Weekday–Weekend Differences in Chrononutritional Variables Depend on Urban or Rural Living
Abstract
1. Introduction
2. Materials and Methods
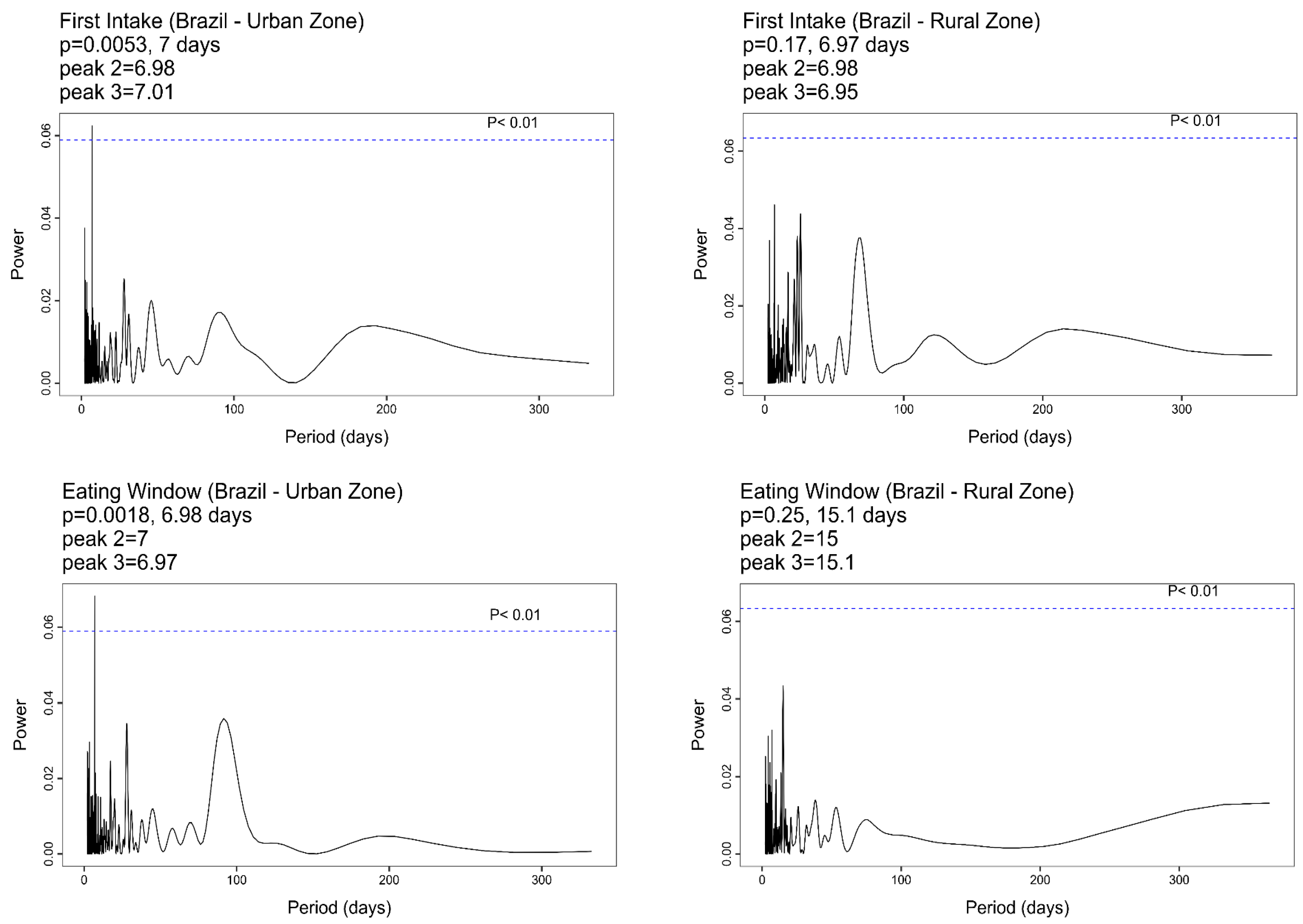
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crispim, C.A.; Mota, M.C. New Perspectives on Chrononutrition. Biol. Rhythm. Res. 2019, 50, 63–77. [Google Scholar] [CrossRef]
- Oike, H.; Oishi, K.; Kobori, M. Nutrients, Clock Genes, and Chrononutrition. Curr. Nutr. Rep. 2014, 3, 204–212. [Google Scholar] [CrossRef]
- Ahluwalia, M.K. Chrononutrition—When We Eat Is of the Essence in Tackling Obesity. Nutrients 2022, 14, 5080. [Google Scholar] [CrossRef] [PubMed]
- Spence, C. Explaining Diurnal Patterns of Food Consumption. Food Qual. Prefer. 2021, 91, 104198. [Google Scholar] [CrossRef]
- Raatz, S.K.; Conrad, Z.; Johnson, L.A.K.; Picklo, M.J.; Jahns, L. Relationship of the Reported Intakes of Fat and Fatty Acids to Body Weight in US Adults. Nutrients 2017, 9, 438. [Google Scholar] [CrossRef] [PubMed]
- Oosterman, J.E.; Kalsbeek, A.; la Fleur, S.E.; Belsham, D.D. Impact of Nutrients on Circadian Rhythmicity. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2014, 308, R337–R350. [Google Scholar] [CrossRef] [PubMed]
- Maury, E. Off the Clock: From Circadian Disruption to Metabolic Disease. Int. J. Mol. Sci. 2019, 20, 1597. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Scheer, F.A.J.L.; Saxena, R.; Garaulet, M. Timing of Food Intake: Identifying Contributing Factors to Design Effective Interventions. Adv. Nutr. 2019, 10, 606–620. [Google Scholar] [CrossRef]
- Dashti, H.S.; Gómez-Abellán, P.; Qian, J.; Esteban, A.; Morales, E.; Scheer, F.; Garaulet, M. Late Eating Is Associated with Cardiometabolic Risk Traits, Obesogenic Behaviors, and Impaired Weight Loss. Am. J. Clin. Nutr. 2021, 113, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Meléndez-Fernández, O.H.; Liu, J.A.; Nelson, R.J. Circadian Rhythms Disrupted by Light at Night and Mistimed Food Intake Alter Hormonal Rhythms and Metabolism. Int. J. Mol. Sci. 2023, 24, 3392. [Google Scholar] [CrossRef]
- Coll, A.P.; Farooqi, I.S.; O’Rahilly, S. The Hormonal Control of Food Intake. Cell 2007, 129, 251–262. [Google Scholar] [CrossRef]
- Nakamura, K.; Tajiri, E.; Hatamoto, Y.; Ando, T.; Shimoda, S.; Yoshimura, E. Eating Dinner Early Improves 24-h Blood Glucose Levels and Boosts Lipid Metabolism after Breakfast the next Day: A Randomized Cross-over Trial. Nutrients 2021, 13, 2424. [Google Scholar] [CrossRef] [PubMed]
