Basics and Frontiers on Pancreatic Cancer for Radiation Oncology: Target Delineation, SBRT, SIB Technique, MRgRT, Particle Therapy, Immunotherapy and Clinical Guidelines
Abstract
:1. Introduction
1.1. Clinical Presentation
1.2. Neoadjuvant Therapy
1.3. Definitive Therapy
1.4. Adjuvant Therapy
1.5. Clinical Presentation: Closing Remarks
2. Overview of Guidelines and Literature Highlights
2.1. Methodology for the Review of the Guidelines
2.2. Resectable Pancreatic Cancer
2.3. Locally Advanced Pancreatic Cancer (LAPC)
2.4. Borderline Resectable Pancreatic Cancer (BRPC)
2.5. Closing Remarks
3. RT Schedules
4. Target Volume Delineation
4.1. Conventional Radiotherapy
4.2. Stereotactic Body Radiation Therapy (SBRT)
5. Future Directions
5.1. Particle Therapy
5.2. MR-guided-RT (MRgRT)
5.3. Stereotactic Ablative Radiation Therapy (SBRT)
5.3.1. Resectable Pancreatic Cancer
5.3.2. Borderline Resectable Pancreatic Cancer (BRPC)
5.3.3. Locally Advanced Pancreatic Cancer (LAPC)
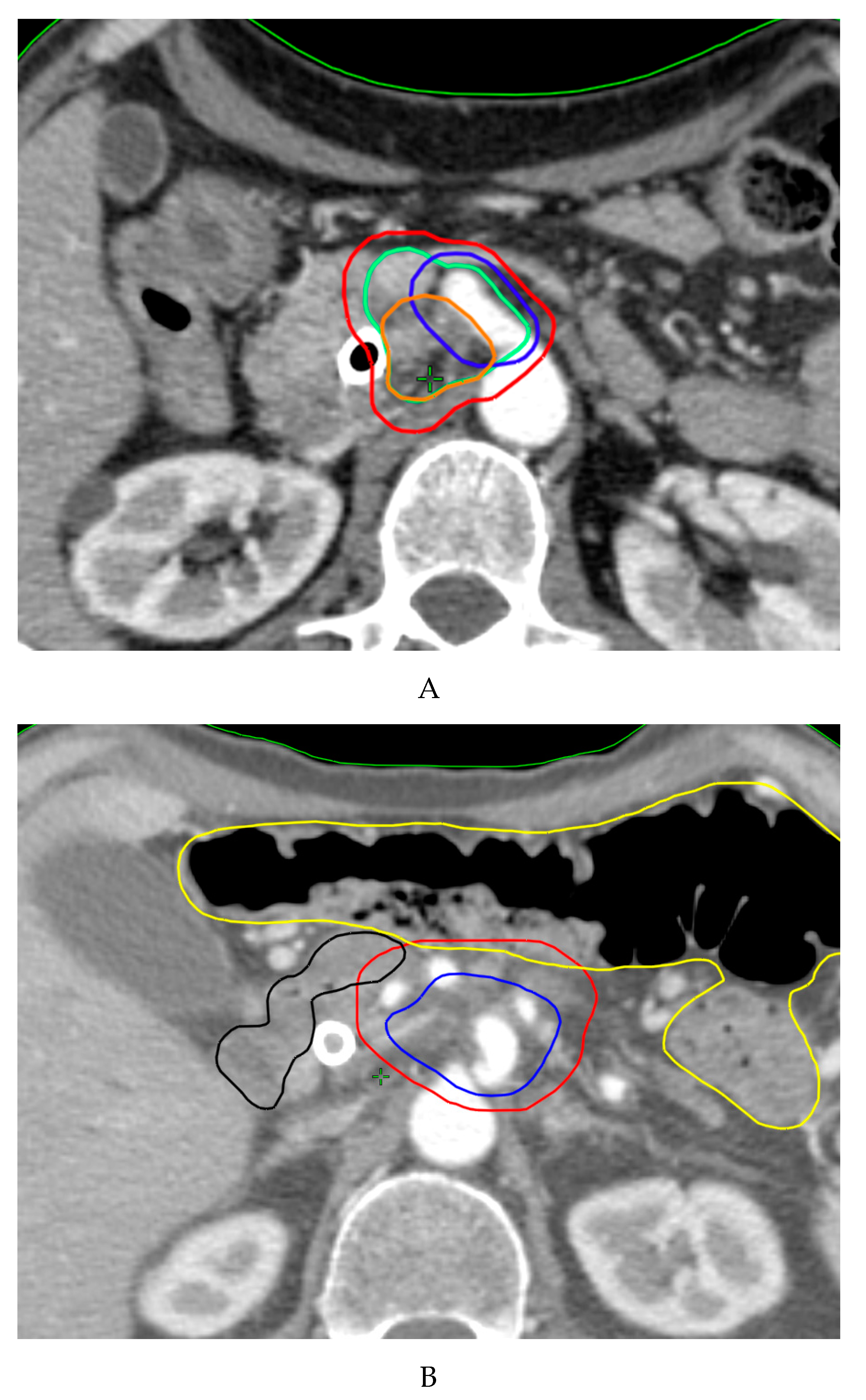
5.4. Simultaneous Integrated Boost (SIB)
5.5. Radiotherapy Combined with Immunotherapy
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [Green Version]
- NCCN. NCCN Clinical Practice Guidelines in Oncology: Pancreatic Adenocarcinoma. Version 1.2020. Available online: https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf (accessed on 26 April 2020).
- Oettle, H.; Post, S.; Neuhaus, P.; Gellert, K.; Langrehr, J.; Ridwelski, K.; Schramm, H.; Fahlke, J.; Zuelke, C.; Burkart, C.; et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: A randomized controlled trial. JAMA 2007, 297, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Regine, W.F.; Winter, K.A.; Abrams, R.A.; Safran, H.; Hoffman, J.P.; Konski, A.; Benson, A.B.; Macdonald, J.S.; Kudrimoti, M.R.; Fromm, M.L.; et al. Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: A randomized controlled trial. JAMA 2008, 299, 1019–1026. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Palmer, D.H.; Ghaneh, P.; Psarelli, E.E.; Valle, J.W.; Halloran, C.M.; Faluyi, O.; O’Reilly, D.A.; Cunningham, D.; Wadsley, J.; et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet 2017, 389, 1011–1024. [Google Scholar] [CrossRef]
- Kamisawa, T.; Wood, L.D.; Itoi, T.; Takaori, K. Pancreatic cancer. Lancet 2016, 388, 73–85. [Google Scholar] [CrossRef]
- Hishinuma, S.; Ogata, Y.; Tomikawa, M.; Ozawa, I.; Hirabayashi, K.; Igarashi, S. Patterns of recurrence after curative resection of pancreatic cancer, based on autopsy findings. J. Gastrointest. Surg. 2006, 10, 511–518. [Google Scholar] [CrossRef]
- Silvestris, N.; Longo, V.; Cellini, F.; Reni, M.; Bittoni, A.; Cataldo, I.; Partelli, S.; Falconi, M.; Scarpa, A.; Brunetti, O.; et al. Neoadjuvant multimodal treatment of pancreatic ductal adenocarcinoma. Crit. Rev. Oncol. Hematol. 2016, 98, 309–324. [Google Scholar] [CrossRef]
- Wagner, M.; Redaelli, C.; Lietz, M.; Seiler, C.A.; Friess, H.; Buchler, M.W. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br. J. Surg. 2004, 91, 586–594. [Google Scholar] [CrossRef]
- Katz, M.H.; Wang, H.; Fleming, J.B.; Sun, C.C.; Hwang, R.F.; Wolff, R.A.; Varadhachary, G.; Abbruzzese, J.L.; Crane, C.H.; Krishnan, S.; et al. Long-term survival after multidisciplinary management of resected pancreatic adenocarcinoma. Ann. Surg. Oncol. 2009, 16, 836–847. [Google Scholar] [CrossRef] [Green Version]
- Winter, J.M.; Cameron, J.L.; Campbell, K.A.; Arnold, M.A.; Chang, D.C.; Coleman, J.; Hodgin, M.B.; Sauter, P.K.; Hruban, R.H.; Riall, T.S.; et al. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J. Gastrointest. Surg. 2006, 10, 1199–1210; discussion 1210–1191. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Stocken, D.D.; Dunn, J.A.; Almond, J.; Beger, H.G.; Pederzoli, P.; Bassi, C.; Dervenis, C.; Fernandez-Cruz, L.; Lacaine, F.; et al. Influence of resection margins on survival for patients with pancreatic cancer treated by adjuvant chemoradiation and/or chemotherapy in the ESPAC-1 randomized controlled trial. Ann. Surg. 2001, 234, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.H.; Crane, C.H.; Varadhachary, G. Management of borderline resectable pancreatic cancer. Semin. Radiat. Oncol. 2014, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Kinsella, T.J.; Seo, Y.; Willis, J.; Stellato, T.A.; Siegel, C.T.; Harpp, D.; Willson, J.K.; Gibbons, J.; Sanabria, J.R.; Hardacre, J.M.; et al. The impact of resection margin status and postoperative CA19-9 levels on survival and patterns of recurrence after postoperative high-dose radiotherapy with 5-FU-based concurrent chemotherapy for resectable pancreatic cancer. Am. J. Clin. Oncol. 2008, 31, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Bilimoria, K.Y.; Talamonti, M.S.; Sener, S.F.; Bilimoria, M.M.; Stewart, A.K.; Winchester, D.P.; Ko, C.Y.; Bentrem, D.J. Effect of hospital volume on margin status after pancreaticoduodenectomy for cancer. J. Am. Coll. Surg. 2008, 207, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Torgeson, A.; Garrido-Laguna, I.; Tao, R.; Cannon, G.M.; Scaife, C.L.; Lloyd, S. Value of surgical resection and timing of therapy in patients with pancreatic cancer at high risk for positive margins. ESMO Open 2018, 3, e000282. [Google Scholar] [CrossRef] [Green Version]
- Hidalgo, M. Pancreatic cancer. N. Engl. J. Med. 2010, 362, 1605–1617. [Google Scholar] [CrossRef] [Green Version]
- Silvestris, N.; Brunetti, O.; Vasile, E.; Cellini, F.; Cataldo, I.; Pusceddu, V.; Cattaneo, M.; Partelli, S.; Scartozzi, M.; Aprile, G.; et al. Multimodal treatment of resectable pancreatic ductal adenocarcinoma. Crit. Rev. Oncol. Hematol. 2017, 111, 152–165. [Google Scholar] [CrossRef] [Green Version]
- Versteijne, E.; Vogel, J.A.; Besselink, M.G.; Busch, O.R.C.; Wilmink, J.W.; Daams, J.G.; van Eijck, C.H.J.; Groot Koerkamp, B.; Rasch, C.R.N.; van Tienhoven, G.; et al. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br. J. Surg. 2018, 105, 946–958. [Google Scholar] [CrossRef] [Green Version]
- Strobel, O.; Berens, V.; Hinz, U.; Hartwig, W.; Hackert, T.; Bergmann, F.; Debus, J.; Jager, D.; Buchler, M.W.; Werner, J. Resection after neoadjuvant therapy for locally advanced, “unresectable” pancreatic cancer. Surgery 2012, 152, S33–S42. [Google Scholar] [CrossRef]
