Donor-Site Morbidity after Fibula Transplantation in Head and Neck Tumor Patients: A Split-Leg Retrospective Study with Focus on Leg Stability and Quality of Life
Abstract
:1. Introduction
- How is the ankle function and thus the balance and stability of a leg restricted by the removal of a fibular graft?
- How much does the aforementioned restriction affect daily activities and quality of life?
2. Results
2.1. Basic Data
Height, Weight and Body Mass Index (BMI)
2.2. Surgical Information
2.2.1. Indications and Localization of Defects
2.2.2. Donor-Site, Type of Fibula Transplantation, and Wound Closure
- osseomyocutan graft (bone, muscle tissue, and skin island);
- osseomuscular graft (bone and muscle tissue); and,
- prefabricated fibula graft (bone covered with pre-transplanted skin graft and already inserted dental implants) (Table 1).
2.2.3. Inpatient Stay
2.3. Follow-Up Examination
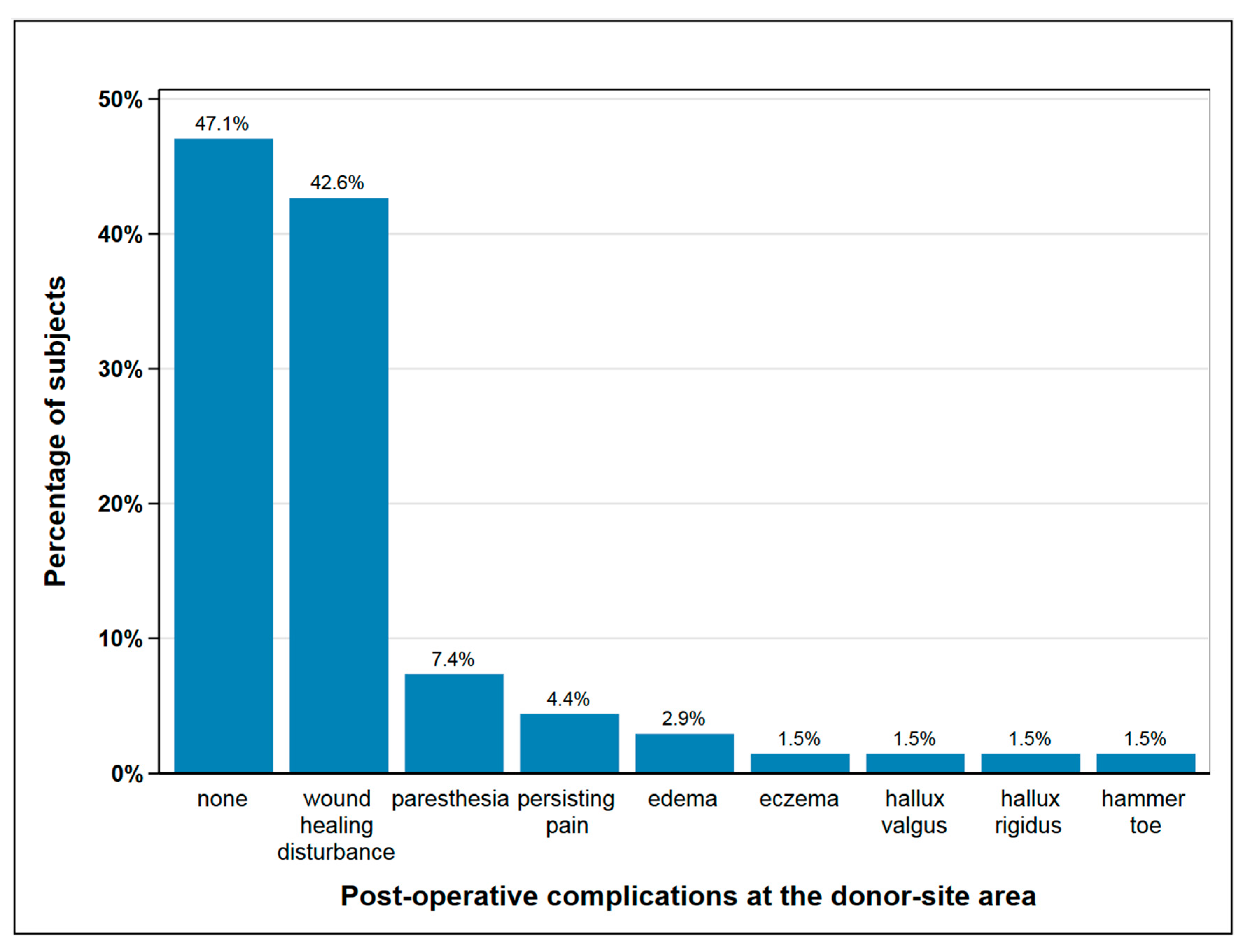
2.3.1. Complications at the Donor-Site
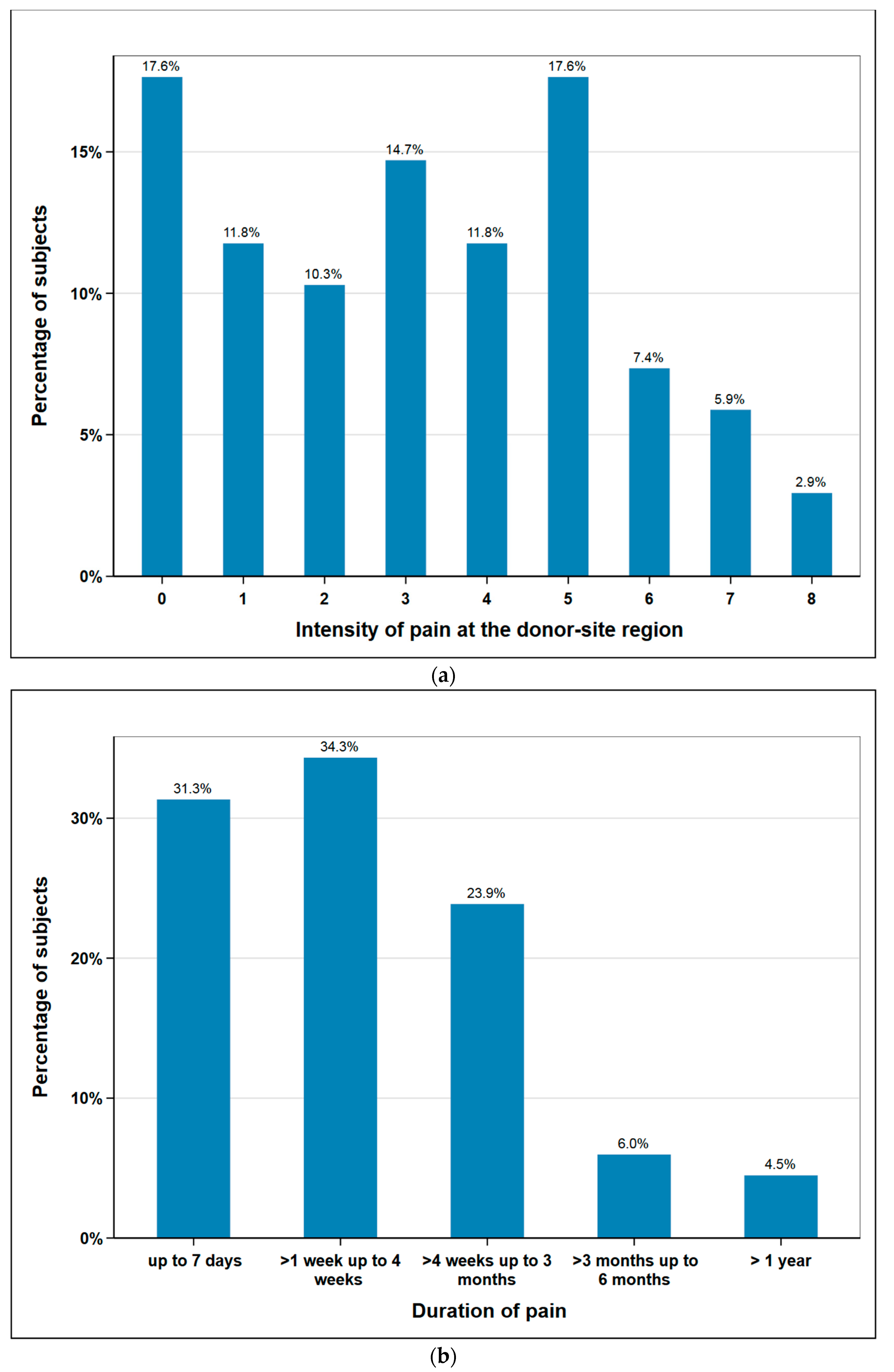
2.3.2. Post-Operative Pain
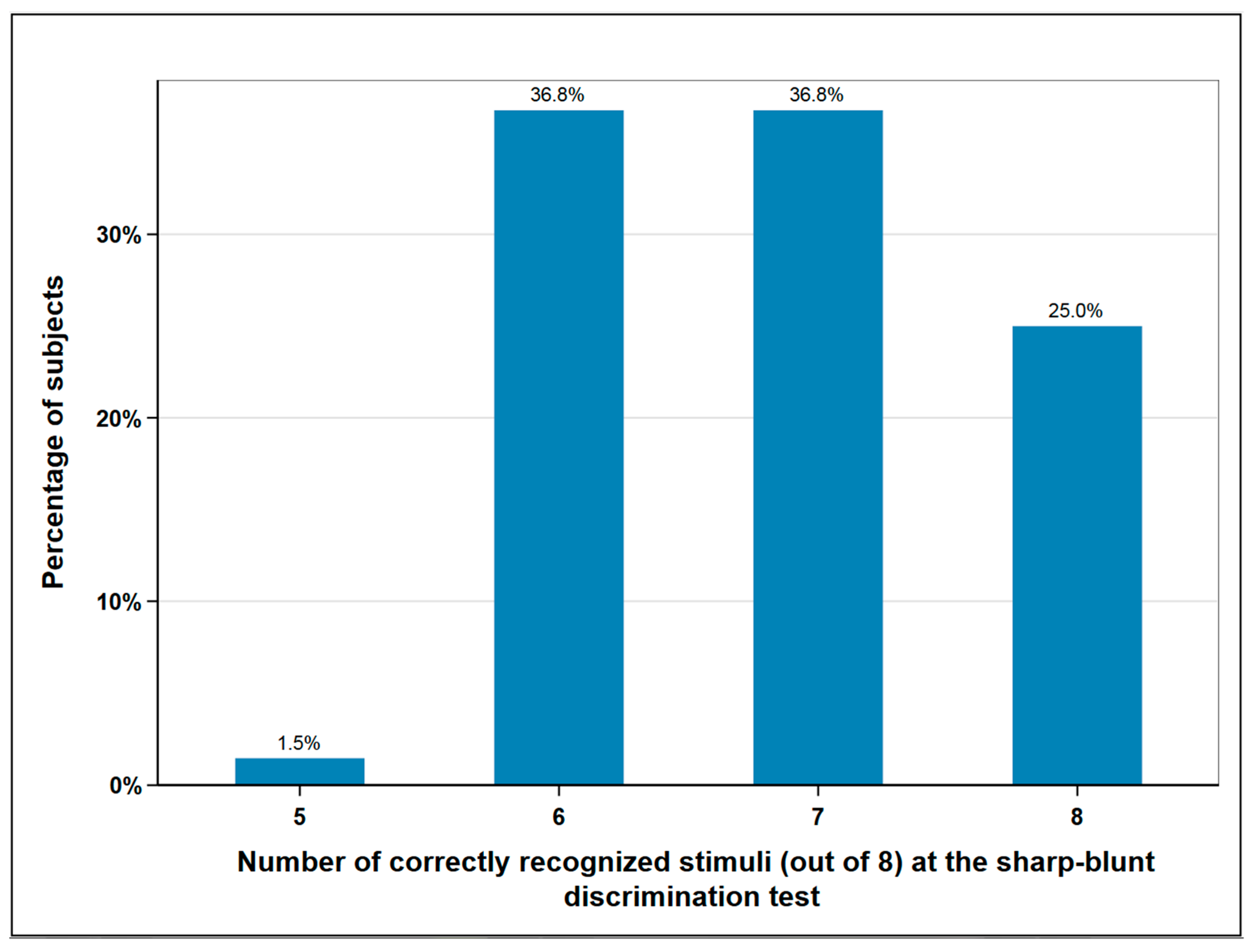
2.3.3. Fibular Nerve Function and Sensitivity Disorder
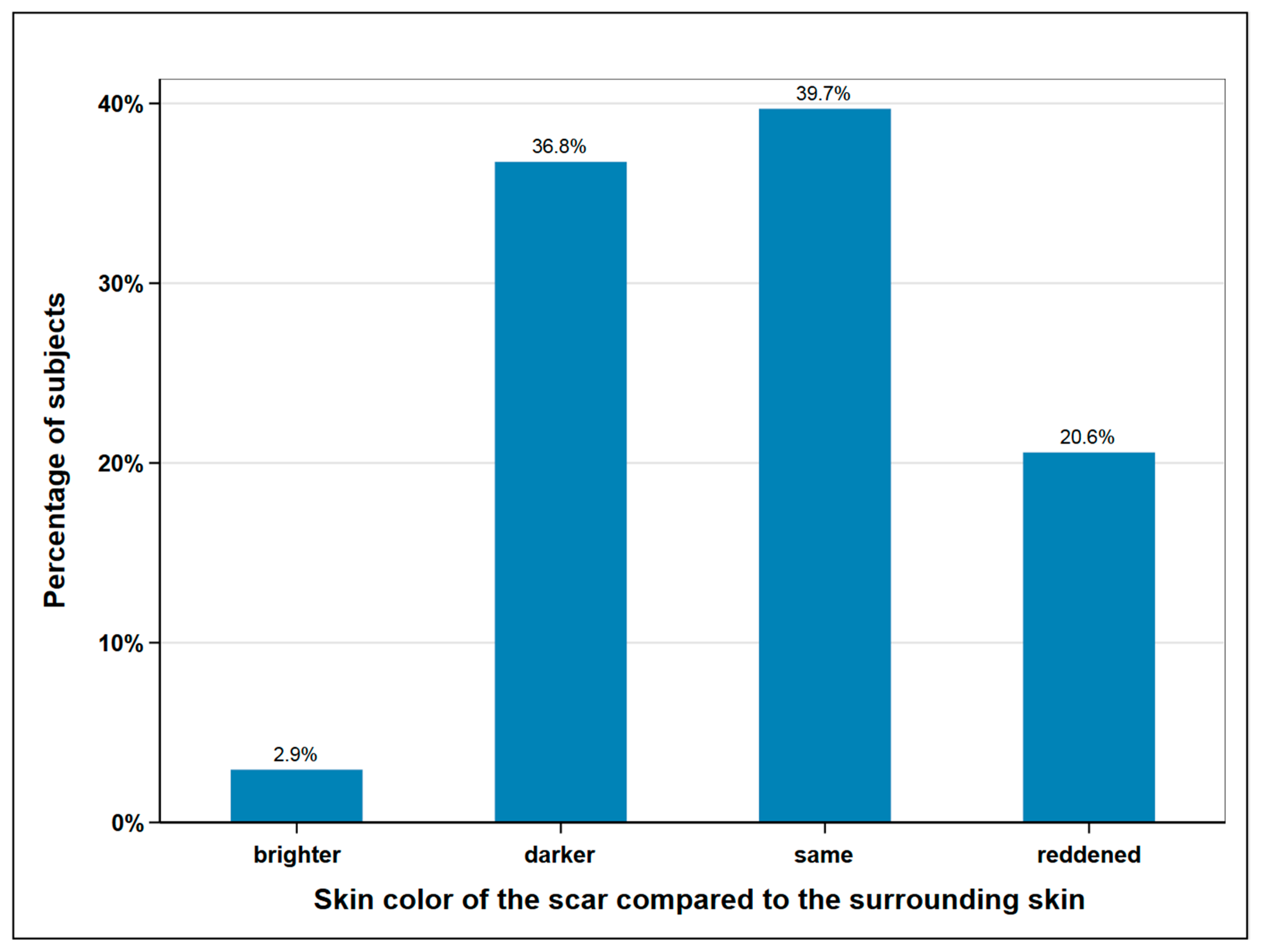
2.3.4. Scar
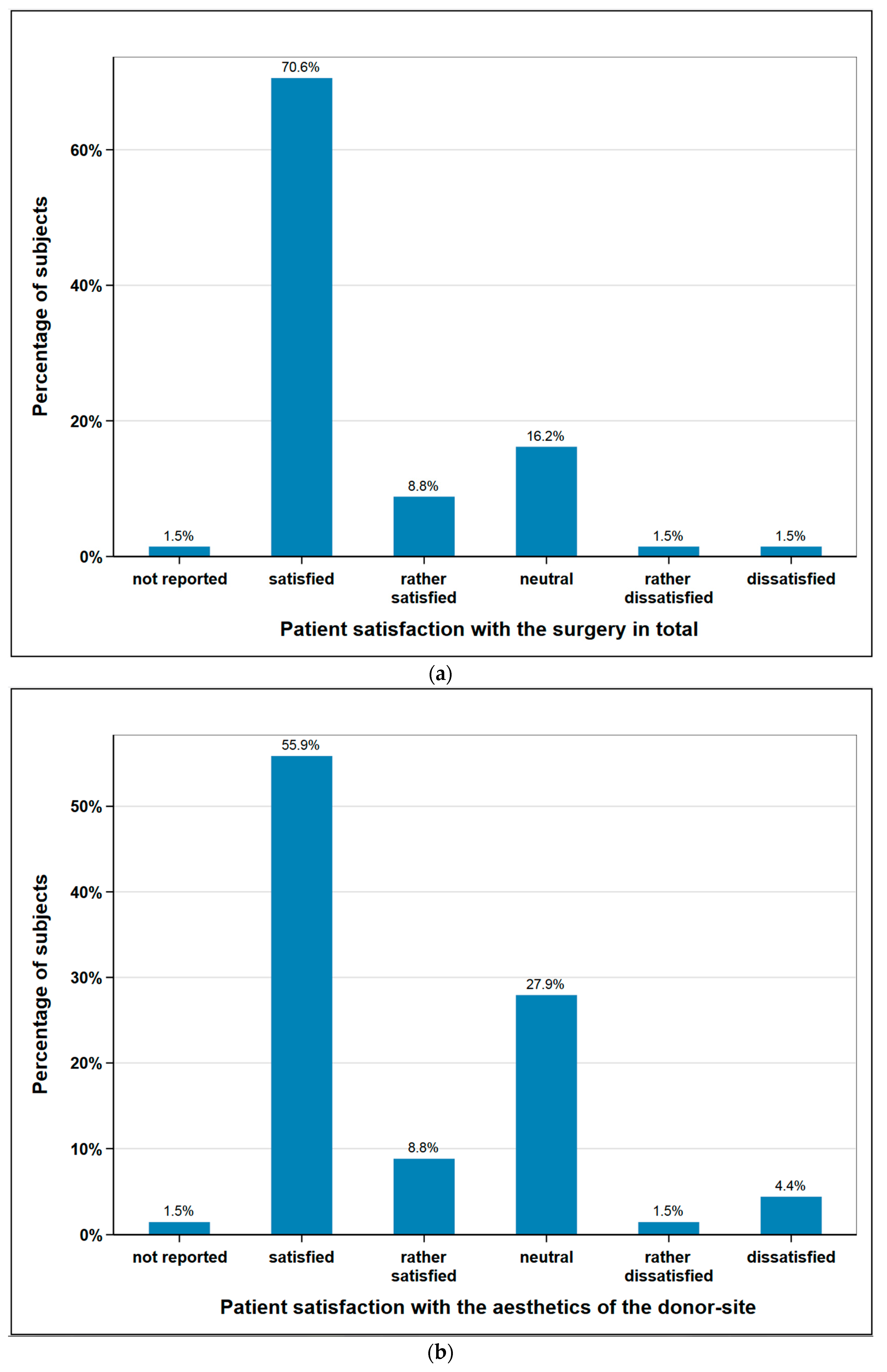
2.3.5. Level of Patient Satisfaction
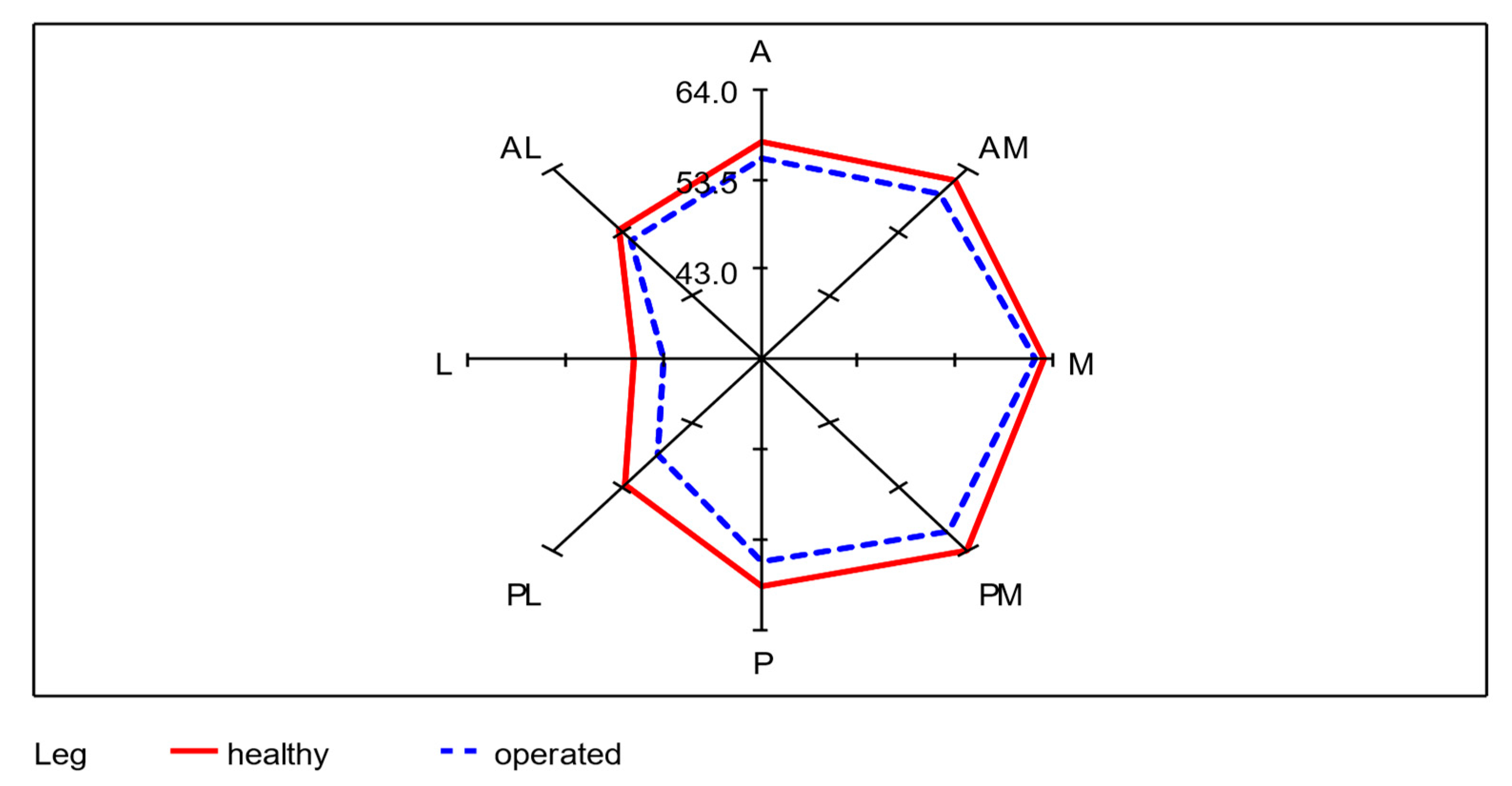
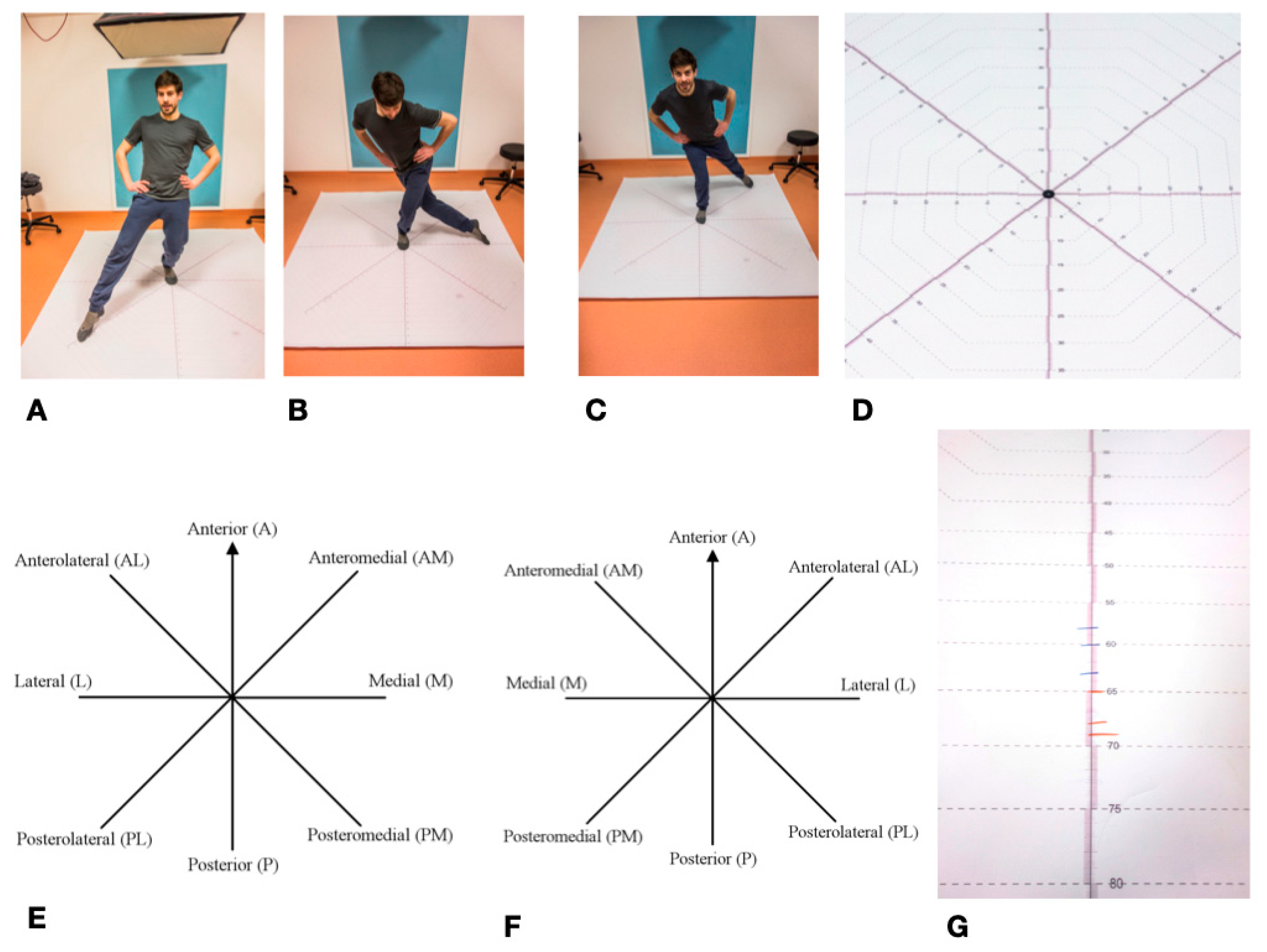
2.4. Star Excursion Balance Test—SEBT
2.5. Foot and Ankle Disability Index—FADI
3. Discussion
3.1. Evaluation of Material and Methods
3.2. Discussion of the Results
3.2.1. Subjects Collective and Surgical Procedures
3.2.2. Surgical Complications
3.2.3. SEBT und FADI
3.3. Limitations of This Study
4. Materials and Methods
4.1. Study Design and Examiner Blinding and Calibration
4.2. Patient Inclusion and Exclusion Criteria
4.3. Study Parameters
4.4. Star Excursion Balance Test—SEBT
4.5. Foot and Ankle Disability Index—FADI
4.6. Ethics, Privacy and Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Akashi, M.; Hashikawa, K.; Takasu, H.; Watanabe, K.; Kusumoto, J.; Sakakibara, A.; Hasegawa, T.; Minamikawa, T.; Komori, T. Comparison between primary closure and skin grafts of the free fibula osteocutaneous flap donor site. Oral Maxillofac. Surg. 2016, 20, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Ferri, J.; Piot, B.; Ruhin, B.; Mercier, J. Advantages and limitations of the fibula free flap in mandibular reconstruction. J. Oral Maxillofac. Surg. 1997, 55, 440–448. [Google Scholar] [CrossRef]
- Attia, S.; Wiltfang, J.; Pons-Kuhnemann, J.; Wilbrand, J.F.; Streckbein, P.; Kahling, C.; Howaldt, H.P.; Schaaf, H. Survival of dental implants placed in vascularised fibula free flaps after jaw reconstruction. J. Cranio-Maxillofac. Surg. 2018, 46, 1205–1210. [Google Scholar] [CrossRef] [PubMed]
- Attia, S.; Wiltfang, J.; Streckbein, P.; Wilbrand, J.F.; El Khassawna, T.; Mausbach, K.; Howaldt, H.P.; Schaaf, H. Functional and aesthetic treatment outcomes after immediate jaw reconstruction using a fibula flap and dental implants. J. Cranio-Maxillofac. Surg. 2019, 47, 786–791. [Google Scholar] [CrossRef]
- Gelband, H.; Jha, P.; Sankaranarayanan, R.; Horton, S. Summary--Cancer: Disease Control Priorities; World Bank Group: Washington, DC, USA, 2015; Volume 3. [Google Scholar]
- Alvi, A. Oral cancer: How to recognize the danger signs. Postgrad. Med. 1996, 99, 149–156. [Google Scholar] [CrossRef]
- Hemprich, A.; Müller, R.-P. Long-term results in treating squamous cell carcinoma of the lip, oral cavity, and oropharynx. Int. J. Oral Maxillofac. Surg. 1989, 18, 39–42. [Google Scholar] [CrossRef]
- Gooi, Z.; Chan, J.Y.; Fakhry, C. The epidemiology of the human papillomavirus related to oropharyngeal head and neck cancer. Laryngoscope 2016, 126, 894–900. [Google Scholar] [CrossRef]
- Jabaley, M.E. Reconstruction in patients with oral and pharyngeal cancer. Curr. Probl. Surg. 1977, 14, 1–65. [Google Scholar] [CrossRef]
- Chiapasco, M.; Biglioli, F.; Autelitano, L.; Romeo, E.; Brusati, R. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin. Oral Implant. Res. 2006, 17, 220–228. [Google Scholar] [CrossRef]
