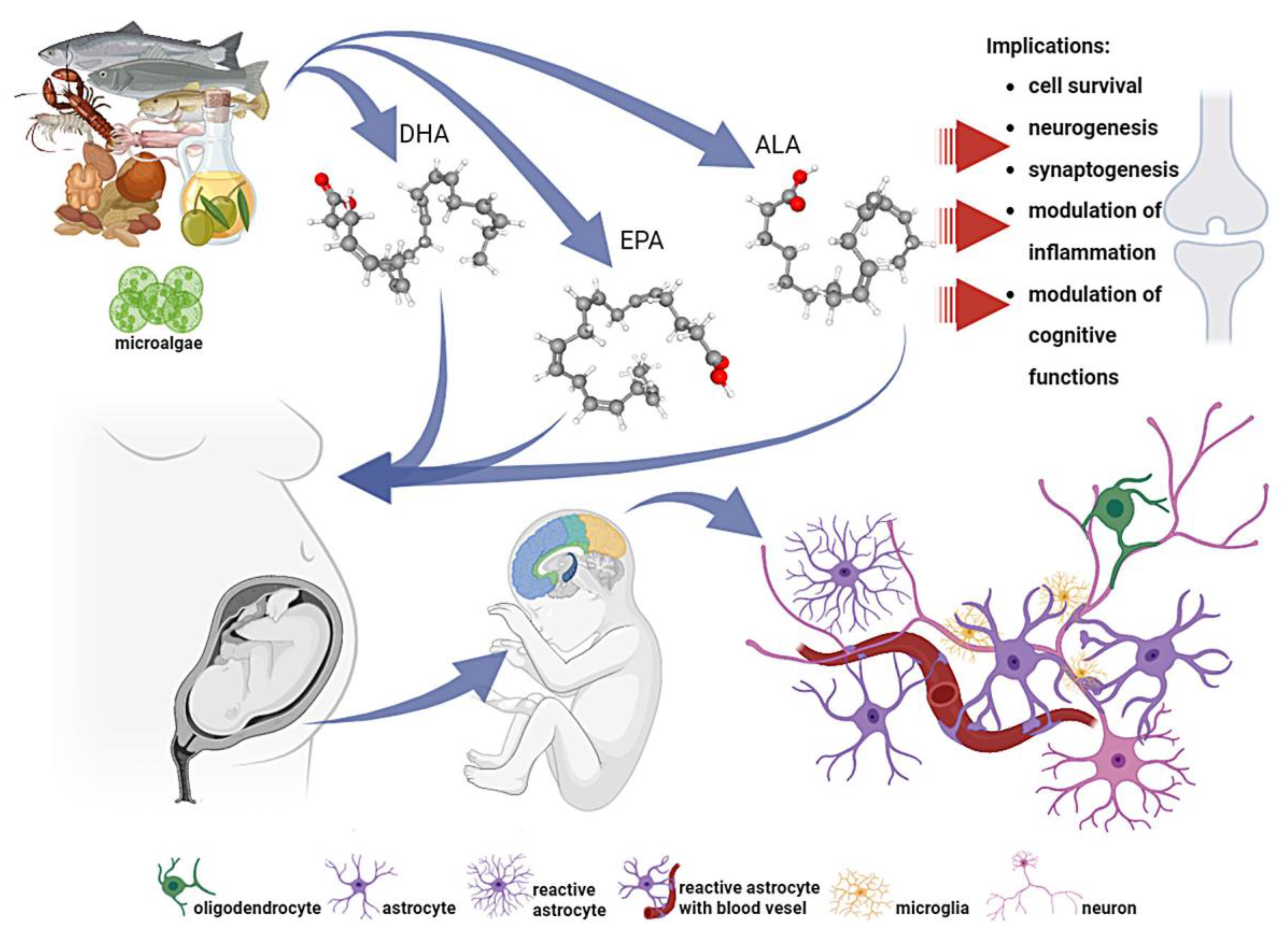
Nutritional Quality Implications: Exploring the Impact of a Fatty Acid-Rich Diet on Central Nervous System Development
Abstract
1. Introduction
2. The Types of Fatty Acids
3. Nutritional Importance of Fatty Acids
4. Dietary Sources of Fatty Acids
5. Omega-3 Polyunsaturated Fatty Acids in Brain Health: Structural and Functional Impacts of Docosahexaenoic Acid on Neural Development and Homeostasis
6. Impact of Malnutrition on Neurodevelopment and Child Health
7. Cognitive Dysfunction in Children and Fatty Acids
8. Polyunsaturated Fatty Acids in Neurodevelopmental Disorders: Therapeutic Potential and Clinical Insights
8.1. ADHD
8.2. Autistic Spectrum Disorders
8.3. Depression
9. Broader Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ALA | α-linolenic acid |
| DHA | all-cis-docosa-4,7,10,13,16,19-hexaenoic acid |
| EFAs | Essential fatty acids |
| EPA | all-cis-5,8,11,14,17-eicosapentaenoic acid |
| FA/FAs | Fatty acid/fatty acids |
| GLA | Gamma linolic acid |
| LA | Linolic acid |
| LC-PUFAs | Long-chain polyunsaturated fatty acids |
| PUFA | Polyunsaturated fatty acid |
| TAGs | Triacylglycerols |
| VLCFAs | Very-long-chain fatty acids |
References
- Dighriri, I.M.; Alsubaie, A.M.; Hakami, F.M.; Hamithi, D.M.; Alshekh, M.M.; Khobrani, F.A.; Dalak, F.E.; Hakami, A.A.; Alsueaadi, E.H.; Alsaawi, L.S.; et al. Effects of Omega-3 Polyunsaturated Fatty Acids on Brain Functions: A Systematic Review. Cureus 2022, 14, e30091. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.C.; Pariante, C.M.; Su, K.P. Omega-3 fatty acids in the psychological and physiological resilience against COVID-19. Prostaglandins Leukot. Essent. Fat. Acids 2020, 161, 102177. [Google Scholar] [CrossRef] [PubMed]
- Dinicolantonio, J.J.; O’keefe, J.H. The importance of marine OMEGA-3S for brain development and the prevention and treatment of behavior, mood, and other brain disorders. Nutrients 2020, 12, 2333. [Google Scholar] [CrossRef] [PubMed]
- Lehner, A.; Staub, K.; Aldakak, L.; Eppenberger, P.; Rühli, F.; Martin, R.D.; Bender, N. Impact of omega-3 fatty acid DHA and EPA supplementation in pregnant or breast-feeding women on cognitive performance of children: Systematic review and meta-analysis. Nutr. Rev. 2021, 79, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Verfuerden, M.L.; Dib, S.; Jerrim, J.; Fewtrell, M.; Gilbert, R.E. Effect of long-chain polyunsaturated fatty acids in infant formula on long-term cognitive function in childhood: A systematic review and meta-analysis of randomised controlled trials. PLoS ONE 2020, 15, e0241800. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, B.; Kapoor, D.; Gautam, S.; Singh, R.; Bhardwaj, S. Dietary Polyunsaturated Fatty Acids (PUFAs): Uses and Potential Health Benefits. Curr. Nutr. Rep. 2021, 10, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, F.; Ambigaipalan, P. Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu. Rev. Food Sci. Technol. 2018, 9, 345–381. [Google Scholar] [CrossRef] [PubMed]
- Saini, R.K.; Keum, Y.S. Omega-3 and omega-6 polyunsaturated fatty acids: Dietary sources, metabolism, and significance—A review. Life Sci. 2018, 203, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.J.; Miles, E.A.; Burdge, G.C.; Yaqoob, P.; Calder, P.C. Metabolism and functional effects of plant-derived omega-3 fatty acids in humans. Prog. Lipid Res. 2016, 64, 30–56. [Google Scholar] [CrossRef] [PubMed]
- Goyens, P.L.L.; Spilker, M.E.; Zock, P.L.; Katan, M.B.; Mensink, R.P. Conversion of α-linolenic acid in humans is influenced by the absolute amounts of α-linolenic acid and linoleic acid in the diet and not by their ratio. Am. J. Clin. Nutr. 2006, 84, 44–53. [Google Scholar] [CrossRef]
- Metherel, A.H.; Bazinet, R.P. Updates to the n-3 polyunsaturated fatty acid biosynthesis pathway: DHA synthesis rates, tetracosahexaenoic acid and (minimal) retroconversion. Prog. Lipid Res. 2019, 76, 101008. [Google Scholar] [CrossRef] [PubMed]
- Bourre, J.M. Dietary omega-3 fatty acids for women. Biomed. Pharmacother. 2007, 61, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 2002, 56, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Howard, T.D.; Mathias, R.A.; Seeds, M.C.; Herrington, D.M.; Hixson, J.E.; Shimmin, L.C.; Hawkins, G.A.; Sellers, M.; Ainsworth, H.C.; Sergeant, S.; et al. DNA methylation in an enhancer region of the FADS cluster is associated with FADS activity in human liver. PLoS ONE 2014, 9, e97510. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B.; Minihane, A.M.; Saleh, R.N.M.; Risérus, U. Intake and metabolism of omega-3 and omega-6 polyunsaturated fatty acids: Nutritional implications for cardiometabolic diseases. Lancet Diabetes Endocrinol. 2020, 8, 915–930. [Google Scholar] [CrossRef] [PubMed]
- Van Dael, P. Role of n-3 long-chain polyunsaturated fatty acids in human nutrition and health: Review of recent studies and recommendations. Nutr. Res. Pract. 2021, 15, 137–159. [Google Scholar] [CrossRef] [PubMed]
- Burlingame, B.; Nishida, C.; Uauy, R.; Weisell, R. Fats and fatty acids in human nutrition: Introduction. Ann. Nutr. Metab. 2009, 55, 5–7. [Google Scholar] [CrossRef] [PubMed]
- WHO. Fats and Fatty Acids in Human Nutrition. Available online: https://www.who.int/news-room/events/detail/2008/11/10/default-calendar/fats-and-fatty-acids-in-human-nutrition (accessed on 5 December 2023).
- NIH. Omega-3 Fatty Acids—Health Professional Fact Sheet. Available online: https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/#ref%0Ahttps://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/ (accessed on 12 December 2023).
- National Institutes of Health Omega-3 Fatty Acids. Available online: https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/#en5 (accessed on 2 December 2023).