- Luz, C.S.d.S.; da Fonseca, A.E.T.P.; Santos, J.S.; Araujo, J.F.; Duarte, L.L.; Moreno, C.R.d.C. Association of Meal Timing with Sleep Quality and Anxiety According to Chronotype: A Study of University Students. Clocks Sleep 2024, 6, 156–169. [Google Scholar] [CrossRef]
- Crispim, C.A.; Zimberg, I.Z.; Reis, B.G.; Diniz, R.M.; Tufik, S.; Mello, M.T. Relationship between Food Intake and Sleep Pattern in Healthy Individuals. J. Clin. Sleep Med. 2011, 7, 659–664. [Google Scholar] [CrossRef]
- Chaput, J.P.; McHill, A.W.; Cox, R.C.; Broussard, J.L.; Dutil, C.; da Costa, B.G.G.; Sampasa-Kanyinga, H.; Wright, K.P. The Role of Insufficient Sleep and Circadian Misalignment in Obesity. Nat. Rev. Endocrinol. 2023, 19, 82–97. [Google Scholar] [CrossRef]
- Pot, G.K.; Hardy, R.; Stephen, A.M. Irregular Consumption of Energy Intake in Meals Is Associated with a Higher Cardiometabolic Risk in Adults of a British Birth Cohort. Int. J. Obes. 2014, 38, 1518–1524. [Google Scholar] [CrossRef]
- Pot, G.K.; Almoosawi, S.; Stephen, A.M. Meal Irregularity and Cardiometabolic Consequences: Results from Observational and Intervention Studies. Proc. Nutr. Soc. 2016, 75, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Crispim, C.A.; Rinaldi, A.E.M.; Azeredo, C.M.; Skene, D.J.; Moreno, C.R.C. Is Time of Eating Associated with BMI and Obesity? A Population-Based Study. Eur. J. Nutr. 2023, 63, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Pot, G.K. Sleep and Dietary Habits in the Urban Environment: The Role of Chrono-Nutrition. Proc. Nutr. Soc. 2018, 77, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Spence, C. Explaining Seasonal Patterns of Food Consumption. Int. J. Gastron. Food Sci. 2021, 24, 100332. [Google Scholar] [CrossRef]
- An, R. Weekend-Weekday Differences in Diet among U.S. Adults, 2003–2012. Ann. Epidemiol. 2016, 26, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Guia Alimentar Para a População Brasileira Guia Alimentar Para a População Brasileira; Ministério da Saúde: Brasília, Brazil, 2014; ISBN 9788561091699.
- Rodrigues, P.R.M.; Monteiro, L.S.; de Vasconcelos, T.M.; da Silva Gomes, L.E.; Alves, I.A.; Baltar, V.T.; Gorgulho, B.M.; Yokoo, E.M.; Sichieri, R.; Pereira, R.A. How Many Meals and Snacks Do Brazilians Eat a Day? Findings from the 2017–2018 Brazilian National Dietary Survey. Cad. Saude Publica 2024, 40, e00009923. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa de Orçamentos Familiares 2008-2009: Análise Do Consumo Alimentar Pessoal No Brasil; IBGE—Coordenação de Trabalho e Rendimento: Rio de Janeiro, Brazil, 2011; ISBN 9788524041983.