- Schusterman, M.A.; Harris, S.W.; Raymond, A.K.; Goepfert, H. Immediate free flap mandibular reconstruction: Significance of adequate surgical margins. Head Neck 1993, 15, 204–207. [Google Scholar] [CrossRef]
- Chana, J.S.; Chang, Y.-M.; Wei, F.-C.; Shen, Y.-F.; Chan, C.-P.; Lin, H.-N.; Tsai, C.-Y.; Jeng, S.-F. Segmental mandibulectomy and immediate free fibula osteoseptocutaneous flap reconstruction with endosteal implants: An ideal treatment method for mandibular ameloblastoma. Plast. Reconstr. Surg. 2004, 113, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Schaaf, H.; Wahab-Göthe, T.; Kerkmann, H.; Streckbein, P.; Obert, M.; Pons-Kuehnemann, J.; Ahrens, M.; Howaldt, H.-P.; Attia, S. Comparison between flat-panel volume computed tomography and histologic assessments of bone invasion of maxillofacial tumors: Utility of an instantaneous radiologic diagnostic tool. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Häfliger, J.; Seto, I.; Rahal, A.; Mericske-Stern, R.; Smolka, K. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants: Factors affecting the functional outcome in patients with oral cancer. Clin. Oral Implant. Res. 2005, 16, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Sieg, P.; Hasse, A.; Zimmermann, C.E. Versatility of vascularized fibula and soft tissue graft in the reconstruction of the mandibulofacial region. Int. J. Oral Maxillofac. Surg. 1999, 28, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.; Miller, G.; Ham, F.J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast. Reconstr. Surg. 1975, 55, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.W.; Yan, W. The study and clinical application of the osteocutaneous flap of fibula. Microsurgery 1983, 4, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Fibula free flap: A new method of mandible reconstruction. Plast. Reconstr. Surg. 1989, 84, 71–79. [Google Scholar] [CrossRef]
- Kniha, K.; Möhlhenrich, S.C.; Foldenauer, A.C.; Peters, F.; Ayoub, N.; Goloborodko, E.; Hölzle, F.; Modabber, A. Evaluation of bone resorption in fibula and deep circumflex iliac artery flaps following dental implantation: A three-year follow-up study. J. Cranio-Maxillofac. Surg. 2017, 45, 474–478. [Google Scholar] [CrossRef]
- Wolff, K.-D.; Ervens, J.; Herzog, K.; Hoffmeister, B. Experience with the osteocutaneous fibula flap: An analysis of 24 consecutive reconstructions of composite mandibular defects. J. Cranio-Maxillofac. Surg. 1996, 24, 330–338. [Google Scholar] [CrossRef]
- Jones, N.F.; Swartz, W.M.; Mears, D.C.; Jupiter, J.B.; Grossman, A. The “double barrel” free vascularized fibular bone graft. Plast. Reconstr. Surg. 1988, 81, 378–385. [Google Scholar] [CrossRef]
- Beppu, M.; Hanel, D.P.; Johnston, G.H.; Carmo, J.M.; Tsai, T.-M. The osteocutaneous fibula flap: An anatomic study. J. Reconstr. Microsurg. 1992, 8, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Ling, X.F.; Peng, X. What is the price to pay for a free fibula flap? A systematic review of donor-site morbidity following free fibula flap surgery. Plast. Reconstr. Surg. 2012, 129, 657–674. [Google Scholar] [CrossRef] [PubMed]
- Kearns, M.; Ermogenous, P.; Myers, S.; Ghanem, A.M. Osteocutaneous flaps for head and neck reconstruction: A focused evaluation of donor site morbidity and patient reported outcome measures in different reconstruction options. Arch. Plast. Surg. 2018, 45, 495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodacre, T.; Walker, C.; Jawad, A.; Jackson, A.; Brough, M. Donor site morbidity following osteocutaneous free fibula transfer. Br. J. Plast. Surg. 1990, 43, 410–412. [Google Scholar] [CrossRef]
- Rendenbach, C.; Kohlmeier, C.; Suling, A.; Assaf, A.T.; Catala-Lehnen, P.; Amling, M.; Heiland, M.; Riecke, B. Prospective biomechanical analysis of donor-site morbidity after fibula free flap. J. Cranio-Maxillofac. Surg. 2016, 44, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Momoh, A.O.; Yu, P.; Skoracki, R.J.; Liu, S.; Feng, L.; Hanasono, M.M. A prospective cohort study of fibula free flap donor-site morbidity in 157 consecutive patients. Plast. Reconstr. Surg. 2011, 128, 714–720. [Google Scholar] [CrossRef]
