Effectiveness of Universal Community Engagement Childhood Obesity Interventions at Improving Weight-Related and Behavioral Outcomes among Children and Adolescents: A Systematic Review and Meta-Analysis
Highlights
- Universal community engagement interventions are a feasible and viable way to address childhood obesity.
- Interventions that engage parents and focus on implementing both environmental and behavioral changes could be more beneficial for children.
- Researchers could collaborate with local community leaders to implement these interventions as part of the public healthcare system.
- Future interventions could prioritize incorporating more parental involvement, as well as simultaneously promoting positive changes in children’s environments and behaviors.
Abstract
1. Introduction
Aims
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Population
2.1.2. Intervention
2.1.3. Comparator
2.1.4. Outcomes
2.1.5. Study Design
2.1.6. Language and Publication Status
2.2. Study Selection
2.3. Data Extraction
2.4. Quality Appraisal
2.5. Data Synthesis
3. Results
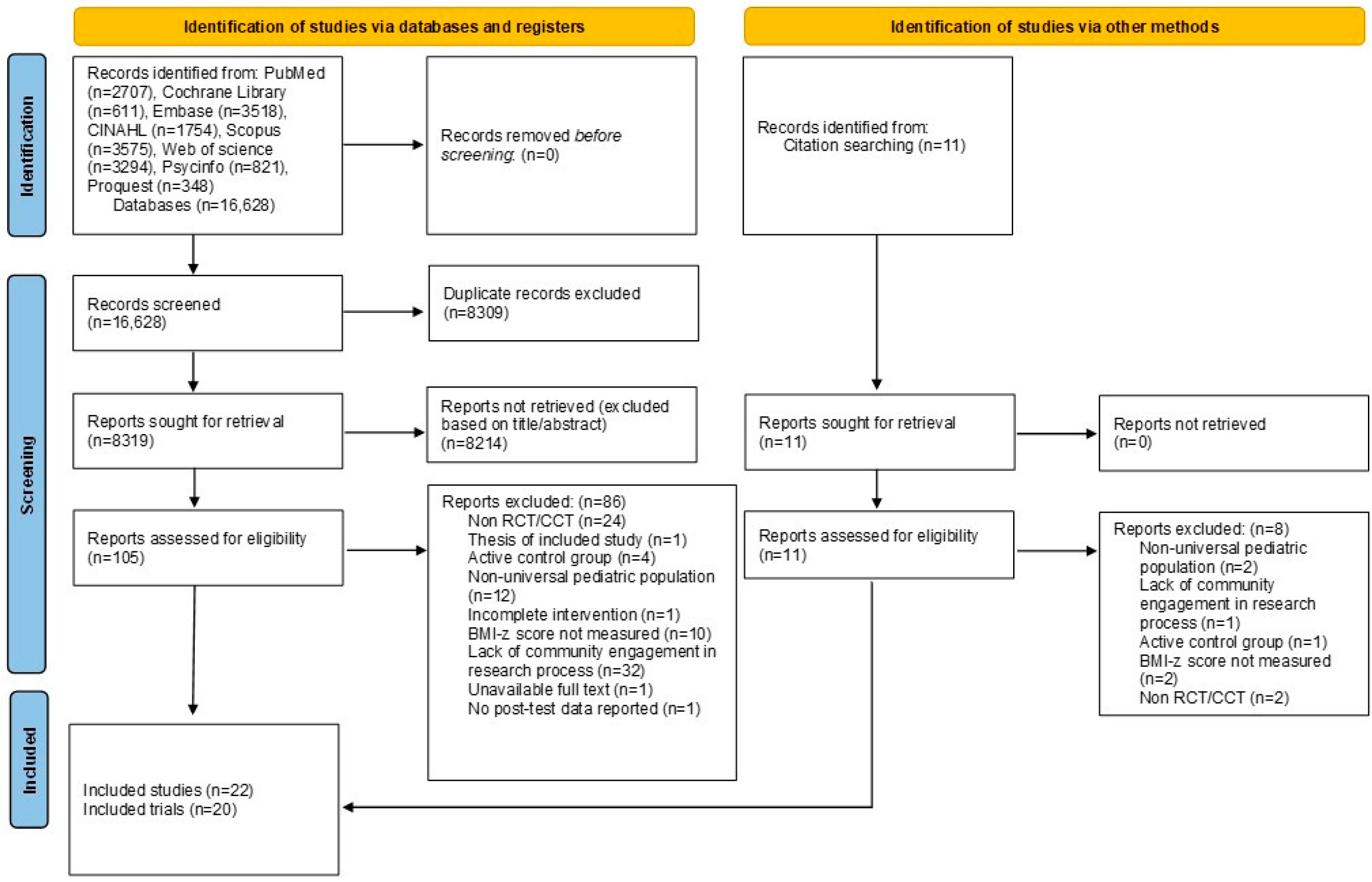
3.1. Search Outcomes
3.2. Characteristics of Included Studies
3.3. Quality Appraisal at Study Level
3.4. BMI-z Scores
3.5. Dietary Choices (Fruit, Vegetable, Sugar-Sweetened Beverage Intake)
3.5.1. Fruit Intake (Dichotomous Data)
3.5.2. Fruit Intake (Continuous Data)
3.5.3. Vegetable Intake (Dichotomous Data)
3.5.4. Vegetable Intake (Continuous Data)
3.5.5. Sugar-Sweetened Beverage Intake (Dichotomous Data)
3.5.6. Sugar-Sweetened Beverage Intake (Continuous Data)
3.6. Activity Levels (MVPA and Screen Time)
3.6.1. MVPA (Continuous Data)
3.6.2. Small Screen Time (Dichotomous Data)
3.6.3. Electronic Game Time (Dichotomous Data)
3.7. Quality Appraisal at Outcome Level
3.8. Narrative Synthesis
3.8.1. BMI-z Scores
3.8.2. Dietary Choices
3.8.3. Activity Levels
4. Discussion
4.1. Limitations
4.2. Implications for Future Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ling, J.; Chen, S.; Zahry, N.R.; Kao, T.-S.A. Economic burden of childhood overweight and obesity: A systematic review and meta-analysis. Obes. Rev. 2023, 24, e13535. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.T.; Krenek, A.; Magge, S.N. Childhood Obesity and Cardiovascular Disease Risk. Curr. Atheroscler. Rep. 2023, 25, 405–415. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adolescent Health. 2024. Available online: https://www.who.int/southeastasia/health-topics/adolescent-health (accessed on 15 February 2024).
- World Health Organization. Child—Demographics. 2024. Available online: https://platform.who.int/data/maternal-newborn-child-adolescent-ageing/child-data/child---demographics (accessed on 18 February 2024).
