Application of Braided Piezoelectric Poly-l-Lactic Acid Cord Sensor to Sleep Bruxism Detection System with Less Physical or Mental Stress
Abstract
:1. Introduction
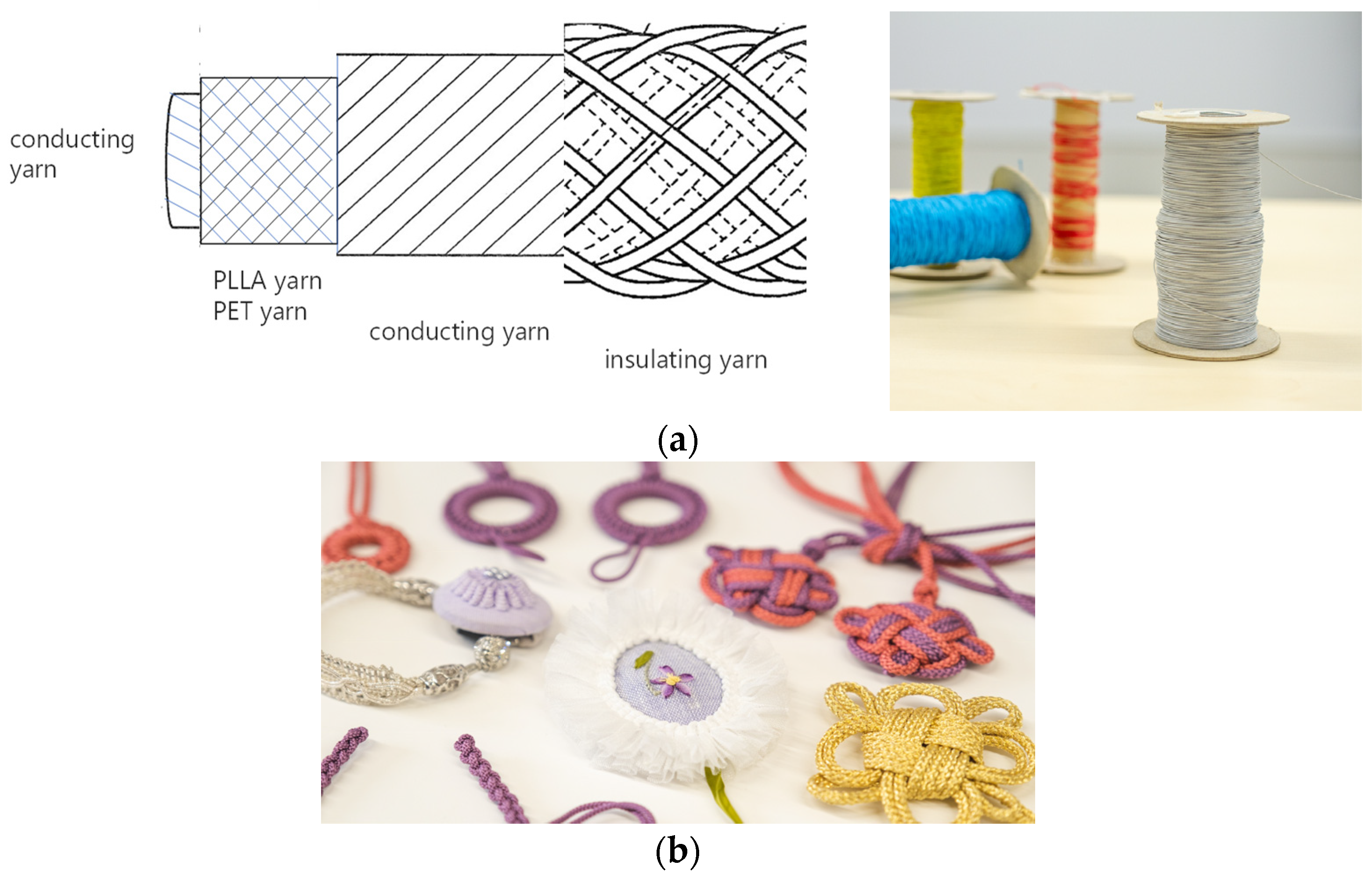
2. Difficulty in Measuring Bruxism