- Durst, A.; Clibbon, J.; Davis, B. Distal tibial fractures are a poorly recognised complication with fibula free flaps. Ann. R. Coll. Surg. Engl. 2015, 97, 409–413. [Google Scholar] [CrossRef] [Green Version]
- Feuvrier, D.; Sagawa, Y., Jr.; Béliard, S.; Pauchot, J.; Decavel, P. Long-term donor-site morbidity after vascularized free fibula flap harvesting: Clinical and gait analysis. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 262–269. [Google Scholar] [CrossRef]
- Zimmermann, C.; Börner, B.-I.; Hasse, A.; Sieg, P. Donor site morbidity after microvascular fibula transfer. Clin. Oral Investig. 2001, 5, 214–219. [Google Scholar] [CrossRef]
- Sieg, P.; Taner, C.; Hakim, S.G.; Jacobsen, H.-C. Long-term evaluation of donor site morbidity after free fibula transfer. Br. J. Oral Maxillofac. Surg. 2010, 48, 267–270. [Google Scholar] [CrossRef]
- Liu, T.-Y.; Huang, Y.-C.; Leong, C.-P.; Tseng, C.-Y.; Kuo, Y.-R. Home-based exercise on functional outcome of the donor lower extremity in oral cancer patients after fibula flap harvest. Biomed. J. 2013, 36. [Google Scholar]
- Lee, J.-H.; Chung, C.-Y.; Myoung, H.; Kim, M.-J.; Yun, P.-Y. Gait analysis of donor leg after free fibular flap transfer. Int. J. Oral Maxillofac. Surg. 2008, 37, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.; Peehal, J.; Shah, A.; Crank, S.; Flora, H. Star excursion balance test for assessment of dynamic instability of the ankle in patients after harvest of a fibular free flap: A two-centre study. Br. J. Oral Maxillofac. Surg. 2017, 55, 256–259. [Google Scholar] [CrossRef] [PubMed]
- Hale, S.A.; Hertel, J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J. Athl. Train. 2005, 40, 35. [Google Scholar] [PubMed]
- Olmsted, L.C.; Carcia, C.R.; Hertel, J.; Shultz, S.J. Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J. Athl. Train. 2002, 37, 501. [Google Scholar] [PubMed]
- Ganesh, G.S.; Chhabra, D.; Mrityunjay, K. Efficacy of the star excursion balance test in detecting reach deficits in subjects with chronic low back pain. Physiother. Res. Int. 2015, 20, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Di Giuli, R.; Zago, M.; Beltramini, G.A.; Pallotta, M.L.; Bolzoni, A.; Baj, A.; Giannì, A.B.; Sforza, C. Donor-site morbidity after osteocutaneous free fibula transfer: Longitudinal analysis of gait performance. J. Oral Maxillofac. Surg. 2019, 77, 648–657. [Google Scholar] [CrossRef] [Green Version]
- Schardt, C.; Schmid, A.; Bodem, J.; Krisam, J.; Hoffmann, J.; Mertens, C. Donor site morbidity and quality of life after microvascular head and neck reconstruction with free fibula and deep-circumflex iliac artery flaps. J. Cranio-Maxillofac. Surg. 2017, 45, 304–311. [Google Scholar] [CrossRef]
- Shindo, M.; Fong, B.P.; Funk, G.F.; Karnell, L.H. The fibula osteocutaneous flap in head and neck reconstruction: A critical evaluation of donor site morbidity. Arch. Otolaryngol.–Head Neck Surg. 2000, 126, 1467–1472. [Google Scholar] [CrossRef] [Green Version]
- Hölzle, F.; Kesting, M.; Hölzle, G.; Watola, A.; Loeffelbein, D.; Ervens, J.; Wolff, K.-D. Clinical outcome and patient satisfaction after mandibular reconstruction with free fibula flaps. Int. J. Oral Maxillofac. Surg. 2007, 36, 802–806. [Google Scholar] [CrossRef]
- González-García, R.; Naval-Gías, L.; Rodríguez-Campo, F.J.; Román-Romero, L. Reconstruction of oromandibular defects by vascularized free flaps: The radial forearm free flap and fibular free flap as major donor sites. J. Oral Maxillofac. Surg. 2009, 67, 1473–1477. [Google Scholar] [CrossRef]
