Ultra-Processed Food and Gut Microbiota: Do Additives Affect Eubiosis? A Narrative Review
Abstract
1. Introduction
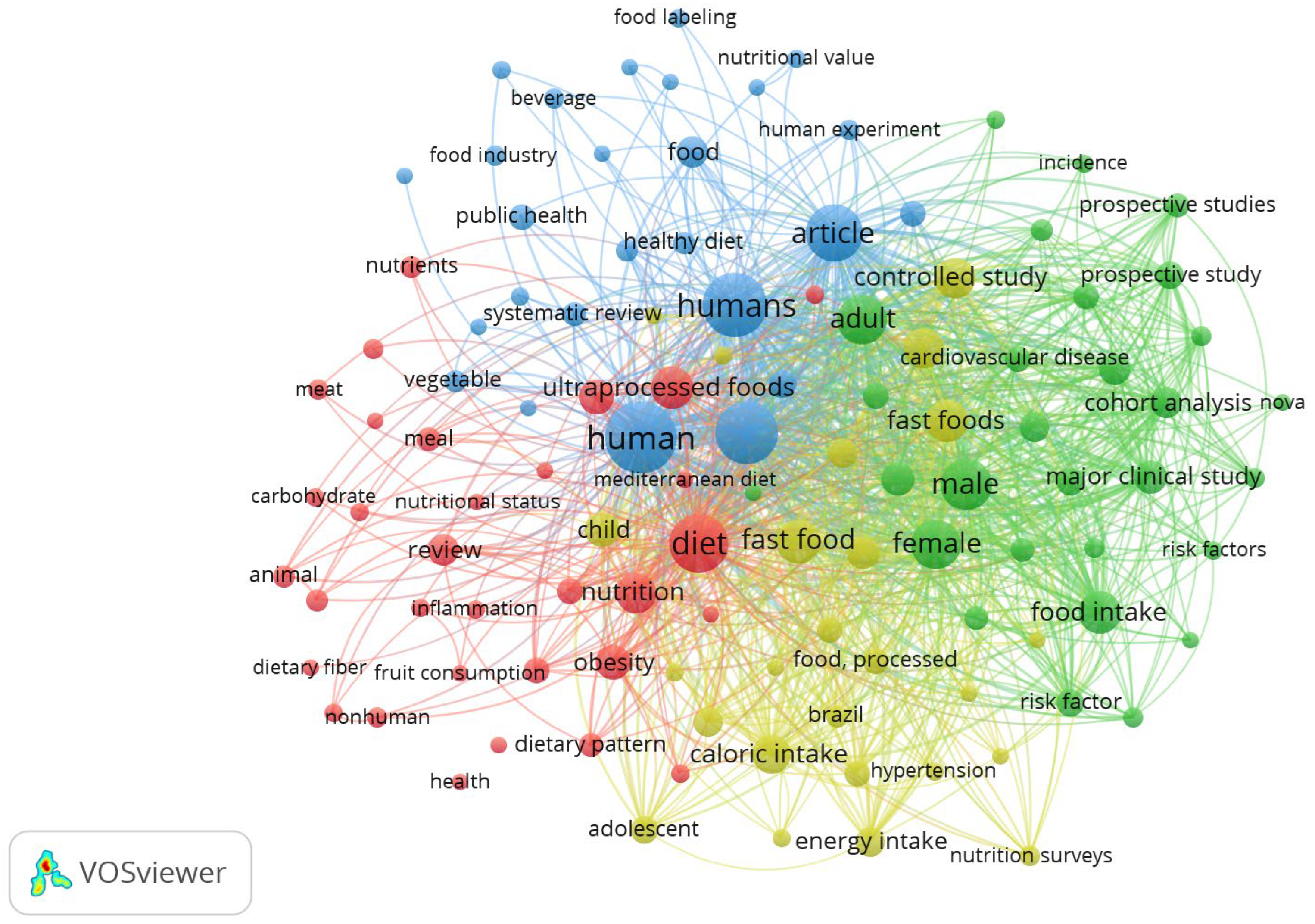
2. Research Methodology
- “Gut microbiota and ultra-processed foods”
- “Diet and gut microbiota”
- “Food additives effects on gut microbiota”
- “Intestinal health”
- “Processed food and intestinal flora”
- “Ultra-processed foods effect”
- Relevance of Title and Abstract: Articles were initially filtered by reading the titles and abstracts. Only those relevant to the topic of gut microbiota and UPFs were included.
- Publication Year: Studies published in the last 10 years were considered to ensure the currency of the information, unless they report essential details.
