Molecular Imaging in Pediatric Brain Tumors
Abstract
1. Introduction
2. Imaging of Cell Metabolism (Buildup of Phospholipid Cell Membranes [11C] Choline ([11C] CH), [18F] Fluoromethylcholine ([18F] FCH) and [18F] Fluoroethylcholine ([18F] FEC)
3. Imaging of Somatostatin Receptors: (111Indium-Diethylenetriaminepentaacetic Acid-d-Phenylalanine-Octreotide ([111In] Pentetreotide), [68Ga] DOTA-Peptides)
4. Imaging of Cell Metabolism (Glucose Metabolism and Mitochondrial Oxidative Metabolism): 18F-Fluorodeoxyglucose ([18F] FDG) and 99mTc-Methoxyisobutylisonitrile ([99mTc] MIBI)
5. Imaging of Amino-Acid Metabolism and DNA Synthesis: [18F]-L-Dihydroxyphenylalanine ([18F] FDOPA), l-[Methyl-11C] Methionine ([11C]MET), O-(2-[18F]Fluoroethyl)-l-Tyrosine ([18F] FET), and 3′-Deoxy-3′-18F-Fluorothymidine ([18F] FLT)
6. Ongoing Clinical Studies and Future Perspectives
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ostrom, Q.T.; Gittleman, H.; Truitt, G.; Boscia, A.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro-Oncology 2018, 20, iv1–iv86. [Google Scholar] [CrossRef] [PubMed]
- Peris-Bonet, R.; Martinez-Garcia, C.; Lacour, B.; Petrovich, S.; Giner-Ripoll, B.; Navajas, A.; Steliarova-Foucher, E. Childhood central nervous system tumours–incidence and survival in Europe (1978–1997): Report from Automated Childhood Cancer Information System project. Eur. J. Cancer 2006, 42, 2064–2080. [Google Scholar] [CrossRef] [PubMed]
- Udaka, Y.T.; Packer, R.J. Pediatric Brain Tumors. Neurol. Clin. 2018, 36, 533–556. [Google Scholar] [CrossRef] [PubMed]
- Villanueva-Meyer, J.E.; Mabray, M.C.; Cha, S. Current Clinical Brain Tumor Imaging. Neurosurgery 2017, 81, 397–415. [Google Scholar] [CrossRef]
- Mabray, M.C.; Barajas, R.F., Jr.; Cha, S. Modern brain tumor imaging. Brain Tumor Res. Treat. 2015, 3, 8–23. [Google Scholar] [CrossRef]
- Dunkl, V.; Cleff, C.; Stoffels, G.; Judov, N.; Sarikaya-Seiwert, S.; Law, I.; Bogeskov, L.; Nysom, K.; Andersen, S.B.; Steiger, H.J.; et al. The usefulness of dynamic O-(2-18F-fluoroethyl)-L-tyrosine PET in the clinical evaluation of brain tumors in children and adolescents. J. Nucl. Med. 2015, 56, 88–92. [Google Scholar] [CrossRef]
- Misch, M.; Guggemos, A.; Driever, P.H.; Koch, A.; Grosse, F.; Steffen, I.G.; Plotkin, M.; Thomale, U.W. (18)F-FET-PET guided surgical biopsy and resection in children and adolescence with brain tumors. Child’s Nerv. Syst. ChNS Off. J. Int. Soc. Pediatric Neurosurg. 2015, 31, 261–267. [Google Scholar] [CrossRef]
- Chukwueke, U.N.; Wen, P.Y. Use of the Response Assessment in Neuro-Oncology (RANO) criteria in clinical trials and clinical practice. CNS Oncol. 2019, 8, CNS28. [Google Scholar] [CrossRef]
- Law, I.; Albert, N.L.; Arbizu, J.; Boellaard, R.; Drzezga, A.; Galldiks, N.; la Fougere, C.; Langen, K.J.; Lopci, E.; Lowe, V.; et al. Joint EANM/EANO/RANO practice guidelines/SNMMI procedure standards for imaging of gliomas using PET with radiolabelled amino acids and [(18)F]FDG: Version 1.0. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 540–557. [Google Scholar] [CrossRef]
- Fei, B.; Schuster, D.M. PET Molecular Imaging-Directed Biopsy: A Review. Am. J. Roentgenol. 2017, 209, 255–269. [Google Scholar] [CrossRef]
- Jeraj, R.; Bradshaw, T.; Simoncic, U. Molecular Imaging to Plan Radiotherapy and Evaluate its Efficacy. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2015, 56, 1752–1765. [Google Scholar] [CrossRef] [PubMed]
- O’Tuama, L.A.; Treves, S.T.; Larar, J.N.; Packard, A.B.; Kwan, A.J.; Barnes, P.D.; Scott, R.M.; Black, P.M.; Madsen, J.R.; Goumnerova, L.C.; et al. Thallium-201 versus technetium-99m-MIBI SPECT in evaluation of childhood brain tumors: A within-subject comparison. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 1993, 34, 1045–1051. [Google Scholar]
- Kirton, A.; Kloiber, R.; Rigel, J.; Wolff, J. Evaluation of pediatric CNS malignancies with (99m)Tc-methoxyisobutylisonitrile SPECT. J. Nucl. Med. 2002, 43, 1438–1443. [Google Scholar] [PubMed]
- Barai, S.; Bandopadhayaya, G.P.; Julka, P.K.; Haloi, A.K.; Seith, A.; Malhotra, A. Evaluation of single photon emission computerised tomography (SPECT) using Tc99m-tetrofosmin as a diagnostic modality for recurrent posterior fossa tumours. J. Postgrad. Med. 2003, 49, 316–320; discussion 320–311. [Google Scholar] [PubMed]