- van Gijn, W.; Marijnen, C.A.; Nagtegaal, I.D.; Kranenbarg, E.M.; Putter, H.; Wiggers, T.; Rutten, H.J.; Pahlman, L.; Glimelius, B.; van de Velde, C.J.; et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011, 12, 575–582. [Google Scholar] [CrossRef]
- Sauer, R.; Liersch, T.; Merkel, S.; Fietkau, R.; Hohenberger, W.; Hess, C.; Becker, H.; Raab, H.R.; Villanueva, M.T.; Witzigmann, H.; et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: Results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J. Clin. Oncol. 2012, 30, 1926–1933. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; Gambacorta, M.A.; Cellini, F.; Aristei, C.; Coco, C.; Barbaro, B.; Alfieri, S.; D’Ugo, D.; Persiani, R.; Deodato, F.; et al. The INTERACT Trial: Long-term results of a randomised trial on preoperative capecitabine-based radiochemotherapy intensified by concomitant boost or oxaliplatin, for cT2 (distal)-cT3 rectal cancer. Radiother. Oncol. 2019, 134, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.; van Lanschot, J.J.B.; Hulshof, M.; van Hagen, P.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; van Laarhoven, H.W.M.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): Long-term results of a randomised controlled trial. Lancet Oncol. 2015, 16, 1090–1098. [Google Scholar] [CrossRef]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef]
- Katz, M.H.; Marsh, R.; Herman, J.M.; Shi, Q.; Collison, E.; Venook, A.P.; Kindler, H.L.; Alberts, S.R.; Philip, P.; Lowy, A.M.; et al. Borderline resectable pancreatic cancer: Need for standardization and methods for optimal clinical trial design. Ann. Surg. Oncol. 2013, 20, 2787–2795. [Google Scholar] [CrossRef]
- Ducreux, M.; Cuhna, A.S.; Caramella, C.; Hollebecque, A.; Burtin, P.; Goere, D.; Seufferlein, T.; Haustermans, K.; Van Laethem, J.L.; Conroy, T.; et al. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26 (Suppl. 5), v56–v68. [Google Scholar] [CrossRef]
- Khorana, A.A.; McKernin, S.E.; Berlin, J.; Hong, T.S.; Maitra, A.; Moravek, C.; Mumber, M.; Schulick, R.; Zeh, H.J.; Katz, M.H.G. Potentially Curable Pancreatic Adenocarcinoma: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2019, 37, 2082–2088. [Google Scholar] [CrossRef]
- Balaban, E.P.; Mangu, P.B.; Yee, N.S. Locally Advanced Unresectable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline Summary. J. Oncol. Pract. 2017, 13, 265–269. [Google Scholar] [CrossRef]
- Palta, M.; Godfrey, D.; Goodman, K.A.; Hoffe, S.; Dawson, L.A.; Dessert, D.; Hall, W.A.; Herman, J.M.; Khorana, A.A.; Merchant, N.; et al. Radiation Therapy for Pancreatic Cancer: Executive Summary of an ASTRO Clinical Practice Guideline. Pract. Radiat. Oncol. 2019, 9, 322–332. [Google Scholar] [CrossRef]
- PDQ®. PDQ® Adult Pancreatic Cancer Treatment; Date last modified 02/14/2020; National Cancer Institute: Bethesda, MD, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26389394 (accessed on 23 April 2020).
- Hidalgo, M.; Alvarez, R.; Gallego, J.; Guillen-Ponce, C.; Laquente, B.; Macarulla, T.; Munoz, A.; Salgado, M.; Vera, R.; Adeva, J.; et al. Consensus guidelines for diagnosis, treatment and follow-up of patients with pancreatic cancer in Spain. Clin. Transl. Oncol. 2017, 19, 667–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuzillet, C.; Gaujoux, S.; Williet, N.; Bachet, J.B.; Bauguion, L.; Colson Durand, L.; Conroy, T.; Dahan, L.; Gilabert, M.; Huguet, F.; et al. Pancreatic cancer: French clinical practice guidelines for diagnosis, treatment and follow-up (SNFGE, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO, ACHBT, AFC). Dig. Liver Dis. 2018, 50, 1257–1271. [Google Scholar] [CrossRef]
- O’Reilly, D.; Fou, L.; Hasler, E.; Hawkins, J.; O’Connell, S.; Pelone, F.; Callaway, M.; Campbell, F.; Capel, M.; Charnley, R.; et al. Diagnosis and management of pancreatic cancer in adults: A summary of guidelines from the UK National Institute for Health and Care Excellence. Pancreatology 2018, 18, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Seufferlein, T.; Porzner, M.; Heinemann, V.; Tannapfel, A.; Stuschke, M.; Uhl, W. Ductal pancreatic adenocarcinoma. Dtsch. Arztebl. Int. 2014, 111, 396–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, K.; Okusaka, T.; Shimizu, K.; Furuse, J.; Ito, Y.; Hanada, K.; Shimosegawa, T.; Okazaki, K.; Committee for Revision of Clinical Guidelines for Pancreatic Cancer of the Japan Pancreas Society. Clinical Practice Guidelines for Pancreatic Cancer 2016 From the Japan Pancreas Society: A Synopsis. Pancreas 2017, 46, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Hyde, A.J.; Nassabein, R.; AlShareef, A.; Armstrong, D.; Babak, S.; Berry, S.; Bosse, D.; Chen, E.; Colwell, B.; Essery, C.; et al. Eastern Canadian Gastrointestinal Cancer Consensus Conference 2018. Curr. Oncol. 2019, 26, e665–e681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Italian Association of Medical Oncology (AIOM). National Guidelines on Esocrine Pancreatic Cancer—Linee Guida AIOM su Carcinoma del Pancreas Esocrino; AIOM: Milano, Italy, 2019.
- van Veldhuisen, E.; van den Oord, C.; Brada, L.J.; Walma, M.S.; Vogel, J.A.; Wilmink, J.W.; Del Chiaro, M.; van Lienden, K.P.; Meijerink, M.R.; van Tienhoven, G.; et al. Locally Advanced Pancreatic Cancer: Work-Up, Staging, and Local Intervention Strategies. Cancers 2019, 11, 976. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.; Verma, V.; Lazenby, A.; Ly, Q.P.; Berim, L.D.; Schwarz, J.K.; Madiyalakan, M.; Nicodemus, C.F.; Hollingsworth, M.A.; Meza, J.L.; et al. Phase I/II Trial of Neoadjuvant Oregovomab-based Chemoimmunotherapy Followed by Stereotactic Body Radiotherapy and Nelfinavir for Locally Advanced Pancreatic Adenocarcinoma. Am. J. Clin. Oncol. 2019, 42, 755–760. [Google Scholar] [CrossRef]
- European Society for Medical Oncology (ESMO): Guidelines—Gastrointestinal Cancers Pancreatic Cancer; eUpdate – Cancer of the Pancreas Treatment Recommendations; Authors: ESMO Guidelines Committee; Published: 15 March 2019. Available online: https://www.esmo.org/guidelines/gastrointestinal-cancers/pancreatic-cancer/eupdate-cancer-of-the-pancreas-treatment-recommendations. (accessed on 16 June 2020).