- Full-Text Availability: Only articles with full-text availability were included to allow detailed evaluation of methodologies and results.
3. Microbiota and Western Diet
4. Gut Microbiota and Additives
4.1. Artificial and Natural Sweeteners
4.2. Emulsifiers and Thickeners
4.3. Preservatives
4.4. Colorants
4.5. Glutamate
4.6. Other Food Additives
4.7. Food Processing Treatments
5. Gut Microbiota, Additives, and Chronic Diseases
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Monteiro, C.A.; Cannon, G.; Moubarac, J.-C.; Bertazzi-Levy, R.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinzez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Lane, M.L.; Gamage, E.; Du, S.; Ashtree, D.N.; McGuinness, A.J.; Gauci, S.; Baker, P.; Lawrence, M.; Rebholz, C.M.; Srour, B.; et al. Ultra-processed food exposure and adverse health outcomes: Umbrella review of epidemiological meta-analyses. BMJ 2024, 384, e077310. [Google Scholar] [CrossRef]
- Gomaa, E.K. Human gut microbiota/microbiome in health and diseases: A review. Antonie Van Leeuwenhoek 2020, 113, 2019–2040. [Google Scholar] [CrossRef] [PubMed]
- Sender, R.; Fuchs, S.; Milo, R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016, 14, e1002533. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Knight, R.; Mazmanian, S.K.; Cryan, J.F.; Tillisch, K. Gut microbes and the brain: Paradigm shift in neuroscience. J. Neurosci. 2015, 35, 14107–14117. [Google Scholar] [CrossRef]
- Belkaid, Y.; Hand, T.W. Role of microbiota in the immunity and inflammation. Cell 2014, 157, 121–141. [Google Scholar] [CrossRef] [PubMed]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, G.; Ianiro, G.; Kelly, C.R.; Mullish, B.H.; Allegretti, J.R.; Kassam, Z.; Putignani, L.; Fischer, M.; Keller, J.J.; Costello, S.P.; et al. International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut 2019, 68, 2111–2121. [Google Scholar] [CrossRef]
- Odamaki, T.; Kato, K.; Sugahara, H.; Hashikura, N.; Takahashi, S.; Xiao, J.Z.; Abe, F. Age-related changes in gut microbiota composition from newborn to centenarian: A cross-sectional study. BMC Microbiol. 2016, 16, 90. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Chang, H.W.; Yan, D.; Lee, K.M.; Ucmak, D.; Wong, K.; Liao, W. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017, 15, 73. [Google Scholar] [CrossRef]
- Goodrich, J.K.; Waters, J.L.; Poole, A.C.; Sutter, J.L.; Koren, O.; Blekhman, R.; Beaumont, M.; Van Treuren, W.; Knight, R.; Bell, J.T.; et al. Human genetics shape the gut microbiome. Cell 2014, 159, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Francino, M.P. Antibiotics and the human gut microbiome: Dysbioses and accumulation of resistances. Front. Microbiol. 2016, 6, 1543. [Google Scholar] [CrossRef] [PubMed]
- Yatsunenko, T.; Rey, F.E.; Manary, M.J.; Trehan, I.; Dominguez-Bello, M.G.; Contreras, M.; Magris, M.; Hidalgo, G.; Baldassano, R.N.; Anokhin, A.P.; et al. Human gut microbiome viewed across age and geography. Nature 2012, 486, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Tohumcu, E.; Raoul, P.; Fiorani, M.; Cintoni, M.; Mele, M.C.; Cammarota, G.; Gasbarrini, A.; Ianiro, G. The role of diet in shapinh huma gut microbiota. Best Pract. Res. Clin. Gastroenterol. 2023, 62–63, 101828. [Google Scholar] [CrossRef] [PubMed]
