Abstract
In bee venom pharmacopuncture (BVP), bee venom isolated from the venom sac of bees is injected into the acupoint or muscle associated with a disease. However, the histamine component in bee venom can cause adverse events; therefore, attention is required for BVP use. This study investigated the frequency, severity and characteristics of patients developing BVP-associated adverse events. The medical records of patients treated with BVP at Kyung Hee University Korean Medicine Hospital between 1 January 2013 and 1 May 2021 were reviewed. The demographic characteristics, disease-related characteristics, treatment-related characteristics and impressions of each patient were analyzed. In this study, >50% of 4821 inpatients were hospitalized for neurological disorders. The mean age of the overall study population was 54.62 ± 16.38 years and 61% were women. The frequency of adverse events was 2.32%. The mean age in the adverse events group was 58.20 ± 16.10 years and 76% were women. Two patients experienced moderate adverse events, with no commonality between these events. Every patient recovered naturally with no sequelae. The results showed that BVP is a relatively safe therapeutic method. However, further studies are needed to determine the frequency of adverse events and identify the causality between baseline characteristics and adverse events.
Key Contribution:
This study investigated the frequency, severity and characteristics of patients developing bee venom pharmacopuncture (BVP)-associated adverse events. The results of the present study showed that BVP is a relatively safe therapeutic method.
1. Introduction
Bee venom pharmacopuncture (BVP) is a treatment method used in traditional East Asian medicine. The method involves the injection of venom extracted and processed from the venom sac of honeybees into an acupoint or intramuscular pressure point associated with disease for therapeutic purposes [1,2,3]. Although BVP is used for the treatment of musculoskeletal disorders as well as various other diseases, some components in the body act as antigens and can cause life-threatening adverse events (AEs), such as anaphylaxis [4,5].
Therefore, skin testing is performed by subcutaneously injecting a solution containing bee venom (BV) before performing BVP to prevent AEs in the clinical setting. However, studies on causality between factors affecting BVP, such as dosage, concentration, purification, patient underlying diseases and AEs are needed to more effectively prevent AEs. In particular, the dilution of BV to a certain concentration and before injection for therapeutic purposes differs from general bee stings. Thus, the causality between BVP and AEs requires continuous evaluation separate from previous studies on allergic reactions to hymenoptera venom.
A single-center, large-scale retrospective study and systematic review of the incidence of AEs related to BVP as well as AE conditions has been conducted. However, since most previous studies included patients with musculoskeletal disorders, neoplasms or autoimmune diseases, there is a lack of studies on patients with internal diseases such as cardiovascular and respiratory disorders, who are relatively vulnerable to bee stings and patients with various disorders [6,7,8].
Therefore, the present study investigated the incidence of post-BVP AEs (including severe AEs such as anaphylaxis) by retrospective chart review and clinical characteristics and risk factors of patients with various disorders who were admitted to Kyung Hee University Korean Medicine Hospital complaining of AEs.
2. Results
From 1 January 2013 to 1 May 2021, a total of 5505 patients were treated with BVP. Among them, 684 patients were excluded since their medical records did not clearly describe BVP, such as missing data on patient condition after the treatment in the hospitalization medical records. Thus, this study included a total of 4821 patients (Figure 1).
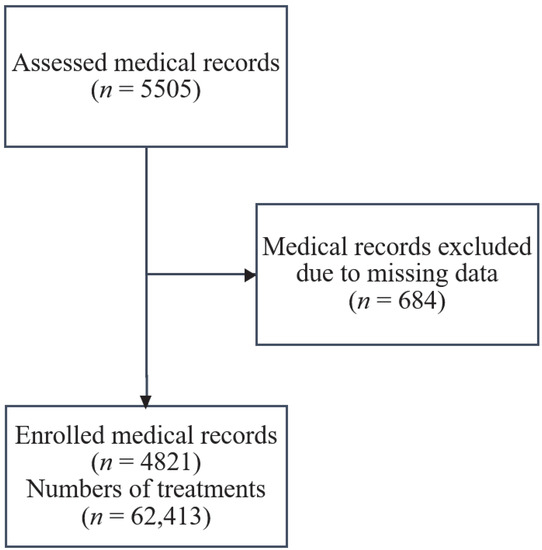
Figure 1.
Study flow diagram.
2.1. Characteristics of Patients Administered BVP
Of 4821 patients that received BVP, 2945 (61%) were women, while 1876 (39%) were men. The mean age was 54.62 ± 16.38 years. A total of 62,413 treatments were administered, with a mean of 11.18 ± 8.49 treatments per patient. Patients were classified as eleventh revision of the International Classification of Diseases (ICD-11) [9]. The most common chief symptom was related to diseases of the nervous system (8A00–8E7Z) reported in ≥50% of the patients, followed by symptoms related to diseases of the musculoskeletal system or connective tissue (FA00–FC0Z). Of the total number of BVP treatments performed (62,413), 97% (60,754) was delivered at a concentration of 1:30,000 (Table 1).