- EFSA. Dietary Reference Values for nutrients Summary report. EFSA Support. Publ. 2017, 14, e15121E. [Google Scholar]
- Sande, D.; de Oliveira, G.P.; e Moura, M.A.F.; Martins, B.d.A.; Lima, M.T.N.S.; Takahashi, J.A. Edible mushrooms as a ubiquitous source of essential fatty acids. Food Res. Int. 2019, 125, 108524. [Google Scholar] [CrossRef] [PubMed]
- Harwood, J.L. Algae: Critical sources of very long-chain polyunsaturated fatty acids. Biomolecules 2019, 9, 708. [Google Scholar] [CrossRef] [PubMed]
- Rocha, C.P.; Pacheco, D.; Cotas, J.; Marques, J.C.; Pereira, L.; Gonçalves, A.M.M. Seaweeds as valuable sources of essential fatty acids for human nutrition. Int. J. Environ. Res. Public Health 2021, 18, 4968. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture; Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 24; U.S. Department of Agriculture: Beltsville, MD, USA, 2011.
- Thompson, M.; Hein, N.; Hanson, C.; Smith, L.M.; Anderson-Berry, A.; Richter, C.K.; Bisselou, K.S.; Appiah, A.K.; Kris-Etherton, P.; Skulas-Ray, A.C.; et al. Omega-3 fatty acid intake by age, gender, and pregnancy status in the United States: National health and nutrition examination survey 2003–2014. Nutrients 2019, 11, 177. [Google Scholar] [CrossRef] [PubMed]
- Bos, D.J.; van Montfort, S.J.T.; Oranje, B.; Durston, S.; Smeets, P.A.M. Effects of omega-3 polyunsaturated fatty acids on human brain morphology and function: What is the evidence? Eur. Neuropsychopharmacol. 2016, 26, 546–561. [Google Scholar] [CrossRef] [PubMed]
- Jové, M.; Pradas, I.; Dominguez-Gonzalez, M.; Ferrer, I.; Pamplona, R. Lipids and lipoxidation in human brain aging. Mitochondrial ATP-synthase as a key lipoxidation target. Redox Biol. 2019, 23, 101082. [Google Scholar] [CrossRef] [PubMed]
- Watkins, P.A.; Hamilton, J.A.; Leaf, A.; Spector, A.A.; Moore, S.A.; Anderson, R.E.; Moser, H.W.; Noetzel, M.J.; Katz, R. Brain uptake and utilization of fatty acids: Applications to peroxisomal biogenesis diseases. Proc. J. Mol. Neurosci. 2001, 16, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Tracey, T.J.; Steyn, F.J.; Wolvetang, E.J.; Ngo, S.T. Neuronal lipid metabolism: Multiple pathways driving functional outcomes in health and disease. Front. Mol. Neurosci. 2018, 11, 10. [Google Scholar] [CrossRef]
- Martinez, M. Tissue levels of polyunsaturated fatty acids during early human development. J. Pediatr. 1992, 120, PS129–PS138. [Google Scholar] [CrossRef]
- Farooqui, A.A. Beneficial Effects of Fish Oil on Human Brain; Springer: Berlin/Heidelberg, Germany, 2009; ISBN 9781441905437. [Google Scholar]
- Tanaka, K.; Farooqui, A.A.; Siddiqi, N.J.; Alhomida, A.S.; Ong, W.Y. Effects of docosahexaenoic acid on neurotransmission. Biomol. Ther. 2012, 20, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Spector, A.A.; Xiong, Z.M. A synaptogenic amide N-docosahexaenoylethanolamide promotes hippocampal development. Prostaglandins Other Lipid Mediat. 2011, 96, 114–120. [Google Scholar] [CrossRef]
- Hashimoto, M.; Hossain, S.; Al Mamun, A.; Matsuzaki, K.; Arai, H. Docosahexaenoic acid: One molecule diverse functions. Crit. Rev. Biotechnol. 2017, 37, 579–597. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Hossain, S. Fatty Acids: From Membrane Ingredients to Signaling Molecules. In Biochemistry and Health Benefits of Fatty Acids; IntechOpen: London, UK, 2018. [Google Scholar]
- Joffre, C. Polyunsaturated Fatty Acid Metabolism in the Brain and Brain Cells. In Feed Your Mind—How Does Nutrition Modulate Brain Function throughout Life? IntechOpen: London, UK, 2019. [Google Scholar]
- Sinclair, A.J. Docosahexaenoic acid and the brain—What is its role? Asia Pac. J. Clin. Nutr. 2019, 28, 675–688. [Google Scholar] [PubMed]
- Barber, C.N.; Raben, D.M. Lipid metabolism crosstalk in the brain: Glia and neurons. Front. Cell. Neurosci. 2019, 13, 212. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, F.; Nishinaka, T.; Yamashita, T.; Nakamoto, K.; Koyama, Y.; Kasuya, F.; Tokuyama, S. Astrocytes release polyunsaturated fatty acids by lipopolysaccharide stimuli. Biol. Pharm. Bull. 2016, 39, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Mencarelli, C.; Martinez-Martinez, P. Ceramide function in the brain: When a slight tilt is enough. Cell. Mol. Life Sci. 2013, 70, 181–203. [Google Scholar] [CrossRef] [PubMed]
- Joffre, C.; Rey, C.; Layé, S. N-3 polyunsaturated fatty acids and the resolution of neuroinflammation. Front. Pharmacol. 2019, 10, 1022. [Google Scholar] [CrossRef] [PubMed]
- Tabernero, A.; Lavado, E.M.; Granda, B.; Velasco, A.; Medina, J.M. Neuronal differentiation is triggered by oleic acid synthesized and released by astrocytes. J. Neurochem. 2001, 79, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C.N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 2014, 510, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Huang, B.X.; Kwon, H.S.; Rashid, M.A.; Kharebava, G.; Desai, A.; Patnaik, S.; Marugan, J.; Kim, H.Y. Orphan GPR110 (ADGRF1) targeted by N-docosahexaenoylethanolamine in development of neurons and cognitive function. Nat. Commun. 2016, 7, 13123. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.X.; Chen, H.; Joo, Y.; Kwon, H.S.; Fu, C.; Spector, A.A.; Kim, H.Y. Interaction between GPR110 (ADGRF1) and tight junction protein occludin implicated in blood-brain barrier permeability. iScience 2023, 26, 106550. [Google Scholar] [CrossRef]
- Niaudet, C.; Hofmann, J.J.; Mäe, M.A.; Jung, B.; Gaengel, K.; Vanlandewijck, M.; Ekvärn, E.; Salvado, M.D.; Mehlem, A.; Al Sayegh, S.; et al. Gpr116 receptor regulates distinctive functions in pneumocytes and vascular endothelium. PLoS ONE 2015, 10, e0137949. [Google Scholar] [CrossRef] [PubMed]
- Langenhan, T.; Piao, X.; Monk, K.R. Adhesion G protein-coupled receptors in nervous system development and disease. Nat. Rev. Neurosci. 2016, 17, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Nakamoto, K.; Nishinaka, T.; Matsumoto, K.; Kasuya, F.; Mankura, M.; Koyama, Y.; Tokuyama, S. Involvement of the long-chain fatty acid receptor GPR40 as a novel pain regulatory system. Brain Res. 2012, 1432, 74–83. [Google Scholar] [CrossRef]
- Nakamoto, K.; Nishinaka, T.; Sato, N.; Aizawa, F.; Yamashita, T.; Mankura, M.; Koyama, Y.; Kasuya, F.; Tokuyama, S. The activation of supraspinal GPR40/FFA1 receptor signalling regulates the descending pain control system. Br. J. Pharmacol. 2015, 172, 1250–1262. [Google Scholar] [CrossRef] [PubMed]
- Petermann, A.B.; Reyna-Jeldes, M.; Ortega, L.; Coddou, C.; Yévenes, G.E. Roles of the Unsaturated Fatty Acid Docosahexaenoic Acid in the Central Nervous System: Molecular and Cellular Insights. Int. J. Mol. Sci. 2022, 23, 5390. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi Fard, S.; Cameron-Smith, D.; Sinclair, A.J. N–3 Docosapentaenoic acid: The iceberg n–3 fatty acid. Curr. Opin. Clin. Nutr. Metab. Care 2021, 24, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.F.; Makrides, M.; Gibson, R.A.; Sullivan, T.R.; McPhee, A.J.; Anderson, P.J.; Best, K.P.; Sharp, M.; Cheong, J.L.Y.; Opie, G.F.; et al. Neonatal Docosahexaenoic Acid in Preterm Infants and Intelligence at 5 Years. N. Engl. J. Med. 2022, 387, 1579–1588. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, A.J.; Wang, Y.; Li, D. What Is the Evidence for Dietary-Induced DHA Deficiency in Human Brains? Nutrients 2022, 15, 161. [Google Scholar] [CrossRef] [PubMed]
- Zerbeto, A.B.; Cortelo, F.M.; Filho, É.B.C. Association between gestational age and birth weight on the language development of Brazilian children: A systematic review. J. Pediatr. 2015, 91, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.L.; Bailey, L.B.; Pietrzik, K.; Shane, B.; Holzgreve, W. Micronutrients and women of reproductive potential: Required dietary intake and consequences of dietary deficienty or excess. Part II—Vitamin D, vitamin A, iron, zinc, iodine, essential fatty acids. J. Matern. Neonatal Med. 2011, 24, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Reyes, L.; Mañalich, R. Long-term consequences of low birth weight. Kidney Int. 2005, 68, S107–S111. [Google Scholar] [CrossRef] [PubMed]
- Anjos, T.; Altmäe, S.; Emmett, P.; Tiemeier, H.; Closa-Monasterolo, R.; Luque, V.; Wiseman, S.; Pérez-García, M.; Lattka, E.; Demmelmair, H.; et al. Nutrition and neurodevelopment in children: Focus on NUTRIMENTHE project. Eur. J. Nutr. 2013, 52, 1825–1842. [Google Scholar] [CrossRef] [PubMed]
- Czeizel, A.E.; Dudás, I. Prevention of the First Occurrence of Neural-Tube Defects by Periconceptional Vitamin Supplementation. N. Engl. J. Med. 1992, 327, 1832–1835. [Google Scholar] [CrossRef] [PubMed]
- Basak, S.; Vilasagaram, S.; Duttaroy, A.K. Maternal dietary deficiency of n-3 fatty acids affects metabolic and epigenetic phenotypes of the developing fetus. Prostaglandins Leukot. Essent. Fat. Acids 2020, 158, 102109. [Google Scholar] [CrossRef] [PubMed]