- García-Montero, C.; Fraile-Martínez, O.; Gómez-Lahoz, A.M.; Pekarek, L.; Castellanos, A.J.; Noguerales-Fraguas, F.; Coca, S.; Guijarro, L.G.; García-Honduvilla, N.; Asúnsolo, A.; et al. Nutritional components in Western diet versus Mediterranean diet at the gut microbiota–immune system interplay. Implications for health and disease. Nutrients 2021, 13, 699. [Google Scholar] [CrossRef] [PubMed]
- Kopp, W. How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2221–2236. [Google Scholar] [CrossRef]
- Toribio-Mateas, M.A.; Bester, A.; Klimenko, N. Impact of plant-based meat alternatives on the gut microbiota of consumers: A real-world study. Foods 2021, 10, 2040. [Google Scholar] [CrossRef] [PubMed]
- Dahl, W.J.; Rivero Mendoza, D.; Lambert, J.M. Diet, nutrients and the microbiome. Prog. Mol. Biol. Transl. Sci. 2020, 171, 237–263. [Google Scholar] [CrossRef]
- Redondo-Useros, N.; Nova, E.; González-Zancadam, N.; Díaz, L.E.; Gómez-Martínez, S.; Marcos, A. Microbiota and lifestyle: A special focus on diet. Nutrients 2020, 12, 1776. [Google Scholar] [CrossRef]
- Cuevas-Sierra, A.; Milagro, F.I.; Aranaz, P.; Martínez, J.A.; Riezu-Boj, J.I. Gut microbiota differences according to ultra-processed food consumption in a Spanish population. Nutrients 2021, 13, 2710. [Google Scholar] [CrossRef]
- Tandel, K.R. Sugar substitutes: Health controversy over perceived benefits. J. Pharmacol. Phar. 2011, 2, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Bian, X.; Chi, L.; Gao, B.; Tu, P.; Ru, H.; Lu, K. The artificial sweetener acesulfame potassium affects the gut microbiome and body weight gain in CD-1 mice. PLoS ONE 2017, 12, e0178426. [Google Scholar] [CrossRef] [PubMed]
- Uebanso, T.; Ohnishi, A.; Kitayama, R.; Yoshimoto, A.; Nakahashi, M.; Shimohata, T.; Mawatari, K.; Takahashi, A. Effects of low-dose non-caloric sweetener consumption on gut Microbiota in mice. Nutrients 2017, 9, 560. [Google Scholar] [CrossRef] [PubMed]
- Palmnäs, M.S.A.; Cowan, T.E.; Bomhof, M.R.; Su, J.; Reimer, R.A.; Vogel, H.J.; Hittel, D.S.; Shearer, J. Low-dose aspartame consumption differentially affects gut microbiota-host metabolic interactions in the diet-induced obese rat. PLoS ONE 2014, 9, e109841. [Google Scholar] [CrossRef]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Frankenfeld, C.L.; Sikaroodi, M.; Lamb, E.; Shoemaker, S.; Gillevet, P.M. High-intensity sweetener consumption and gut microbiome content and predicted gene function in a cross-sectional study of adults in the United States. Ann. Epidemiol. 2015, 25, 736–742. [Google Scholar] [CrossRef]
- Rodriguez-Palacios, A.; Harding, A.; Menghini, P.; Himmelman, C.; Retuerto, M.; Nickerson, K.P.; Lam, M.; Croniger, C.M.; McLean, M.H.; Durum, S.K.; et al. The artificial sweetener Splenda promotes gut Proteobacteria, dysbiosis, and myeloperoxidase reactivity in Crohn’s disease-like ileitis. Inflamm. Bowel Dis. 2018, 24, 1005–1020. [Google Scholar] [CrossRef]
- Oser, B.L.; Carson, S.; Cox, G.E.; Vogin, E.E.; Sternberg, S.S. Long-term and multigeneration toxicity studies with cyclohexylamine hydrochloride. Toxicology 1976, 6, 47–65. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Evaluations of the Joint FAO/WHO Expert Committee on Food Additives (JECFA), Cyclamic Acid. 2009. Available online: https://apps.who.int/food-additives-contaminants-jecfa-database/Home/Chemical/995 (accessed on 1 November 2024).
