Identification of High-Risk Atypical Meningiomas According to Semantic and Radiomic Features
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
2.1. Patients
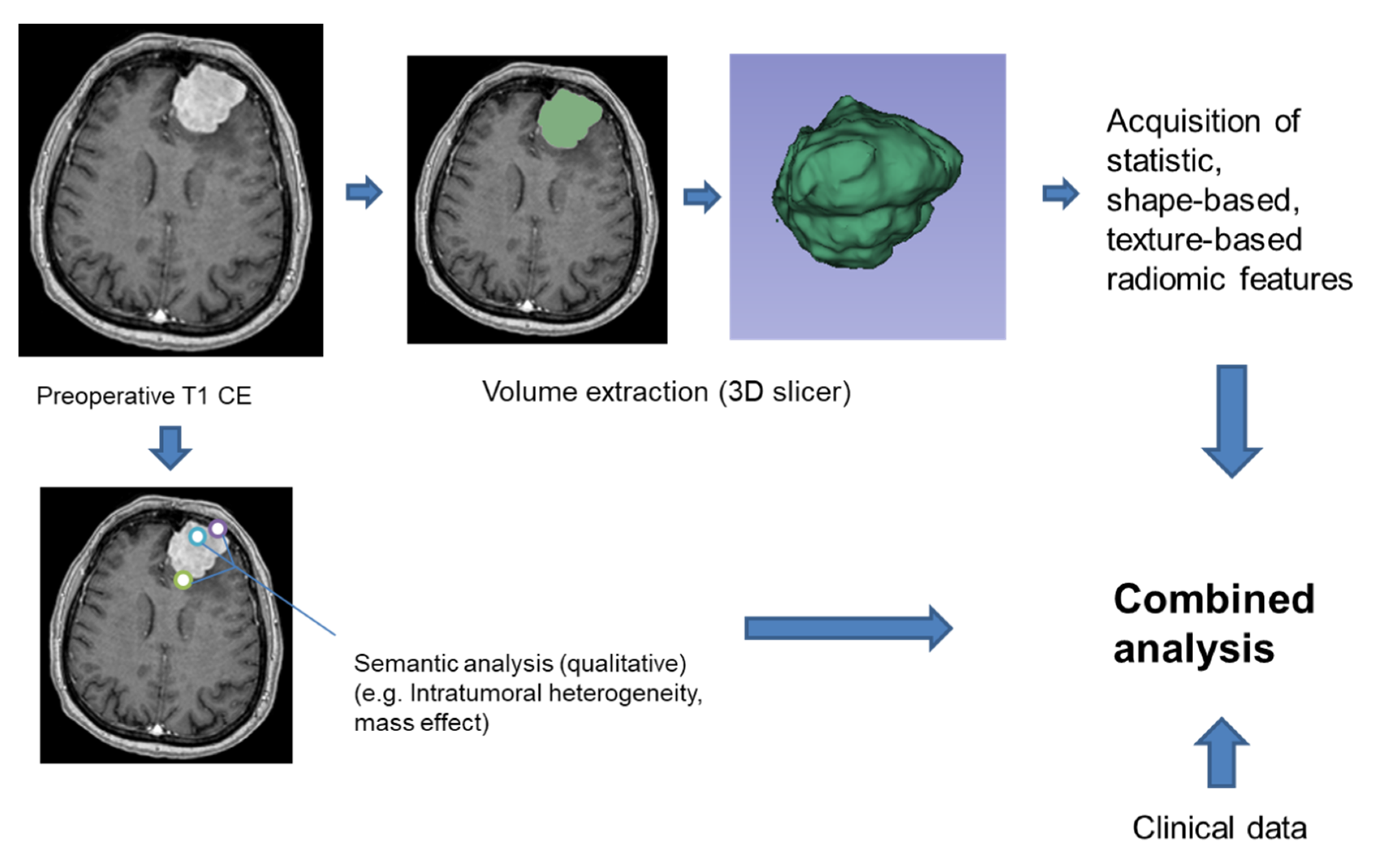
2.2. Semantic and Radiomic Features
3. Discussion
4. Materials and Methods
4.1. Patient Sample and Study Design
4.2. Radiomic and Semantic Analysis
4.3. H3K27me3 Immunohistochemistry
4.4. Sequencing of Genomic DNA from Formalin-Fixed, Paraffin-Embedded Meningioma Samples
4.5. Statistics
4.6. Ethical Approval
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, L.; Gilbert, M.; Vogelbaum, M.A. Intracranial meningiomas of atypical (WHO grade II) histology. J. Neuro-Oncol. 2010, 99, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Hao, S.; Wu, Z.; Wang, L.; Jia, G.; Zhang, L.; Zhang, J. Treatment response and prognosis after recurrence of atypical meningiomas. World Neurosurg. 2015, 84, 1014–1019. [Google Scholar] [CrossRef] [PubMed]
- Keric, N.; Kalasauskas, D.; Freyschlag, C.F.; Gempt, J.; Misch, M.; Poplawski, A.; Lange, N.; Ayyad, A.; Thomé, C.; Vajkoczy, P. Impact of postoperative radiotherapy on recurrence of primary intracranial atypical meningiomas. J. Neuro-Oncol. 2020, 146, 347–355. [Google Scholar] [CrossRef]
- Shakir, S.I.; Souhami, L.; Petrecca, K.; Mansure, J.J.; Singh, K.; Panet-Raymond, V.; Shenouda, G.; Al-Odaini, A.A.; Abdulkarim, B.; Guiot, M.-C. Prognostic factors for progression in atypical meningioma. J. Neurosurg. 2018, 129, 1240–1248. [Google Scholar] [CrossRef]
- Masalha, W.; Heiland, D.H.; Franco, P.; Delev, D.; Haaker, J.G.; Schnell, O.; Scheiwe, C.; Grauvogel, J. Atypical meningioma: Progression-free survival in 161 cases treated at our institution with surgery versus surgery and radiotherapy. J. Neuro-Oncol. 2018, 136, 147–154. [Google Scholar] [CrossRef]
- Schmidt, M.; Mock, A.; Jungk, C.; Sahm, F.; Ull, A.T.; Warta, R.; Lamszus, K.; Gousias, K.; Ketter, R.; Roesch, S. Transcriptomic analysis of aggressive meningiomas identifies PTTG1 and LEPR as prognostic biomarkers independent of WHO grade. Oncotarget 2016, 7, 14551. [Google Scholar] [CrossRef] [Green Version]