- Kalser, M.H.; Ellenberg, S.S. Pancreatic cancer. Adjuvant combined radiation and chemotherapy following curative resection. Arch. Surg. 1985, 120, 899–903. [Google Scholar]
- Klinkenbijl, J.H.; Jeekel, J.; Sahmoud, T.; van Pel, R.; Couvreur, M.L.; Veenhof, C.H.; Arnaud, J.P.; Gonzalez, D.G.; de Wit, L.T.; Hennipman, A.; et al. Adjuvant radiotherapy and 5-fluorouracil after curative resection of cancer of the pancreas and periampullary region: Phase III trial of the EORTC gastrointestinal tract cancer cooperative group. Ann. Surg. 1999, 230, 776–782. [Google Scholar] [CrossRef] [Green Version]
- Neoptolemos, J.P.; Stocken, D.D.; Friess, H.; Bassi, C.; Dunn, J.A.; Hickey, H.; Beger, H.; Fernandez-Cruz, L.; Dervenis, C.; Lacaine, F.; et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N. Engl. J. Med. 2004, 350, 1200–1210. [Google Scholar] [CrossRef] [Green Version]
- Narang, A.K.; Herman, J.M. The promise of modern radiotherapy in resected pancreatic adenocarcinoma: A response to Bekaii-Saab et al. Ann. Surg. Oncol. 2014, 21, 1064–1066. [Google Scholar] [CrossRef] [Green Version]
- Franke, A.J.; Rosati, L.M.; Pawlik, T.M.; Kumar, R.; Herman, J.M. The role of radiation therapy in pancreatic ductal adenocarcinoma in the neoadjuvant and adjuvant settings. Semin. Oncol. 2015, 42, 144–162. [Google Scholar] [CrossRef]
- Brunner, T.B.; Scott-Brown, M. The role of radiotherapy in multimodal treatment of pancreatic carcinoma. Radiat. Oncol. 2010, 5, 64. [Google Scholar] [CrossRef] [Green Version]
- Berger, A.C.; Winter, K.; Hoffman, J.P.; Regine, W.F.; Abrams, R.A.; Safran, H.; Freedman, G.M.; Benson, A.B., 3rd; Macdonald, J.; Willett, C.G. Five year results of US intergroup/RTOG 9704 with postoperative CA 19-9 </=90 U/mL and comparison to the CONKO-001 trial. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, e291–e297. [Google Scholar] [CrossRef]
- Hsu, C.C.; Herman, J.M.; Corsini, M.M.; Winter, J.M.; Callister, M.D.; Haddock, M.G.; Cameron, J.L.; Pawlik, T.M.; Schulick, R.D.; Wolfgang, C.L.; et al. Adjuvant chemoradiation for pancreatic adenocarcinoma: The Johns Hopkins Hospital-Mayo Clinic collaborative study. Ann. Surg. Oncol. 2010, 17, 981–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morganti, A.G.; Falconi, M.; van Stiphout, R.G.; Mattiucci, G.C.; Alfieri, S.; Calvo, F.A.; Dubois, J.B.; Fastner, G.; Herman, J.M.; Maidment, B.W., 3rd; et al. Multi-institutional pooled analysis on adjuvant chemoradiation in pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Morganti, A.G.; Cellini, F.; Buwenge, M.; Arcelli, A.; Alfieri, S.; Calvo, F.A.; Casadei, R.; Cilla, S.; Deodato, F.; Di Gioia, G.; et al. Adjuvant chemoradiation in pancreatic cancer: Impact of radiotherapy dose on survival. BMC Cancer 2019, 19, 569. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.L.; Chone, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef] [PubMed]
- Safran, H.; Winter, K.A.; Abrams, R.A.; Regine, W.; Goodman, K.A.; Berger, A.C.; Gillin, M.; Philip, P.A.; Lowy, A.M.; Wu, A.J.; et al. Results of the randomized phase II portion of NRG Oncology/RTOG 0848 evaluating the addition of erlotinib to adjuvant gemcitabine for patients with resected pancreatic head adenocarcinoma. J. Clin. Oncol. 2017, 35. [Google Scholar] [CrossRef]
- Hammel, P.; Huguet, F.; van Laethem, J.L.; Goldstein, D.; Glimelius, B.; Artru, P.; Borbath, I.; Bouche, O.; Shannon, J.; Andre, T.; et al. Effect of Chemoradiotherapy vs Chemotherapy on Survival in Patients with Locally Advanced Pancreatic Cancer Controlled After 4 Months of Gemcitabine With or Without Erlotinib: The LAP07 Randomized Clinical Trial. JAMA 2016, 315, 1844–1853. [Google Scholar] [CrossRef]
- Scartozzi, M.; Giampieri, R.; Del Prete, M.; Faloppi, L.; Bianconi, M.; Vincenzi, B.; Tonini, G.; Santini, D.; Cascinu, S. Selected gastrointestinal cancer presentations from the American Society of Clinical Oncology annual meeting 2013 in review: It is not about the destination, it is about the journey. Expert Opin. Pharmacother. 2014, 15, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.; Chadha, A.S.; Suh, Y.; Chen, H.C.; Rao, A.; Das, P.; Minsky, B.D.; Mahmood, U.; Delclos, M.E.; Sawakuchi, G.O.; et al. Focal Radiation Therapy Dose Escalation Improves Overall Survival in Locally Advanced Pancreatic Cancer Patients Receiving Induction Chemotherapy and Consolidative Chemoradiation. Int. J. Radiat. Oncol. Biol. Phys. 2016, 94, 755–765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colbert, L.E.; Moningi, S.; Chadha, A.; Amer, A.; Lee, Y.; Wolff, R.A.; Varadhachary, G.; Fleming, J.; Katz, M.; Das, P.; et al. Dose escalation with an IMRT technique in 15 to 28 fractions is better tolerated than standard doses of 3DCRT for LAPC. Adv. Radiat. Oncol. 2017, 2, 403–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morganti, A.G.; Trodella, L.; Valentini, V.; Barbi, S.; Macchia, G.; Mantini, G.; Turriziani, A.; Cellini, N. Pain relief with short-term irradiation in locally advanced carcinoma of the pancreas. J. Palliat. Care 2003, 19, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Buwenge, M.; Macchia, G.; Arcelli, A.; Frakulli, R.; Fuccio, L.; Guerri, S.; Grassi, E.; Cammelli, S.; Cellini, F.; Morganti, A.G. Stereotactic radiotherapy of pancreatic cancer: A systematic review on pain relief. J. Pain Res. 2018, 11, 2169–2178. [Google Scholar] [CrossRef] [Green Version]
- Badiyan, S.N.; Molitoris, J.K.; Chuong, M.D.; Regine, W.F.; Kaiser, A. The Role of Radiation Therapy for Pancreatic Cancer in the Adjuvant and Neoadjuvant Settings. Surg. Oncol. Clin. N. Am. 2017, 26, 431–453. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.Y.; Han, Y.; Lee, H.; Kim, S.W.; Kwon, W.; Lee, K.H.; Oh, D.Y.; Chie, E.K.; Lee, J.M.; Heo, J.S.; et al. Oncological Benefits of Neoadjuvant Chemoradiation With Gemcitabine Versus Upfront Surgery in Patients with Borderline Resectable Pancreatic Cancer: A Prospective, Randomized, Open-label, Multicenter Phase 2/3 Trial. Ann. Surg. 2018, 268, 215–222. [Google Scholar] [CrossRef]
- Robin, T.P.; Goodman, K.A. Radiation therapy in the management of pancreatic adenocarcinoma: Review of current evidence and future opportunities. Chin. Clin. Oncol. 2017, 6, 28. [Google Scholar] [CrossRef]
- Versteijne, E.; Suker, M.; Groothuis, K.; Akkermans-Vogelaar, J.M.; Besselink, M.G.; Bonsing, B.A.; Buijsen, J.; Busch, O.R.; Creemers, G.M.; van Dam, R.M.; et al. Preoperative Chemoradiotherapy Versus Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J. Clin. Oncol. 2020, 38, 1763–1773. [Google Scholar] [CrossRef]
- Abrams, R.A.; Winter, K.A.; Regine, W.F.; Safran, H.; Hoffman, J.P.; Lustig, R.; Konski, A.A.; Benson, A.B.; Macdonald, J.S.; Rich, T.A.; et al. Failure to adhere to protocol specified radiation therapy guidelines was associated with decreased survival in RTOG 9704--a phase III trial of adjuvant chemotherapy and chemoradiotherapy for patients with resected adenocarcinoma of the pancreas. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 809–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodman, K.A.; Regine, W.F.; Dawson, L.A.; Ben-Josef, E.; Haustermans, K.; Bosch, W.R.; Turian, J.; Abrams, R.A. Radiation Therapy Oncology Group consensus panel guidelines for the delineation of the clinical target volume in the postoperative treatment of pancreatic head cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 901–908. [Google Scholar] [CrossRef]
- Luterstein, E.; Cao, M.; Lamb, J.; Raldow, A.C.; Low, D.A.; Steinberg, M.L.; Lee, P. Stereotactic MRI-guided Adaptive Radiation Therapy (SMART) for Locally Advanced Pancreatic Cancer: A Promising Approach. Cureus 2018, 10, e2324. [Google Scholar] [CrossRef] [Green Version]
