Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches
Abstract
Simple Summary
Abstract
1. Introduction
2. The Role of the Blood–Brain Barrier, Blood–Tumor Barrier and Blood–CSF Barrier in Drug Delivery
3. Pathogenesis of Leptomeningeal Metastases
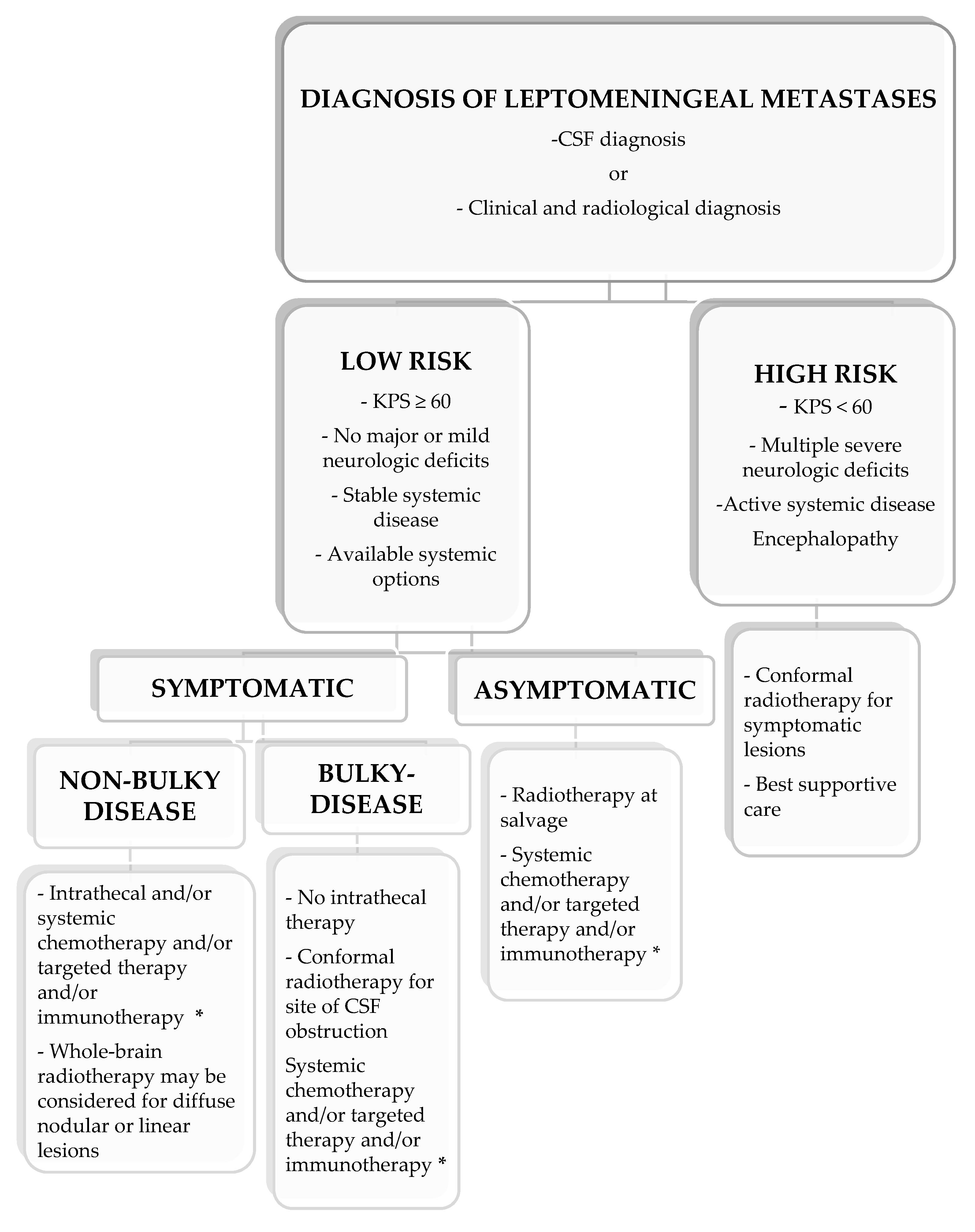
4. Diagnosis of Leptomeningeal Metastases
4.1. Neurological Symptoms
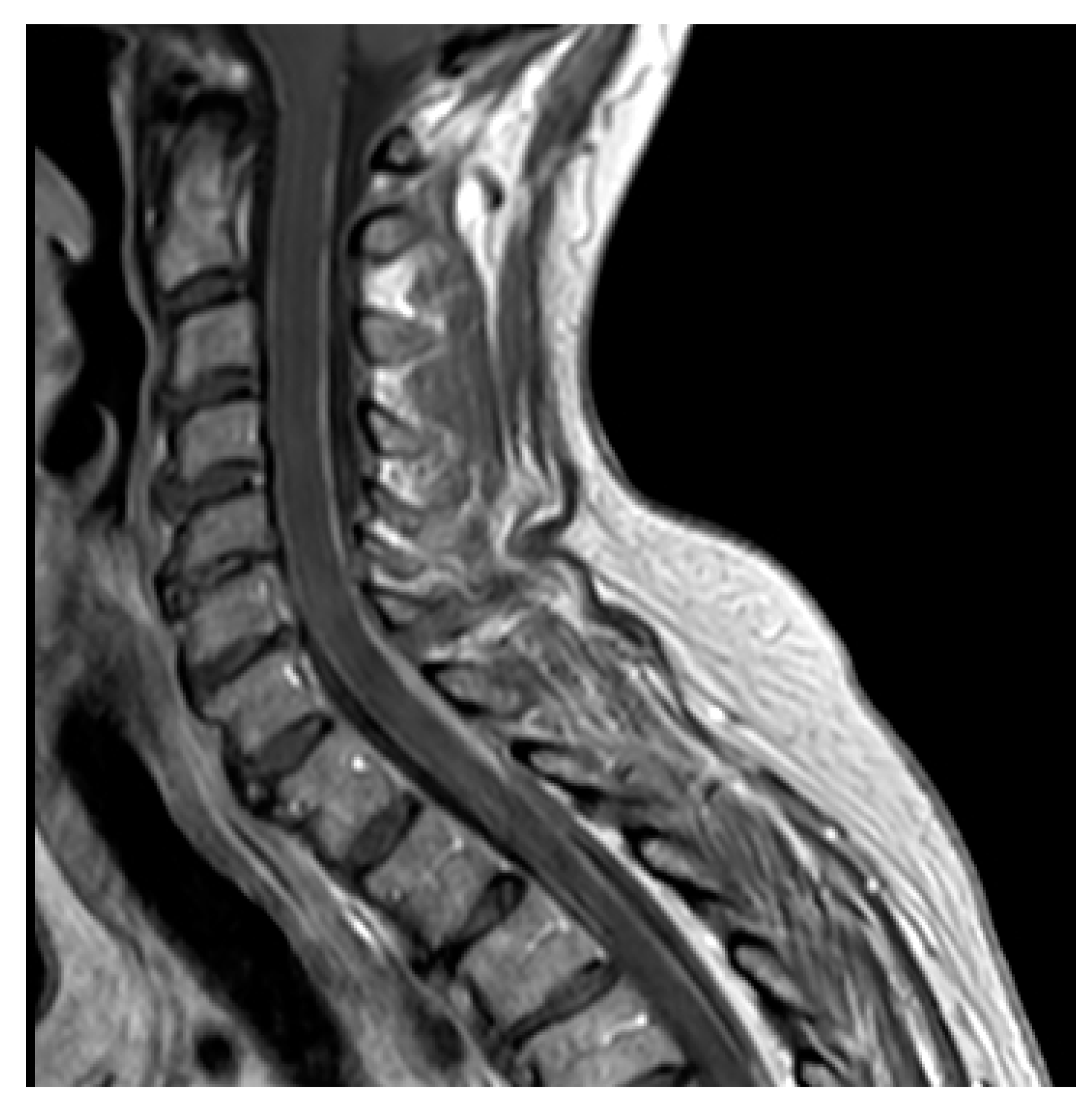
4.2. Neuroimaging Assessment
4.3. CSF Cytology and Liquid Biopsy
5. Targeting LM with Systemic and Intrathecal Approaches
5.1. LM from EGFR-Mutated NSCLC
5.2. LM from ALK-Rearranged NSCLC
5.3. LM from Breast Cancer
5.3.1. HER2-Positive LM from Breast Cancer
5.3.2. ER-Positive LM from Breast Cancer
5.3.3. LM from Triple-Negative BC
5.4. LM from Melanoma
6. Novel Techniques to Improve Drug Delivery across the BBB
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Le Rhun, E.; Galanis, E. Leptomeningeal metastases of solid cancer. Curr. Opin. Neurol. 2016, 29, 797–805. [Google Scholar] [CrossRef]
- Le Rhun, E.; Taillibert, S.; Chamberlain, M.C. Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. Surg. Neurol. Int. 2013, 4, S265–S288. [Google Scholar] [CrossRef]
- Glitza, I.C.; Smalley, K.S.M.; Brastianos, P.K.; Davies, M.A.; McCutcheon, I.; Liu, J.K.C.; Ahmed, K.A.; Arrington, J.A.; Evernden, B.R.; Smalley, I.; et al. Leptomeningeal disease in melanoma patients: An update to treatment, challenges, and future directions. Pigment Cell Melanoma Res. 2020, 33, 527–541. [Google Scholar] [CrossRef]
- Cheng, H.; Perez-Soler, R. Leptomeningeal metastases in non-small-cell lung cancer. Lancet Oncol. 2018, 19, e43–e55. [Google Scholar] [CrossRef]
- Franzoi, M.A.; Hortobagyi, G.N. Leptomeningeal carcinomatosis in patients with breast cancer. Crit. Rev. Oncol. Hematol. 2019, 135, 85–94. [Google Scholar] [CrossRef]
- O’Brown, N.M.; Pfau, S.J.; Gu, C. Bridging barriers: A comparative look at the blood-brain barrier across organisms. Genes Dev. 2018, 32, 466–478. [Google Scholar] [CrossRef]
- Ayloo, S.; Gu, C. Transcytosis at the blood-brain barrier. Curr. Opin. Neurobiol. 2019, 57, 32–38. [Google Scholar] [CrossRef]
- Obermeier, B.; Daneman, R.; Ransohoff, R.M. Development, maintenance and disruption of the blood-brain barrier. Nat. Med. 2013, 19, 1584–1596. [Google Scholar] [CrossRef]
