Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes
Abstract
:1. Introduction
- (i)
- The traditional pathway is based on APC and KRAS mutations (by CIN alterations). These neoplasms usually involve the left colon.
- (ii)
- The alternative pathway is characterized by a CIMP-low phenotype, predominant KRAS and occasional BRAF mutations, with no CIN. The prognosis of these CRC is aggressive.
- (iii)
- The serrated pathway is characterized by BRAF mutations and epigenomic instability (CIMP-high). These lesions are located mainly in the right colon with MSI morphology (mucinous, medullary and tumours with intraepithelial lymphocytes) or MSS with a serrated morphology (eosinophilic cytoplasm, epithelial serration and tufts and vescicular basal nuclei) [1,3].
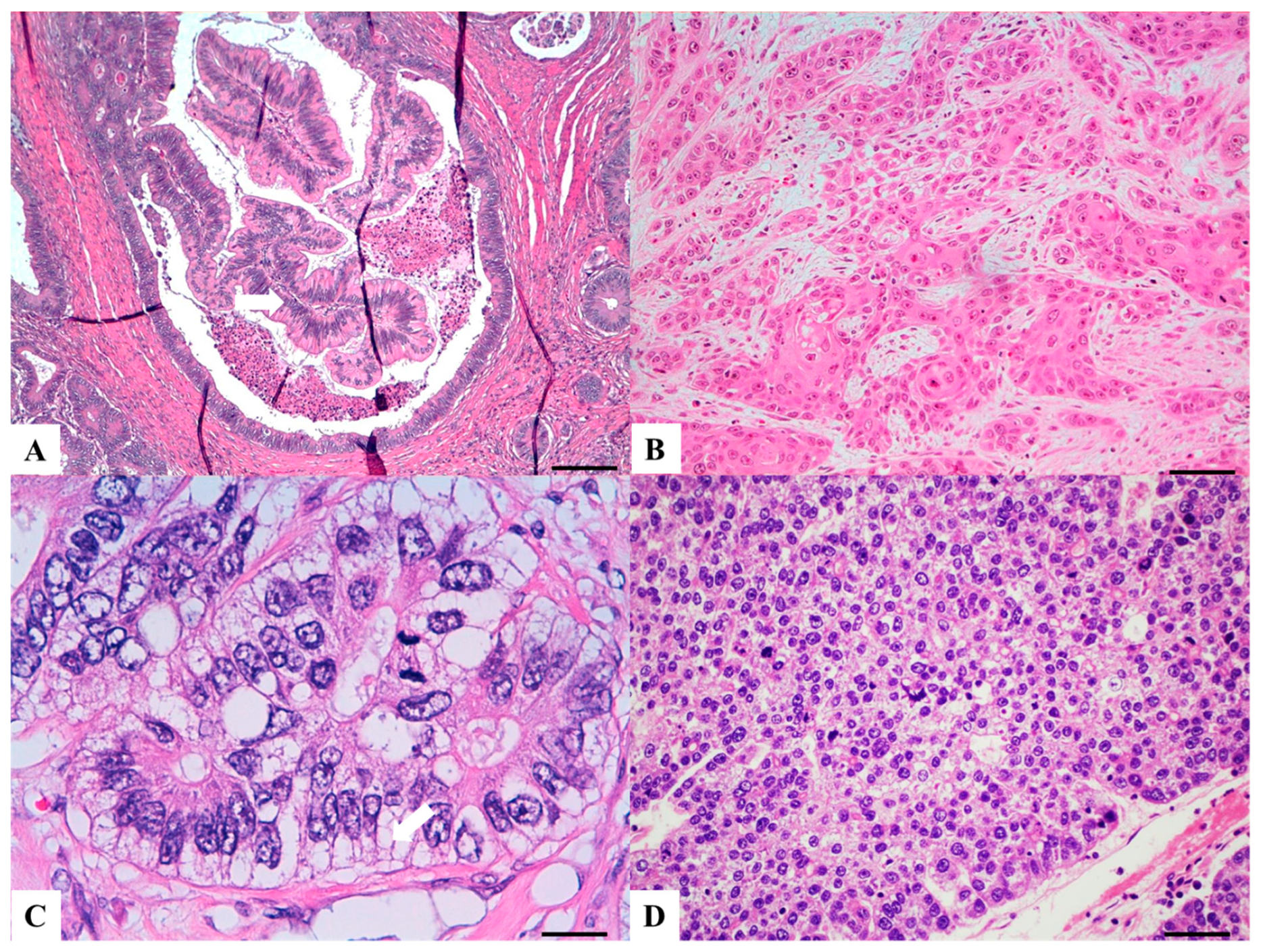
2. Serrated Adenocarcinoma (SA)
2.1. Background
2.2. Clinical Presentation
2.3. Sidedness
2.4. Morphologic Diagnostic Criteria
2.5. Molecular Alterations
2.6. Prognosis
3. Mucinous (Colloid) Adenocarcinoma (MA)
3.1. Background
3.2. Clinical Presentation
3.3. Sidedness
3.4. Morphologic Diagnostic Criteria
3.5. Molecular Genotype
3.6. Prognosis
4. Signet Ring Cell Carcinoma (SRC)
4.1. Background
4.2. Clinical Presentation
4.3. Sidedness
4.4. Morphologic Diagnostic Criteria
4.5. Molecular Genotype
4.6. Prognosis
5. Medullary Carcinoma (MC)
5.1. Background
5.2. Clinical Presentation
5.3. Sidedness
5.4. Morphologic Diagnostic Criteria
5.5. Molecular Genotype
5.6. Prognosis
6. Lymphoepitelioma-Like Carcinoma (LELC)
6.1. Background
6.2. Clinical Presentation
6.3. Sidedness
6.4. Morphologic Diagnostic Criteria
6.5. Molecular Genotype
6.6. Prognosis
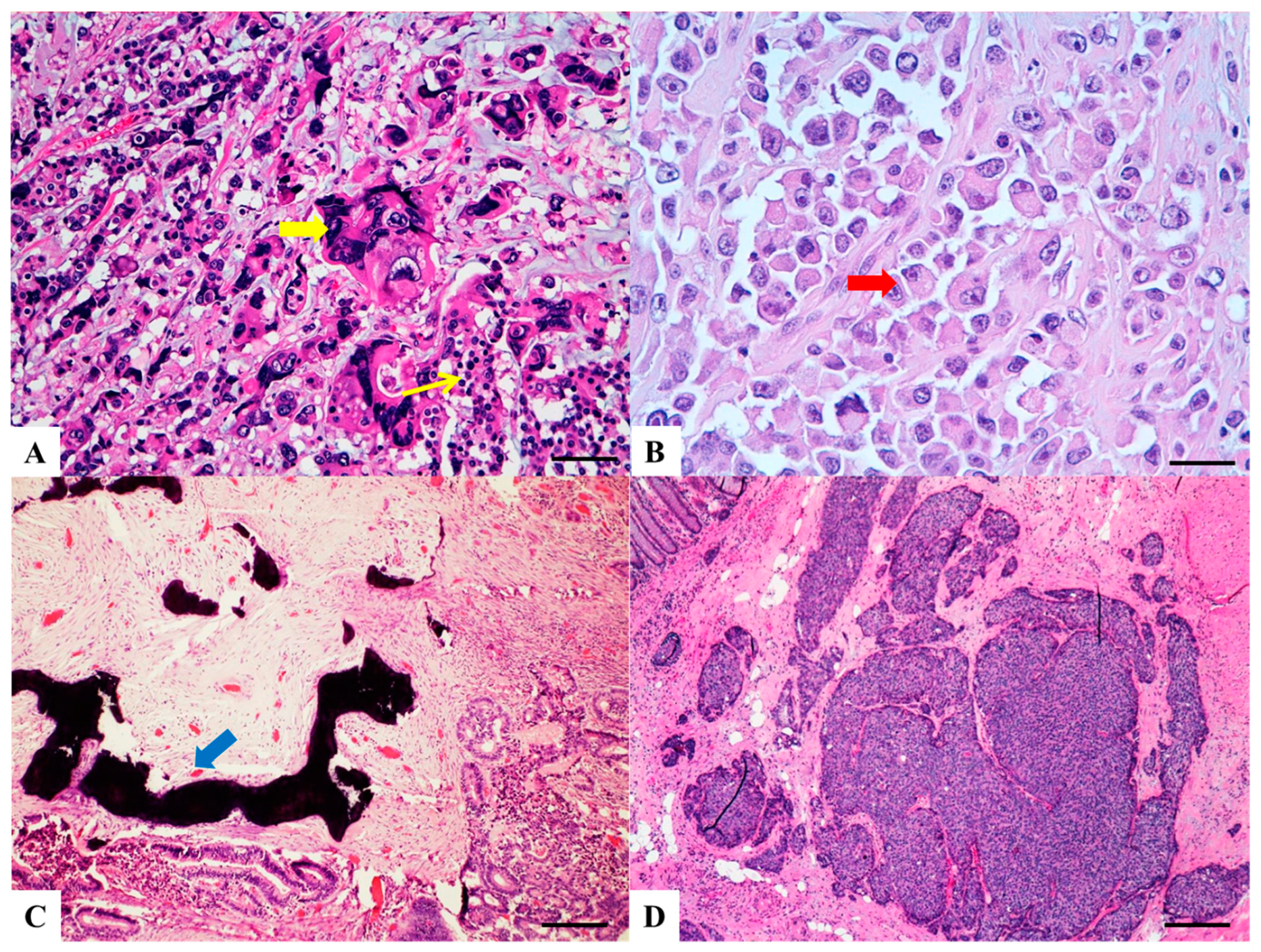
7. Cribriform Comedo-Type Carcinoma (CC-Type)
7.1. Background
7.2. Clinical Presentation
7.3. Sidedness
7.4. Morphologic Diagnostic Criteria
7.5. Molecular Genotype
7.6. Prognosis
8. Micropapillary Adenocarcinoma (MPA)
8.1. Background
8.2. Clinical Presentation
8.3. Sidedness
8.4. Morphology
8.5. Molecular Genotype
8.6. Prognosis
9. Low Grade Tubuloglandular Adenocarcinoma (LGTGA)
9.1. Background
9.2. Clinical Presentation
9.3. Sidedness
9.4. Morphologic Diagnostic Criteria
9.5. Molecular Genotype
9.6. Prognosis
10. Villous Carcinoma (VC)
10.1. Background
10.2. Clinical Presentation
10.3. Sidedness
10.4. Morphologic Diagnostic Criteria
10.5. Molecular Genotype
10.6. Prognosis
11. Squamous (SCC) and Adenosquamous Carcinoma (ASC)
11.1. Background
11.2. Clinical Presentation
11.3. Sidedness
11.4. Morphologic Diagnostic Criteria
11.5. Molecular Genotype
11.6. Prognosis
12. Primary Clear Cell Carcinoma (CCC)
12.1. Background
12.2. Clinical Presentation
12.3. Sidedness
12.4. Morphologic Diagnostic Criteria
12.5. Molecular Genotype
12.6. Prognosis
13. Hepatoid Adenocarcinoma (HepAC)
13.1. Background
13.2. Clinical Presentation
13.3. Sidedness
13.4. Morphologic Diagnostic Criteria
13.5. Molecular Genotype
13.6. Prognosis
14. Primary Colorectal Choriocarcinoma (pChC)
14.1. Background
14.2. Clinical Presentation
14.3. Sidedness
14.4. Morphologic Diagnostic Criteria
14.5. Molecular Genotype
14.6. Prognosis
15. Rhabdoid Colorectal Carcinoma (RhC)
15.1. Background
15.2. Clinical Presentation
15.3. Sidedness
15.4. Morphologic Diagnostic Criteria
15.5. Molecular Genotype
15.6. Prognosis
16. Carcinoma with Osseous Metaplasia (COM)
16.1. Background
16.2. Clinical Presentation
16.3. Sidedness
16.4. Morphologic Diagnostic Criteria
16.5. Molecular Genotype
16.6. Prognosis
17. Spindle Cell Carcinoma (SpCC)
17.1. Background
17.2. Clinical Presentation
17.3. Sidedness
17.4. Morphologic Diagnostic Criteria
17.5. Molecular Genotype
17.6. Prognosis
18. Pleomorphic Carcinoma (PlC)
18.1. Background
18.2. Clinical Presentation
18.3. Sidedness
18.4. Morphologic Diagnostic Criteria
18.5. Molecular Genotype
18.6. Prognosis
19. Undifferentiated Carcinoma (UC)
19.1. Background
19.2. Clinical Presentation
19.3. Sidedness
19.4. Morphologic Diagnostic Criteria
19.5. Molecular Genotype
19.6. Prognosis
20. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Remo, A.; Pancione, M.; Zanella, C.; Vendraminelli, R. Molecular pathology of colorectal carcinoma. A systematic review centred on the new role of the pathologist. Pathologica 2012, 104, 432–441. [Google Scholar] [PubMed]
- Pancione, M.; Giordano, G.; Remo, A.; Febbraro, A.; Sabatino, L.; Manfrin, E.; Ceccarelli, M.; Colantuoni, V. Immune escape mechanisms in colorectal cancer pathogenesis and liver metastasis. J. Immunol. Res. 2014, 2014, 686879. [Google Scholar] [CrossRef]
