The CINs of Polo-Like Kinase 1 in Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
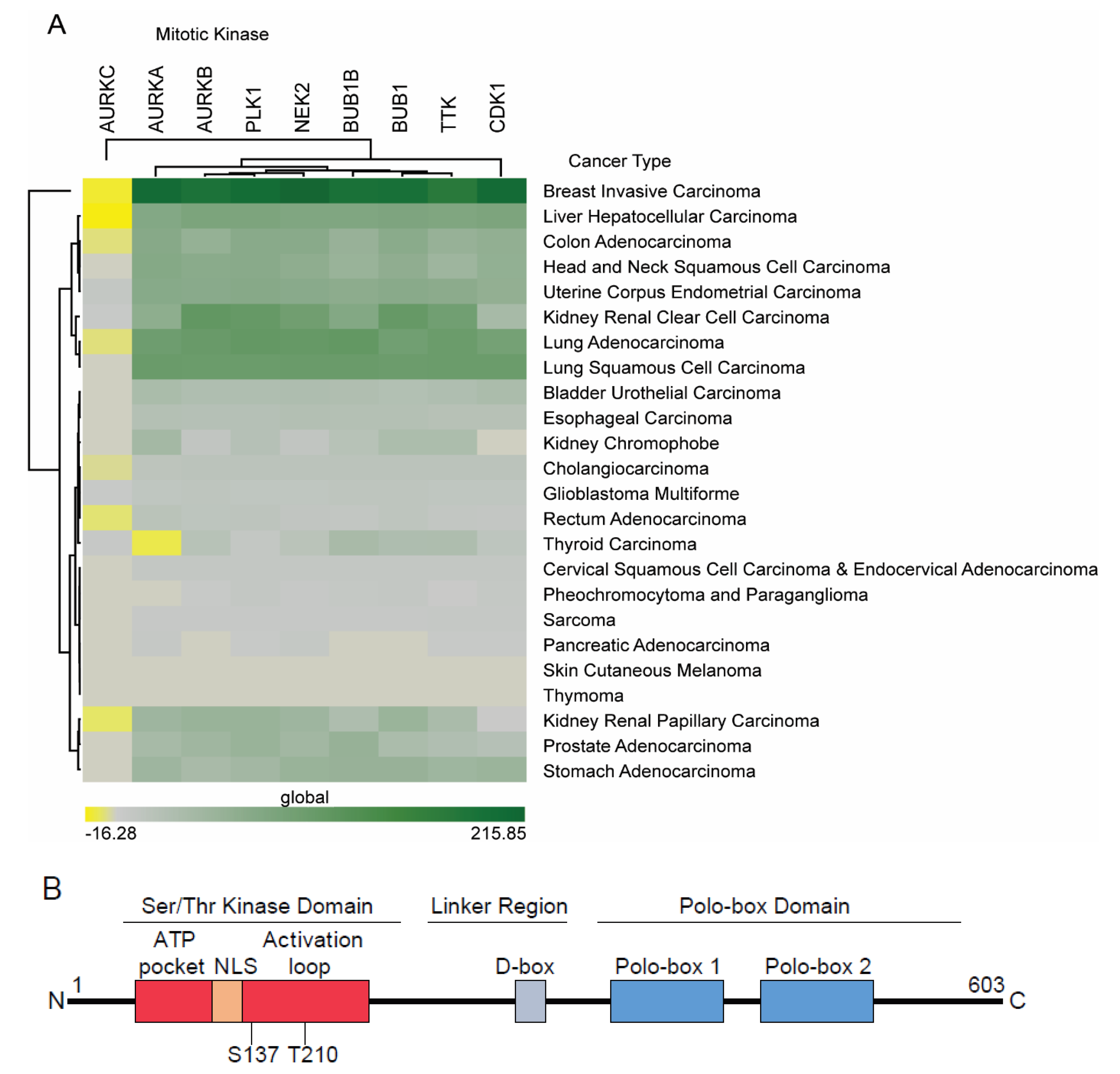
2. Regulation and Activity of PLK1 in the Cell Cycle
3. The Role of PLK1 in Driving Cell Cycle Progression
3.1. PLK1 and DNA Replication
3.2. PLK1 and Mitotic Entry
3.3. PLK1 and Mitotic Entry Following DNA Damage
4. Role of PLK1 during Mitosis and Cytokinesis
4.1. PLK1 and Centrosome Function
4.2. PLK1 and Chromosome Alignment
4.3. PLK1 and Kinetochore-Microtubule Dynamics
4.4. PLK1 and Cytokinesis
5. PLK1 and Maintenance of DNA Integrity
5.1. PLK1 and DNA Damage Checkpoint Function
5.2. PLK1 and DNA Damage Repair Pathways
5.3. PLK1 and Telomerase
6. Targeting Cancer Cells through PLK1
6.1. PLK1 Inhibitors as Therapeutic Agents and Associated Challenges
6.2. Genetic Interactions of PLK1 as Therapeutic Targets
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| PLK1 | Polo-like kinase 1 |
| CIN | Chromosomal instability |
| SDL | Synthetic dosage lethalality |
| MT | Microtubule |
| CDK1 | Cyclin dependent kinase 1 |
| AURKA/B/C | Aurora kinases A, B, C |
| NEK2 | NIMA related kinase 2 |
| CDC25C | Cell division cycle 25C |
| Bub1 | Budding uninhibited by benzimidazoles 1 |
| BubR | Budding uninhibited by benzimidazole-related |
| SAC | Spindle assembly checkpoint |
| APC/C | Anaphase promoting cyclosome proteasome complex |
| PBD | Polo-box domain |
| Hsp90 | Heat shock protein 90 |
| NLS | Nuclear localization signal |
| ATR | Ataxia-telangiectasia and Rad3 related |
| FoxM1 | Forkhead box protein M1 |
| CHEK1/2 | Checkpoint kinase 1/2 |
| ORC2 | Origin recognition complex subunit 2 |
| MRN | Mre11/Rad50/Nibrin |
| ATM | Ataxia-telangiectasia mutated |
| STK11 | Liver kinase B1 |
| γ-TuRC | γ-tubulin ring complex |
| Nlp or NINL | Ninein-like protein |
| NEDD1 | Neural precursor cell expressed developmentally down-regulated protein 1 |
| HAUS6 | HAUS augmin-like complex subunit 6 |
| MAP9 | MT-associated protein 9 |
| SMC | Structural maintenance of chromosomes |
| PICH | PLK1-interacting checkpoint helicase |
| PP2A | Protein phosphotase 2A |
| SGO1 | Shugoshin 1 |
| MELT | Met-Glu-Leu-Thr |
| CLIP-170 | Cytoplasmic linker protein |
| SGT1 | Suppressor of G2 allele of SKP1 |
| NudC | Nuclear distribution protein C |
| PRC1 | Protein regulator of cytokinesis 1 |
| CEP55 | Centrosomal protein 55 |
| KIF20A | Kinesin family member 20A |
| DNA-PKcs | DNA-dependent protein kinase catalytic subunit |
| BRCA1/2 | Hereditary breast cancer type 1/2 susceptibility protein |
| HR | Homologous recombination |
| NHEJ | Non-homologous end-joining |
| CK2 | Casein kinase 2 |
| DSB | Double strand DNA break |
| XRCC4 | X-ray cross complementing 4 |
| 53BP1 | TP53 binding protein |
| TERF1 | Telomeric repeat binding factor 1 |
| POT1 | Protection of telomeres protein 1 |
| TINF2 | TERF1 interacting nuclear factor 2 |
| TPP1 | Tripeptidyl-peptidase 1 |
| RAP1 | Repressor activator protein 1 |
| hTERT | Human telomerase reverse transcriptase |
| TNKS | Tankyrase |
| PARP | Poly-ADP-ribose polymerase |
| PINX1 | PIN2 Interacting Telomerase Inhibitor 1 |
| TIC | Tumor-initiating cell |
| AML | Acute myeloid leukemia |
| APC | Adenomatous polyposis coli protein |
| SL | Synthetic lethality |
| RAD54B | RAD54 homolog B |
References
- Dagogo-Jack, I.; Shaw, A.T. Tumour heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 2018, 15, 81–94. [Google Scholar] [PubMed]
- Yamamoto, Y.; Matsuyama, H.; Kawauchi, S.; Matsumoto, H.; Nagao, K.; Ohmi, C.; Sakano, S.; Furuya, T.; Oga, A.; Naito, K.; et al. Overexpression of polo-like kinase 1 (PLK1) and chromosomal instability in bladder cancer. Oncology 2006, 70, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Lengauer, C.; Kinzler, K.W.; Vogelstein, B. Genetic instability in colorectal cancers. Nature 1997, 10, 623–627. [Google Scholar]
- Weaver, B.A.; Cleveland, D.W. Does aneuploidy cause cancer? Curr. Opin. Cell Biol. 2006, 18, 658–667. [Google Scholar] [CrossRef] [PubMed]
- Smiraldo, P.G.; Gruver, A.M.; Osborn, J.C.; Pittman, D.L. Extensive chromosomal instability in Rad51d-deficient mouse cells. Cancer Res. 2005, 65, 2089–2096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burrell, R.A.; McClelland, S.E.; Endesfelder, D.; Groth, P.; Weller, M.-C.; Shaikh, N.; Domingo, E.; Kanu, N.; Dewhurst, S.M.; Gronross, E.; et al. Replication stress links structural and numerical cancer chromosomal instability. Nature 2013, 494, 492–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, H.; Lampson, M.; Efimov, A.; Yen, T.J. Chromosome instability in tumor cells due to defects in Aurora B mediated error correction at kinetochores. Cell Cycle 2018, 17, 2622–2636. [Google Scholar] [CrossRef] [Green Version]
- Ganem, N.J.; Godinho, S.A.; Pellman, D. A mechanism linking extra centrosomes to chromosomal instability. Nature 2009, 460, 278–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silkworth, W.T.; Cimini, D. Transient defects of mitotic spindle geometry and chromosome segregation errors. Cell Div. 2012, 7, 19. [Google Scholar] [CrossRef] [Green Version]
- Barber, T.D.; McManus, K.; Yuen, K.W.Y.; Reis, M.; Parmigiani, G.; Shen, D.; Barrett, I.; Nouhi, Y.; Spencer, F.; Markowitz, S. Chromatid cohesion defects may underlie chromosome instability in human colorectal cancers. Proc. Natl. Acad. Sci. USA 2008, 105, 3443–3448. [Google Scholar] [CrossRef] [Green Version]
- Nakayama, Y.; Soeda, S.; Ikeuchi, M.; Kakae, K.; Yamaguchi, N. Cytokinesis failure leading to chromosome instability in v-SRC-induced oncogenesis. Int. J. Mol. Sci. 2017, 18, 811. [Google Scholar]
- Boukamp, P.; Popp, S.; Krunic, D. Telomere-dependent chromosomal instability. J. Investig. Dermatol. Symp. Proc. 2005, 10, 89–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nigg, E.A. Mitotic kinases as regulators of cell division and its checkpoints. Nat. Rev. Mol. Cell Biol. 2001, 2, 21–32. [Google Scholar] [PubMed]
- Gheghiani, L.; Loew, D.; Lombard, B.; Mansfeld, J.; Gavet, O. PLK1 activation in late G2 sets up commitment to mitosis. Cell Rep. 2017, 19, 2060–2073. [Google Scholar] [CrossRef]
- Helps, N.R.; Luo, X.; Barker, H.M.; Cohen, P.T. NIMA-related kinase 2 (Nek2), a cell-cycle-regulated protein kinase localized to centrosomes, is complexed to protein phosphatase 1. Biochem. J. 2000, 349, 509–518. [Google Scholar] [CrossRef]
- De Luca, M.; Lavia, P.; Guarguaglini, G. A functional interplay between Aurora-A, Plk1 and TPX2 at spindle poles: Plk1 controls centrosomal localization of Aurora-A and TPX2 spindle association. Cell Cycle 2006, 5, 296–303. [Google Scholar] [CrossRef] [Green Version]
- Courthéoux, T.; Reboutier, D.; Vazeille, T.; Cremet, J.-Y.; Benaud, C.; Vernos, I.; Prigent, C. Microtubule nucleation during central spindle assembly requires NEDD1 phosphorylation on serine 405 by Aurora, A. J. Cell Sci. 2019, 132. Available online: http://jcs.biologists.org/content/132/10/jcs231118 (accessed on 18 September 2020). [CrossRef] [Green Version]
- Leber, B.; Maier, B.; Fuchs, F.; Chi, J.; Riffel, P.; Anderhub, S.; Wagner, L.; Ho, A.D.; Salisbury, J.L.; Boutros, M.; et al. Proteins required for centrosome clustering in cancer cells. Sci. Transl. Med. 2010, 2, 33–38. [Google Scholar] [CrossRef]
- Tipton, A.R.; Ji, W.; Sturt-Gillespie, B.; Bekier, M.E.; Wang, K.; Taylor, W.R.; Liu, S.T. Monopolar spindle 1 (MPS1) kinase promotes production of closed MAD2 (C-MAD2) conformer and assembly of the mitotic checkpoint complex. J. Biol. Chem. 2013, 288, 35149–35158. [Google Scholar] [CrossRef] [Green Version]
- Golan, A.; Yudkovsky, Y.; Hershko, A. The cyclin-ubiquitin ligase activity of cyclosome/APC is jointly activated by protein kinases Cdk1-cyclin B and Plk. J. Biol. Chem. 2002, 277, 15552–15557. [Google Scholar] [CrossRef] [Green Version]