- Ohtani, T.; Kurihara, H.; Ishiuchi, S.; Saito, N.; Oriuchi, N.; Inoue, T.; Sasaki, T. Brain tumour imaging with carbon-11 choline: Comparison with FDG PET and gadolinium-enhanced MR imaging. Eur. J. Nucl. Med. 2001, 28, 1664–1670. [Google Scholar] [CrossRef] [PubMed]
- Fraioli, F.; Shankar, A.; Hargrave, D.; Hyare, H.; Gaze, M.N.; Groves, A.M.; Alongi, P.; Stoneham, S.; Michopoulou, S.; Syed, R.; et al. 18F-fluoroethylcholine (18F-Cho) PET/MRI functional parameters in pediatric astrocytic brain tumors. Clin. Nucl. Med. 2015, 40, e40–e45. [Google Scholar] [CrossRef]
- Tsouana, E.; Stoneham, S.; Fersht, N.; Kitchen, N.; Gaze, M.; Bomanji, J.; Fraioli, F.; Hargrave, D.; Shankar, A. Evaluation of treatment response using integrated 18F-labeled choline positron emission tomography/magnetic resonance imaging in adolescents with intracranial non-germinomatous germ cell tumours. Pediatric Blood Cancer 2015, 62, 1661–1663. [Google Scholar] [CrossRef]
- Muller, H.L.; Fruhwald, M.C.; Scheubeck, M.; Rendl, J.; Warmuth-Metz, M.; Sorensen, N.; Kuhl, J.; Reubi, J.C. A possible role for somatostatin receptor scintigraphy in the diagnosis and follow-up of children with medulloblastoma. J. Neuro-Oncol. 1998, 38, 27–40. [Google Scholar] [CrossRef]
- Fruhwald, M.C.; Rickert, C.H.; O’Dorisio, M.S.; Madsen, M.; Warmuth-Metz, M.; Khanna, G.; Paulus, W.; Kuhl, J.; Jurgens, H.; Schneider, P.; et al. Somatostatin receptor subtype 2 is expressed by supratentorial primitive neuroectodermal tumors of childhood and can be targeted for somatostatin receptor imaging. Clin. Cancer Res. 2004, 10, 2997–3006. [Google Scholar] [CrossRef]
- Abongwa, C.; Mott, S.; Schafer, B.; McNeely, P.; Abusin, G.; O’Dorisio, T.; Zamba, G.; O’Dorisio, M.S.; Menda, Y. Safety and accuracy of (68)Ga-DOTATOC PET/CT in children and young adults with solid tumors. Am. J. Nucl. Med. Mol. Imaging 2017, 7, 228–235. [Google Scholar]
- Arunraj, S.T.; Parida, G.K.; Damle, N.A.; Arora, S.; Reddy, S.; Chakraborty, D.; Prabhu, M.; Tripathi, M.; Bal, C. 68Ga-DOTANOC PET/CT in Medulloblastoma. Clin. Nucl. Med. 2018, 43, e145–e146. [Google Scholar] [CrossRef]
- Menda, Y.; O’Dorisio, M.S.; Kao, S.; Khanna, G.; Michael, S.; Connolly, M.; Babich, J.; O’Dorisio, T.; Bushnell, D.; Madsen, M. Phase I trial of 90Y-DOTATOC therapy in children and young adults with refractory solid tumors that express somatostatin receptors. J. Nucl. Med. 2010, 51, 1524–1531. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Salamon, N.; Jackson, H.A.; Bluml, S.; Panigrahy, A. PET imaging in pediatric neuroradiology: Current and future applications. Pediatric Radiol. 2010, 40, 82–96. [Google Scholar] [CrossRef] [PubMed]
- Uslu, L.; Donig, J.; Link, M.; Rosenberg, J.; Quon, A.; Daldrup-Link, H.E. Value of 18F-FDG PET and PET/CT for evaluation of pediatric malignancies. J. Nucl. Med. 2015, 56, 274–286. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.; Fahey, F.H.; Treves, S.T.; Kocak, M.; Pollack, I.F.; Boyett, J.M.; Kun, L.E.; Poussaint, T.Y. Exploratory evaluation of two-dimensional and three-dimensional methods of FDG PET quantification in pediatric anaplastic astrocytoma: A report from the Pediatric Brain Tumor Consortium (PBTC). Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 1651–1658. [Google Scholar] [CrossRef] [PubMed]
- Zukotynski, K.A.; Fahey, F.H.; Kocak, M.; Alavi, A.; Wong, T.Z.; Treves, S.T.; Shulkin, B.L.; Haas-Kogan, D.A.; Geyer, J.R.; Vajapeyam, S.; et al. Evaluation of 18F-FDG PET and MRI associations in pediatric diffuse intrinsic brain stem glioma: A report from the Pediatric Brain Tumor Consortium. J. Nucl. Med. 2011, 52, 188–195. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kruer, M.C.; Kaplan, A.M.; Etzl, M.M., Jr.; Carpentieri, D.F.; Dickman, P.S.; Chen, K.; Mathieson, K.; Irving, A. The value of positron emission tomography and proliferation index in predicting progression in low-grade astrocytomas of childhood. J. Neuro-Oncol. 2009, 95, 239–245. [Google Scholar] [CrossRef]
- Kwon, J.W.; Kim, I.O.; Cheon, J.E.; Kim, W.S.; Moon, S.G.; Kim, T.J.; Chi, J.G.; Wang, K.C.; Chung, J.K.; Yeon, K.M. Paediatric brain-stem gliomas: MRI, FDG-PET and histological grading correlation. Pediatric Radiol. 2006, 36, 959–964. [Google Scholar] [CrossRef]
