 (35.6) b | 9 (18.8) c |
| Copper, mg | ≥0.7 | 48 (96.0) | 91 (90.0) b | 25 (52.1) c |
| Manganese, mg | 2.3/1.8 | 45 (90.0) | 92 (91.1) b | 25 (52.1) c |
| Vitamin A, µg | ≥630/500 | 30 (60.0) | 65 (64.4) b | 13 (27.1) c |
| Vitamin E, mg | ≥10/8 | 32 (64.0) | 74 (73.3) b | 13 (27.1) c |
| Vitamin B1, mg | ≥1.1/0.9 | 30 (60.0) a | 45 (34.7) | 15 (31.3) c |
| Vitamin B2, mg | ≥1.1/0.9 | 28 (56.0) a | 70 (69.3) b | 19 (39.6) |
| Niacin, mg | ≥16/14 | 12 (24.0) | 19 (18.8) | 9 (18.8) |
| Vitamin B6, mg | ≥1.1/1.3 | 35 (70.0) | 63 (62.4) b | 19 (39.6) c |
| Vitamin C, mg | ≥75/60 | 40 (80.0) | 79 (79.8) b | 21 (43.8) c |
| Folate, µg | ≥320 | 26 (52.0) | 52 (51.5) b | 10 (20.8) c |
| Vitamin B12, µg | ≥2 | 8 (16.0) a | 37 (36.6) | 11 (22.9) |
| Vitamin D, µg | ≥15 ug (600 IU) | 23 (46) a | 69 (68.3) b | 22 (45.8) |
| LS7 | Diet | PA | Smoking | BMI | TC | Glucose | BP |
|---|---|---|---|---|---|---|---|
| Vegan, f (%) | |||||||
| Poor | 0/49 (0.0) | 6/50 (12.0) | 3/50 (6.0) | 2/50 (4.0) | 0/50 (0.0) | 0/50 (0.0) | 1/45 (2.2) |
| Intermediate | 19/49 (38.7) | 27/50 (54.0) | 0/50 (0.0) | 6/50 (12.0) | 0/50 (0.0) | 0/50 (0.0) | 15/45 (30.3) |
| Ideal | 30/49 (61.3) | 17/50 (34.0) | 47/50 (94.0) | 42/50 (84.0) | 50/50 (100.0) | 50/50 (100.0) | 29/45 (64.5) |
| Vegetarians, f (%) | |||||||
| Poor | 26/99 (26.3) | 11/101 (10.9) | 21/101 (20.8) | 1/101 (1.0) | 0/101 (0.0) | 1/101 (1.0) | 4/98 (4.1) |
| Intermediate | 62/99 (62.6) | 43/101 (42.6) | 0/101 (0.0) | 18/101 (17.8) | 0/101 (0.0) | 3/101 (3.0) | 34/98 (34.7) |
| Ideal | 11/99 (11.1) | 47/101 (46.5) | 80/101 (79.2) | 82/101 (81.2) | 101 (100.0) | 97/101 (96.0) | 60/98 (61.2) |
| Omnivores, f (%) | |||||||
| Poor | 3/47 (6.4) | 6/43 (14.0) | 10/47 (21.3) | 3/44 (6.8) | 0/46 (0.0) | 0/46 (0.0) | 1/31 (3.2) |
| Intermediate | 33/47 (70.2) | 13/43 (30.2) | 0/47 (0.0) | 8/44 (18.2) | 0/46 (0.0) | 3/46 (6.5) | 8/31 (25.8) |
| Ideal | 11/47 (23.4) | 24/43 (55.8) | 37/47 (78.7) | 33/44 (75.0) | 46/46 (100.0) | 43/46 (93.5) | 22/31 (71.0) |
| Vegans | Vegetarians | Omnivores | |
|---|---|---|---|
| BMI (kg/m2) | 22.2 ± 2.4 1 | 22.5 (21.6; 24.9) | 23.0 (22.2; 24.5) |
| Waist circumference (cm) | 75.0 (74.1; 82) | 75.0 (74.7; 78.5) | 77.0 (77.7; 85.2) |
| SBP (mmHg) | 110.0 (105.6; 112.7) | 110.0 (104.6; 111.2) | 100.0 (102.5; 112.4) |
| DBP (mmHg) | 70.0 (64.3; 68.9) | 65.0 (63.1; 68.1) | 60.0 (62.0; 67.9) |
| TC (mmol/L) | 4.1 (4.1; 4.5) a | 4.5 (4.4; 4.8) | 5.2 ± 1.0 1,b,c |
| LDL-C (mmol/L) | 2.3 (2.3; 2.7) a | 2.6 (2.6; 2.8) | 3.1 ±0.8 1,b,c |
| HDL-C (mmol/L) | 1.5 ± 0.4 | 1.5 ± 0.5 1 | 1.6 (1.5; 1.8) b |
| TG (mmol/L) | 0.7 (0.7; 0.9) a | 0.9 (0.9; 1.1) | 0.9 (0.9; 1.1) b |
| Glucose (mmol/L) | 4.7 ± 0.3 1 | 4.8 (4.7; 4.9) | 4.8 (4.8; 5.0) b |
| HbA1c (%) | 5.0 ± 0.2 1 | 5.00 (5.0; 5.1) | 5.1 (4.2; 7.4) |
| hsCRP(mg/L) | 0.3 (0.4; 1.1) a | 0.56 (0.6; 1.9) | 0.6 (0.8; 4.2) b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grygorczuk, O.; Mrozik, M.; Lipert, A.; Kamińska, S.; Białas, A.; Drygas, W.; Rębowska, E.; Łęgocki, S.; Jegier, A.; Szmigielska, K.; et al. Cardiovascular Health and Diet Quality among Vegetarians, Vegans and Omnivores: Insights from a Large Urban Population in Poland. Nutrients 2024, 16, 3438. https://doi.org/10.3390/nu16203438
Grygorczuk O, Mrozik M, Lipert A, Kamińska S, Białas A, Drygas W, Rębowska E, Łęgocki S, Jegier A, Szmigielska K, et al. Cardiovascular Health and Diet Quality among Vegetarians, Vegans and Omnivores: Insights from a Large Urban Population in Poland. Nutrients. 2024; 16(20):3438. https://doi.org/10.3390/nu16203438
Chicago/Turabian StyleGrygorczuk, Oliwia, Martyna Mrozik, Anna Lipert, Sylwia Kamińska, Adam Białas, Wojciech Drygas, Ewa Rębowska, Stanisław Łęgocki, Anna Jegier, Katarzyna Szmigielska, and et al. 2024. "Cardiovascular Health and Diet Quality among Vegetarians, Vegans and Omnivores: Insights from a Large Urban Population in Poland" Nutrients 16, no. 20: 3438. https://doi.org/10.3390/nu16203438
APA StyleGrygorczuk, O., Mrozik, M., Lipert, A., Kamińska, S., Białas, A., Drygas, W., Rębowska, E., Łęgocki, S., Jegier, A., Szmigielska, K., & Kwaśniewska, M. (2024). Cardiovascular Health and Diet Quality among Vegetarians, Vegans and Omnivores: Insights from a Large Urban Population in Poland. Nutrients, 16(20), 3438. https://doi.org/10.3390/nu16203438








