Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position
Abstract
1. Introduction
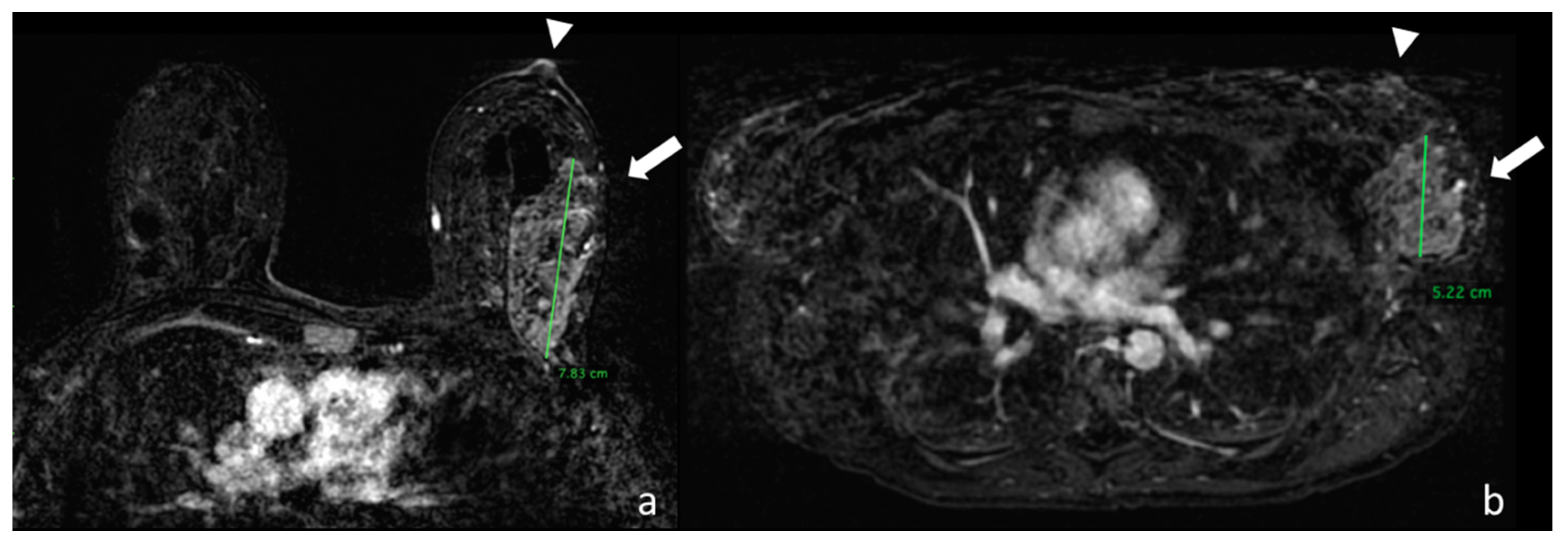
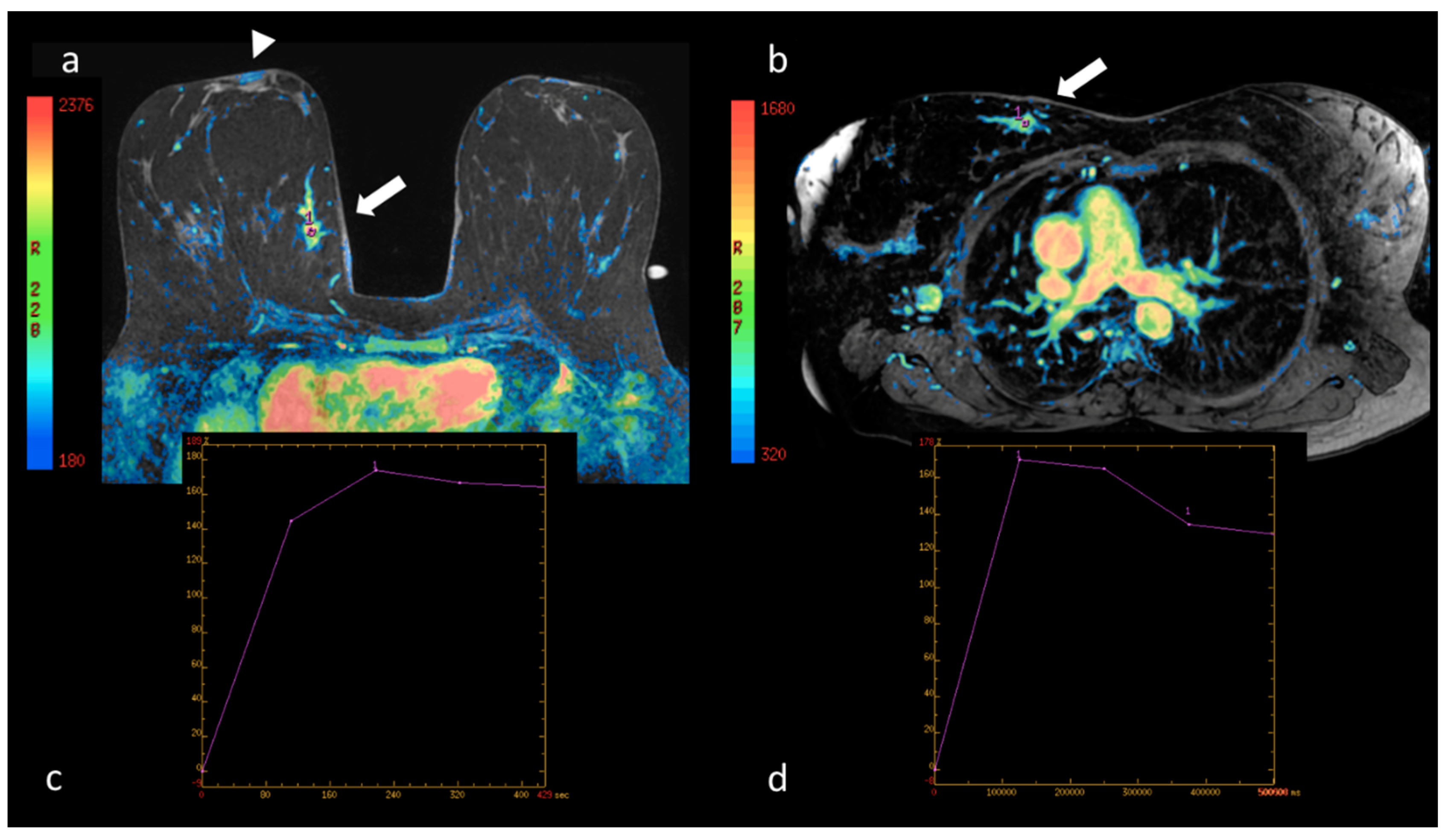
2. Patients and Methods
2.1. Study Population
2.2. MRI in the Prone Position
2.3. MRI in the Supine Position
2.4. Contrast Medium
2.5. Recommendations before the MR Examination
2.6. Image Evaluation
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kaiser, W. MRI of the female breast. First clinical results. Arch. Int. Physiol. Biochim. 1985, 93, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Heywang, S.H.; Hahn, D.; Schmidt, H.; Krischke, I.; Eiermann, W.; Bassermann, R.; Lissner, J. MR Imaging of the Breast Using Gadolinium-DTPA. J. Comput. Assist. Tomogr. 1986, 10, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Kuhl, C. The Current Status of Breast MR Imaging Part I. Choice of Technique, Image Interpretation, Diagnostic Accuracy, and Transfer to Clinical Practice. Radiology 2007, 244, 356–378. [Google Scholar] [CrossRef] [PubMed]
- Baum, F.; Fischer, U.; Vosshenrich, R.; Grabbe, E. Classification of hypervascularized lesions in CE MR imaging of the breast. Eur. Radiol. 2002, 12, 1087–1092. [Google Scholar] [CrossRef]
- American College of Radiology. Breast Imaging Reporting, Data System (BI-RADS®) 5th ed. Available online: http//www.acr.org (accessed on 5 May 2020).