Table 1.
Demographic characteristics of the patients and specific details of bee venom pharmacopuncture (n = 4821, numbers of procedures = 62,413).
2.2. Incidence of AEs after BVP
A total of 112 patients (86 women and 26 men) complained of AEs after receiving a total of 324 procedures. The incidence rates were 2.32% of the total of 4821 patients and 0.51% of 62,413 treatments. Of the 112 patients, two complained of systemic edema and shortness of breath, respectively, which were classified as moderate adverse events (2 of 62,413 treatments). Thus, the incidence of moderate AEs was 0.04% of total patients and 0.003% of total treatments. Most AEs occurred when BVP was delivered at a concentration of 1:30,000. The patients complained of the following AEs: itching (92 patients), local redness (73 patients), local edema (28 patients), subcutaneous bleeding (6 patients), vesicle (2 patients), purulent discharge (2 patients), local pain (1 patient), rash (1 patient), chest discomfort (1 patient) and systemic edema (1 patient). All symptoms resolved in a range of 24 h (1 day) to 552 h (23 days) (Table 2). Detailed information about the patients who exhibited AEs is provided in Appendix A (Table A1).

Table 2.
Summary of the characteristics of the patients who experienced adverse events (n = 4821, number of treatments = 62,413).
2.3. Comparisons of the Characteristics between Patients with and without Post-BVP AEs
The proportion of male patients in the group with AEs was significantly lower than that in the group without AEs (23.21% vs. 39.3%, p < 0.001). The mean age of patients with AEs was 58.20 ± 16.10 years, which was significantly higher than that of patients without AEs (54.53 ± 16.38 years). Regarding disease types, the proportion of AEs was relatively high in diseases of the ear or mastoid process (11.1%) and diseases of the musculoskeletal system (6.47%) (Table 3).

Table 3.
Comparison of the characteristics of patients with and without adverse events after bee venom pharmacopuncture.
2.4. Characteristics of Patients Who Complained of Moderate AEs
Both patients who showed moderate AEs were women in their 50s or older. Both patients complained of AEs after receiving one BVP treatment. Patient 1 reported chest discomfort and itching, while Patient 2 reported systemic edema and itching. However, they did not experience life-threatening symptoms and the related symptoms completely disappeared within 24 h without particular treatment. Neither patient complained of resultant sequelae. A review of their medical records to investigate their prior medical history, treatment site, BVP concentration and hematology tests performed at the time of initial hospitalization, showed no common factors other than the treatment concentration used (Table 4).

Table 4.
Characteristics of patients with grade 2 adverse events.
3. Discussion
In traditional East Asian medicine, BVP is used for the treatment of various diseases. Studies on the incidence of AEs and relevant factors are continuously published to prevent and identify AEs that can occur when performing BVP [6,7,8,10].
The present study investigated the incidence of AEs in patients treated with BVP while hospitalized at Kyung Hee University Korean Medicine Hospital between 1 January 2013 and 1 May 2021. Among 4821 total patients, 112 patients reported 324 AEs. This accounts for 2.32% of the total number of patients and 0.51% of the total number of treatments administered (62,413). Of the 112 patients, two patients reported one moderate AE, respectively. Of them, Patient 1 complained of chest discomfort, while Patient 2 complained of systemic edema. However, none of the 112 patients showed anaphylactic shock. Patients fully recovered from AEs within a minimum of 24 h (1 day) or a maximum of 552 h (23 days), without other sequelae. Given these results, BVP can be considered a relatively safe treatment.
There was no occurrence of anaphylaxis in this study, which is lower than the result of previous study. Ko et al., reported that incidence rate of anaphylaxis was 0.045% in a systematic review [5]. However, the incidence of overall AEs in this study was higher than that reported by other retrospective studies investigating post–BVP AEs (0.025% by Lee et al. [8] and 0.23% by Kim et al. [7]). This difference is assumed to result from the proportion of women (≥60%), a higher mean number of procedures in the present study compared to other studies and differences between investigators in determining causality between the drug and AEs due to the limitation of the retrospective study design.
In general, drug adverse reactions (ADRs) are affected by sex, age, underlying disease, concomitant medication and the dose and frequency of drug administration [11,12]. In terms of sex, women are reportedly relatively more vulnerable to ADRs compared to men [13,14]. In the present study, the proportion of women in the group that reported AEs was significantly higher than that in the group that did not report AEs (p < 0.001). Other studies reported high proportions of AEs in female patients [8], while others reported similar proportions between men and women [7] or only a 9% higher proportion of women [8]. In contrast, in the present study, the proportion of women was very high, at 60% or higher.