- Ikeda, M.; Tanaka, K. Plk1 bound to Bub1 contributes to spindle assembly checkpoint activity during mitosis. Sci. Rep. 2017, 7, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.G.; Pereira, A.J.; Akhmanova, A.; Maiato, H. Aurora B spatially regulates EB3 phosphorylation to coordinate daughter cell adhesion with cytokinesis. J. Cell Biol. 2013, 201, 709–724. [Google Scholar]
- Tao, W. The mitotic checkpoint in cancer therapy. Cell Cycle 2005, 4, 1495–14999. [Google Scholar] [CrossRef] [Green Version]
- Prevo, R.; Pirovano, G.; Puliyadi, R.; Herbert, K.J.; Rodriguez-Berriguete, G.; O’Docherty, A.; Greaves, W.; McKenna, W.G.; Higgins, G.S. CDK1 inhibition sensitizes normal cells to DNA damage in a cell cycle dependent manner. Cell Cycle 2018, 17, 1513–1523. [Google Scholar] [PubMed]
- Kokuryo, T.; Yokoyama, Y.; Yamaguchi, J.; Tsunoda, N.; Ebata, T.; Nagino, M. NEK2 Is an effective target for cancer therapy with potential to induce regression of multiple human malignancies. Anticancer Res. 2019, 39, 2251–2258. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.; Gao, K.; Chu, L.; Zhang, R.; Yang, J.; Zheng, J. Aurora kinases: Novel therapy targets in cancers. Oncotarget 2017, 8, 23937–23954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricke, R.M.; Jeganathan, K.B.; van Deursen, J.M. Bub1 overexpression induces aneuploidy and tumor formation through Aurora B kinase hyperactivation. J. Cell Biol. 2011, 193, 1049–1064. [Google Scholar] [PubMed] [Green Version]
- Xie, Y.; Wang, A.; Lin, J.; Wu, L.; Zhang, H.; Yang, X.; Wan, X.; Miao, R.; Sang, X.; Zhao, H. Mps1/TTK: A novel target and biomarker for cancer. J. Drug Target 2017, 25, 112–118. [Google Scholar]
- Lens, S.M.A.; Voest, E.E.; Medema, R.H. Shared and separate functions of polo-like kinases and aurora kinases in cancer. Nat. Rev. Cancer 2010, 10, 825–841. [Google Scholar]
- Cheng, K.-Y.; Lowe, E.D.; Sinclair, J.; Nigg, E.A.; Johnson, L.N. The crystal structure of the human polo-like kinase-1 polo box domain and its phospho-peptide complex. EMBO J. 2003, 22, 5757–5768. [Google Scholar] [CrossRef] [Green Version]
- Elia, A.E.H.; Cantley, L.C.; Yaffe, M.B. Proteomic screen finds pSer/pThr-binding domain localizing Plk1 to mitotic substrates. Science 2003, 299, 1228–1231. [Google Scholar] [CrossRef] [PubMed]
- Seong, Y.-S.; Kamijo, K.; Lee, J.-S.; Fernandez, E.; Kuriyama, R.; Miki, T.; Lee, K.S. A spindle checkpoint arrest and a cytokinesis failure by the dominant-negative polo-box domain of Plk1 in U-2 OS cells. J. Biol. Chem. 2002, 277, 32282–32293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, Z.; Malureanu, L.; Huang, J.; Wang, W.; Li, H.; van Deursen, J.M.; Tindall, D.J.; Chen, J. Plk1-dependent phosphorylation of FoxM1 regulates a transcriptional programme required for mitotic progression. Nat. Cell Biol. 2008, 10, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Kraft, C.; Herzog, F.; Gieffers, C.; Mechtler, K.; Hagting, A.; Pines, J.; Peters, J.-M. Mitotic regulation of the human anaphase-promoting complex by phosphorylation. EMBO J. 2003, 22, 6598–6609. [Google Scholar] [CrossRef] [Green Version]
- Chan, E.H.Y.; Santamaria, A.; Silljé, H.H.W.; Nigg, E.A. Plk1 regulates mitotic Aurora A function through βTrCP-dependent degradation of hBora. Chromosoma 2008, 117, 457–469. [Google Scholar]
- Golsteyn, R.M.; Schultz, S.J.; Bartek, J.; Ziemiecki, A.; Ried, T.; Nigg, E.A. Cell cycle analysis and chromosomal localization of human Plk1, a putative homologue of the mitotic kinases Drosophila polo and Saccharomyces cerevisiae Cdc5. J. Cell Sci. 1994, 107, 1509–1517. [Google Scholar]
- Holtrich, U.; Wolf, G.; Bräuninger, A.; Karn, T.; Böhme, B.; Rübsamen-Waigmann, H.; Strebhardt, K. Induction and down-regulation of PLK, a human serine/threonine kinase expressed in proliferating cells and tumors. Proc. Natl. Acad. Sci. USA 1994, 91, 1736–1740. [Google Scholar] [CrossRef] [Green Version]
- Yuan, J.; Hörlin, A.; Hock, B.; Stutte, H.J.; Rübsamen-Waigmann, H.; Strebhardt, K. Polo-like kinase, a novel marker for cellular proliferation. Am. J. Pathol. 1997, 150, 1165–1172. [Google Scholar]
- Lu, L.-Y.; Wood, J.L.; Minter-Dykhouse, K.; Ye, L.; Saunders, T.L.; Yu, X.; Chen, J. Polo-like kinase 1 is essential for early embryonic development and tumor suppression. Mol. Cell Biol. 2008, 28, 6870–6876. [Google Scholar] [CrossRef] [Green Version]
- Uchiumi, T.; Longo, D.L.; Ferris, D.K. Cell cycle regulation of the human polo-like kinase (PLK) promoter. J. Biol. Chem. 1997, 272, 9166–9174. [Google Scholar] [CrossRef] [Green Version]
- Golsteyn, R.M.; Mundt, K.E.; Fry, A.M.; Nigg, E.A. Cell cycle regulation of the activity and subcellular localization of Plk1, a human protein kinase implicated in mitotic spindle function. J. Cell Biol. 1995, 129, 1617–1628. [Google Scholar] [CrossRef]
- Seki, A.; Coppinger, J.A.; Jang, C.-Y.; Yates, J.R.; Fang, G. Bora and the kinase Aurora a cooperatively activate the kinase Plk1 and control mitotic entry. Science 2008, 320, 1655–1658. [Google Scholar] [CrossRef] [Green Version]
- Giráldez, S.; Galindo-Moreno, M.; Limón-Mortés, M.C.; Rivas, A.C.; Herrero-Ruiz, J.; Mora-Santos, M.; Saez, C.; Japon, M.A.; Tortolero, M.; Romero, F. G1/S phase progression is regulated by PLK1 degradation through the CDK1/βTrCP axis. FASEB J. 2017, 31, 2925–2936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Cárcer, G. Heat shock protein 90 regulates the metaphase-anaphase transition in a polo-like kinase-dependent manner. Cancer Res. 2004, 64, 5106–5112. [Google Scholar] [CrossRef]
- Mundt, K.E.; Golsteyn, R.M.; Lane, H.A.; Nigg, E.A. On the regulation and function of human polo-like kinase 1 (PLK1): Effects of overexpression on cell cycle progression. Biochem. Biophys. Res. Commun. 1997, 239, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.-J.; Ma, S.; Terada, Y.; Erikson, R.L. Phosphorylation of threonine 210 and the role of serine 137 in the regulation of mammalian polo-like kinase. J. Biol. Chem. 2002, 277, 44115–44120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van de Weerdt, B.C.M.; van Vugt, M.A.T.M.; Lindon, C.; Kauw, J.J.W.; Rozendaal, M.J.; Klompmaker, R.; Wolthuis, R.M.F.; Medema, R.H. Uncoupling anaphase-promoting complex/cyclosome activity from spindle assembly checkpoint control by deregulating polo-like kinase 1. Mol. Cell Biol. 2005, 25, 2031–2044. [Google Scholar] [PubMed] [Green Version]
- Jang, Y.-J.; Lin, C.-Y.; Ma, S.; Erikson, R.L. Functional studies on the role of the C-terminal domain of mammalian polo-like kinase. Proc. Natl. Acad. Sci. USA 2002, 99, 1984–1989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petronczki, M.; Glotzer, M.; Kraut, N.; Peters, J.-M. Polo-like kinase 1 triggers the initiation of cytokinesis in human cells by promoting recruitment of the RhoGEF Ect2 to the central spindle. Dev. Cell. 2007, 12, 713–725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taniguchi, E.; Toyoshima-Morimoto, F.; Nishida, E. Nuclear translocation of Plk1 mediated by its bipartite nuclear localization signal. J. Biol. Chem. 2002, 277, 48884–48888. [Google Scholar] [CrossRef] [Green Version]
- Kishi, K.; van Vugt, M.A.T.M.; Okamoto, K.; Hayashi, Y.; Yaffe, M.B. Functional dynamics of polo-like kinase 1 at the centrosome. Mol. Cell Biol. 2009, 29, 3134–3150. [Google Scholar] [PubMed] [Green Version]
- Lemmens, B.; Hegarat, N.; Akopyan, K.; Sala-Gaston, J.; Bartek, J.; Hochegger, H.; Lindqvist, A. DNA Replication Determines Timing of Mitosis by Restricting CDK1 and PLK1 Activation. Mol. Cell. 2018, 71, 117–128. [Google Scholar] [CrossRef] [Green Version]