- Wolff, K.D.; Hölzle, F.; Kolk, A.; Hohlweg-Majert, B.; Steiner, T.; Kesting, M.R. Raising the osteocutaneous fibular flap for oral reconstruction with reduced tissue alteration. J. Oral Maxillofac. Surg. 2011, 69, e260–e267. [Google Scholar] [CrossRef] [PubMed]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral cavity and oropharyngeal squamous cell carcinoma—An update. CA: A Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef]
- Hoffman, G.; Islam, S.; Eisenberg, R. Microvascular reconstruction of the mouth, face and jaws. Oromandibular reconstruction–free fibula flap. Aust. Dent. J. 2012, 57, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-Y.; Djohan, R.; Dobryansky, M.; Chou, S.-W.; Hou, W.-H.; Chen, M.-H.; Wei, F.-C. Assessment of donor-site morbidity using balance and gait tests after bilateral fibula osteoseptocutaneous free flap transfer. Ann. Plast. Surg. 2009, 62, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Schaaf, H.; Lendeckel, S.; Howaldt, H.-P.; Streckbein, P. Donor site morbidity after bone harvesting from the anterior iliac crest. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 109, 52–58. [Google Scholar] [CrossRef]
- Hyong, I.H.; Kim, J.H. Test of intrarater and interrater reliability for the star excursion balance test. J. Phys. Ther. Sci. 2014, 26, 1139–1141. [Google Scholar] [CrossRef] [Green Version]
- Gribble, P.A.; Hertel, J.; Plisky, P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. J. Athl. Train. 2012, 47, 339–357. [Google Scholar] [CrossRef] [Green Version]
- Carcia, C.R.; Martin, R.L.; Drouin, J.M. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J. Athl. Train. 2008, 43, 179–183. [Google Scholar] [CrossRef] [Green Version]
- Munro, A.G.; Herrington, L.C. Between-session reliability of the star excursion balance test. Phys. Ther. Sport 2010, 11, 128–132. [Google Scholar] [CrossRef]
- Coughlan, G.F.; Fullam, K.; Delahunt, E.; Gissane, C.; Caulfield, B.M. A comparison between performance on selected directions of the star excursion balance test and the Y balance test. J. Athl. Train. 2012, 47, 366–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ni, Y.; Zhang, X.; Zhang, Z.; Liang, W.; Zhao, L.; Li, Z.; Li, S.; Lu, P.; Xu, Z.; Dai, W. Assessment of fibula flap with flexor hallucis longus’s effect on head & neck tumor patients’ quality of life and function of donor site. Oral Oncol. 2020, 100, 104489. [Google Scholar] [PubMed]
- Shazadeh Safavi, P.; Janney, C.; Jupiter, D.; Kunzler, D.; Bui, R.; Panchbhavi, V.K. A systematic review of the outcome evaluation tools for the foot and ankle. Foot Ankle Spec. 2019, 12, 461–470. [Google Scholar] [CrossRef]
- Martin, R.; Burdett, R.; Irrgang, J.; Martin, L.; Burdett, R.; Irrgang, J. Development of the foot and ankle disability index (FADI). J Orthop. Sports Phys. Ther. 1999, 29, A32–A33. [Google Scholar]
- Enright, P.L. The six-minute walk test. Respir. Care 2003, 48, 783–785. [Google Scholar] [PubMed]
- Price, D.D.; Bush, F.M.; Long, S.; Harkins, S.W. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 1994, 56, 217–226. [Google Scholar] [CrossRef]
- Williamson, A.; Hoggart, B. Pain: A review of three commonly used pain rating scales. J. Clin. Nurs. 2005, 14, 798–804. [Google Scholar] [CrossRef]
- Robinson, P.; Smith, K.; Johnson, F.; Coppins, D. Equipment and methods for simple sensory testing. Br. J. Oral Maxillofac. Surg. 1992, 30, 387–389. [Google Scholar] [CrossRef]
- Zuniga, J.R.; Meyer, R.A.; Gregg, J.M.; Miloro, M.; Davis, L.F. The accuracy of clinical neurosensory testing for nerve injury diagnosis. J. Oral Maxillofac. Surg. 1998, 56, 2–8. [Google Scholar] [CrossRef]
- Guerra, M.F.M.; Gías, L.N.; Campo, F.J.R.; González, F.J.D. Vascularized free fibular flap for mandibular reconstruction: A report of 26 cases. J. Oral Maxillofac. Surg. 2001, 59, 140–144. [Google Scholar] [CrossRef]