- Instituto Brasileiro de Geografia e Estatística—IBGE. Pesquisa de Orçamentos Familiares 2008–2009: Despesas, Rendimentos e Condições de Vida; IBGE—Coordenação de Trabalho e Rendimento: Rio de Janeiro, Brazil, 2010; ISBN 9788524041310.
- Ruf, T. The Lomb-Scargle Periodogram in Biological Rhythm Research: Analysis of Incomplete and Unequally Spaced Time-Series. Biol. Rhythm Res. 1999, 30, 178–201. [Google Scholar] [CrossRef]
- Díez-Noguera, A. Methods for Serial Analysis of Long Time Series in the Study of Biological Rhythms. J. Circadian Rhythms 2013, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Lumley, T. Analysis of Complex Survey Samples. J. Stat. Softw. 2004, 9, 1–19. [Google Scholar] [CrossRef]
- Tang, R.; Wang, J.; Zhang, W.; Fu, W.; Zhuo, L.; Yang, J.; Wang, Q.; Yang, K. Eating Window and Eating Habits of Adults in China: A Cross-Sectional Study. Heliyon 2023, 9, e17233. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.S.; Skene, D.J.; Crispim, C.A.; Moreno, C.R.d.C. Seasonal and Regional Differences in Eating Times in a Representative Sample of the Brazilian Population. Nutrients 2023, 15, 4019. [Google Scholar] [CrossRef]
- Esposito, F.; Sanmarchi, F.; Marini, S.; Masini, A.; Scrimaglia, S.; Adorno, E.; Soldà, G.; Arrichiello, F.; Ferretti, F.; Rangone, M.; et al. Weekday and Weekend Differences in Eating Habits, Physical Activity and Screen Time Behavior among a Sample of Primary School Children: The “Seven Days for My Health” Project. Int. J. Environ. Res. Public Health 2022, 19, 4215. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, C.A.; Conroy, D.E.; Phillips, S.M.; Pfammatter, A.F.; McFadden, H.G.; Spring, B. Daily and Seasonal Influences on Dietary Self-Monitoring Using a Smartphone Application. J. Nutr. Educ. Behav. 2018, 50, 56–61.e1. [Google Scholar] [CrossRef]
- Monteiro, L.S.; Hassan, B.K.; Estima, C.C.P.; Souza, A.d.M.; Junior, E.V.; Sichieri, R.; Pereira, R.A. Food Consumption According to the Days of the Week—National Food Survey, 2008-2009. Rev. Saude Publica 2017, 51, 93. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.H.; Gu, Y.; Yan, S.; Craig, H.C.; Adams, L.; Poirier, L.; Park, R.; Gunen, B.; Gittelsohn, J. Healthy Mondays or Sundays? Weekday Preferences for Healthy Eating and Cooking among a Food Insecure Population in a U.S. Urban Environ. J. Hunger. Environ. Nutr. 2022, 17, 14–31. [Google Scholar] [CrossRef]
- Peters, B.; Vahlhaus, J.; Pivovarova-Ramich, O. Meal Timing and Its Role in Obesity and Associated Diseases. Front. Endocrinol. 2024, 15, 1359772. [Google Scholar] [CrossRef] [PubMed]