- Saldivar, J.C.; Hamperl, S.; Bocek, M.J.; Chung, M.; Bass, T.E.; Cisneros-Soberanis, F.; Samejina, K.; Xie, L.; Paulson, J.R.; Earnshaw, W.C.; et al. An intrinsic S/G2 checkpoint enforced by ATR. Science 2018, 24, 806–810. [Google Scholar]
- Akopyan, K.; Silva Cascales, H.; Hukasova, E.; Saurin, A.T.; Müllers, E.; Jaiswal, H.; Hollamn, D.A.A.; Kops, G.J.P.L.; Medema, R.H.; Lindqvist, A. Assessing kinetics from fixed cells reveals activation of the mitotic entry network at the S/G2 transition. Mol Cell. 2014, 6, 843–853. [Google Scholar]
- Song, B.; Liu, X.S.; Davis, K.; Liu, X. Plk1 phosphorylation of Orc2 promotes DNA replication under conditions of stress. Mol. Cell Biol. 2011, 31, 4844–4856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yim, H.; Erikson, R.L. Polo-like kinase 1 depletion induces DNA damage in early S prior to caspase activation. Mol. Cell Biol. 2009, 29, 2609–2621. [Google Scholar]
- Toyoshima-Morimoto, F.; Taniguchi, E.; Shinya, N.; Iwamatsu, A.; Nishida, E. Polo-like kinase 1 phosphorylates cyclin B1 and targets it to the nucleus during prophase. Nature 2001, 410, 215–220. [Google Scholar] [CrossRef]
- Toyoshima-Morimoto, F.; Taniguchi, E.; Nishida, E. Plk1 promotes nuclear translocation of human Cdc25C during prophase. EMBO Rep. 2002, 3, 341–348. [Google Scholar]
- Lewis, C.W.; Golsteyn, R.M. Cancer cells that survive checkpoint adaptation contain micronuclei that harbor damaged DNA. Cell Cycle 2016, 15, 3131–3145. [Google Scholar]
- Syljuåsen, R.G.; Jensen, S.; Bartek, J.; Lukas, J. Adaptation to the ionizing radiation-induced G2 checkpoint occurs in human cells and depends on checkpoint kinase 1 and Polo-like kinase 1 kinases. Cancer Res. 2006, 66, 10253–10257. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Li, J.; Kong, Y.; Yan, S.; Ahmad, N.; Liu, X. Plk1 phosphorylation of Mre11 antagonizes the DNA damage response. Cancer Res. 2017, 15, 3169–3180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.S.; Li, H.; Song, B.; Liu, X. Polo-like kinase 1 phosphorylation of G2 and S-phase-expressed 1 protein is essential for p53 inactivation during G2 checkpoint recovery. EMBO Rep. 2010, 11, 626–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; Li, H.; Zhou, Z.; Wang, W.-H.; Deng, A.; Andrisani, O.; Liu, X.S. Plk1-mediated Phosphorylation of Topors Regulates p53 Stability. J. Biol. Chem. 2009, 284, 18588–18592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ando, K.; Ozaki, T.; Yamamoto, H.; Furuya, K.; Hosoda, M.; Hayashi, S.; Fukuzawa, M.; Nakagawara, A. Polo-like Kinase 1 (Plk1) Inhibits p53 Function by Physical Interaction and Phosphorylation. J. Biol. Chem. 2004, 279, 25549–25561. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Erikson, R.L. Activation of Cdc2/cyclin B and inhibition of centrosome amplification in cells depleted of Plk1 by siRNA. Proc. Natl. Acad. Sci. USA 2002, 99, 8672–8676. [Google Scholar] [CrossRef] [Green Version]
- Tsou, M.-F.B.; Wang, W.-J.; George, K.A.; Uryu, K.; Stearns, T.; Jallepalli, P.V. Polo kinase and separase regulate the mitotic licensing of centriole duplication in human cells. Dev. Cell 2009, 17, 344–354. [Google Scholar] [CrossRef] [Green Version]
- Shukla, A.; Kong, D.; Sharma, M.; Magidson, V.; Loncarek, J. Plk1 relieves centriole block to reduplication by promoting daughter centriole maturation. Nat. Commun. 2015, 6, 8077. [Google Scholar]
- Zou, J.; Zhang, D.; Qin, G.; Chen, X.; Wang, H.; Zhang, D. BRCA1 and FancJ cooperatively promote interstrand crosslinker induced centrosome amplification through the activation of polo-like kinase 1. Cell Cycle 2014, 13, 3685–3697. [Google Scholar] [CrossRef] [Green Version]
- Werle, K.; Chen, J.; Xu, H.-G.; Zhao, R.-X.; He, Q.; Lu, C.; Cui, R.; Liang, J.; Li, Y.-L.; Xu, Z.-X. Liver kinase B1 regulates the centrosome via PLK1. Cell Death Dis. 2014, 5, e1157. [Google Scholar]
- Izumi, H.; Matsumoto, Y.; Ikeuchi, T.; Saya, H.; Kajii, T.; Matsuura, S. BubR1 localizes to centrosomes and uppresses centrosome amplification via regulating Plk1 activity in interphase cells. Oncogene 2009, 28, 2806–2820. [Google Scholar]
- Yamashiro, S.; Yamakita, Y.; Totsukawa, G.; Goto, H.; Kaibuchi, K.; Ito, M.; Hartshorne, D.J.; Matsumura, F. Myosin phosphatase-targeting subunit 1 regulates mitosis by antagonizing polo-like kinase 1. Dev. Cell 2008, 14, 787–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nai, S.; Shi, Y.; Ru, H.; Ding, Y.; Geng, Q.; Li, Z.; Dong, M.-Q.; Xu, X.; Li, J. Chk2-dependent phosphorylation of myosin phosphatase targeting subunit 1 (MYPT1) regulates centrosome maturation. Cell Cycle 2019, 18, 2651–2659. [Google Scholar] [CrossRef] [PubMed]
- Casenghi, M.; Meraldi, P.; Weinhart, U.; Duncan, P.I.; Körner, R.; Nigg, E.A. Polo-like Kinase 1 Regulates Nlp, a Centrosome Protein Involved in Microtubule Nucleation. Dev. Cell 2003, 5, 113–125. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Chen, Q.; Feng, J.; Hou, J.; Yang, F.; Liu, J.; Jiang, Q.; Zhang, C. Sequential phosphorylation of Nedd1 by Cdk1 and Plk1 is required for targeting of the TuRC to the centrosome. J. Cell Sci. 2009, 122, 2240–2251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, H.; Fang, K.; Fang, G. FAM29A, a target of Plk1 regulation, controls the partitioning of NEDD1 between the mitotic spindle and the centrosomes. J. Cell Sci. 2009, 122, 2750–2759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eot-Houllier, G.; Venoux, M.; Vidal-Eychenié, S.; Hoang, M.-T.; Giorgi, D.; Rouquier, S. Plk1 Regulates Both ASAP Localization and Its Role in Spindle Pole Integrity. J. Biol. Chem. 2010, 285, 29556–29568. [Google Scholar] [CrossRef] [Green Version]
- Oshimori, N.; Ohsugi, M.; Yamamoto, T. The Plk1 target Kizuna stabilizes mitotic centrosomes to ensure spindle bipolarity. Nat. Cell Biol. 2006, 8, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Morris, E.J.; Kawamura, E.; Gillespie, J.A.; Balgi, A.; Kannan, N.; Muller, W.J.; Roberge, M.; Dedhar, S. Stat3 regulates centrosome clustering in cancer cells via Stathmin/PLK1. Nat. Commun. 2017, 8, 15289. [Google Scholar] [CrossRef]
- Smith, E.; Hégarat, N.; Vesely, C.; Roseboom, I.; Larch, C.; Streicher, H.; Straatman, K.; Flynn, H.; Skehel, M.; Hirota, T.; et al. Differential control of Eg5-dependent centrosome separation by Plk1 and Cdk1. EMBO J. 2011, 30, 2233–2245. [Google Scholar] [CrossRef] [Green Version]
- Bertran, M.T.; Sdelci, S.; Regué, L.; Avruch, J.; Caelles, C.; Roig, J. Nek9 is a Plk1-activated kinase that controls early centrosome separation through Nek6/7 and Eg5. EMBO J. 2011, 30, 2634–2647. [Google Scholar]
- Marthiens, V.; Piel, M.; Basto, R. Never tear us apart—The importance of centrosome clustering. J. Cell Sci. 2012, 125, 3281–3292. [Google Scholar] [CrossRef] [Green Version]
- Kagami, Y.; Ono, M.; Yoshida, K. Plk1 phosphorylation of CAP-H2 triggers chromosome condensation by condensin II at the early phase of mitosis. Sci. Rep. 2017, 7, 5583. [Google Scholar] [PubMed] [Green Version]
- Abe, S.; Nagasaka, K.; Hirayama, Y.; Kozuka-Hata, H.; Oyama, M.; Aoyagi, Y.; Obuse, C.; Hirota, T. The initial phase of chromosome condensation requires Cdk1-mediated phosphorylation of the CAP-D3 subunit of condensin II. Genes Dev. 2011, 25, 863–874. [Google Scholar] [PubMed] [Green Version]
- Dai, J.; Sullivan, B.A.; Higgins, J.M.G. Regulation of mitotic chromosome cohesion by Haspin and Aurora, B. Dev. Cell 2006, 11, 741–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, L.; Tian, X.; Zhu, C.; Wang, F.; Higgins, J.M.G. Polo-like kinase-1 triggers histone phosphorylation by Haspin in mitosis. EMBO Rep. 2014, 15, 273–281. [Google Scholar] [PubMed]
