Achievements in the Pathophysiology and Treatment of Insulin Resistance: Every Step Matters
Conflicts of Interest
References
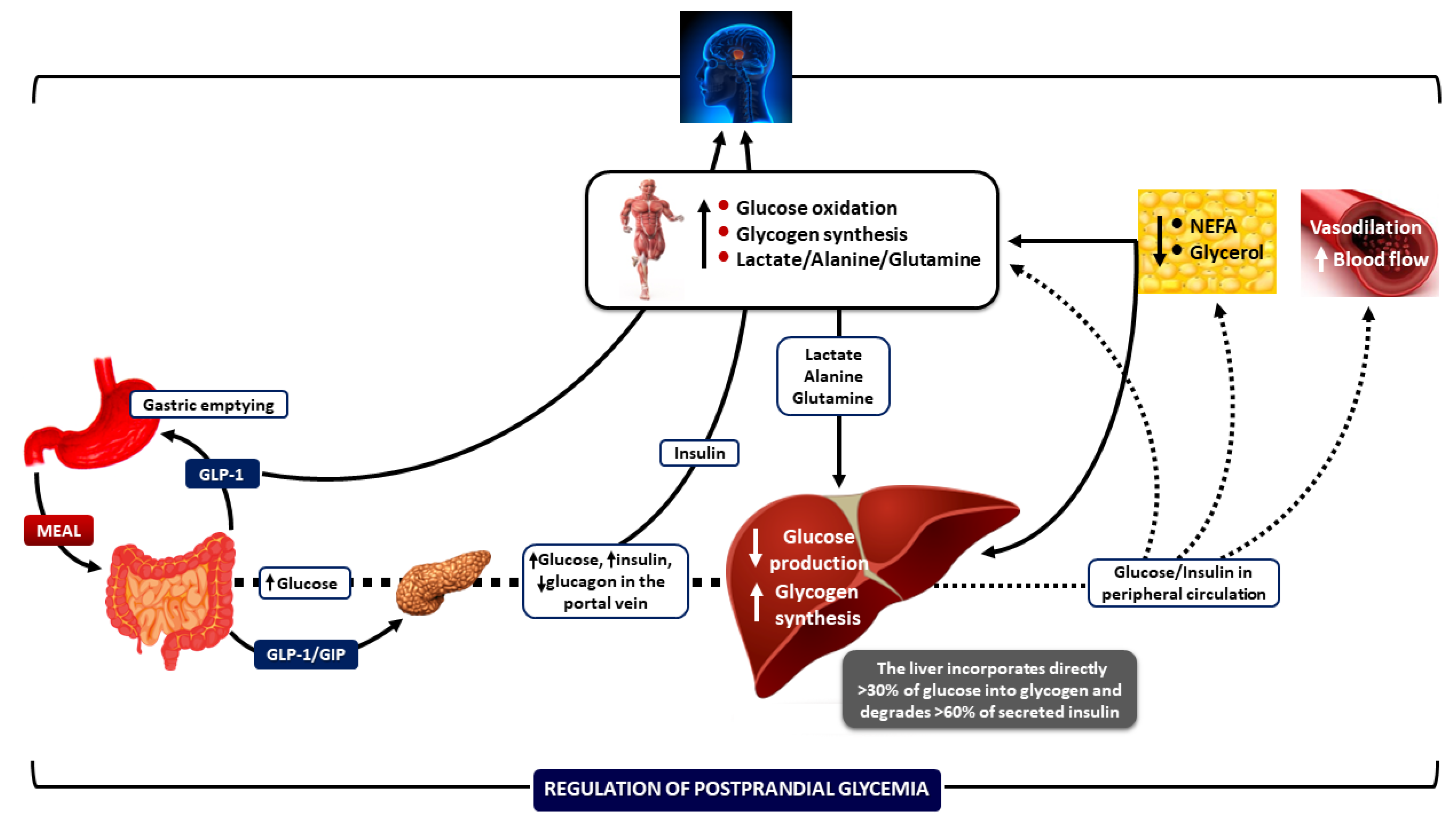
- Dimitriadis, G.D.; Maratou, E.; Kountouri, A.; Board, M.; Lambadiari, V. Regulation of postabsorptive and postprandial glucose metabolism by insulin-dependent and insulin-independent mechanisms: An integrative approach. Nutrients 2021, 13, 159. [Google Scholar] [CrossRef] [PubMed]
- Roden, M.; Shulman, G.I. The Integrative Biology of Type 2 Diabetes. Nature 2019, 576, 51–60. [Google Scholar] [CrossRef]
- Ward, C.W.; Lawrence, M.C. Landmarks in insulin research. Front. Endocrinol. 2011, 2, 76. [Google Scholar] [CrossRef]
- Rowlands, J.; Heng, J.; Newsholme, P.; Carlessi, R. Pleiotropic effects of GLP-1 and analogs on cell signaling, metabolism and function. Front. Endocrinol. 2018, 9, 672. [Google Scholar] [CrossRef] [PubMed]
- Marilly, E.; Cottin, J.; Cabrera, N.; Cornu, C.; Boussageon, R.; Moulin, P.; Lega, J.C.; Gueyffier, F.; Cucherat, M.; Grenet, G. SGLT2 inhibitors in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials balancing their risks and benefits. Diabetologia 2022, 65, 2000–2010. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Juneja, R.; Beals, J.M.; Moyers, J.S.; Ilag, L.; McCrimmon, R.J. The Basis for Weekly Insulin Therapy: Evolving Evidence with Insulin Icodec and Insulin Efsitora Alfa. Endocr. Rev. 2024, 45, 379–413. [Google Scholar] [CrossRef]
- Tessari, P. Stepwise Discovery of Insulin Effects on Amino Acid and Protein Metabolism. Nutrients 2024, 16, 119. [Google Scholar] [CrossRef]
- Veneti, S.; Grammatikopoulou, M.G.; Kintiraki, E.; Mintziori, G.; Goulis, D.G. Ketone Bodies in Diabetes Mellitus: Friend or Foe? Nutrients 2023, 15, 4383. [Google Scholar] [CrossRef]
- Małodobra-Mazur, M.; Lewoń, D.; Cierzniak, A.; Okulus, M.; Gliszczyńska, A. Phospholipid Derivatives of Cinnamic Acid Restore Insulin Sensitivity in Insulin Resistance in 3T3-L1 Adipocytes. Nutrients 2021, 13, 3619. [Google Scholar] [CrossRef]