- Medicine, I. Seafood Choices: Balancing Benefits and Risks; Nesheim, M.C., Yaktine, A.L., Eds.; The National Academies Press: Washington, DC, USA, 2007; ISBN 978-0-309-10218-6. [Google Scholar]
- Marshall, N.E.; Abrams, B.; Barbour, L.A.; Catalano, P.; Christian, P.; Friedman, J.E.; Hay, W.W.; Hernandez, T.L.; Krebs, N.F.; Oken, E.; et al. The importance of nutrition in pregnancy and lactation: Lifelong consequences. Am. J. Obstet. Gynecol. 2022, 226, 607–632. [Google Scholar] [CrossRef] [PubMed]
- Van Pelt, A.E.; Lipow, M.I.; Scott, J.C.; Lowenthal, E.D. Interventions for children with neurocognitive impairments in resource-limited settings: A systematic review. Child. Youth Serv. Rev. 2020, 118, 105393. [Google Scholar] [CrossRef] [PubMed]
- Dooling, E.C. Cognitive disorders in children. Curr. Opin. Pediatr. 1993, 5, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Chmielewska, A.; Dziechciarz, P.; Gieruszczak-Białek, D.; Horvath, A.; Pieścik-Lech, M.; Ruszczyński, M.; Skórka, A.; Szajewska, H. Effects of prenatal and/or postnatal supplementation with iron, PUFA or folic acid on neurodevelopment: Update. Br. J. Nutr. 2019, 122, S10–S15. [Google Scholar] [CrossRef] [PubMed]
- Nickels, K.C.; Zaccariello, M.J.; Hamiwka, L.D.; Wirrell, E.C. Cognitive and neurodevelopmental comorbidities in paediatric epilepsy. Nat. Rev. Neurol. 2016, 12, 465–476. [Google Scholar] [CrossRef]
- Brooks, B.L.; Iverson, G.L.; Sherman, E.M.S.; Roberge, M.C. Identifying cognitive problems in children and adolescents with wepression using computerized neuropsychological testing. Appl. Neuropsychol. 2010, 17, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Lipkin, P.H. Childhood Cognitive Disorders, 2nd ed.; Johnston, M.V., Gross, R., Eds.; Oxford University Press: New York, NY, USA, 2010; ISBN 9780195146837. [Google Scholar]
- Morrison, S.; Chawner, S.J.R.A.; van Amelsvoort, T.A.M.J.; Swillen, A.; Vingerhoets, C.; Vergaelen, E.; Linden, D.E.J.; Linden, S.; Owen, M.J.; van den Bree, M.B.M. Cognitive deficits in childhood, adolescence and adulthood in 22q11.2 deletion syndrome and association with psychopathology. Transl. Psychiatry 2020, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Compas, B.E.; Jaser, S.S.; Reeslund, K.; Patel, N.; Yarboi, J. Neurocognitive deficits in children with chronic health conditions. Am. Psychol. 2017, 72, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Bryan, J.; Osendarp, S.; Hughes, D.; Calvaresi, E.; Baghurst, K.; Van Klinken, J.W. Nutrients for cognitive development in school-aged children. Nutr. Rev. 2004, 62, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Helland, I.B.; Smith, L.; Blomen, B.; Saarem, K.; Saugstad, O.D.; Drevon, C.A. Effect of supplementing pregnant and lactating mothers with n-3 very-long-chain fatty acids on children’s iq and body mass index at 7 years of age. Pediatrics 2008, 122, e472–e479. [Google Scholar] [CrossRef]
- Cohen, J.T.; Bellinger, D.C.; Connor, W.E.; Shaywitz, B.A. A quantitative analysis of prenatal intake of n-3 polyunsaturated fatty acids and cognitive development. Am. J. Prev. Med. 2005, 29, P366. [Google Scholar] [CrossRef] [PubMed]
- Zou, R.; El Marroun, H.; Voortman, T.; Hillegers, M.; White, T.; Tiemeier, H. Maternal polyunsaturated fatty acids during pregnancy and offspring brain development in childhood. Am. J. Clin. Nutr. 2021, 114, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Stonehouse, W. Does consumption of LC omega-3 PUFA enhance cognitive performance in healthy school-aged children and throughout adulthood? Evidence from clinical trials. Nutrients 2014, 6, 2730–2758. [Google Scholar] [CrossRef] [PubMed]
- Clandinin, M.T.; Chappell, J.E.; Leong, S.; Heim, T.; Swyer, P.R.; Chance, G.W. Intrauterine fatty acid accretion rates in human brain: Implications for fatty acid requirements. Early Hum. Dev. 1980, 4, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Allotey, J.; Zamora, J.; Cheong-See, F.; Kalidindi, M.; Arroyo-Manzano, D.; Asztalos, E.; van der Post, J.A.M.; Mol, B.W.; Moore, D.; Birtles, D.; et al. Cognitive, motor, behavioural and academic performances of children born preterm: A meta-analysis and systematic review involving 64 061 children. BJOG An Int. J. Obstet. Gynaecol. 2018, 125, 16–25. [Google Scholar] [CrossRef]
- Twilhaar, E.S.; Wade, R.M.; De Kieviet, J.F.; Van Goudoever, J.B.; Van Elburg, R.M.; Oosterlaan, J. Cognitive outcomes of children born extremely or very preterm since the 1990s and associated risk factors: A meta-analysis and meta-regression. JAMA Pediatr. 2018, 172, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Burnett, A.C.; Youssef, G.; Anderson, P.J.; Duff, J.; Doyle, L.W.; Cheong, J.L.Y. Exploring the “preterm Behavioral Phenotype” in Children Born Extremely Preterm. J. Dev. Behav. Pediatr. 2019, 40, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Julvez, J.; Méndez, M.; Fernandez-Barres, S.; Romaguera, D.; Vioque, J.; Llop, S.; Ibarluzea, J.; Guxens, M.; Avella-Garcia, C.; Tardón, A.; et al. Maternal consumption of seafood in pregnancy and child neuropsychological development: A longitudinal study based on a population with high consumption levels. Am. J. Epidemiol. 2016, 183, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Davidson, P.W.; Cory-Slechta, D.A.; Thurston, S.W.; Huang, L.S.; Shamlaye, C.F.; Gunzler, D.; Watson, G.; van Wijngaarden, E.; Zareba, G.; Klein, J.D.; et al. Fish consumption and prenatal methylmercury exposure: Cognitive and behavioral outcomes in the main cohort at 17 years from the Seychelles child development study. Neurotoxicology 2011, 32, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Daniels, J.L.; Longnecker, M.P.; Rowland, A.S.; Golding, J. Fish intake during pregnancy and early cognitive development of offspring. Epidemiology 2004, 15, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Hibbeln, J.R.; Davis, J.M.; Steer, C.; Emmett, P.; Rogers, I.; Williams, C.; Golding, J. Maternal seafood consumption in pregnancy and neurodevelopmental outcomes in childhood (ALSPAC study): An observational cohort study. Lancet 2007, 369, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Shulkin, M.; Pimpin, L.; Bellinger, D.; Kranz, S.; Fawzi, W.; Duggan, C.; Mozaffarian, D. N-3 fatty acid supplementation in mothers, preterm infants, and term infants and childhood psychomotor and visual development: A systematic review and meta-analysis. J. Nutr. 2018, 148, 409–418. [Google Scholar] [CrossRef]
- Jasani, B.; Simmer, K.; Patole, S.K.; Rao, S.C. Long chain polyunsaturated fatty acid supplementation in infants born at term. Cochrane Database Syst. Rev. 2017, 2017, CD000376. [Google Scholar] [CrossRef]
- Meldrum, S.; Simmer, K. Docosahexaenoic acid and neurodevelopmental outcomes of term infants. Ann. Nutr. Metab. 2016, 69, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Simmer, K. Fish-oil supplementation: The controversy continues. Am. J. Clin. Nutr. 2016, 103, 1–2. [Google Scholar] [CrossRef][Green Version]
- Hadders-Algra, M. Prenatal and early postnatal supplementation with long-chain polyunsaturated fatty acids: Neurodevelopmental considerations. Proc. Am. J. Clin. Nutr. 2011, 94, S1874–S1879. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.F.; Smithers, L.G.; Makrides, M. The effect of maternal omega-3 (n23) LCPUFA supplementation during pregnancy on early childhood cognitive and visual development: A systematic review and meta-analysis of randomized controlled trials1-3. Am. J. Clin. Nutr. 2013, 97, 531–544. [Google Scholar] [CrossRef]
- Delgado-Noguera, M.F.; Calvache, J.A.; Bonfill Cosp, X.; Kotanidou, E.P.; Galli-Tsinopoulou, A. Supplementation with long chain polyunsaturated fatty acids (LCPUFA) to breastfeeding mothers for improving child growth and development. Cochrane Database Syst. Rev. 2015, 2015, CD007901. [Google Scholar] [CrossRef] [PubMed]
- Dziechciarz, P.; Horvath, A.; Szajewska, H. Effects of n-3 long-chain polyunsaturated fatty acid supplementation during pregnancy and/or lactation on neurodevelopment and visual function in children: A systematic review of randomized controlled trials. J. Am. Coll. Nutr. 2010, 29, 443–454. [Google Scholar] [CrossRef]
- Emery, S.; Häberling, I.; Berger, G.; Walitza, S.; Schmeck, K.; Albert, T.; Baumgartner, N.; Strumberger, M.; Albermann, M.; Drechsler, R. Omega-3 and its domain-specific effects on cognitive test performance in youths: A meta-analysis. Neurosci. Biobehav. Rev. 2020, 112, 420–436. [Google Scholar] [CrossRef] [PubMed]
- Nevins, J.E.H.; Donovan, S.M.; Snetselaar, L.; Dewey, K.G.; Novotny, R.; Stang, J.; Taveras, E.M.; Kleinman, R.E.; Bailey, R.L.; Raghavan, R.; et al. Omega-3 Fatty Acid Dietary Supplements Consumed during Pregnancy and Lactation and Child Neurodevelopment: A Systematic Review. J. Nutr. 2021, 151, 3483–3494. [Google Scholar] [CrossRef] [PubMed]