- Pardridge, W.M. CSF, blood-brain barrier, and brain drug delivery. Expert Opin. Drug Deliv. 2016, 13, 963–975. [Google Scholar] [CrossRef]
- Liu, Y.; Cao, X. Characteristics and Significance of the Pre-metastatic Niche. Cancer Cell 2016, 30, 668–681. [Google Scholar] [CrossRef]
- Olson, E.M.; Abdel-Rasoul, M.; Maly, J.; Wu, C.S.; Lin, N.U.; Shapiro, C.L. Incidence and risk of central nervous system metastases as site of first recurrence in patients with HER2-positive breast cancer treated with adjuvant trastuzumab. Ann. Oncol. 2013, 24, 1526–1533. [Google Scholar] [CrossRef]
- Patil, T.; Smith, D.E.; Bunn, P.A.; Aisner, D.L.; Le, A.T.; Hancock, M.; Purcell, W.T.; Bowles, D.W.; Camidge, D.R.; Doebele, R.C. The Incidence of Brain Metastases in Stage IV ROS1-Rearranged Non-Small Cell Lung Cancer and Rate of Central Nervous System Progression on Crizotinib. J. Thorac. Oncol. 2018, 13, 1717–1726. [Google Scholar] [CrossRef]
- Schinkel, A.H.; Smit, J.J.; van Tellingen, O.; Beijnen, J.H.; Wagenaar, E.; van Deemter, L.; Mol, C.A.; van der Valk, M.A.; Robanus-Maandag, E.C.; te Riele, H.P.; et al. Disruption of the mouse mdr1a P-glycoprotein gene leads to a deficiency in the blood-brain barrier and to increased sensitivity to drugs. Cell 1994, 77, 491–502. [Google Scholar] [CrossRef]
- Sanchez-Covarrubias, L.; Slosky, L.M.; Thompson, B.J.; Davis, T.P.; Ronaldson, P.T. Transporters at CNS barrier sites: Obstacles or opportunities for drug delivery? Curr. Pharm. Des. 2014, 20, 1422–1449. [Google Scholar] [CrossRef]
- Wijaya, J.; Fukuda, Y.; Schuetz, J.D. Obstacles to Brain Tumor Therapy: Key ABC Transporters. Int. J. Mol. Sci. 2017, 18, 2544. [Google Scholar] [CrossRef]
- Soffietti, R.; Ahluwalia, M.; Lin, N.; Rudà, R. Management of brain metastases according to molecular subtypes. Nat. Rev. Neurol. 2020, 16, 557–574. [Google Scholar] [CrossRef]
- Lyle, L.T.; Lockman, P.R.; Adkins, C.E.; Mohammad, A.S.; Sechrest, E.; Hua, E.; Palmieri, D.; Liewehr, D.J.; Steinberg, S.M.; Kloc, W.; et al. Alterations in Pericyte Subpopulations Are Associated with Elevated Blood-Tumor Barrier Permeability in Experimental Brain Metastasis of Breast Cancer. Clin. Cancer Res. 2016, 22, 5287–5299. [Google Scholar] [CrossRef]
- Tiwary, S.; Morales, J.E.; Kwiatkowski, S.C.; Lang, F.F.; Rao, G.; McCarty, J.H. Metastatic Brain Tumors Disrupt the Blood-Brain Barrier and Alter Lipid Metabolism by Inhibiting Expression of the Endothelial Cell Fatty Acid Transporter Mfsd2a. Sci. Rep. 2018, 8, 8267. [Google Scholar] [CrossRef]