- Heerkens, H.D.; Hall, W.A.; Li, X.A.; Knechtges, P.; Dalah, E.; Paulson, E.S.; van den Berg, C.A.T.; Meijer, G.J.; Koay, E.J.; Crane, C.H.; et al. Recommendations for MRI-based contouring of gross tumor volume and organs at risk for radiation therapy of pancreatic cancer. Pract. Radiat. Oncol. 2017, 7, 126–136. [Google Scholar] [CrossRef] [Green Version]
- Hall, W.A.; Heerkens, H.D.; Paulson, E.S.; Meijer, G.J.; Kotte, A.N.; Knechtges, P.; Parikh, P.J.; Bassetti, M.F.; Lee, P.; Aitken, K.L.; et al. Pancreatic gross tumor volume contouring on computed tomography (CT) compared with magnetic resonance imaging (MRI): Results of an international contouring conference. Pract. Radiat. Oncol. 2018, 8, 107–115. [Google Scholar] [CrossRef]
- Caravatta, L.; Macchia, G.; Mattiucci, G.C.; Sainato, A.; Cernusco, N.L.; Mantello, G.; Di Tommaso, M.; Trignani, M.; De Paoli, A.; Boz, G.; et al. Inter-observer variability of clinical target volume delineation in radiotherapy treatment of pancreatic cancer: A multi-institutional contouring experience. Radiat. Oncol. 2014, 9, 198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caravatta, L.; Cellini, F.; Simoni, N.; Rosa, C.; Niespolo, R.M.; Lupattelli, M.; Picardi, V.; Macchia, G.; Sainato, A.; Mantello, G.; et al. Magnetic resonance imaging (MRI) compared with computed tomography (CT) for interobserver agreement of gross tumor volume delineation in pancreatic cancer: A multi-institutional contouring study on behalf of the AIRO group for gastrointestinal cancers. Acta Oncol. 2019, 58, 439–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morganti, A.G.; Cellini, N.; Mattiucci, G.C.; Macchia, G.; Smaniotto, D.; Luzi, S.; Balducci, M.; Deodato, F.; Valentini, V.; Trodella, L. Lymphatic drainage and CTV in pancreatic carcinoma. Rays 2003, 28, 311–315. [Google Scholar] [PubMed]
- Brunner, T.B.; Merkel, S.; Grabenbauer, G.G.; Meyer, T.; Baum, U.; Papadopoulos, T.; Sauer, R.; Hohenberger, W. Definition of elective lymphatic target volume in ductal carcinoma of the pancreatic head based on histopathologic analysis. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 1021–1029. [Google Scholar] [CrossRef]
- Sun, W.; Leong, C.N.; Zhang, Z.; Lu, J.J. Proposing the lymphatic target volume for elective radiation therapy for pancreatic cancer: A pooled analysis of clinical evidence. Radiat. Oncol. 2010, 5, 28. [Google Scholar] [CrossRef] [Green Version]
- Caravatta, L.; Sallustio, G.; Pacelli, F.; Padula, G.D.; Deodato, F.; Macchia, G.; Massaccesi, M.; Picardi, V.; Cilla, S.; Marinelli, A.; et al. Clinical target volume delineation including elective nodal irradiation in preoperative and definitive radiotherapy of pancreatic cancer. Radiat. Oncol. 2012, 7, 86. [Google Scholar] [CrossRef] [Green Version]
- Oar, A.; Lee, M.; Le, H.; Hruby, G.; Dalfsen, R.; Pryor, D.; Lee, D.; Chu, J.; Holloway, L.; Briggs, A.; et al. Australasian Gastrointestinal Trials Group (AGITG) and Trans-Tasman Radiation Oncology Group (TROG) Guidelines for Pancreatic Stereotactic Body Radiation Therapy (SBRT). Pract. Radiat. Oncol. 2019. [Google Scholar] [CrossRef]
- Katz, M.H.G.; Ou, F.S.; Herman, J.M.; Ahmad, S.A.; Wolpin, B.; Marsh, R.; Behr, S.; Shi, Q.; Chuong, M.; Schwartz, L.H.; et al. Alliance for clinical trials in oncology (ALLIANCE) trial A021501: Preoperative extended chemotherapy vs. chemotherapy plus hypofractionated radiation therapy for borderline resectable adenocarcinoma of the head of the pancreas. BMC Cancer 2017, 17, 505. [Google Scholar] [CrossRef]
- Mellon, E.A.; Hoffe, S.E.; Springett, G.M.; Frakes, J.M.; Strom, T.J.; Hodul, P.J.; Malafa, M.P.; Chuong, M.D.; Shridhar, R. Long-term outcomes of induction chemotherapy and neoadjuvant stereotactic body radiotherapy for borderline resectable and locally advanced pancreatic adenocarcinoma. Acta Oncol. 2015, 54, 979–985. [Google Scholar] [CrossRef]
- Mendenhall, N.P.; Malyapa, R.S.; Su, Z.; Yeung, D.; Mendenhall, W.M.; Li, Z. Proton therapy for head and neck cancer: Rationale, potential indications, practical considerations, and current clinical evidence. Acta Oncol. 2011, 50, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Nichols, R.C.; Huh, S.; Li, Z.; Rutenberg, M. Proton therapy for pancreatic cancer. World J. Gastrointest. Oncol. 2015, 7, 141–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiroshima, Y.; Fukumitsu, N.; Saito, T.; Numajiri, H.; Murofushi, K.N.; Ohnishi, K.; Nonaka, T.; Ishikawa, H.; Okumura, T.; Sakurai, H. Concurrent chemoradiotherapy using proton beams for unresectable locally advanced pancreatic cancer. Radiother Oncol. 2019, 136, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Hong, T.S.; Ryan, D.P.; Borger, D.R.; Blaszkowsky, L.S.; Yeap, B.Y.; Ancukiewicz, M.; Deshpande, V.; Shinagare, S.; Wo, J.Y.; Boucher, Y.; et al. A phase 1/2 and biomarker study of preoperative short course chemoradiation with proton beam therapy and capecitabine followed by early surgery for resectable pancreatic ductal adenocarcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 830–838. [Google Scholar] [CrossRef] [Green Version]
- Ebner, D.K.; Kamada, T. The Emerging Role of Carbon-Ion Radiotherapy. Front. Oncol. 2016, 6, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shinoto, M.; Yamada, S.; Yasuda, S.; Imada, H.; Shioyama, Y.; Honda, H.; Kamada, T.; Tsujii, H.; Saisho, H.; Working Group for Pancreas, C. Phase 1 trial of preoperative, short-course carbon-ion radiotherapy for patients with resectable pancreatic cancer. Cancer 2013, 119, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Kawashiro, S.; Yamada, S.; Okamoto, M.; Ohno, T.; Nakano, T.; Shinoto, M.; Shioyama, Y.; Nemoto, K.; Isozaki, Y.; Tsuji, H.; et al. Multi-institutional Study of Carbon-ion Radiotherapy for Locally Advanced Pancreatic Cancer: Japan Carbon-ion Radiation Oncology Study Group (J-CROS) Study 1403 Pancreas. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 1212–1221. [Google Scholar] [CrossRef] [PubMed]
- Heerkens, H.D.; van Vulpen, M.; Erickson, B.; Reerink, O.; Intven, M.P.; van den Berg, C.A.; Molenaar, I.Q.; Vleggaar, F.P.; Meijer, G.J. MRI guided stereotactic radiotherapy for locally advanced pancreatic cancer. Br. J. Radiol. 2018, 91, 20170563. [Google Scholar] [CrossRef] [PubMed]
- Boldrini, L.; Cusumano, D.; Cellini, F.; Azario, L.; Mattiucci, G.C.; Valentini, V. Online adaptive magnetic resonance guided radiotherapy for pancreatic cancer: State of the art, pearls and pitfalls. Radiat. Oncol. 2019, 14, 71. [Google Scholar] [CrossRef] [PubMed]
- Boldrini, L.; Cellini, F.; Manfrida, S.; Chiloiro, G.; Teodoli, S.; Cusumano, D.; Fionda, B.; Mattiucci, G.C.; De Gaetano, A.M.; Azario, L.; et al. Use of Indirect Target Gating in Magnetic Resonance-guided Liver Stereotactic Body Radiotherapy: Case Report of an Oligometastatic Patient. Cureus 2018, 10, e2292. [Google Scholar] [CrossRef] [Green Version]
- Massaccesi, M.; Cusumano, D.; Boldrini, L.; Dinapoli, N.; Fionda, B.; Teodoli, S.; Azario, L.; Mattiucci, G.C.; Balducci, M.; Cellini, F.; et al. A new frontier of image guidance: Organs at risk avoidance with MRI-guided respiratory-gated intensity modulated radiotherapy: Technical note and report of a case. J. Appl. Clin. Med. Phys. 2019, 20, 194–198. [Google Scholar] [CrossRef] [Green Version]
- Bruynzeel, A.M.E.; Lagerwaard, F.J. The role of biological dose-escalation for pancreatic cancer. Clin. Transl. Radiat. Oncol. 2019, 18, 128–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henke, L.; Kashani, R.; Robinson, C.; Curcuru, A.; DeWees, T.; Bradley, J.; Green, O.; Michalski, J.; Mutic, S.; Parikh, P.; et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother. Oncol. 2018, 126, 519–526. [Google Scholar] [CrossRef] [Green Version]