- Gardana, C.; Simonetti, P.; Canzi, E.; Zanchi, R.; Pietta, P. Metabolisms of stevioside and rebaudioside A from Stevia rebaudiana extracts by human microflora. J. Agric. Food Chem. 2003, 51, 6618–6622. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ojeda, F.J.; Plaza-Diaz, F.; Sàez-Lara, M.J.; Gil, A. Effect of sweeteners on the gut microbiota: A review of experimental studies and clinical trials. Adv. Nutr. 2019, 10, S31–S48. [Google Scholar] [CrossRef]
- Kasti, A.N.; Nikolaki, M.D.; Synodinou, K.-D.; Katsas, K.N.; Petsis, K.; Lambrinou, S.; Pyrousis, I.A.; Triantafyllou, K. The effects of stevia consumption on gut Bacteria: Friend or foe? Microorganisms 2022, 10, 744. [Google Scholar] [CrossRef]
- Swidsinski, A.; Ung, V.; Sydora, B.C.; Loening-Baucke, V.; Doerffel, Y.; Verstraelen, H.; Fedorak, R.N. Bacterial overgrowth and inflammation of small intestine after carboxymethylcellulose ingestion in genetically susceptible mice. Inflamm. Bowel Dis. 2009, 15, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Viennois, E.; Merlin, D.; Gewirtz, A.T.; Chassaing, B. Dietary emulsifier-induced low-grade inflammation promotes colon carcinogenesis. Cancer Res. 2017, 77, 27–40. [Google Scholar] [CrossRef]
- Chassaing, B.; Van de Wiele, T.; De Bodt, J.; Marzorati, M.; Gewirtz, A.T. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut 2017, 66, 1414–1427. [Google Scholar] [CrossRef] [PubMed]
- González-Bermúdez, C.A.; López-Nicolás, R.; Peso-Echarri, P.; Frontela-Saseta, C.; Martínez-Graciá, C. Effects of different thickening agents on infant gut microbiota. Food Funct. 2018, 9, 1768–1778. [Google Scholar] [CrossRef]
- Wu, W.; Zhou, J.; Xuan, R.; Chen, J.; Han, H.; Liu, J.; Niu, T.; Chen, H.; Wang, F. Dietary κ-carrageenan facilitates gut microbiota-mediated intestinal inflammation. Carbohydr. Polym. 2022, 277, 118830. [Google Scholar] [CrossRef] [PubMed]
- Bellanco, A.; Félix, J.; Dìaz del Cerro, E.; Martìnez Cuesta, M.C.; De La Fuente, M.; Requena, T. Influence of consumption of food additive carrageenan on the gut microbiota and the intestinal homestostasis of mice. Food Funct. 2024, 15, 6759. [Google Scholar] [CrossRef]
- Baerber, C.; Sabater, C.; Guarner, F.; Margolles, A.; Azpiroz, F. Metabolic response of intestinal microbiota to guar gum consumption. Front. Nutr. 2023, 10, 1160694. [Google Scholar] [CrossRef]
- Paudel, D.; Nair, D.V.T.; Tian, S.; Hao, F.; Goand, U.K.; Joseph, G.; Prodes, E.; Chai, Z.; Robert, C.E.M.; Chassaing, B.; et al. Dietary fiber guar gum-induced shift in gut microbiota metabolism and intestinal immune activity enhances susceptibility to colonic inflammation. Gut Microbes 2024, 16, 2341457. [Google Scholar] [CrossRef]
- Mafra, D.; Baptista, B.A.; Sahiun, E.; Abuznada, S.; Leal, V.O.; Borges, N.A. May polydextrose potentially improve gut health in patients with chronic kidney disease? Clin. Nutr. ESPEN 2022, 51, 7–16. [Google Scholar] [CrossRef]
- Costabile, A.; Fava, F.; Röytiö, H.; Forssten, S.D.; Olli, K.; Klievink, J.; Rowland, I.R.; Ouwehand, A.C.; Rastall, R.A.; Gibson, G.R.; et al. Impact of polydextrose on the faecal microbiota: A double-blind, crossover, placebo-controlled feeding study in healthy human subjects. Br. J. Nutr. 2012, 108, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Shere Raza, G.; Ptaala, H.; Hibberd, A.A.; Alhoniemi, E.; Tiihonen, K.; Mäkelä, K.A.; Herzig, K.-H. Polydextrose changes the gut microbiome and attenuates fasting triglyceride and cholesterol levels in Western diet fed mice. Sci. Rep. 2017, 7, 5294. [Google Scholar] [CrossRef]
- Arnold, A.R.; Chassaing, B. Maltodextrin, modern stressor of the intestinal environment. Cell. Mol. Gastroenterol. Hepatol. 2019, 7, 475. [Google Scholar] [CrossRef] [PubMed]
- Zangara, M.T.; Ponti, A.K.; Miller, N.D.; Engelhart, M.J.; Ahern, P.P.; Sangwan, N.; McDonald, C. Maltodextrin consumption impairs the intestinal mucus barrier and accelerates colitis through direct actions on the epithelium. Front. Immunol. 2022, 13, 841188. [Google Scholar] [CrossRef]