- Lee, C.H.; Dershaw, D.D.; Kopans, D.; Evans, P.; Monsees, B.; Monticciolo, D.; Brenner, R.J.; Bassett, L.; Berg, W.; Feig, S.; et al. Breast Cancer Screening With Imaging: Recommendations From the Society of Breast Imaging and the ACR on the Use of Mammography, Breast MRI, Breast Ultrasound, and Other Technologies for the Detection of Clinically Occult Breast Cancer. J. Am. Coll. Radiol. 2010, 7, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Fausto, A.; Casella, D.; Mantovani, L.; Giacalone, G.; Volterrani, L. Clinical value of second-look ultrasound: Is there a way to make it objective? Eur. J. Radiol. 2012, 81, S36–S40. [Google Scholar] [CrossRef]
- Spick, C.; Baltzer, P. Diagnostic Utility of Second-Look US for Breast Lesions Identified at MR Imaging: Systematic Review and Meta-Analysis. Radiology 2014, 273, 401–409. [Google Scholar] [CrossRef]
- Fausto, A.; Bernini, M.; La Forgia, D.; Fanizzi, A.; Marcasciano, M.; Volterrani, L.; Casella, D.; Mazzei, M.A. Six-year prospective evaluation of second-look US with volume navigation for MRI-detected additional breast lesions. Eur. Radiol. 2018, 29, 1799–1808. [Google Scholar] [CrossRef]
- Kucukkaya, F.; Aribal, E.; Tureli, D.; Altas, H.; Kaya, H. Use of a Volume Navigation Technique for Combining Real-Time Ultrasound and Contrast-Enhanced MRI: Accuracy and Feasibility of a Novel Technique for Locating Breast Lesions. Am. J. Roentgenol. 2016, 206, 217–225. [Google Scholar] [CrossRef]
- Pons, E.P.; Azcon, F.; Casas, M.C.; Meca, S.M.; Espona, J.L.G. Real-time MRI navigated US: Role in diagnosis and guided biopsy of incidental breast lesions and axillary lymph nodes detected on breast MRI but not on second look US. Eur. J. Radiol. 2014, 83, 942–950. [Google Scholar] [CrossRef]
- Aribal, E.; Tureli, D.; Kucukkaya, F.; Kaya, H. Volume Navigation Technique for Ultrasound-Guided Biopsy of Breast Lesions Detected Only at MRI. Am. J. Roentgenol. 2017, 208, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mazzei, M.A.; Di Giacomo, L.; Fausto, A.; Gentili, F.; Mazzei, F.G.; Volterrani, L. Efficacy of Second-Look Ultrasound with MR Coregistration for Evaluating Additional Enhancing Lesions of the Breast: Review of the Literature. BioMed Res. Int. 2018, 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Park, A.Y.; Seo, B.K.; Han, H.; Cho, K.R.; Woo, O.H.; Cha, S.H.; Cha, J. Clinical Value of Real-Time Ultrasonography-MRI Fusion Imaging for Second-Look Examination in Preoperative Breast Cancer Patients: Additional Lesion Detection and Treatment Planning. Clin. Breast Cancer 2018, 18, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Joukainen, S.; Masarwah, A.; Könönen, M.; Husso, M.; Sutela, A.; Kärjä, V.; Vanninen, R.; Sudah, M. Feasibility of mapping breast cancer with supine breast MRI in patients scheduled for oncoplastic surgery. Eur. Radiol. 