- Mahumud, R.A.; Sahle, B.W.; Owusu-Addo, E.; Chen, W.; Morton, R.L.; Renzaho, A.M.N. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int. J. Obes. 2021, 45, 2404–2418. [Google Scholar] [CrossRef]
- Porter, R.M.; Tindall, A.; Gaffka, B.J.; Kirk, S.; Santos, M.; Abraham-Pratt, I.; Gray, J.; Heckler, D.; Ward, W.L.; Tucker, J.M.; et al. A Review of Modifiable Risk Factors for Severe Obesity in Children Ages 5 and Under. Child. Obes. 2018, 14, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.-P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Peng, W.; Xue, H.; Wu, Y.; Zhou, H.; Jia, P.; Wang, Y. Spatial–temporal trends in global childhood overweight and obesity from 1975 to 2030: A weight mean center and projection analysis of 191 countries. Glob. Health 2023, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Blasco, B.V.; García-Jiménez, J.; Bodoano, I.; Gutiérrez-Rojas, L. Obesity and Depression: Its Prevalence and Influence as a Prognostic Factor: A Systematic Review. Psychiatry Investig. 2020, 17, 715–724. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.H. Endocrine comorbidities of pediatric obesity. Clin. Exp. Pediatr. 2021, 64, 619–627. [Google Scholar] [CrossRef]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef]
- Campbell, M.K. Biological, environmental, and social influences on childhood obesity. Pediatr. Res. 2016, 79, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Brunton, G.; Thomas, J.; O’Mara-Eves, A.; Jamal, F.; Oliver, S.; Kavanagh, J. Narratives of community engagement: A systematic review-derived conceptual framework for public health interventions. BMC Public Health 2017, 17, 944. [Google Scholar] [CrossRef]
- Gómez, S.F.; Casas Esteve, R.; Subirana, I.; Serra-Majem, L.; Fletas Torrent, M.; Homs, C.; Bawaked, R.A.; Estrada, L.; Fíto, M.; Schröder, H. Effect of a community-based childhood obesity intervention program on changes in anthropometric variables, incidence of obesity, and lifestyle choices in Spanish children aged 8 to 10 years. Eur. J. Pediatr. 2018, 177, 1531–1539. [Google Scholar] [CrossRef]
- Economos, C.D.; Hyatt, R.R.; Must, A.; Goldberg, J.P.; Kuder, J.; Naumova, E.N.; Collins, J.J.; Nelson, M.E. Shape Up Somerville two-year results: A community-based environmental change intervention sustains weight reduction in children. Prev. Med. 2013, 57, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Mast, M.; Asbeck, I.; Langnäse, K.; Grund, A. Prevention of obesity—Is it possible? Obes. Rev. 2001, 2, 15–28. [Google Scholar] [CrossRef]