- Nabdi, S.; Boujraf, S.; Benzagmout, M. Evaluation of Rural-Urban Patterns in Dietary Intake: A Descriptive Analytical Study—Case Series. Ann. Med. Surg. 2022, 84, 104972. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, B.; Garcia, R.W.D. Práticas e Comportamento Alimentar No Meio Urbano: Um Estudo No Centro Da Cidade de São Paulo. Cad. Saude Publica 1997, 13, 455–467. [Google Scholar] [CrossRef]
- Collaço, J.H.L. Um Olhar Antropológico Sobre o Hábito de Comer Fora. CAMPOS-Rev. de Antropol. 2003, 4, 171–194. [Google Scholar] [CrossRef][Green Version]
- Forkert, E.C.O.; De Moraes, A.C.F.; Carvalho, H.B.; Manios, Y.; Widhalm, K.; González-Gross, M.; Gutierrez, A.; Kafatos, A.; Censi, L.; De Henauw, S.; et al. Skipping Breakfast Is Associated with Adiposity Markers Especially When Sleep Time Is Adequate in Adolescents. Sci. Rep. 2019, 9, 6380. [Google Scholar] [CrossRef]
- Canella, D.S.; Louzada, M.L.d.C.; Claro, R.M.; Costa, J.C.; Bandoni, D.H.; Levy, R.B.; Martins, A.P.B. Consumption of Vegetables and Their Relation with Ultra-Processed Foods in Brazil. Rev. Saúde Pública 2018, 52, 50. [Google Scholar] [CrossRef] [PubMed]
- Andrade, G.C.; Gombi-Vaca, M.F.; Louzada, M.L.D.C.; Azeredo, C.M.; Levy, R.B. The Consumption of Ultra-Processed Foods According to Eating out Occasions. Public Health Nutr. 2020, 23, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Lopes, T.d.V.C.; Borba, M.E.; Lopes, R.d.V.C.; Fisberg, R.M.; Paim, S.L.; Teodoro, V.V.; Zimberg, I.Z.; Crispim, C.A. Eating Late Negatively Affects Sleep Pattern and Apnea Severity in Individuals With Sleep Apnea. J. Clin. Sleep Med. 2019, 15, 383–392. [Google Scholar] [CrossRef]
- Arab, A.; Karimi, E.; Garaulet, M.; Scheer, F.A.J.L. Social jetlag and dietary intake: A systematic review. Sleep Med. Rev. 2023, 71, 101820. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- McHill, A.W.; Phillips, A.J.K.; Czeisler, C.A.; Keating, L.; Yee, K.; Barger, L.K.; Garaulet, M.; Scheer, F.A.J.L.; Klerman, E.B. Later Circadian Timing of Food Intake Is Associated with Increased Body Fat. Am. J. Clin. Nutr. 2017, 106, 1213–1219. [Google Scholar] [CrossRef]
- Pilz, L.K.; Levandovski, R.; Oliveira, M.A.B.; Hidalgo, M.P.; Roenneberg, T. Sleep and Light Exposure across Different Levels of Urbanisation in Brazilian Communities. Sci. Rep. 2018, 8, 11389. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, T.; Liu, J.; Probst, J.; Merchant, A.; Jones, S.; Martin, A.B. Obesity and Obesity-Related Behaviors among Rural and Urban Adults in the USA. Rural. Remote Health 2015, 15, 217–227. [Google Scholar] [CrossRef]