- Rudra, S.; Jiang, N.; Rosenberg, S.A.; Olsen, J.R.; Roach, M.C.; Wan, L.; Portelance, L.; Mellon, E.A.; Bruynzeel, A.; Lagerwaard, F.; et al. Using adaptive magnetic resonance image-guided radiation therapy for treatment of inoperable pancreatic cancer. Cancer Med. 2019, 8, 2123–2132. [Google Scholar] [CrossRef]
- Bohoudi, O.; Bruynzeel, A.M.E.; Senan, S.; Cuijpers, J.P.; Slotman, B.J.; Lagerwaard, F.J.; Palacios, M.A. Fast and robust online adaptive planning in stereotactic MR-guided adaptive radiation therapy (SMART) for pancreatic cancer. Radiother. Oncol. 2017, 125, 439–444. [Google Scholar] [CrossRef]
- El-Bared, N.; Portelance, L.; Spieler, B.O.; Kwon, D.; Padgett, K.R.; Brown, K.M.; Mellon, E.A. Dosimetric Benefits and Practical Pitfalls of Daily Online Adaptive MRI-Guided Stereotactic Radiation Therapy for Pancreatic Cancer. Pract. Radiat. Oncol. 2019, 9, e46–e54. [Google Scholar] [CrossRef]
- Bohoudi, O.; Bruynzeel, A.M.E.; Meijerink, M.R.; Senan, S.; Slotman, B.J.; Palacios, M.A.; Lagerwaard, F.J. Identification of patients with locally advanced pancreatic cancer benefitting from plan adaptation in MR-guided radiation therapy. Radiother. Oncol. 2019, 132, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Lagerwaard, F.; Bohoudi, O.; Tetar, S.; Admiraal, M.A.; Rosario, T.S.; Bruynzeel, A. Combined Inter- and Intrafractional Plan Adaptation Using Fraction Partitioning in Magnetic Resonance-guided Radiotherapy Delivery. Cureus 2018, 10, e2434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tyran, M.; Jiang, N.; Cao, M.; Raldow, A.; Lamb, J.M.; Low, D.; Luterstein, E.; Steinberg, M.L.; Lee, P. Retrospective evaluation of decision-making for pancreatic stereotactic MR-guided adaptive radiotherapy. Radiother. Oncol. 2018, 129, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Potters, L.; Kavanagh, B.; Galvin, J.M.; Hevezi, J.M.; Janjan, N.A.; Larson, D.A.; Mehta, M.P.; Ryu, S.; Steinberg, M.; Timmerman, R.; et al. American Society for Therapeutic Radiology and Oncology (ASTRO) and American College of Radiology (ACR) practice guideline for the performance of stereotactic body radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 326–332. [Google Scholar] [CrossRef]
- Schellenberg, D.; Goodman, K.A.; Lee, F.; Chang, S.; Kuo, T.; Ford, J.M.; Fisher, G.A.; Quon, A.; Desser, T.S.; Norton, J.; et al. Gemcitabine chemotherapy and single-fraction stereotactic body radiotherapy for locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 678–686. [Google Scholar] [CrossRef] [PubMed]
- Gurka, M.K.; Collins, S.P.; Slack, R.; Tse, G.; Charabaty, A.; Ley, L.; Berzcel, L.; Lei, S.; Suy, S.; Haddad, N.; et al. Stereotactic body radiation therapy with concurrent full-dose gemcitabine for locally advanced pancreatic cancer: A pilot trial demonstrating safety. Radiat. Oncol. 2013, 8, 44. [Google Scholar] [CrossRef] [Green Version]
- Chen-Zhao, X.; Hernando, O.; Lopez, M.; Sanchez, E.; Montero, A.; Garcia-Aranda, M.; Ciervide, R.; Valero, J.; Alonso, R.; Cardenas-Rebollo, J.M.; et al. A prospective observational study of the clinical and pathological impact of stereotactic body radiotherapy (SBRT) as a neoadjuvant strategy of chemoradiation in pancreatic cancer. Clin. Transl. Oncol. 2020, 1–7. [Google Scholar] [CrossRef]
- Xiang, M.; Heestand, G.M.; Chang, D.T.; Pollom, E.L. Neoadjuvant treatment strategies for resectable pancreas cancer: A propensity-matched analysis of the National Cancer Database. Radiother. Oncol. 2020, 143, 101–107. [Google Scholar] [CrossRef]
- Golcher, H.; Brunner, T.B.; Witzigmann, H.; Marti, L.; Bechstein, W.O.; Bruns, C.; Jungnickel, H.; Schreiber, S.; Grabenbauer, G.G.; Meyer, T.; et al. Neoadjuvant chemoradiation therapy with gemcitabine/cisplatin and surgery versus immediate surgery in resectable pancreatic cancer: Results of the first prospective randomized phase II trial. Strahlenther. Onkol. 2015, 191, 7–16. [Google Scholar] [CrossRef] [Green Version]
- Casadei, R.; Di Marco, M.; Ricci, C.; Santini, D.; Serra, C.; Calculli, L.; D’Ambra, M.; Guido, A.; Morselli-Labate, A.M.; Minni, F. Neoadjuvant Chemoradiotherapy and Surgery Versus Surgery Alone in Resectable Pancreatic Cancer: A Single-Center Prospective, Randomized, Controlled Trial Which Failed to Achieve Accrual Targets. J. Gastrointest. Surg. 2015, 19, 1802–1812. [Google Scholar] [CrossRef]
- Petrelli, F.; Inno, A.; Barni, S.; Ghidini, A.; Labianca, R.; Falconi, M.; Reni, M.; Cascinu, S.; GISCAD; San Raffaele Hospital. Borderline resectable pancreatic cancer: More than an anatomical concept. Dig. Liver Dis. 2017, 49, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Callery, M.P.; Chang, K.J.; Fishman, E.K.; Talamonti, M.S.; William Traverso, L.; Linehan, D.C. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: Expert consensus statement. Ann. Surg. Oncol. 2009, 16, 1727–1733. [Google Scholar] [CrossRef] [PubMed]
- Landry, J.; Catalano, P.J.; Staley, C.; Harris, W.; Hoffman, J.; Talamonti, M.; Xu, N.; Cooper, H.; Benson, A.B., 3rd. Randomized phase II study of gemcitabine plus radiotherapy versus gemcitabine, 5-fluorouracil, and cisplatin followed by radiotherapy and 5-fluorouracil for patients with locally advanced, potentially resectable pancreatic adenocarcinoma. J. Surg. Oncol. 2010, 101, 587–592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Truty, M.J.; Thomas, R.M.; Katz, M.H.; Vauthey, J.N.; Crane, C.; Varadhachary, G.R.; Wolff, R.A.; Abbruzzese, J.L.; Lee, J.E.; Fleming, J.B. Multimodality therapy offers a chance for cure in patients with pancreatic adenocarcinoma deemed unresectable at first operative exploration. J. Am. Coll. Surg. 2012, 215, 41–51. [Google Scholar] [CrossRef] [Green Version]
- Katz, M.H.; Pisters, P.W.; Evans, D.B.; Sun, C.C.; Lee, J.E.; Fleming, J.B.; Vauthey, J.N.; Abdalla, E.K.; Crane, C.H.; Wolff, R.A.; et al. Borderline resectable pancreatic cancer: The importance of this emerging stage of disease. J. Am. Coll. Surg. 2008, 206, 833–846. [Google Scholar] [CrossRef] [Green Version]
- Varadhachary, G.R.; Tamm, E.P.; Abbruzzese, J.L.; Xiong, H.Q.; Crane, C.H.; Wang, H.; Lee, J.E.; Pisters, P.W.; Evans, D.B.; Wolff, R.A. Borderline resectable pancreatic cancer: Definitions, management, and role of preoperative therapy. Ann. Surg. Oncol. 2006, 13, 1035–1046. [Google Scholar] [CrossRef]
- Takai, S.; Satoi, S.; Yanagimoto, H.; Toyokawa, H.; Takahashi, K.; Terakawa, N.; Araki, H.; Matsui, Y.; Sohgawa, M.; Kamiyama, Y. Neoadjuvant chemoradiation in patients with potentially resectable pancreatic cancer. Pancreas 2008, 36, e26–e32. [Google Scholar] [CrossRef]
- Brown, K.M.; Siripurapu, V.; Davidson, M.; Cohen, S.J.; Konski, A.; Watson, J.C.; Li, T.; Ciocca, V.; Cooper, H.; Hoffman, J.P. Chemoradiation followed by chemotherapy before resection for borderline pancreatic adenocarcinoma. Am. J. Surg. 2008, 195, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Chung, Y.E.; Park, J.Y.; Sung, J.S.; Hwang, H.K.; Choi, H.J.; Kim, H.; Song, S.Y.; Lee, W.J. Potential contribution of preoperative neoadjuvant concurrent chemoradiation therapy on margin-negative resection in borderline resectable pancreatic cancer. J. Gastrointest. Surg. 2012, 16, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Massucco, P.; Capussotti, L.; Magnino, A.; Sperti, E.; Gatti, M.; Muratore, A.; Sgotto, E.; Gabriele, P.; Aglietta, M. Pancreatic resections after chemoradiotherapy for locally advanced ductal adenocarcinoma: Analysis of perioperative outcome and survival. Ann. Surg. Oncol. 2006, 13, 1201–1208. [Google Scholar] [CrossRef]
- Kim, E.J.; Ben-Josef, E.; Herman, J.M.; Bekaii-Saab, T.; Dawson, L.A.; Griffith, K.A.; Francis, I.R.; Greenson, J.K.; Simeone, D.M.; Lawrence, T.S.; et al. A multi-institutional phase 2 study of neoadjuvant gemcitabine and oxaliplatin with radiation therapy in patients with pancreatic cancer. Cancer 2013, 119, 2692–2700. [Google Scholar] [CrossRef] [Green Version]