- Wake, M.A.; McCallum, Z. Secondary prevention of overweight in primary school children: What place for general practice? Med. J. Aust. 2004, 181, 82–84. [Google Scholar] [CrossRef]
- Crespo, N.C.; Elder, J.P.; Ayala, G.X.; Slymen, D.J.; Campbell, N.R.; Sallis, J.F.; McKenzie, T.L.; Baquero, B.; Arredondo, E.M. Results of a Multi-level Intervention to Prevent and Control Childhood Obesity among Latino Children: The Aventuras Para Niños Study. Ann. Behav. Med. 2012, 43, 84–100. [Google Scholar] [CrossRef] [PubMed]
- Horan, M.; Gibney, E.; Molloy, E.; McAuliffe, F. Methodologies to assess paediatric adiposity. Ir. J. Med. Sci. 2015, 184, 53–68. [Google Scholar] [CrossRef]
- Jakobsen, D.D.; Brader, L.; Bruun, J.M. Association between Food, Beverages and Overweight/Obesity in Children and Adolescents—A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2023, 15, 764. [Google Scholar] [CrossRef]
- Liberali, R.; Kupek, E.; de Assis, M.A.A. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2019, 16, 70–85. [Google Scholar] [CrossRef]
- Nagata, J.M.; Smith, N.; Alsamman, S.; Lee, C.M.; Dooley, E.E.; Kiss, O.; Ganson, K.T.; Wing, D.; Baker, F.C.; Gabriel, K.P. Association of Physical Activity and Screen Time With Body Mass Index Among US Adolescents. JAMA Network Open 2023, 6, e2255466. [Google Scholar] [CrossRef] [PubMed]
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef] [PubMed]
- Boelsen-Robinson, T.; Peeters, A.; Beauchamp, A.; Chung, A.; Gearon, E.; Backholer, K. A systematic review of the effectiveness of whole-of-community interventions by socioeconomic position. Obes. Rev. 2015, 16, 806–816. [Google Scholar] [CrossRef]
- Krishnaswami, J.; Martinson, M.; Wakimoto, P.; Anglemeyer, A. Community-Engaged Interventions on Diet, Activity, and Weight Outcomes in U.S. Schools: A Systematic Review. Am. J. Prev. Med. 2012, 43, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Frerichs, L.; Ataga, O.; Corbie-Smith, G.; Tessler Lindau, S. Child and youth participatory interventions for addressing lifestyle-related childhood obesity: A systematic review. Obes. Rev. 2016, 17, 1276–1286. [Google Scholar] [CrossRef]
- Wolfenden, L.; Wyse, R.; Nichols, M.; Allender, S.; Millar, L.; McElduff, P. A systematic review and meta-analysis of whole of community interventions to prevent excessive population weight gain. Prev. Med. 2014, 62, 193–200. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Table 27. Obesity among Children and Adolescents Aged 2–19 Years, by Selected Characteristics: United States, Selected Years 1988–1994 through 2015–2018. 2019. Available online: https://www.cdc.gov/nchs/data/hus/2019/027-508.pdf (accessed on 31 August 2024).