- Kang, Y.H.; Park, J.-E.; Yu, L.-R.; Soung, N.-K.; Yun, S.-M.; Bang, J.K.; Seong, Y.-S.; Yu, H.; Garfield, S.; Veenstra, T.; et al. Self-regulated Plk1 recruitment to kinetochores by the Plk1-PBIP1 interaction is critical for proper chromosome segregation. Mol. Cell 2006, 24, 409–422. [Google Scholar] [CrossRef]
- Sumara, I.; Vorlaufer, E.; Stukenberg, P.; Kelm, O.; Redemann, N.; Nigg, E.A.; Peters, J.-M. The dissociation of cohesin from chromosomes in prophase is regulated by polo-like kinase. Mol. Cell 2002, 9, 515–525. [Google Scholar] [CrossRef]
- Kurasawa, Y.; Yu-Lee, L.-Y. PICH and Cotargeted Plk1 Coordinately Maintain Prometaphase Chromosome Arm Architecture. Mol. Biol. Cell 2010, 21, 1188–1199. [Google Scholar] [CrossRef] [Green Version]
- Tang, Z.; Shu, H.; Qi, W.; Mahmood, N.A.; Mumby, M.C.; Yu, H. PP2A Is Required for Centromeric Localization of Sgo1 and Proper Chromosome Segregation. Dev. Cell 2006, 10, 575–585. [Google Scholar] [CrossRef] [Green Version]
- Von Schubert, C.; Cubizolles, F.; Bracher, J.M.; Sliedrecht, T.; Kops, G.J.; Nigg, E.A. Plk1 and Mps1 Cooperatively Regulate the Spindle Assembly Checkpoint in Human Cells. Cell Rep. 2015, 12, 66–78. [Google Scholar] [CrossRef] [Green Version]
- Bollen, M. Kinetochore signalling: The KIss that MELTs Knl1. Curr. Biol. 2014, 24, R68–R70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Liu, X.S.; Yang, X.; Wang, Y.; Wang, Y.; Turner, J.R.; Liu, X. Phosphorylation of CLIP-170 by Plk1 and CK2 promotes timely formation of kinetochore–microtubule attachments. EMBO J. 2010, 29, 2953–2965. [Google Scholar] [PubMed] [Green Version]
- Liu, X.S.; Song, B.; Tang, J.; Liu, W.; Kuang, S.; Liu, X. Plk1 Phosphorylates Sgt1 at the Kinetochores to Promote Timely Kinetochore-Microtubule Attachment. Mol. Cell. Biol. 2012, 32, 4053–4067. [Google Scholar] [PubMed] [Green Version]
- Liu, D.; Davydenko, O.; Lampson, M.A. Polo-like kinase-1 regulates kinetochore–microtubule dynamics and spindle checkpoint silencing. J. Cell Biol. 2012, 198, 491–499. [Google Scholar] [PubMed]
- Bakhoum, S.F.; Thompson, S.L.; Manning, A.L.; Compton, D.A. Genome stability is ensured by temporal control of kinetochore–microtubule dynamics. Nat. Cell Biol. 2008, 11, 27–35. [Google Scholar] [PubMed] [Green Version]
- Dumitru, A.M.G.; Rusin, S.F.; Clark, A.E.M.; Kettenbach, A.N.; Compton, D.A. Cyclin A/Cdk1 modulates Plk1 activity in prometaphase to regulate kinetochore-microtubule attachment stability. ELife 2017, 6, e29303. [Google Scholar]
- Ahonen, L.J.; Kallio, M.J.; Daum, J.R.; Bolton, M.; Manke, I.A.; Yaffe, M.B.; Stukenberg, P.T.; Gorbsky, G.J. Polo-like kinase 1 creates the tension-sensing 3F3/2 phosphoepitope and modulates the association of spindle-checkpoint proteins at kinetochores. Curr. Biol. 2005, 15, 1078–1089. [Google Scholar] [CrossRef] [Green Version]
- Van Vugt, M.A.T.M.; Van De Weerdt, B.C.M.; Vader, G.; Janssen, H.; Calafat, J.; Klompmaker, R.; Wolthuis, R.M.F.; Medema, R.H.; Yakunin, A.F.; Proudfoot, M.; et al. Polo-like kinase-1 is required for bipolar spindle formation but is dispensable for anaphase promoting complex/cdc20 Activation and Initiation of cytokinesis. J. Biol. Chem. 2004, 279, 36841–368540. [Google Scholar]
- Daum, J.R.; Tugendreich, S.; Topper, L.M.; Jorgensen, P.M.; Hoog, C.; Hieter, P.; Gorbsky, G.J. The 3F3/2 anti-phosphoepitope antibody binds the mitotically phosphorylated anaphase-promoting complex/cyclosome. Curr. Biol. 2000, 10, R850–R852. [Google Scholar] [CrossRef] [Green Version]
- Nishino, M.; Kurasawa, Y.; Evans, R.; Lin, S.-H.; Brinkley, B.R.; Yu-Lee, L.-Y. NudC Is Required for Plk1 Targeting to the Kinetochore and Chromosome Congression. Curr. Biol. 2006, 16, 1414–1421. [Google Scholar] [CrossRef] [Green Version]
- Glotzer, M. The 3Ms of central spindle assembly: Microtubules, motors and MAPs. Nat. Rev. Mol. Cell Biol. 2009, 10, 9–209. [Google Scholar] [PubMed] [Green Version]
- Neef, R.; Preisinger, C.; Sutcliffe, J.; Kopajtich, R.; Nigg, E.A.; Mayer, T.U.; Barr, F.A. Phosphorylation of mitotic kinesin-like protein 2 by polo-like kinase 1 is required for cytokinesis. J. Cell Biol. 2003, 162, 863–876. [Google Scholar]
- Liu, X.; Zhou, T.; Kuriyama, R.; Erikson, R.L. Molecular interactions of Polo-like-kinase 1 with the mitotic kinesin-like protein CHO1/MKLP-1. J. Cell Sci. 2004, 117, 3233–3246. [Google Scholar] [PubMed] [Green Version]
- Zhang, L.; Shao, H.; Huang, Y.; Yan, F.; Chu, Y.; Hou, H.; Zhu, M.; Fu, C.; Aikhionbare, F.; Fang, G.; et al. PLK1 phosphorylates mitotic centromere-associated kinesin and promotes its depolymerase activity. J. Biol. Chem. 2010, 286, 3033–3046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakhoum, S.F.; Genovese, G.; Compton, D.A. Deviant kinetochore microtubule dynamics underlie chromosomal instability. Curr. Biol. 2009, 19, 1937–1942. [Google Scholar] [CrossRef] [Green Version]
- Lindon, C.; Pines, J. Ordered proteolysis in anaphase inactivates Plk1 to contribute to proper mitotic exit in human cells. J. Cell Biol. 2004, 164, 233–241. [Google Scholar] [CrossRef] [Green Version]
- De Cárcer, G.; Venkateswaran, S.V.; Salgueiro, L.; El Bakkali, A.; Somogyi, K.; Rowald, K.; Montañés, P.; Sanclemente, M.; Escobar, B.; De Martino, A.; et al. Plk1 overexpression induces chromosomal instability and suppresses tumor development. Nat. Commun. 2018, 9, 3012. [Google Scholar]
- Adriaans, I.E.; Basant, A.; Ponsioen, B.; Glotzer, M.; Lens, S.M.A. PLK1 plays dual roles in centralspindlin regulation during cytokinesis. J. Cell Biol. 2019, 218, 1250–1264. [Google Scholar] [CrossRef] [Green Version]
- Burkard, M.E.; Maciejowski, J.; Rodríguez-Bravo, V.; Repka, M.; Lowery, E.M.; Clauser, K.R.; Zhang, C.; Shokat, K.M.; Carr, S.A.; Yaffe, M.B.; et al. Plk1 self-organization and priming phosphorylation of HsCYK-4 at the spindle midzone regulate the onset of division in human cells. PLoS Biol. 2009, 7, e1000111. [Google Scholar] [CrossRef] [Green Version]
- Burkard, M.E.; Randall, C.L.; LaRochelle, S.; Zhang, C.; Shokat, K.M.; Fisher, R.P.; Jallepalli, P.V. Chemical genetics reveals the requirement for Polo-like kinase 1 activity in positioning RhoA and triggering cytokinesis in human cells. Proc. Natl. Acad. Sci. USA 2007, 104, 4383–4388. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.-C.; Wu, C.-H.; Yen, T.-C.; Ouyang, P. centrosomal protein 55 (Cep55) stability is negatively regulated by p53 protein through polo-like kinase 1 (Plk1). J. Biol. Chem. 2011, 287, 4376–4385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastos, R.N.; Barr, F.A. Plk1 negatively regulates Cep55 recruitment to the midbody to ensure orderly abscission. J. Cell Biol. 2010, 191, 751–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fabbro, M.; Zhou, B.-B.; Takahashi, M.; Sarcevic, B.; Lal, P.; Graham, M.E.; Gabrielli, B.G.; Robinson, P.J.; Nigg, E.A.; Ono, Y.; et al. Cdk1/Erk2- and Plk1-dependent phosphorylation of a centrosome protein, Cep55, is required for its recruitment to midbody and cytokinesis. Dev. Cell 2005, 9, 477–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smits, V.A.J.; Klompmaker, R.; Arnaud, L.; Rijksen, G.; Nigg, E.A.; Medema, R.H. Polo-like kinase-1 is a target of the DNA damage checkpoint. Nat. Cell Biol. 2000, 2, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Van Vugt, M.A.T.M.; Smits, V.A.J.; Klompmaker, R.; Medema, R.H. Inhibition of Polo-like Kinase-1 by DNA Damage Occurs in an ATM- or ATR-dependent Fashion. J. Biol. Chem. 2001, 276, 41656–41660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.-J.; Hwang, H.-I.; Jang, Y.-J. Mitotic DNA damage response: Polo-like Kinase-1 is dephosphorylated through ATM-Chk1 pathway. Cell Cycle 2010, 9, 2389–2398. [Google Scholar] [CrossRef]