2018, 29, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Barth, R.J.; Krishnaswamy, V.; Paulsen, K.D.; Rooney, T.B.; Wells, W.A.; Rizzo, E.; Angeles, C.V.; Marotti, J.D.; Zuurbier, R.A.; Black, C.C. A Patient-Specific 3D-Printed Form Accurately Transfers Supine MRI-Derived Tumor Localization Information to Guide Breast-Conserving Surgery. Ann. Surg. Oncol. 2017, 24, 2950–2956. [Google Scholar] [CrossRef] [PubMed]
- Ando, T.; Ito, Y.; Ido, M.; Osawa, M.; Kousaka, J.; Mouri, Y.; Fujii, K.; Nakano, S.; Kimura, J.; Ishiguchi, T.; et al. Pre-Operative Planning Using Real-Time Virtual Sonography, an MRI/Ultrasound Image Fusion Technique, for Breast-Conserving Surgery in Patients with Non-Mass Enhancement on Breast MRI: A Preliminary Study. Ultrasound Med. Boil. 2018, 44, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Gombos, E.C.; Jayender, J.; Richman, D.M.; Caragacianu, D.L.; Mallory, M.A.; Jolesz, F.A.; Golshan, M. Intraoperative Supine Breast MR Imaging to Quantify Tumor Deformation and Detection of Residual Breast Cancer: Preliminary Results. Radiology 2016, 281, 720–729. [Google Scholar] [CrossRef]
- den Hartogh, M.D.; Philippens, M.E.P.; Van Dam, I.E.; Kleynen, C.E.; Tersteeg, R.J.H.A.; Pijnappel, R.M.; Kotte, A.N.T.J.; Verkooijen, H.M.; van den Bosch, M.A.A.J.; Van Vulpen, M.; et al. MRI and CT imaging for preoperative target volume delineation in breast-conserving therapy. Radiat. Oncol. 2014, 9, 63. [Google Scholar] [CrossRef]
- Kumar, S.; Holloway, L.; Roach, D.; Pogson, E.; Veera, J.; Batumalai, V.; Lim, K.; Delaney, G.; Lazarus, E.; Borok, N.; et al. The impact of a radiologist-led workshop on MRI target volume delineation for radiotherapy. J. Med. Radiat. Sci. 2018, 65, 300–310. [Google Scholar] [CrossRef]
- Zuo, L. MRI in breast cancer radiotherapy in prone and supine positions. Front. Biosci. 2017, 22, 570–579. [Google Scholar] [CrossRef]
- Kasiulevičius, V.; Šapoka, V.; Filipavičiūtė, R. Sample size calculation in epidemiological studies. Gerontologija 2006, 7, 225–231. [Google Scholar]
- Wilcoxon, F. Individual Comparisons by Ranking Methods. Biom. Bull. 1945, 1, 80. [Google Scholar] [CrossRef]
- Fanizzi, A.; Basile, T.M.A.; Losurdo, L.; Bellotti, R.; Bottigli, U.; Dentamaro, R.; Didonna, V.; Fausto, A.; Massafra, R.; Moschetta, M.; et al. A machine learning approach on multiscale texture analysis for breast microcalcification diagnosis. BMC Bioinform. 2020, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Basile, T.M.; Fanizzi, A.; Losurdo, L.; Bellotti, R.; Bottigli, U.; Dentamaro, R.; Didonna, V.; Fausto, A.; Massafra, R.; Moschetta, M.; et al. Microcalcification detection in full-field digital mammograms: A fully automated computer-aided system. Phys. Medica 2019, 64, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fanizzi, A.; Basile, T.M.; Losurdo, L.; Bellotti, R.; Bottigli, U.; Campobasso, F.; Didonna, V.; Fausto, A.; Massafra, R.; Tagliafico, A.; et al. Ensemble Discrete Wavelet Transform and Gray-Level Co-Occurrence Matrix for Microcalcification Cluster Classification in Digital Mammography. Appl. Sci. 2019, 9, 5388. [Google Scholar] [CrossRef]