- Centers for Disease Control and Prevention. Principles of Community Engagement, 2nd ed.; Clinical and Translational Science Awards (CTSA) Community Engagement Key Function Committee: La Jolla, CA, USA, 2011. Available online: https://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf (accessed on 20 January 2024).
- Skelton, J.A.; Palakshappa, D.; Moore, J.B.; Irby, M.B.; Montez, K.; Rhodes, S.D. Community engagement and pediatric obesity: Incorporating social determinants of health into treatment. J. Clin. Transl. Sci. 2019, 4, 279–285. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, H.-J. Use of Percentiles and Z-Scores in Anthropometry. In Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease; Preedy, V.R., Ed.; Springer: New York, NY, USA, 2012; pp. 29–48. [Google Scholar]
- Hariton, E.; Locascio, J.J. Randomised controlled trials—The gold standard for effectiveness research: Study design: Randomised controlled trials. BJOG 2018, 125, 1716. [Google Scholar] [CrossRef]
- Weijer, C.; Grimshaw, J.M.; Taljaard, M.; Binik, A.; Boruch, R.; Brehaut, J.C.; Donner, A.; Eccles, M.P.; Gallo, A.; McRae, A.D.; et al. Ethical issues posed by cluster randomized trials in health research. Trials 2011, 12, 100. [Google Scholar] [CrossRef]
- Jackson, S.L. Research Methods and Statistics: A Critical Thinking Approach, 4th ed.; Wadsworth Cengage Learning: Belmont, CA, USA, 2012. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.4; John Wiley & Sons: Chichester, UK, 2023; Available online: www.training.cochrane.org/handbook (accessed on 10 January 2024).
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2016, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Luo, D.; Weng, H.; Zeng, X.-T.; Lin, L.; Chu, H.; Tong, T. Optimally estimating the sample standard deviation from the five-number summary. Res. Synth. Methods 2020, 11, 641–654. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Kempler, L.; Sharpe, L.; Miller, C.B.; Bartlett, D.J. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Med. Rev. 2016, 29, 15–22. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, M.; Peterson, K.; Raina, P.; Chang, S.; Shekelle, P. Avoiding Bias in Selecting Studies. In Methods Guide for Effectiveness and Comparative Effectiveness Reviews; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2013. [Google Scholar]
- Phillips, V.; Barker, E. Systematic reviews: Structure, form and content. J. Perioper. Pract. 2021, 31, 349–353. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- GRADEpro. Available online: https://www.gradepro.org/ (accessed on 30 January 2024).