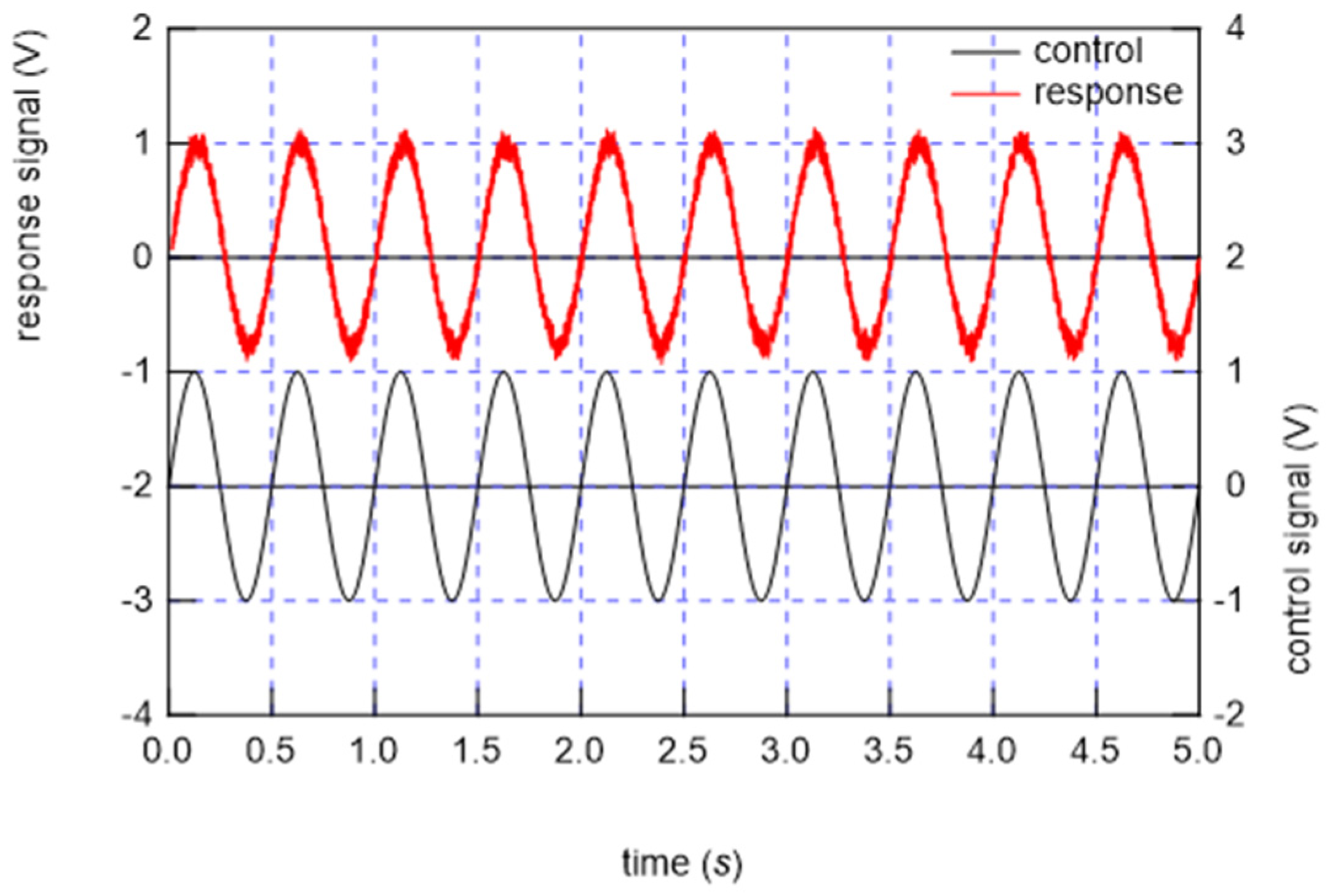
3. Braided Piezoelectric PLLA Cord Sensor
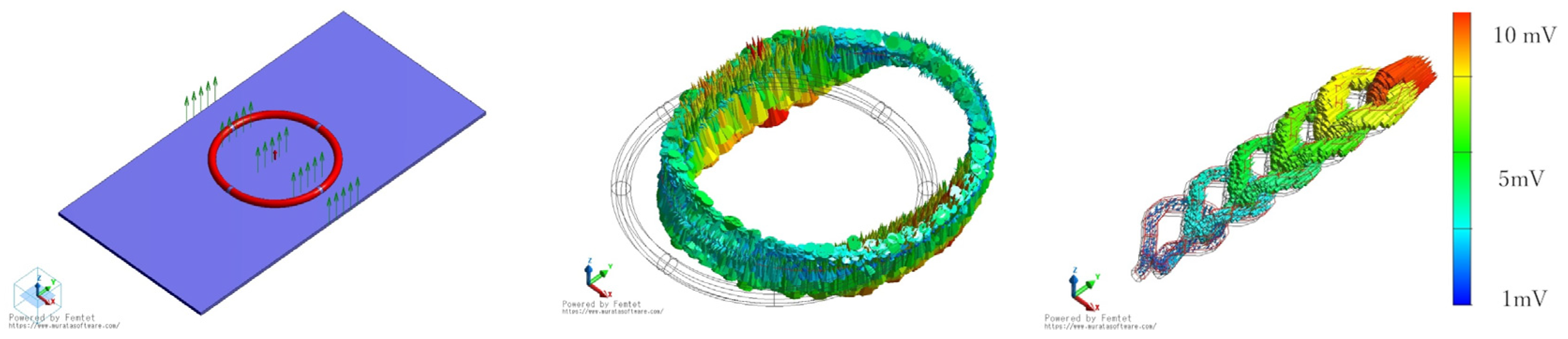
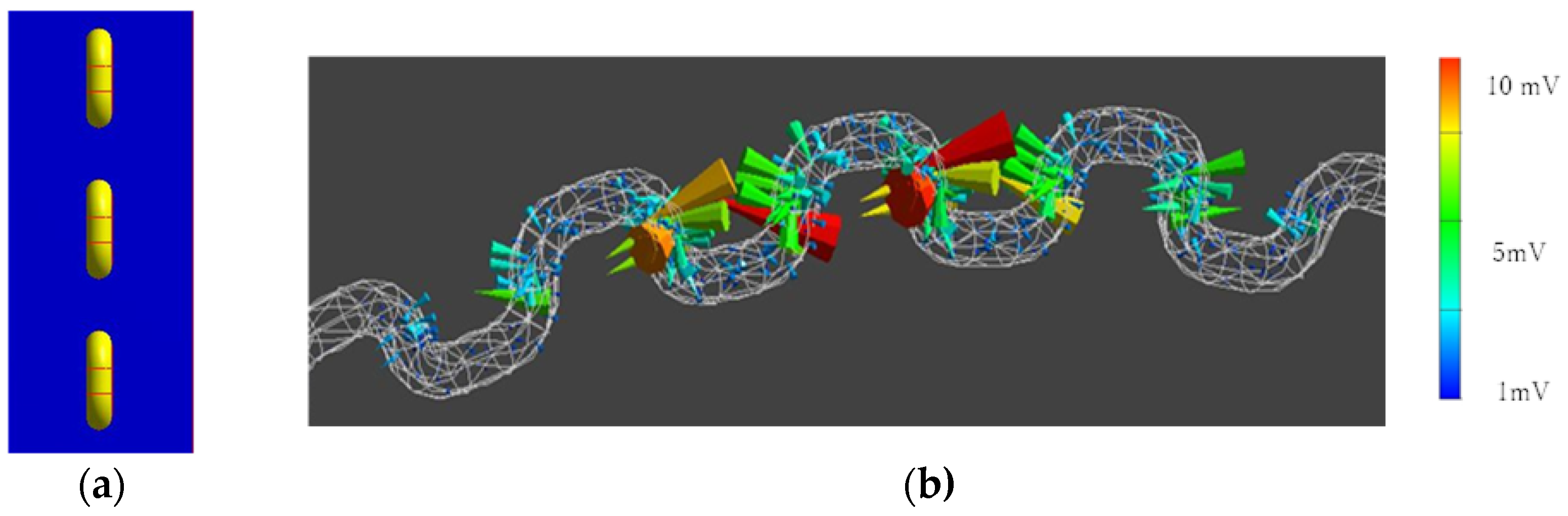
3.1. FEM
3.2. Bed-Sheet Sensor Blueprint
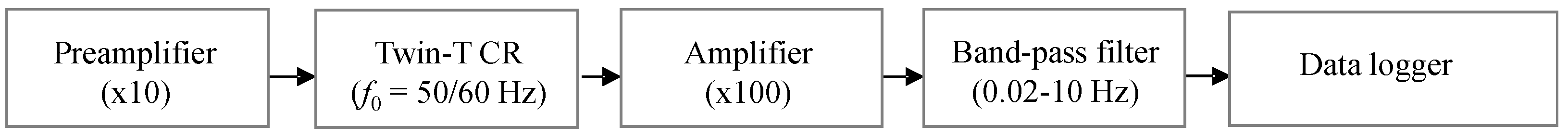