- van der Wurff, I.S.M.; Meyer, B.J.; de Groot, R.H.M. Effect of omega-3 long chain polyunsaturated fatty acids (N-3 LCPUFA) supplementation on cognition in children and adolescents: A systematic literature review with a focus on n-3 LCPUFA blood values and dose of DHA and EPA. Nutrients 2020, 12, 3115. [Google Scholar] [CrossRef] [PubMed]
- Kadosh, K.C.; Muhardi, L.; Parikh, P.; Basso, M.; Mohamed, H.J.J.; Prawitasari, T.; Samuel, F.; Ma, G.; Geurts, J.M.W. Nutritional support of neurodevelopment and cognitive function in infants and young children—An update and novel insights. Nutrients 2021, 13, 199. [Google Scholar] [CrossRef] [PubMed]
- Lehner, A.; Staub, K.; Aldakak, L.; Eppenberger, P.; Rühli, F.; Martin, R.D.; Bender, N. Fish consumption is associated with school performance in children in a non-linear way. Evol. Med. Public Health 2020, 2020, 2–11. [Google Scholar] [CrossRef] [PubMed]
- De Groot, R.H.M.; Ouwehand, C.; Jolles, J. Eating the right amount of fish: Inverted U-shape association between fish consumption and cognitive performance and academic achievement in Dutch adolescents. Prostaglandins Leukot. Essent. Fat. Acids 2012, 86, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Strain, J.J.; Love, T.M.; Yeates, A.J.; Weller, D.; Mulhern, M.S.; Mcsorley, E.M.; Thurston, S.W.; Watson, G.E.; Mruzek, D.; Broberg, K.; et al. Associations of prenatal methylmercury exposure and maternal polyunsaturated fatty acid status with neurodevelopmental outcomes at 7 years of age: Results from the Seychelles Child Development Study Nutrition Cohort 2. Am. J. Clin. Nutr. 2021, 113, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Burdge, G.C.; Tan, S.-Y.; Henry, C.J. Long-chain n-3 PUFA in vegetarian women: A metabolic perspective. J. Nutr. Sci. 2017, 6, e58. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.A.B.; Reddy, S. The influence of a vegetarian diet on the fatty acid composition of human milk and the essential fatty acid status of the infant. J. Pediatr. 1992, 120, PS71–PS77. [Google Scholar] [CrossRef] [PubMed]
- Crozier, S.R.; Godfrey, K.M.; Calder, P.C.; Robinson, S.M.; Inskip, H.M.; Baird, J.; Gale, C.R.; Cooper, C.; Sibbons, C.M.; Fisk, H.L.; et al. Vegetarian diet during pregnancy is not associated with poorer cognitive performance in children at age 6–7 years. Nutrients 2019, 11, 3029. [Google Scholar] [CrossRef] [PubMed]
- Sass, L.; Bjarnadóttir, E.; Stokholm, J.; Chawes, B.; Vinding, R.K.; Mora-Jensen, A.R.C.; Thorsen, J.; Noergaard, S.; Ebdrup, B.H.; Jepsen, J.R.M.; et al. Fish Oil Supplementation in Pregnancy and Neurodevelopment in Childhood—A Randomized Clinical Trial. Child Dev. 2021, 92, 1624–1635. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Casanova, I.; Schoen, M.; Tandon, S.; Stein, A.D.; Barraza Villarreal, A.; DiGirolamo, A.M.; Demmelmair, H.; Ramirez Silva, I.; Feregrino, R.G.; Rzehak, P.; et al. Maternal FADS2 single nucleotide polymorphism modified the impact of prenatal docosahexaenoic acid (DHA) supplementation on child neurodevelopment at 5 years: Follow-up of a randomized clinical trial. Clin. Nutr. 2021, 40, 5339–5345. [Google Scholar] [CrossRef] [PubMed]
- Campoy, C.; Azaryah, H.; Torres-Espínola, F.J.; Martínez-Zaldívar, C.; García-Santos, J.A.; Demmelmair, H.; Haile, G.; Rzehak, P.; Koletzko, B.; Györei, E.; et al. Long-chain polyunsaturated fatty acids, homocysteine at birth and fatty acid desaturase gene cluster polymorphisms are associated with children’s processing speed up to age 9 years. Nutrients 2021, 13, 131. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.F.; Bednarz, J.M.; Sullivan, T.R.; McPhee, A.J.; Gibson, R.A.; Makrides, M. Subgroup analyses of a randomized trial of DHA supplementation for infants born preterm with assessments of cognitive development up to 7-years of age: What happens in infants born <29 weeks’ gestation? Prostaglandins Leukot. Essent. Fat. Acids 2023, 198–199, 198–199. [Google Scholar]
- Meldrum, S.J.; Heaton, A.E.; Foster, J.K.; Prescott, S.L.; Simmer, K. Do infants of breast-feeding mothers benefit from additional long-chain PUFA from fish oil? A 6-year follow-up. Br. J. Nutr. 2020, 124, 701–708. [Google Scholar] [CrossRef]
- Stephenson, K.; Callaghan-Gillespie, M.; Maleta, K.; Nkhoma, M.; George, M.; Park, H.G.; Lee, R.; Humphries-Cuff, I.; Lacombe, R.J.S.; Wegner, D.R.; et al. Low linoleic acid foods with added DHA given to Malawian children with severe acute malnutrition improve cognition: A randomized, triple-blinded, controlled clinical trial. Am. J. Clin. Nutr. 2022, 115, 1322–1333. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.B.; Franceschini, M.A.; Silver, R.E.; Taylor, S.F.; De Sa, A.B.; Có, R.; Sonco, A.; Krauss, A.; Taetzsch, A.; Webb, P.; et al. Effects of food supplementation on cognitive function, cerebral blood flow, and nutritional status in young children at risk of undernutrition: Randomized controlled trial. BMJ 2020, 370, m2397. [Google Scholar] [CrossRef] [PubMed]
- Demmelmair, H.; Øyen, J.; Pickert, T.; Rauh-Pfeiffer, A.; Stormark, K.M.; Graff, I.E.; Lie, Ø.; Kjellevold, M.; Koletzko, B. The effect of Atlantic salmon consumption on the cognitive performance of preschool children—A randomized controlled trial. Clin. Nutr. 2019, 38, 2558–2568. [Google Scholar] [CrossRef] [PubMed]
- Nieto-Ruiz, A.; García-Santos, J.A.; Verdejo-Román, J.; Diéguez, E.; Sepúlveda-Valbuena, N.; Herrmann, F.; Cerdó, T.; De-Castellar, R.; Jiménez, J.; Bermúdez, M.G.; et al. Infant Formula Supplemented With Milk Fat Globule Membrane, Long-Chain Polyunsaturated Fatty Acids, and Synbiotics Is Associated With Neurocognitive Function and Brain Structure of Healthy Children Aged 6 Years: The COGNIS Study. Front. Nutr. 2022, 9, 820224. [Google Scholar] [CrossRef] [PubMed]
- Naveed, S.; Venäläinen, T.; Eloranta, A.M.; Erkkilä, A.T.; Jalkanen, H.; Lindi, V.; Lakka, T.A.; Haapala, E.A. Associations of dietary carbohydrate and fatty acid intakes with cognition among children. Public Health Nutr. 2020, 23, 1657–1663. [Google Scholar] [CrossRef] [PubMed]
- Teisen, M.N.; Vuholm, S.; Niclasen, J.; Aristizabal-Henao, J.J.; Stark, K.D.; Geertsen, S.S.; Damsgaard, C.T.; Lauritzen, L. Effects of oily fish intake on cognitive and socioemotional function in healthy 8-9-year-old children: The FiSK Junior randomized trial. Am. J. Clin. Nutr. 2020, 112, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Teisen, M.N.; Niclasen, J.; Vuholm, S.; Lundbye-Jensen, J.; Stark, K.D.; Damsgaard, C.T.; Geertsen, S.S.; Lauritzen, L. Exploring correlations between neuropsychological measures and domain-specific consistency in associations with n-3 LCPUFA status in 8-9 year-old boys and girls. PLoS ONE 2019, 14, e0216696. [Google Scholar] [CrossRef] [PubMed]
- Azaryah, H.; Verdejo-Román, J.; Martin-Pérez, C.; García-Santos, J.A.; Martínez-Zaldívar, C.; Torres-Espínola, F.J.; Campos, D.; Koletzko, B.; Pérez-García, M.; Catena, A.; et al. Effects of maternal fish oil and/or 5-methyl-tetrahydrofolate supplementation during pregnancy on offspring brain resting-state at 10 years old: A follow-up study from the nuheal randomized controlled trial. Nutrients 2020, 12, 2701. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.Y.; Wu, T.; Huang, S.Y.; Huang, B.X.; Wang, H.L.; Lan, Q.Y.; Li, C.L.; Zhu, H.L.; Fang, A.P. No effect of 6-month supplementation with 300 mg/d docosahexaenoic acid on executive functions among healthy school-aged children: A randomized, double-blind, placebo-controlled trial. Eur. J. Nutr. 2021, 60, 1985–1997. [Google Scholar] [CrossRef] [PubMed]
- Petrova, D.; Bernabeu Litrán, M.A.; García-Mármol, E.; Rodríguez-Rodríguez, M.; Cueto-Martín, B.; López-Huertas, E.; Catena, A.; Fonollá, J. Effects of fortified milk on cognitive abilities in school-aged children: Results from a randomized-controlled trial. Eur. J. Nutr. 2019, 58, 1863–1872. [Google Scholar] [CrossRef] [PubMed]
- Bozzatello, P.; Brignolo, E.; De Grandi, E.; Bellino, S. Supplementation with omega-3 fatty acids in psychiatric disorders: A review of literature data. J. Clin. Med. 2016, 5, 67. [Google Scholar] [CrossRef] [PubMed]
- Tarui, T.; Rasool, A.; O’Tierney-Ginn, P. How the placenta-brain lipid axis impacts the nutritional origin of child neurodevelopmental disorders: Focus on attention deficit hyperactivity disorder and autism spectrum disorder. Exp. Neurol. 2022, 347, 113910. [Google Scholar] [CrossRef] [PubMed]
- Banaschewski, T.; Belsham, B.; Bloch, M.H.; Ferrin, M.; Johnson, M.; Kustow, J.; Robinson, S.; Zuddas, A. Supplementation with polyunsaturated fatty acids (PUFAs) in the management of attention deficit hyperactivity disorder (ADHD). Nutr. Health 2018, 24, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.C.; Su, K.P.; Mondelli, V.; Pariante, C.M. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacology 2018, 43, 534–545. [Google Scholar] [CrossRef]