- Pancione, M.; Remo, A.; Colantuoni, V. Genetic and epigenetic events generate multiple pathways in colorectal cancer progression. Pathol. Res. Int. 2012, 2012, 509348. [Google Scholar] [CrossRef] [PubMed]
- Shih, I.M.; Wang, T.L.; Traverso, G.; Romans, K.; Hamilton, S.R.; Ben-Sasson, S.; Kinzler, K.W.; Vogelstein, B. Top-down morphogenesis of colorectal tumors. Proc. Natl. Acad. Sci. USA 2001, 98, 2640–2645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, J.; Jenkins, M.; Parry, S.; Young, B.; Nancarrow, D.; English, D.; Giles, G.; Jass, J. Serrated pathway colorectal cancer in the population: Genetic consideration. Gut 2007, 56, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
- Hurt, C.; Ramaraj, R.; Farr, A.; Morgan, M.; Williams, N.; Philips, C.J.; Williams, G.T.; Gardner, G.; Porter, C.; Sampson, J.; et al. CONSCOP Clinical Research Consortium. Feasibility and economic assessment of chromocolonoscopy for detection of proximal serrated neoplasia within a population-based colorectal cancer screening programme (CONSCOP): An open-label, randomised controlled non-inferiority trial. Lancet Gastroenterol. Hepatol. 2019, 4, 364–375. [Google Scholar]
- Missiaglia, E.; Jacobs, B.; D’Ario, G.; Di Narzo, A.F.; Soneson, C.; Budinska, E.; Popovici, V.; Vecchione, L.; Gerster, S.; Yan, P.; et al. Distal and proximal colon cancers differ in terms of molecular, pathological, and clinical features. Ann. Oncol. 2014, 25, 1995–2001. [Google Scholar] [CrossRef] [PubMed]
- Jass, J.R.; Smith, M. Sialic acid and epithelial differentiation in colorectal polyps and cancer—A morphological, mucin and lectinhistochemical study. Pathology 1992, 24, 233–242. [Google Scholar] [CrossRef]
- Mäkinen, M.J.; George, S.M.; Jernvall, P.; Mäkelä, J.; Vihko, P.; Karttunen, T.J. Colorectal carcinoma associated with serrated adenoma—Prevalence, histological features, and prognosis. J. Pathol. 2001, 193, 286–294. [Google Scholar] [CrossRef]
- García-Solano, J.; Pérez-Guillermo, M.; Conesa-Zamora, P.; Acosta-Ortega, J.; Trujillo-Santos, J.; Cerezuela-Fuentes, P.; Mäkinen, M.J. Clinicopathologic study of 85 colorectal serrated adenocarcinomas: Further insights into the full recognition of a new subset of colorectal carcinoma. Hum. Pathol. 2010, 41, 1359–1368. [Google Scholar] [CrossRef]
- Stefanius, K.; Ylitalo, L.; Tuomisto, A.; Kuivila, R.; Kantola, T.; Sirniö, P.; Karttunen, T.J.; Mäkinen, M.J. Frequent mutations of KRAS in addition to BRAF in colorectal serrated adenocarcinoma. Histopathology 2011, 58, 679–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuppurainen, K.; Mäkinen, J.M.; Junttila, O.; Liakka, A.; Kyllönen, A.P.; Tuominen, H.; Karttunen, T.J.; Mäkinen, M.J. Morphology and microsatellite instability in sporadic serrated and non-serrated colorectal cancer. J. Pathol. 2005, 207, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Laiho, P.; Kokko, A.; Vanharanta, S.; Salovaara, R.; Sammalkorpi, H.; Järvinen, H.; Mecklin, J.P.; Karttunen, T.J.; Tuppurainen, K.; Davalos, V.; et al. Serrated carcinomas form a subclass of colorectal cancer with distinct molecular basis. Oncogene 2007, 26, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Conesa-Zamora, P.; García-Solano, J.; García-García, F.; Turpin Mdel, C.; Trujillo-Santos, J.; Torres-Moreno, D.; Oviedo-Ramírez, I.; Carbonell-Muñoz, R.; Muñoz-Delgado, E.; Rodriguez-Braun, E.; et al. Expression profiling shows differential molecular pathways and provides potential new diagnostic biomarkers for colorectal serrated adenocarcinoma. Int. J. Cancer 2013, 132, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Conesa-Zamora, P.; García-Solano, J.; TurpinMdel, C.; Sebastián-León, P.; Torres-Moreno, D.; Estrada, E.; Tuomisto, A.; Wilce, J.; Mäkinen, M.J.; Pérez-Guillermo, M.; et al. Methylome profiling reveals functions and genes which are differentially methylated in serrated compared to conventional colorectal carcinoma. Clin. Epigenetics 2015, 7, 101. [Google Scholar] [CrossRef] [PubMed]
- García-Solano, J.; Conesa-Zamora, P.; Trujillo-Santos, J.; Mäkinen, M.J.; Pérez-Guillermo, M. Tumour budding and other prognostic pathological features at invasive margins in serrated colorectal adenocarcinoma: A comparative study with conventional carcinoma. Histopathology 2011, 59, 1046–1056. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Qin, H.; Huang, Z.; Li, S.; Zhu, X.; He, J.; Yang, J.; Yu, X.; Yi, X. Clinical significance of programmed death ligand-1 (PD-L1) in colorectal serrated adenocarcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 9351–9359. [Google Scholar]
