Prognostic Implications of CD10 and CD15 Expression in Papillary Thyroid Carcinoma
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics
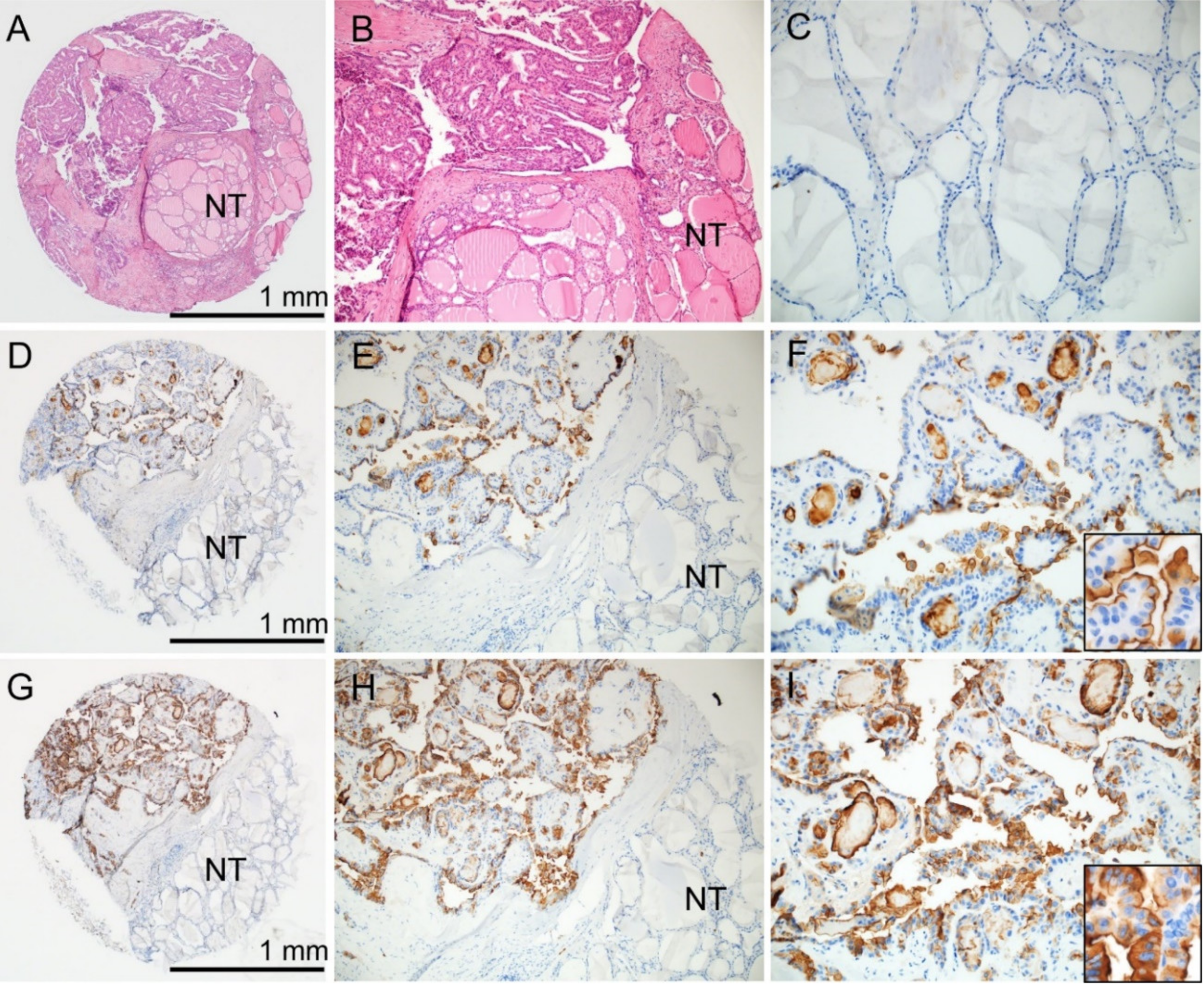
2.2. Clinicopathologic Significance of CD10 and CD15 Protein Expression
2.3. Analysis of Recurrence-Free Survival
2.4. Therapeutic Response to RAI
2.5. Clinicopathologic Significance of MME and FUT4 mRNA Expression in TCGA Dataset
2.6. Relationship between FUT4 (CD15) mRNA Expression and the Tumor Microenvironment
2.7. Relationship between FUT4 (CD15) and SLC5A5 (NIS) mRNA Expression
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Tissue Microarray
4.3. Immunohistochemistry
4.4. Evaluation of Immunostaining
4.5. BRAF Mutational Analysis
4.6. TCGA Data Analysis
4.7. Immunoprofiling of PTC in the TCGA Database
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lloyd, R.V.; Osamura, R.Y.; Klöppel, G.; Rosai, J. WHO Classification of Tumors of Endocrine Organs, 4th ed.; International Agency for Research on Cancer (IARC): Lyon, France, 2017; Volume 10, pp. 65–91. [Google Scholar]
- Bychkov, A.; Jung, C.K.; Liu, Z.; Kakudo, K. Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features in Asian Practice: Perspectives for Surgical Pathology and Cytopathology. Endocr. Pathol. 2018, 29, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Kakudo, K.; Bychkov, A.; Bai, Y.; Li, Y.; Liu, Z.; Jung, C.K. The new 4th edition World Health Organization classification for thyroid tumors, Asian perspectives. Pathol. Int. 2018, 68, 641–664. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Won, Y.J.; Kong, H.J.; Lee, E.S. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2016. Cancer Res. Treat. 2019, 51, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Schlumberger, M.J. Papillary and follicular thyroid carcinoma. N. Engl. J. Med. 1998, 338, 297–306. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Engel, P.; Boumsell, L.; Balderas, R.; Bensussan, A.; Gattei, V.; Horejsi, V.; Jin, B.Q.; Malavasi, F.; Mortari, F.; Schwartz-Albiez, R.; et al. CD Nomenclature 2015: Human Leukocyte Differentiation Antigen Workshops as a Driving Force in Immunology. J. Immunol. 2015, 195, 4555–4563. [Google Scholar] [CrossRef]
- Bychkov, A.; Jung, C.K. Aberrant expression of CD20 in thyroid cancer and its clinicopathologic significance. Hum. Pathol. 2018, 71, 74–83. [Google Scholar] [CrossRef]
- Mishra, D.; Singh, S.; Narayan, G. Role of B Cell Development Marker CD10 in Cancer Progression and Prognosis. Mol. Biol. Int. 2016, 2016, 4328697. [Google Scholar] [CrossRef]
- Maguer-Satta, V.; Besancon, R.; Bachelard-Cascales, E. Concise review: Neutral endopeptidase (CD10): A multifaceted environment actor in stem cells, physiological mechanisms, and cancer. Stem Cells 2011, 29, 389–396. [Google Scholar] [CrossRef]