- Hawkey, E.; Nigg, J.T. Omega-3 fatty acid and ADHD: Blood level analysis and meta-analytic extension of supplementation trials. Clin. Psychol. Rev. 2014, 34, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Kidd, P.M. Omega-3 DHA and EPA for cognition, behavior, and mood: Clinical findings and structural-functional synergies with cell membrane phospholipids. Altern. Med. Rev. 2007, 12, 207–227. [Google Scholar]
- Milte, C.M.; Sinn, N.; Buckley, J.D.; Coates, A.M.; Young, R.M.; Howe, P.R.C. Polyunsaturated fatty acids, cognition and literacy in children with ADHD with and without learning difficulties. J. Child Health Care 2011, 15, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Bellino, S.; Bozzatello, P.; Badino, C.; Mantelli, E.; Rocca, P. Efficacy of polyunsaturated fatty acids (PUFAs) on impulsive behaviours and aggressiveness in psychiatric disorders. Int. J. Mol. Sci. 2021, 22, 620. [Google Scholar] [CrossRef] [PubMed]
- Martins, B.P.; Bandarra, N.M.; Figueiredo-Braga, M. The role of marine omega-3 in human neurodevelopment, including Autism Spectrum Disorders and Attention-Deficit/Hyperactivity Disorder–a review. Crit. Rev. Food Sci. Nutr. 2020, 60, 1431–1446. [Google Scholar] [CrossRef] [PubMed]
- Chaplin, S. Attention deficit hyperactivity disorder: Diagnosis and management. Prog. Neurol. Psychiatry 2018, 22, 27–29. [Google Scholar] [CrossRef]
- Sarris, J.; Ravindran, A.; Yatham, L.N.; Marx, W.; Rucklidge, J.J.; McIntyre, R.S.; Akhondzadeh, S.; Benedetti, F.; Caneo, C.; Cramer, H.; et al. Clinician guidelines for the treatment of psychiatric disorders with nutraceuticals and phytoceuticals: The World Federation of Societies of Biological Psychiatry (WFSBP) and Canadian Network for Mood and Anxiety Treatments (CANMAT) Taskforce. World J. Biol. Psychiatry 2022, 23, 424–455. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Sinn, J.K.H.; Lad, S.S.; Leach, M.J.; Ross, M.J. Polyunsaturated fatty acids (PUFA) for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst. Rev. 2012, 2012, CD007986. [Google Scholar] [CrossRef] [PubMed]
- Bloch, M.H.; Qawasmi, A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: Systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 991–1000. [Google Scholar] [CrossRef] [PubMed]
- Rosi, E.; Grazioli, S.; Villa, F.M.; Mauri, M.; Gazzola, E.; Pozzi, M.; Molteni, M.; Nobile, M. Use of non-pharmacological supplementations in children and adolescents with attention deficit/hyperactivity disorder: A critical review. Nutrients 2020, 12, 1573. [Google Scholar] [CrossRef] [PubMed]
- Händel, M.N.; Rohde, J.F.; Rimestad, M.L.; Bandak, E.; Birkefoss, K.; Tendal, B.; Lemcke, S.; Callesen, H.E. Efficacy and safety of polyunsaturated fatty acids supplementation in the treatment of attention deficit hyperactivity disorder (Adhd) in children and adolescents: A systematic review and meta-analysis of clinical trials. Nutrients 2021, 13, 1226. [Google Scholar] [CrossRef]
- Abdullah, M.; Jowett, B.; Whittaker, P.J.; Patterson, L. The effectiveness of omega-3 supplementation in reducing ADHD associated symptoms in children as measured by the Conners’ rating scales: A systematic review of randomized controlled trials. J. Psychiatr. Res. 2019, 110, 64–73. [Google Scholar] [CrossRef] [PubMed]
- D’Helft, J.; Caccialanza, R.; Derbyshire, E.; Maes, M. Relevance of ω-6 GLA Added to ω-3 PUFAs Supplements for ADHD: A Narrative Review. Nutrients 2022, 14, 3273. [Google Scholar] [CrossRef] [PubMed]
- Barragán, E.; Breuer, D.; Döpfner, M. Efficacy and Safety of Omega-3/6 Fatty Acids, Methylphenidate, and a Combined Treatment in Children With ADHD. J. Atten. Disord. 2017, 21, 433–441. [Google Scholar] [CrossRef]
- Sinn, N.; Bryan, J.; Wilson, C. Cognitive effects of polyunsaturated fatty acids in children with attention deficit hyperactivity disorder symptoms: A randomised controlled trial. Prostaglandins Leukot. Essent. Fat. Acids 2008, 78, 311–326. [Google Scholar] [CrossRef] [PubMed]
- Checa-Ros, A.; Haro-García, A.; Seiquer, I.; Molina-Carballo, A.; Uberos-Fernández, J.; Muñoz-Hoyos, A. Early monitoring of fatty acid profile in children with attention deficit and/or hyperactivity disorder under treatment with omega-3 polyunsaturated fatty acids. Minerva Pediatr. 2019, 71, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Döpfner, M.; Dose, C.; Breuer, D.; Heintz, S.; Schiffhauer, S.; Banaschewski, T. Efficacy of Omega-3/Omega-6 Fatty Acids in Preschool Children at Risk of ADHD: A Randomized Placebo-Controlled Trial. J. Atten. Disord. 2021, 25, 1096–1106. [Google Scholar] [CrossRef]
- Al-Ghannami, S.S.; Al-Adawi, S.; Ghebremeskel, K.; Hussein, I.S.; Min, Y.; Jeyaseelan, L.; Al-Shammakhi, S.M.; Mabry, R.M.; Al-Oufi, H.S. Randomized open-label trial of docosahexaenoic acid–enriched fish oil and fish meal on cognitive and behavioral functioning in Omani children. Nutrition 2019, 57, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Carucci, S.; Romaniello, R.; Demuru, G.; Curatolo, P.; Grelloni, C.; Masi, G.; Liboni, F.; Mereu, A.; Contu, P.; Lamberti, M.; et al. Omega-3/6 supplementation for mild to moderate inattentive ADHD: A randomised, double-blind, placebo-controlled efficacy study in Italian children. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 1453–1467. [Google Scholar] [CrossRef] [PubMed]
- Crippa, A.; Tesei, A.; Sangiorgio, F.; Salandi, A.; Trabattoni, S.; Grazioli, S.; Agostoni, C.; Molteni, M.; Nobile, M. Behavioral and cognitive effects of docosahexaenoic acid in drug-naïve children with attention-deficit/hyperactivity disorder: A randomized, placebo-controlled clinical trial. Eur. Child Adolesc. Psychiatry 2019, 28, 571–583. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.C.; Su, K.P.; Mondelli, V.; Satyanarayanan, S.K.; Yang, H.T.; Chiang, Y.J.; Chen, H.T.; Pariante, C.M. High-dose eicosapentaenoic acid (EPA) improves attention and vigilance in children and adolescents with attention deficit hyperactivity disorder (ADHD) and low endogenous EPA levels. Transl. Psychiatry 2019, 9, 303. [Google Scholar] [CrossRef] [PubMed]
- San Mauro Martin, I.; Sanz Rojo, S.; González Cosano, L.; Conty de la Campa, R.; Garicano Vilar, E.; Blumenfeld Olivares, J.A. Impulsiveness in children with attention-deficit/hyperactivity disorder after an 8-week intervention with the Mediterranean diet and/or omega-3 fatty acids: A randomised clinical trial. Neurologia 2022, 37, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Cornu, C.; Mercier, C.; Ginhoux, T.; Masson, S.; Mouchet, J.; Nony, P.; Kassai, B.; Laudy, V.; Berquin, P.; Franc, N.; et al. A double-blind placebo-controlled randomised trial of omega-3 supplementation in children with moderate ADHD symptoms. Eur. Child Adolesc. Psychiatry 2018, 27, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, C.; García, T.; Areces, D.; Fernández, E.; García-Noriega, M.; Domingo, J.C. Supplementation with high-content docosahexaenoic acid triglyceride in attentiondeficit hyperactivity disorder: A randomized double-blind placebo-controlled trial. Neuropsychiatr. Dis. Treat. 2019, 15, 1193–1209. [Google Scholar] [CrossRef]
- Boone, K.M.; Parrott, A.; Rausch, J.; Yeates, K.O.; Klebanoff, M.A.; Turner, A.N.; Keim, A. Fatty acid supplementation and socioemotional outcomes: Secondary analysis of a randomized trial. Pediatrics 2020, 146, e20200284. [Google Scholar] [CrossRef] [PubMed]
- Boone, K.M.; Klebanoff, M.A.; Rogers, L.K.; Rausch, J.; Coury, D.L.; Keim, S.A. Effects of Omega-3-6-9 fatty acid supplementation on behavior and sleep in preterm toddlers with autism symptomatology: Secondary analysis of a randomized clinical trial. Early Hum. Dev. 2022, 169, 105588. [Google Scholar] [CrossRef] [PubMed]
- Doaei, S.; Bourbour, F.; Teymoori, Z.; Jafari, F.; Kalantari, N.; Torki, S.A.; Ashoori, N.; Gorgani, S.N.; Gholamalizadeh, M. The effect of omega-3 fatty acids supplementation on social and behavioral disorders of children with autism: A randomized clinical trial. Pediatr. Endocrinol. Diabetes Metab. 2021, 27, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Keim, S.A.; Jude, A.; Smith, K.; Khan, A.Q.; Coury, D.L.; Rausch, J.; Udaipuria, S.; Norris, M.; Bartram, L.R.; Narayanan, A.R.; et al. Randomized Controlled Trial of Omega-3 and -6 Fatty Acid Supplementation to Reduce Inflammatory Markers in Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2022, 52, 5342–5355. [Google Scholar] [CrossRef] [PubMed]
- Mazahery, H.; Conlon, C.A.; Beck, K.L.; Mugridge, O.; Kruger, M.C.; Stonehouse, W.; Camargo, C.A.; Meyer, B.J.; Tsang, B.; Jones, B.; et al. A Randomised-Controlled Trial of Vitamin D and Omega-3 Long Chain Polyunsaturated Fatty Acids in the Treatment of Core Symptoms of Autism Spectrum Disorder in Children. J. Autism Dev. Disord. 2019, 49, 1778–1794. [Google Scholar] [CrossRef]