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. Appl. Stat. Methods 2009, 8, 597–599. [Google Scholar] [CrossRef]
- da Costa, B.R.; Nüesch, E.; Rutjes, A.W.; Johnston, B.C.; Reichenbach, S.; Trelle, S.; Guyatt, G.H.; Jüni, P. Combining follow-up and change data is valid in meta-analyses of continuous outcomes: A meta-epidemiological study. J. Clin. Epidemiol. 2013, 66, 847–855. [Google Scholar] [CrossRef]
- Rücker, G.; Cates, C.J.; Schwarzer, G. Methods for including information from multi-arm trials in pairwise meta-analysis. Res. Synth. Methods 2017, 8, 392–403. [Google Scholar] [CrossRef]
- Adab, P.; Pallan, M.J.; Lancashire, E.R.; Hemming, K.; Frew, E.; Barrett, T.; Bhopal, R.; Cade, J.E.; Canaway, A.; Clarke, J.L.; et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: Cluster randomised controlled trial (WAVES study). BMJ 2018, 360, k211. [Google Scholar] [CrossRef]
- Kremer, P.; Waqa, G.; Vanualailai, N.; Schultz, J.T.; Roberts, G.; Moodie, M.; Mavoa, H.; Malakellis, M.; McCabe, M.P.; Swinburn, B.A. Reducing unhealthy weight gain in Fijian adolescents: Results of the Healthy Youth Healthy Communities study. Obes. Rev. 2011, 12, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Malakellis, M.; Hoare, E.; Sanigorski, A.; Crooks, N.; Allender, S.; Nichols, M.; Swinburn, B.; Chikwendu, C.; Kelly, P.M.; Petersen, S.; et al. School-based systems change for obesity prevention in adolescents: Outcomes of the Australian Capital Territory ‘It’s Your Move!’. Aust. N. Z. J. Public Health 2017, 41, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; McAuley, K.A.; Barbezat, W.; Strong, A.; Williams, S.M.; Mann, J.I. APPLE Project: 2-y findings of a community-based obesity prevention program in primary school age children. Am. J. Clin. Nutr. 2007, 86, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Buch-Andersen, T.; Eriksson, F.; Bloch, P.; Glümer, C.; Mikkelsen, B.E.; Toft, U. The Danish SoL Project: Effects of a Multi-Component Community-Based Health Promotion Intervention on Prevention of Overweight among 3–8-Year-Old Children. Int. J. Environ. Res. Public Health 2021, 18, 8419. [Google Scholar] [CrossRef]
- Folta, S.C.; Kuder, J.F.; Goldberg, J.P.; Hyatt, R.R.; Must, A.; Naumova, E.N.; Nelson, M.E.; Economos, C.D. Changes in diet and physical activity resulting from the Shape Up Somerville community intervention. BMC Pediatr. 2013, 13, 157. [Google Scholar] [CrossRef]
- Elinder, L.S.; Heinemans, N.; Hagberg, J.; Quetel, A.-K.; Hagströmer, M. A participatory and capacity-building approach to healthy eating and physical activity—SCIP-school: A 2-year controlled trial. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 145. [Google Scholar] [CrossRef]
- Tomayko, E.J.; Prince, R.J.; Cronin, K.A.; Kim, K.; Parker, T.; Adams, A.K. The Healthy Children, Strong Families 2 (HCSF2) Randomized Controlled Trial Improved Healthy Behaviors in American Indian Families with Young Children. Curr. Dev. Nutr. 2019, 3, 53–62. [Google Scholar] [CrossRef]
- Black, M.M.; Hager, E.R.; Le, K.; Anliker, J.; Arteaga, S.S.; DiClemente, C.; Gittelsohn, J.; Magder, L.; Papas, M.; Snitker, S.; et al. Challenge! Health Promotion/Obesity Prevention Mentorship Model Among Urban, Black Adolescents. Pediatrics 2010, 126, 280–288. [Google Scholar] [CrossRef]
- Davis, S.M.; Myers, O.B.; Cruz, T.H.; Morshed, A.B.; Canaca, G.F.; Keane, P.C.; O’Donald, E.R. CHILE: Outcomes of a group randomized controlled trial of an intervention to prevent obesity in preschool Hispanic and American Indian children. Prev. Med. 2016, 89, 162–168. [Google Scholar] [CrossRef]
- Fotu, K.F.; Millar, L.; Mavoa, H.; Kremer, P.; Moodie, M.; Snowdon, W.; Utter, J.; Vivili, P.; Schultz, J.T.; Malakellis, M.; et al. Outcome results for the Ma’alahi Youth Project, a Tongan community-based obesity prevention programme for adolescents. Obes. Rev. 2011, 12, 41–50. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Horning, M.; Barr-Anderson, D.J.; Sidebottom, A.; Linde, J.A.; Lindberg, R.; Friend, S.; Beaudette, J.; Flattum, C.; Freese, R.L. Weight outcomes of NU-HOME: A randomized controlled trial to prevent obesity among rural children. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 29. [Google Scholar] [CrossRef] [PubMed]