- O’Tuama, L.A.; Phillips, P.C.; Strauss, L.C.; Carson, B.C.; Uno, Y.; Smith, Q.R.; Dannals, R.F.; Wilson, A.A.; Ravert, H.T.; Loats, S.; et al. Two-phase [11C]L-methionine PET in childhood brain tumors. Pediatric Neurol. 1990, 6, 163–170. [Google Scholar] [CrossRef]
- Utriainen, M.; Metsahonkala, L.; Salmi, T.T.; Utriainen, T.; Kalimo, H.; Pihko, H.; Makipernaa, A.; Harila-Saari, A.; Jyrkkio, S.; Laine, J.; et al. Metabolic characterization of childhood brain tumors: Comparison of 18F-fluorodeoxyglucose and 11C-methionine positron emission tomography. Cancer 2002, 95, 1376–1386. [Google Scholar] [CrossRef]
- Pirotte, B.; Acerbi, F.; Lubansu, A.; Goldman, S.; Brotchi, J.; Levivier, M. PET imaging in the surgical management of pediatric brain tumors. Child’s Nerv. Syst. 2007, 23, 739–751. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.T., Jr.; Serrano, N.; Kim, H.; Li, X.; Snyder, S.E.; Hwang, S.; Li, Y.; Hua, C.H.; Broniscer, A.; Merchant, T.E.; et al. (11)C-Methionine positron emission tomography delineates non-contrast enhancing tumor regions at high risk for recurrence in pediatric high-grade glioma. J. Neuro-Oncol. 2017, 132, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Morana, G.; Piccardo, A.; Puntoni, M.; Nozza, P.; Cama, A.; Raso, A.; Mascelli, S.; Massollo, M.; Milanaccio, C.; Garre, M.L.; et al. Diagnostic and prognostic value of 18F-DOPA PET and 1H-MR spectroscopy in pediatric supratentorial infiltrative gliomas: A comparative study. Neuro-Oncol. 2015, 17, 1637–1647. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morana, G.; Piccardo, A.; Tortora, D.; Puntoni, M.; Severino, M.; Nozza, P.; Ravegnani, M.; Consales, A.; Mascelli, S.; Raso, A.; et al. Grading and outcome prediction of pediatric diffuse astrocytic tumors with diffusion and arterial spin labeling perfusion MRI in comparison with 18F-DOPA PET. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 2084–2093. [Google Scholar] [CrossRef]
- Morana, G.; Puntoni, M.; Garre, M.L.; Massollo, M.; Lopci, E.; Naseri, M.; Severino, M.; Tortora, D.; Rossi, A.; Piccardo, A. Ability of (18)F-DOPA PET/CT and fused (18)F-DOPA PET/MRI to assess striatal involvement in paediatric glioma. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1664–1672. [Google Scholar] [CrossRef]
- Hutterer, M.; Hattingen, E.; Palm, C.; Proescholdt, M.A.; Hau, P. Current standards and new concepts in MRI and PET response assessment of antiangiogenic therapies in high-grade glioma patients. Neuro-Oncology 2015, 17, 784–800. [Google Scholar] [CrossRef]
- Morana, G.; Piccardo, A.; Garre, M.L.; Nozza, P.; Consales, A.; Rossi, A. Multimodal magnetic resonance imaging and 18F-L-dihydroxyphenylalanine positron emission tomography in early characterization of pseudoresponse and nonenhancing tumor progression in a pediatric patient with malignant transformation of ganglioglioma treated with bevacizumab. J. Clin. Oncol. 2013, 31, e1–e5. [Google Scholar] [CrossRef]
- Gauvain, K.; Ponisio, M.R.; Barone, A.; Grimaldi, M.; Parent, E.; Leeds, H.; Goyal, M.; Rubin, J.; McConathy, J. (18)F-FDOPA PET/MRI for monitoring early response to bevacizumab in children with recurrent brain tumors. Neuro-Oncol. Pract. 2018, 5, 28–36. [Google Scholar] [CrossRef]
- Pauleit, D.; Stoffels, G.; Bachofner, A.; Floeth, F.W.; Sabel, M.; Herzog, H.; Tellmann, L.; Jansen, P.; Reifenberger, G.; Hamacher, K.; et al. Comparison of (18)F-FET and (18)F-FDG PET in brain tumors. Nucl. Med. Biol. 2009, 36, 779–787. [Google Scholar] [CrossRef]
- Plotkin, M.; Blechschmidt, C.; Auf, G.; Nyuyki, F.; Geworski, L.; Denecke, T.; Brenner, W.; Stockhammer, F. Comparison of F-18 FET-PET with F-18 FDG-PET for biopsy planning of non-contrast-enhancing gliomas. Eur. Radiol. 2010, 20, 2496–2502. [Google Scholar] [CrossRef]
- Pauleit, D.; Floeth, F.; Hamacher, K.; Riemenschneider, M.J.; Reifenberger, G.; Muller, H.W.; Zilles, K.; Coenen, H.H.; Langen, K.J. O-(2-[18F]fluoroethyl)-L-tyrosine PET combined with MRI improves the diagnostic assessment of cerebral gliomas. Brain J. Neurol. 2005, 128, 678–687. [Google Scholar] [CrossRef] [PubMed]