The patients in the present study also received more BVP treatments compared to the numbers reported in similar studies. Dose and frequency have been reported to affect the development of ADRs [11]. Lee et al. [8] reported a 0.025% incidence of AEs and a mean of seven treatments. In contrast, the patients in the present study received an average of 11.18 ± 8.49 treatments. The increased exposures to BV likely affected the incidence of AEs.
In addition, domestic and overseas studies conducted on AEs of BVP reported incidence rates of AEs ranging from 0% to 90.63%, although similar criteria to those in this study were used to determine the causality between the drug and AEs [15]. The discordant results might stem from BVP performed by various doctors according to site, different investigators, or differences in the determination of causality due to the limitations of the retrospective study design.
Comparison of the patient groups with and without AEs showed a significantly higher proportion of women in the group with AEs (p < 0.001). The mean age was also significantly higher (p = 0.030) than that in the group without AEs. Thus, women and aged people may be more vulnerable to the development of AEs following BVP therapy. As mentioned above, these results are assumed to reflect the fact that women are more vulnerable to ADRs compared to men and pharmacokinetic changes in the body with age increased the risk of ADR development [16].
The incidence of AEs by treated disease was higher in diseases of the ear and mastoid process and diseases of the musculoskeletal system and connective tissue compared to those of other diseases. BVP therapy for diseases of the musculoskeletal system and connective tissue is likely to be performed mostly on one site unlike procedures performed for other diseases (for example, therapy is intensively performed on the lower back for patients with lumbar pain) [17,18]. These treatment patterns likely increase the incidence of AEs. However, regarding diseases of the ear and mastoid, it is difficult to discuss the clinical significance of these findings since few patients in this study received BVP for this condition.
The present study has some strengths. First, unlike previous studies, the present study assessed the safety of BVP in patients with chief complaints of various diseases [6,7,8]. As mentioned above, underlying diseases affect the development of ADRs [11,12]; however, previous studies on AEs from BVP included patients mainly presenting with chief complaints of diseases of the musculoskeletal system, injury, poisoning and certain other consequences of external causes for investigation, neoplasm or autoimmune system [6,7,8]. Meanwhile, the present study evaluated the safety related to BVP in patients hospitalized with chief complaints of diseases of the nervous or internal disease like endocrine, respiratory or circulatory systems, which no previous study has evaluated. The results of this study showed that the incidence of AEs was not significantly high in these patient groups.
Second, the results of the comparisons of the characteristics of the group of patients with and without AEs resulting from BVP confirmed that AEs resulting from BVP were affected by patient sex and age (women) similarly to AEs of other drugs. Furthermore, the incidence of AEs tended to be high in diseases of the musculoskeletal system, where BVP was intensively performed on one area, thus providing a useful clue for the application of BVP in clinical settings.
Lastly, the present study comprehensively investigated the characteristics of patients requiring BVP therapy, the number of treatments and the treatment concentrations in Korea to provide the beginning of the provision for guidelines for the administration of BVP.
However, the present study has some limitations. First, since most patients included in this study were older, patients of all ages (between their 20s and 50s) were not included. Moreover, most of the patients were female, which likely biased the results. Second, although the incidence of AEs by disease was compared, the analysis was conducted only using general disease classification according to the ICD-11 [9], instead of each disease. The number of patients for each group was not consistent and group sizes varied. These differences affected the accuracy of the results. Third, since the number of patients with moderate AEs was lower than those with mild AEs, the comparisons were not significant. It was difficult to find common ground between the patients in the group with moderate or greater AEs. Finally, the comparison of the incidence of AEs by BVP concentration was not significant because most patients were administered BVP at 1:30,000.
The results of this study demonstrated that BVP can be safely used for patients with various underlying diseases, including internal medicine and those of the nervous system, s well as aged patients. Although two patients showed moderate to greater AEs, these AEs were not life-threatening and the symptoms improved within 24 h without special measures and no sequelae. Thus, BVP therapy is relatively safe. However, since cases of moderate to greater AEs have been reported after multiple exposures to BVP [19], continuous monitoring is required if repeated BVP is needed.
4. Materials and Methods
This study was conducted after receiving approval from the Institutional Review Board of Kyung Hee University Korean Medicine Hospital (KOMCIRB 2021–10–011). The study protocol was registered in the Clinical Research Information Service (CRIS) (KCT0006942).
4.1. Subjects
4.1.1. Inclusion Criteria
The medical records of patients who met the following criteria were included in the analysis.