- Losurdo, L.; Fanizzi, A.; Basile, T.M.; Bellotti, R.; Bottigli, U.; Dentamaro, R.; Didonna, V.; Fausto, A.; Massafra, R.; Monaco, A.; et al. A Combined Approach of Multiscale Texture Analysis and Interest Point/Corner Detectors for Microcalcifications Diagnosis. Appl. Evol. Comput. 2018, 1, 302–313. [Google Scholar] [CrossRef]
- Basile, T.M.; Fanizzi, A.; Losurdo, L.; Bellotti, R.; Tangaro, S.; La Forgia, D.; Didonna, V.; Massafra, R.; Tamborra, P.; Moschetta, M.; et al. Hough transform for clustered microcalcifications detection in full-field digital mammograms. In Applications of Digital Image Processing XL; SPIE: Bellingham, WA, USA, 2017; Volume 10396, p. 41. [Google Scholar]
- Losurdo, L.; Basile, T.M.; Fanizzi, A.; Bellotti, R.; Bottigli, U.; Carbonara, R.; Dentamaro, R.; Diacono, D.; Didonna, V.; Lombardi, A.; et al. A Gradient-Based Approach for Breast DCE-MRI Analysis. BioMed Res. Int. 2018, 2018, 1–10. [Google Scholar] [CrossRef]
- Del Palomar, A.P.; Calvo, B.; Herrero, J.; Lopez, J.; Doblaré, M. A finite element model to accurately predict real deformations of the breast. Med. Eng. Phys. 2008, 30, 1089–1097. [Google Scholar] [CrossRef]
- Satake, H.; Ishigaki, S.; Kitano, M.; Naganawa, S. Prediction of prone-to-supine tumor displacement in the breast using patient position change: Investigation with prone MRI and supine CT. Breast Cancer 2014, 23, 149–158. [Google Scholar] [CrossRef]
- Telegrafo, M.; Rella, L.; Ianora, A.A.S.; Angelelli, G.; Moschetta, M. Supine breast US: How to correlate breast lesions from prone MRI. Br. J. Radiol. 2016, 89. [Google Scholar] [CrossRef]
- Marcasciano, M.; Conversi, A.; Kaciulyte, J.; Dessy, L.A. RE: Prosthetic Breast Implant Rupture: Imaging—Pictorial Essay. Aesthetic Plast. Surg. 2017, 41, 1478–1480. [Google Scholar] [CrossRef] [PubMed]





| Type | N |
|---|---|
| FA | 19 |
| FBS | 9 |
| LYMP | 6 |
| FLO CRO | 4 |
| NA | 4 |
| PAP | 3 |
| SCL AD | 3 |
| LCIS | 2 |
| ADH | 2 |
| SIL | 1 |
| PAP M | 1 |
| 54 |
| Type | N |
|---|---|
| IDC | 27 |
| IDC + DCIS | 19 |
| DCIS | 10 |
| ILC | 5 |
| IDC + ILC | 2 |
| ILC + LCIS | 2 |
| DCIS + LCIS | 1 |
| 66 |
| (a) Intraobserver Test | |||||||||
| P | S | ||||||||
| idx1 | Idx2 | Sign | idx1 | Idx2 | Sign | ||||
| Op_A | 18.5 [13.0; 35.0] | 19.5 [12.0; 36.0] | - | 17.0 [12.0; 25.0] | 18.0 [11.0; 25.5] | - | |||
| OP_B | 21.0 [12.0; 35.0] | 21.0 [12.0; 36.5] | - | 16.5 [12.0; 24.5] | 17.0 [11.0; 25.0] | - | |||
| (b) Interobserver Test | |||||||||