- Bosman, F.T.; Carneiro, F.; Hruban, R.H.; Theise, N.D. WHO Classification of Tumours of the Digestive System, 4th ed.; IARC: Lyon, France, 2010; pp. 137–138. [Google Scholar]
- Marzouk, O.; Schofield, J. Review of histopathological and molecular prognostic features in colorectal cancer. Cancers 2011, 3, 2767–2810. [Google Scholar] [CrossRef]
- Green, J.B.; Timmcke, A.E.; Mitchell, W.T.; Hicks, T.C.; Gathright, J.B.J.; Ray, J.E. Mucinous carcinoma—Just another colon cancer? Dis. Colon Rectum 1993, 36, 49–54. [Google Scholar] [CrossRef]
- Hugen, N.; van de Velde, C.J.; de Wilt, J.H.; Nagtegaal, I.D. Metastatic pattern in colorectal cancer is strongly influenced by histological subtype. Ann. Oncol. 2014, 25, 651–657. [Google Scholar] [CrossRef]
- Gonzalez, R.S.; Cates, J.M.M.; Washington, K. Associations among histological characteristics and patient outcomes in colorectal carcinoma with a mucinous component. Histopathology 2019, 74, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Laufman, H.; Saphir, O. Primary linitis plastic type carcinoma of the colon. AMA Arch. Surg. 1951, 62, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Tajiri, K.; Sudou, T.; Fujita, F.; Hisaka, T.; Kinugasa, T.; Akagi, Y. Clinicopathological and corresponding genetic features of colorectal signet ring cell carcinoma. Anticancer Res. 2017, 37, 3817–3823. [Google Scholar]
- Hartman, D.J.; Nikiforova, M.N.; Chang, D.T.; Chu, E.; Bahary, N.; Brand, R.E.; Zureikat, A.H.; Zeh, H.J.; Choudry, H.; Pai, R.K. Signet ring cell colorectal carcinoma: A distinct subset of mucin-poor microsatellite-stable signet ring cell carcinoma associated with dismal prognosis. Am. J. Surg. Pathol. 2013, 37, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Wang, X.; Gao, J.; Li, J.; Li, J.; Qi, C.; Li, Y.; Li, Z.; Shen, L. Clinicopathologic and molecular features of colorectal adenocarcinoma with signet-ring cell component. PLoS ONE 2016, 11, e0156659. [Google Scholar] [CrossRef] [PubMed]
- Alvi, M.A.; Loughrey, M.B.; Dunne, P.; McQuaid, S.; Turkington, R.; Fuchs, M.A.; McGready, C.; Bingham, V.; Pang, B.; Moore, W.; et al. Molecular profiling of signet ring cell colorectal cancer provides a strong rationale for genomic targeted and immune checkpoint inhibitor therapies. Br. J. Cancer 2017, 117, 203–209. [Google Scholar] [CrossRef]
- Nitsche, U.; Zimmermann, A.; Späth, C.; Müller, T.; Maak, M.; Schuster, T.; Slotta-Huspenina, J.; Käser, S.A.; Michalski, C.W.; Janssen, K.P.; et al. Mucinous and signet-ring cell colorectal cancers differ from classical adenocarcinomas in tumor biology and prognosis. Ann. Surg. 2013, 258, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Jessurun, J.; Romero-Guadarrama, M.; Manivel, J.C. Medullary adenocarcinoma of the colon: Clinicopathologic study of 11 cases. Hum. Pathol. 1999, 30, 843–848. [Google Scholar] [CrossRef]
- Kim, H.; Jen, J.; Vogelstein, B.; Hamilton, S.R. Clinical and pathological characteristics of sporadic colorectal carcinomas with DNA replication errors in microsatellite sequences. Am. J. Pathol. 1994, 145, 148–156. [Google Scholar]
- Rüschoff, J.; Dietmaier, W.; Lüttges, J.; Seitz, G.; Bocker, T.; Zirngibl, H.; Schlegel, J.; Schackert, H.K.; Jauch, K.W.; Hofstaedter, F. Poorly differentiated colonic adenocarcinoma, medullary type: Clinical, phenotypic, and molecular characteristics. Am. J. Pathol. 1997, 150, 1815–1825. [Google Scholar]
- Lanza, G.; Gafà, R.; Matteuzzi, M.; Santini, A. Medullary-type poorly differentiated adenocarcinoma of the large bowel: A distinct clinicopathologic entity characterized by microsatellite instability and improved survival. J. Clin. Oncol. 1999, 17, 2429–2438. [Google Scholar] [CrossRef] [PubMed]
- Pyo, J.S.; Sohn, J.H.; Kang, G. Medullary carcinoma in the colorectum: A systematic review and meta-analysis. Hum. Pathol. 2016, 53, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.H.; Yantiss, R.K.; Sadot, E.; Ren, B.; Calvacanti, M.S.; Hechtman, J.F.; Ivelja, S.; Huynh, B.; Xue, Y.; Shitilbans, T.; et al. Diagnosing colorectal medullary carcinoma: Interobserver variability and clinicopathological implications. Hum. Pathol. 2017, 62, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Hinoi, T.; Tani, M.; Lucas, P.C.; Caca, K.; Dunn, R.L.; Macri, E.; Loda, M.; Appelman, H.D.; Cho, K.R.; Fearon, E.R. Loss of CDX2 expression and microsatellite instability are prominent features of large cell minimally differentiated carcinomas of the colon. Am. J. Pathol. 2001, 159, 2239–2248. [Google Scholar] [CrossRef]