- Tomoda, C.; Kushima, R.; Takeuti, E.; Mukaisho, K.; Hattori, T.; Kitano, H. CD10 expression is useful in the diagnosis of follicular carcinoma and follicular variant of papillary thyroid carcinoma. Thyroid 2003, 13, 291–295. [Google Scholar] [CrossRef]
- Mokhtari, M.; Ameri, F. Diagnostic value of CD-10 marker in differentiating of papillary thyroid carcinoma from benign thyroid lesions. Adv. Biomed. Res. 2014, 3, 206. [Google Scholar] [CrossRef]
- Gabal, S.M.; Salem, M.M.; Mostafa, R.R.; Abdelsalam, S.M. Role of CD10 Marker in Differentiating Malignant Thyroid Neoplasms from Benign Thyroid Lesions (Immunohistochemical & Histopathological Study). Open Access Maced. J. Med. Sci. 2018, 6, 2295–2300. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, T.; Kondo, T.; Vuong, H.G.; Odate, T.; Kawai, M.; Tahara, I.; Kasai, K.; Inoue, T.; Oishi, N.; Mochizuki, K.; et al. High expression of CD10 in anaplastic thyroid carcinomas. Histopathology 2018, 73, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Gadhoum, S.Z.; Sackstein, R. CD15 expression in human myeloid cell differentiation is regulated by sialidase activity. Nat. Chem. Biol. 2008, 4, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Kansal, R.; Singleton, T.P.; Ross, C.W.; Finn, W.G.; Padmore, R.F.; Schnitzer, B. Follicular hodgkin lymphoma: A histopathologic study. Am. J. Clin. Pathol. 2002, 117, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, Z.; Wang, S.; Fan, Y.; Zhang, S.; Yang, X.; Hou, K.; Tong, J.; Hu, X.; Shi, X.; et al. FUT4 is involved in PD-1-related immunosuppression and leads to worse survival in patients with operable lung adenocarcinoma. J. Cancer Res. Clin. Oncol. 2019, 145, 65–76. [Google Scholar] [CrossRef]
- Feng, X.; Zhao, L.; Gao, S.; Song, X.; Dong, W.; Zhao, Y.; Zhou, H.; Cheng, L.; Miao, X.; Jia, L. Increased fucosylation has a pivotal role in multidrug resistance of breast cancer cells through miR-224-3p targeting FUT4. Gene 2016, 578, 232–241. [Google Scholar] [CrossRef]
- Giordano, G.; Febbraro, A.; Tomaselli, E.; Sarnicola, M.L.; Parcesepe, P.; Parente, D.; Forte, N.; Fabozzi, A.; Remo, A.; Bonetti, A.; et al. Cancer-related CD15/FUT4 overexpression decreases benefit to agents targeting EGFR or VEGF acting as a novel RAF-MEK-ERK kinase downstream regulator in metastatic colorectal cancer. J. Exp. Clin. Cancer Res. 2015, 34, 108. [Google Scholar] [CrossRef]
- Jang, T.J.; Park, J.B.; Lee, J.I. The Expression of CD10 and CD15 Is Progressively Increased during Colorectal Cancer Development. Korean. J. Pathol. 2013, 47, 340–347. [Google Scholar] [CrossRef]