- Floeth, F.W.; Pauleit, D.; Wittsack, H.J.; Langen, K.J.; Reifenberger, G.; Hamacher, K.; Messing-Junger, M.; Zilles, K.; Weber, F.; Stummer, W.; et al. Multimodal metabolic imaging of cerebral gliomas: Positron emission tomography with [18F]fluoroethyl-L-tyrosine and magnetic resonance spectroscopy. J. Neurosurg. 2005, 102, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Popperl, G.; Gotz, C.; Rachinger, W.; Gildehaus, F.J.; Tonn, J.C.; Tatsch, K. Value of O-(2-[18F]fluoroethyl)- L-tyrosine PET for the diagnosis of recurrent glioma. Eur. J. Nucl. Med. Mol. Imaging 2004, 31, 1464–1470. [Google Scholar] [CrossRef] [PubMed]
- Stockhammer, F.; Misch, M.; Horn, P.; Koch, A.; Fonyuy, N.; Plotkin, M. Association of F18-fluoro-ethyl-tyrosin uptake and 5-aminolevulinic acid-induced fluorescence in gliomas. Acta Neurochir. 2009, 151, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Tscherpel, C.; Dunkl, V.; Ceccon, G.; Stoffels, G.; Judov, N.; Rapp, M.; Meyer, P.T.; Kops, E.R.; Ermert, J.; Fink, G.R.; et al. The use of O-(2-18F-fluoroethyl)-L-tyrosine PET in the diagnosis of gliomas located in the brainstem and spinal cord. Neuro-Oncology 2017, 19, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Floeth, F.W.; Sabel, M.; Stoffels, G.; Pauleit, D.; Hamacher, K.; Steiger, H.J.; Langen, K.J. Prognostic value of 18F-fluoroethyl-L-tyrosine PET and MRI in small nonspecific incidental brain lesions. J. Nucl. Med. 2008, 49, 730–737. [Google Scholar] [CrossRef]
- Suchorska, B.; Giese, A.; Biczok, A.; Unterrainer, M.; Weller, M.; Drexler, M.; Bartenstein, P.; Schuller, U.; Tonn, J.C.; Albert, N.L. Identification of time-to-peak on dynamic 18F-FET-PET as a prognostic marker specifically in IDH1/2 mutant diffuse astrocytoma. Neuro-Oncology 2018, 20, 279–288. [Google Scholar] [CrossRef]
- Vettermann, F.J.; Felsberg, J.; Reifenberger, G.; Hasselblatt, M.; Forbrig, R.; Berding, G.; la Fougere, C.; Galldiks, N.; Schittenhelm, J.; Weis, J.; et al. Characterization of Diffuse Gliomas With Histone H3-G34 Mutation by MRI and Dynamic 18F-FET PET. Clin. Nucl. Med. 2018, 43, 895–898. [Google Scholar] [CrossRef]
- Utriainen, M.; Komu, M.; Vuorinen, V.; Lehikoinen, P.; Sonninen, P.; Kurki, T.; Utriainen, T.; Roivainen, A.; Kalimo, H.; Minn, H. Evaluation of brain tumor metabolism with [11C]choline PET and 1H-MRS. J. Neuro-Oncol. 2003, 62, 329–338. [Google Scholar] [CrossRef]
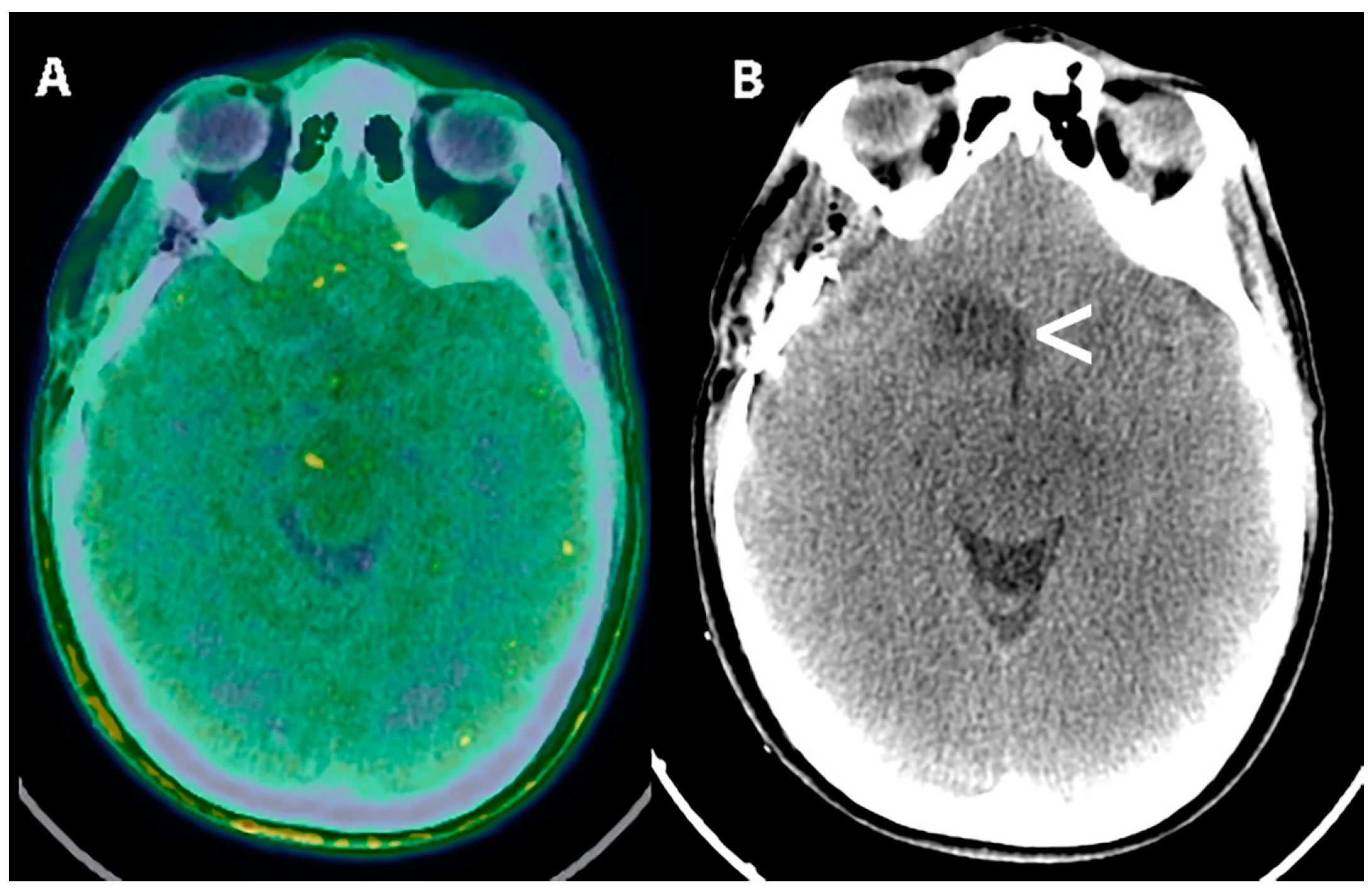
- Veldhuijzen van Zanten, S.E.M.; Sewing, A.C.P.; van Lingen, A.; Hoekstra, O.S.; Wesseling, P.; Meel, M.H.; van Vuurden, D.G.; Kaspers, G.J.L.; Hulleman, E.; Bugiani, M. Multiregional Tumor Drug-Uptake Imaging by PET and Microvascular Morphology in End-Stage Diffuse Intrinsic Pontine Glioma. J. Nucl. Med. 2018, 59, 612–615. [Google Scholar] [CrossRef]
- Friedland, R.P.; Mathis, C.A.; Budinger, T.F.; Moyer, B.R.; Rosen, M. Labeled choline and phosphorylcholine: Body distribution and brain autoradiography: Concise communication. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 1983, 24, 812–815. [Google Scholar]
- Beauregard, J.M.; Williams, S.G.; Degrado, T.R.; Roselt, P.; Hicks, R.J. Pilot comparison of F-fluorocholine and F-fluorodeoxyglucose PET/CT with conventional imaging in prostate cancer. J. Med Imaging Radiat. Oncol. 2010, 54, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Kwee, S.A.; DeGrado, T.R.; Talbot, J.N.; Gutman, F.; Coel, M.N. Cancer imaging with fluorine-18-labeled choline derivatives. Semin. Nucl. Med. 2007, 37, 420–428. [Google Scholar] [CrossRef] [PubMed]
- DeGrado, T.R.; Coleman, R.E.; Wang, S.; Baldwin, S.W.; Orr, M.D.; Robertson, C.N.; Polascik, T.J.; Price, D.T. Synthesis and evaluation of 18F-labeled choline as an oncologic tracer for positron emission tomography: Initial findings in prostate cancer. Cancer Res. 2001, 61, 110–117. [Google Scholar]
- Bansal, A.; Shuyan, W.; Hara, T.; Harris, R.A.; Degrado, T.R. Biodisposition and metabolism of [(18)F]fluorocholine in 9L glioma cells and 9L glioma-bearing fisher rats. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 1192–1203. [Google Scholar] [CrossRef]
- Hara, T.; Kosaka, N.; Kishi, H. Development of (18)F-fluoroethylcholine for cancer imaging with PET: Synthesis, biochemistry, and prostate cancer imaging. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2002, 43, 187–199. [Google Scholar]