- Vittayakittipong, P. Donor-site morbidity after fibula free flap transfer: A comparison of subjective evaluation using a visual analogue scale and point evaluation system. Int. J. Oral Maxillofac. Surg. 2013, 42, 956–961. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.I.; Yu, P. Prospective series of reconstruction of complex composite mandibulectomy defects with double island free fibula flap. J. Surg. Oncol. 2017, 116, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Catalá-Lehnen, P.; Rendenbach, C.; Heiland, M.; Khakpour, P.; Rueger, J.M.; Schmelzle, R.; Blake, F. Long-term donor-site morbidity after microsurgical fibular graft: Is there a difference between the medial approach and the lateral approach? J. Oral Maxillofac. Surg. 2012, 70, 2198–2204. [Google Scholar] [CrossRef]
- Li, P.; Fang, Q.; Qi, J.; Luo, R.; Sun, C. Risk factors for early and late donor-site morbidity after free fibula flap harvest. J. Oral Maxillofac. Surg. 2015, 73, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- González-García, R.; Naval-Gías, L.; Rodríguez-Campo, F.J.; Muñoz-Guerra, M.F.; Sastre-Pérez, J. Vascularized free fibular flap for the reconstruction of mandibular defects: Clinical experience in 42 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 106, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Colletti, G.; Autelitano, L.; Rabbiosi, D.; Biglioli, F.; Chiapasco, M.; Mandalà, M.; Allevi, F. Technical refinements in mandibular reconstruction with free fibula flaps: Outcome-oriented retrospective review of 99 cases. Acta Otorhinolaryngol. Ital. 2014, 34, 342. [Google Scholar]
- Shpitzer, T.; Neligan, P.C.; Gullane, P.J.; Freeman, J.E.; Boyd, B.J.; Rotstein, L.E.; Brown, D.H.; Irish, J.C.; Gur, E. Oromandibular reconstruction with the fibular free flap: Analysis of 50 consecutive flaps. Arch. Otolaryngol.–Head Neck Surg. 1997, 123, 939–944. [Google Scholar] [CrossRef]
- Papadopulos, N.A.; Schaff, J.; Sader, R.; Kovacs, L.; Deppe, H.; Kolk, A.; Biemer, E. Mandibular reconstruction with free osteofasciocutaneous fibula flap: A 10 years experience. Injury 2008, 39, 75–82. [Google Scholar] [CrossRef]
- Hidalgo, D.A.; Rekow, A. A review of 60 consecutive fibula free flap mandible reconstructions. Plast. Reconstr. Surg. 1995, 96, 585–596. [Google Scholar] [CrossRef]
- López-Arcas, J.M.; Arias, J.; Del Castillo, J.L.; Burgueño, M.; Navarro, I.; Morán, M.J.; Chamorro, M.; Martorell, V. The fibula osteomyocutaneous flap for mandible reconstruction: A 15-year experience. J. Oral Maxillofac. Surg. 2010, 68, 2377–2384. [Google Scholar] [CrossRef]
- Kansy, K.; Hoffmann, J.; Alhalabi, O.; Mistele, N.; Freier, K.; Shavlokhova, V.; Mertens, C.; Freudlsperger, C.; Engel, M. Long-term donor site morbidity in head and neck cancer patients and its impact on quality of life: A cross-sectional study. Int. J. Oral Maxillofac. Surg. 2019, 48, 875–885. [Google Scholar] [CrossRef] [PubMed]
- Anthony, J.P.; Rawnsley, J.D.; Benhaim, P.; Ritter, E.F.; Sadowsky, S.H.; Singer, M.I. Donor leg morbidity and function after fibula free flap mandible reconstruction. Plast. Reconstr. Surg. 1995, 96, 146–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.C.; Leong, C.P.; Pong, Y.P.; Liu, T.Y.; Kuo, Y.R. Functional assessment of donor-site morbidity after harvest of a fibula chimeric flap with a sheet of soleus muscle for mandibular composite defect reconstruction. Microsurgery 2012, 32, 20–25. [Google Scholar] [CrossRef]
- Pototschnig, H.; Schaff, J.; Kovacs, L.; Biemer, E.; Papadopulos, N.A. The free osteofasciocutaneous fibula flap: Clinical applications and surgical considerations. Injury 2013, 44, 366–369. [Google Scholar] [CrossRef]
- Nathan, S.S.; Athanasian, E.; Boland, P.J.; Healey, J.H. Valgus ankle deformity after vascularized fibular reconstruction for oncologic disease. Ann. Surg. Oncol. 2009, 16, 1938–1945. [Google Scholar] [CrossRef] [PubMed]
- Bodde, E.W.; De Visser, E.; Duysens, J.E.; Hartman, E.H. Donor-site morbidity after free vascularized autogenous fibular transfer: Subjective and quantitative analyses. Plast. Reconstr. Surg. 2003, 111, 2237–2242. [Google Scholar] [CrossRef] [Green Version]
- Chou, S.W.; Liao, H.T.; Yazar, S.; Lin, C.H.; Lin, Y.C.; Wei, F.C. Assessment of fibula osteoseptocutaneous flap donor-site morbidity using balance and gait test. J. Orthop. Res. 2009, 27, 555–560. [Google Scholar] [CrossRef]