- Sahm, F.; Schrimpf, D.; Olar, A.; Koelsche, C.; Reuss, D.; Bissel, J.; Kratz, A.; Capper, D.; Schefzyk, S.; Hielscher, T. TERT promoter mutations and risk of recurrence in meningioma. J. Natl. Cancer Inst. 2016, 108, djv377. [Google Scholar] [CrossRef]
- Lee, G.; Lee, H.Y.; Park, H.; Schiebler, M.L.; van Beek, E.J.; Ohno, Y.; Seo, J.B.; Leung, A. Radiomics and its emerging role in lung cancer research, imaging biomarkers and clinical management: State of the art. Eur. J. Radiol. 2017, 86, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Scalera, J.; Khalid, M.; Touret, A.-S.; Bloch, N.; Li, B.; Qureshi, M.M.; Soto, J.A.; Anderson, S.W. Texture analysis as a radiomic marker for differentiating renal tumors. Abdom. Radiol. 2017, 42, 2470–2478. [Google Scholar] [CrossRef] [PubMed]
- Kickingereder, P.; Burth, S.; Wick, A.; Götz, M.; Eidel, O.; Schlemmer, H.-P.; Maier-Hein, K.H.; Wick, W.; Bendszus, M.; Radbruch, A. Radiomic profiling of glioblastoma: Identifying an imaging predictor of patient survival with improved performance over established clinical and radiologic risk models. Radiology 2016, 280, 880–889. [Google Scholar] [CrossRef]
- Coroller, T.P.; Bi, W.L.; Huynh, E.; Abedalthagafi, M.; Aizer, A.A.; Greenwald, N.F.; Parmar, C.; Narayan, V.; Wu, W.W.; de Moura, S.M. Radiographic prediction of meningioma grade by semantic and radiomic features. PLoS ONE 2017, 12, e0187908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morin, O.; Chen, W.C.; Nassiri, F.; Susko, M.; Magill, S.T.; Vasudevan, H.N.; Wu, A.; Vallières, M.; Gennatas, E.D.; Valdes, G. Integrated models incorporating radiologic and radiomic features predict meningioma grade, local failure, and overall survival. Neuro-Oncol. Adv. 2019, 1, vdz011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laukamp, K.R.; Shakirin, G.; Baeßler, B.; Thiele, F.; Zopfs, D.; Hokamp, N.G.; Timmer, M.; Kabbasch, C.; Perkuhn, M.; Borggrefe, J. Accuracy of radiomics-based feature analysis on multiparametric MR images for non-invasive meningioma grading. World Neurosurg. 2019, 132, e366–e390. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.W.; Oh, J.; You, S.C.; Han, K.; Ahn, S.S.; Choi, Y.S.; Chang, J.H.; Kim, S.H.; Lee, S.