- Almutairi, R.; Basson, A.R.; Wearsh, P.; Cominelli, F.; Rodriguez-Palacios, A. Validity of food additive maltodextrin as placebo and effects on human gut physiology: Systematic review of placebo-controlled clinical trials. Eur. J. Nutr. 2022, 61, 2853–2871. [Google Scholar] [CrossRef] [PubMed]
- Chassaing, B.; Koren, O.; Goodrich, J.C.; Poole, A.C.; Srinivasan, S.; Ley, R.E.; Gewirtz, A.T. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 2015, 519, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Panyod, S.; Wu, W.-K.; Chang, C.-T.; Wada, N.; Ho, H.-C.; Lo, Y.-L.; Tsai, S.-P.; Chen, R.-A.; Huang, H.-S.; Liu, P.-Y.; et al. Common dietary emulsifiers promote metabolic disorders and intestinal microbial dysbiosis in mice. Comm. Biol. 2024, 7, 749. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Penhoat, A.; Coüedelo, L.; Monnoye, M.; Rainteau, D.; Meugnier, E.; Bary, S.; Abrous, H.; Loizon, E.; Krasniqi, P.; et al. Natural emulsifiers lecithins preserve gut microbiota diversity in relation with specific faecal lipids in high fat-fed mice. J. Funct. Foods 2023, 105, 105540. [Google Scholar] [CrossRef]
- Irwin, S.V.; Fisher, P.; Graham, E.; Malek, A.; Robidoux, A. Sulfites inhibit the growth of four species of beneficial gut bacteria at concentrations regarded as safe for food. PLoS ONE 2017, 12, e0186629. [Google Scholar] [CrossRef]
- Hrncirova, L.; Hudcovic, T.; Sukova, E.; Machova, V.; Trckova, E.; Krejsek, J.; Hrncir, T. Human gut microbes are susceptible to antimicrobial food additives in vitro. Folia Microbiol. 2019, 64, 497–508. [Google Scholar] [CrossRef]
- Le Lay, C.; Fernandez, B.; Hammami, R.; Ouellette, M.; Fliss, I. On Lactococcus lactis UL719 competitivity and nisin (Nisaplin®) capacity to inhibit Clostridium difficile in a model of human colon. Front. Microbiol. 2015, 6, 1020. [Google Scholar] [CrossRef]
- Barciela, P.; Perez-Vazquez, A.; Prieto, M.A. Azo dyes in the food industry: Features, classification, toxicity, alternatives, and regulation. Food Chem. Toxicol. 2023, 178, 113935. [Google Scholar] [CrossRef] [PubMed]
- Lehto, S.; Buchweitz, M.; Klimm, A.; Strassburger, R.; Bechtold, C.; Ulberth, F. Comparison of food colour regulations in the EU and the US: A review of current provisions. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2017, 34, 335–355. [Google Scholar] [CrossRef]
- Miller, M.D.; Steinmaus, C.; Golub, M.S.; Castorina, R.; Thilakartne, R.; Bradman, A.; Marty, M.A. Potential impacts of synthetic food dyes on activity and attention in children: A review of the human and animal evidence. Environ. Health 2022, 21, 45. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Lv, X.; Zhang, Y.; Xin, Q.; Zou, Y.; Li, X. Tartrazine exposure results in histological damage, oxidative stress, immune disorders and gut microbiota dysbiosis in juvenile crucian carp (Carassius carassius). Aquat. Toxicol. 2021, 241, 105998. [Google Scholar] [CrossRef]
- Bettini, S.; Boutet-Robinet, E.; Cartier, C.; Coméra, C.; Gaultier, E.; Dupuy, J.; Naud, N.; Taché, S.; Grysan, P.; Reguer, S.; et al. Food-grade TiO2 impairs intestinal and systemic immune homeostasis, initiates preneoplastic lesions and promotes aberrant crypt development in the rat colon. Sci. Rep. 2017, 7, 40373. [Google Scholar] [CrossRef]
- Yan, J.; Wang, D.; Li, K.; Chen, Q.; Lai, W.; Tian, L.; Lin, B.; Tan, Y.; Liu, X.; Xi, Z. Toxic effects of the food additives titanium dioxide and silica on the murine intestinal tract: Mechanisms related to intestinal barrier dysfunction involved by gut microbiota. Environ. Toxicol. Pharmacol. 2020, 80, 103485. [Google Scholar] [CrossRef]
- Mu, W.; Wang, Y.; Huang, C.; Fu, Y.; Li, J.; Wang, H.; Jia, H.; Ba, Q. Effect of long-term intake of dietary titanium dioxide nanoparticles on intestine inflammation in mice. J. Agric. Food Chem. 2019, 67, 9382–9389. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Chang, H.; Wang, R.; You, Z.; Jiang, S.; Ma, C.; Huo, D.; Zu, X.; Zhang, J. Potassium sorbate suppresses intestinal microbial activity and triggers immune regulation in zebrafish (Danio rerio). Food Funct. 2019, 10, 7164–7173. [Google Scholar] [CrossRef]