- Escrevente, C.; Machado, E.; Brito, C.; Reis, C.A.; Stoeck, A.; Runz, S.; Marme, A.; Altevogt, P.; Costa, J. Different expression levels of alpha3/4 fucosyltransferases and Lewis determinants in ovarian carcinoma tissues and cell lines. Int. J. Oncol. 2006, 29, 557–566. [Google Scholar]
- Tozawa, K.; Okamoto, T.; Kawai, N.; Hashimoto, Y.; Hayashi, Y.; Kohri, K. Positive correlation between sialyl Lewis X expression and pathologic findings in renal cell carcinoma. Kidney Int. 2005, 67, 1391–1396. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, C.Y.; Huo, J.P.; Zhang, X.K.; Zhang, Y.J.; Hu, W.M.; Yang, P.; Lu, J.B.; Zhang, Z.L.; Cao, Y. Loss of CD15 expression in clear cell renal cell carcinoma is correlated with worse prognosis in Chinese patients. Jpn. J. Clin. Oncol. 2017, 47, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Hardin, H.; Zhang, R.; Sundling, K.; Buehler, D.; Lloyd, R.V. Stage-Specific Embryonic Antigen-1 (SSEA-1) Expression in Thyroid Tissues. Endocr. Pathol. 2016, 27, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.M.; Koo, J.S. Immunohistochemical Analysis of Cancer Stem Cell Marker Expression in Papillary Thyroid Cancer. Front. Endocrinol. 2019, 10, 523. [Google Scholar] [CrossRef]
- Shimamura, M.; Nagayama, Y.; Matsuse, M.; Yamashita, S.; Mitsutake, N. Analysis of multiple markers for cancer stem-like cells in human thyroid carcinoma cell lines. Endocr. J. 2014, 61, 481–490. [Google Scholar] [CrossRef]
- Calon, A.; Lonardo, E.; Berenguer-Llergo, A.; Espinet, E.; Hernando-Momblona, X.; Iglesias, M.; Sevillano, M.; Palomo-Ponce, S.; Tauriello, D.V.; Byrom, D.; et al. Stromal gene expression defines poor-prognosis subtypes in colorectal cancer. Nat. Genet. 2015, 47, 320–329. [Google Scholar] [CrossRef]
- De Biase, D.; Cesari, V.; Visani, M.; Casadei, G.P.; Cremonini, N.; Gandolfi, G.; Sancisi, V.; Ragazzi, M.; Pession, A.; Ciarrocchi, A.; et al. High-sensitivity BRAF mutation analysis: BRAF V600E is acquired early during tumor development but is heterogeneously distributed in a subset of papillary thyroid carcinomas. J. Clin. Endocrinol. Metab. 2014, 99, E1530–E1538. [Google Scholar] [CrossRef]
- Yoshihara, K.; Shahmoradgoli, M.; Martinez, E.; Vegesna, R.; Kim, H.; Torres-Garcia, W.; Trevino, V.; Shen, H.; Laird, P.W.; Levine, D.A.; et al. Inferring tumour purity and stromal and immune cell admixture from expression data. Nat. Commun. 2013, 4, 2612. [Google Scholar] [CrossRef]
- Newman, A.M.; Liu, C.L.; Green, M.R.; Gentles, A.J.; Feng, W.; Xu, Y.; Hoang, C.D.; Diehn, M.; Alizadeh, A.A. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods. 2015, 12, 453–457. [Google Scholar] [CrossRef]