- Babovic, S.; Johnson, C.H.; Finical, S.J. Free fibula donor-site morbidity: The Mayo experience with 100 consecutive harvests. J. Reconstr. Microsurg. 2000, 16, 0107–0110. [Google Scholar] [CrossRef]
- Gribble, P.A.; Hertel, J.; Denegar, C.R.; Buckley, W.E. The effects of fatigue and chronic ankle instability on dynamic postural control. J. Athl. Train. 2004, 39, 321. [Google Scholar]
- Hertel, J.; Braham, R.A.; Hale, S.A.; Olmsted-Kramer, L.C. Simplifying the star excursion balance test: Analyses of subjects with and without chronic ankle instability. J. Orthop. Sports Phys. Ther. 2006, 36, 131–137. [Google Scholar] [CrossRef] [Green Version]
- Hale, S.A.; Hertel, J.; Olmsted-Kramer, L.C. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2007, 37, 303–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delahunt, E.; Chawke, M.; Kelleher, J.; Murphy, K.; Prendiville, A.; Sweeny, L.; Patterson, M. Lower limb kinematics and dynamic postural stability in anterior cruciate ligament-reconstructed female athletes. J. Athl. Train. 2013, 48, 172–185. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Lachman, H.; Freilich, N. Long-term impact of ankle sprains on postural control and fascial densification. J. Bodyw. Mov. Ther. 2016, 20, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Rosen, A.B.; Brown, C.N. Functional performance deficits in adolescent athletes with a history of lateral ankle sprain (s). Phys. Ther. Sport 2018, 33, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Watanabe, K.; Ito, T.; Tanaka, M.; Shida, M.; Katayose, M.; Gamada, K. The effect of novel ankle-realigning socks on dynamic postural stability in individuals with chronic ankle instability. Int. J. Sports Phys. Ther. 2019, 14, 264. [Google Scholar] [CrossRef]
- Hadadi, M.; Abbasi, F. Comparison of the effect of the combined mechanism ankle support on static and dynamic postural control of chronic ankle instability patients. Foot Ankle Int. 2019, 40, 702–709. [Google Scholar] [CrossRef]
- Karagiannakis, D.N.; Iatridou, K.I.; Mandalidis, D.G. Ankle muscles activation and postural stability with Star Excursion Balance Test in healthy individuals. Hum. Mov. Sci. 2020, 69, 102563. [Google Scholar] [CrossRef]
- Hakim, S.G.; Tehrany, A.S.; Wendlandt, R.; Jacobsen, H.-C.; Trenkle, T.; Sieg, P. The impact of harvest length and detachment of the interosseous membrane on donor-site morbidity following free fibula flap surgery—A biomechanical experimental study. J. Cranio-Maxillofac. Surg. 2018, 46, 1939–1942. [Google Scholar] [CrossRef]
- McKeon, P.O.; Ingersoll, C.D.; Kerrigan, D.C.; Saliba, E.; Bennett, B.C.; Hertel, J. Balance training improves function and postural control in those with chronic ankle instability. Medicine Sci. Sports Exerc. 2008, 40, 1810–1819. [Google Scholar] [CrossRef]
- Cook, C.; Queen, R.M.; Slaven, E.J.; DeOrio, J.K.; Easley, M.E.; Nunley, J.A. Dimensionality of measures for severe unilateral ankle arthritis. PM R 2010, 2, 987–994. [Google Scholar] [CrossRef]
- Hubbard-Turner, T. Relationship between mechanical ankle joint laxity and subjective function. Foot Ankle Int. 2012, 33, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Wikstrom, E.A.; Tillman, M.D.; Chmielewski, T.L.; Cauraugh, J.H.; Naugle, K.E.; Borsa, P.A. Discriminating between copers and people with chronic ankle instability. J. Athl. Train. 2012, 47, 136–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Chung, E.; Lee, B.-H. A comparison of the foot and ankle condition between elite athletes and non-athletes. J. Phys. Ther. Sci. 2013, 25, 1269–1272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanders, D.; Schneider, P.; Taylor, M.; Tieszer, C.; Lawendy, A.-R. Improved Reduction of the Tibiofibular Syndesmosis with TightRope Compared with Screw Fixation: Results of a Randomized Controlled Study. J. Orthop. Trauma 2019, 33, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Carter, T.H.; Duckworth, A.D.; Oliver, W.M.; Molyneux, S.G.; Amin, A.K.; White, T.O. Open Reduction and Internal Fixation of Distal Tibial Pilon Fractures. JBJS Essent. Surg. Tech. 2019, 9. [Google Scholar] [CrossRef]