4. Bed-Sheet Sensor
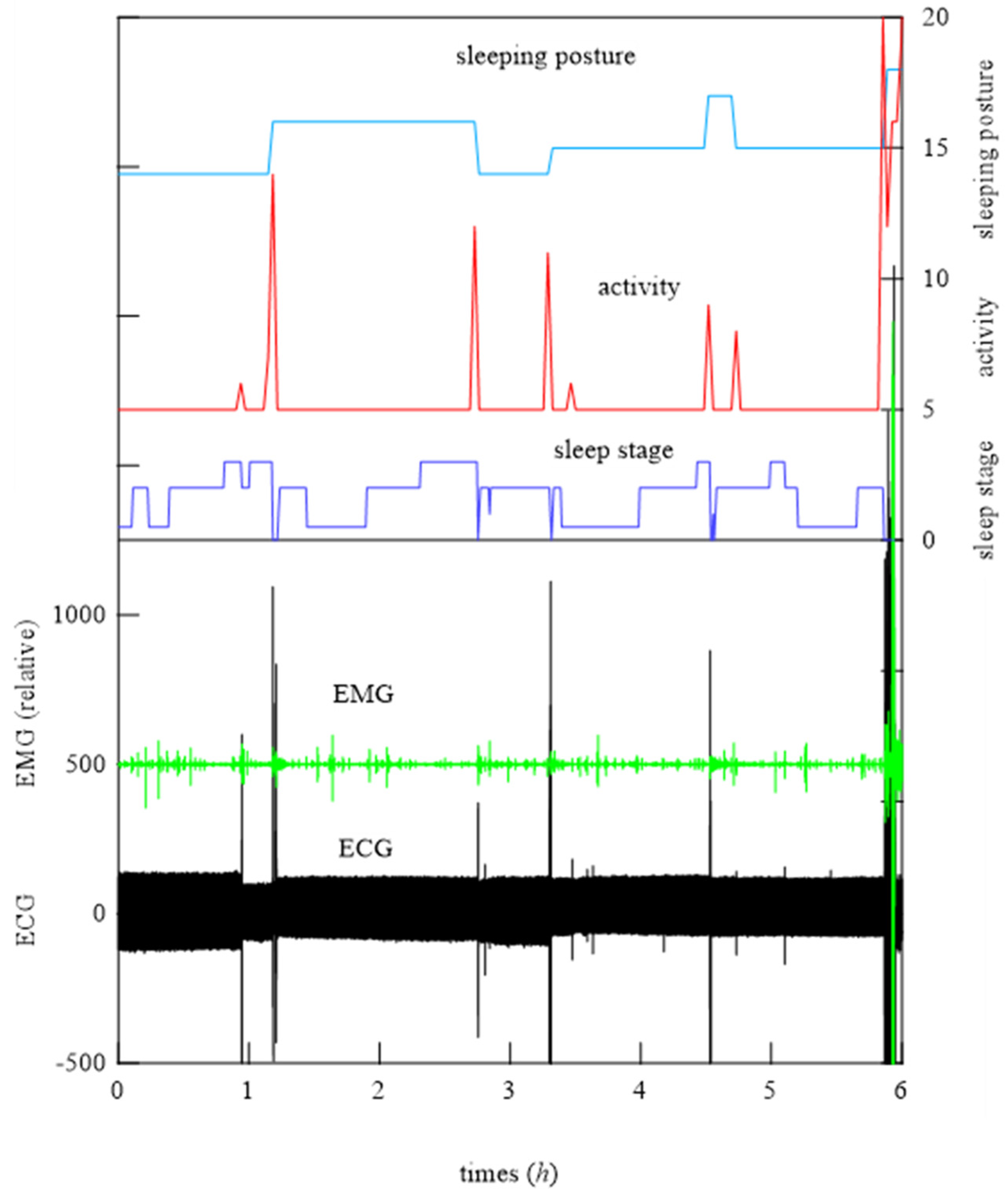
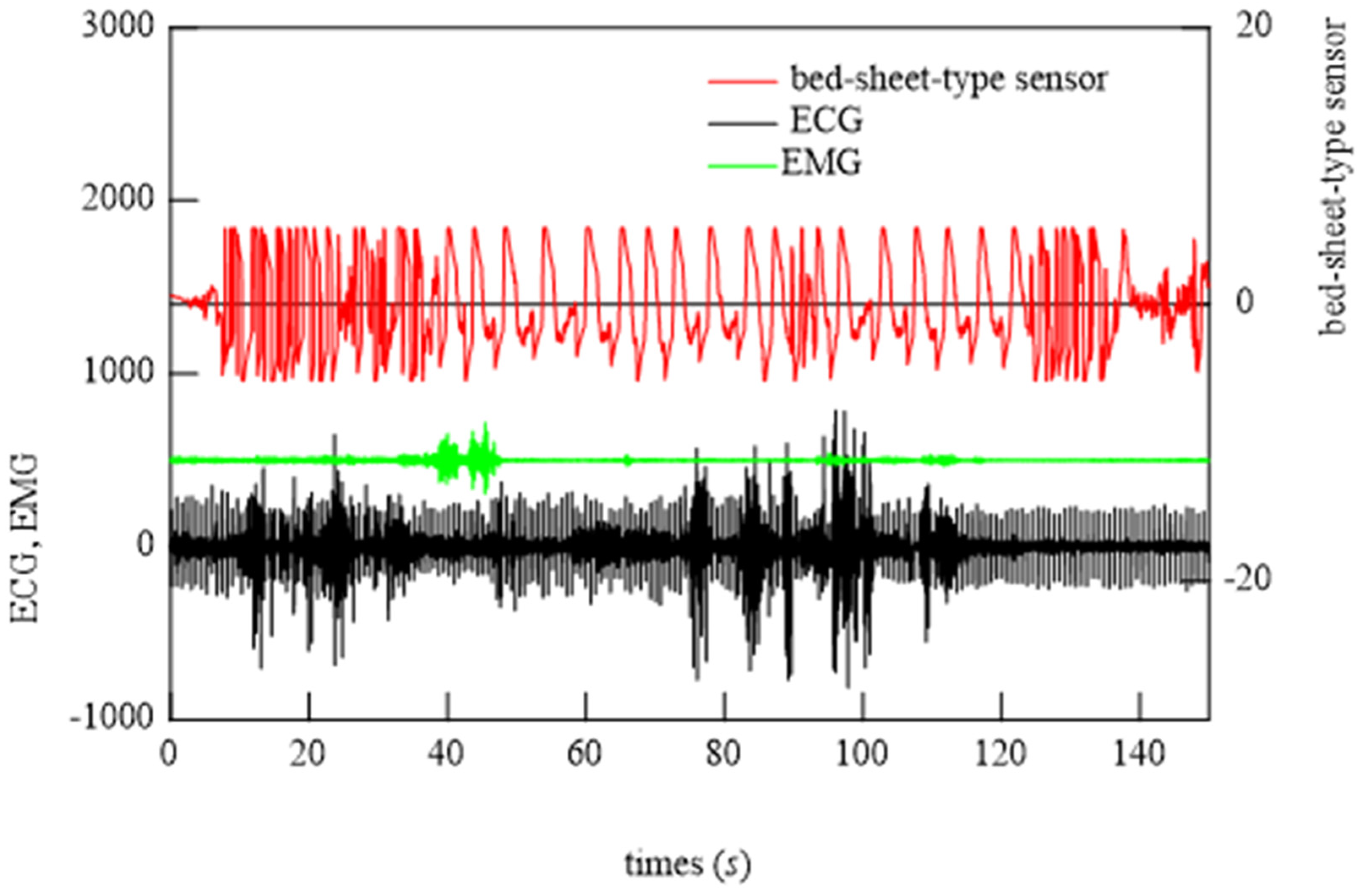
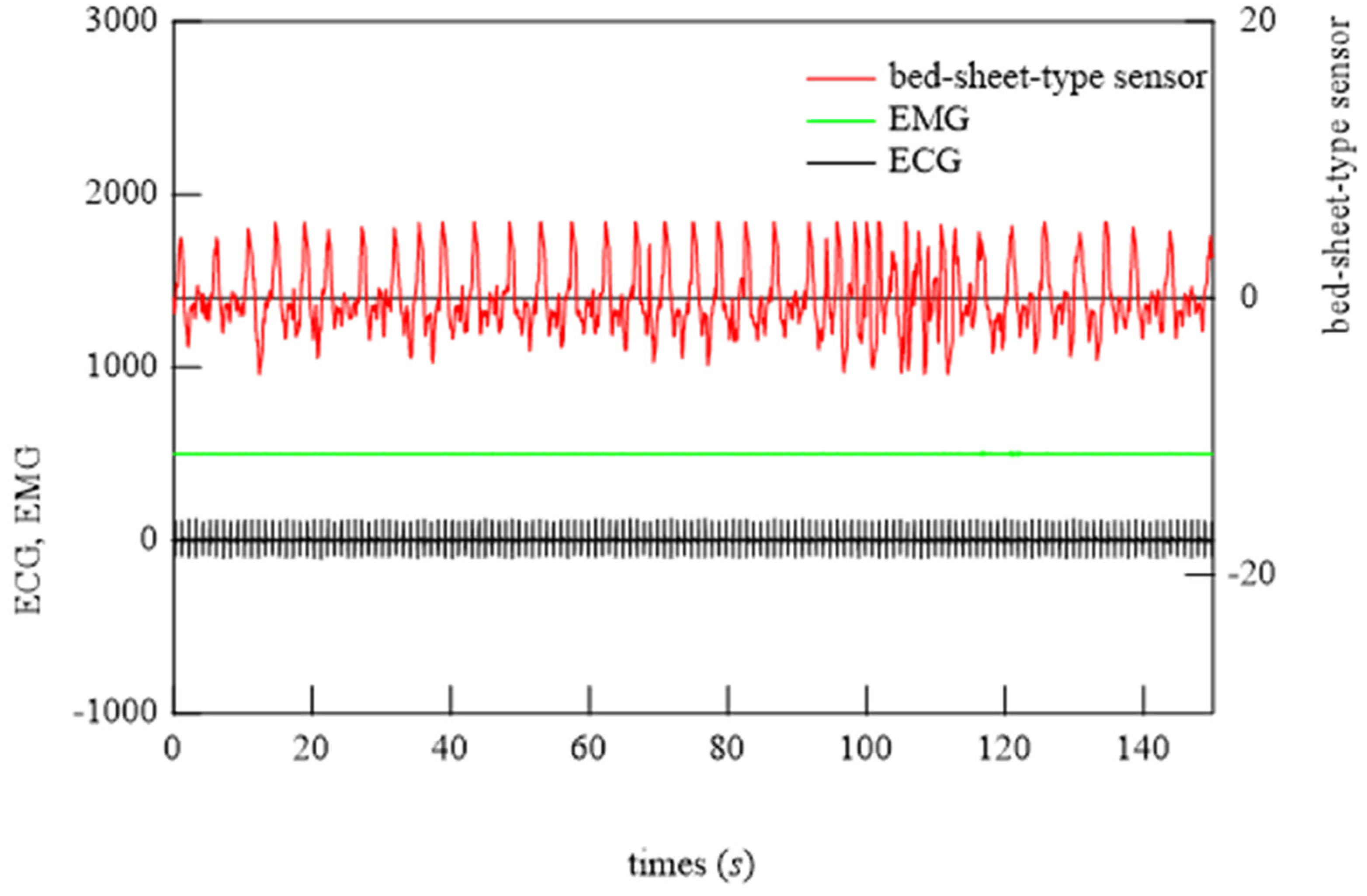
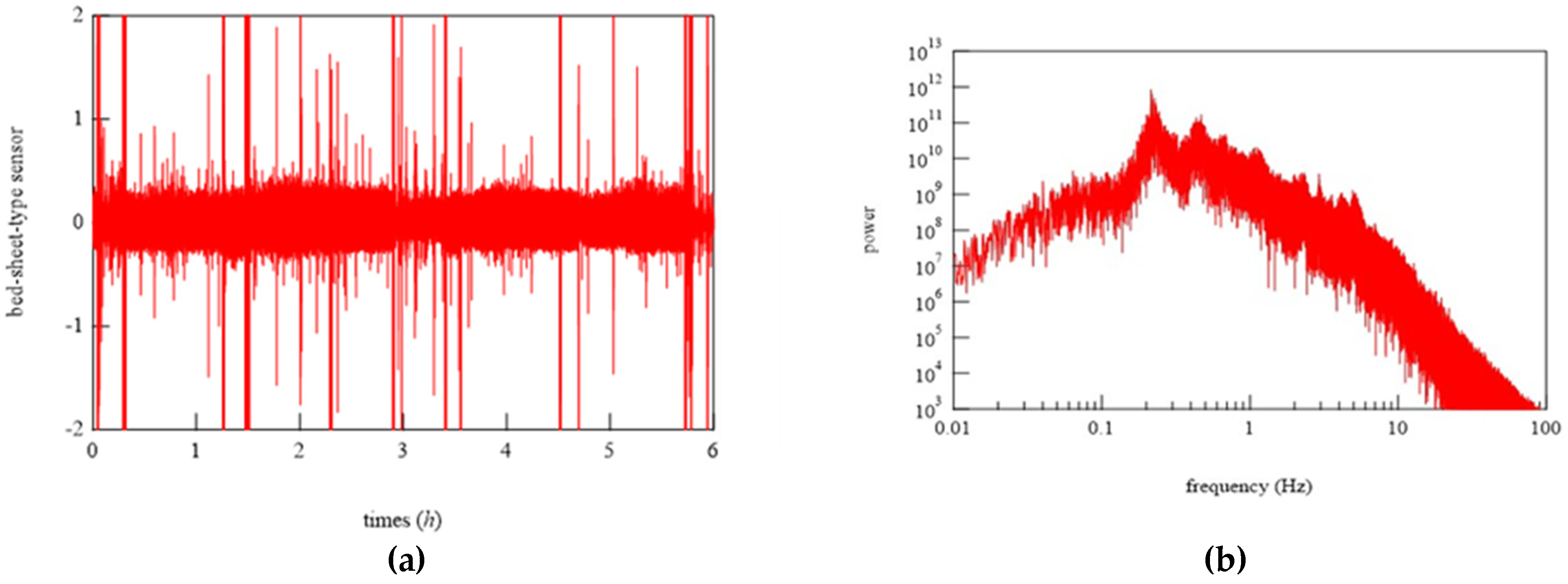
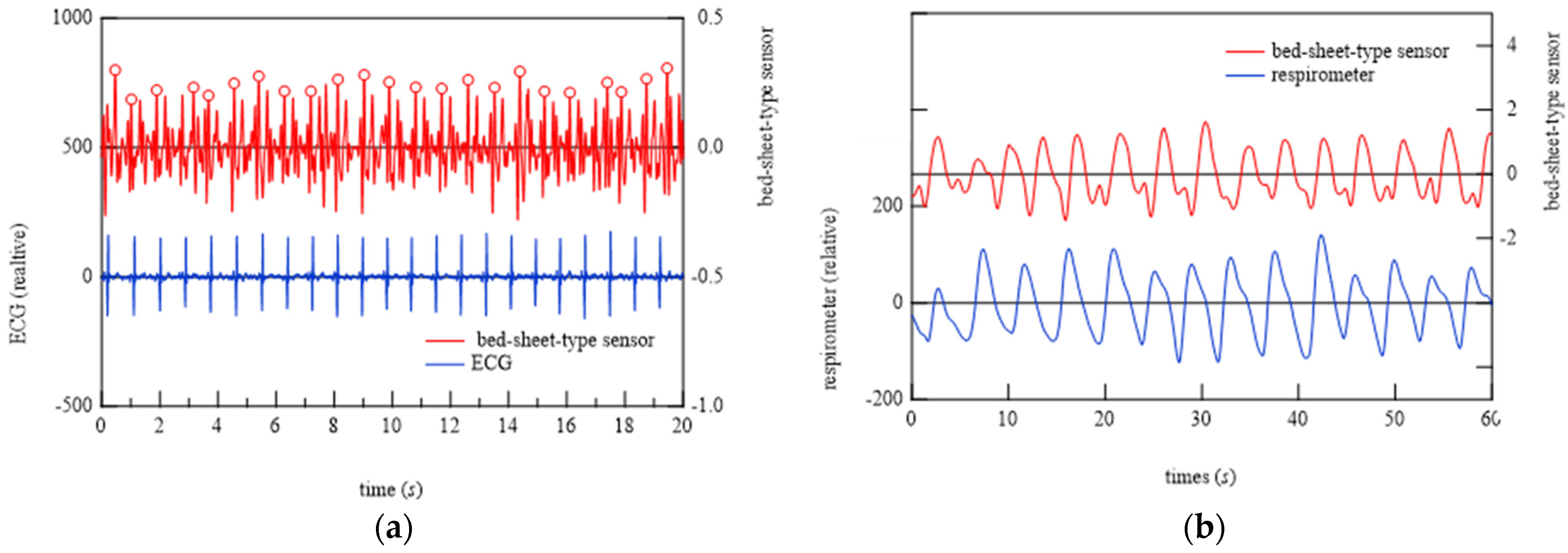