- Gril, B.; Paranjape, A.N.; Woditschka, S.; Hua, E.; Dolan, E.L.; Hanson, J.; Wu, X.; Kloc, W.; Izycka-Swieszewska, E.; Duchnowska, R.; et al. Reactive astrocytic S1P3 signaling modulates the blood-tumor barrier in brain metastases. Nat. Commun. 2018, 9, 2705. [Google Scholar] [CrossRef]
- Yonemori, K.; Tsuta, K.; Ono, M.; Shimizu, C.; Hirakawa, A.; Hasegawa, T.; Hatanaka, Y.; Narita, Y.; Shibui, S.; Fujiwara, Y. Disruption of the blood brain barrier by brain metastases of triple-negative and basal-type breast cancer but not HER2/neu-positive breast cancer. Cancer 2010, 116, 302–308. [Google Scholar] [CrossRef]
- Taskar, K.S.; Rudraraju, V.; Mittapalli, R.K.; Samala, R.; Thorsheim, H.R.; Lockman, J.; Gril, B.; Hua, E.; Palmieri, D.; Polli, J.W.; et al. Lapatinib distribution in HER2 overexpressing experimental brain metastases of breast cancer. Pharm. Res. 2012, 29, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.Y.; Friboulet, L.; Kodack, D.P.; Engstrom, L.D.; Li, Q.; West, M.; Tang, R.W.; Wang, H.; Tsaparikos, K.; Wang, J.; et al. PF-06463922, an ALK/ROS1 Inhibitor, Overcomes Resistance to First and Second Generation ALK Inhibitors in Preclinical Models. Cancer Cell 2015, 28, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Henry, M.N.; Chen, Y.; McFadden, C.D.; Simedrea, F.C.; Foster, P.J. In-vivo longitudinal MRI study: An assessment of melanoma brain metastases in a clinically relevant mouse model. Melanoma Res. 2015, 25, 127–137. [Google Scholar] [CrossRef]
- Kienast, Y.; von Baumgarten, L.; Fuhrmann, M.; Klinkert, W.E.; Goldbrunner, R.; Herms, J.; Winkler, F. Real-time imaging reveals the single steps of brain metastasis formation. Nat. Med. 2010, 16, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Murrell, D.H.; Hamilton, A.M.; Mallett, C.L.; van Gorkum, R.; Chambers, A.F.; Foster, P.J. Understanding Heterogeneity and Permeability of Brain Metastases in Murine Models of HER2-Positive Breast Cancer Through Magnetic Resonance Imaging: Implications for Detection and Therapy. Transl. Oncol. 2015, 8, 176–184. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arvanitis, C.D.; Askoxylakis, V.; Guo, Y.; Datta, M.; Kloepper, J.; Ferraro, G.B.; Bernabeu, M.O.; Fukumura, D.; McDannold, N.; Jain, R.K. Mechanisms of enhanced drug delivery in brain metastases with focused ultrasound-induced blood-tumor barrier disruption. Proc. Natl. Acad. Sci. USA 2018, 115, E8717–E8726. [Google Scholar] [CrossRef]