| Position | Op_A (idx1 + idx2) | Op_B (idx1 + idx2) | Sign | ||||||
| P | 19.0 [12.0; 35.0] | 21.0 [12.0; 35.5] | - | ||||||
| S | 17.0 [11.0; 25.0] | 17.0 [12.0; 25.0] | - | ||||||
| (c) Test P vs. S | |||||||||
| P | S | Sign | |||||||
| Op_A (idx1 + idx2) | 19.0 [12.0; 35.0] | 17.0 [11.0; 25.0] | * | ||||||
| Op_B (idx1 + idx2) | 21.0 [12.0; 35.5] | 17.0 [12.0; 25.0] | * | ||||||
| 20.0 [12.0; 35.0] | 17.0 [12.0; 25.0] | ||||||||
| (d) Test idx1–2 vs. HP | |||||||||
| Position | Op_A | Op_B | HP | ||||||
| idx1 | Sign | idx2 | Sign | idx1 | Sign | idx2 | Sign | ||
| P | 18.5 [13.0; 35.0] | * | 19.5 [12.0; 36.0] | * | 21.0 [12.0; 35.0] | * | 21.0 [12.0; 36.5] | * | 17.0 [12.0; 23.5] |
| S | 17.0 [12.0; 25.0] | - | 18.0 [11.0; 25.5] | - | 16.5 [12.0; 24.5] | - | 17.0 [11.0; 25.0] | - | 17.0 [12.0; 23.5] |
| Type | Sample Size | P | S | HP | P vs. HP | S vs. HP |
|---|---|---|---|---|---|---|
| Mass-like | 62 | 13.0 [10.0; 21.0] | 13.0 [10.0; 19.0] | 14.0 [11.0; 21.0] | - | - |
| Non-mass-like | 58 | 28.5 [21.0; 42.0] | 23.0 [16.0; 34.0] | 20.0 [13.0; 25.0] | * | * |
| Type | Sample Size | P | S | HP | P vs. HP | S vs. HP |
|---|---|---|---|---|---|---|
| 1 | 25 | 24.0 [16.5; 28.0] | 20.0 [13.5; 24.5] | 19.0 [12.8; 21.0] | * | - |
| 2 | 27 | 11.0 [9.0; 16.0] | 11.0 [9.0; 15.5] | 12.0 [8.3; 18.8] | - | - |
| 3 | 27 | 15.0 [12.0; 20.0] | 15.0 [11.0; 21.0] | 13.0 [12.0; 22.8] | - | - |
| 4 | 22 | 34.5 [20.5; 43.0] | 23.0 [15.0; 36.0] | 24.5 [17.0; 32.0] | * | - |
| 4 + 5 | 41 | 37.0 [22.0; 47.5] | 25.0 [16.0; 36.5] | 23.0 [13.0; 28.3] | * | * |
| 5 | 19 | 42.0 [23.0; 52.5] | 33.0 [16.5; 37.0] | 17.0 [9.0; 25.0] | * | * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fausto, A.; Fanizzi, A.; Volterrani, L.; Mazzei, F.G.; Calabrese, C.; Casella, D.; Marcasciano, M.; Massafra, R.; La Forgia, D.; Mazzei, M.A. Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position. Cancers 2020, 12, 2364. https://doi.org/10.3390/cancers12092364
Fausto A, Fanizzi A, Volterrani L, Mazzei FG, Calabrese C, Casella D, Marcasciano M, Massafra R, La Forgia D, Mazzei MA. Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position. Cancers. 2020; 12(9):2364. https://doi.org/10.3390/cancers12092364
Chicago/Turabian StyleFausto, Alfonso, Annarita Fanizzi, Luca Volterrani, Francesco Giuseppe Mazzei, Claudio Calabrese, Donato Casella, Marco Marcasciano, Raffaella Massafra, Daniele La Forgia, and Maria Antonietta Mazzei. 2020. "Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position" Cancers 12, no. 9: 2364. https://doi.org/10.3390/cancers12092364
APA StyleFausto, A., Fanizzi, A., Volterrani, L., Mazzei, F. G., Calabrese, C., Casella, D., Marcasciano, M., Massafra, R., La Forgia, D., & Mazzei, M. A. (2020). Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position. Cancers, 12(9), 2364. https://doi.org/10.3390/cancers12092364