5. Detection of Bruxism during Sleep
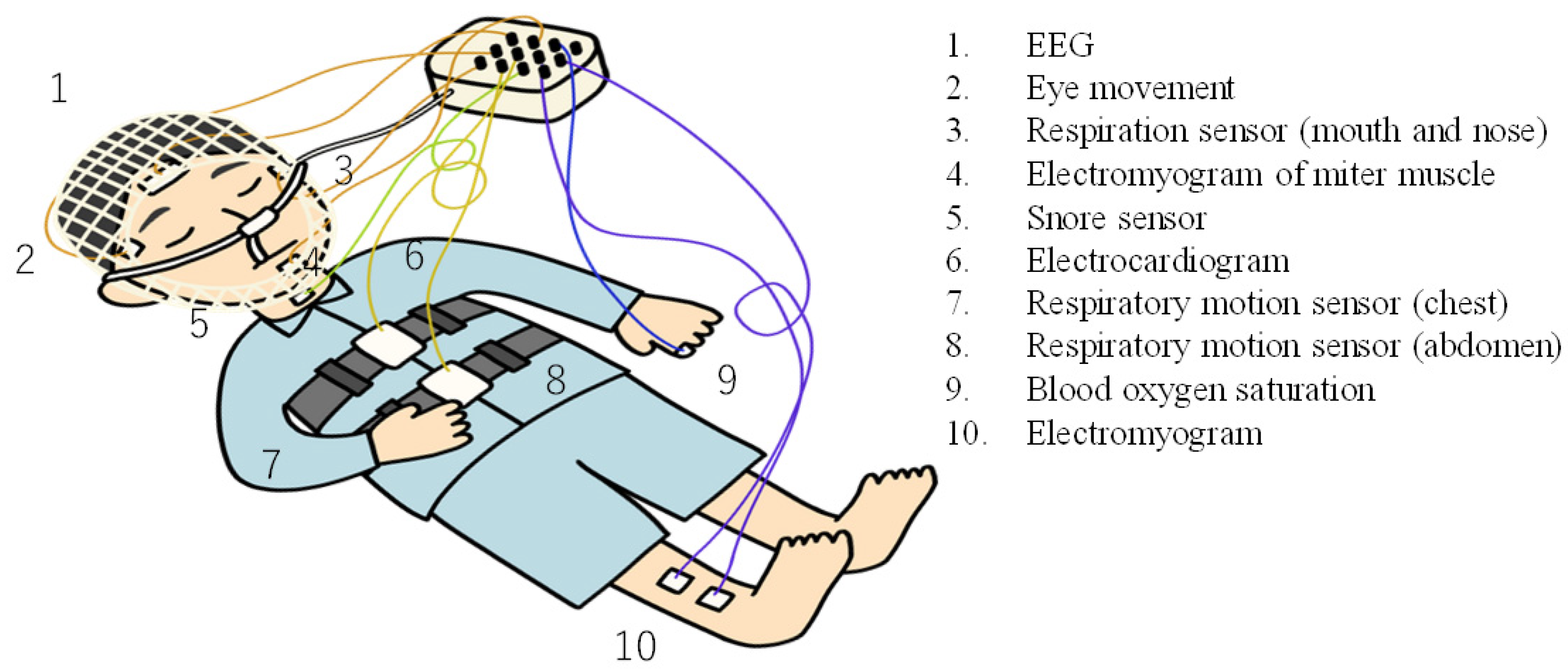
5.1. Medical Diagnostic Measurements
- 1)
- Mean amplitude of the electromyogram:More than 10% of the maximum occlusal force (masseter muscle) at waking time.