- Winn, B.; Tavares, R.; Fanion, J.; Noble, L.; Gao, J.; Sabo, E.; Resnick, M.B. Differentiating the undifferentiated: Immunohistochemical profile of medullary carcinoma of the colon with an emphasis on intestinal differentiation. Hum. Pathol. 2009, 40, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Friedman, K.; Brodsky, A.S.; Lu, S.; Wood, S.; Gill, A.J.; Lombardo, K.; Yang, D.; Resnick, M.B. Medullary carcinoma of the colon: A distinct morphology reveals a distinctive immunoregulatory microenvironment. Mod. Pathol. 2016, 29, 528–541. [Google Scholar] [CrossRef]
- Rosenbaum, M.W.; Bledsoe, J.R.; Morales-Oyarvide, V.; Huynh, T.G.; Mino-Kenudson, M. PD-L1 expression in colorectal cancer is associated with microsatellite instability, BRAF mutation, medullary morphology and cytotoxic tumor-infiltrating lymphocytes. Mod. Pathol. 2016, 29, 1104–1112. [Google Scholar] [CrossRef]
- Johncilla, M.; Chen, Z.; Sweeney, J.; Yantiss, R.K. Tumor grade is prognostically relevant among mismatch repair deficient colorectal carcinomas. Am. J. Surg. Pathol. 2018, 42, 1686–1692. [Google Scholar] [CrossRef]
- Del Arco, C.D.; Collazo, F.E.; Aceñero, M.J.F. Lymphoepithelioma-like carcinoma of the large intestine: A case report and literature review. Rev. Esp. Patol. 2018, 51, 18–22. [Google Scholar] [CrossRef]
- De Petris, G.; Lev, R.; Quirk, D.M.; Ferbend, P.R.; Butmarc, J.R.; Elenitoba-Johnson, K. Lymphoepithelioma-like carcinoma of the colon in a patient with hereditary non polyposis colorectal cancer. Arch. Pathol. Lab. Med. 1999, 123, 720–724. [Google Scholar]
- Kon, S.; Kasai, K.; Tsuzuki, N.; Nishibe, M.; Kitagawa, T.; Nishibe, T.; Sato, N. Lymphoepithelioma-like carcinoma of rectum: Possible relation with EBV. Pathol. Res. Pract. 2001, 197, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Kojima, Y.; Mogaki, M.; Takagawa, R.; Ota, I.; Sugita, M.; Natori, S.; Hamaguchi, Y.; Kurosawa, H.; Fukushima, T.; Masui, H.; et al. A case of lymphoepithelioma-like carcinoma of the colon with ulcerative colitis. J. Gastroenterol. 2007, 42, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Delaney, D.; Chetty, R. Lymphoepithelioma-like carcinoma of the colon. Int. J. Clin. Exp. Pathol. 2012, 5, 105–109. [Google Scholar] [PubMed]
- Lino-Silva, L.S.; Salcedo-Hernández, R.A.; Herrera-Gómez, A.; Padilla-Rosciano, A.; Ramírez-Jaramillo, M.; Herrera-Goepfert, R.E.; Meneses-García, A. Colonic cribriform carcinoma, a morphologic pattern associated with low survival. Int. J. Surg. Pathol. 2015, 23, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Doi, H.; Konishi, K.; Omori, R.; Yanagawa, T.; Katagiri, A.; Yamochi, T.; Date, Y.; Kubota, Y.; Muramoto, T.; Yano, Y.; et al. Primary micropapillary carcinoma of the colon: A case report and literature review. Clin. J. Gastroenterol. 2011, 4, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Branca, G.; Ieni, A.; Barresi, V.; Tuccari, G.; Caruso, R.A. An updated review of cribriform carcinomas with emphasis on histopathological diagnosis and prognostic significance. Oncol. Rev. 2017, 11, 317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egashira, Y.; Yoshida, T.; Hirata, I.; Hamamoto, N.; Akutagawa, H.; Takeshita, A.; Noda, N.; Kurisu, Y.; Shibayama, Y. Analysis of pathological risk factors for lymph node metastasis of submucosal invasive colon cancer. Mod. Pathol. 2004, 17, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, K.; Watanabe, M.; De La Cruz, C.; Honda, H.; Ise, H.; Mitsui, K.; Namiki, K.; Mikami, Y.; Moriya, T.; Sasano, H. Primary invasive micropapillary carcinoma of the colon. Histopathology 2005, 47, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Guzińska-Ustymowicz, K.; Niewiarowska, K.; Pryczynicz, A. Invasive micropapillary carcinoma: A distinct type of adenocarcinomas in the gastrointestinal tract. World J. Gastroenterol. 2014, 20, 4597–4606. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Zhang, H.; Zhang, X.B.; Lonser, R.; Thompson, K.; Raza, A. Consensus and conflict in invasive micropapillary carcinoma: A case report and review of the literature. J. Gastrointest. Oncol. 2016, 7, S55–S61. [Google Scholar] [PubMed]