- Kodack, D.P.; Chung, E.; Yamashita, H.; Incio, J.; Duyverman, A.M.; Song, Y.; Farrar, C.T.; Huang, Y.; Ager, E.; Kamoun, W.; et al. Combined targeting of HER2 and VEGFR2 for effective treatment of HER2-amplified breast cancer brain metastases. Proc. Natl. Acad. Sci. USA 2012, 109, E3119–E3127. [Google Scholar] [CrossRef]
- Wyatt, E.A.; Davis, M.E. Method of establishing breast cancer brain metastases affects brain uptake and efficacy of targeted, therapeutic nanoparticles. Bioeng. Transl. Med. 2018, 4, 30–37. [Google Scholar] [CrossRef]
- Morikawa, A.; Peereboom, D.M.; Thorsheim, H.R.; Samala, R.; Balyan, R.; Murphy, C.G.; Lockman, P.R.; Simmons, A.; Weil, R.J.; Tabar, V.; et al. Capecitabine and lapatinib uptake in surgically resected brain metastases from metastatic breast cancer patients: A prospective study. Neuro Oncol. 2015, 17, 289–295. [Google Scholar] [CrossRef]
- Saleem, A.; Searle, G.E.; Kenny, L.M.; Huiban, M.; Kozlowski, K.; Waldman, A.D.; Woodley, L.; Palmieri, C.; Lowdell, C.; Kaneko, T.; et al. Lapatinib access into normal brain and brain metastases in patients with Her-2 overexpressing breast cancer. EJNMMI Res. 2015, 5, 1–10. [Google Scholar] [CrossRef]
- Lewis Phillips, G.D.; Nishimura, M.C.; Lacap, J.A.; Kharbanda, S.; Mai, E.; Tien, J.; Malesky, K.; Williams, S.P.; Marik, J.; Phillips, H.S. Trastuzumab uptake and its relation to efficacy in an animal model of HER2-positive breast cancer brain metastasis. Breast Cancer Res. Treat. 2017, 164, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Askoxylakis, V.; Ferraro, G.B.; Kodack, D.P.; Badeaux, M.; Shankaraiah, R.C.; Seano, G.; Kloepper, J.; Vardam, T.; Martin, J.D.; Naxerova, K.; et al. Preclinical Efficacy of Ado-trastuzumab Emtansine in the Brain Microenvironment. J. Natl. Cancer Inst. 2015, 108, djv313. [Google Scholar] [CrossRef] [PubMed]
- Kummar, S.; Rubinstein, L.; Kinders, R.; Parchment, R.E.; Gutierrez, M.E.; Murgo, A.J.; Ji, J.; Mroczkowski, B.; Pickeral, O.K.; Simpson, M.; et al. Phase 0 clinical trials: Conceptions and misconceptions. Cancer J. 2008, 14, 133–137. [Google Scholar] [CrossRef]