- 2)
- Muscle contraction pattern during sleep bruxism episodes:
- (a)
- Phasic episode: 3 or more bursts (duration of 0.25 s to 2.0 s for each burst).
- (b)
- Tonic episode: one burst lasting more than 2 s.
- (c)
- Mixed episodes: bursts of both phasic and tonic episodes are present.
5.2. Bed-Sheet-Type Sensor Measurements
6. Results
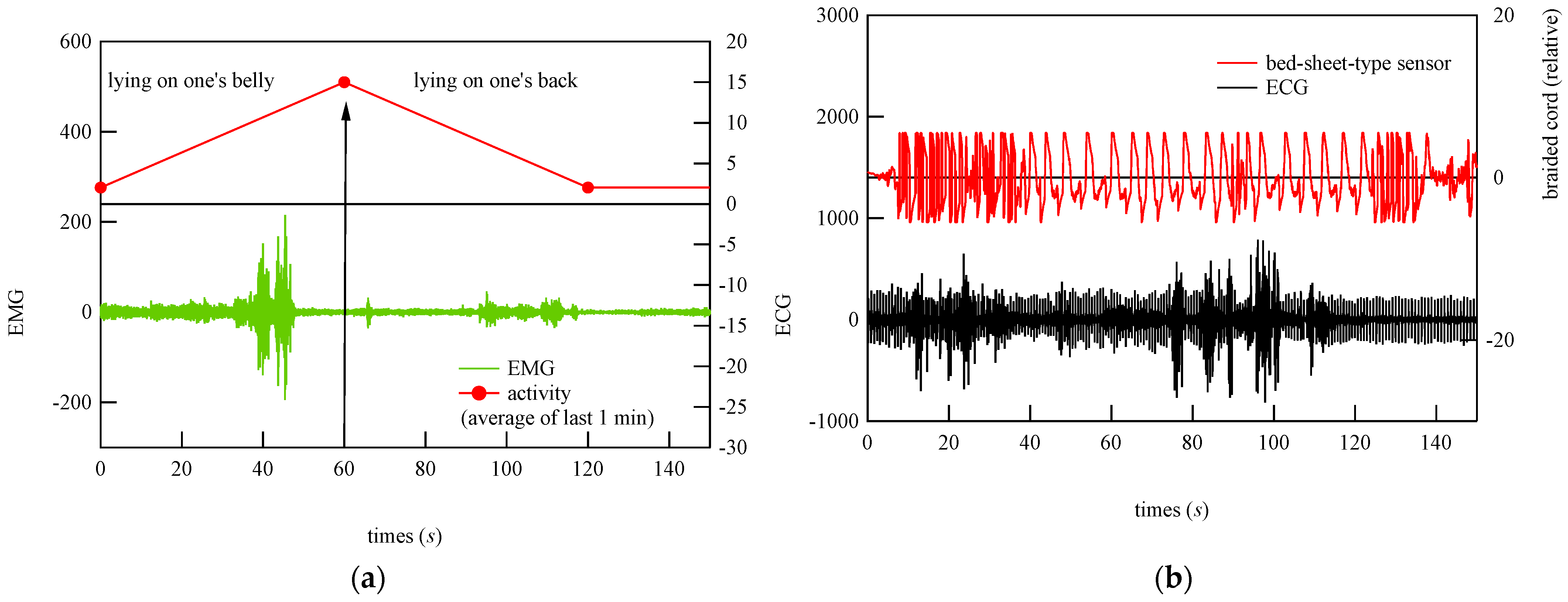
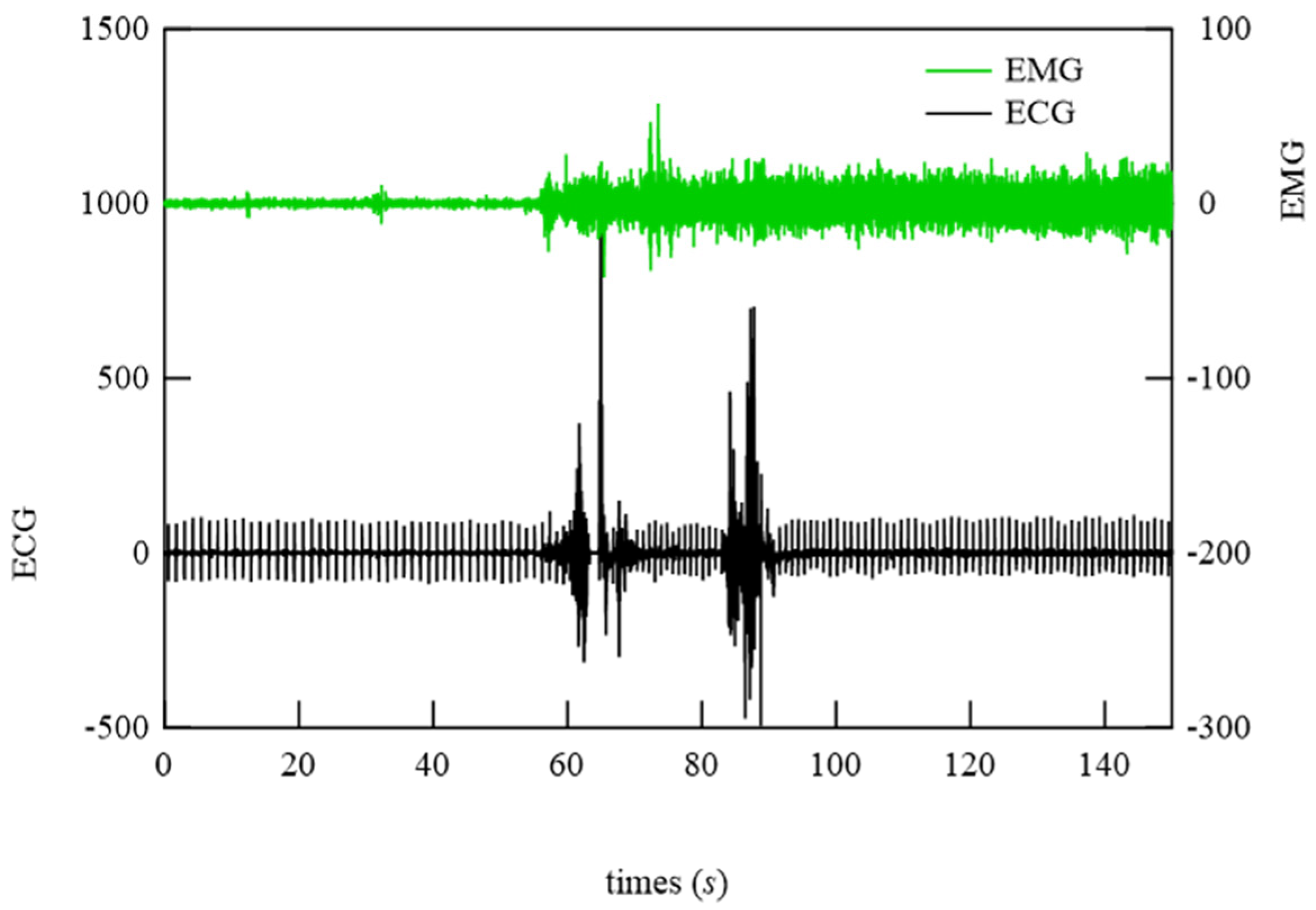
6.1. Medical Judgment
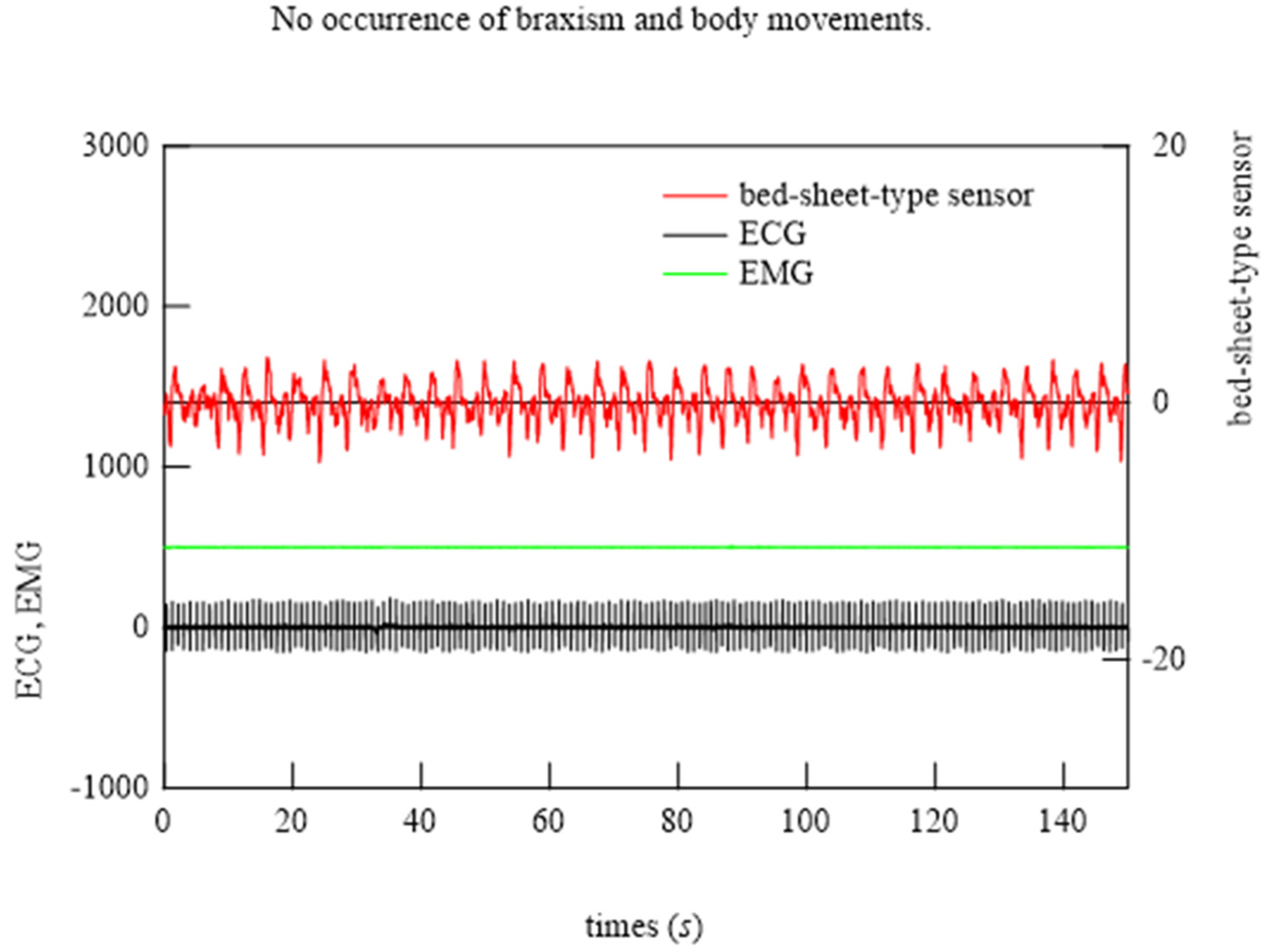
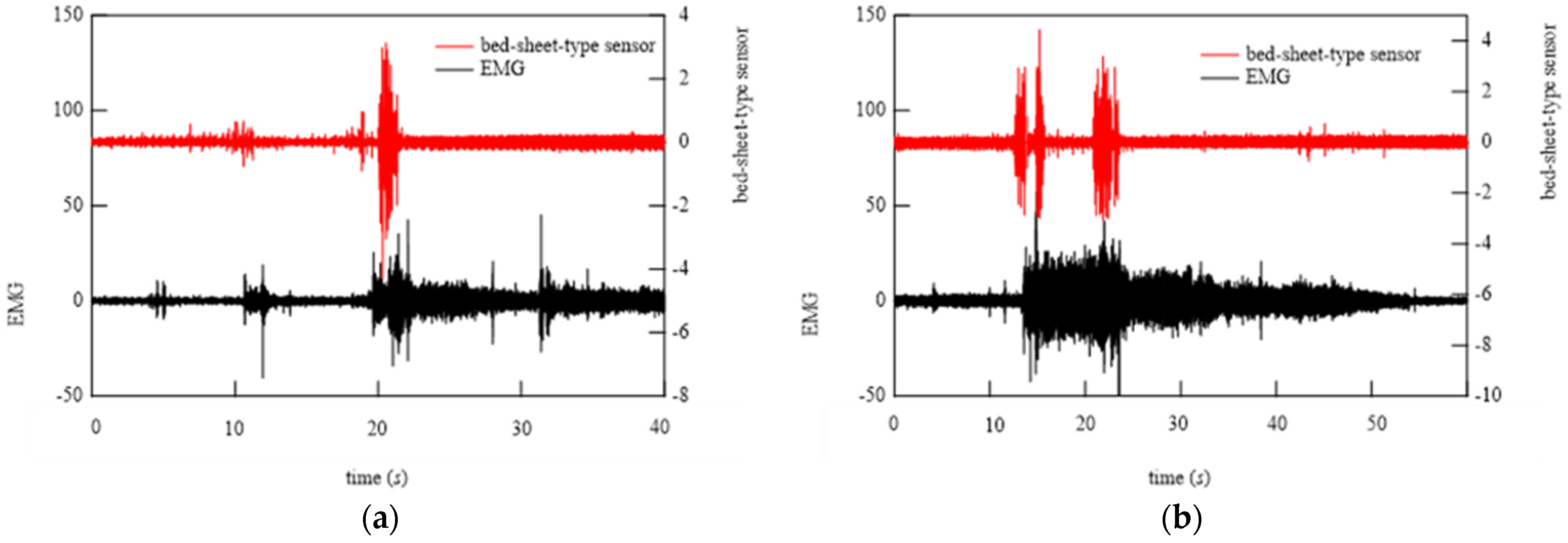
6.2. Demonstration of Bed-Sheet-Type Sensor
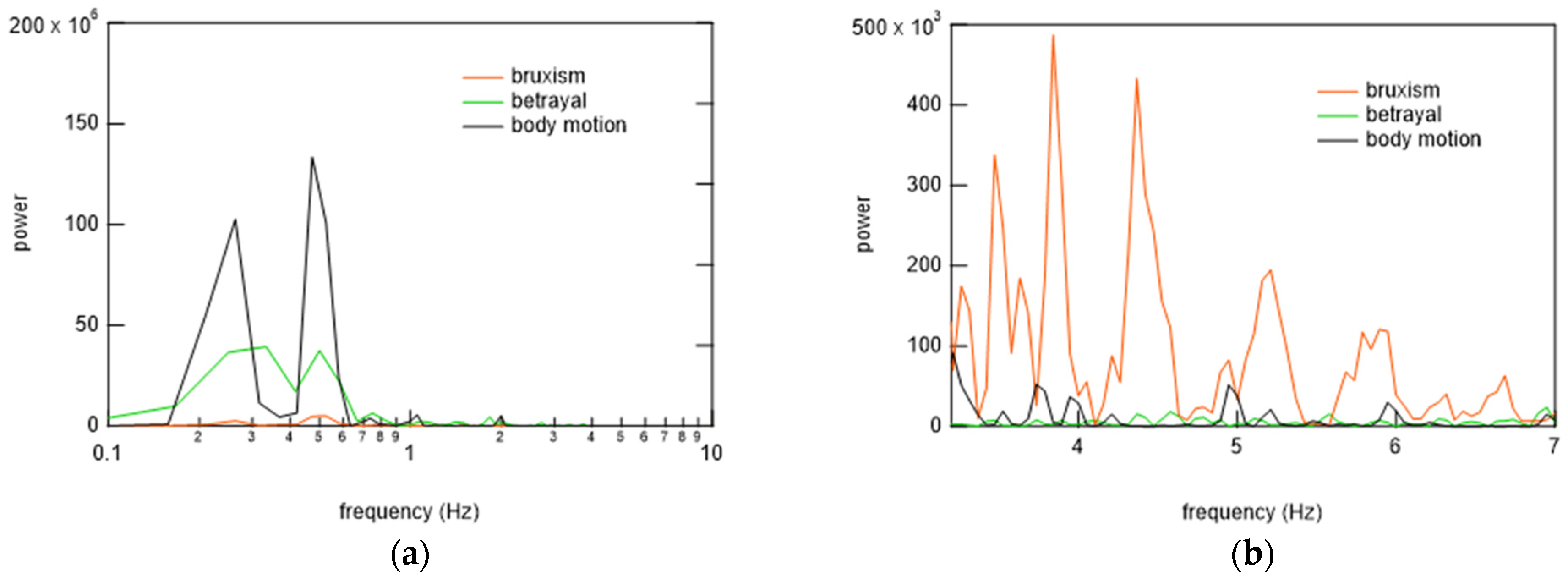
6.3. Algorithm for Bruxism Detection
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hobson, J.A. Sleep is of the brain, by the brain and for the brain. Nature 2005, 437, 1254–1256. [Google Scholar] [CrossRef] [PubMed]
- Imeri, L.; Opp, M. How (and why) the immune system makes us sleep. Nat. Rev. Neurosci. 2009, 10, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, E.C.; Van Cauter, E. Quantification of sleep behavior and of its impact on the cross-talk between the brain and peripheral metabolism. Proc. Natl. Acad. Sci. USA 2011, 108, 15609–15616. [Google Scholar] [CrossRef] [PubMed]
- Faraut, B.; Boudjeltia, K.Z.; Vanhamme, L.; Kerkhofs, M. Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. Sleep Med. Rev. 2012, 16, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.H. The energy allocation function of sleep: A unifying theory of sleep, torpor, and continuous wakefulness. Neurosci. Bowbearer. 2014, 47, 122–153. [Google Scholar] [CrossRef] [PubMed]
- Zielinski, M.R.; McKenna, J.T.; McCarley, R.W. Functions and mechanisms of sleep. AIMS Neurosci. 2016, 3, 67–104. [Google Scholar] [CrossRef] [PubMed]
- Rockstrom, M.D.; Chen, L.; Taishi, P.; Nguyen, J.T.; Gibbons, C.M.; Veasey, S.C.; Krueger, J.M. Tumor necrosis factor alpha in sleep regulation. Sleep Med. Rev. 2018, 40, 69–78. [Google Scholar] [CrossRef]
- Harding, E.C.; Franks, N.P.; Wisden, W. Sleep and thermoregulation. Curr. Opin. Physiol. 2020, 15, 7–13. [Google Scholar] [CrossRef]
- Berry, R.B.; Brooks, R.; Gamaldo, S.E.; Harding, M.; Lloyd, R.; Quan, S.; Troester, M.; Vaughn, B. The AASM Manual for the Scoring of Sleep and Associated Events Rules, Terminology and Technical Specifications Version 2.4; American Academy of Sleep Medicine: Darien, IL, USA, 2017. [Google Scholar]
- Geyer, J.; Carney, P. Atlas of Polysomnography; Wolters Kluwer Health: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Mattice, C.; Brooks, R.; Chiong, L. Fundamentals of Sleep Technology; Wolters Kluwer Health: Alphen aan den Rijn, The Netherlands, 2020. [Google Scholar]
- Tajitsu, Y.; Kawase, Y.; Katsuya, K.; Tamura, M.; Sakamoto, K.; Kawahara, K.; Harada, Y.; Kondo, T.; Imada, Y. New wearable sensor in the shape of a braided cord (Kumihimo). IEEE Trans. Dielectr. Electr. Insul. 2018, 25, 772–777. [Google Scholar] [CrossRef]
- Tajitsu, Y. Development of E-textile Sewn Together with Embroidered Fabric Having Motion-Sensing Function Using Piezoelectric Braided Cord for Embroidery. IEEE Trans. Dielectr. Electr. Insul. 2020, 27, 1644–1649. [Google Scholar] [CrossRef]