- Swaminath, A.; Chu, W. Stereotactic body radiotherapy for the treatment of medically inoperable primary renal cell carcinoma: Current evidence and future directions. Can. Urol. Assoc. J. 2015, 9, 275–280. [Google Scholar] [CrossRef] [Green Version]
- Boone, B.A.; Steve, J.; Krasinskas, A.M.; Zureikat, A.H.; Lembersky, B.C.; Gibson, M.K.; Stoller, R.G.; Zeh, H.J.; Bahary, N. Outcomes with FOLFIRINOX for borderline resectable and locally unresectable pancreatic cancer. J. Surg. Oncol. 2013, 108, 236–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajagopalan, M.S.; Heron, D.E.; Wegner, R.E.; Zeh, H.J.; Bahary, N.; Krasinskas, A.M.; Lembersky, B.; Brand, R.; Moser, A.J.; Quinn, A.E.; et al. Pathologic response with neoadjuvant chemotherapy and stereotactic body radiotherapy for borderline resectable and locally-advanced pancreatic cancer. Radiat. Oncol. 2013, 8, 254. [Google Scholar] [CrossRef] [Green Version]
- Moningi, S.; Dholakia, A.S.; Raman, S.P.; Blackford, A.; Cameron, J.L.; Le, D.T.; De Jesus-Acosta, A.M.; Hacker-Prietz, A.; Rosati, L.M.; Assadi, R.K.; et al. The Role of Stereotactic Body Radiation Therapy for Pancreatic Cancer: A Single-Institution Experience. Ann. Surg. Oncol. 2015, 22, 2352–2358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pollom, E.L.; Alagappan, M.; von Eyben, R.; Kunz, P.L.; Fisher, G.A.; Ford, J.A.; Poultsides, G.A.; Visser, B.C.; Norton, J.A.; Kamaya, A.; et al. Single- versus multifraction stereotactic body radiation therapy for pancreatic adenocarcinoma: Outcomes and toxicity. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Shaib, W.L.; Hawk, N.; Cassidy, R.J.; Chen, Z.; Zhang, C.; Brutcher, E.; Kooby, D.; Maithel, S.K.; Sarmiento, J.M.; Landry, J.; et al. A Phase 1 Study of Stereotactic Body Radiation Therapy Dose Escalation for Borderline Resectable Pancreatic Cancer After Modified FOLFIRINOX (NCT01446458). Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Kharofa, J.; Mierzwa, M.; Olowokure, O.; Sussman, J.; Latif, T.; Gupta, A.; Xie, C.; Patel, S.; Esslinger, H.; McGill, B.; et al. Pattern of Marginal Local Failure in a Phase II Trial of Neoadjuvant Chemotherapy and Stereotactic Body Radiation Therapy for Resectable and Borderline Resectable Pancreas Cancer. Am. J. Clin. Oncol. 2019, 42, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Willett, C.G.; Czito, B.G.; Bendell, J.C.; Ryan, D.P. Locally advanced pancreatic cancer. J. Clin. Oncol. 2005, 23, 4538–4544. [Google Scholar] [CrossRef]
- Iacobuzio-Donahue, C.A.; Fu, B.; Yachida, S.; Luo, M.; Abe, H.; Henderson, C.M.; Vilardell, F.; Wang, Z.; Keller, J.W.; Banerjee, P.; et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J. Clin. Oncol. 2009, 27, 1806–1813. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, H.; Takamori, H.; Kanemitsu, K.; Chikamoto, A.; Beppu, T.; Baba, H. An autopsy study to clarify characteristics of local recurrence after extended pancreatectomy with intraoperative radiation therapy in patients with pancreatic cancer. Langenbecks Arch. Surg. 2012, 397, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Loehrer, P.J., Sr.; Feng, Y.; Cardenes, H.; Wagner, L.; Brell, J.M.; Cella, D.; Flynn, P.; Ramanathan, R.K.; Crane, C.H.; Alberts, S.R.; et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: An Eastern Cooperative Oncology Group trial. J. Clin. Oncol. 2011, 29, 4105–4112. [Google Scholar] [CrossRef] [PubMed]
- Koong, A.C.; Le, Q.T.; Ho, A.; Fong, B.; Fisher, G.; Cho, C.; Ford, J.; Poen, J.; Gibbs, I.C.; Mehta, V.K.; et al. Phase I study of stereotactic radiosurgery in patients with locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2004, 58, 1017–1021. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, D.; Kim, J.; Christman-Skieller, C.; Chun, C.L.; Columbo, L.A.; Ford, J.M.; Fisher, G.A.; Kunz, P.L.; Van Dam, J.; Quon, A.; et al. Single-fraction stereotactic body radiation therapy and sequential gemcitabine for the treatment of locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 181–188. [Google Scholar] [CrossRef]
- Song, Y.; Yuan, Z.; Li, F.; Dong, Y.; Zhuang, H.; Wang, J.; Chen, H.; Wang, P. Analysis of clinical efficacy of CyberKnife((R)) treatment for locally advanced pancreatic cancer. OncoTargets Ther. 2015, 8, 1427–1431. [Google Scholar] [CrossRef] [Green Version]
- Tozzi, A.; Comito, T.; Alongi, F.; Navarria, P.; Iftode, C.; Mancosu, P.; Reggiori, G.; Clerici, E.; Rimassa, L.; Zerbi, A.; et al. SBRT in unresectable advanced pancreatic cancer: Preliminary results of a mono-institutional experience. Radiat. Oncol. 2013, 8, 148. [Google Scholar] [CrossRef] [Green Version]
- Goyal, K.; Einstein, D.; Ibarra, R.A.; Yao, M.; Kunos, C.; Ellis, R.; Brindle, J.; Singh, D.; Hardacre, J.; Zhang, Y.; et al. Stereotactic body radiation therapy for nonresectable tumors of the pancreas. J. Surg. Res. 2012, 174, 319–325. [Google Scholar] [CrossRef] [Green Version]
- Polistina, F.; Costantin, G.; Casamassima, F.; Francescon, P.; Guglielmi, R.; Panizzoni, G.; Febbraro, A.; Ambrosino, G. Unresectable locally advanced pancreatic cancer: A multimodal treatment using neoadjuvant chemoradiotherapy (gemcitabine plus stereotactic radiosurgery) and subsequent surgical exploration. Ann. Surg. Oncol. 2010, 17, 2092–2101. [Google Scholar] [CrossRef]
- Rwigema, J.C.; Parikh, S.D.; Heron, D.E.; Howell, M.; Zeh, H.; Moser, A.J.; Bahary, N.; Quinn, A.; Burton, S.A. Stereotactic body radiotherapy in the treatment of advanced adenocarcinoma of the pancreas. Am. J. Clin. Oncol. 2011, 34, 63–69. [Google Scholar] [CrossRef]
- Mahadevan, A.; Miksad, R.; Goldstein, M.; Sullivan, R.; Bullock, A.; Buchbinder, E.; Pleskow, D.; Sawhney, M.; Kent, T.; Vollmer, C.; et al. Induction gemcitabine and stereotactic body radiotherapy for locally advanced nonmetastatic pancreas cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, e615–e622. [Google Scholar] [CrossRef]
- Herman, J.M.; Chang, D.T.; Goodman, K.A.; Dholakia, A.S.; Raman, S.P.; Hacker-Prietz, A.; Iacobuzio-Donahue, C.A.; Griffith, M.E.; Pawlik, T.M.; Pai, J.S.; et al. Phase 2 multi-institutional trial evaluating gemcitabine and stereotactic body radiotherapy for patients with locally advanced unresectable pancreatic adenocarcinoma. Cancer 2015, 121, 1128–1137. [Google Scholar] [CrossRef] [PubMed]
- Arcelli, A.; Guido, A.; Buwenge, M.; Simoni, N.; Mazzarotto, R.; Macchia, G.; Deodato, F.; Cilla, S.; Bonomo, P.; Scotti, V.; et al. Higher Biologically Effective Dose Predicts Survival in SBRT of Pancreatic Cancer: A Multicentric Analysis (PAULA-1). Anticancer Res. 2020, 40, 465–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, J.; Yoon, S.M.; Park, J.H.; Seo, D.W.; Lee, S.S.; Kim, M.H.; Lee, S.K.; Park, D.H.; Song, T.J.; Ryoo, B.Y.; et al. Stereotactic body radiation therapy for locally advanced pancreatic cancer. PLoS ONE 2019, 14, e0214970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, B.C.; Gleisner, A.; Rigg, D.; Meguid, C.; Goodman, K.; Brauer, B.; Gajdos, C.; Schulick, R.D.; Edil, B.H.; McCarter, M.D. Perioperative outcomes and survival following neoadjuvant stereotactic body radiation therapy (SBRT) versus intensity-modulated radiation therapy (IMRT) in pancreatic adenocarcinoma. J. Surg. Oncol. 2018, 117, 1073–1083. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.F.; Rosati, L.M.; Groot, V.P.; Le, D.T.; Zheng, L.; Laheru, D.A.; Shin, E.J.; Jackson, J.; Moore, J.; Narang, A.K.; et al. Stereotactic body radiation therapy for palliative management of pancreatic adenocarcinoma in elderly and medically inoperable patients. Oncotarget 2018, 9, 16427–16436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukherjee, S.; Hurt, C.N.; Bridgewater, J.; Falk, S.; Cummins, S.; Wasan, H.; Crosby, T.; Jephcott, C.; Roy, R.; Radhakrishna, G.; et al. Gemcitabine-based or capecitabine-based chemoradiotherapy for locally advanced pancreatic cancer (SCALOP): A multicentre, randomised, phase 2 trial. Lancet Oncol. 2013, 14, 317–326. [Google Scholar] [CrossRef] [Green Version]