- Trebatická, J.; Hradečná, Z.; Surovcová, A.; Katrenčíková, B.; Gushina, I.; Waczulíková, I.; Sušienková, K.; Garaiova, I.; Šuba, J.; Ďuračková, Z. Omega-3 fatty-acids modulate symptoms of depressive disorder, serum levels of omega-3 fatty acids and omega-6/omega-3 ratio in children. A randomized, double-blind and controlled trial. Psychiatry Res. 2020, 287, 112911. [Google Scholar] [CrossRef]
- van der Wurff, I.S.M.; von Schacky, C.; Bergeland, T.; Leontjevas, R.; Zeegers, M.P.; Kirschner, P.A.; de Groot, R.H.M. Effect of one year krill oil supplementation on depressive symptoms and self-esteem of Dutch adolescents: A randomized controlled trial. Prostaglandins Leukot. Essent. Fat. Acids 2020, 163, 102208. [Google Scholar] [CrossRef] [PubMed]
- Katrenčíková, B.; Vaváková, M.; Waczulíková, I.; Oravec, S.; Garaiova, I.; Nagyová, Z.; Hlaváčová, N.; Ďuračková, Z.; Trebatická, J. Lipid profile, lipoprotein subfractions, and fluidity of membranes in children and adolescents with depressive disorder: Effect of omega-3 fatty acids in a double-blind randomized controlled study. Biomolecules 2020, 10, 1427. [Google Scholar] [CrossRef]
- McNamara, R.K.; Strawn, J.R.; Tallman, M.J.; Welge, J.A.; Patino, L.R.; Blom, T.J.; Delbello, M.P. Effects of Fish Oil Monotherapy on Depression and Prefrontal Neurochemistry in Adolescents at High Risk for Bipolar i Disorder: A 12-Week Placebo-Controlled Proton Magnetic Resonance Spectroscopy Trial. J. Child Adolesc. Psychopharmacol. 2020, 30, 293–305. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.C.; Su, K.P. Nutritional Neuroscience as Mainstream of Psychiatry: The Evidence-Based Treatment Guidelines for Using Omega-3 Fatty Acids as a New Treatment for Psychiatric Disorders in Children and Adolescents. Clin. Psychopharmacol. Neurosci. 2020, 18, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Kohlboeck, G.; Glaser, C.; Tiesler, C.; Demmelmair, H.; Standl, M.; Romanos, M.; Koletzko, B.; Lehmann, I.; Heinrich, J. Effect of fatty acid status in cord blood serum on children’s behavioral difficulties at 10 y of age: Results from the LISAplus Study. Am. J. Clin. Nutr. 2011, 94, 1592–1599. [Google Scholar] [CrossRef] [PubMed]
- Gale, C.R.; Robinson, S.M.; Godfrey, K.M.; Law, C.M.; Schlotz, W.; O’Callaghan, F.J. Oily fish intake during pregnancy—Association with lower hyperactivity but not with higher full-scale IQ in offspring. J. Child Psychol. Psychiatry Allied Discip. 2008, 49, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Sagiv, S.K.; Thurston, S.W.; Bellinger, D.C.; Amarasiriwardena, C.; Korrick, S.A. Prenatal exposure to mercury and fish consumption during pregnancy and attention-deficit/hyperactivity disorder-related behavior in children. Arch. Pediatr. Adolesc. Med. 2012, 166, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.L.; Voigt, R.G.; Llorente, A.M.; Peters, S.U.; Prager, T.C.; Zou, Y.L.; Rozelle, J.C.; Turcich, M.R.; Fraley, J.K.; Anderson, R.E.; et al. Effects of early maternal docosahexaenoic acid intake on neuropsychological status and visual acuity at five years of age of breast-fed term infants. J. Pediatr. 2010, 157, 900–905. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Gonzalez-Casanova, I.; Schnaas, L.; DiGirolamo, A.; Quezada, A.D.; Pallo, B.C.; Hao, W.; Neufeld, L.M.; Rivera, J.A.; Stein, A.D.; et al. Prenatal supplementation with DHA improves attention at 5 y of age: A randomized controlled trial. Am. J. Clin. Nutr. 2016, 104, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.F.; Makrides, M.; Colombo, J.; Smithers, L.G. Randomized controlled trial of maternal omega-3 long-chain PUFA supplementation during pregnancy and early childhood development of attention, working memory, and inhibitory control. Am. J. Clin. Nutr. 2014, 99, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.F.; Anderson, P.J.; Yelland, L.N.; Gibson, R.A.; Makrides, M. The influence of prenatal dha supplementation on individual domains of behavioral functioning in school-aged children: Follow-up of a randomized controlled trial. Nutrients 2021, 13, 2996. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.M.; Buoli, M.; Ciappolino, V.; Agostoni, C.; Brambilla, P. The role of cholesterol and fatty acids in the etiology and diagnosis of autism spectrum disorders. Int. J. Mol. Sci. 2021, 22, 3550. [Google Scholar] [CrossRef] [PubMed]
- Hellings, J. Pharmacotherapy in autism spectrum disorders, including promising older drugs warranting trials. World J. Psychiatry 2023, 13, 262–277. [Google Scholar] [CrossRef] [PubMed]
- Lyall, K.; Munger, K.L.; O’Reilly, É.J.; Santangelo, S.L.; Ascherio, A. Maternal dietary fat intake in association with autism spectrum disorders. Am. J. Epidemiol. 2013, 178, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Iosif, A.M.; Hansen, R.L.; Schmidt, R.J. Maternal polyunsaturated fatty acids and risk for autism spectrum disorder in the MARBLES high-risk study. Autism 2020, 24, 1191–1200. [Google Scholar] [CrossRef] [PubMed]
- Steenweg-De Graaff, J.; Tiemeier, H.; Ghassabian, A.; Rijlaarsdam, J.; Jaddoe, V.W.V.; Verhulst, F.C.; Roza, S.J. Maternal Fatty Acid Status during Pregnancy and Child Autistic Traits: The Generation R Study. Am. J. Epidemiol. 2016, 183, 792–799. [Google Scholar] [CrossRef]
- Cekici, H.; Sanlier, N. Current nutritional approaches in managing autism spectrum disorder: A review. Nutr. Neurosci. 2019, 22, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Fraguas, D.; Díaz-Caneja, C.M.; Pina-Camacho, L.; Moreno, C.; Durán-Cutilla, M.; Ayora, M.; González-Vioque, E.; De Matteis, M.; Hendren, R.L.; Arango, C.; et al. Dietary interventions for autism spectrum disorder: A meta-analysis. Pediatrics 2019, 144, e20183218. [Google Scholar] [CrossRef] [PubMed]
- Mazahery, H.; Stonehouse, W.; Delshad, M.; Kruger, M.C.; Conlon, C.A.; Beck, K.L.; von Hurst, P.R. Relationship between long chain n-3 polyunsaturated fatty acids and autism spectrum disorder: Systematic review and meta-analysis of case-control and randomised controlled trials. Nutrients 2017, 9, 155. [Google Scholar] [CrossRef] [PubMed]
- de Andrade Wobido, K.; de Sá Barreto da Cunha, M.; Miranda, S.S.; da Mota Santana, J.; da Silva, D.C.G.; Pereira, M. Non-specific effect of omega-3 fatty acid supplementation on autistic spectrum disorder: Systematic review and meta-analysis. Nutr. Neurosci. 2022, 25, 1995–2007. [Google Scholar] [CrossRef] [PubMed]
- Barón-Mendoza, I.; González-Arenas, A. Relationship between the effect of polyunsaturated fatty acids (PUFAs) on brain plasticity and the improvement on cognition and behavior in individuals with autism spectrum disorder. Nutr. Neurosci. 2022, 25, 387–410. [Google Scholar] [CrossRef] [PubMed]
- De Crescenzo, F.; D’Alò, G.L.; Morgano, G.P.; Minozzi, S.; Mitrova, Z.; Saulle, R.; Cruciani, F.; Fulceri, F.; Davoli, M.; Scattoni, M.L.; et al. Impact of polyunsaturated fatty acids on patient-important outcomes in children and adolescents with autism spectrum disorder: A systematic review. Health Qual. Life Outcomes 2020, 18, 28. [Google Scholar] [CrossRef]
- James, S.; Montgomery, P.; Williams, K. Omega-3 fatty acids supplementation for autism spectrum disorders (ASD). Cochrane Database Syst. Rev. 2011, 11, CD007992. [Google Scholar] [CrossRef] [PubMed]
- Horvath, A.; Łukasik, J.; Szajewska, H. ω-3 Fatty Acid Supplementation Does Not Affect Autism Spectrum Disorder in Children: A Systematic Review and Meta-Analysis. J. Nutr. 2017, 147, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Bozzatello, P.; Blua, C.; Rocca, P.; Bellino, S. Mental health in childhood and adolescence: The role of polyunsaturated fatty acids. Biomedicines 2021, 9, 850. [Google Scholar] [CrossRef]
- Veselinović, A.; Petrović, S.; Žikić, V.; Subotić, M.; Jakovljević, V.; Jeremić, N.; Vučić, V. Neuroinflammation in autism and supplementation based on omega-3 polyunsaturated fatty acids: A narrative review. Medicina 2021, 57, 893. [Google Scholar] [CrossRef] [PubMed]
- Pancheva, R.Z.; Nikolova, S.; Serbezova, A.; Zaykova, K.; Zhelyazkova, D.; Dimitrov, L. Evidence or no evidence for essential fatty acids in the treatment of autism spectrum disorders? Front. Nutr. 2023, 10, 1251083. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Dang, W.; Nie, H.; Kong, X.; Jiang, Z.; Guo, J. Omega-3 polyunsaturated fatty acids and/or vitamin D in autism spectrum disorders: A systematic review. Front. Psychiatry 2023, 14, 1238973. [Google Scholar] [CrossRef] [PubMed]
- Donovan, S.; Dewey, K.; Novotny, R.; Stang, J.; Taveras, E.; Kleinman, R.; Nevins, J.; Raghavan, R.; Scinto-Madonich, S.; Venkatramanan, S.; et al. Omega-3 Fatty Acids from Supplements Consumed before and during Pregnancy and Lactation and Developmental Milestones, Including Neurocognitive Development, in the Child: A Systematic Review; USDA Nutrition Evidence Systematic Review: Alexandria, VA, USA, 2020.