-K. Radiomics and machine learning may accurately predict the grade and histological subtype in meningiomas using conventional and diffusion tensor imaging. Eur. Radiol. 2019, 29, 4068–4076. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.; Zhou, X.; Duan, C.; Zhao, J.; Sui, Q.; Liu, X.; Zhang, X. Differentiation Researches on the Meningioma Subtypes by Radiomics from Contrast-Enhanced Magnetic Resonance Imaging: A Preliminary Study. World Neurosurg. 2019, 126, e646–e652. [Google Scholar] [CrossRef] [PubMed]
- Nanda, A.; Bir, S.C.; Konar, S.; Maiti, T.; Kalakoti, P.; Jacobsohn, J.A.; Guthikonda, B. Outcome of resection of WHO Grade II meningioma and correlation of pathological and radiological predictive factors for recurrence. J. Clin. Neurosci. 2016, 31, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Stafford, S.L.; Perry, A.; Suman, V.J.; Meyer, F.B.; Scheithauer, B.W.; Lohse, C.M.; Shaw, E.G. Primarily resected meningiomas: Outcome and prognostic factors in 581 Mayo Clinic patients, 1978 through 1988. Mayo Clin. Proc. 1988, 73, 936–942. [Google Scholar] [CrossRef]
- Aghi, M.K.; Carter, B.S.; Cosgrove, G.R.; Ojemann, R.G.; Amin-Hanjani, S.; Martuza, R.L.; Curry, W.T., Jr.; Barker, F.G. Long Term Recurrence Rates of Atypical Meningiomas After Gross Total Resection With or Without Postoperative Adjuvant Radiation. Neurosurgery 2009, 64, 56–60. [Google Scholar] [CrossRef]
- Mair, R.; Morris, K.; Scott, I.; Carroll, T.A. Radiotherapy for atypical meningiomas: Clinical article. J. Neurosurg. 2011, 115, 811–819. [Google Scholar] [CrossRef]
- Komotar, R.J.; Iorgulescu, J.B.; Raper, D.M.; Holland, E.C.; Beal, K.; Bilsky, M.H.; Brennan, C.W.; Tabar, V.; Sherman, J.H.; Yamada, Y. The role of radiotherapy following gross-total resection of atypical meningiomas: Clinical article. J. Neurosurg. 2012, 117, 679–686. [Google Scholar] [CrossRef] [Green Version]