- (1)
- Patients aged ≥18 years hospitalized at Kyung Hee University Korean Medicine Hospital and who received at least 1 BVP treatment between 1 January 2013 and 1 May 2021;
- (2)
- Patients with available medical records for identifying underlying diseases, demographic and clinical characteristics, BVP site and concentration and AEs occurring during the procedure.
4.1.2. Exclusion Criteria
The medical records of patients who met the following criteria were excluded from the study.
If post-BVP AEs could not be identified because BVP site and concentration were not documented in the medical records during hospitalization.
4.2. Study Design
This retrospective medical record review study included data from the medical records of patients who received BVP therapy regardless of concentration and who met the above inclusion criteria. Information was collected from progress notes provided by the doctor of each patient, admission and discharge records, nursing progress notes and clinical observation notes.
4.3. Bee Venom
The BV used for treatment was produced by the Korea Bee Venom Agriculture Corporation (Changnyeong, South Gyeongsang Province, Korea). Component analysis showed that melittin constituted 60% of the BV. Dried BV power was diluted in normal saline to concentrations of 1:1000–1:70,000. The diluted solution was injected intramuscularly or subcutaneously into an acupoint according to the disease at a minimum of one day apart or as needed.
4.4. Observation and Evaluation
Information about the following items was collected and evaluated by reviewing patient medical records.
4.4.1. Characteristics of the Patients Administered BVP Therapy
Demographic characteristics and chief complaint (CC).
Patient medical records were reviewed to obtain data on demographic characteristics, such as sex, age and CC.
4.4.2. BVP Concentrations
Patient medical records were reviewed to identify the concentrations administered for the treatments (1:1000–1: 70,000).
4.4.3. Sites of BVP Therapy
Patient medical records were reviewed to determine the sites of BVP therapy: head (cephalus), face, neck, shoulders, waist, both upper extremities, both lower extremities, all extremities, left upper extremity, left lower extremity, right upper extremity and right lower extremity. In cases in which only the knees were involved, each was divided into left, right, or both knees.
4.5. Evaluation of Post-BVP AEs
4.5.1. AE Incidence and Causality
After identifying the incidence of post-BVP AEs via patient medical records, the total number of patients who exhibited AEs and the number of treatments performed compared to the incidence of AEs were identified. Causality between BVP and AEs was evaluated using the World Health Organization-Uppsala Monitoring Centre (WHO-UMC) causality scale [20]. If the causality between BVP and an AE was “possible” or higher, the AE was considered to be caused by BVP.
4.5.2. Evaluation of AE Severity
Patient medical records were reviewed to determine the AE severity. The severity was assessed using the three-category grading system described by Brown et al., in 2004 to evaluate anaphylaxis. The severity was categorized as mild, moderate, or severe depending on the changes in vital signs and onset site of AEs, as confirmed by hospitalization medical records [21]. The criteria for the three grades are described below.
- -
- Mild: After BVP, an immediate or delayed reaction appearing at sites other than the treatment site, with symptoms confined to the skin and subcutaneous tissue
- -
- Moderate: Symptoms related to the respiratory, cardiovascular, or digestive systems in addition to symptoms confined to the skin and subcutaneous tissue
- -
- Severe: In addition to mild-moderate symptoms, confirmed changes in vital signs (i.e., hypoxia or hypotension) or neurological changes. Arterial oxygen saturation ≤ 92%, systolic blood pressure ≤ 90 mmHg, confusion, collapse, loss of consciousness, or incontinence.
4.5.3. AE Onset Time
Patient medical records were reviewed to identify the number of treatments performed in patients who exhibited AEs from the time of the first treatment to AE onset. The unit was set to ‘number.’
4.5.4. Time to Remission
Patient medical records were reviewed to identify the time elapsed from when patients who exhibited AEs first complained of AEs to when the symptoms completely disappeared, in hours.
4.6. Characteristics of Subjects with Moderate or Greater AEs
4.6.1. Demographic Characteristics
Patient medical records were reviewed to identify demographic characteristics such as sex and age, in patients with moderate or greater AEs.
4.6.2. Clinical Characteristics
Patient medical records were reviewed to identify clinical characteristics, such as moderate or greater underlying diseases in patients with moderate or greater AEs.
4.7. Statistical Analysis
IBM SPSS for Windows, version 25.0 (IBM Corp., Armonk, New York, NY, USA) was used to analyze the collected data. The statistical methods were as follows. Percentages were determined to verify the incidence of AEs. Means and standard deviation (SD) were used to assess patient sex and age, number of treatments, treatment site, AE onset time and number of complaints about AEs. Kolmogorov–Smirnov tests were used to test the normality of age of patient groups. Regarding age, chi-square tests were performed to compare and assess the significance of the differences in the number of treatments performed, age, or sex between each group. p < 0.05 was considered statistically significant.