- Kattelmann, K.K.; Meendering, J.R.; Hofer, E.J.; Merfeld, C.M.; Olfert, M.D.; Hagedorn, R.L.; Colby, S.E.; Franzen-Castle, L.; Moyer, J.; Mathews, D.R.; et al. The iCook 4-H Study: Report on Physical Activity and Sedentary Time in Youth Participating in a Multicomponent Program Promoting Family Cooking, Eating, and Playing Together. J. Nutr. Educ. Behav. 2019, 51, S30–S40. [Google Scholar] [CrossRef] [PubMed]
- Millar, L.; Kremer, P.; de Silva-Sanigorski, A.; McCabe, M.P.; Mavoa, H.; Moodie, M.; Utter, J.; Bell, C.; Malakellis, M.; Mathews, L.; et al. Reduction in overweight and obesity from a 3-year community-based intervention in Australia: The ‘It’s Your Move!’ project. Obes. Rev. 2011, 12, 20–28. [Google Scholar] [CrossRef]
- Peña, S.; Carranza, M.; Cuadrado, C.; Parra, D.C.; Villalobos Dintrans, P.; Castillo, C.; Cortinez-O’Ryan, A.; Espinoza, P.; Müller, V.; Rivera, C.; et al. Effectiveness of a Gamification Strategy to Prevent Childhood Obesity in Schools: A Cluster Controlled Trial. Obesity 2021, 29, 1825–1834. [Google Scholar] [CrossRef]
- Sanigorski, A.M.; Bell, A.C.; Kremer, P.J.; Cuttler, R.; Swinburn, B.A. Reducing unhealthy weight gain in children through community capacity-building: Results of a quasi-experimental intervention program, Be Active Eat Well. Int. J. Obes. 2008, 32, 1060–1067. [Google Scholar] [CrossRef]
- Scherr, R.E.; Linnell, J.D.; Dharmar, M.; Beccarelli, L.M.; Bergman, J.J.; Briggs, M.; Brian, K.M.; Feenstra, G.; Hillhouse, J.C.; Keen, C.L.; et al. A Multicomponent, School-Based Intervention, the Shaping Healthy Choices Program, Improves Nutrition-Related Outcomes. J. Nutr. Educ. Behav. 2017, 49, 368–379.e1. [Google Scholar] [CrossRef] [PubMed]
- White, A.A.; Colby, S.E.; Franzen-Castle, L.; Kattelmann, K.K.; Olfert, M.D.; Gould, T.A.; Hagedorn, R.L.; Mathews, D.R.; Moyer, J.; Wilson, K.; et al. The iCook 4-H Study: An Intervention and Dissemination Test of a Youth/Adult Out-of-School Program. J. Nutr. Educ. Behav. 2019, 51, S2–S20. [Google Scholar] [CrossRef]
- Wong, W.W.; Ortiz, C.L.; Stuff, J.E.; Mikhail, C.; Lathan, D.; Moore, L.A.; Alejandro, M.E.; Butte, N.F.; Smith, E.O.B. A Community-based Healthy Living Promotion Program Improved Self-esteem Among Minority Children. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 106–112. [Google Scholar] [CrossRef]
- Olsen, N.J.; Østergaard, J.N.; Bjerregaard, L.G.; Høy, T.V.; Kierkegaard, L.; Michaelsen, K.F.; Sørensen, T.I.A.; Grønbæk, M.K.; Bruun, J.M.; Heitmann, B.L. A literature review of evidence for primary prevention of overweight and obesity in healthy weight children and adolescents: A report produced by a working group of the Danish Council on Health and Disease Prevention. Obes. Rev. 2024, 25, e13641. [Google Scholar] [CrossRef]
- Stice, E.; Shaw, H.; Marti, C.N. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychol. Bull. 2006, 132, 667–691. [Google Scholar] [CrossRef]
- Yin, Z.; Parra-Medina, D.; Cordova, A.; He, M.; Trummer, V.; Sosa, E.; Gallion, K.J.; Sintes-Yallen, A.; Huang, Y.; Wu, X.; et al. Míranos! Look at Us, We Are Healthy! An Environmental Approach to Early Childhood Obesity Prevention. Child. Obes. 2012, 8, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Ling, J.; Gebremariam, M. Embracing parenting role in childhood obesity. BMC Public Health 2023, 23, 1118. [Google Scholar] [CrossRef]
- Kelishadi, R.; Azizi-Soleiman, F. Controlling childhood obesity: A systematic review on strategies and challenges. J. Res.Med. Sci. 2014, 19, 993–1008. [Google Scholar]
- World Health Organization. New WHO Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age. 2019. Available online: https://www.who.int/news/item/24-04-2019-to-grow-up-healthy-children-need-to-sit-less-and-play-more (accessed on 31 August 2024).