- Jenkinson, M.D.; Waqar, M.; Farah, J.O.; Farrell, M.; Barbagallo, G.M.; McManus, R.; Looby, S.; Hussey, D.; Fitzpatrick, D.; Certo, F. Early adjuvant radiotherapy in the treatment of atypical meningioma. J. Clin. Neurosci. 2016, 28, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, F.; Roda, J.M.; Romero, M.P.; Morales, C.; Sarmiento, M.A.; Blázquez, M.G. Malignant and atypical meningiomas: A reappraisal of clinical, histological, and computed tomographic features. Neurosurgery 1987, 20, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.L.; Marciscano, A.E.; Niemierko, A.; Kim, D.W.; Stemmer-Rachamimov, A.O.; Curry, W.T.; Barker, F.G.; Martuza, R.L.; Loeffler, J.S.; Oh, K.S. Imaging and extent of surgical resection predict risk of meningioma recurrence better than WHO histopathological grade. Neuro-Oncol. 2016, 18, 863–872. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-C.; Pai, C.-Y.; Kao, H.-W.; Hsueh, C.-J.; Hsu, W.-L.; Lo, C.-P. Do aggressive imaging features correlate with advanced histopathological grade in meningiomas? J. Clin. Neurosci. 2010, 17, 584–587. [Google Scholar] [CrossRef] [PubMed]
- Spille, D.C.; Sporns, P.B.; Heß, K.; Stummer, W.; Brokinkel, B. Prediction of high-grade histology and recurrence in meningiomas using routine preoperative magnetic resonance imaging—A systematic review. World Neurosurg. 2019, 128, 174–181. [Google Scholar] [CrossRef]
- Katz, L.M.; Hielscher, T.; Liechty, B.; Silverman, J.; Zagzag, D.; Sen, R.; Wu, P.; Golfinos, J.G.; Reuss, D.; Neidert, M.C. Loss of histone H3K27me3 identifies a subset of meningiomas with increased risk of recurrence. Acta Neuropathol. 2018, 135, 955–963. [Google Scholar] [CrossRef] [Green Version]
- Surov, A.; Hamerla, G.; Meyer, H.J.; Winter, K.; Schob, S.; Fiedler, E. Whole lesion histogram analysis of meningiomas derived from ADC values. Correlation with several cellularity parameters, proliferation index KI 67, nucleic content, and membrane permeability. Magn. Reson. Imaging 2018, 51, 158–162. [Google Scholar] [CrossRef]
- Hale, A.T.; Stonko, D.P.; Wang, L.; Strother, M.K.; Chambless, L.B. Machine learning analyses can differentiate meningioma grade by features on magnetic resonance imaging. Neurosurg. Focus 2018, 45, E4. [Google Scholar] [CrossRef] [Green Version]