Author Contributions
Conceptualization, I.-H.B. and S.K.; methodology, S.K. and W.-S.J.; validation, I.-H.B. and S.K.; formal analysis, I.-H.B., S.K., H.-G.L. and W.-S.J.; investigation, I.-H.B., S.K., H.-G.L. and W.-S.J.; data curation, I.-H.B. and S.K.; writing—original draft preparation, I.-H.B., S.K. and W.-S.J.; writing—review and editing, I.-H.B., W.-S.J., S.K., H.-G.L., S.-Y.C., S.-U.P., S.-K.M., J.-M.P., C.-N.K. and K.-H.C.; supervision, S.K.; project administration, W.-S.J. and S.K.; funding acquisition, W.-S.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HF20C0113).
Institutional Review Board Statement
This study was conducted after receiving approval from the Institutional Review Board of Kyung Hee University Korean Medicine Hospital (Code: KOMCIRB 2021–10–011; Approved date: 15 November 2021).
Informed Consent Statement
Patient consent was waived due to the design of study, a retrospective chart review study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to protection of personal information.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A

Table A1.
Characteristics of the 112 patients who experienced adverse events associated with bee venom pharamacopuncture.
Table A1.
Characteristics of the 112 patients who experienced adverse events associated with bee venom pharamacopuncture.
| Case (Age/Sex) | Chief Complaints (KCD–6) | Allergic Disorders | Number of Treatments * | Adverse Events | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Main Symptoms | Grade † | Outcome | Resolution Time (Hours) ‡ | Concentration § | ||||||
| P1 | 95 | F | Gonarthrosis (knee) | None | 1 | Itching, chest discomfort | 2 | Recovered | 24 | 1:30,000 |
| P2 | 51 | F | Bell’s palsy | None | 1 | Itching, systemic edema | 2 | Recovered | 24 | 1:30,000 |
| P3 | 83 | F | Facial nerve disorders | None | 2 | Redness, local edema | 1 | Recovered | 24 | 1:3000 |
| P4 | 65 | M | Fracture of lumbar vertebra | None | 3 | Itching, rash | 1 | Recovered | 24 | 1:30,000 |
| P5 | 52 | F | Lumbar herniated nucleus pulposus | None | 8 | Subcutaneous bleeding. Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P6 | 66 | F | Facial nerve disorders | None | 6 | Subcutaneous bleeding. Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P7 | 55 | F | Secondary coxarthrosis | None | 3 | Itching, redness, local edema | 1 | Recovered | 24 | 1:30,000 |
| P8 | 68 | F | Fracture of lumbar vertebra | None | 6 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P9 | 47 | F | Fibromyalgia | Asthma | 7 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P10 | 26 | F | Sprain and strain of the lumbar spine | None | 3 | Redness, vesicle | 1 | Recovered | 48 | 1:30,000 |
| P11 | 80 | F | Lumbar stenosis | None | 5 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P12 | 77 | M | Parkinson’s disease | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P13 | 50 | F | Myalgia | None | 12 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P14 | 72 | F | dermatomyositis | None | 5 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P15 | 59 | F | Facial nerve disorders | None | 22 | Itching, redness. Local edema, purulent discharge | 1 | Recovered | 24 | 1:30,000 |
| P16 | 59 | M | Cervical disc disorder with radiculopathy | None | 1 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:20,000 |
| P17 | 86 | M | Cerebral infarction | None | 8 | Subcutaneous bleeding, itching, redness | 1 | Recovered | 24 | 1:20,000 |
| P18 | 56 | F | Malignant neoplasm of ovary | None | 1 | Itching, redness local edema | 1 | Recovered | 24 | 1:30,000 |
| P19 | 88 | F | Tremor | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P20 | 46 | M | Lumbar herniated nucleus pulposus | None | 2 | Subcutaneous bleeding, itching | 1 | Recovered | 24 | 1:30,000 |
| P21 | 74 | F | Gonarthrosis | None | 6 | Itching, Redness | 1 | Recovered | 312 | 1:30,000 |
| P22 | 43 | F | Meniscus derangements | None | 6 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P23 | 53 | F | Rheumatoid arthritis | None | 2 | Itching, redness | 1 | Recovered | 96 | 1:30,000 |
| P24 | 64 | M | Intracerebral hemorrhage | None | 7 | Local edema | 1 | Recovered | 24 | 1:20,000 |
| P25 | 71 | F | Parkinson’s Disease | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P26 | 53 | F | Shoulder lesions | None | 4 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P27 | 78 | F | Sprain and strain of the cervical spine | None | 6 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P28 | 67 | F | Parkinson’s disease | None | 7 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P29 | 43 | M | Intracerebral hemorrhage | None | 5 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P30 | 37 | M | Myalgia | None | 5 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P31 | 80 | F | Spondylosis with myelopathy | None | 5 | Redness | 1 | Recovered | 72 | 1:30,000 |