- Pellerino, A.; Bertero, L.; Rudà, R.; Soffietti, R. Neoplastic meningitis in solid tumors: From diagnosis to personalized treatments. Ther. Adv. Neurol. Disord. 2018, 11, 1756286418759618. [Google Scholar] [CrossRef]
- Chang, P.C.; Fischbein, N.J.; McCalmont, T.H.; Kashani-Sabet, M.; Zettersten, E.M.; Liu, A.Y.; Weissman, J.L. Perineural spread of malignant melanoma of the head and neck: Clinical and imaging features. AJNR Am. J. Neuroradiol. 2004, 25, 5–11. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ahn, J.H.; Lee, S.H.; Kim, S.; Joo, J.; Yoo, H.; Lee, S.H.; Shin, S.H.; Gwak, H.S. Risk for leptomeningeal seeding after resection for brain metastases: Implication of tumor location with mode of resection. J. Neurosurg. 2012, 116, 984–993. [Google Scholar] [CrossRef]
- Mahajan, A.; Ahmed, S.; McAleer, M.F.; Weinberg, J.S.; Li, J.; Brown, P.; Settle, S.; Prabhu, S.S.; Lang, F.F.; Levine, N.; et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: A single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1040–1048. [Google Scholar] [CrossRef]
- Foreman, P.M.; Jackson, B.E.; Singh, K.P.; Romeo, A.K.; Guthrie, B.L.; Fisher, W.S.; Riley, K.O.; Markert, J.M.; Willey, C.D.; Bredel, M.; et al. Postoperative radiosurgery for the treatment of metastatic brain tumor: Evaluation of local failure and leptomeningeal disease. J. Clin. Neurosci. 2018, 49, 48–55. [Google Scholar] [CrossRef]
- Boire, A.; Zou, Y.; Shieh, J.; Macalinao, D.G.; Pentsova, E.; Massagué, J. Complement Component 3 Adapts the Cerebrospinal Fluid for Leptomeningeal Metastasis. Cell 2017, 168, 1101–1113. [Google Scholar] [CrossRef]
- Conrad, C.; Dorzweiler, K.; Miller, M.A.; Lauffenburger, D.A.; Strik, H.; Bartsch, J.W. Profiling of metalloprotease activities in cerebrospinal fluids of patients with neoplastic meningitis. Fluids Barriers CNS 2017, 14, 22. [Google Scholar] [CrossRef]
- Chi, Y.; Remsik, J.; Kiseliovas, V.; Derderian, C.; Sener, U.; Alghader, M.; Saadeh, F.; Nikishina, K.; Bale, T.; Iacobuzio-Donahue, C.; et al. Cancer cells deploy lipocalin-2 to collect limiting iron in leptomeningeal metastasis. Science 2020, 369, 276–282. [Google Scholar] [CrossRef]