- George, T.P.; Morash, S.C.; Cook, H.W.; Byers, D.M.; Palmer, F.B.; Spence, M.W. Phosphatidylcholine biosynthesis in cultured glioma cells: Evidence for channeling of intermediates. Biochim. et Biophys. Acta 1989, 1004, 283–291. [Google Scholar] [CrossRef]
- Hara, T.; Kosaka, N.; Shinoura, N.; Kondo, T. PET imaging of brain tumor with [methyl-11C]choline. J. Nucl. Med. 1997, 38, 842–847. [Google Scholar]
- Fulham, M.J.; Bizzi, A.; Dietz, M.J.; Shih, H.H.; Raman, R.; Sobering, G.S.; Frank, J.A.; Dwyer, A.J.; Alger, J.R.; Di Chiro, G. Mapping of brain tumor metabolites with proton MR spectroscopic imaging: Clinical relevance. Radiology 1992, 185, 675–686. [Google Scholar] [CrossRef]
- Epelbaum, J. Somatostatin in the central nervous system: Physiology and pathological modifications. Prog. Neurobiol. 1986, 27, 63–100. [Google Scholar] [CrossRef]
- Pashankar, F.D.; O’Dorisio, M.S.; Menda, Y. MIBG and somatostatin receptor analogs in children: Current concepts on diagnostic and therapeutic use. J. Nucl. Med. 2005, 46, 55s–61s. [Google Scholar] [PubMed]
- Filippi, L.; Valentini, F.B.; Gossetti, B.; Gossetti, F.; De Vincentis, G.; Scopinaro, F.; Massa, R. Intraoperative gamma probe detection of head and neck paragangliomas with 111In-pentetreotide: A pilot study. Tumori 2005, 91, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Schillaci, O. Somatostatin receptor imaging in patients with neuroendocrine tumors: Not only SPECT? J. Nucl. Med. 2007, 48, 498–500. [Google Scholar] [CrossRef] [PubMed]
- Ugur, O.; Kothari, P.J.; Finn, R.D.; Zanzonico, P.; Ruan, S.; Guenther, I.; Maecke, H.R.; Larson, S.M. Ga-66 labeled somatostatin analogue DOTA-DPhe1-Tyr3-octreotide as a potential agent for positron emission tomography imaging and receptor mediated internal radiotherapy of somatostatin receptor positive tumors. Nucl. Med. Biol. 2002, 29, 147–157. [Google Scholar] [CrossRef]
- Filippi, L.; Scopinaro, F.; Pelle, G.; Cianni, R.; Salvatori, R.; Schillaci, O.; Bagni, O. Molecular response assessed by (68)Ga-DOTANOC and survival after (90)Y microsphere therapy in patients with liver metastases from neuroendocrine tumours. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 432–440. [Google Scholar] [CrossRef]
- Kilian, K. 68Ga-DOTA and analogs: Current status and future perspectives. Rep. Pract. Oncol. Radiother. 2014, 19, S13–S21. [Google Scholar] [CrossRef]
- Ambrosini, V.; Fanti, S. 68Ga-DOTA-peptides in the diagnosis of NET. PET Clin. 2014, 9, 37–42. [Google Scholar] [CrossRef]
- Alexander, N.; Vali, R.; Ahmadzadehfar, H.; Shammas, A.; Baruchel, S. Review: The Role of Radiolabeled DOTA-Conjugated Peptides for Imaging and Treatment of Childhood Neuroblastoma. Curr. Radiopharm. 2018, 11, 14–21. [Google Scholar] [CrossRef]
- Hartmann, H.; Zophel, K.; Freudenberg, R.; Oehme, L.; Andreeff, M.; Wunderlich, G.; Eisenhofer, G.; Kotzerke, J. Radiation exposure of patients during 68Ga-DOTATOC PET/CT examinations. Nukl. Nucl. Med. 2009, 48, 201–207. [Google Scholar] [CrossRef]
- Filippi, L.; Santoni, R.; Nicoli, P.; Danieli, R.; Schillaci, O. Intracranial tumors after radiation therapy: Role of 99mTc-tetrofosmin SPECT/CT with a hybrid camera. Cancer Biother. Radiopharm. 2009, 24, 229–235. [Google Scholar] [CrossRef]
- Attwell, D.; Laughlin, S.B. An energy budget for signaling in the grey matter of the brain. J. Cereb. Blood Flow Metab. 2001, 21, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, S.J.; Lind, T.; Antoch, G.; Bockisch, A. False-positive FDG PET uptake–the role of PET/CT. Eur. Radiol. 2006, 16, 1054–1065. [Google Scholar] [CrossRef] [PubMed]
- Maffioli, L.; Steens, J.; Pauwels, E.; Bombardieri, E. Applications of 99mTc-sestamibi in oncology. Tumori 1996, 82, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Delmon-Moingeon, L.I.; Piwnica-Worms, D.; Van den Abbeele, A.D.; Holman, B.L.; Davison, A.; Jones, A.G. Uptake of the cation hexakis(2-methoxyisobutylisonitrile)-technetium-99m by human carcinoma cell lines in vitro. Cancer Res. 1990, 50, 2198–2202. [Google Scholar]
- Leung, K. L-3,4-Dihydroxy-6-[18F]fluorophenylalanine. 2005 Mar 21 [Updated 2011 Dec 21]. In Molecular Imaging and Contrast Agent Database (MICAD) [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2004–2013. Available online: https://www.ncbi.nlm.nih.gov/books/NBK23043/ (accessed on 24 October 2019).