- Patankar, M.; Vayrynen, S.; Tuomisto, A.; Makinen, M.; Eskelinen, S.; Karttunen, T.J. Micropapillary structures in colorectal cancer: An anoikis-resistant subpopulation. Anticancer Res. 2018, 38, 2915–2921. [Google Scholar] [PubMed]
- Sonoo, H.; Kameyama, M.; Inatugi, N.; Nonomura, A.; Enomoto, Y. Pedunculated polyp of early sigmoid colon cancer with invasive micropapillary carcinoma. Jpn. J. Clin. Oncol. 2009, 39, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Otsubo, K.; Kubo, N.; Nakashima, N.; Izumi, M.; Nakamori, M.; Koto, H. A juvenile case of pulmonary lymphangitic carcinomatosis caused by sigmoid colon cancer with a component of micropapillary carcinoma. Intern. Med. 2011, 50, 2361–2365. [Google Scholar] [CrossRef] [PubMed]
- Ueno, H.; Kajiwara, Y.; Shimazaki, H.; Shinto, E.; Hashiguchi, Y.; Nakanishi, K.; Maekawa, K.; Katsurada, Y.; Nakamura, T.; Mochizuki, H.; et al. New criteria for histologic grading of colorectal cancer. Am. J. Surg. Pathol. 2012, 36, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Jakubowska, K.; Guzińska-Ustymowicz, K.; Pryczynicz, A. Invasive micropapillary component and its clinico-histopathological significance in patients with colorectal cancer. Oncol. Lett. 2016, 12, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Barresi, V.; Branca, G.; Vitarelli, E.; Tuccari, G. Micropapillary pattern and poorly differentiated clusters represent the same biological phenomenon in colorectal cancer: A proposal for a change in terminology. Am. J. Clin. Pathol. 2014, 142, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, N.; Oonishi, K.; Ohara, M.; Hirouchi, T.; Mizuno, K.; Hayashi, Y.; Lee, G.H. Invasive micropapillary carcinoma of the colon: An immunohistochemical study. Med. Mol. Morphol. 2007, 40, 226–230. [Google Scholar] [CrossRef]
- Reggiani Bonetti, L.; Barresi, V.; Bettelli, S.; Domati, F.; Palmiere, C. Poorly differentiated clusters (PDC) in colorectal cancer: What is and ought to be known. Diagn. Pathol. 2016, 11, 31. [Google Scholar] [CrossRef]
- Levi, G.S.; Harpaz, N. Intestinal low-grade tubule glandular adenocarcinoma in inflammatory bowel disease. Am. J. Surg. Pathol. 2006, 30, 1022–1029. [Google Scholar] [CrossRef]
- Vanoli, A.; Di Sabatino, A.; Furlan, D.; Klersy, C.; Grillo, F.; Fiocca, R.; Mescoli, C.; Rugge, M.; Nesi, G.; Fociani, P.; et al. Small Bowel Carcinomas in Coeliac or Crohn’s Disease: Clinico-pathological, molecular, and prognostic features. A study from the Small Bowel Cancer Italian Consortium. J. Crohns Colitis 2017, 11, 942–953. [Google Scholar] [CrossRef]
- Hartman, D.J.; Binion, D.; Regueiro, M.; Schraut, W.; Bahary, N.; Sun, W.; Nikiforova, M.; Pai, R.K. Isocitrate dehydrogenase-1 is mutated in inflammatory bowel disease-associated intestinal adenocarcinoma with low-grade tubuloglandular histology but not in sporadic intestinal adenocarcinoma. Am. J. Surg. Pathol. 2014, 38, 1147–1156. [Google Scholar] [CrossRef] [PubMed]
- Loy, T.S.; Kaplan, P.A. Villous adenocarcinoma of the colon and rectum: A clinicopathologic study of 36 cases. Am. J. Surg. Pathol. 2004, 28, 1460–1465. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, R.S.; Cates, J.M.; Washington, M.K.; Beauchamp, R.D.; Coffey, R.J.; Shi, C. Adenoma-like adenocarcinoma: A subtype of colorectal carcinoma with good prognosis, deceptive appearance on biopsy and frequent KRAS mutation. Histopathology 2016, 68, 183–190. [Google Scholar] [CrossRef]
- Yao, T.; Kajiwara, M.; Kouzuki, T.; Iwashita, A.; Tsuneyoshi, M. Villous tumor of the colon and rectum with special reference to roles of p53 and bcl-2 in adenoma–carcinoma sequence. Pathol. Int. 1999, 49, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Palazzo, J.P.; Edmonston, T.B.; Chaille-Arnold, L.M.; Burkholder, S. Invasive papillary adenocarcinoma of the colon. Hum. Pathol. 2002, 33, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Crissman, J.D. Adenosquamous and squamous cell carcinoma of the colon. Am. J. Surg Pathol. 1978, 2, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Masoomi, H.; Ziogas, A.; Lin, B.S.; Barleben, A.; Mills, S.; Stamos, M.J.; Zell, J.A. Population-based evaluation of adenosquamous carcinoma of the colon and rectum. Dis. Colon Rectum 2012, 55, 509–514. [Google Scholar] [CrossRef]
- Fujita, T.; Fukuda, K.; Nishi, H.; Takao, T.; Ohmura, Y.; Mano, M.; Komatsubara, S. Paraneoplastich ypercalcemia with adenosquamous carcinoma of the colon. Int. J. Clin. Oncol. 2005, 10, 144–147. [Google Scholar] [CrossRef]