- Kikinis, R.; Pieper, S.D.; Vosburgh, K.G. 3D Slicer: A platform for subject-specific image analysis, visualization, and clinical support. In Intraoperative Imaging and Image-Guided Therapy; Springer: Berlin/Heidelberg, Germany, 2014; pp. 277–289. [Google Scholar]
- Jolesz, F.A. Intraoperative Imaging and Image-Guided Therapy; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Vallières, M.; Freeman, C.R.; Skamene, S.R.; El Naqa, I. A radiomics model from joint FDG-PET and MRI texture features for the prediction of lung metastases in soft-tissue sarcomas of the extremities. Phys. Med. Biol. 2015, 60, 5471. [Google Scholar] [CrossRef]

| Characteristic | All Patients | Radiomic Data Available | Semantic Data Available |
|---|---|---|---|
| N (%) | 76 (100) | 51 (67.1) | 55 (72.4) |
| Age (SD) | 58.7 (13.8) | 59.1 (14.1) | 58.8 (13.9) |
| Women, % | 59.2 | 64.7 | 65.5 |
| Tumor localization, % | |||
| Convexity/falx | 59.2 | 58.8 | 61.8 |
| Scull base | 39.5 | 39.2 | 36.4 |
| Ventricular | 1.3 | 2 | |
| Simpson Grade, % | |||
| 1° | 71.1 | 66.7 | 68.5 |
| 2° | 14.5 | 15.7 | 14.5 |
| 3° | 7.9 | 7.8 | 9.1 |
| 4° | 5.3 | 7.8 | 7.3 |
| Postoperative radiation, % | 28.9 | 31.4 | 30.9 |
| Tumor relapse, N (%) | 17 (22.4) | 11 (21.6) | 15 (27.3) |
| Univariate Analysis | Odds Ratio | 95%CI |
|---|---|---|
| Intra-tumoral heterogeneity | 0.19 | 0.02–1.61 |
| Multifocality | 0 | |
| Midline shift | 2.75 | 0.75–10.11 |
| Sinus invasion | 0.62 | 0.12–3.30 |
| Necrosis Hemorrhage | 2.71 | 0.78–9.38 |
| Mass effect | 4.67 | 0.54–40.11 |
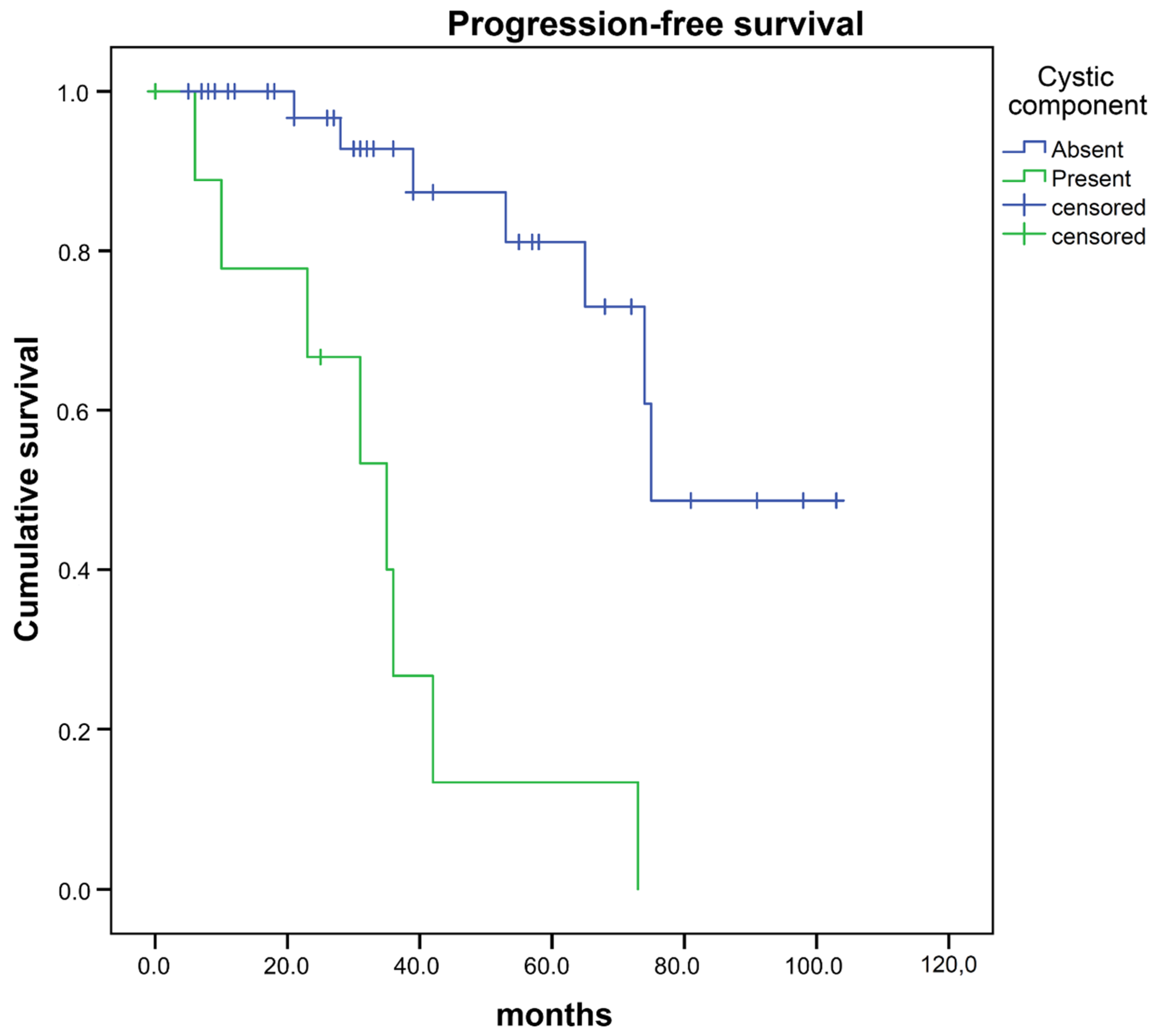
| Cystic component† | 21.74 | 3.79–124.54 |
| Bone invasion | 2.12 | 0.64–7.08 |
| Hyperostosis | 2.04 | 0.60–6.91 |
| Spiculation | 1.18 | 0.31–4.45 |
| Edema | 1.18 | 0.31–4.45 |
| High cluster prominence * | 3.79 | 0.93–15.47 |
| Multivariate Analysis | Hazard Ratio | 95%CI |
| Cystic component † | 20.21 | 2.46–166.02 |
| High cluster prominence †,* | 5.89 | 1.03–33.73 |
| Univariate Analysis | Odds Ratio | 95%CI |
|---|---|---|
| Completeness of resection † | 0.35 | 0.12–0.99 |
| Tumor localization ‡ | 1.62 | 0.59–4.47 |
| Gender | 0.44 | 0.17–1.17 |
| Age older than 65 years | 1.36 | 0.50–3.68 |