| P32 | 51 | F | Polyarthritis | None | 12 | Local edema | 1 | Recovered | 24 | 1:30,000 |
| P33 | 50 | F | Lumbar herniated nucleus pulposus | None | 9 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P34 | 42 | M | Lumbar herniated nucleus pulposus | None | 1 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P35 | 33 | F | Cervical disc disorder with radiculopathy | None | 7 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P36 | 79 | M | Parkinson’s disease | None | 1 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:20,000 |
| P37 | 63 | F | Lumbar herniated nucleus pulposus | None | 7 | Itching, local edema | 1 | Recovered | 432 | 1:30,000 |
| P38 | 58 | F | Bell’s palsy | None | 8 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P39 | 72 | F | Lumbar herniated nucleus pulposus | None | 4 | Itching, redness | 1 | Recovered | 72 | 1:30,000 |
| P40 | 52 | F | Polyarthritis | None | 9 | Itching, redness. Local edema | 1 | Recovered | 96 | 1:30,000 |
| P41 | 51 | F | Submucous leiomyoma of uterus | None | 1 | Itching, redness | 1 | Recovered | 120 | 1:30,000 |
| P42 | 60 | F | Ménière’s Disease | None | 5 | Itching, redness | 1 | Recovered | 552 | 1:30,000 |
| P43 | 75 | F | Parkinson’s Disease | None | 1 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P44 | 54 | F | Lumbar herniated nucleus pulposus | None | 11 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P45 | 62 | F | Polyneuropathy | None | 1 | Itching, redness | 1 | Recovered | 408 | 1:30,000 |
| P46 | 49 | F | Menopausal and female climacteric states | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P47 | 71 | F | Lumbar herniated nucleus pulposus | None | 3 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P48 | 63 | F | Lumbar herniated nucleus pulposus | None | 1 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P49 | 70 | F | Ankle contusion | None | 6 | Itching, redness | 1 | Recovered | 312 | 1:30,000 |
| P50 | 46 | M | Lumbar herniated nucleus pulposus | None | 7 | Itching, redness | 1 | Recovered | 120 | 1:30,000 |
| P51 | 77 | F | Bell’s palsy | None | 15 | Redness | 1 | Recovered | 48 | 1:30,000 |
| P52 | 57 | F | Sicca syndrome | None | 1 | Itching, redness | 1 | Recovered | 192 | 1:30,000 |
| P53 | 36 | M | Guillain-Barré Syndrome | None | 7 | Local edema | 1 | Recovered | 168 | 1:30,000 |
| P54 | 18 | F | Lumbar herniated nucleus pulposus | Allergic rhinitis | 1 | Redness, local edema | 1 | Recovered | 96 | 1:30,000 |
| P55 | 26 | M | Lumbar herniated nucleus pulposus | None | 9 | Itching, redness | 1 | Recovered | 96 | 1:30,000 |
| P56 | 39 | M | Lumbar Herniated Nucleus Pulposus | Allergic rhinitis | 4 | Itching, redness | 1 | Recovered | 168 | 1:30,000 |
| P57 | 76 | M | Gonarthrosis | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P58 | 28 | M | Bell’s palsy | None | 10 | Itching, redness | 1 | Recovered | 72 | 1:30,000 |
| P59 | 61 | F | Bell’s palsy | None | 1 | Redness | 1 | Recovered | 24 | 1:30,000 |
| P60 | 41 | M | Sprain and strain of the lumbar spine | None | 1 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P61 | 74 | F | Lumbar stenosis | None | 6 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P62 | 62 | F | Fracture of thoracic vertebra | None | 12 | Redness | 1 | Recovered | 24 | 1:30,000 |
| P63 | 71 | F | Bell’s palsy | None | 1 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P64 | 18 | M | Lumbar Herniated Nucleus Pulposus | None | 22 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P65 | 30 | M | Bell’s palsy | None | 1 | Local edema | 1 | Recovered | 24 | 1:30,000 |
| P66 | 64 | F | Rheumatoid arthritis | None | 9 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P67 | 66 | F | Cervical disc disorder with radiculopathy | None | 13 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P68 | 40 | F | Leiomyoma of Uterus | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P69 | 55 | F | Lumbar Herniated Nucleus Pulposus | Asthma | 1 | Itching | 1 | Recovered | 192 | 1:30,000 |
| P70 | 34 | M | Raynaud’s Syndrome | None | 10 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P71 | 61 | F | Parkinson’s Disease | None | 4 | Itching, redness | 1 | Recovered | 96 | 1:30,000 |