- Bragg, M.; Chavarro, J.E.; Hamra, G.B.; Hart, J.E.; Tabb, L.P.; Weisskopf, M.G.; Volk, H.E.; Lyall, K. Prenatal Diet as a Modifier of Environmental Risk Factors for Autism and Related Neurodevelopmental Outcomes. Curr. Environ. Health Rep. 2022, 9, 324–338. [Google Scholar] [CrossRef]
- Stachowicz, K. The role of polyunsaturated fatty acids in neuronal signaling in depression and cognitive processes. Arch. Biochem. Biophys. 2023, 737, 109555. [Google Scholar] [CrossRef] [PubMed]
- Sabião, T.d.S.; de Oliveira, F.C.; Bressan, J.; Pimenta, A.M.; Hermsdorff, H.H.M.; de Oliveira, F.L.P.; Mendonça, R.d.D.; Carraro, J.C.C. Fatty acid intake and prevalence of depression among Brazilian graduates and postgraduates (CUME Study). J. Affect. Disord. 2024, 346, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Kim, Y.; Je, Y. Fish consumption and risk of depression: Epidemiological evidence from prospective studies. Asia-Pac. Psychiatry 2018, 10, e12335. [Google Scholar] [CrossRef] [PubMed]
- Osuna, E.; Herter-Aeberli, I.; Probst, S.; Emery, S.; Albermann, M.; Baumgartner, N.; Strumberger, M.; Ricci, C.; Schmeck, K.; Walitza, S.; et al. Associations of n-3 polyunsaturated fatty acid status and intake with paediatric major depressive disorder in Swiss adolescents: A case-control study. J. Affect. Disord. 2023, 339, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Häberling, I.; Berger, G.; Schmeck, K.; Held, U.; Walitza, S. Omega-3 Fatty Acids as a Treatment for Pediatric Depression. A Phase III, 36 Weeks, Multi-Center, Double-Blind, Placebo-Controlled Randomized Superiority Study. Front. Psychiatry 2019, 10, 863. [Google Scholar] [CrossRef]
- Thakur, T.; Mann, S.K.; Malhi, N.K.; Marwaha, R. The Role of Omega-3 Fatty Acids in the Treatment of Depression in Children and Adolescents: A Literature Review. Cureus 2023, 15, e44584. [Google Scholar] [CrossRef] [PubMed]
| Food | PUFAs Content (g/100 g of Product) | ||
|---|---|---|---|
| ALA | DHA | EPA | |
| Seeds and nuts | |||
| Walnuts | 9.05 | - | - |
| Chia seeds | 17.81 | - | - |
| Flaxseed | 19.4 | - | - |
| Oils | |||
| Canola | 7.45 | - | - |
| Soybean | 6.62 | - | - |
| Olive | 0.65 | - | - |
| Fish | |||
| Salmon, Atlantic | - | 1.45 | 0.69 |
| Herring, Atlantic | - | 1.09 | 0.9 |
| Sardines | - | 0.86 | 0.5 |
| Seafood | |||
| Lobster | 0.05 | 0.08 | 0.12 |
| Shrimps | - | 0.14 | 0.14 |
| Scallops | - | 0.10 | 0.07 |
| Type of Study | Participants | Intervention | Main Outcomes | Ref. |
|---|---|---|---|---|
| Single-center, double-blind, placebo-controlled randomized clinical trial | Mother–child cohort, 736 women at pregnancy week 24, 654 participants | The pregnant women received four 1 g capsules of fish oil per day, providing 2.4 g/day of omega-3 LC-PUFA (55% EPA and 37% DHA) or four capsules with olive oil (72% n-9 oleic acid and 12% omega-6 LA; control group) | Maternal administration of omega-3 LC-PUFA (EPA and DHA) during pregnancy was correlated with improved early language development and reduced emotional and behavioral issues in children at 6 years of age, with particular cognitive development advantages observed in male children at 2.5 years. | [102] |
| Randomized, controlled trial | Mother–child pairs, 622 participants | Pregnant women in their 18–22 week of gestation received 400 mg/day of algal DHA or a placebo mixture of corn and soybean oil through delivery | Maternal fatty acid desaturase 2 (FADS2) single nucleotide polymorphisms rs174602 may modify the effect of prenatal DHA supplementation on child cognitive development at 5 years. | [103] |
| Multicenter, randomized, double-blind, placebo-controlled trial | Pregnant women and their children, 311 participants | Pregnant women received either a modified fish-oil (FO) preparation (500 mg DHA + 150 mg EPA/day), 5-methyl-tetrahydrofolate (5-MTHF) (400 g/day), a combination of both supplements (FO + 5-MTHF), or placebo, from gestational week 20 until delivery | No definitive impact of prenatal omega-3 supplementation on processing speed was observed in children up to 9 years old. | [104] |
| Subgroup analyses of a randomized trial | Infants born <29 weeks of gestation, 227 participants | Breastfeeding mothers consumed either six capsules, each containing 500 mg of DHA-rich tuna oil (to achieve a breastmilk DHA concentration of approx. 1% of total fatty acids) + a dietary supplement that provided approx. 60 mg/kg/day of DHA (high-DHA group) or 500 mg soy oil (which does not alter the fatty acid composition of the breastmilk) + a dietary supplement that provided approx. 20 mg/kg/day of DHA (standard-DHA group) | High-dose DHA supplementation in preterm infants did not demonstrate a clear benefit to IQ. | [105] |
| Double-blind, randomized, controlled trial | Healthy term infants, 420 participants | Infants received either fish oil (containing at least 250 mg of DHA and at least 60 mg of EPA) or placebo (olive oil) daily from birth to 6 months of age | Supplementation with fish oil from birth to 6 months did not confer significant cognitive benefits at 6 years of age. | [106] |
| Triple-blind, randomized, controlled clinical trial | Children with uncomplicated severe acute malnutrition (SAM), 2758 participants | Children with severe acute malnutrition were treated with three RUTF variants, i.e., DHA-HO-RUTF, HO-RUTF, and S-RUTF, in a clinical trial. | Children with severe acute malnutrition showed cognitive improvement after treatment with DHA-enriched therapeutic food. | [107] |
| Randomized, controlled trial | Children aged 15 months to 7 years, 1059 participants | Children received supervised isocaloric servings (≈1300 kJ, five mornings each week, 23 weeks) of a new food supplement (NEWSUP, high in plant polyphenols and omega-3 FAs, within a wide variety and high fortification of micronutrients and a high protein content), a fortified blended food (FBF) used in nutrition programs, or a control meal (traditional rice breakfast) | Nutrient-rich supplementary feeding improved cognitive function in undernourished children. | [108] |
| Randomized, controlled trial | Healthy children aged 4–6 years, 205 participants | Children received three prepared meals weekly for 16 weeks, containing either approximately 50 g of Atlantic salmon or 50 g of meat per meal | Moderate consumption of fish was related to better performance in specific fluid intelligence tests but did not affect overall IQ in preschoolers. | [109] |
| Multicenter, blinded, parallel-group, randomized, controlled trial | Children born before 29 week’s gestation, 656 participants | Children received an enteral intervention emulsion that provided 60 mg of DHA per kilogram of body weight per day or a control emulsion that provided contained no DHA from the first 3 days of enteral feeds until 36 weeks of postmenstrual age or discharge home, whichever occurred first | The use of enteral emulsion containing DHA until 36 weeks of postmenstrual age was associated with moderately higher full-scale IQ (FSIQ) scores at the age of 5 years compared to control feeding. | [53] |
| Prospective, randomized, double-blind study | Children aged 6 years, 108 participants | Infants received up to 18 months of life a standard infant formula (SF) or experimental infant formula (EF) enriched with milk fat globule membrane (MFGM), LC-PUFAs, and synbiotics, and a reference group of breastfed (BF) infants were also recruited | An infant formula enriched with nutrients such as MFGM, LC-PUFAs, and synbiotics led to better cognitive outcomes compared to standard formula or breast milk. | [110] |
| Cross-sectional study | Children aged 6–8 years, 487 participants | Parents recorded all food and drinks consumed by their children at home, at school, in afternoon care, and elsewhere outside home using household or other measures | No consistent relationship was found between dietary FAs and cognitive performance in children aged 6–8 years. | [111] |
| Randomized, controlled trial | Children 8–9 years old, 198 participants | Children consumed 375 g/week of oily fish or poultry (control) for 12 ± 2 week | Weekly consumption of oily fish improved cognitive functions, particularly attention and cognitive flexibility in children aged 8–9 years. | [112] |
| Cross-sectional study | Children aged 8–9 years, 199 participants | None | Performance in particular cognitive domains did not consistently correlate with omega-3 LC-PUFAs levels, with the exception of processing speed metrics, where all indications suggested quicker cognitive processing associated with higher omega-3 PUFAs status. | [113] |
| Follow-up of double-blind, randomized clinical trial | Children aged 9.5–10 years, 85 participants | Mother’s supplementation with fish oil | Pregnant mothers who supplement with fish oil may influence resting-state network function in school-aged children and generate long-lasting impacts on their cognitive processing. | [114] |
| Double-blind, placebo-controlled, randomized trial | Children aged 7–12 years, 106 participants | Children received either 300 mg/d of DHA or placebo for 6 months | DHA supplementation did not improve executive functions in school-aged children. | [115] |
| Randomized, controlled trial | Children aged 8–14 years, 119 participants | Children consumed either 0.6 L/day of a fortified milk beverage containing vitamins (A, B complex, C, D, and E), minerals (calcium, phosphorus, and zinc), fish oils (with high levels of DHA and EPA), oleic acid, and carbohydrates (sugar and honey) or 0.6 L/day of regular full milk every day for 5 months. | Fortified milk beverages with micronutrients and PUFAs appeared to support the cognitive development in children aged 8–14 years. | [116] |
| Type of Condition | Type of Study | Participants | Intervention | Main Outcomes | Reference |
|---|---|---|---|---|---|
| ADHD | Open-label | Children 7–15 years old, 40 participants | All participants received a combination of methylphenidate (1 mg/kg/day) and EPA (70 mg/day) + DHA (250 mg/day) for 1 month | Significantly increased quality of attention, improvement of ADHD core symptoms, significantly increased levels of EPA and DHA, significantly decreased levels of several omega-6 FAs (including arachidonic acid), and slightly decreased omega-6/omega-3 index slightly decreased. No severe side effects. | [136] |
| None | Randomized, open-label | Children 9–10 years old, 132 participants (57 males, 75 females) | Each group with 66 subjects. DHA-enriched fish oil capsules containing 403 mg of DHA or a daily midday lunch snack comprising 100 g of a lightly grilled fish (grouper, seabream, kingfish, emperor, or snapper) sandwich with some vegetables (providing 150–200 mg of DHA) 5 days in a week for 12 weeks | Fish oil supplement increased the DHA level more profoundly than the meal. Improvement in verbal fluency and executive functioning was noted in all children, but a significantly greater effect was seen only with executive functioning in the group receiving the DHA supplement. | [138] |