- Tsvetkov, L.; Stern, D.F. Phosphorylation of Plk1 at S137 and T210 is Inhibited in Response to DNA Damage. Cell Cycle 2004, 4, 166–171. [Google Scholar] [CrossRef] [Green Version]
- Bruinsma, W.; Aprelia, M.; García-Santisteban, I.; Kool, J.; Xu, Y.J.; Medema, R.H. Inhibition of Polo-like kinase 1 during the DNA damage response is mediated through loss of Aurora A recruitment by Bora. Oncogene 2016, 36, 1840–1848. [Google Scholar] [CrossRef] [Green Version]
- Van Vugt, M.A.T.M.; Gardino, A.K.; Linding, R.; Ostheimer, G.J.; Reinhardt, H.C.; Ong, S.-E.; Tan, C.S.; Miao, H.; Keezer, S.M.; Li, J.; et al. A mitotic phosphorylation feedback network connects Cdk1, Plk1, 53BP1, and Chk2 to Inactivate the G2/M DNA Damage Checkpoint. PLoS Biol. 2010, 8, e1000287. [Google Scholar]
- Douglas, P.; Ye, R.; Trinkle-Mulcahy, L.; Neal, J.A.; De Wever, V.; Morrice, N.A.; Meek, K.; Lees-Miller, S.P. Polo-like kinase 1 (PLK1) and protein phosphatase 6 (PP6) regulate DNA-dependent protein kinase catalytic subunit (DNA-PKcs) phosphorylation in mitosis. Biosci. Rep. 2014, 34, 257–271. [Google Scholar]
- Lee, K.-J.; Shang, Z.-F.; Lin, Y.-F.; Sun, J.; Morotomi-Yano, K.; Saha, D.; Chen, B.P. The Catalytic Subunit of DNA-Dependent Protein Kinase Coordinates with Polo-Like Kinase 1 to Facilitate Mitotic Entry. Neoplasia 2015, 17, 329–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mamely, I.; Van Vugt, M.A.; Smits, V.A.J.; Semple, J.I.; Lemmens, B.; Perrakis, A.; Medema, R.H.; Freire, R. Polo-like Kinase-1 Controls Proteasome-Dependent Degradation of Claspin during Checkpoint Recovery. Curr. Biol. 2006, 16, 1950–1955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macůrek, L.; Lindqvist, A.; Lim, D.; Lampson, M.A.; Klompmaker, R.; Freire, R.; Clouin, C.; Taylor, S.S.; Yaffe, M.B.; Medema, R.H. Polo-like kinase-1 is activated by aurora A to promote checkpoint recovery. Nat. Cell Biol. 2008, 455, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Wakida, T.; Ikura, M.; Kuriya, K.; Ito, S.; Shiroiwa, Y.; Habu, T.; Kawamoto, T.; Okumura, K.; Ikura, T.; Furuya, K. The CDK-PLK1 axis targets the DNA damage checkpoint sensor protein RAD9 to promote cell proliferation and tolerance to genotoxic stress. ELife 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Yuan, J.-H.; Feng, Y.; Fisher, R.H.; Maloid, S.; Longo, D.L.; Ferris, D.K. Polo-Like Kinase 1 inactivation following mitotic dna damaging treatments is independent of ataxia telangiectasia mutated kinase11federal funds from the National Cancer Institute, NIH, under contract NO1-CO-12400.Note: The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. Mol Cancer Res. 2004, 2, 417–426. [Google Scholar] [PubMed]
- Yata, K.; Lloyd, J.; Maslen, S.; Bleuyard, J.-Y.; Skehel, M.; Smerdon, S.J.; Esashi, F. Plk1 and CK2 Act in Concert to Regulate Rad51 during DNA Double Strand Break Repair. Mol. Cell 2012, 45, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Daniels, M.J.; Venkitaraman, A.R. Phosphorylation of BRCA2 by the Polo-like kinase Plk1 is regulated by DNA damage and mitotic progression. Oncogene 2003, 23, 865–872. [Google Scholar] [CrossRef] [Green Version]
- Terasawa, M.; Shinohara, A.; Shinohara, M. Canonical Non-Homologous End Joining in Mitosis Induces Genome Instability and Is Suppressed by M-phase-Specific Phosphorylation of XRCC4. PLoS Genet. 2014, 10, e10045633. [Google Scholar]
- Benada, J.; Burdová, K.; Lidak, T.; Von Morgen, P.; Macurek, L. Polo-like kinase 1 inhibits DNA damage response during mitosis. Cell Cycle 2015, 14, 219–231. [Google Scholar] [CrossRef] [Green Version]
- Orthwein, A.; Fradet-Turcotte, A.; Noordermeer, S.M.; Canny, M.D.; Brun, C.M.; Strecker, J.; Escribano-Diaz, C.; Durocher, D. Mitosis Inhibits DNA Double-Strand Break Repair to Guard Against Telomere Fusions. Science 2014, 344, 189–193. [Google Scholar] [CrossRef]
- Huang, Y.; Sun, L.; Liu, N.; Wei, Q.; Jiang, L.; Tong, X.; Ye, X. Polo-like Kinase 1 (Plk1) Up-regulates Telomerase Activity by Affecting Human Telomerase Reverse Transcriptase (hTERT) Stability. J. Biol. Chem. 2015, 290, 18865–18873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Lange, T. Shelterin: The protein complex that shapes and safeguards human telomeres. Genes Dev. 2005, 19, 2100–2110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez, P.; Thanasoula, M.; Muñoz, P.; Liao, C.; Tejera, A.; McNees, C.; Flores, J.M.; Fernández-Capetillo, O.; Tarsounas, M.; Blasco, M.A. Increased telomere fragility and fusions resulting from TRF1 deficiency lead to degenerative pathologies and increased cancer in mice. Genes Dev. 2009, 23, 2060–2075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shay, J.; Bacchetti, S. A survey of telomerase activity in human cancer. Eur. J. Cancer 1997, 33, 787–791. [Google Scholar] [CrossRef]
- Leão, R.R.; Apolónio, J.D.; Lee, D.; Figueiredo, A.; Tabori, U.; Castelo-Branco, P. Mechanisms of human telomerase reverse transcriptase (hTERT) regulation: Clinical impacts in cancer. J. Biomed. Sci. 2018, 25, 22. [Google Scholar]
- Ha, G.-H.; Kim, H.-S.; Go, H.; Lee, H.; Seimiya, H.; Chung, D.H.; Lee, C.-W. Tankyrase-1 function at telomeres and during mitosis is regulated by Polo-like kinase-1-mediated phosphorylation. Cell Death Differ. 2011, 19, 321–332. [Google Scholar] [CrossRef] [Green Version]
- Smith, S. Tankyrase, a Poly(ADP-Ribose) Polymerase at Human Telomeres. Science 1998, 282, 1484–1487. [Google Scholar] [CrossRef] [Green Version]
- Wu, Z.-Q.; Yang, X.; Weber, G.; Liu, X.S. Plk1 Phosphorylation of TRF1 Is Essential for Its Binding to Telomeres. J. Biol. Chem. 2008, 283, 25503–25513. [Google Scholar] [CrossRef] [Green Version]
- Pang, Q.; Qian, D.; Cheng, J.; Ding, X.; Chen, X.; Chen, X.; Guan, Y.; Zhang, B.; Wang, J.; Er, P.; et al. PinX1 suppresses tumorigenesis by negatively regulating telomerase/telomeres in colorectal carcinoma cells and is a promising molecular marker for patient prognosis. OncoTargets Ther. 2016, 9, 4821–4831. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Yu, J.; Yuan, K.; Lan, J.; Jin, C.; Huang, H. Plk1-mediated mitotic phosphorylation of PinX1 regulates its stability. Eur. J. Cell Biol. 2010, 89, 748–756. [Google Scholar]
- Yuan, X.; Larsson, C.; Xu, D. Mechanisms underlying the activation of TERT transcription and telomerase activity in human cancer: Old actors and new players. Oncogene 2019, 38, 6172–6183. [Google Scholar]
- Chen, Z.; Koeneman, K.S.; Corey, D.R. Consequences of telomerase inhibition and combination treatments for the proliferation of cancer cells. Cancer Res. 2003, 63, 5917–5925. [Google Scholar] [PubMed]
- Falchetti, M.L.; Pallini, R.; Levi, A. Telomerase and Cancer. Am. J. Cancer 2004, 3, 1–11. [Google Scholar] [CrossRef]
- Bentham Science Publisher; Cunningham, A.; Love, W.; Zhang, R.; Andrews, L.; Tollefsbol, T. Telomerase inhibition in cancer therapeutics: Molecular-based approaches. Curr. Med. Chem. 2006, 13, 2875–2888. [Google Scholar] [PubMed]
- Wu, X.; Zhang, J.; Yang, S.; Kuang, Z.; Tan, G.; Yang, G.; Wei, Q.; Guo, Z. Telomerase antagonist imetelstat increases radiation sensitivity in esophageal squamous cell carcinoma. Oncotarget 2017, 8, 13600–13610. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, Z.G.; Gellert, G.C.; Jackson, S.; Gryaznov, S.; Tressler, R.; Dogan, P.; Wright, W.E.; Shay, J.W. In vivoInhibition of Lung Cancer by GRN163L: A Novel Human Telomerase Inhibitor. Cancer Res. 2005, 65, 7866–7873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frink, R.E.; Peyton, M.; Schiller, J.H.; Gazdar, A.F.; Shay, J.W.; Minna, J.D. Telomerase inhibitor imetelstat has preclinical activity across the spectrum of non-small cell lung cancer oncogenotypes in a telomere length dependent manner. Oncotarget 2016, 7, 31639–31651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, E.S.; Wu, K.; Chin, A.C.; Chen-Kiang, S.; Pongracz, K.; Gryaznov, S.; Moore, M.A.S. Telomerase inhibition with an oligonucleotide telomerase template antagonist: In vitro and in vivo studies in multiple myeloma and lymphoma. Blood 2004, 103, 258–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akiyama, M.; Hideshima, T.; Shammas, M.A.; Hayashi, T.; Hamasaki, M.; Tai, Y.T.; Richardson, P.; Gryaznov, S.; Munshi, N.C.; Anderson, K.C. Effects of oligonucleotide N3′→P5′ thio-phosphoramidate (GRN163) targeting telomerase RNA in human multiple myeloma cells. Cancer Res. 2003, 63, 6187–6194. [Google Scholar]