- Remsik, J.; Chi, Y.; Tong, X.; Sener, U.; Derderian, C.; Park, A.; Saadeh, F.; Bale, T.; Boire, A. Leptomeningeal metastatic cells adopt two phenotypic states. Cancer Rep. 2020, e1236. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, D.; Bronder, J.L.; Herring, J.M.; Yoneda, T.; Weil, R.J.; Stark, A.M.; Kurek, R.; Vega-Valle, E.; Feigenbaum, L.; Halverson, D.; et al. Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res. 2007, 67, 4190–4198. [Google Scholar] [CrossRef]
- Allen, J.E.; Patel, A.S.; Prabhu, V.V.; Dicker, D.T.; Sheehan, J.M.; Glantz, M.J.; El-Deiry, W.S. COX-2 drives metastatic breast cells from brain lesions into the cerebrospinal fluid and systemic circulation. Cancer Res. 2014, 74, 2385–2390. [Google Scholar] [CrossRef]
- Dankner, M.; Caron, M.; Al-Saadi, T.; Yu, W.; Ouellet, V.; Ezzeddine, R.; Maritan, S.M.; Annis, M.G.; Le, P.U.; Nadaf, J.; et al. Invasive growth associated with Cold-Inducible RNA-Binding Protein expression drives recurrence of surgically resected brain metastases. Neuro Oncol. 2021, noab002. [Google Scholar] [CrossRef] [PubMed]
- Nanjo, S.; Arai, S.; Wang, W.; Takeuchi, S.; Yamada, T.; Hata, A.; Katakami, N.; Okada, Y.; Yano, S. MET Copy Number Gain Is Associated with Gefitinib Resistance in Leptomeningeal Carcinomatosis of EGFR-mutant Lung Cancer. Mol. Cancer Ther. 2017, 16, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Balak, M.N.; Gong, Y.; Riely, G.J.; Somwar, R.; Li, A.R.; Zakowski, M.F.; Chiang, A.; Yang, G.; Ouerfelli, O.; Kris, M.G.; et al. Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors. Clin. Cancer Res. 2006, 12, 6494–6501. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Hu, M.; Zhu, X.; Wang, M.; Xu, Y.; Lv, X.; Xu, H.; Ding, J.; Ye, X.; Fang, L.; et al. Exploration of the underlying mechanisms of leptomeningeal metastasis in NSCLC patients through NGS of cerebrospinal fluid. J. Thorac. Oncol. 2017, 12, S271. [Google Scholar] [CrossRef][Green Version]
- Jiang, B.Y.; Yangsi, L.; Chuai, S.; Zhang, Z.; Yang, J.J.; Zhong, W.; Zhou, Q.; Wu, I.L. NGS to reveal heterogeneity between cerebrospinal fluid and plasma ctDNA among non-small cell lung cancer patients with leptomeningeal carcinomatosis. Proc. Am. Soc. Clin. Oncol. 2017, 35, 9022. [Google Scholar] [CrossRef]
- Oxnard, G.R.; Arcila, M.E.; Sima, C.S.; Riely, G.J.; Chmielecki, J.; Kris, M.G.; Pao, W.; Ladanyi, M.; Miller, V.A. Acquired resistance to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer: Distinct natural history of patients with tumors harboring the T790M mutation. Clin. Cancer Res. 2011, 17, 1616–1622. [Google Scholar] [CrossRef]