- Mukhopadhyay, S. Wearable Electronics Sensors: For Safe and Healthy Living (Smart Sensors, Measurement and Instrumentation, 15); Springer: Berlin, Germany, 2015. [Google Scholar]
- King, C. Application of Data Fusion Techniques and Technologies for Wearable Health Monitoring. Med. Eng. Phys. 2017, 42, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Witt, R.; Kellogg, A.; Snyder, P.; Dunn, J. Windows into Human Health through Wearables Data Analytics. Curr. Opin. Biomed. Eng. 2019, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, A.; Mahgoub, E.; Leavitt, A.; Asghar, W. Advances in Healthcare Wearable Devices. Flex. Electron. 2021, 5, 9. [Google Scholar] [CrossRef]
- Chakraborty, T.; Ghosh, I. Real-time Forecasts and Risk Assessment of Novel Coronavirus (COVID-19) Cases: A Data-Driven Analysis. Chaos Solitons Fractals 2020, 135, 109850. [Google Scholar] [CrossRef] [PubMed]
- Ates, H.C.; Nguyen, P.Q.; Gonzalez-Macia, L.; Morales-Narváez, E.; Güder, F.; Collins, J.J.; Dincer, C. End-to-end Design of Wearable Sensors. Nat. Rev. Mater. 2022, 7, 887. [Google Scholar] [CrossRef] [PubMed]
- Demrozi, F.; Borzì, L.; Olmo, G. Wearable Sensors for Supporting Diagnosis, Prognosis, and Monitoring of Neurodegenerative Diseases. Electronics 2023, 12, 1269. [Google Scholar] [CrossRef]
- Galetti, P.; DeRossi, D.; DeReggi, A. Medical Applications of Piezoelectric Polymers; Wiley: New York, NY, USA, 1988. [Google Scholar]
- Nalwa, H. Ferroelectric Polymers; Marcel Dekker: New York, NY, USA, 1995. [Google Scholar]
- Fukada, E. History and Recent Progress in Piezoelectric Polymers. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2000, 47, 1277–1290. [Google Scholar] [CrossRef]
- Tajitsu, Y. Piezoelectricity of Chiral Polymeric Fiber and Its Application in Biomedical Engineering. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2008, 55, 1000–1008. [Google Scholar] [CrossRef]
- Carpi, F.; Smela, E. Biomedical Applications of Electroactive Polymer Actuators; Wiley: Chichester, UK, 2009. [Google Scholar]
- Okuzaki, H.; Asaka, K. Soft Actuators; Springer: Cham, Switzerland, 2014. [Google Scholar]
- Ohki, Y. Development of a Braided Piezoelectric Cord for Wearable Sensors. Electr. Insul. Mag. 2020, 36, 59–64. [Google Scholar] [CrossRef]
- Yin, L. A Self-sustainable Wearable Multi-modular E-textile Bioenergy Microgrid System. Nat. Commun. 2021, 12, 1542–1555. [Google Scholar] [CrossRef]
- Sateia, M. International Classification of Sleep Disorders, 3rd ed.; The American College of Chest Physicians: Glenview, IL, USA, 2014; Volume 146, pp. 1387–1394. [Google Scholar]
- Thomas, D.; Patel, J.; Kumar, S.; Dakshinamoorthy, J.; Greenstein, Y.; Ravindran, H.; Pitchumani, P. Sleep Related Bruxism—Comprehensive Review of the Literature Based on a Rare Case presentation. Front. Oral Maxillofac. Med. 2024, 6, 3–23. [Google Scholar] [CrossRef]