- Wang, X.; Hu, C.S.; Petersen, B.; Qiu, J.; Ye, F.; Houldsworth, J.; Eng, K.; Huang, F.; Hoffman, R. Imetelstat, a telomerase inhibitor, is capable of depleting myelofibrosis stem and progenitor cells. Blood Adv. 2018, 2, 2378–2388. [Google Scholar] [CrossRef] [Green Version]
- Bruedigam, C.; Porter, A.H.; Wackrow, B.; Straube, J.; Cooper, L.T.; Song, A.; Lee, S.C.-W.; Abdel-Wahab, O.; Hill, G.R.; Lane, S.W. Integrated molecular analysis identifies replicative stress as sensitizer to imetelstat therapy in AML. Blood 2017, 130, 798. [Google Scholar]
- Thompson, C.A.H.; Gu, A.; Yang, S.Y.; Mathew, V.; Fleisig, H.B.; Wong, J.M. Transient Telomerase Inhibition with Imetelstat Impacts DNA Damage Signals and Cell-Cycle Kinetics. Mol. Cancer Res. 2018, 16, 1215–1225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, J.; Hannon, G.J. The centrosomal kinase Aurora-A/STK15 interacts with a putative tumor suppressor NM23-H1. Nucleic Acids Res. 2002, 30, 5465–5475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strebhardt, K. Prognostic Value of Pololike Kinase Expression in Melanomas. JAMA 2000, 283, 479–480. [Google Scholar] [CrossRef]
- Wolf, G.; Elez, R.; Doermer, A.; Holtrich, U.; Ackermann, H.; Stutte, H.J.; Altmannsberger, H.-M.; Rübsamen-Waigmann, H.; Strebhardt, K. Prognostic significance of polo-like kinase (PLK) expression in non-small cell lung cancer. Oncogene 1997, 14, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Knecht, R.; Elez, R.; Oechler, M.; Solbach, C.; Von Ilberg, C.; Strebhardt, K. Prognostic significance of polo-like kinase (PLK) expression in squamous cell carcinomas of the head and neck. Cancer Res. 1999, 59, 2794–2797. [Google Scholar] [PubMed]
- Takai, N.; Miyazaki, T.; Fujisawa, K.; Nasu, K.; Hamanaka, R.; Miyakawa, I. Expression of polo-like kinase in ovarian cancer is associated with histological grade and clinical stage. Cancer Lett. 2001, 164, 41–49. [Google Scholar] [CrossRef]
- Takai, N.; Miyazaki, T.; Fujisawa, K.; Nasu, K.; Hamanaka, R.; Miyakawa, I. Polo-like kinase (PLK) expression in endometrial carcinoma. Cancer Lett. 2001, 169, 41–49. [Google Scholar] [CrossRef]
- Zhao, C.; Gong, L.; Li, W.; Chen, L. Overexpression of Plk1 promotes malignant progress in human esophageal squamous cell carcinoma. J. Cancer Res. Clin. Oncol. 2009, 136, 9–16. [Google Scholar] [CrossRef]
- Mok, W.C. Polo-like kinase 1, a new therapeutic target in hepatocellular carcinoma. World J. Gastroenterol. 2012, 18, 3527–3536. [Google Scholar] [CrossRef]
- Sun, W.; Su, Q.; Cao, X.; Shang, B.; Chen, A.; Yin, H.; Liu, B. High Expression of Polo-Like Kinase 1 Is Associated with Early Development of Hepatocellular Carcinoma. Int. J. Genom. 2014, 2014, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamada, S.-I.; Ohira, M.; Horie, H.; Ando, K.; Takayasu, H.; Suzuki, Y.; Sugano, S.; Hirata, T.; Goto, T.; Matsunaga, T.; et al. Expression profiling and differential screening between hepatoblastomas and the corresponding normal livers: Identification of high expression of the PLK1 oncogene as a poor-prognostic indicator of hepatoblastomas. Oncogene 2004, 23, 5901–5911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, T.; Sano, B.; Nagata, T.; Kato, H.; Sugiyama, Y.; Kunieda, K.; Kimura, M.; Okano, Y.; Saji, S. Polo-like kinase 1 (PLK1) is overexpressed in primary colorectal cancers. Cancer Sci. 2003, 94, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.P.; Chen, L.D.; Bin Song, H.; Zhang, C.X.; Yuan, Z.W.; Xiang, Z.X. PLK1 promotes epithelial-mesenchymal transition and metastasis of gastric carcinoma cells. Am. J. Transl. Res. 2016, 8, 4172–4183. [Google Scholar]
- Gray, P.J.; Bearss, D.; Han, H.; Nagle, R.; Tsao, M.-S.; Dean, N.; Von Hoff, D.D. Identification of human polo-like kinase 1 as a potential therapeutic target in pancreatic cancer. Mol. Cancer Ther. 2004, 3, 641–646. [Google Scholar]
- Dietzmann, K.; Kirches, E.; Jachau, K.; Mawrin, C.; Von Bossanyi, P. Increased Human Polo-Like Kinase-1 Expression in Gliomas. J. Neuro Oncol. 2001, 53, 1–11. [Google Scholar] [CrossRef]
- King, S.I.; Purdie, C.A.; Bray, S.E.; Quinlan, P.R.; Jordan, L.B.; Thompson, A.M.; Meek, D.W. Immunohistochemical detection of Polo-like kinase-1 (PLK1) in primary breast cancer is associated with TP53mutation and poor clinical outcome. Breast Cancer Res. 2012, 14, 40. [Google Scholar] [CrossRef] [Green Version]
- Maire, V.; Nemati, F.; Richardson, M.; Vincent-Salomon, A.; Tesson, B.; Rigaill, G.; Gravier, E.; Marty-Prouvost, B.; De Koning, L.; Lang, G.; et al. Polo-like Kinase 1: A Potential Therapeutic Option in Combination with Conventional Chemotherapy for the Management of Patients with Triple-Negative Breast Cancer. Cancer Res. 2012, 73, 813–823. [Google Scholar] [CrossRef] [Green Version]
- Deeraksa, A.; Pan, J.; Sha, Y.; Liu, X.-D.; Eissa, N.T.; Lin, S.-H.; Yu-Lee, L.-Y. Plk1 is upregulated in androgen-insensitive prostate cancer cells and its inhibition leads to necroptosis. Oncogene 2012, 32, 2973–2983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Z.; Chen, L.; Wang, H.; Ahmad, N.; Liu, X.S. Inhibition of Plk1 represses androgen signaling pathway in castration-resistant prostate cancer. Cell Cycle 2015, 14, 2142–2148. [Google Scholar] [CrossRef] [Green Version]
- Hu, K.; Law, J.H.; Fotovati, A.; Dunn, S.E. Small interfering RNA library screen identified polo-like kinase-1 (PLK1) as a potential therapeutic target for breast cancer that uniquely eliminates tumor-initiating cells. Breast Cancer Res. 2012, 14, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lerner, R.G.; Grossauer, S.; Kadkhodaei, B.; Meyers, I.; Sidorov, M.; Koeck, K.; Hashizume, R.; Ozawa, T.; Phillips, J.J.; Berger, M.S.; et al. Targeting a Plk1-Controlled Polarity Checkpoint in Therapy-Resistant Glioblastoma-Propagating Cells. Cancer Res. 2015, 75, 5355–5366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spänkuch-Schmitt, B.; Wolf, G.; Solbach, C.; Loibl, S.; Knecht, R.; Stegmüller, M.; Von Minckwitz, G.; Kaufmann, M.; Strebhardt, K. Downregulation of human polo-like kinase activity by antisense oligonucleotides induces growth inhibition in cancer cells. Oncogene 2002, 21, 3162–3171. [Google Scholar] [CrossRef] [Green Version]
- Gumireddy, K.; Reddy, M.R.; Cosenza, S.C.; Boominathan, R.; Baker, S.J.; Papathi, N.; Jiang, J.; Holland, J.; Reddy, E.P. ON01910, a non-ATP-competitive small molecule inhibitor of Plk1, is a potent anticancer agent. Cancer Cell 2005, 7, 497. [Google Scholar] [CrossRef] [Green Version]
- Gleixner, K.V.; Ferenc, V.; Peter, B.; Gruze, A.; Meyer, R.A.; Hadzijusufovic, E.; Cerny-Reiterer, S.; Mayerhofer, M.; Pickl, W.F.; Sillaber, C.; et al. Polo-like Kinase 1 (Plk1) as a Novel Drug Target in Chronic Myeloid Leukemia: Overriding Imatinib Resistance with the Plk1 Inhibitor BI 2536. Cancer Res. 2010, 70, 1513–1523. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Lei, M.; Erikson, R.L. Normal Cells, but Not Cancer Cells, Survive Severe Plk1 Depletion. Mol. Cell. Biol. 2006, 26, 2093–2108. [Google Scholar] [CrossRef] [Green Version]