- Glave, A.P.; Didier, J.J.; Weatherwax, J.; Browning, S.J.; Fiaud, V. Testing postural stability: Are the star excursion balance test and biodex balance system limits of stability tests consistent? Gait Posture 2016, 43, 225–227. [Google Scholar] [CrossRef]
- Hertel, J.; Miller, S.J.; Denegar, C.R. Intratester and intertester reliability during the Star Excursion Balance Tests. J. Sport Rehabil. 2000, 9, 104–116. [Google Scholar] [CrossRef] [Green Version]
- Kinzey, S.J.; Armstrong, C.W. The reliability of the star-excursion test in assessing dynamic balance. J. Orthop. Sports Phys. Ther. 1998, 27, 356–360. [Google Scholar] [CrossRef] [Green Version]
- Basnett, C.R.; Hanish, M.J.; Wheeler, T.J.; Miriovsky, D.J.; Danielson, E.L.; Barr, J.; Grindstaff, T.L. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int. J. Sports Phys. Ther. 2013, 8, 121. [Google Scholar]
- Robinson, R.H.; Gribble, P.A. Support for a reduction in the number of trials needed for the star excursion balance test. Arch. Phys. Med. Rehabil. 2008, 89, 364–370. [Google Scholar] [CrossRef]
- Eechaute, C.; Vaes, P.; Van Aerschot, L.; Asman, S.; Duquet, W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: A systematic review. BMC Musculoskelet. Disord. 2007, 8, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.-Y.; Lee, H.-J.; Kim, S.-E.; Choi, P.-B.; Song, S.-H.; Jee, Y.-S. Short term rehabilitation and ankle instability. Int. J. Sports Med. 2012, 33, 485–496. [Google Scholar] [CrossRef] [PubMed]

| Variable | Mean (Standard Deviation) or Percentage % (Absolute Frequency) |
|---|---|
| Age (years) at surgery | 55.4 (12.5) |
| Gender (m/f) | 67.6% (n = 46)/32.4% (n = 22) |
| Height (cm) at surgery | 174 (11) |
| Weight (kg) at surgery | 74 (17) |
| BMI at surgery | |
| underweight | 8.8% (n = 6) |
| normal weight | 54.4% (n = 37) |
| pre-obesity | 25.0% (n = 17) |
| obesity grade I | 8.8% (n = 6) |
| obesity grade II | 2.9% (n = 2) |
| Indication of fibula transplantation | |
| squamous cell carcinoma | 69.1% (n = 47) |
| ameloblastoma | 8.8% (n = 6) |
| keratocystic odontogenic tumor | 7.4% (n = 5) |
| jaw atrophy | 2.9% (n = 2) |
| adenoid cystic carcinoma | 2.9% (n = 2) |
| acinar cell carcinoma | 1.5% (n = 1) |
| adenosquamous carcinoma | 1.5% (n = 1) |
| mucoepidermoid carcinoma | 1.5% (n = 1) |
| myoepithelial carcinoma | 1.5% (n = 1) |
| hemangiopericytoma | 1.5% (n = 1) |
| osteoradione necrosis | 1.5% (n = 1) |
| Operated Leg (left/right) | 25% (n = 17)/ 75% (n = 51) |
| Type of transplant | |
| osseomyocutan | 76.5% (n = 52) |
| osseomuscular | 14.7% (n = 10) |
| prefabricated | 8.8% (n = 6) |
| Wound closure | |
| graft from thigh region | 73.5% (n = 50) |
| primary sutured | 26.5% (n = 18) |
| Hospitalisation time | |
| up to 1 week | 1.5% (n = 1) |
| >1 up to 2 weeks | 35.3% (n = 24) |
| >2 up to 3 weeks | 27.9% (n = 19) |
| >3 up to 4 weeks | 14.7% (n = 10) |
| >4 up to 5 weeks | 13.2% (n = 9) |
| more than 5 weeks | 7.4% (n = 5) |
| Direction | Operated Leg | Healthy Leg | Difference Operated—Healthy Leg | p Value 1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Mean | Std | Min | Max | Mean | Std | Min | Max | Mean | Std | ||
| A | 39.3 | 78.0 | 56.7 | 8.1 | 41.0 | 81.0 | 58.8 | 8.5 | −15.0 | 9.7 | −2.1 | 3.9 | 0.001 |
| AM | 40.3 | 81.0 | 60.8 | 8.7 | 46.0 | 82.7 | 62.8 | 9.0 | −18.0 | 8.2 | −2.0 | 4.6 | 0.001 |
| M | 39.7 | 82.7 | 62.1 | 8.5 | 43.7 | 85.0 | 63.9 | 8.6 | −15.0 | 8.7 | −1.8 | 4.0 | <0.001 |
| PM | 44.0 | 87.0 | 61.8 | 9.4 | 41.2 | 89.3 | 64.6 | 9.4 | −14.0 | 7.7 | −2.7 | 4.3 | <0.0001 |
| P | 22.3 | 89.3 | 56.3 | 11.1 | 27.5 | 90.3 | 59.5 | 11.1 | −11.7 | 7.3 | −3.2 | 4.0 | <0.0001 |
| PL | 23.7 | 75.7 | 48.9 | 11.5 | 21.3 | 86.0 | 53.0 | 12.1 | −22.0 | 7.7 | −4.1 | 5.9 | <0.0001 |