- Tavares, C.; Coelho, M.J.; Eloy, C.; Melo, M.; da Rocha, A.G.; Pestana, A.; Batista, R.; Ferreira, L.B.; Rios, E.; Selmi-Ruby, S.; et al. NIS expression in thyroid tumors, relation with prognosis clinicopathological and molecular features. Endocr. Connect. 2018, 7, 78–90. [Google Scholar] [CrossRef]
- Keeley, T.S.; Yang, S.; Lau, E. The Diverse Contributions of Fucose Linkages in Cancer. Cancers 2019, 11, 1241. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-C.; Yen, H.-Y.; Chen, C.-Y.; Chen, C.-H.; Cheng, P.-F.; Juan, Y.-H.; Chen, C.-H.; Khoo, K.-H.; Yu, C.-J.; Yang, P.-C.; et al. Sialylation and fucosylation of epidermal growth factor receptor suppress its dimerization and activation in lung cancer cells. Proc. Natl. Acad. Sci. USA 2011, 108, 11332–11337. [Google Scholar] [CrossRef] [PubMed]
- Isella, C.; Terrasi, A.; Bellomo, S.E.; Petti, C.; Galatola, G.; Muratore, A.; Mellano, A.; Senetta, R.; Cassenti, A.; Sonetto, C.; et al. Stromal contribution to the colorectal cancer transcriptome. Nat. Genet. 2015, 47, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Flavell, R.A.; Sanjabi, S.; Wrzesinski, S.H.; Licona-Limon, P. The polarization of immune cells in the tumour environment by TGFbeta. Nat. Rev. Immunol. 2010, 10, 554–567. [Google Scholar] [CrossRef]
- Rooney, M.S.; Shukla, S.A.; Wu, C.J.; Getz, G.; Hacohen, N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 2015, 160, 48–61. [Google Scholar] [CrossRef]
- Brunner-Weinzierl, M.C.; Rudd, C.E. CTLA-4 and PD-1 Control of T-Cell Motility and Migration: Implications for Tumor Immunotherapy. Front. Immunol. 2018, 9, 2737. [Google Scholar] [CrossRef]
- Amin, M.B.; Edge, S.; Greene, F.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. AJCC Cancer Staging Manual, 8th ed.; Springer: New York, NY, USA, 2017; pp. 873–890. [Google Scholar]
- Landa, I.; Ibrahimpasic, T.; Boucai, L.; Sinha, R.; Knauf, J.A.; Shah, R.H.; Dogan, S.; Ricarte-Filho, J.C.; Krishnamoorthy, G.P.; Xu, B.; et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Invest. 2016, 126, 1052–1066. [Google Scholar] [CrossRef]
- Bonhomme, B.; Godbert, Y.; Perot, G.; Al Ghuzlan, A.; Bardet, S.; Belleannee, G.; Criniere, L.; Do Cao, C.; Fouilloux, G.; Guyetant, S.; et al. Molecular Pathology of Anaplastic Thyroid Carcinomas: A Retrospective Study of 144 Cases. Thyroid 2017, 27, 682–692. [Google Scholar] [CrossRef]
- Jung, C.K.; Im, S.Y.; Kang, Y.J.; Lee, H.; Jung, E.S.; Kang, C.S.; Bae, J.S.; Choi, Y.J. Mutational patterns and novel mutations of the BRAF gene in a large cohort of Korean patients with papillary thyroid carcinoma. Thyroid 2012, 22, 791–797. [Google Scholar] [CrossRef]