- Francescangeli, F.; Patrizii, M.; Signore, M.; Federici, G.; Di Franco, S.; Pagliuca, A.; Baiocchi, M.; Biffoni, M.; Ricci-Vitiani, L.; Todaro, M.; et al. Proliferation State and Polo-Like Kinase1 Dependence of Tumorigenic Colon Cancer Cells. Stem Cells 2012, 30, 1819–1830. [Google Scholar] [CrossRef] [Green Version]
- Grinshtein, N.; Datti, A.; Fujitani, M.; Uehling, D.; Prakesch, M.; Isaac, M.; Irwin, M.S.; Wrana, J.L.; Al-Awar, R.; Kaplan, D.R. Small Molecule Kinase Inhibitor Screen Identifies Polo-Like Kinase 1 as a Target for Neuroblastoma Tumor-Initiating Cells. Cancer Res. 2011, 71, 1385–1395. [Google Scholar] [CrossRef] [Green Version]
- Lund-Andersen, C.; Patzke, S.; Nahse-Kumpf, V.; Syljuåsen, R.G. PLK1-inhibition can cause radiosensitization or radioresistance dependent on the treatment schedule. Radiother. Oncol. 2014, 110, 355–361. [Google Scholar] [CrossRef]
- Gilmartin, A.G.; Bleam, M.R.; Richter, M.C.; Erskine, S.G.; Kruger, R.G.; Madden, L.; Hassler, D.F.; Smith, G.K.; Gontarek, R.R.; Courtney, M.P.; et al. Distinct concentration-dependent effects of the polo-like kinase 1-specific inhibitor GSK461364A, including differential effect on apoptosis. Cancer Res. 2009, 69, 6969–6977. [Google Scholar]
- O’Neil, B.H.; Scott, A.J.; Ma, W.W.; Cohen, S.J.; Leichman, L.; Aisner, D.L.; Menter, A.R.; Tejani, M.A.; Cho, J.K.; Granfortuna, J.; et al. A phase II/III randomized study to compare the efficacy and safety of rigosertib plus gemcitabine versus gemcitabine alone in patients with previously untreated metastatic pancreatic cancer. Ann. Oncol. 2015, 26, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Steegmaier, M.; Hoffmann, M.; Baum, A.; Lénárt, P.; Petronczki, M.; Krššák, M.; Gürtler, U.; Garin-Chesa, P.; Lieb, S.; Quant, J.; et al. BI 2536, a potent and selective inhibitor of polo-like kinase 1, inhibits tumor growth in vivo. Curr. Biol. 2007, 17, 316–322. [Google Scholar] [CrossRef] [Green Version]
- Mross, K.; Dittrich, C.E.; Aulitzky, W.; Strumberg, D.; Schutte, J.; Schmid, R.M.; Hollerbach, S.; Merger, M.; Munzert, G.; Fleischer, F.; et al. A randomised phase II trial of the Polo-like kinase inhibitor BI 2536 in chemo-naïve patients with unresectable exocrine adenocarcinoma of the pancreas—A study within the Central European Society Anticancer Drug Research (CESAR) collaborative network. Br. J. Cancer 2012, 107, 2800–2867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehringer Ingelheim’s Investigational Volasertib Receives FDA Breakthrough Therapy Designation. Available online: https://www.boehringer-ingelheim.us/press-release/boehringer-ingelheims-investigational-volasertib-receives-fda-breakthrough-therapy (accessed on 13 September 2019).
- Stadler, W.M.; Vaughn, D.J.; Sonpavde, G.; Vogelzang, N.J.; Tagawa, S.T.; Petrylak, D.P.; Rosen, P.; Lin, C.-C.; Mahoney, J.; Modi, S.; et al. An open-label, single-arm, phase 2 trial of the Polo-like kinase inhibitor volasertib (BI 6727) in patients with locally advanced or metastatic urothelial cancer. Cancer 2013, 120, 976–982. [Google Scholar] [CrossRef] [Green Version]
- Ellis, P.M.; Leighl, N.B.; Hirsh, V.; Reaume, M.N.; Blais, N.; Wierzbicki, R.; Sadrolhefazi, B.; Gu, Y.; Liu, D.; Pilz, K.; et al. A Randomized, Open-Label Phase II Trial of Volasertib as Monotherapy and in Combination With Standard-Dose Pemetrexed Compared With Pemetrexed Monotherapy in Second-Line Treatment for Non–Small-Cell Lung Cancer. Clin. Lung Cancer 2015, 16, 457–465. [Google Scholar]
- Reindl, W.; Yuan, J.; Krämer, A.; Strebhardt, K.; Berg, T. Inhibition of Polo-like Kinase 1 by Blocking Polo-Box Domain-Dependent Protein-Protein Interactions. Chem. Biol. 2008, 15, 459–466. [Google Scholar] [CrossRef] [Green Version]
- Scharow, A.; Raab, M.; Saxena, K.; Sreeramulu, S.; Kudlinzki, D.; Gande, S.; Dötsch, V.; Kurunci-Csacsko, E.; Klaeger, S.; Kuster, B.; et al. Optimized Plk1 PBD inhibitors based on poloxin induce mitotic arrest and apoptosis in tumor cells. ACS Chem. Biol. 2015, 10, 2570–2579. [Google Scholar] [CrossRef]
- Yuan, J.; Sanhaji, M.; Krämer, A.; Reindl, W.; Hofmann, M.; Kreis, N.-N.; Zimmer, B.; Berg, T.; Strebhardt, K. Polo-box domain inhibitor poloxin activates the spindle assembly checkpoint and inhibits tumor growth in vivo. Am. J. Pathol. 2011, 179, 2091–2099. [Google Scholar] [CrossRef]
- Hikichi, Y.; Honda, K.; Hikami, K.; Miyashita, H.; Kaieda, I.; Murai, S.; Uchiyama, N.; Hasegawa, M.; Kawamoto, T.; Sato, T.; et al. TAK-960, a novel, orally available, selective inhibitor of polo-like kinase 1, shows broad-spectrum preclinical antitumor activity in multiple dosing regimens. Mol. Cancer Ther. 2011, 11, 700–709. [Google Scholar] [CrossRef] [Green Version]
- Klauck, P.J.; Bagby, S.M.; Capasso, A.; Bradshaw-Pierce, E.L.; Selby, H.M.; Spreafico, A.; Tentler, J.J.; Tan, A.C.; Kim, J.; Arcaroli, J.J.; et al. Antitumor activity of the polo-like kinase inhibitor, TAK-960, against preclinical models of colorectal cancer. BMC Cancer 2018, 18, 136. [Google Scholar]
- Beria, I.; Ballinari, D.; Bertrand, J.A.; Borghi, D.; Bossi, R.T.; Brasca, M.G.; Cappella, P.; Caruso, M.; Ceccarelli, W.; Ciavolella, A.; et al. Identification of 4,5-dihydro-1H-pyrazolo[4,3-h]quinazoline derivatives as a new class of orally and selective polo-like kinase 1 inhibitors. J. Med. Chem. 2010, 53, 3532–3551. [Google Scholar] [CrossRef] [PubMed]
- Sero, V.; Tavanti, E.; Vella, S.; Hattinger, C.M.; Fanelli, M.; Michelacci, F.; Versteeg, R.; Valsasina, B.; Gudeman, B.; Picci, P.; et al. Targeting polo-like kinase 1 by NMS-P937 in osteosarcoma cell lines inhibits tumor cell growth and partially overcomes drug resistance. Investig. New Drugs 2014, 32, 1167–1180. [Google Scholar]
- Olmos, D.; Barker, D.; Sharma, R.; Brunetto, A.T.; Yap, T.A.; Taegtmeyer, A.B.; Barriuso, J.; Medani, H.; Degenhardt, Y.Y.; Allred, A.J.; et al. Phase I Study of GSK461364, a Specific and Competitive Polo-like Kinase 1 Inhibitor, in Patients with Advanced Solid Malignancies. Clin. Cancer Res. 2011, 17, 3420–3430. [Google Scholar] [CrossRef] [Green Version]
- Orr, B.; Talje, L.; Liu, Z.; Kwok, B.H.; Compton, D.A. Adaptive Resistance to an Inhibitor of Chromosomal Instability in Human Cancer Cells. Cell Rep. 2016, 17, 1755–1763. [Google Scholar] [CrossRef] [Green Version]
- Ma, S.; Charron, J.; Erikson, R.L. Role of Plk2 (Snk) in mouse development and cell proliferation. Mol. Cell. Biol. 2003, 23, 6936–6943. [Google Scholar] [CrossRef] [Green Version]
- Warnke, S.; Kemmler, S.; Hames, R.; Tsai, H.-L.; Hoffmann-Rohrer, U.; Fry, A.M.; Hoffmann, I. Polo-like kinase-2 is required for centriole duplication in mammalian cells. Curr. Biol. 2004, 14, 1200–1207. [Google Scholar] [CrossRef] [Green Version]
- Matthew, E.M.; Yang, Z.; Peri, S.; Andrake, M.; Dunbrack, R.L.; Ross, E.; El-Deiry, W.S. Plk2 loss commonly occurs in colorectal carcinomas but not adenomas: Relationship to mTOR signaling. Neoplasia 2018, 20, 244–255. [Google Scholar] [CrossRef]
- Syed, N.; Smith, P.; Sullivan, A.; Spender, L.C.; Dyer, M.J.; Karran, L.; O’Nions, J.; Allday, M.; Hoffmann, I.; Crawford, D.; et al. Transcriptional silencing of Polo-like kinase 2(SNK/PLK2)is a frequent event in B-cell malignancies. Blood 2005, 107, 250–256. [Google Scholar]
- Burns, T.F.; Fei, P.; Scata, K.A.; Dicker, D.T.; El-Deiry, W.S. Silencing of the novel p53 target gene Snk/Plk2 leads to mitotic catastrophe in paclitaxel (taxol)-exposed cells. Mol. Cell Biol. 2003, 23, 5556–5571. [Google Scholar] [CrossRef] [Green Version]