- Brastianos, P.K.; Carter, S.L.; Santagata, S.; Cahill, D.P.; Taylor-Weiner, A.; Jones, R.T.; Van Allen, E.M.; Lawrence, M.S.; Horowitz, P.M.; Cibulskis, K.; et al. Genomic Characterization of Brain Metastases Reveals Branched Evolution and Potential Therapeutic Targets. Cancer Discov. 2015, 5, 1164–1177. [Google Scholar] [CrossRef] [PubMed]
- Shih, D.J.H.; Nayyar, N.; Bihun, I.; Dagogo-Jack, I.; Gill, C.M.; Aquilanti, E.; Bertalan, M.; Kaplan, A.; D’Andrea, M.R.; Chukwueke, U.; et al. Genomic characterization of human brain metastases identifies drivers of metastatic lung adenocarcinoma. Nat. Genet. 2020, 52, 371–377. [Google Scholar] [CrossRef]
- Hohensee, I.; Lamszus, K.; Riethdorf, S.; Meyer-Staeckling, S.; Glatzel, M.; Matschke, J.; Witzel, I.; Westphal, M.; Brandt, B.; Müller, V.; et al. Frequent genetic alterations in EGFR- and HER2-driven pathways in breast cancer brain metastases. Am. J. Pathol. 2013, 183, 83–95. [Google Scholar] [CrossRef]
- Wikman, H.; Lamszus, K.; Detels, N.; Uslar, L.; Wrage, M.; Benner, C.; Hohensee, I.; Ylstra, B.; Eylmann, K.; Zapatka, M.; et al. Relevance of PTEN loss in brain metastasis formation in breast cancer patients. Breast Cancer Res. 2012, 14, R49. [Google Scholar] [CrossRef] [PubMed]
- Le Rhun, E.; Weller, M.; Brandsma, D.; Van den Bent, M.; de Azambuja, E.; Henriksson, R.; Boulanger, T.; Peters, S.; Watts, C.; Wick, W.; et al. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann. Oncol. 2017, 28, iv84–iv99. [Google Scholar] [CrossRef]
- Le Rhun, E.; Devos, P.; Weller, J.; Seystahl, K.; Mo, F.; Compter, A.; Berghoff, A.S.; Jongen, J.L.M.; Wolpert, F.; Rudà, R.; et al. Prognostic validation and clinical implications of the EANO ESMO classification of leptomeningeal metastasis from solid tumors. Neuro Oncol. 2020, noaa298. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, M.; Junck, L.; Brandsma, D.; Soffietti, R.; Rudà, R.; Raizer, J.; Boogerd, W.; Taillibert, S.; Groves, M.D.; Le Rhun, E.; et al. Leptomeningeal metastases: A RANO proposal for response criteria. Neuro Oncol. 2017, 19, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Le Rhun, E.; Devos, P.; Boulanger, T.; Smits, M.; Brandsma, D.; Rudà, R.; Furtner, J.; Hempel, J.M.; Postma, T.J.; Roth, P.; et al. The RANO Leptomeningeal Metastasis Group proposal to assess response to treatment: Lack of feasibility and clinical utility and a revised proposal. Neuro Oncol. 2019, 21, 648–658. [Google Scholar] [CrossRef]