- Serbis, A.; Giapros, V.; Tsamis, K.; Balomenou, F.; Galli-Tsinopoulou, A.; Siomou, E. Beta Cell Dysfunction in Youth- and Adult-Onset Type 2 Diabetes: An Extensive Narrative Review with a Special Focus on the Role of Nutrients. Nutrients 2023, 15, 2217. [Google Scholar] [CrossRef]
- Papakonstantinou, E.; Oikonomou, C.; Nychas, G.; Dimitriadis, G.D. Effects of Diet, Lifestyle, Chrononutrition and Alternative Dietary Interventions on Postprandial Glycemia and Insulin Resistance. Nutrients 2022, 14, 823. [Google Scholar] [CrossRef]
- Tsitsou, S.; Zacharodimos, N.; Poulia, K.-A.; Karatzi, K.; Dimitriadis, G.; Papakonstantinou, E. Effects of Time-Restricted Feeding and Ramadan Fasting on Body Weight, Body Composition, Glucose Responses, and Insulin Resistance: A Systematic Review of Randomized Controlled Trials. Nutrients 2022, 14, 4778. [Google Scholar] [CrossRef] [PubMed]
- Mourouti, N.; Mavrogianni, C.; Mouratidou, T.; Liatis, S.; Valve, P.; Rurik, I.; Torzsa, P.; Cardon, G.; Bazdarska, Y.; Iotova, V.; et al. The Association of Lifestyle Patterns with Prediabetes in Adults from Families at High Risk for Type 2 Diabetes in Europe: The Feel4Diabetes Study. Nutrients 2023, 15, 3155. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Sun, Q.; Czernichow, S.; Kivimäki, M.; Batty, G.D. Bidirectional Association Between Depression and Metabolic Syndrome: A Systematic Review and Meta-Analysis. Lancet Psychiatry 2017, 4, 1–10. [Google Scholar]
- Yang, F.; Wang, X.; Qi, J.; Zhang, K.; Jiang, Y.; Feng, B.; Lv, T.; Yang, L.; Yang, Q.; Zhao, M.; et al. Glucagon-like Peptide 1 Receptor Activation Inhibits Microglial Pyroptosis via Promoting Mitophagy to Alleviate Depression-like Behaviors in Diabetic Mice. Nutrients 2023, 15, 38. [Google Scholar] [CrossRef]
- Lu, S.; Li, Y.; Qian, Z.; Zhao, T.; Feng, Z.; Weng, X.; Yu, L. Role of the Inflammasome in Insulin Resistance and Type 2 Diabetes Mellitus. Front. Immunol. 2023, 14, 1052756. [Google Scholar] [CrossRef] [PubMed]
- Kounatidis, D.; Vallianou, N.; Evangelopoulos, A.; Vlahodimitris, I.; Grivakou, E.; Kotsi, E.; Dimitriou, K.; Skourtis, A.; Mourouzis, I. SGLT-2 Inhibitors and the Inflammasome: What’s Next in the 21st Century? Nutrients 2023, 15, 2294. [Google Scholar] [CrossRef]