| Mild to moderate ADHD | Randomized, double-blind, controlled for 6 months + open-label for 6 months | Children 6–12 years old, 160 participants (118 males, 42 females) | Intervention group 79 subjects): 2 capsules/day (each capsule containing 279 mg of EPA, 87 mg of DHA, and 30 mg of GLA) for 6 months; Control group (81 subjects): 2 capsules of placebo for 6 months; Open-label phase: All children were given: 2 capsules/day (each capsule containing 279 mg of EPA, 87 mg of DHA, and 30 mg of GLA) for 6 months | Omega-3/6 dietary supplementation was not significantly correlated with the clinical improvement in ADHD symptoms or with essential fatty acids blood levels. | [139] |
| ADHD | Randomized, double-blind, controlled | Children 7–14 years old, 50 participants (46 males, 4 females) | Intervention group (25 subjects): 2 soft gelatin pearls/day providing a dose of 500 mg of algal DHA for 6 months; Control group (25 subjects): 2 pearls/day containing 500 mg of wheat germ oil with vitamin E (placebo) for 6 months | DHA supplementation had no beneficial effect on the symptoms of ADHD, but it had small positive effects on other behavioral and cognitive difficulties related to ADHD, such as psychosocial functioning, emotional problems, and focused attention. | [140] |
| ADHD | Randomized, double-blind, controlled | Children 6–18 years old, 92 participants (79 males, 13 females) | Intervention group (48 subjects): 1.2 g/day of EPA for 12 weeks; Control group (44 subjects): placebo (1.2 g/day of soybean oil) for 12 weeks | EPA supplementation improved focused attention and vigilance. | [141] |
| ADHD | observational cohort study | Children 6–16 years old, 60 participants (42 males, 18 females) | Intervention groups: 1st group received Mediterranean diet for 8 weeks (19 subjects); 2nd group received 4 soft gels/day providing 550 mg of EPA and 225 mg of DHA/day for 8 weeks (29 subjects); 3rd group received Mediterranean diet and 4 soft gels/day providing 550 mg of EPA and 225 mg of DHA/day for 8 weeks (19 subjects); Control group (19 subjects): Usual diet for 8 weeks | Supplementation of EPA and DHA is associated with less marked impulsive behavior in children with ADHD. A Mediterranean diet may improve the Barratt Impulsiveness Scale score, although obtained results were not conclusive in the studied population. | [142] |
| ADHD | Randomized, double-blind, controlled | Children 6–15 years old, 162 participants (127 males, 35 females) | Intervention group (77 subjects): for 3 months capsules containing: (1) For children 6–8 years old 336 mg of EPA + 84 mg of DHA/day; (2) For children 9–11 years old 504 mg of EPA + 126 mg of DHA/day; (3) for children 12–15 years old 672 mg of EPA + 168 mg of DHA/day. Control group (44 subjects): placebo for 3 months | No beneficial effect of omega-3 supplementation was detected. | [143] |
| ADHD | Randomized, double-blind, controlled | Children 6–12 years old, 60 participants (49 males, 11 females) | All participants were taking methylphenidate at a dose of 10 mg/day (in 2 doses) and 20–30 mg/kg/day (in 2 doses) from the second week. Intervention group: 1 capsule and from the 2nd week 2 capsules containing 180 mg of EPA + 120 mg of DHA/day for 8 weeks; Control group: 1 capsule and from the 2nd week 2 capsules of placebo for 8 weeks | No beneficial effect of omega-3 supplementation was detected. | [144] |
| None | Randomized, double-blind, controlled | Children 10 to 16 months at enrollment, born at 35 weeks’ gestation, 377 participants (195 males, 182 females) | Intervention group (189 subjects): dissolvable, 200 mg microencapsulated DHA and 200 mg of arachidonic acid powder/day for 180 days; Control group (188 subjects): placebo (400 mg of a daily microencapsulated corn oil powder) for 180 days | No overall treatment effect of DHA and arachidonic acid supplementation on caregiver-reported outcomes of child competence and problem behaviors were observed. Children in the intervention group had a decreased risk of clinical concern for autistic spectrum disorder compared with the placebo-treated group. | [145] |
| None | Randomized, double-blind, controlled | Children 18–38 months of calendar age who were born at ≤29 completed weeks’ gestation, 31 participants (21 males, 10 females) | Intervention group (15 subjects): oral omega 3-6-9 FA supplementation in the form of a lemon-flavored fish and borage oil (706 mg total omega-3 FAs 338 mg EPA, 225 mg DHA; 280 mg total omega-6 FAs: 83 mg GLA; and 306 mg total omega-9 FAs (oleic acid)/day for 90 days. Control group (16 subjects): Placebo (canola oil—124 mg palmitic acid, 39 mg stearic acid, 513 mg LA, 225 mg ALA, 1346 mg oleic acid/day) for 90 days | Omega 3-6-9 supplementation had beneficial effects on anxious and depressed behaviors, internalizing behaviors, and interpersonal relationship adaptive behaviors. No effects were observed on other aspects of behavior or sleep. | [146] |
| Autism | Randomized, double-blind, controlled | Children 5–15 years old, 54 participants (39 males, 15 females) | Intervention group (28 subjects): 1 capsule with omega-3 FAs (180 mg of EPA + 120 mg of DHA) for 8 weeks; Control group (26 subjects): 1 capsule of placebo (medium chain triglyceride) for 8 weeks | Omega-3 supplementation improved GARS score, stereotyped behaviors, and social communication. | [147] |
| Autism | Randomized, double-blind, controlled | Children (2–6 years old), 70 participants (57 males, 13 females) | Children were assigned to 1 of 3 different doses of treatment (25 “low”, 50 “medium”, or 100 “high” mg/kg/day of GLA + EPA + DHA) or 1 of 3 doses of placebo. Intervention groups (37 subjects): oral Complete Omega™ supplementation in the form of lemon oil flavored fish and borage oils (providing 185 mg of total omega-3 fatty acids including 112 mg of EPA, 67 mg of DHA, 122 mg of total omega-6 fatty acids including 32 mg of GLA, and 83 mg of total omega-9 fatty acids per milliliter of supplement) for 90 days; Control groups (33 subjects): Placebo (canola oil—providing 188 mg of LA, 81 mg of ALA, and 590 mg of oleic acid per milliliter) for 90 days | Intervention increased levels of omega-3 and omega-6 FAs and reduced IL-2 levels. Omega 3-6 treatment was tolerable. | [148] |
| Autism | Randomized, double-blind, controlled | Children (2.5–8 years old), 117 participants (100 males, 17 females) | Intervention groups: 1st group received 4 capsules/day with vitamin D3 (2000 IU/day) for 12 months (31 subjects); 2nd group received 4 capsules/day with DHA (722 mg/day) for 12 months (29 subjects); 3rd group received 4 capsules/day with vitamin D3 (2000 IU/day) and of DHA (722 mg/day) for 12 months (28 subjects). Control group (29 subjects): 4 capsules/day with placebo for 12 months | Possible efficacy of the intake of omega-3 FAs alone or in combination with vitamin D in the management of core symptoms of autism spectrum disorders. | [149] |
| Depressive disorder (n = 31) or mixed anxiety and depressive disorder (n = 29) | Randomized, double-blind, controlled | Children (7–18 years old), 60 participants | All participants received standard antidepressant therapy. Intervention group: omega-3 fish oil emulsion providing 2400 mg of total omega-3 FAs (1000 mg EPA and 750 mg DHA, EPA:DHA ratio = 1.33:1) for 12 weeks; Control group: omega-6 sunflower oil emulsion containing 2467 mg of omega-6 LA in triacylglycerol form for 12 weeks | Significant reduction in Children’s Depression Inventory scores in the group receiving omega-3 fish oil emulsion when compared to the group receiving omega-6 fish oil emulsion. At the baseline, significantly lower concentrations of EPA and DHA levels as well as a higher omega-6/omega-3 ratio were detected. | [150] |
| None | Randomized, double-blind, controlled | Adolescents (second-year high school students), 267 participants | Cohort I Intervention group: 4 krill oil capsules/day (260 mg of EPA/day and 140 mg DHA/day) for 3 months; Control group: 4 placebo capsules/day for 3 months; After 3 months: Intervention group:8 krill oil capsules/day (520 mg of EPA/day and 280 mg of DHA/day) for 9 months; Control group: 8 placebo capsules/day for 9 months. Cohort II Intervention group:8 krill oil capsules/day (520 mg of EPA/day and 280 mg of DHA/day) for 12 months; Control group: 8 placebo capsules/day for 12 months | No effect of one year of krill oil supplementation on depression score and on self-esteem score was demonstrated. However, high drop-out rate and lack of compliance could have influenced the obtained results. | [151] |
| Depressive disorder or mixed anxiety and depressive disorder | Randomized, double-blind, controlled | Children (7–18 years old), 58 participants | All patients received standard antidepressant therapy. Intervention group: 20 mL of omega-3 FAs rich fish oil emulsion (providing 2400 mg of total omega-3 FAs: 1000 mg of EPA and 750 mg of DHA, EPA:DHA ratio = 1.33:1) for 12 weeks; Control group: omega-6 FAs rich sunflower oil emulsion for 12 weeks | Improvement of symptoms measured by the Children’s Depression Inventory in the group supplemented with omega-3 fatty acids was observed. | [152] |
| Major depressive disorder or depressive disorder not otherwise specified | Randomized, double-blind, controlled | Adolescents (9–21 years old) | Intervention group: 3 capsules/day with fish oil for 12 weeks (1 capsule contains 450 mg of EPA, 40 mg DHA, and 260 mg of DHA; the total daily dose of EPA + DHA was 2130 mg; EPA:DHA ratio was 1.7:1); Control group: 3 capsules of placebo/day for 12 weeks | Monotherapy with fish oil was not superior to placebo for reducing depressive symptoms in high-risk youth as assessed by the Childhood Depression Rating Scale-Revised. | [153] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smolińska, K.; Szopa, A.; Sobczyński, J.; Serefko, A.; Dobrowolski, P. Nutritional Quality Implications: Exploring the Impact of a Fatty Acid-Rich Diet on Central Nervous System Development. Nutrients 2024, 16, 1093. https://doi.org/10.3390/nu16071093
Smolińska K, Szopa A, Sobczyński J, Serefko A, Dobrowolski P. Nutritional Quality Implications: Exploring the Impact of a Fatty Acid-Rich Diet on Central Nervous System Development. Nutrients. 2024; 16(7):1093. https://doi.org/10.3390/nu16071093
Chicago/Turabian StyleSmolińska, Katarzyna, Aleksandra Szopa, Jan Sobczyński, Anna Serefko, and Piotr Dobrowolski. 2024. "Nutritional Quality Implications: Exploring the Impact of a Fatty Acid-Rich Diet on Central Nervous System Development" Nutrients 16, no. 7: 1093. https://doi.org/10.3390/nu16071093
APA StyleSmolińska, K., Szopa, A., Sobczyński, J., Serefko, A., & Dobrowolski, P. (2024). Nutritional Quality Implications: Exploring the Impact of a Fatty Acid-Rich Diet on Central Nervous System Development. Nutrients, 16(7), 1093. https://doi.org/10.3390/nu16071093