- Xing, M. BRAF mutation in papillary thyroid cancer: Pathogenic role, molecular bases, and clinical implications. Endocr. Rev. 2007, 28, 742–762. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, M.H.; Jeon, S.; Kim, J.; Kim, C.; Bae, J.S.; Jung, C.K. Prognostic implication of histological features associated with EHD2 expression in papillary thyroid carcinoma. PLoS ONE 2017, 12, e0174737. [Google Scholar] [CrossRef] [PubMed]
- Choden, S.; Keelawat, S.; Jung, C.K.; Bychkov, A. VE1 Immunohistochemistry Improves the Limit of Genotyping for Detecting BRAF(V600E) Mutation in Papillary Thyroid Cancer. Cancers 2020, 12, 596. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Liu, R.; Basolo, F.; Giannini, R.; Shen, X.; Teng, D.; Guan, H.; Shan, Z.; Teng, W.; Musholt, T.J.; et al. Differential Clinicopathological Risk and Prognosis of Major Papillary Thyroid Cancer Variants. J. Clin. Endocrinol. Metab. 2016, 101, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 2014, 159, 676–690. [Google Scholar] [CrossRef]
- Edge, S.B.; Byrd, D.R.; Compton, C.C.; Fritz, A.G.; Greene, F.L.; Trotti, A. AJCC Cancer Staging Manual, 7th ed.; Springer: New York, NY, USA, 2010; pp. 87–96. [Google Scholar]
- Kim, K.; Jeon, S.; Kim, T.M.; Jung, C.K. Immune Gene Signature Delineates a Subclass of Papillary Thyroid Cancer with Unfavorable Clinical Outcomes. Cancers 2018, 10, 494. [Google Scholar] [CrossRef]




| n | CD10 Expression | CD15 Expression | |||||
|---|---|---|---|---|---|---|---|
| Positive | Negative | p Value | Positive | Negative | p Value | ||
| Age (years) | 0.772 | 0.233 | |||||
| <55 | 365 | 141 (38.6%) | 224 (61.4%) | 203 (55.6%) | 162 (44.4%) | ||
| ≥55 | 150 | 60 (40.0%) | 90 (60.0%) | 92 (61.3%) | 58 (38.7%) | ||
| Sex | 0.049 | 0.009 | |||||
| Female | 405 | 167 (41.2%) | 238 (58.8%) | 244 (60.2%) | 161 (39.8%) | ||
| Male | 110 | 34 (30.9%) | 76 (69.1%) | 51 (46.4%) | 59 (53.6%) | ||
| Histologic type | 0.009 | 0.002 | |||||
| Classic | 453 | 174 (38.4%) | 279 (61.6%) | 260 (57.4%) | 193 (42.6%) | ||
| Follicular variant | 17 | 2 (11.8%) | 15 (88.2%) | 3 (17.6%) | 14 (82.4%) | ||
| Tall cell variant | 21 | 10 (47.6%) | 11 (52.4%) | 15 (71.4%) | 6 (28.6%) | ||
| Other | 24 | 15 (62.5%) | 9 (37.5%) | 17 (70.8%) | 7 (29.2%) | ||
| Extrathyroidal extension | |||||||
| Absent | 137 | 38 (27.7%) | 99 (72.3%) | 64 (46.7%) | 73 (53.3%) | ||
| Minimal * | 279 | 120 (43.0%) | 159 (57.0%) | 0.003 | 166 (59.5%) | 113 (40.5%) | 0.014 |
| Gross | 99 | 43 (43.4%) | 56 (56.6%) | 0.317 | 65 (65.7%) | 34 (34.3%) | 0.061 |
| Pathological (p) T stage | 0.164 | 0.181 | |||||
| pT1 | 357 | 129 (36.1%) | 228 (63.9%) | 197 (55.2%) | 160 (44.8%) | ||
| pT2 | 56 | 27 (48.2%) | 29 (51.8%) | 30 (53.6%) | 26 (46.4%) | ||
| pT3 | 81 | 34 (42.0%) | 47 (58.0%) | 55 (67.9%) | 26 (32.1%) | ||
| pT4 | 20 | 10 (50.0%) | 10 (50.0%) | 12 (60.0%) | 8 (40.0%) | ||
| Lymph node metastasis | 0.143 | 0.735 | |||||