| P72 | 74 | F | Lumbar stenosis | None | 9 | Itching, redness | 1 | Recovered | 24 | 1:20,000 |
| P73 | 62 | F | Lumbar stenosis | None | 7 | Redness | 1 | Recovered | 48 | 1:30,000 |
| P74 | 84 | F | Pain in joint, ankle and foot | None | 24 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P75 | 79 | F | Cerebral infarction | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P76 | 60 | F | Fracture of the thoracic vertebra | None | 3 | Itching | 1 | Recovered | 48 | 1:10,000 |
| P77 | 62 | F | Cerebral infarction | None | 7 | Redness | 1 | Recovered | 24 | 1:30,000 |
| P78 | 22 | F | Multiple fractures of the thoracic spine | None | 1 | Redness | 1 | Recovered | 24 | 1:20,000 |
| P79 | 57 | F | Palmar fascial fibromatosis (Dupuytren) | None | 5 | Itching | 1 | Recovered | 48 | 1:30,000 |
| P80 | 34 | F | Malignant neoplasm of bone and articular cartilage | None | 3 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P81 | 62 | F | Lumbar herniated nucleus pulposus | None | 8 | Itching | 1 | Recovered | 240 | 1:30,000 |
| P82 | 52 | F | Rotator cuff syndrome | None | 8 | Local pain | 1 | Recovered | 24 | 1:30,000 |
| P83 | 47 | F | Sprain and strain of the cervical spine | None | 2 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P84 | 56 | F | Fracture of thoracic vertebra | None | 2 | Itching, redness | 1 | Recovered | 120 | 1:30,000 |
| P85 | 71 | F | Bell’s palsy | None | 1 | Redness, local edema | 1 | Recovered | 24 | 1:30,000 |
| P86 | 54 | F | Fibromyalgia | None | 1 | Redness | 1 | Recovered | 24 | 1:30,000 |
| P87 | 53 | F | Bell’s palsy | None | 14 | Itching Redness | 1 | Recovered | 24 | 1:30,000 |
| P88 | 42 | M | Lumbar herniated nucleus pulposus | None | 3 | Itching | 1 | Recovered | 48 | 1:30,000 |
| P89 | 62 | F | Bell’s palsy | None | 16 | Itching, vesicle | 1 | Recovered | 24 | 1:30,000 |
| P90 | 56 | M | Cerebral infarction | None | 9 | Redness | 1 | Recovered | 48 | 1:30,000 |
| P91 | 69 | F | Lumbar herniated nucleus pulposus | None | 5 | Itching | 1 | Recovered | 240 | 1:30,000 |
| P92 | 79 | F | Parkinson’s Disease | None | 3 | Itching, local edema | 1 | Recovered | 24 | 1:30,000 |
| P93 | 90 | F | Cerebral infarction | None | 1 | Itching | 1 | Recovered | 72 | 1:30,000 |
| P94 | 47 | F | Sprain and strain of the lumbar spine | None | 1 | Subcutaneous bleeding, local edema, purulent discharge | 1 | Recovered | 24 | 1:30,000 |
| P95 | 75 | F | Cerebral infarction | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P96 | 49 | F | Nerve root and plexus compressions | None | 8 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P97 | 74 | M | Spinal stenosis | None | 1 | Itching, Rednessm Local edema | 1 | Recovered | 24 | 1:30,000 |
| P98 | 57 | F | Spinal stenosis | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P99 | 50 | F | Sprain and strain of cervical spine | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P100 | 53 | F | Bell’s palsy | None | 1 | Itching, redness | 1 | Recovered | 48 | 1:30,000 |
| P101 | 68 | F | Cerebral infarction | None | 1 | Itching | 1 | Recovered | 48 | 1:30,000 |
| P102 | 70 | F | Lumbar herniated nucleus pulposus | None | 1 | Itching, redness | 1 | Recovered | 24 | 1:30,000 |
| P103 | 60 | M | Polyneuropathy | None | 2 | Itching, local edema | 1 | Recovered | 48 | 1:30,000 |
| P104 | 50 | F | Lumbar herniated nucleus pulposus | None | 1 | Itching, redness. Local edema | 1 | Recovered | 24 | 1:30,000 |
| P105 | 77 | F | Spinal stenosis | None | 7 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P106 | 52 | M | Superficial injury of wrist and hand | None | 1 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P107 | 49 | F | Migraine | None | 1 | Itching, redness. Local edema | 1 | Recovered | 72 | 1:30,000 |
| P108 | 44 | M | Lumbar herniated nucleus pulposus | None | 3 | Itching | 1 | Recovered | 24 | 1:30,000 |
| P109 | 51 | F | Parkinson’s Disease | None | 3 | Itching | 1 | Recovered | 96 | 1:30,000 |
| P110 | 65 | F | Bronchiectasis | None | 3 | Itching, local edema | 1 | Recovered | 48 | 1:30,000 |
| P111 | 80 | F | Bell’s palsy | None | 1 | Redness, local edema | 1 | Recovered | 24 | 1:30,000 |
| P112 | 41 | F | Lumbar herniated nucleus pulposus | None | 2 | Subcutaneous bleeding, itching | 1 | Recovered | 96 | 1:30,000 |
* Number of bee venom pharmacopuncture treatments before symptom onset. † Assessed with Brown’s grade. ‡ Time elapsed (hours) before the symptom completely disappeared. § Concentration of bee venom used for pharmacopuncture.