- Petrelli, F.; Comito, T.; Ghidini, A.; Torri, V.; Scorsetti, M.; Barni, S. Stereotactic Body Radiation Therapy for Locally Advanced Pancreatic Cancer: A Systematic Review and Pooled Analysis of 19 Trials. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Brunner, T.B.; Nestle, U.; Grosu, A.L.; Partridge, M. SBRT in pancreatic cancer: What is the therapeutic window? Radiother. Oncol. 2015, 114, 109–116. [Google Scholar] [CrossRef]
- Denost, Q.; Laurent, C.; Adam, J.P.; Capdepont, M.; Vendrely, V.; Collet, D.; Cunha, A.S. Pancreaticoduodenectomy following chemoradiotherapy for locally advanced adenocarcinoma of the pancreatic head. HPB 2013, 15, 716–723. [Google Scholar] [CrossRef] [Green Version]
- Orlandi, E.; Palazzi, M.; Pignoli, E.; Fallai, C.; Giostra, A.; Olmi, P. Radiobiological basis and clinical results of the simultaneous integrated boost (SIB) in intensity modulated radiotherapy (IMRT) for head and neck cancer: A review. Crit. Rev. Oncol. Hematol. 2010, 73, 111–125. [Google Scholar] [CrossRef]
- Crane, C.H. Hypofractionated ablative radiotherapy for locally advanced pancreatic cancer. J. Radiat. Res. 2016, 57 (Suppl. 1), i53–i57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, S.Y.; Chang, J.S.; Lee, B.M.; Kim, K.H.; Lee, K.J.; Seong, J. Dose escalation in locally advanced pancreatic cancer patients receiving chemoradiotherapy. Radiother. Oncol. 2017, 123, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Chuong, M.D.; Springett, G.M.; Freilich, J.M.; Park, C.K.; Weber, J.M.; Mellon, E.A.; Hodul, P.J.; Malafa, M.P.; Meredith, K.L.; Hoffe, S.E.; et al. Stereotactic body radiation therapy for locally advanced and borderline resectable pancreatic cancer is effective and well tolerated. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Passoni, P.; Reni, M.; Cattaneo, G.M.; Slim, N.; Cereda, S.; Balzano, G.; Castoldi, R.; Longobardi, B.; Bettinardi, V.; Gianolli, L.; et al. Hypofractionated image-guided IMRT in advanced pancreatic cancer with simultaneous integrated boost to infiltrated vessels concomitant with capecitabine: A phase I study. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 1000–1006. [Google Scholar] [CrossRef]
- Murphy, J.E.; Wo, J.Y.; Ryan, D.P.; Jiang, W.; Yeap, B.Y.; Drapek, L.C.; Blaszkowsky, L.S.; Kwak, E.L.; Allen, J.N.; Clark, J.W.; et al. Total Neoadjuvant Therapy with FOLFIRINOX Followed by Individualized Chemoradiotherapy for Borderline Resectable Pancreatic Adenocarcinoma: A Phase 2 Clinical Trial. JAMA Oncol. 2018, 4, 963–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, J.E.; Wo, J.Y.; Ryan, D.P.; Clark, J.W.; Jiang, W.; Yeap, B.Y.; Drapek, L.C.; Ly, L.; Baglini, C.V.; Blaszkowsky, L.S.; et al. Total Neoadjuvant Therapy with FOLFIRINOX in Combination with Losartan Followed by Chemoradiotherapy for Locally Advanced Pancreatic Cancer: A Phase 2 Clinical Trial. JAMA Oncol. 2019, 5, 1020–1027. [Google Scholar] [CrossRef]
- Koay, E.J.; Hanania, A.N.; Hall, W.A.; Taniguchi, C.M.; Rebueno, N.; Myrehaug, S.; Aitken, K.L.; Dawson, L.A.; Crane, C.H.; Herman, J.M.; et al. Dose-Escalated Radiation Therapy for Pancreatic Cancer: A Simultaneous Integrated Boost Approach. Pract. Radiat. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Brunner, T.B.; Nestle, U.; Adebahr, S.; Gkika, E.; Wiehle, R.; Baltas, D.; Grosu, A.L. Simultaneous integrated protection: A new concept for high-precision radiation therapy. Strahlenther. Onkol. 2016, 192, 886–894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, C.E.; Hingorani, S.R.; Mick, R.; Combs, C.; Tuveson, D.A.; Vonderheide, R.H. Dynamics of the immune reaction to pancreatic cancer from inception to invasion. Cancer Res. 2007, 67, 9518–9527. [Google Scholar] [CrossRef] [Green Version]
- Hruban, R.H.; Klimstra, D.S. Adenocarcinoma of the pancreas. Semin. Diagn. Pathol. 2014, 31, 443–451. [Google Scholar] [CrossRef] [Green Version]
- Fukunaga, A.; Miyamoto, M.; Cho, Y.; Murakami, S.; Kawarada, Y.; Oshikiri, T.; Kato, K.; Kurokawa, T.; Suzuoki, M.; Nakakubo, Y.; et al. CD8+ tumor-infiltrating lymphocytes together with CD4+ tumor-infiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas 2004, 28, e26–e31. [Google Scholar] [CrossRef] [PubMed]
- Vonderheide, R.H.; Bayne, L.J. Inflammatory networks and immune surveillance of pancreatic carcinoma. Curr. Opin. Immunol. 2013, 25, 200–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feig, C.; Jones, J.O.; Kraman, M.; Wells, R.J.; Deonarine, A.; Chan, D.S.; Connell, C.M.; Roberts, E.W.; Zhao, Q.; Caballero, O.L.; et al. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc. Natl. Acad. Sci. USA 2013, 110, 20212–20217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, E.; El-Rayes, B. Pancreatic Cancer and Immunotherapy: Resistance Mechanisms and Proposed Solutions. J. Gastrointest. Cancer 2019, 50, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Barker, H.E.; Paget, J.T.; Khan, A.A.; Harrington, K.J. The tumour microenvironment after radiotherapy: Mechanisms of resistance and recurrence. Nat. Rev. Cancer 2015, 15, 409–425. [Google Scholar] [CrossRef]
- Burnette, B.; Weichselbaum, R.R. Radiation as an immune modulator. Semin. Radiat. Oncol. 2013, 23, 273–280. [Google Scholar] [CrossRef]
- Rech, A.J.; Dada, H.; Kotzin, J.J.; Henao-Mejia, J.; Minn, A.J.; Twyman-Saint Victor, C.; Vonderheide, R.H. Radiotherapy and CD40 Activation Separately Augment Immunity to Checkpoint Blockade in Cancer. Cancer Res. 2018, 78, 4282–4291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, W.; Skowron, K.B.; Namm, J.P.; Burnette, B.; Fernandez, C.; Arina, A.; Liang, H.; Spiotto, M.T.; Posner, M.C.; Fu, Y.X.; et al. Combination of radiotherapy and vaccination overcomes checkpoint blockade resistance. Oncotarget 2016, 7, 43039–43051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azad, A.; Yin Lim, S.; D’Costa, Z.; Jones, K.; Diana, A.; Sansom, O.J.; Kruger, P.; Liu, S.; McKenna, W.G.; Dushek, O.; et al. PD-L1 blockade enhances response of pancreatic ductal adenocarcinoma to radiotherapy. EMBO Mol. Med. 2017, 9, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Sharabi, A.B.; Lim, M.; DeWeese, T.L.; Drake, C.G. Radiation and checkpoint blockade immunotherapy: Radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 2015, 16, e498–e509. [Google Scholar] [CrossRef]

| Guideline/Year | International/National (State) | Main Option | Alternative |
|---|---|---|---|
| NCCN 2020 [3] | International |
|
|
| ESMO 2015 [21,41] | International |
| - |
| PDQ® 2020 [32] | International |
|
|
| ASCO Khoarana 2019 [29] | International |
|
|
| ASTRO 2019 [31] | International |
|
|
| Hidalgo 2017 [33] | National (Spain) |
|
|
| Neuzillet 2018 [34] | National (French) |
|
|
| O’Reilly 2018 [35] | National (UK) |
|
|
| Seufferlein 2014 - (S3 Guideline) [36] | National (German) |
|
|
| Yamaguchi 2017 [37] | National (Japan) |
|
|
| AIOM 2019 [39] | National (Italian) |
|
|
| Hyde 2019 [38] | National (Eastern Canada) Consensus Conference |
|
|
| Guideline/Year | International/National (State) | Main Option | Alternative |
|---|---|---|---|
| NCCN 2020 [3] | International |
|
|
| ESMO 2015 [28,42] | International |
|
|
| PDQ® 2020 [32] | International |
|
|
| ASCO Balaban 2017 [30] | International |
|
|
| ASTRO 2019 [31] | International |
| - |
| Hidalgo 2017 [33] | National (Spain) |
| For pt candidates for CT with limitations:
|