| L | 21.7 | 70.7 | 43.6 | 8.3 | 20.7 | 69.0 | 46.5 | 8.5 | −19.0 | 8.0 | −2.8 | 4.4 | <0.0001 |
| AL | 36.7 | 77.0 | 52.3 | 7.9 | 37.0 | 78.3 | 54.2 | 8.0 | −14.0 | 11.0 | −2.0 | 4.5 | 0.001 |
| Literature Review | Age (y) | SEBT Ø (%) | A (%) | AM (%) | M (%) | PM (%) | P (%) | PL (%) | L (%) | AL (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Olmsted 2002 n = 20 CAI, SL [36] | 19.8 | 5.5 | 3.9 | 5.4 | 3.8 | 6.3 | 3.8 | 3.1 | 10.6 | 4.2 |
| Gribble 2004 n = 30 CAI [80] | 22.3 | - | 5.6 | - | 5.9 | - | 7.4 | - | - | - |
| Hertel 2006 n = 48 CAI, SL [81] | 20.9 | 3.3 | 3.8 | 2.4 | 3.4 | 4.5 | 2.4 | 2.5 | 4.3 | 2.8 |
| Hale 2007 * n = 29 CAI,SL [82] | 21.4 | 4.2 | 2.8 | 3.9 | 3.5 | 4.7 | 3.2 | 5.2 | 6.4 | 3.8 |
| Delahunt 2013 n = 17 CL [83] | 20.8 | - | 3.8 | - | - | 8.6 | - | 9.4 | - | - |
| Kalichmann 2016 n = 20 AD, SL [84] | 25.4 | 2.2 | 2 | 2.4 | 1.6 | 3.7 | 2.8 | 1.7 | 0.6 | 3 |
| Ko 2018 n = 24 CAI, SL [85] | 15.5 | - | 11.3 | - | - | 9.4 | - | 7 | - | - |
| Kobayashi 2019 n = 50 CAI [86] | 20.8 | 8.8 | 7.3 | 7.1 | 7.2 | 7.7 | 9.7 | 13 | 10 | 8.3 |
| Hadadi 2019 n = 44 CAI [87] | 22.9 | - | - | 5.3 | 9.3 | 6.4 | - | - | - | - |
| average | 22 | 5.1 | 5.8 | 4.5 | 5.2 | 6.3 | 5.2 | 6.3 | 6.4 | 4.6 |
| our study n = 61 | 55.4 | 4.5 | 3.6 | 3.2 | 2.8 | 4.2 | 5.4 | 7.8 | 6.1 | 3.6 |
| Shah 2017 * n = 26 FT SL [34] | 49.4 | −0.2 | −1.6 | 3.1 | −1.6 | −3.3 | 0 | 0 | 1.6 | 0 |
| Literature Review | Medical Condition | n | Age (y) | Score (%) |
|---|---|---|---|---|
| Hale & Hertel 2005 [35] | CAI | 30 | 21.5 | 89.6 |
| Hale 2007 * [82] | CAI | 29 | 21.4 | 89.7 |
| McKeon 2008 [90] | CAI | 31 | 20.9 | 84.2 |
| Cook 2010 [91] | severe arthritis | 79 | 63.9 | 46 |
| Hubbard-Turner 2012 [92] | CAI | 120 | 20.6 | 87.6 |
| Wikstrom 2012 [93] | CAI | 24 | 21.7 | 95.2 |
| Kim 2013 [94] | professional athletes | 85 | 19.8 | 88.9 |
| Shah 2017 * [34] | Fibula Transplant | 26 | 46.4 | 89 |
| Sanders 2019 [95] | Fibula fracture surgery | 103 | 39.5 | 91.4 |
| Carter 2019 [96] | Tibia Pilon fracture | 99 | - | 76 |
| CAI average | CAI | 46,8 | 21.2 | 89.26 |
| FADI average | 62,6 | 30.6 | 83.8 | |
| Our study * | Fibula transplant | 68 | 55.4 | 89.4 |
| Basic Data | Surgical Data | Follow-Up Examination |
|---|---|---|
| Indication for surgery | Subjective pain intensity (harvested leg) | |
| Follow-up time | Duration of pain | |
| Age of the patient (surgery) | Localisation of the harvested flap (right or left leg) | Fibular nerve lesion |
| Type of graft removed (osseocutaneus, osseomuscular, prefabricated) | blunt sharp discrimination test (harvested leg) | |
| Height | Type of wound closure | Scar length and width (harvested leg) |
| Body weight | Hospitalization time | Skin color (harvested leg) |
| Body Mass Index (BMI) | Post-operative complications | Subjects satisfaction aesthetics (harvested leg) |
| Subjects general satisfaction |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attia, S.; Diefenbach, J.; Schmermund, D.; Böttger, S.; Pons-Kühnemann, J.; Scheibelhut, C.; Heiss, C.; Howaldt, H.-P. Donor-Site Morbidity after Fibula Transplantation in Head and Neck Tumor Patients: A Split-Leg Retrospective Study with Focus on Leg Stability and Quality of Life. Cancers 2020, 12, 2217. https://doi.org/10.3390/cancers12082217
Attia S, Diefenbach J, Schmermund D, Böttger S, Pons-Kühnemann J, Scheibelhut C, Heiss C, Howaldt H-P. Donor-Site Morbidity after Fibula Transplantation in Head and Neck Tumor Patients: A Split-Leg Retrospective Study with Focus on Leg Stability and Quality of Life. Cancers. 2020; 12(8):2217. https://doi.org/10.3390/cancers12082217
Chicago/Turabian StyleAttia, Sameh, Jonas Diefenbach, Daniel Schmermund, Sebastian Böttger, Jörn Pons-Kühnemann, Christine Scheibelhut, Christian Heiss, and Hans-Peter Howaldt. 2020. "Donor-Site Morbidity after Fibula Transplantation in Head and Neck Tumor Patients: A Split-Leg Retrospective Study with Focus on Leg Stability and Quality of Life" Cancers 12, no. 8: 2217. https://doi.org/10.3390/cancers12082217