- Maddah, M.; Rashidi, A.; Mohammadpour, B.; Vafa, R.; Karandish, M. In-School Snacking, Breakfast Consumption, and Sleeping Patterns of Normal and Overweight Iranian High School Girls: A Study in Urban and Rural Areas in Guilan, Iran. J. Nutr. Educ. Behav. 2009, 41, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Mayén, A.L.; Marques-Vidal, P.; Paccaud, F.; Bovet, P.; Stringhini, S. Socioeconomic Determinants of Dietary Patterns in Low- and Middle-Income Countries: A Systematic Review. Am. J. Clin. Nutr. 2014, 100, 1520–1531. [Google Scholar] [CrossRef]
- Teixeira, G.P.; Da Cunha, N.B.; Azeredo, C.M.; Rinaldi, A.E.M.; Crispim, C.A. Eating Time Variation from Weekdays to Weekends and Its Association with Dietary Intake and BMI in Different Chronotypes: Findings from National Health and Nutrition Examination Survey (NHANES) 2017–2018. Br. J. Nutr. 2024, 131, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- De Castro, J.M. Weekly Rhythms of Spontaneous Nutrient Intake and Meal Pattern of Humans. Physiol. Behav. 1991, 50, 729–738. [Google Scholar] [CrossRef]
- Faber, J.; Fonseca, L.M. How Sample Size Influences Research Outcomes. Dental. Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Tracy, P.E.; Carkin, D.M. Adjusting for Design Effects in Disproportionate Stratified Sampling Designs Through Weighting. Crime Delinq. 2014, 60, 306–325. [Google Scholar] [CrossRef]
| Areas | |||
|---|---|---|---|
| Brazil (n = 5770) | Urban (n = 4400) | Rural (n = 1370) | |
| Sociodemographic Variables | % (95% CI) | % (95% CI) | % (95% CI) |
| Sex | |||
| Male | 50.4 | 49.5 * | 54.4 * |
| (49.0–51.7) | (47.9–51.1) | (52.0–56.8) | |
| Female | 49.6 | 50.5 * | 45.6 * |
| (48.2–51.0) | (48.9–52.1) | (43.2–48.0) | |
| Age (years) | |||
| 18–25 | 21.3 | 21.1 | 22.4 |
| (19.8–22.9) | (19.3–22.9) | (19.3–25.5) | |
| 26–35 | 28.1 | 28.3 | 27.2 |
| (26.2–30.0) | (26.1–30.4) | (23.7–30.7) | |
| 36–45 | 26.1 | 26.1 | 25.9 |
| (24.3–27.8) | (24.1–28.1) | (22.6–29.3) | |
| 45–59 | 24.5 | 24.5 | 24.5 |
| (22.8–26.2) | (22.6–26.4) | (21.2–27.7) | |
| Years of education | |||
| 0–10 | 56.6 | 51.3 * | 80.6 * |
| (54.4–56.7) | (48.8–53.7) | (77.8–83.5) | |
| >11 | 43.4 | 48.7 * | 19.4 * |
| (41.3–45.6) | (46.2–51.2) | (16.5–22.2) | |
| Race/ethnicity | |||
| White | 47.5 | 51.1 * | 31.3 * |
| (45.3–49.6) | (48.5–53.6) | (27.1–35.4) | |
| Black/Brown | 51.5 | 47.9 * | 67.1 * |
| (49.2–53.5) | (45.4–50.5) | (62.8–71.5) | |
| Asian/Indigenous | 0.7 | 0.6 * | 1.3 * |
| (0.4–1.1) | (0.3–1.0) | (0.2–2.4) | |