- Zhu, J.; Hu, Z.; Luo, Y.; Liu, Y.; Luo, W.; Du, X.; Luo, Z.; Hu, J.; Peng, S. Diabetic peripheral neuropathy: Pathogenetic mechanisms and treatment. Front. Endocrinol. 2024, 14, 1265372. [Google Scholar] [CrossRef]
- Ntavidi, S.; Katsanou, P.; Marakomichelakis, G.; Kasdagli, M.-I.; Antiochou, E.; Mpali, I.; Kakou, A.M.; Tsioufis, K.; Dimitriadis, G.; Lambadiari, V. Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece. Nutrients 2023, 15, 72. [Google Scholar] [CrossRef]
- Sulaiman, M.K. Diabetic nephropathy: Recent advances in pathophysiology and challenges in dietary management. Diabetol. Metab. Syndr. 2019, 11, 7. [Google Scholar] [CrossRef]
- Lin, S.-P.; Chen, C.-M.; Wang, K.-L.; Wu, K.-L.; Li, S.-C. Association of Dietary Fish and n-3 Unsaturated Fatty Acid Consumption with Diabetic Nephropathy from a District Hospital in Northern Taiwan. Nutrients 2022, 14, 2148. [Google Scholar] [CrossRef] [PubMed]
- Plows, J.F.; Stanley, J.L.; Baker, P.N.; Reynolds, C.M.; Vickers, M.H. The Pathophysiology of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 3342. [Google Scholar] [CrossRef] [PubMed]
- Tranidou, A.; Magriplis, E.; Tsakiridis, I.; Pazaras, N.; Apostolopoulou, A.; Chourdakis, M.; Dagklis, T. Effect of Gestational Weight Gain during the First Half of Pregnancy on the Incidence of GDM, Results from a Pregnant Cohort in Northern Greece. Nutrients 2023, 15, 893. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitriadis, G. Achievements in the Pathophysiology and Treatment of Insulin Resistance: Every Step Matters. Nutrients 2025, 17, 1223. https://doi.org/10.3390/nu17071223
Dimitriadis G. Achievements in the Pathophysiology and Treatment of Insulin Resistance: Every Step Matters. Nutrients. 2025; 17(7):1223. https://doi.org/10.3390/nu17071223
Chicago/Turabian StyleDimitriadis, George. 2025. "Achievements in the Pathophysiology and Treatment of Insulin Resistance: Every Step Matters" Nutrients 17, no. 7: 1223. https://doi.org/10.3390/nu17071223
APA StyleDimitriadis, G. (2025). Achievements in the Pathophysiology and Treatment of Insulin Resistance: Every Step Matters. Nutrients, 17(7), 1223. https://doi.org/10.3390/nu17071223