- Yitta, S.; Liang, M.K.; Berman, R.; Carter, J.J.; Yee, H.T.; Marks, J.L. Primary squamous cell carcinoma of the colon associated with hypercalcemia and hyperleukocytosis. Report of a case. Dig. Surg. 2005, 22, 371–374. [Google Scholar] [CrossRef]
- Shafaghi, A.; Askari, K.; Ashoobi, M.T.; Mansour-Ghanaei, F. Adenosquamous carcinoma of the sigmoid colon: A case report and review of literature. Int. J. Clin. Exp. Med. 2013, 6, 390–392. [Google Scholar]
- Frizelle, F.A.; Hobday, K.S.; Batts, K.P.; Nelson, H. Adenosquamous and squamous carcinoma of the colon and upper rectum: A clinical and histopathologic study. Dis. Colon Rectum 2001, 44, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Audeau, A.; Han, H.W.; Johnston, M.J.; Whitehead, M.W.; Frizelle, F.A. Does human papilloma virus have a role in squamous cell carcinoma of the colon and upper rectum? Eur. J. Surg. Oncol. 2002, 28, 657–660. [Google Scholar] [CrossRef] [PubMed]
- Remo, A.; Grillo, F.; Mastracci, L.; Fassan, M.; Sina, S.; Zanella, C.; Parcesepe, P.; Damiano Urso, E.; Pancione, M.; Bortuzzo, G.; et al. Clear cell colorectal carcinoma: Time to clarify diagnosis. Pathol. Res. Pract. 2017, 213, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Fassan, M.; Pennelli, G.; Mastracci, L.; Remo, A.; Cappellesso, R.; Lo Mele, M.; Realdon, S.; Munari, G.; Lazzi, S.; Rugge, M. Clear cell dysplasia in a sessile serrated adenoma. Pathol. Res. Pract. 2018, 214, 2121–2122. [Google Scholar] [CrossRef] [PubMed]
- Barrera-Maldonado, C.D.; Wiener, I.; Sim, S. Clear cell adenocarcinoma of the colon: A case report and review of the literature. Case Rep. Oncol. Med. 2014, 2014, 9054788. [Google Scholar] [CrossRef] [PubMed]
- Okazawa, Y.; Takahashi, R.; Mizukoshi, K.; Takehara, K.; Ishiyama, S.; Sugimoto, K.; Takahashi, M.; Kojima, Y.; Goto, M.; Okuzawa, A.; et al. A case of clear cell adenocarcinoma arising from endometriosis of the rectum treated by laparoscopic surgery. Int. J. Surg. Case Rep. 2014, 5, 979–983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourreille, J.; Metayer, P.; Sauger, F.; Matray, F.; Fondimare, A. Existence of alpha feto protein during gastric-origin secondary cancer of the liver. Presse Med. 1970, 78, 1277–1278. [Google Scholar] [PubMed]
- Ishikura, H.; Kirimoto, K.; Shamoto, M.; Miyamoto, Y.; Yamagiva, H.; Itoh, T.; Aizawa, M. Hepatoid adenocarcinomas of the stomach. An analysis of seven cases. Cancer 1986, 58, 119–126. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, P.; Xiao, H.; Wu, X.; Liu, W.; He, J.; Gao, J.; Wang, G.; Shuai, X.; Tao, K. Clinicopathological features and prognosis of intestinal hepatoid adenocarcinoma: Evaluation of a pooled case series. Oncotarget 2017, 9, 2715–2725. [Google Scholar] [CrossRef]
- Su, J.S.; Chen, Y.T.; Wang, R.C.; Wu, C.Y.; Lee, S.W.; Lee, T.Y. Clinicopathological characteristics in the differential diagnosis of hepatoid adenocarcinoma: A literature review. World J. Gastoenterol. 2013, 19, 321–327. [Google Scholar] [CrossRef]
- Cappetta, A.; Bergamo, F.; Mescoli, C.; Lonardi, S.; Rugge, M.; Zagonel, V. Hepatoid adenocarcinoma of the colon: What should we target? Pathol. Oncol. Res. 2012, 18, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Koelzer, V.H.; Steuer, K.; Gross, U.C.; Zimmermann, D.; Paasinen-Sohns, A.; Mertz, K.D.; Cathomas, G. Colorectal choriocarcinoma in a patient with probable Lynch Syndrome. Front. Oncol. 2016, 6, 252. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Inoue, T.; Hamano, K. Choriocarcinoma of the sigmoid colon: Report of a case. Surg. Today 2012, 42, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Kubosawa, H.; Nagao, K.; Kondo, Y.; Ishige, H.; Inaba, N. Coexistence of adenocarcinoma and choriocarcinoma in the sigmoid colon. Cancer 1984, 54, 866–868. [Google Scholar] [CrossRef]
- Verbeek, W.; Schulten, H.J.; Sperling, M.; Tiesmeier, J.; Stoop, H.; Dinjens, W.; Looijenga, L.; Wörmann, B.; Füzesi, L.; Donhuijsen, K. Rectal adenocarcinoma with choriocarcinomatous differentiation: Clinical and genetic aspects. Hum. Pathol. 2004, 35, 1427–1430. [Google Scholar] [CrossRef]
- Maehira, H.; Shimizu, T.; Sonoda, H.; Mekata, E.; Yamaguchi, T.; Miyake, T.; Ishida, M.; Tani, T. A rare case of primary choriocarcinoma in the sigmoid colon. World J. Gastroenterol. 2013, 19, 6683–6688. [Google Scholar] [CrossRef] [PubMed]