| Absent | 197 | 69 (35.0%) | 128 (65.0%) | 111 (56.3%) | 86 (43.7%) | ||
| Present | 318 | 132 (41.5%) | 186 (58.5%) | 184 (57.9%) | 134 (42.1%) | ||
| Distant metastasis | 0.286 | 0.062 | |||||
| Absent | 504 | 195 (38.7%) | 309 (61.3%) | 292 (57.9%) | 212 (42.1%) | ||
| Present | 11 | 6 (54.5%) | 5 (45.5%) | 3 (27.3%) | 8 (72.7%) | ||
| AJCC stage 8th | 0.229 | 0.646 | |||||
| Stage I | 421 | 160 (38.0%) | 261 (62.0%) | 240 (57.0%) | 181 (43.0%) | ||
| Stage II | 81 | 34 (42.0%) | 47 (58.0%) | 49 (60.5%) | 32 (39.5%) | ||
| Stage III | 9 | 5 (55.6%) | 4 (44.4%) | 6 (66.7%) | 3 (33.3%) | ||
| Stage IV | 4 | 2 (50.0%) | 2 (50.0%) | 0 | 4 (100.0%) | ||
| Recurrence | 0.656 | 0.034 | |||||
| Absent | 461 | 179 (38.8%) | 282 (61.2%) | 270 (58.6%) | 191 (41.4%) | ||
| Present | 45 | 19 (42.2%) | 26 (57.8%) | 19 (42.2%) | 26 (57.8%) | ||
| BRAFV600E | 0.011 | <0.001 | |||||
| Absent | 83 | 22 (26.5%) | 61 (73.5%) | 13 (15.7%) | 70 (84.3%) | ||
| Present | 432 | 179 (41.4%) | 253 (58.6%) | 282 (65.3%) | 150 (34.7%) | ||
| Variable | Adjusted Hazard Ratio | 95% CI | p Value |
|---|---|---|---|
| Age (years), ≥55 vs. <55 | 0.900 | 0.443–1.830 | 0.900 |
| Sex, male vs. female | 0.936 | 0.475–1.844 | 0.848 |
| Histologic subtype, aggressive vs. non-aggressive | 1.395 | 0.424–4.594 | 0.584 |
| Pathological T stage, pT3-4 vs. pT1-2 | 1.825 | 0.972–3.426 | 0.061 |
| Lymph node metastasis, present vs. absent | 7.026 | 2.167–22.786 | 0.001 |
| CD15 expression, present vs. absent | 0.500 | 0.274–0.911 | 0.024 |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Age (years), ≥55 vs. <55 | 0.991 (0.427–2.297) | 0.982 | 0.985 (0.415–2.339) | 0.973 |
| Sex, male vs. female | 0.708 (0.304–1.649) | 0.423 | 0.822 (0.345–1.957) | 0.657 |
| Histologic subtype, aggressive vs. non-aggressive | 0.478 (0.128–2.624) | 0.478 | 0.683(0.139–3.350) | 0.638 |
| Pathologic T stage, pT3-4 vs. pT1-2 | 0.336 (0.155–0.731) | 0.006 | 0.298 (0.135–0.658) | 0.003 |
| CD15 expression, present vs. absent | 2.368 (1.092–5.134) | 0.029 | 2.678 (1.215–5.902) | 0.015 |
| Variable | n | MME (CD10) mRNA | FUT4 (CD15) mRNA | ||||
|---|---|---|---|---|---|---|---|
| High | Low | p Value | High | Low | p Value | ||
| Age (years) | 454 | 0.657 | 0.001 | ||||
| <45 | 211 | 106 (50.2%) | 105 (49.8%) | 120 (56.9%) | 91 (43.1%) | ||
| ≥45 | 243 | 117 (48.1%) | 126 (51.9%) | 101 (41.6%) | 142 (58.4%) | ||
| Sex | 454 | 0.765 | 0.279 | ||||
| Female | 123 | 59 (48.0%) | 64 (52.0%) | 65 (52.8%) | 58 (47.2%) | ||
| Male | 331 | 164 (49.5%) | 167 (50.5%) | 156 (47.1%) | 175 (52.9%) | ||
| Histologic type | 454 | 0.410 | 0.031 | ||||
| Classic | 312 | 172 (55.1%) | 140 (44.9%) | 165 (52.9%) | 147 (47.1%) | ||
| Follicular | 99 | 17 (17.2%) | 82 (82.8%) | 36 (36.4%) | 63 (63.6%) | ||