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 31 August 2024).
- World Health Organization. Guideline: Sugars Intake for Adults and Children. 2015. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 31 August 2024).
- Key, K.D.; Furr-Holden, D.; Lewis, E.Y.; Cunningham, R.; Zimmerman, M.A.; Johnson-Lawrence, V.; Selig, S. The Continuum of Community Engagement in Research: A Roadmap for Understanding and Assessing Progress. Prog. Community Health Partnersh. 2019, 13, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Lipek, T.; Igel, U.; Gausche, R.; Kiess, W.; Grande, G. Obesogenic environments: Environmental approaches to obesity prevention. J. Pediatr. Endocrinol. Metab. 2015, 28, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Campbell, R.; Hildon, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015, 9, 323–344. [Google Scholar] [CrossRef]
- Rodríguez-Ventura, A.L.; Pelaez-Ballestas, I.; Sámano-Sámano, R.; Jimenez-Gutierrez, C.; Aguilar-Salinas, C. Barriers to lose weight from the perspective of children with overweight/obesity and their parents: A sociocultural approach. J. Obes. 2014, 2014, 575184. [Google Scholar] [CrossRef]
- Walugembe, D.R.; Sibbald, S.; Le Ber, M.J.; Kothari, A. Sustainability of public health interventions: Where are the gaps? Health Res. Policy Syst. 2019, 17, 8. [Google Scholar] [CrossRef]
- Jakes, S.; Hardison-Moody, A.; Bowen, S.; Blevins, J. Engaging community change: The critical role of values in asset mapping. Community Dev. 2015, 46, 392–406. [Google Scholar] [CrossRef]
- Whelan, J.; Love, P.; Millar, L.; Allender, S.; Bell, C. Sustaining obesity prevention in communities: A systematic narrative synthesis review. Obes. Rev. 2018, 19, 839–851. [Google Scholar] [CrossRef]
- Burke, J.F.; Sussman, J.B.; Kent, D.M.; Hayward, R.A. Three simple rules to ensure reasonably credible subgroup analyses. BMJ 2015, 351, h5651. [Google Scholar] [CrossRef] [PubMed]
- Hollis, J.L.; Collins, C.E.; DeClerck, F.; Chai, L.K.; McColl, K.; Demaio, A.R. Defining healthy and sustainable diets for infants, children and adolescents. Glob. Food Secur. 2020, 27, 100401. [Google Scholar] [CrossRef]
| Study | Selection Bias: Random Sequence Generation | Selection Bias: Allocation Concealment | Performance Bias: Blinding of Participants and Personnel | Detection Bias: Blinding of Outcome Assessment (BMI-z Score) | Detection Bias: Blinding of Outcome Assessment (Secondary Outcomes) | Attrition Bias: Incomplete Outcome Data | Reporting Bias: Selective Reporting | Other Bias | Overall Bias |
|---|---|---|---|---|---|---|---|---|---|
| Adab et al., 2018 [49] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Black et al., 2010 [57] | Unclear risk | Unclear risk | Unclear risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Unclear risk |
| Buch-Andersen et al., 2021 [53] | High risk | Unclear risk | Low risk | Unclear risk | Not applicable (no secondary outcome assessed) | Low risk | Low risk | Low risk | High risk |
| Crespo et al., 2012 [19] | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Davis et al., 2016 [58] | Low risk | Unclear risk | Low risk | Unclear risk | Not applicable (no secondary outcome assessed) | Unclear risk | Unclear risk | Low risk | Unclear risk |
| Economos et al., 2013 [16] | High risk | Unclear risk | Low risk | Unclear risk | Not applicable (no secondary outcome assessed) | Low risk | Low risk | Low risk | High risk |