- Remo, A.; Zanella, C.; Molinari, E.; Talamini, A.; Tollini, F.; Piacentini, P.; Battaglia, P.; Baritono, E.; Bonetti, A.; Lanza, F.; et al. Rhabdoid carcinoma of the colon: A distinct entity with a very aggressive behavior. A case report associated with a polyposis coli and review of the literature. Int. J. Surg. Pathol. 2012, 20, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Remo, A.; Manfrin, E.; Parcesepe, P.; Ferrarini, A.; Han, H.S.; Ugnius, M.; Laudanna, C.; Simbolo, M.; Malanga, D.; Mendes Oliveira, D.; et al. Centrosome linker-induced tetraploid segregation errors link rhabdoid phenotypes and lethal colorectal cancers. Mol. Cancer Res. 2018, 16, 1385–1395. [Google Scholar] [CrossRef]
- Remo, A.; Cecchini, M.P.; Benati, D.; Bernardi, P.; Manfrin, E.; Giordano, G.; Bonomi, F.; Parcesepe, P.; Fassan, M.; Colombari, R.; et al. CROCC-mutated rhabdoid colorectal carcinoma showing in intercellular spaces lamellipodia and cellular projections revealed by electron microscopy. Virchows Arch. 2019. [Google Scholar] [CrossRef]
- Pancione, M.; Remo, A.; Zanella, C.; Sabatino, L.; Di Blasi, A.; Laudanna, C.; Astati, L.; Rocco, M.; Bifano, D.; Piacentini, P.; et al. The chromatin remodelling component SMARCB1/INI1 influences the metastatic behavior of colorectal cancer through a gene signature mapping to chromosome 22. J. Transl. Med. 2013, 28, 297. [Google Scholar] [CrossRef]
- Agaimy, A.; Daum, O.; Markl, B.; Lichtmannegger, I.; Michal, M.; Hartmann, A. SWI/SNF complex–eficient undifferentiated/rhabdoid carcinomas of the gastrointestinal tract. A series of 13 cases highlighting mutually exclusive loss of SMARCA4 and SMARCA2 and frequent co-inactivation of SMARCB1 and SMARCA2. Am. J. Surg. Pathol. 2016, 40, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, T. Zur Kenntnis der stomaerkno: Cherungin Kazinomen des Digestionstraktes. Wein. Klin. Wochenschr. 1923, 36, 653–656. [Google Scholar]
- Dukes, C.E. Ossification in rectal cancer. Proc. R. Soc. Med. 1939, 32, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xu, J.; Chen, L. Colorectal cancer with osseous metaplasia. Oncotarget 2017, 8, 65407–65413. [Google Scholar] [PubMed]
- Mastracci, L.; Ficarra, G.; Bianchi, R.; Pesce, F.; Grillo, F. Adenocarcinoma with osseous metaplasia: Is It Bad to the Bone? Int. J. Surg. Pathol. 2019. [Google Scholar] [CrossRef]
- Imai, N.; Iwai, A.; Hatekeyama, S.; Matsuzaki, K.; Kitagawa, Y.; Kato, S.; Hokari, R.; Kawaguchi, A.; Nagao, S.; Miyahara, T.; et al. Expression of bone morphogenetic proteins in colon carcinoma with heteroplastic ossification. Pathol. Int. 2001, 51, 643–648. [Google Scholar] [CrossRef]
- Lee, J.K.; Ghosh, P.; McWhorter, V.; Payne, M.; Olson, R.; Krinsky, M.L.; Ramamoorthy, S.; Carethers, J.M. Evidence for colorectal sarcomatoid carcinoma arising from tubulovillous adenoma. World J. Gastroenterol. 2008, 14, 4389–4394. [Google Scholar] [CrossRef]
- Choi, Y.Y.; Jeen, Y.M.; Kim, Y.J. Sarcomatoid carcinoma of colon: Extremely poor prognosis. J. Korean Surg. Soc. 2011, 80, S26–S30. [Google Scholar] [CrossRef]
- De Luca-Johnson, J.; Zenali, M. Education and Imaging. Gastrointestinal: Sarcomatoid carcinoma of the colon, a rare and highly aggressive tumor subtype. J. Gastroenterol. Hepatol. 2016, 31, 7. [Google Scholar] [CrossRef]
- Bak, M.; Teglbjaerg, P.S. Pleomorphic (giant cell) carcinoma of the intestine. An immunohistochemical and electron microscopic study. Cancer 1989, 64, 2557–2564. [Google Scholar] [CrossRef]
- Branca, G.; Barresi, V.; Ieni, A.; Irato, E.; Caruso, R.A. Pleomorphic carcinoma of the colon: Morphological and immunohistochemical findings. Case Rep. Gastroenterol. 2016, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Serio, G.; Aguzzi, A. Spindle and giant cell carcinoma of the colon. Histopathology 1997, 30, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Qiu, M.Z.; Pan, W.T.; Lin, J.Z.; Wang, Z.X.; Pan, Z.Z.; Wang, F.H.; Yang, D.J.; Xu, R.H. Comparison of survival between right-sided and left-sided colon cancer in different situations. Cancer Med. 2018, 7, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Wachtel, M.S.; Haynes, A.L.; Griswold, J.A. Signet ring, high grade, and undifferentiated colorectal adenocarcinomas differ. J. Surg. Res. 2010, 163, 250–256. [Google Scholar] [CrossRef] [PubMed]



| Histotype | Mean Age | Site | Prognosis# | Main Diagnostic Criteria | Immunoprofile | Molecular Profile | |
|---|---|---|---|---|---|---|---|