| Tall cell | 34 | 30 (88.2%) | 4 (11.8%) | 18 (52.9%) | 16 (47.1%) | ||
| Other | 9 | 4 (44.4%) | 5 (55.6%) | 2 (22.2%) | 7 (77.8%) | ||
| Extrathyroidal extension | 441 | ||||||
| Absent | 309 | 130 (42.1%) | 179 (57.9%) | 146 (47.2%) | 163 (52.8%) | ||
| Minimal (T3) * | 117 | 77 (65.8%) | 40 (34.2%) | <0.001 | 63 (53.8%) | 54 (46.2%) | 0.224 |
| Advanced (T4) | 15 | 11 (73.3%) | 4 (26.7%) | 0.060 | 5 (33.3%) | 10 (66.7%) | 0.231 |
| Pathologic (p) T stage | 452 | 0.001 | 0.356 | ||||
| pT1-T2 | 283 | 122 (43.1%) | 161 (56.9%) | 133 (47.0%) | 150 (53.0%) | ||
| pT3-T4 | 169 | 100 (59.2%) | 69 (40.8%) | 87 (51.5%) | 82 (48.5%) | ||
| pN stage | 409 | <0.001 | 0.154 | ||||
| pN0 | 208 | 82 (39.4%) | 126 (60.6%) | 94 (45.2%) | 114 (54.8%) | ||
| pN1 | 201 | 124 (61.7%) | 77 (38.3%) | 105 (52.5%) | 96 (47.8%) | ||
| M stage | 250 | 1.000 | 0.148 | ||||
| M0 | 242 | 128 (52.9%) | 114 (47.1%) | 133 (55.0%) | 109 (45.0%) | ||
| M1 | 8 | 4 (50.0%) | 4 (50.0%) | 2 (25.0%) | 6 (75.0%) | ||
| AJCC stage 7th | 452 | 0.007 | 0.428 | ||||
| Stage I–II | 309 | 139 (45.0%) | 170 (55.0%) | 155 (50.2%) | 154 (49.8%) | ||
| Stage III–IV | 143 | 84 (58.7%) | 59 (41.3%) | 66 (46.2%) | 77 (53.8%) | ||
| Recurrence risk group | 442 | <0.001 | 0.023 | ||||
| Low | 166 | 56 (33.7%) | 110 (66.3%) | 78 (47.0%) | 88 (53.0%) | ||
| Intermediate | 252 | 148 (58.7%) | 104 (41.3%) | 134 (53.2%) | 118 (46.8%) | ||
| High | 24 | 14 (58.3%) | 10 (41.7%) | 6 (25.0%) | 18 (75.0%) | ||
| BRAF-RAS signature | 391 | <0.001 | 0.002 | ||||
| BRAF-like | 272 | 177 (65.1%) | 95 (34.9%) | 151 (55.5%) | 121 (44.5%) | ||
| RAS-like | 119 | 16 (13.4%) | 103 (86.6%) | 46 (38.7%) | 73 (61.3%) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, E.J.; Bychkov, A.; Cho, H.; Kim, T.-M.; Bae, J.S.; Lim, D.-J.; Jung, C.K. Prognostic Implications of CD10 and CD15 Expression in Papillary Thyroid Carcinoma. Cancers 2020, 12, 1413. https://doi.org/10.3390/cancers12061413
Oh EJ, Bychkov A, Cho H, Kim T-M, Bae JS, Lim D-J, Jung CK. Prognostic Implications of CD10 and CD15 Expression in Papillary Thyroid Carcinoma. Cancers. 2020; 12(6):1413. https://doi.org/10.3390/cancers12061413
Chicago/Turabian StyleOh, Eun Ji, Andrey Bychkov, Haejin Cho, Tae-Min Kim, Ja Seong Bae, Dong-Jun Lim, and Chan Kwon Jung. 2020. "Prognostic Implications of CD10 and CD15 Expression in Papillary Thyroid Carcinoma" Cancers 12, no. 6: 1413. https://doi.org/10.3390/cancers12061413
APA StyleOh, E. J., Bychkov, A., Cho, H., Kim, T.-M., Bae, J. S., Lim, D.-J., & Jung, C. K. (2020). Prognostic Implications of CD10 and CD15 Expression in Papillary Thyroid Carcinoma. Cancers, 12(6), 1413. https://doi.org/10.3390/cancers12061413