- Cao, Y.; Liu, H.; Qin, N.; Ren, X.; Zhu, B.; Xia, X. Impact of food additives on the composition and function of gut microbiota: A review. Trends Food Sci. Technol. 2020, 99, 295–310. [Google Scholar] [CrossRef]
- Ahangari, H.; Bahramian, B.; Khezerlou, A.; Tavassoli, M.; Kiani-Silani, N.; Tarhriz, V.; Ehsani, A. Association between monosodium glutamate consumption with changes in gut microbiota and related metabolic dysbiosis—A systematic review. Food Sci. Nutr. 2024, 12, 5285–5295. [Google Scholar] [CrossRef]
- Onyesife, C.O.; Chukwuma, I.F.; Okagu, I.U.; Ndefo, J.C.; Amujiri, N.A.; Ogugua, V.N. Nephroprotective effects of Piper nigrum extracts against monosodium glutamate-induced renal toxicity in rats. Sci. Afr. 2023, 19, e01453. [Google Scholar] [CrossRef]
- Shosha, H.M.; Ebaid, H.M.; Toraih, E.A.; Abdelrazek, H.M.; Elrayess, R.A. Effect of monosodium glutamate on fetal development and progesterone level in pregnant Wistar albino rats. Environ. Sci. Pol. Res. 2023, 30, 49779–49797. [Google Scholar] [CrossRef]
- Jakobsson, H.E.; Rodríguez-Piñeiro, A.M.; Schütte, A.; Ermund, A.; Boysen, P.; Bemark, M.; Sommer, F.; Bäckhed, F.; Hansson, G.C.; Johansson, M.E. The composition of the gut microbiota shapes the colon mucus barrier. EMBO Rep. 2015, 16, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-J.; Chen, M.; Wang, F.-Z.; Bao, Y.-M.; Xin, F.-J.; Wen, B.-T. In vitro fermentation of monosodium glutamate with human gut microbes. Biotechnol. Bull. 2020, 36, 104. [Google Scholar] [CrossRef]
- Balamurugan, R.; George, G.; Kabeerdoss, J.; Hepsiba, J.; Chandragunasekaran, A.M.; Ramakrishna, B.S. Quantitative differences in intestinal Faecalibacterium prausnitzii in obese Indian children. Br. J. Nutr. 2010, 103, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Xie, S.; Lv, D.; Zhang, Y.; Deng, J.; Zeng, L.; Chen, Y. A reduction in the butyrate producing species Roseburia spp. and Faecalibacterium prausnitzii is associated with chronic kidney disease progression. Antonie Van Leeuwenhoek 2016, 109, 1389–1396. [Google Scholar] [CrossRef]
- Kikuchi, K.; Saigusa, D.; Kanemitsu, Y.; Matsumoto, Y.; Thanai, P.; Suzuki, N.; Mise, K.; Yamaguchi, H.; Nakamura, T.; Asaji, K. Gut microbiome-derived phenyl sulfate contributes to albuminuria in diabetic kidney disease. Nat. Comm. 2019, 10, 1835. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Huo, D.; Ma, C.; Jiang, S.; Wang, L.; Zhang, J. Monosodium glutamate induces limited modulation in gut microbiota. J. Funct. Foods 2018, 49, 493–500. [Google Scholar] [CrossRef]
- Bento, M.H.L.; Ouwehand, A.C.; Tiihonen, K.; Lahtinen, S.; Nurminen, P.; Saarinen, M.T.; Schulze, H.; Mygind, T.; Fischer, J. Essential oils and their use in animal feeds for monogastric animals—Effects on feed quality, gut microbiota, growth performance and food safety: A review. Vet. Med. 2013, 58, 449–458. [Google Scholar] [CrossRef]
- Wei, X.; Bottoms, K.A.; Stein, H.H.; Blavi, L.; Bradley, C.L.; Bergstrom, J.; Knapp, J.; Story, R.; Maxwell, C.; Tsai, T.; et al. Dietary organic acids modulate gut microbiota and improve growth performance of nursery pigs. Microorganisms 2021, 9, 110. [Google Scholar] [CrossRef]
- Resende, M.; Chaves, R.F.; Garcia, R.M.; Barbosa, J.A.; Marques, A.S.; Rezende, L.R.; Peconick, A.P.; Garbossa, C.A.P.; Mesa, D.; Silva, C.C.; et al. Benzoic acid and essential oils modify the cecum microbiota composition in weaned piglets and improve growth performance in finishing pigs. Livest. Sci. 2020, 242, 104311. [Google Scholar] [CrossRef]
- Gerasimidis, K.; Bryden, K.; Chen, X.; Papachristou, E.; Verney, A.; Roig, M.; Hansen, R.; Nichols, B.; Papadopoulou, R.; Parrett, A. The impact of food additives, artificial sweeteners and domestic hygiene products on the human gut microbiome and its fibre fermentation capacity. Eur. J. Nutr. 2020, 59, 3213–3230. [Google Scholar] [CrossRef]