- Ang, X.L.; Seeburg, D.P.; Sheng, M.; Harper, J.W. Regulation of postsynaptic RapGAP SPAR by Polo-like kinase 2 and the SCFbeta-TRCP ubiquitin ligase in hippocampal neurons. J. Biol. Chem. 2008, 283, 29424–29432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inglis, K.J.; Chereau, D.; Brigham, E.F.; Chiou, S.-S.; Schöbel, S.; Frigon, N.L.; Yu, M.; Caccavello, R.J.; Nelson, S.; Motter, R.; et al. Polo-like kinase 2 (PLK2) phosphorylates α-synuclein at serine 129 in central nervous system. J. Biol. Chem. 2008, 284, 2598–2602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruan, Q.; Wang, Q.; Xie, S.; Fang, Y.; Darzynkiewicz, Z.; Guan, K.; Jhanwar-Uniyal, M.; Dai, W. Polo-like kinase 3 is Golgi localized and involved in regulating Golgi fragmentation during the cell cycle. Exp. Cell Res. 2004, 294, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Xie, S. Plk3 functionally links DNA damage to cell cycle arrest and apoptosis at least in part via the p53 pathway. J. Biol. Chem. 2001, 276, 43305–43312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dai, W.; Li, Y.; Ouyang, B.; Pan, H.; Reissmann, P.; Li, J.; Wiest, J.; Stambrook, P.; Gluckman, J.L.; Noffsinger, A.; et al. PRK, a cell cycle gene localized to 8p21, is downregulated in head and neck cancer. Genes Chromosom. Cancer 2000, 27, 332–336. [Google Scholar]
- Li, B.; Ouyang, B.; Pan, H.; Reissmann, P.T.; Slamon, D.J.; Arceci, R.; Lu, L.; Dai, W. prk, a Cytokine-inducible Human Protein Serine/Threonine Kinase Whose Expression Appears to be Down-regulated in Lung Carcinomas. J. Biol. Chem. 1996, 271, 19402–19408. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Bai, J.; Shen, R.; Brown, S.A.; Komissarova, E.V.; Huang, Y.; Jiang, N.; Alberts, G.F.; Costa, M.; Lu, L.; et al. Polo-like kinase 3 functions as a tumor suppressor and is a negative regulator of hypoxia-inducible factor-1 alpha under hypoxic conditions. Cancer Res. 2008, 68, 4077–4085. [Google Scholar]
- Liu, X.S. Targeting Polo-Like Kinases: A Promising Therapeutic Approach for Cancer Treatment. Transl. Oncol. 2015, 8, 185–195. [Google Scholar] [CrossRef] [Green Version]
- Silk, A.D.; Zasadil, L.M.; Holland, A.J.; Vitre, B.; Cleveland, D.W.; Weaver, B.A. Chromosome missegregation rate predicts whether aneuploidy will promote or suppress tumors. Proc. Natl. Acad. Sci. USA 2013, 110, E4134–E4141. [Google Scholar] [CrossRef] [Green Version]
- Cunningham, C.E.; Macauley, M.J.; Yadav, G.; Vizeacoumar, F.S.; Freywald, A.; Vizeacoumar, F.J. Targeting the CINful genome: Strategies to overcome tumor heterogeneity. Prog. Biophys. Mol. Biol. 2019, 147, 77–91. [Google Scholar] [CrossRef]
- Zasadil, L.M.; Britigan, E.M.C.; Ryan, S.D.; Kaur, C.; Guckenberger, D.J.; Beebe, D.J.; Moser, A.R.; Weaver, B.A. High rates of chromosome missegregation suppress tumor progression but do not inhibit tumor initiation. Mol. Biol. Cell 2016, 27, 1981–1989. [Google Scholar] [CrossRef]
- Birkbak, N.J.; Eklund, A.C.; Li, Q.; McClelland, S.E.; Endesfelder, D.; Tan, P.; Tan, I.B.; Richardson, A.L.; Szallasi, Z.; Swanton, C. Paradoxical relationship between chromosomal instability and survival outcome in cancer. Cancer Res. 2011, 71, 3447–3452. [Google Scholar] [CrossRef] [Green Version]
- Smith, M.R.; Wilson, M.L.; Hamanaka, R.; Chase, D.; Kung, H.-F.; Longo, D.L.; Ferris, D.K. Malignant transformation of mammalian cells initiated by constitutive expression of the polo-like kinase. Biochem. Biophys. Res. Commun. 1997, 234, 397–405. [Google Scholar]
- Raab, M.; Sanhaji, M.; Matthess, Y.; Hörlin, A.; Lorenz, I.; Dötsch, C.; Habbe, N.; Waidmann, O.; Kurunci-Csacsko, E.; Firestein, R.; et al. PLK1 has tumor-suppressive potential in APC-truncated colon cancer cells. Nat. Commun. 2018, 9, 1106. [Google Scholar] [PubMed] [Green Version]
- Li, Z.; Liu, J.; Li, J.; Kong, Y.; Sandusky, G.; Rao, X.; Liu, Y.; Wan, J.; Liu, X. Polo-like kinase 1 (Plk1) overexpression enhances ionizing radiation-induced cancer formation in mice. J. Biol. Chem. 2017, 292, 17461–17472. [Google Scholar] [CrossRef] [Green Version]
- Boone, C.; Bussey, H.; Andrews, B.J. Exploring genetic interactions and networks with yeast. Nat. Rev. Genet. 2007, 8, 437–449. [Google Scholar] [CrossRef]
- Davierwala, A.P.; Haynes, J.; Li, Z.; Brost, R.L.; Robinson, M.D.; Yu, L.; Mnaimneh, S.; Ding, H.; Zhu, H.; Chen, Y.; et al. The synthetic genetic interaction spectrum of essential genes. Nat. Genet. 2005, 37, 1147–1152. [Google Scholar] [CrossRef]
- Mani, R.; St. Onge, R.P.; Hartman, J.L.; Giaever, G.; Roth, F.P. Defining genetic interaction. Proc. Natl. Acad. Sci. USA 2008, 105, 3461–3466. [Google Scholar] [CrossRef] [Green Version]
- Eboucher, B.; Ejenna, S. Genetic interaction networks: Better understand to better predict. Front Genet. 2013, 4, 290. [Google Scholar]
- Nair, S.P.; Kundapur, D.; Vizeacoumar, F.S.; Freywald, A.; Uppalapati, M.; Vizeacoumar, F.J. A road map to personalizing targeted cancer therapies using synthetic lethality. Trends Cancer 2019, 5, 11–29. [Google Scholar]
- Paul, J.M.; Templeton, S.D.; Baharani, A.; Freywald, A.; Vizeacoumar, F.J. Building high-resolution synthetic lethal networks: A ‘Google map’ of the cancer cell. Trends Mol. Med. 2014, 20, 704–715. [Google Scholar] [CrossRef]
- Vizeacoumar, F.J.; Arnold, R.; Vizeacoumar, F.S.; Chandrashekhar, M.; Buzina, A.; Young, J.T.F.; Kwan, J.H.M.; Sayad, A.; Mero, P.; Lawo, S.; et al. A negative genetic interaction map in isogenic cancer cell lines reveals cancer cell vulnerabilities. Mol. Syst. Biol. 2013, 9, 696. [Google Scholar]
- Bryant, H.E.; Schultz, N.; Thomas, H.D.; Parker, K.M.; Flower, D.; Lopez, E.; Kyle, S.; Meuth, M.; Curtin, N.J.; Helelday, T. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 2005, 434, 913–917. [Google Scholar] [CrossRef]
- Farmer, H.; McCabe, N.; Lord, C.J.; Tutt, A.N.J.; Johnson, D.A.; Richardson, T.B.; Santarosa, M.; Dillon, K.J.; Hickson, I.; Knights, C.; et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nat. Cell Biol. 2005, 434, 917–921. [Google Scholar] [CrossRef]
- Koppensteiner, R.; Samartzis, E.P.; Noske, A.; Von Teichman, A.; Dedes, I.; Gwerder, M.; Imesch, P.; Ikenberg, K.; Moch, H.; Fink, D.; et al. Effect of MRE11 loss on PARP-inhibitor sensitivity in endometrial cancer in vitro. PLoS ONE 2014, 9, e100041. [Google Scholar]
- Mohni, K.N.; Thompson, P.S.; Luzwick, J.W.; Glick, G.G.; Pendleton, C.S.; Lehmann, B.D.; Pietenpol, J.A.; Cortez, D. A Synthetic lethal screen identifies DNA Repair pathways that sensitize cancer cells to combined ATR inhibition and cisplatin treatments. PLoS ONE 2015, 10, e0125482. [Google Scholar] [CrossRef] [Green Version]
- Subhash, V.V.; Tan, S.H.; Yeo, M.S.; Yan, F.L.; Peethala, P.C.; Liem, N.; Krishnan, V.; Yong, W.P. ATM Expression predicts veliparib and irinotecan sensitivity in gastric cancer by mediating P53-independent regulation of cell cycle and apoptosis. Mol. Cancer Ther. 2016, 15, 3087–3096. [Google Scholar] [CrossRef] [Green Version]
- McAndrew, E.N.; Lepage, C.C.; McManus, K.J. The synthetic lethal killing of RAD54B-deficient colorectal cancer cells by PARP1 inhibition is enhanced with SOD1 inhibition. Oncotarget 2016, 7, 87417–87430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunningham, C.E.; MacAuley, M.J.; Vizeacoumar, F.S.; Abuhussein, O.; Freywald, A.; Vizeacoumar, F.J. The CINs of Polo-Like Kinase 1 in Cancer. Cancers 2020, 12, 2953. https://doi.org/10.3390/cancers12102953
Cunningham CE, MacAuley MJ, Vizeacoumar FS, Abuhussein O, Freywald A, Vizeacoumar FJ. The CINs of Polo-Like Kinase 1 in Cancer. Cancers. 2020; 12(10):2953. https://doi.org/10.3390/cancers12102953
Chicago/Turabian StyleCunningham, Chelsea E., Mackenzie J. MacAuley, Frederick S. Vizeacoumar, Omar Abuhussein, Andrew Freywald, and Franco J. Vizeacoumar. 2020. "The CINs of Polo-Like Kinase 1 in Cancer" Cancers 12, no. 10: 2953. https://doi.org/10.3390/cancers12102953