- Heiss, W.D.; Wienhard, K.; Wagner, R.; Lanfermann, H.; Thiel, A.; Herholz, K.; Pietrzyk, U. F-Dopa as an amino acid tracer to detect brain tumors. J. Nucl. Med. 1996, 37, 1180–1182. [Google Scholar]
- Youland, R.S.; Kitange, G.J.; Peterson, T.E.; Pafundi, D.H.; Ramiscal, J.A.; Pokorny, J.L.; Giannini, C.; Laack, N.N.; Parney, I.F.; Lowe, V.J.; et al. The role of LAT1 in (18)F-DOPA uptake in malignant gliomas. J. Neuro-Oncol. 2013, 111, 11–18. [Google Scholar] [CrossRef]
- Saier, M.H., Jr.; Daniels, G.A.; Boerner, P.; Lin, J. Neutral amino acid transport systems in animal cells: Potential targets of oncogene action and regulators of cellular growth. J. Membr. Biol. 1988, 104, 1–20. [Google Scholar] [CrossRef]
- Langen, K.J.; Jarosch, M.; Muhlensiepen, H.; Hamacher, K.; Broer, S.; Jansen, P.; Zilles, K.; Coenen, H.H. Comparison of fluorotyrosines and methionine uptake in F98 rat gliomas. Nucl. Med. Biol. 2003, 30, 501–508. [Google Scholar] [CrossRef]
- Leung, K. O-(2-[18F]Fluoroethyl)-L-tyrosine. 2005 Sep 15 [Updated 2011 Dec 6]. In Molecular Imaging and Contrast Agent Database (MICAD) [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2004-2013. Available online: https://www.ncbi.nlm.nih.gov/books/NBK23454/ (accessed on 24 October 2019).
- Sherley, J.L.; Kelly, T.J. Regulation of human thymidine kinase during the cell cycle. J. Biol. Chem. 1988, 263, 8350–8358. [Google Scholar]
- Chiaravalloti, A.; Esposito, V.; Ursini, F.; Di Giorgio, E.; Zinzi, M.; Calabria, F.; Cimini, A.; Schillaci, O. Overall survival and progression-free survival in patients with primary brain tumors after treatment: Is the outcome of [(18)F] FDOPA PET a prognostic factor in these patients? Ann. Nucl. Med. 2019, 33, 471–480. [Google Scholar] [CrossRef]
- Villani, V.; Carapella, C.M.; Chiaravalloti, A.; Terrenato, I.; Piludu, F.; Vidiri, A.; Schillaci, O.; Floris, R.; Marzi, S.; Fabi, A.; et al. The Role of PET [18F]FDOPA in Evaluating Low-grade Glioma. Anticancer Res. 2015, 35, 5117–5122. [Google Scholar] [PubMed]
- Chiaravalloti, A.; Rubello, D.; Chondrogiannis, S.; Giammarile, F.; Colletti, P.M.; Schillaci, O. Low-dose CT and contrast-medium CT in hybrid PET/CT systems for oncologic patients. Nucl. Med. Commun. 2015, 36, 867–870. [Google Scholar] [CrossRef] [PubMed]
- Grant, F.; Sexton-Stallone, B.; Falone, A.; Brown, D.; Zurakowski, D.; Onar, A.; Dunkel, I.; Poussaint, T.; Fahey, F.; Treves, S.T. [18F] FLT PET predicts cellular proliferation in pediatric brain tumors. J. Nucl. Med. 2019, 60, 156. [Google Scholar]
- Anthony, C.; Mladkova-Suchy, N.; Adamson, D.C. The evolving role of antiangiogenic therapies in glioblastoma multiforme: Current clinical significance and future potential. Expert Opin. Investig. Drugs 2019, 28, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Levenbaum, E.; Ellika, S.; Korones, D.N. Bevacizumab in treating the cystic components of pediatric low-grade gliomas: A report of four patients. Pediatric Blood Cancer 2019, 66, e27917. [Google Scholar] [CrossRef] [PubMed]
- van Es, S.C.; Brouwers, A.H.; Mahesh, S.V.K.; Leliveld-Kors, A.M.; de Jong, I.J.; Lub-de Hooge, M.N.; de Vries, E.G.E.; Gietema, J.A.; Oosting, S.F. (89)Zr-Bevacizumab PET: Potential Early Indicator of Everolimus Efficacy in Patients with Metastatic Renal Cell Carcinoma. J. Nucl. Med. 2017, 58, 905–910. [Google Scholar] [CrossRef]
- Jansen, M.H.; Veldhuijzen van Zanten, S.E.M.; van Vuurden, D.G.; Huisman, M.C.; Vugts, D.J.; Hoekstra, O.S.; van Dongen, G.A.; Kaspers, G.L. Molecular Drug Imaging: (89)Zr-Bevacizumab PET in Children with Diffuse Intrinsic Pontine Glioma. J. Nucl. Med. 2017, 58, 711–716. [Google Scholar] [CrossRef]
- Darvin, P.; Toor, S.M.; Sasidharan Nair, V.; Elkord, E. Immune checkpoint and potential biomarkers. Exp. Mol. Med. 2018, 50, 165. [Google Scholar] [CrossRef]
- Fried, I.; Lossos, A.; Ben Ami, T.; Dvir, R.; Toledano, H.; Ben Arush, M.W.; Postovski, S.; Abu Kuidar, A.; Yalon, M.; Weintraub, M.; et al. Preliminary results of immune modulating antibody MDV9300 (pidilizumab) treatment in children with diffuse intrinsic pontine glioma. J. Neuro-Oncol. 2018, 136, 189–195. [Google Scholar] [CrossRef]
- Wierstra, P.; Sandker, G.; Aarntzen, E.; Gotthardt, M.; Adema, G.; Bussink, J.; Raave, R.; Heskamp, S. Tracers for non-invasive radionuclide imaging of immune checkpoint expression in cancer. EJNMMI Radiopharm. Chem. 2019, 4, 29. [Google Scholar] [CrossRef]





| Authors | Year | Radiopharmaceutical | Type of Study | Setting | Patients | Comment | Type of Population |
|---|---|---|---|---|---|---|---|
| O’ Tuama et al. [12] | 1993 | [99mTc] MIBI | Case series | Pre-operative imaging Restaging post-therapy | N = 19 | SPECT with MIBI was able to detect primary brain tumors, especially gliomas, but lesions in the para-ventricular spaces are of difficult visualization. | Pediatric |
| Kirton et al. [13] | 2002 | ([99mTc] MIBI | Case series | Pre-operative imaging Monitoring after therapy | N = 20 | SPECT with MIBI correlates with MRI in astrocytomas, but present reduced sensitivity in disclosing some histotypes such as medulloblastoma and optic glioma. MIBI was able to disclose recurrence earlier than MRI. | Pediatric |
| Barai et al. [14] | 2003 | [99mTc]-Tetrofosmin | Case series | Restaging post radiotherapy | N = 12 | SPECT with tetrofosmin was not accurate for the detection of recurrent tumors in the posterior cranial fossa. | Mixed |
| Ohtani et al. [15] | 2001 | [11C] CH | Prospective, single-center | Pre-operative imaging | N = 3 | PET-CT with 11C-choline performed better than 18F-FDG for the detection of brain lesions but failed in discriminating low-grade gliomas and non-neoplastic lesions. | Mixed |