- Li, P.; Li, M.; Wu, T.; Song, Y.; Li, Y.; Huang, X.; Lu, H.; Xu, Z.Z. Systematic evaluation of antimicrobial food preservatives on glucose metabolism and gut microbiota in healthy mice. NPJ Sci. Food 2022, 6, 42. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, D. Thermal processing of food reduces gut microbiota diversity of the host and triggers adaptation of the microbiota: Evidence from two vertebrates. Microbiome 2018, 6, 99. [Google Scholar] [CrossRef]
- Pérez-Burillo, S.; Pastoriza, S.; Jiménez-Hernández, N.; D’Auria, G.; Francino, M.P.; Rufián-Henares, J.A. Effect of food thermal processing on the composition of gut microbiota. J. Agric. Food Chem. 2018, 66, 11500–11509. [Google Scholar] [CrossRef]
- Lerma-Aguilera, A.M.; Pérez-Burillo, S.; Navajas-Porras, B.; León, E.D.; Ruíz-Pérez, S.; Pastoriza, S.; Jiménez-Hernández, N.; Cämmerer, B.-M.; Rufián-Henares, J.A.; Gosalbes, M.J.; et al. Effects of different cooking methods on the gut microbiota: An in vitro approach. Front. Microbiol. 2024, 14, 1334623. [Google Scholar] [CrossRef]
- Martínez Leo, E.E.; Segura Campos, M.R. Effect of ultra-processed diet on gut microbiota and thus its role in neurodegenerative diseases. Nutrition 2020, 71, 110609. [Google Scholar] [CrossRef] [PubMed]
- Atzeni, A.; Martínez, M.A.; Babio, N.; Konstanti, P.; Tinahones, F.J.; Vioque, J.; Corella, D.; Fitó, M.; Vidal, J.; Moreno-Indias, I.; et al. Association between ultra-processed food consumption and gut microbiota in senior subjects with overweight/obesity and metabolic syndrome. Front. Nutr. 2022, 9, 976547. [Google Scholar] [CrossRef]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed foods and cardiovascular diseases: Potential mechanisms of action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef]
- Song, Z.; Song, R.; Liu, Y.; Wu, Z.; Zhang, X. Effects of ultra-processed foods on the microbiota-gut-brain axis: The bread-and-butter issue. Food Res. Int. 2023, 167, 112730. [Google Scholar] [CrossRef]
- Laudanno, O.M. Cambios en la microbiota por ultraprocesados: Obesidad, cáncer y muerte prematura [Changes in the microbiota due to ultra-processed foods: Obesity, cancer and premature death]. Med.-Buenos Aire 2023, 83, 278–282. [Google Scholar]
- Elechi, J.O.G.; Sirianni, R.; Conforti, F.L.; Cione, E.; Pellegrino, M. Food system transformation and gut microbiota transition: Evidence on advancing obesity, cardiovascular diseases, and cancers-a narrative review. Foods 2023, 12, 2286. [Google Scholar] [CrossRef]
| Sweetener | Effects on Gut Microbiota | References |
|---|---|---|
| Acesulfame Potassium | Significant increase in body weight in male mice, changes in bacterial composition with an increase in specific genera (Bacteroides, Sutterella, Anaerostipes) in male mice, variations in bacterial metabolites and gene expression in female mice | [25] |
| Aspartame | Increase in Clostridium leptum and Enterobacteriaceae in mice, changes in bacterial composition in diet-induced obese mice, variations in glucose response in mice and humans | [27] |
| Saccharin | Proliferation of bacteria like Clostridiales and Bacteroidetes, reduction in Lactobacillus and Firmicutes, increased glucose response, changes in bacterial composition in mice and humans | [23,26] |
| Sucralose | Changes in bacterial composition with an increase in specific genera, reduction of butyrate levels in the intestinal lumen, potential correlation with conditions such as colitis | [23,24,28] |
| Thickener/Emulsifier | Main Effects on Gut Microbiota | References |
|---|---|---|
| Carboxymethyl cellulose (CMC) | Increased bacterial proliferation in the intestine, induction of intestinal inflammation, changes in microbiota composition and functionality | [34,35] |
| Carrageenan | Mucus degradation Oxidative stress | [38,39] |