| Do not know | 0.3 | 0.4 * | 0.3 * |
| (0.1–0.6) | (0.1–0.6) | (0.0–0.7) | |
| BMI (kg/m2) | |||
| <24.9 | 54.4 | 53.4 * | 58.7 * |
| (52.5–56.3) | (51.2–55.6) | (55.4–62.0) | |
| 25–29.9 | 32.2 | 32.9 * | 29.3 * |
| (30.5–33.9) | (30.9–34.8) | (26.2–32.3) | |
| ≥30 | 13.4 | 13.7 * | 12.0 * |
| (12.1–14.7) | (12.2–15.2) | (9.4–14.6) | |
| Weekday vs. Weekend | Area | Effects/Interaction | |||||
|---|---|---|---|---|---|---|---|
| Weekday | Weekend | Urban | Rural | Weekday vs. Weekend | Area | Weekday vs. Weekend × Area | |
| Chrononutritional Variables | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | F (p-Value) | F (p-Value) | F (p-Value) |
| First Food Intake Time (h:min) | 07:42 | 07:53 | 07:57 | 07:17 | 36.04 | 64.43 | 0.38 |
| (07:37–07:46) | (07:48–07:58) | (07:51–08:03) | (07:10–07:25) | (<0.001 *) | (<0.001 *) | (0.54) | |
| Last Food Intake Time (h:min) | 20:07 | 19:59 | 20:12 | 19:39 | 4.11 | 36.03 | 3.55 |
| (20:02–20:12) | (19:53–20:04) | (20:05–20:18) | (19:30–19:47) | (0.04 *) | (<0.001 *) | (0.06) | |
| Eating Midpoint (h:min) | 13:54 | 13:56 | 14:04 | 13:28 | 2.72 | 87.64 | 3.17 |
| (13:51–13:58) | (13:52–13:59) | (14:00–14:09) | (13:22–13:34) | (0.09) | (<0.001 *) | (0.07) | |
| Caloric Midpoint (h:min) | 13:29 | 13:21 | 13:36 | 12:59 | 3.77 | 31.77 | 0.01 |
| (13:22–13:35) | (13:15–13:28) | (13:29–13:43) | (12:48–13:10) | (0.05) | (<0.001 *) | (0.96) | |
| Eating Window (decimal hour) | 12.42 | 12.09 | 12.25 | 12.30 | 30.05 | 0.86 | 1.66 |
| (12.32–12.53) | (11.96–12.23) | (12.12–12.38) | (12.15–12.45) | (<0.001 *) | (0.35) | (0.20) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, J.S.; Crispim, C.A.; Skene, D.J.; Moreno, C.R.d.C. Weekday–Weekend Differences in Chrononutritional Variables Depend on Urban or Rural Living. Nutrients 2025, 17, 108. https://doi.org/10.3390/nu17010108
Santos JS, Crispim CA, Skene DJ, Moreno CRdC. Weekday–Weekend Differences in Chrononutritional Variables Depend on Urban or Rural Living. Nutrients. 2025; 17(1):108. https://doi.org/10.3390/nu17010108
Chicago/Turabian StyleSantos, Jefferson Souza, Cibele Aparecida Crispim, Debra Jean Skene, and Claudia Roberta de Castro Moreno. 2025. "Weekday–Weekend Differences in Chrononutritional Variables Depend on Urban or Rural Living" Nutrients 17, no. 1: 108. https://doi.org/10.3390/nu17010108
APA StyleSantos, J. S., Crispim, C. A., Skene, D. J., & Moreno, C. R. d. C. (2025). Weekday–Weekend Differences in Chrononutritional Variables Depend on Urban or Rural Living. Nutrients, 17(1), 108. https://doi.org/10.3390/nu17010108