| Fraioli et al. [16] | 2015 | [18F] FEC | Prospective, single-center | Pre-operative imaging Restaging post-therapy | N = 12 | PET-MRI with a hybrid scanner may represent a useful diagnostic tool in pediatric astrocytomas. An inverse correlation trend was found between SUVmax and ADC. | Pediatric |
| Tsouana et al. [17] | 2015 | [18F] FEC | Case series | Pre-operative imaging Restaging post-therapy | N = 4 | PET-MRI with 18F-choline was able to correctly characterize intracranial non-germinomatous germ cell tumors and monitor the response to chemotherapy. | Adolescent |
| Muller et al. [18] | 1998 | [111In] pentetreotide | Case series | Pre-operative imaging Restaging post-therapy | N = 16 | Somatostatin receptor imaging with 111In-pentetreotide identified medulloblastoma before surgery and residual viable tissue after therapy. | Pediatric |
| Frühwald et al. [19] | 2004 | [111In] pentetreotide | Case series | Restaging post-therapy | N = 13 | Somatostatin receptor imaging with 111In-pentetreotide was able to detect residual disease or relapse in selected pediatric brain tumors. | Pediatric |
| Abongwa et al. [20] | 2017 | [68Ga]DOTATOC | Prospective Clinical Trial | Safety Study | N = 2 | Safety and accuracy of 68Ga-DOTATOC PET/CT in children and young adults with solid tumor | Mixed |
| Arunraj et al. [21] | 2018 | [68Ga]DOTANOC | Case report | Restaging post therapy | N = 1 | 68Ga-DOTANOC PET is able to detect medulloblastoma recurrence. | Adolescent |
| Menda et al. [22] | 2010 | [90Y]DOTANOC | Phase I study | Safety and efficacy of PRRT | N = 17 | 90Y-DOTANOC presented a favorable safety profile and an overall response rate of 76% in refractory children tumors overexpressing somatostatin receptors. | Mixed |
| Dunkl et al. [6] | 2015 | [18F] FET | Case series | Pre-operative imaging Restaging post-therapy | N = 49 | PET with FET was helpful in decision making in PBT. | Pediatric |
| Misch et al. [7] | 2015 | [18F] FET | Case series | Pre-operative imaging PET guided surgical biopsy and resection | N = 26 | Biopsy guided by PET with FET increased the accuracy of histological diagnosis with decent specificity and high sensitivity | Pediatric |
| Law et al. [9] | 2019 | [18F] FET; ([11C]MET); ([18F] FDOPA) | Practice guidelines | Pre-operative imaging Monitoring after therapy Restaging post-therapy | Guidelines aimed to assist nuclear medicine practitioners in recommending, performing, interpreting and reporting the results of brain PET with MET, FET, and FDOPA. | - | |
| Kim et al. [23] | 2010 | [18F] FDG; [11C]MET | Review article | Pre-operative imaging | The usefulness of PET and PET/CT in the evaluation of pediatric pediatric brain tumors. | - | |
| Uslu et al. [24] | 2015 | [18F] FDG | Review article | Pre-operative imaging | The usefulness of FDG PET/CT in the evaluation of pediatric malignancies and the role of PET/MR in the reduction of radiation exposure. | - | |
| Williams et al. [25] | 2008 | [18F] FDG | Case series | Pre-operative imaging Monitoring after therapy | N = 12 | 3D PET for the estimation of metabolically active tumor burden; possible prognostic value after tumor grade is determined | Pediatric |
| Zukotynski et al. [26] | 2011 | [18F] FDG | Case series | Pre-operative imaging Monitoring after therapy | N = 40 | Prognostic value of FDG PET in PBT. | Pediatric |
| Kruer et al. [27] | 2009 | [18F] FDG | Case series | Pre-operative imaging Monitoring after therapy | N = 46 | The role of PET in high-risk Low-grade astrocytomas. | Pediatric |
| Kwon et al. [28] | 2006 | [18F] FDG | Case series | Pre-operative imaging Monitoring after therapy | N = 20 | The role of FDG-PET in differentiating between anaplastic astrocytoma and glioblastomas among high-grade tumors | Pediatric |
| O’ Tuama et al. [29] | 1990 | [11C]MET | Case series | Pre-operative imaging Restaging post-therapy | N = 13 | The role of PET with MET in PBT: differential diagnosis between tumor recurrence and cerebral radiation injury. | Pediatric |
| Utriainen et al. [30] | 2002 | [18F] FDG; [11C]MET | Case series | Pre-operative imaging Restaging post-therapy | N = 27 | Association between FDG and MET uptake and malignancy grade in PBT. | Pediatric |
| Pirotte et al. [31] | 2007 | [18F] FDG; [11C]MET | Case series | Pre-operative imaging Restaging post-therapy | N = 126 | The role of PET imaging in the surgical management of PBT at the diagnostic, surgical, and post-operative steps | Pediatric |
| Lucas at al. [32] | 2017 | [11C]MET | Case series | Pre-operative imaging Restaging post-therapy | N = 31 | The role of MET PET in PBT at increased risk for recurrence | Pediatric |
| Morana et al. [33] | 2015 | [18F] FDOPA | Retrospective comparative study | Pre-operative imaging Monitoring after therapy | N = 27 | The role of FDOPA in discriminating low-grade from high-grade gliomas | Pediatric |
| Morana et al. [34] | 2017 | [18F] FDOPA | Retrospective study | Pre-operative imaging Monitoring after therapy | N = 26 | Combination of MRI and FDOPA PET show the highest predictive power for prognosticating PBT progression | Pediatric |
| Morana et al. [35] | 2016 | [18F] FDOPA | Retrospective study | Pre-operative imaging Monitoring after therapy | N = 28 | The technical paper aimed to investigate the physiological striatal FDOPA uptake in the evaluation of basal ganglia involvement of PBT in PET/TC. | Pediatric |
| Hutterer et al. [36] | 2015 | [18F] FDG; [18F] FET; [11C]MET; [18F] FDOPA | Review article | Pre-operative imaging Monitoring after therapy | Paper aimed to investigate multimodal imaging that combines standard and advanced MRI with amino acid PET imaging to detect drug susceptibility or resistance of PBT | ||
| Morana et al. [37] | 2013 | [18F] FDOPA | Case report | Pre-operative imaging Monitoring after therapy | N = 1 | The role of FDOPA PET in distinguishing tumor pseudoresponse and progression. | Pediatric |