| Guar gum | Modulation of gut microbiota with changes in Parabacteroides, Ruminococcus, Faecalibacterium, Alistipes, Fusicatenibacter, and Eubacterium, among others Possible induction of colitis | [40] [41] |
| Polydextrose | Increased levels of SCFA; positive effects on peristalsis | [42] |
| Maltodextrin | Possible detrimental effects on Akkermansia, Lactobacillus, and Bifidobacterium | [46] |
| Polysorbate 80 (P80) | Altered microbiota composition, potential induction of intestinal inflammation, changes in cell proliferation and apoptosis | [36,48] |
| Lecithin and sucrose fatty acid esters | Changes in alpha and beta biodiversities | [49,50] |
| Preservative | Main Effects on Gut Microbiota | References |
|---|---|---|
| Sulfur dioxide | Inhibition of beneficial bacterial growth, potential impact on gut microbiota composition | [51] |
| Sodium Benzoate, Potassium Sorbate | Variable sensitivity of bacterial species, possible effect on microbiota diversity and composition | [52] |
| Na-nitrite | Enhancement of pro-inflammatory genera | [52] |
| Nisin | Possible impact on microbiota diversity and composition, effects on pathogenic and beneficial bacterial growth | [53] |
| Aspect | Changes Induced by UPFs | Health Consequences |
|---|---|---|
| Gut Microbiota Balance | Significant alteration | Onset of chronic diseases, including neurodegenerative diseases |
| Bacterial Composition | Increase in bacteria associated with metabolic disorders (e.g., Alloprevotella, Negativibacillus, Prevotella, Sutterella) | Risk of adverse metabolic conditions |
| SCFA Production | Reduction due to diets high in simple sugars and fats | Alterations in energy metabolism and intermediate metabolism with effects on the brain |
| Intestinal Inflammation | Increased pro-inflammatory potential caused by food additives (e.g., polysorbate 80, carboxymethylcellulose) | Enhanced intestinal inflammation |
| Metabolic Diseases | 32% increased risk | Growth of chronic metabolic diseases prevalence |
| Neurodegenerative Diseases | Dysregulation of gut microbiota | Contribution to the development of Alzheimer’s, Parkinson’s, ALS, Friedreich’s ataxia |
| Cardiovascular Health | Harmful effects from saturated fats, added sugars, salt, and food additives | Increased risk of heart disease, high cholesterol, systemic inflammation |
| Microbiota Composition and Diversity | Negative influence from Western diet rich in UPFs | Gut dysbiosis, contribution to neurological and metabolic diseases |
| Cancer Risk | 29% increased risk of colon cancer in men | Carcinogenesis, obesity, type 2 diabetes, cardiovascular diseases |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bevilacqua, A.; Speranza, B.; Racioppo, A.; Santillo, A.; Albenzio, M.; Derossi, A.; Caporizzi, R.; Francavilla, M.; Racca, D.; Flagella, Z.; et al. Ultra-Processed Food and Gut Microbiota: Do Additives Affect Eubiosis? A Narrative Review. Nutrients 2025, 17, 2. https://doi.org/10.3390/nu17010002
Bevilacqua A, Speranza B, Racioppo A, Santillo A, Albenzio M, Derossi A, Caporizzi R, Francavilla M, Racca D, Flagella Z, et al. Ultra-Processed Food and Gut Microbiota: Do Additives Affect Eubiosis? A Narrative Review. Nutrients. 2025; 17(1):2. https://doi.org/10.3390/nu17010002
Chicago/Turabian StyleBevilacqua, Antonio, Barbara Speranza, Angela Racioppo, Antonella Santillo, Marzia Albenzio, Antonio Derossi, Rossella Caporizzi, Matteo Francavilla, Deborah Racca, Zina Flagella, and et al. 2025. "Ultra-Processed Food and Gut Microbiota: Do Additives Affect Eubiosis? A Narrative Review" Nutrients 17, no. 1: 2. https://doi.org/10.3390/nu17010002
APA StyleBevilacqua, A., Speranza, B., Racioppo, A., Santillo, A., Albenzio, M., Derossi, A., Caporizzi, R., Francavilla, M., Racca, D., Flagella, Z., De Santis, M. A., Elia, A., Conversa, G., Luchetti, L., Sinigaglia, M., & Corbo, M. R. (2025). Ultra-Processed Food and Gut Microbiota: Do Additives Affect Eubiosis? A Narrative Review. Nutrients, 17(1), 2. https://doi.org/10.3390/nu17010002