| Postoperative radiation | 2.12 | 0.81–5.53 |
| Cystic component † | 9.77 | 3.14–30.41 |
| High cluster prominence * | 1.15 | 0.32–4.09 |
| Multivariate Analysis | Hazard Ratio | 95%CI |
| Completeness of resection | 1.27 | 0.31–5.24 |
| Cystic component † | 22.74 | 4.29–120.66 |
| High cluster prominence * | 1.35 | 0.34–5.47 |
| Radiomic Characteristics | Semantic Characteristics | Clinical Characteristics |
|---|---|---|
| Mean | Intra-tumoral heterogeneity | Age |
| Median | Multifocality | Gender |
| Minimum | Midline shift | Tumor localization |
| Skewness | Sinus invasion | Completeness of resection |
| Spherical Disproportion | Necrosis/Hemorrhage | Postoperative radiation |
| Cluster Prominence | Mass effect | Progression-free survival |
| Difference Entropy | Cystic component | |
| Inverse Difference Normalized | Bone invasion | |
| Run Length Non-uniformity | Hyperostosis | |
| Short-Run Low Gray-Level Emphasis | Spiculation | |
| High-Intensity Large Area Emphasis | Edema | |
| Low-Intensity Large Area Emphasis | ||
| Low-Intensity Small Area Emphasis | ||
| Filters | ||
| Wavelet | ||
| Laplacian of Gaussian |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalasauskas, D.; Kronfeld, A.; Renovanz, M.; Kurz, E.; Leukel, P.; Krenzlin, H.; Brockmann, M.A.; Sommer, C.J.; Ringel, F.; Keric, N. Identification of High-Risk Atypical Meningiomas According to Semantic and Radiomic Features. Cancers 2020, 12, 2942. https://doi.org/10.3390/cancers12102942
Kalasauskas D, Kronfeld A, Renovanz M, Kurz E, Leukel P, Krenzlin H, Brockmann MA, Sommer CJ, Ringel F, Keric N. Identification of High-Risk Atypical Meningiomas According to Semantic and Radiomic Features. Cancers. 2020; 12(10):2942. https://doi.org/10.3390/cancers12102942
Chicago/Turabian StyleKalasauskas, Darius, Andrea Kronfeld, Mirjam Renovanz, Elena Kurz, Petra Leukel, Harald Krenzlin, Marc A. Brockmann, Clemens J. Sommer, Florian Ringel, and Naureen Keric. 2020. "Identification of High-Risk Atypical Meningiomas According to Semantic and Radiomic Features" Cancers 12, no. 10: 2942. https://doi.org/10.3390/cancers12102942