| Elinder et al., 2012 [55] | High risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Folta et al., 2013 [54] | High risk | Unclear risk | Low risk | Not applicable (no primary outcome assessed) | Low risk | Low risk | Low risk | Low risk | High risk |
| Fotu et al., 2011 [59] | High risk | Unclear risk | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | High risk |
| Fulkerson et al., 2022 [60] | Low risk | Unclear risk | High risk | High risk | Low risk | Low risk | Unclear risk | Low risk | High risk |
| Gómez et al., 2018 [15] | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | High risk | Low risk | High risk |
| Kattelmann et al., 2019 [61] | Low risk | Unclear risk | Unclear risk | Not applicable (no primary outcome assessed) | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Kremer et al., 2011 [50] | High risk | Unclear risk | Low risk | High risk | Low risk | High risk | Low risk | Unclear risk | High risk |
| Malakellis et al., 2017 [51] | High risk | High risk | Low risk | High risk | High risk | High risk | Low risk | Unclear risk | High risk |
| Millar et al., 2011 [62] | High risk | Unclear risk | Low risk | Unclear risk | Low risk | High risk | Low risk | Unclear risk | High risk |
| Peña et al.,2021 [63] | High risk | Unclear risk | Low risk | Low risk | Not applicable (no secondary outcome assessed) | Low risk | Low risk | Low risk | High risk |
| Sanigorski et al., 2008 [64] | High risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk | High risk |
| Scherr et al., 2017 [65] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Taylor et al., 2007 [52] | High risk | Unclear risk | Low risk | Unclear risk | Unclear risk | High risk | Low risk | Low risk | High risk |
| Tomayko et al., 2019 [56] | Low risk | Unclear risk | High risk | Unclear risk | High risk | Unclear risk | High risk | High risk | High risk |
| White et al., 2019 [66] | Low risk | Unclear risk | Unclear risk | Unclear risk | Not applicable (no secondary outcome assessed) | Low risk | Low risk | Low risk | Unclear risk |
| Wong et al., 2016 [67] | High risk | Unclear risk | Low risk | Unclear risk | Low risk | High risk | Low risk | Unclear risk | High risk |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koh, P.Y.; Chua, J.Y.X.; Chan, P.Y.; Shorey, S. Effectiveness of Universal Community Engagement Childhood Obesity Interventions at Improving Weight-Related and Behavioral Outcomes among Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 3465. https://doi.org/10.3390/nu16203465
Koh PY, Chua JYX, Chan PY, Shorey S. Effectiveness of Universal Community Engagement Childhood Obesity Interventions at Improving Weight-Related and Behavioral Outcomes among Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients. 2024; 16(20):3465. https://doi.org/10.3390/nu16203465
Chicago/Turabian StyleKoh, Pei Yong, Joelle Yan Xin Chua, Pao Yi Chan, and Shefaly Shorey. 2024. "Effectiveness of Universal Community Engagement Childhood Obesity Interventions at Improving Weight-Related and Behavioral Outcomes among Children and Adolescents: A Systematic Review and Meta-Analysis" Nutrients 16, no. 20: 3465. https://doi.org/10.3390/nu16203465
APA StyleKoh, P. Y., Chua, J. Y. X., Chan, P. Y., & Shorey, S. (2024). Effectiveness of Universal Community Engagement Childhood Obesity Interventions at Improving Weight-Related and Behavioral Outcomes among Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients, 16(20), 3465. https://doi.org/10.3390/nu16203465