References
- Lee, J.D. Bee-venom therapy: Method of clinical approach. J. Korean Orient. Med. 2000, 21, 3–8. [Google Scholar]
- Sung, S.-H.; Lee, G. Bee Venom Acupuncture Effects on Pain and Its Mechanisms: An Updated Review. Toxins 2021, 13, 608. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Kim, K.H. Clinical Effectiveness and Adverse Events of Bee Venom Therapy: A Systematic Review of Randomized Controlled Trials. Toxins 2020, 12, 558. [Google Scholar] [CrossRef] [PubMed]
- Sin, M.S. The comparative study of bee venom and BV partner on D.I.T.I. J. Acupunct. Res. 2003, 20, 17–33. [Google Scholar]
- Ko, S.-H.; Oh, H.-M.; Kwon, D.-Y.; Yang, J.-E.; Kim, B.-J.; Ha, H.-J.; Lim, E.-J.; Oh, M.-S.; Son, C.-G.; Lee, E.-J. Incidence Rate of Bee Venom Acupuncture Related Anaphylaxis: A Systematic Review. Toxins 2022, 14, 238. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.; Lee, G. Adverse Events Associated with the Clinical Use of Bee Venom: A Review. Toxins 2022, 14, 562. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.R.; Shin, J.S.; Lee, J.H.; Lee, Y.J.; Ahn, Y.J.; Park, K.B.; Lee, H.D.; Lee, Y.M.; Kim, S.G.; Ha, I.H. Safety of acupuncture and pharmacopuncture in 80,523 musculoskeletal disorder patients. Medicine 2016, 95, e3635. [Google Scholar] [CrossRef]
- Lee, E.J.; Ahn, Y.C.; Kim, Y.I.; Oh, M.S.; Park, Y.C.; Son, C.G. Incidence rate of hypersensitivity reactions to bee-venom acupuncture. Front. Pharmacol. 2020, 11, 1575. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Diseases 11th Revision. Available online: https://icd.who.int/browse11/l-m/en (accessed on 2 September 2022).
- Kim, K.; Jeong, H.; Lee, G.; Jang, S.; Yook, T. Characteristics of Adverse Events in Bee Venom Therapy Reported in South Korea: A Survey Study. Toxins 2022, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Alomar, M.J. Factors affecting the development of adverse drug reactions: Review article. Saudi Pharm. J. 2014, 22, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Lavan, A.H.; Gallagher, P. Predicting risk of adverse drug reactions in older adults. Ther. Adv. Drug Saf. 2016, 7, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Rademaker, M. Do women have more adverse drug reactions? Am. J. Clin. Dermatol. 2001, 2, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Zucker, I.; Prendergast, B.J. Sex differences in pharmacokinetics predict adverse drug reactions in women. Biol. Sex Differ. 2020, 11, 32. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Yim, B.K.; Lee, J.H.; Lee, S.H.; Kim, T.H. Risk associated with bee venom therapy: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0126971. [Google Scholar] [CrossRef] [PubMed]
- Brahma, D.K.; Wahlang, J.B.; Marak, M.D.; Sangma, M.C. Adverse drug reactions in the elderly. J. Pharmacol. Pharmacother. 2013, 4, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Pittler, M.H.; Shin, B.C.; Kong, J.C.; Ernst, E. Bee venom acupuncture for musculoskeletal pain: A review. J. Pain 2008, 9, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.D.; Park, H.J.; Chae, Y.B.; Lim, S.B.N. An overview of bee venom acupuncture in the treatment of arthritis. Evid. Based Complement Altern. Med. 2005, 2, 397319. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H. The case report of anaphylaxis after treated with bee-venom acupuncture. J. Korean Med. Rehabil. 2015, 25, 175–182. [Google Scholar] [CrossRef]
- WHO. The Use of the WHO-UMC System for Standardized Case Causality Assessment. Available online: https://who-umc.org/media/164200/who-umc-causality-assessment_new-logo.pdf (accessed on 12 August 2022).
- Brown, S.G. Clinical features and severity grading of anaphylaxis. J. Allergy Clin. Immunol. 2004, 114, 371. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).