| Serrated Adenocarcinoma (SA) | 67 | Right colon and rectum | Aggressive | Epithelial serrations +/− tufts; eosinophilic cytoplasm; vescicular nuclei | KRASmut BRAFmut MSI | ||
| Mucinous (colloid) adenocarcinoma (MA) | 60 | Right colon | Similar to conventional | Abundant extracellular mucin in more than 50% | MMRd, PDL1+ | KRASmut BRAFmut, MSI | |
| Signet ring cell carcinoma (SRC) | 65 | No site predilection | Aggressive | Signet ring cells in more than 50% | MMRd, PDL1+ | KRASmut BRAFmut, MSI | |
| Medullary carcinoma (MC) | 70 | Right colon | Favourable | Solid growth pattern with circumscribed tumor borders; tumor cells with a syncytial appearance; conspicuous intra and peri tumor lymphocytes. | MMRd, CDX-2−, CK20+, calretinin+ | MSI, BRAFmut | |
| Lymphoepitelioma-like (LELC) | 62 | No site predilection | Favourable | Poorly differentiated carcinoma with abundant intratumour infiltrating lymphocytes; presence of EBV | MMRd | EBV+ | |
| Cribriform comedo-type adenocarcinoma (CC-type) | 56 | No site predilection | Aggressive | Tightly packed neoplastic glands and cribriform architecture and large glands with central necrosis | CK20+, CDX-2+, MUC2+ | ||
| Micropapillary carcinoma (MPA) | 69 | Right colon and rectum | Aggressive | Clusters with lacunar space of more than 5 neoplastic cells; inverse polarity | Inverted MUC1, MUC2−, E-cadherin altered pattern | TP53mut, KRASmut, BRAFmut, CIN | |
| Low -grade tubuloglandular carcinoma (LGTGA) | 42 | No site predilection | Favourable | Tubular architecture composed of neoplastic glands with little atypia | MMRd (MLH1d) | MSI, KRASmut, IDH1mut | |
| Villous carcinoma (VC) | 66 | Left colon | Favourable | Villous architecture in >50% | KRASmut | ||
| Squamous/Adenosquamous carcinoma (SCC/ASC) | 60 | Right colon | Aggressive | Squamous differentiation either pure or composite with glandular component | p63+, CK5/6+ | ||
| Clear cell carcinoma | Mullerian-mCCC | 52 | Exclusively rectum | Favourable | Clear cells in more than 50%; endometriosis or pregnancy | CK20−, CK7+, CEA−, CA125+ | |
| Intestinal-iCCC | 61 | No site predilection | Aggressive | Clear cell in more than 50% | CK20+, CK7−, CEA+, CDX-2+) | KRASmut, MSI | |
| Hepatoid carcinoma (HepAC) | 50 | Rectum | Aggressive | Neoplastic cells with hepatoid appearence in solid, trabecular o pseudoacinar architectural patterns | AFP+ (also serum), Glypican-3+, CK18+, CK19+, CEA+, Hep Par1 + (40%) | ||
| Primary Choriocarcinoma (pChC) | 54 | Left colon | Aggressive | Syncytiotrophoblast-like cells | β-HCG (also serum) | ||
| Rhabdoid carcinoma (RhC) | 70 | Right colon | Aggressive | Rhabdoid cells >5% | CK20−, Vimentin+, CDX-2−, INI1−, CROCC reduction signals. | BRAFmut, MSI, CROCCmut | |
| Carcinoma with osseous metaplasia (COM) | 58 | Left colon | Similar to conventional | Presence of osseous metaplasia in a conventional adenocarcinoma | |||
| Spindle cell or mesenchymal carcinoma* (SpCC) | 70 | Left colon and Rectum | Aggressive | Biphasic carcinoma with a spindle-cell sarcomatoid component (cytokeratin +); may have giant cells | Vimentin+, CK+ (focal) | ||
| Undifferentiated carcinoma (UC) | 70 | No site predilection | Aggressive | Evidence of epithelial differentiation with minimal or without gland formation | CK+, absence of other differentiation markers | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Remo, A.; Fassan, M.; Vanoli, A.; Bonetti, L.R.; Barresi, V.; Tatangelo, F.; Gafà, R.; Giordano, G.; Pancione, M.; Grillo, F.; et al. Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes. Cancers 2019, 11, 1036. https://doi.org/10.3390/cancers11071036
Remo A, Fassan M, Vanoli A, Bonetti LR, Barresi V, Tatangelo F, Gafà R, Giordano G, Pancione M, Grillo F, et al. Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes. Cancers. 2019; 11(7):1036. https://doi.org/10.3390/cancers11071036
Chicago/Turabian StyleRemo, Andrea, Matteo Fassan, Alessandro Vanoli, Luca Reggiani Bonetti, Valeria Barresi, Fabiana Tatangelo, Roberta Gafà, Guido Giordano, Massimo Pancione, Federica Grillo, and et al. 2019. "Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes" Cancers 11, no. 7: 1036. https://doi.org/10.3390/cancers11071036
APA StyleRemo, A., Fassan, M., Vanoli, A., Bonetti, L. R., Barresi, V., Tatangelo, F., Gafà, R., Giordano, G., Pancione, M., Grillo, F., & Mastracci, L. (2019). Morphology and Molecular Features of Rare Colorectal Carcinoma Histotypes. Cancers, 11(7), 1036. https://doi.org/10.3390/cancers11071036