- Kato, T.; Yamaguchi, T.; Okura, K.; Abe, S.; Lavigne, G. Sleep less and bite more: Sleep disorders associated with occlusal loads during sleep. J. Prosthodont. Res. 2013, 57, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.; Rugh, D.; Handelman, L. Nocturnal Masseter Muscle Activity and Urinary Catecholamine Levels in Bruxers. J. Dent Res. 1980, 59, 1571–1576. [Google Scholar] [CrossRef] [PubMed]
- Macedo, R.; Silva, A.; Machado, A.; Saconato, H.; Prado, F. Occlusal splints for Treating Sleep Bruxism (tooth grinding). Cochrane Database Syst Rev. 2007, 17, CD005514. [Google Scholar] [CrossRef] [PubMed]
- Seraidarian, P.; Seraidarian, I.; Cavalcanti, B.; Marchini, L.; Neves, C. Urinary Levels of Catecholamines among Individuals with and without Sleep bruxism. Sleep Breath 2009, 13, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Furihata, R.; Saitoha, K.; Suzuki, M.; Jike, M.; Kaneita, Y.; Ohida, T.; Buysse, D.; Uchiyama, M. A Composite Measure of Sleep Health Is Associated with Symptoms of Depression among Japanese Female Hospital Nurses. Compr. Psychiatry 2012, 97, 152151. [Google Scholar] [CrossRef]
- Nonoue, S.; Mashita, M.; Haraki, S.; Mikami, A.; Adachi, H.; Yatani, H.; Yoshida, A.; Taniike, M.; Kato, T. Inter-scorer Reliability of Sleep Assessment Using EEG and EOG Recording System in Comparison to Polysomnography. Sleep Biol. Rhythm. 2017, 15, 39–48. [Google Scholar] [CrossRef]
- Borbely, A.; Achermann, P. Sleep homeostasis and models of sleep regulation. In Principles and Practice of Sleep Medicine, 5th ed.; Kryger, M.H., Roth, T., Dement, W.C., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2010; pp. 431–444. [Google Scholar]
- Urade, Y.; Hayaishi, O. Prostaglandin D2 and sleep/wake regulation. Sleep Med. Rev. 2011, 15, 411–418. [Google Scholar] [CrossRef]
- Nye, J. Physical Properties of Crystals; Clarendon Press: Oxford, UK, 1985. [Google Scholar]
- Lang, S.B. Guide to the Literature of Piezoelectricity and Pyroelectricity. Ferroelectrics 2005, 321, 91–204. [Google Scholar] [CrossRef]
- Tajitsu, Y.; Takarada, J.; Takatani, K.; Nakanishi, R.; Yanagimoto, H.; Shiomi, S.; Nakagawa, I.; Kawahara, I.; Nakiri, T.; Shimda, S.; et al. Prototype Sensor System Using Fabricated Piezoelectric Braided Cord for Work-Environment Measurement during Work from Home. Micromachines 2021, 12, 966–978. [Google Scholar] [CrossRef]
- Tajitsu, Y.; Takarada, J.; Tokiya, H.; Sugii, R.; Takatani, K.; Yanagimoto, H.; Riku Nakanishi, R.; Seita Shiomi, S.; Daiki Kitamoto, D.; Nakiri, T.; et al. Application of Piezoelectric PLLA Braided Cord as Wearable Sensor to Realize Monitoring System for Indoor Dogs withLess Physical or Mental Stress. Micromachines 2023, 14, 143–163. [Google Scholar] [CrossRef] [PubMed]







| Distance between Right and Left Acromion (Not Necessarily a Straight Line) | Vertical Distance from the Acromion to the Lower End of the Elbow Bone Bent at a Right Angle | Horizontal Linear Distance between the Anterior and Posterior Surfaces of the Chest at the Nipple Point | |||
|---|---|---|---|---|---|
| male | female | male | female | male | female |
| mm | mm | mm | |||
| 403 | 358 | 340 | 338 | 201 | 201 |