| Gauvain et al. [38] | 2018 | [18F] FDOPA | Case series | Pre-operative imaging Monitoring after therapy | N = 6 | The role of FDOPA PET/MRI in the early prediction of therapy response at 3 months | Pediatric |
| Pauleit et al. [39] | 2008 | [18F] FDG; [18F] FET | Comparative study | Pre-operative imaging Monitoring after therapy | N = 52 | FET PET is superior to FDG for biopsy guidance and treatment planning of cerebral gliomas. | Adult |
| Plotkin et al. [40] | 2010 | [18F] FDG; [18F] FET | Comparative study | Pre-operative imaging Monitoring after therapy | N = 15 | FET PET is superior to FDG for biopsy planning in non-contrast-enhancing PBT. | Adult |
| Pauleit et al. [41] | 2005 | [18F] FET | Case series | Pre-operative imaging Monitoring after therapy | N =31 | The combined use of MRI and FET PET in patients with cerebral gliomas improves the identification of cancer recurrence | Adult |
| Floeth et al. [42] | 2005 | [18F] FET | Case series | Pre-operative imaging Monitoring after therapy | N =50 | The role of FET-PET and MR spectroscopy in patients with intracerebral lesions: efficacy of targeted biopsies. | Mixed |
| Pöpperl et al. [43] | 2014 | [18F] FET | Case series | Pre-operative imaging Monitoring after therapy | N =53 | The role of FET PET reliably in distinguishing between post-therapeutic benign lesions and tumor recurrence after treatment in low and high-grade gliomas. | Mixed |
| Stockhammer et al. [44] | 2009 | [18F] FET | Case series | Pre-operative imaging | N =13 | FET-PET provides useful information for planning glioma resection. | Adult |
| Tscherpel at al. [45] | 2017 | [18F] FET | Case series | Pre-operative imaging | N = 36 | Added-value of FET PET in the brainstem and spinal cord glioma, particularly when MRI is equivocal | Mixed |
| Floeth at al. [46] | 2008 | [18F] FET | Prospective clinical trial | Pre-operative imaging Monitoring after therapy | N = 21 | The prognostic role of FET uptake for the development of a high-grade glioma | Mixed |
| Suchorska et al. [47] | 2018 | [18F] FET | Case series | Pre-operative imaging Monitoring after therapy | N = 300 | Differences in FET uptake patterns in subgroups of IDH1/2 mutant-1p/19q non-codel gliomas | Mixed |
| Vettermann at al. [48] | 2018 | [18F] FET | Case series | Pre-operative imaging Monitoring after therapy | N = 8 | Paper on FET PET uptake patterns in high-grade glioma with H3-G34-mutation. | Mixed |
| Utriainen et al. [49] | 2003 | [11C] CH | Case series | Pre-operative imaging Monitoring after therapy | N = 12 | 11C-choline PET uptake patterns differ according to the proliferative activity of tumors | Adult |
| Fraioli at al. [16] | 2015 | [18F] FEC | Case series | Pre-operative imaging Monitoring after therapy | N = 12 | Coupled imaging of 11C-choline and MRI in children with astrocytic tumors | Pediatric |
| Veldhuijzen van Zanten et al. [50] | 2018 | [89Zr] Bevacizumab | Case report | Pre-operative imaging | N = 1 | Correlation between tracer uptake and tumor’s histochemistry at post mortem examination | Pediatric |
| Molecular Imaging Probe | Advantages | Drawbacks |
|---|---|---|
| [11C] choline | High uptake in gliomas. | [11C] short half-life |
| High uptake in choroid plexus | ||
| [18F] FEC [18F] FCH | High uptake in brain tumors. The adequately long half-life of the [18F] adionuclide | High uptake in choroid plexus |
| [68Ga]-DOTATOC [68Ga]-DOTANOC [68Ga]-DOTATE | In vivo detection of receptorial status. Potential therapeutic implications if labeled with [177Lu] or [90Y] | Need for on-site generator Sensitivity limited to brain tumors expressing somatostatin receptors (i.e., medulloblastoma, pineoblastoma, etc.) |
| [99mTc] MIBI [99mTc] Tetrofosmin | Widespread availability in the majority of the nuclear medicine centers | Poor spatial resolution. High uptake in the choroid plexus. Poor diagnostic accuracy for tumors of the posterior cranial fossa. |
| [18F] FDG | High uptake of [18F] FDG may reflect a poor differentiation of the tumor. | High Physiological uptake of [18F] FDG in the brain limits the tumor evaluation and detection. Moreover, [18F] FDG may show variable uptake by inflammatory lesions. |
| [18F] FDOPA [18F] FLT [11C] MET | Amino-acid tracers show a reduced uptake in the normal brain cortex, thus providing a better characterization of the tumor. Amino-acid uptake in pediatric brain tumors is correlated with tumor grade. High potential in defining the outcome in pediatric brain tumors. | Short Half-life of [11C] MET (20 min.); physiological uptake of [18F] FDOPA in basal ganglia may limit the evaluation of striatal involvement in brain tumors. Reports on pediatric brain tumors are limited. |
| [18F] FLT | Tumor uptake of [18F] FLT correlated significantly with the Ki-67 labeling index. | Reports on pediatric brain tumors are very limited. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiaravalloti, A.; Filippi, L.; Ricci, M.; Cimini, A.; Schillaci, O. Molecular Imaging in Pediatric Brain Tumors. Cancers 2019, 11, 1853. https://doi.org/10.3390/cancers11121853
Chiaravalloti A, Filippi L, Ricci M, Cimini A, Schillaci O. Molecular Imaging in Pediatric Brain Tumors. Cancers. 2019; 11(12):1853. https://doi.org/10.3390/cancers11121853
Chicago/Turabian StyleChiaravalloti, Agostino, Luca Filippi, Maria Ricci, Andrea Cimini, and Orazio Schillaci. 2019. "Molecular Imaging in Pediatric Brain Tumors" Cancers 11, no. 12: 1853. https://doi.org/10.3390/cancers11121853
APA StyleChiaravalloti, A., Filippi, L., Ricci, M., Cimini, A., & Schillaci, O. (2019). Molecular Imaging in Pediatric Brain Tumors. Cancers, 11(12), 1853. https://doi.org/10.3390/cancers11121853