| Neuzillet 2018 [34] | National (French) |
|
|
| O’Reilly 2018 [35] | National (UK) |
|
|
| Seufferlein 2014 - (S3 Guideline) [36] | National (German) |
|
|
| Yamaguchi 2017 [37] | National (Japan) |
|
|
| AIOM 2019 [39] | National (Italian) |
|
|
| Hyde 2019 [38] | National (Eastern Canada) Consensus Conference |
|
|
| van Veldhuisen 2019 [40] | National (Dutch) |
|
|
| Guideline/Year | International/National (State) | Main Option | Alternative |
|---|---|---|---|
| NCCN 2020 [3] | International |
Neoadjuvant Therapy Includes:
|
|
| ESMO Ducreux 2015 [28,42] | International |
| - |
| PDQ® 2020 [32] | International |
|
|
| ASCO [29] | International | Not expressly specified: see “resectable” | - |
| ASTRO 2019 [31] | International | Conditional recommendation for:
| - |
| Hidalgo 2017 [33] | National (Spain) |
Includes:
| - |
| Neuzillet 2018 [34] | National (French) |
| - |
| O’Reilly 2018 [35] | National (UK) |
| - |
| Seufferlein 2014 -(S3 Guideline) [36] | National (German) | Not specifically addressed | - |
| Yamaguchi 2017 [37] | National (Japan) |
| - |
| AIOM 2019 [39] | National (Italian) |
|
|
| Hyde 2019 [38] | National (Eastern Canada) Consensus Conference |
Includes
|
|
| Author, Year | Enrolment Period | Study Design | Study Sample | N° BRPC | N° LAPC | % of Patients Treated with Total Dose (Gy) and Fractionation (N°) | Technique | Pre-SBRT CT (%) | Total Median OS (Months) | BRPC Median OS (Months) | LAPC Median OS (Months) | Total Resectios (%) | BRPC Resection (%) | LAPC Resection (%) | Total R0 Resections (%) | BRPC R0 Resection (%) | LAPC R0 Resection (%) | Late GI Toxicity Grade (G): (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arcelli, 2020 [136] | 2013-2018 | Retr | 56 | 56 | 18–45/3–5 | VMAT IMRT RS 3-D | 55.3 | 19.0 | G ≥3: 2.5 | |||||||||
| Kharofa, 2019 [122] | 2014–2017 | Ph II | 18 | 15 | 44%: 33/5 56%: 33/5 + 25/5 (SIB) | mFolfirinox: 100.0 | 21.0 | 67.0 | 92.0 | G ≥3: 0 | ||||||||
| Jung, 2019 [137] | 2011–2016 | Retr | 95 | 95 | 24–36/4 | VMAT IMRT | Gem-based: 10.0 Folfirinox: 3.2 | 16.7 | 7.4 | 3.2 | G ≥3: 3.2 | |||||||
| Chapman, 2018 [138] | 2012–2016 | Retr | 75 | 53 | 22 | 24–40/NR | Folfirinox: 64.0 Gem-based:34.7 Other: 1.3 | 23.5 | 19.7 | 81.6 | 7.0 | |||||||
| Ryan, 2018 [139] | 2010–2016 | Retr | 29 | 25–33/5 | 13.0 | G ≥3: 4 | ||||||||||||
| Mellon, 2015 [78] | 2009–2014 | Retr | 159 | 110 | 49 | 28–30/5 | IMRT | Gem: 86.0 Folfirinox: 14.0 | 18.1 | 19.2 | 15.0 | 38.0 | 51.0 | 14.0 | 38.3 | 96.0 | 10.0 | G ≥3: 7 |
| Shaib, 2016 [121] | 2011–2015 | Ph I | 13 | 12 | 25%: 30/3 + 6/3 (SIB) 25%: 36/3 + 6/3 (SIB) 25%: 36/3 + 7.5/3 (SIB) 25%: 36/3 + 9/3 (SIB) | VMAT (SIB) | mFolfirinox: 100.0 | 11.0 | 66.6 | 66.6 | G ≥3: 0 | |||||||
| Moningi, 2015 [119] | 2010–2014 | Retr | 88 | 14 | 74 | 25–33/5 | NR | 88.0 | 18.4 | 18.4 | 14.4 | 21.6 | 28.5 | 20.2 | 84.0 | G ≥3: 1.1 | ||
| Herman, 2015 [135] | 2010–2012 | Ph II | 49 | 49 | 33/5 | VMAT-IMRT | Gem: 90.0 | 13.9 | 8.0 | 8.0 | G ≥2: 11 | |||||||
| Song, 2015 [129] | 2006–2014 | Retr | 59 | 59 | 35–50/3–5–8 | RS | 12.5 | G ≥3: 2 | ||||||||||
| Pollom, 2014 [120] | 2002–2013 | Retr | 167 | 11 | 133 | 45%: 25/1 55%: 25–45/>1 | VMAT | 87.5 | ||||||||||
| Tozzi, 2013 [130] | 2010–2011 | Retr | 30 | 21 | 83%: 45/6 17%: 36/6 | VMAT | 30.0 | 11.0 | G ≥3: 0 | |||||||||
| Rajagopalan, 2013 [118] | 2008–2011 | Retr | 12 | 7 | 5 | 58%: 36/3 42%: 24/1 | RS | 91.7 | 47.2 | 91.7 | G ≥3: 0 | |||||||
| Gurka, 2013 [100] | 2009–2011 | Ph I | 10 | 10 | 25/5 | RS | Gem: 100.0 | 12.2 | G ≥3: 0 | |||||||||
| Boone, 2013 [117] | 2011–2012 | Retr | 9 | 4 | 5 | 36/3 | RS | 100.0 | 75.0 | 20.0 | 50.0 | |||||||
| Goyal, 2012 [131] | 2007–2010 | Retr | 19 | 19 | 74%: 20–25/1 26%: 24–30/3 | RS | 68.0 | 14.3 | G ≥3: 16 | |||||||||
| Schellenberg, 2011 [128] | 2006–2007 | Ph II | 20 | 20 | 25/1 | IMRT | Gem: 100 | 11.8 | G ≥3: 5 | |||||||||
| Polistina, 2010 [132] | 2004–2007 | Ph II | 23 | 23 | 30/3 | RS | Gem: 100 | 10.6 | 8.0 | G ≥3: 0 | ||||||||
| Rwigema, 2011 [133] | 2004–2009 | Retr | 71 | 40 | 18–25/1–3 | RS | 10.3 | 6.2 | G ≥3: 0 | |||||||||
| Mahadevan, 2011 [134] | 2007–2010 | Retr | 47 | 39 | 71.7%: 24/3 28.3%: 30/3 | RS | Gem: 100 | 20.0 | G ≥3: 9 | |||||||||
| Schellenberg, 2008 [128] | 2004–2006 | Ph II | 16 | 16 | 25/1 | RS | Gem: 100 | 11.4 | G ≥3: 12.5 | |||||||||
| Koong, 2004 [127] | 2001–2006 | Retr | 15 | 15 | 20.0%: 15/1 33.3%: 20/1 46.7%: 25/1 | RS | 11.0 | G ≥3: 0 |
| Study, Year [ref] | Study Type | Tumor Stage | Fractions (n) Tumor Target Definition | Tumor Target Dose (Gy) | SIB Target | SIB Dose (Gy) | Study Primary Endpoint | Late Toxicity G ≥ 3 | |
|---|---|---|---|---|---|---|---|---|---|
| Chuong, 2013 [147] | Retrospective | BRPC/LAPC | 5 | PTV = entire tumor + 3–5 mm | 25 | TVI (region of vessel abutment/encasement) | 35 | OS (m): 16.4/15 PFS (m): 9.7/9.8 BRPC/LAPC | 5.3% |
| Passoni, 2013 [148] | Phase II | LAPC | 15 | PTV = ITV (tumor and enlarged lymph nodes plus motion) + BTV + 5/7 mm | 44.25 | Infiltrating vessel + 1 cm within GTV | 48-58 | DLT: not reached | 0% |
| Mellon, 2015 [78] | Retrospective | BRPC/LAPC | 5 | PTV = GTV (plus motion) + 3–5 mm | 30 | TVI (areas of vessel involvement by tumor) | 40 | OS (m): 19.2/15 LCR: 78% * | 7% |
| Krishnan, 2016 [8] | Retrospective | LAPC | 28 15 | PTV = GTV + 15 mm | 50.4 37.5 | GTV + 2–5 mm | 63–70 67.5 | OS (m): 17.8 PFS (m): 10.2 | No additional compared to SDR |
| Shaib, 2016 [121] | Phase I | LAPC | 3 | PTV = GTV with at-risk area of microscopic spread + 5 mm | 12 | PM = volume between the posterior 1 cm of GTV and mesenteric vessel/retroperitoneal soft tissue | 15 | DLT: not reached | 0% |
| Murphy, 2018 [149] | Phase II | BRPC | 28 | PTV = CTV (GTV + 1 cm margin and elective nodal coverage) + 7 mm | 50.4 | TVI (tumor involvement of critical blood vessels) | 58.8 | R0 resection rate: 97% | 0% |
| Murphy, 2019 [150] | Phase II | LAPC | 28 | PTV = CTV (GTV + 1 cm margin and elective nodal coverage) + 7 mm | 50.4 | TVI (tumor involvement of critical blood vessels) | 58.8 | R0 resection rate: 81% | 0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cellini, F.; Arcelli, A.; Simoni, N.; Caravatta, L.; Buwenge, M.; Calabrese, A.; Brunetti, O.; Genovesi, D.; Mazzarotto, R.; Deodato, F.; et al. Basics and Frontiers on Pancreatic Cancer for Radiation Oncology: Target Delineation, SBRT, SIB Technique, MRgRT, Particle Therapy, Immunotherapy and Clinical Guidelines. Cancers 2020, 12, 1729. https://doi.org/10.3390/cancers12071729
Cellini F, Arcelli A, Simoni N, Caravatta L, Buwenge M, Calabrese A, Brunetti O, Genovesi D, Mazzarotto R, Deodato F, et al. Basics and Frontiers on Pancreatic Cancer for Radiation Oncology: Target Delineation, SBRT, SIB Technique, MRgRT, Particle Therapy, Immunotherapy and Clinical Guidelines. Cancers. 2020; 12(7):1729. https://doi.org/10.3390/cancers12071729
Chicago/Turabian StyleCellini, Francesco, Alessandra Arcelli, Nicola Simoni, Luciana Caravatta, Milly Buwenge, Angela Calabrese, Oronzo Brunetti, Domenico Genovesi, Renzo Mazzarotto, Francesco Deodato, and et al. 2020. "Basics and Frontiers on Pancreatic Cancer for Radiation Oncology: Target Delineation, SBRT, SIB Technique, MRgRT, Particle Therapy, Immunotherapy and Clinical Guidelines" Cancers 12, no. 7: 1729. https://doi.org/10.3390/cancers12071729
APA StyleCellini, F., Arcelli, A., Simoni, N., Caravatta, L., Buwenge, M., Calabrese, A., Brunetti, O., Genovesi, D., Mazzarotto, R., Deodato, F., Mattiucci, G. C., Silvestris, N., Valentini, V., & Morganti, A. G. (2020). Basics and Frontiers on Pancreatic Cancer for Radiation Oncology: Target Delineation, SBRT, SIB Technique, MRgRT, Particle Therapy, Immunotherapy and Clinical Guidelines. Cancers, 12(7), 1729. https://doi.org/10.3390/cancers12071729