| 404 | 360 | 315 | 309 | 212 | 200 |
| 406 | 358 | 341 | 335 | 222 | 200 |
| 406 | 359 | 316 | 308 | 225 | 204 |
| 404 | 360 | 342 | 329 | 228 | 209 |
| 403 | 359 | 314 | 307 | 230 | 210 |
| 399 | 358 | 341 | 329 | 231 | 214 |
| 395 | 359 | 314 | 306 | 229 | 219 |
| 391 | 356 | 339 | 330 | 225 | 222 |
| 388 | 352 | 312 | 305 | 228 | 229 |
| 385 | 350 | 339 | 328 | 230 | 231 |
| 380 | 347 | 309 | 300 | 228 | 233 |
| From the Ministry of Economy, Trade and Industry Japan | |||||
| Subject | Gender | Age | Height (cm) | Weight (kg) | BMI | Medical Diagnosis | Bed-Sheet-Type Sensor | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Determination by Bed-sheet-Type Sensor | Number of Times of Correct Judgment | Number of Times of Misjudgment | Success Rate (%) | |||||||
| 1 | male | 34 | 163 | 96 | 36 | 150 | 158 | 150 | 8 | 94.9 |
| 2 | female | 81 | 159 | 58 | 23 | 30 | 35 | 30 | 5 | 85.7 |
| 3 | male | 39 | 173 | 67 | 22 | 51 | 53 | 51 | 2 | 96.2 |
| 4 | male | 35 | 155 | 60 | 25 | 34 | 38 | 34 | 4 | 89.5 |
| 5 | male | 15 | 164 | 49 | 18 | 46 | 54 | 46 | 8 | 85.2 |
| 6 | male | 47 | 181 | 68 | 21 | 88 | 94 | 88 | 6 | 93.6 |
| 7 | male | 46 | 170 | 90 | 31 | 91 | 97 | 91 | 6 | 93.8 |
| 8 | male | 58 | 170 | 64 | 22 | 93 | 99 | 93 | 6 | 93.9 |
| 9 | female | 38 | 170 | 82 | 28 | 41 | 47 | 41 | 6 | 87.2 |
| 10 | male | 61 | 167 | 69 | 25 | 74 | 82 | 74 | 8 | 90.2 |
| 11 | male | 64 | 175 | 98 | 32 | 47 | 49 | 47 | 2 | 95.9 |
| 12 | female | 58 | 163 | 66 | 25 | 47 | 49 | 47 | 2 | 95.9 |
| average of success rate (%) | 91.9 | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tajitsu, Y.; Shimda, S.; Nonomura, T.; Yanagimoto, H.; Nakamura, S.; Ueshima, R.; Kawanobe, M.; Nakiri, T.; Takarada, J.; Takeuchi, O.; et al. Application of Braided Piezoelectric Poly-l-Lactic Acid Cord Sensor to Sleep Bruxism Detection System with Less Physical or Mental Stress. Micromachines 2024, 15, 86. https://doi.org/10.3390/mi15010086
Tajitsu Y, Shimda S, Nonomura T, Yanagimoto H, Nakamura S, Ueshima R, Kawanobe M, Nakiri T, Takarada J, Takeuchi O, et al. Application of Braided Piezoelectric Poly-l-Lactic Acid Cord Sensor to Sleep Bruxism Detection System with Less Physical or Mental Stress. Micromachines. 2024; 15(1):86. https://doi.org/10.3390/mi15010086
Chicago/Turabian StyleTajitsu, Yoshiro, Saki Shimda, Takuto Nonomura, Hiroki Yanagimoto, Shun Nakamura, Ryoma Ueshima, Miyu Kawanobe, Takuo Nakiri, Jun Takarada, Osamu Takeuchi, and et al. 2024. "Application of Braided Piezoelectric Poly-l-Lactic Acid Cord Sensor to Sleep Bruxism Detection System with Less Physical or Mental Stress" Micromachines 15, no. 1: 86. https://doi.org/10.3390/mi15010086
APA StyleTajitsu, Y., Shimda, S., Nonomura, T., Yanagimoto, H., Nakamura, S., Ueshima, R., Kawanobe, M., Nakiri, T., Takarada, J., Takeuchi, O., Nisho, R., Takeshita, K., Takahashi, M., & Sugiyama, K. (2024). Application of Braided Piezoelectric Poly-l-Lactic Acid Cord Sensor to Sleep Bruxism Detection System with Less Physical or Mental Stress. Micromachines, 15(1), 86. https://doi.org/10.3390/mi15010086