- Prabhu, R.S.; Turner, B.E.; Asher, A.L.; Marcrom, S.R.; Fiveash, J.B.; Foreman, P.M.; Press, R.H.; Patel, K.R.; Curran, W.J.; Breen, W.G.; et al. A multi-institutional analysis of presentation and outcomes for leptomeningeal disease recurrence after surgical resection and radiosurgery for brain metastases. Neuro Oncol. 2019, 21, 1049–1059. [Google Scholar] [CrossRef]
- Turner, B.E.; Prabhu, R.S.; Burri, S.H.; Brown, P.D.; Pollom, E.L.; Milano, M.T.; Weiss, S.E.; Iv, M.; Fischbein, N.; Soliman, H.; et al. Nodular Leptomeningeal Disease-A Distinct Pattern of Recurrence After Postresection Stereotactic Radiosurgery for Brain Metastases: A Multi-institutional Study of Interobserver Reliability. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.K.; Sahgal, A.; Detsky, J.; Atenafu, E.G.; Myrehaug, S.; Tseng, C.L.; Husain, Z.; Heyn, C.; Maralani, P.; Ruschin, M.; et al. Predictors of leptomeningeal disease following hypofractionated stereotactic radiotherapy for intact and resected brain metastases. Neuro Oncol. 2020, 22, 84–93. [Google Scholar] [CrossRef]
- Morikawa, A.; Jordan, L.; Rozner, R.; Patil, S.; Boire, A.; Pentsova, E.; Seidman, A.D. Characteristics and Outcomes of Patients With Breast Cancer With Leptomeningeal Metastasis. Clin. Breast Cancer 2017, 17, 23–28. [Google Scholar] [CrossRef]
- Subirá, D.; Serrano, C.; Castañón, S.; Gonzalo, R.; Illán, J.; Pardo, J.; Martínez-García, M.; Millastre, E.; Aparisi, F.; Navarro, M.; et al. Role of flow cytometry immunophenotyping in the diagnosis of leptomeningeal carcinomatosis. Neuro Oncol. 2012, 14, 43–52. [Google Scholar] [CrossRef]
- Nayak, L.; Fleisher, M.; Gonzalez-Espinoza, R.; Lin, O.; Panageas, K.; Reiner, A.; Liu, C.M.; Deangelis, L.M.; Omuro, A. Rare cell capture technology for the diagnosis of leptomeningeal metastasis in solid tumors. Neurology 2013, 80, 1598–1605. [Google Scholar] [CrossRef] [PubMed]
- Subirá, D.; Simó, M.; Illán, J.; Serrano, C.; Castañón, S.; Gonzalo, R.; Granizo, J.J.; Martínez-García, M.; Navarro, M.; Pardo, J.; et al. Diagnostic and prognostic significance of flow cytometry immunophenotyping in patients with leptomeningeal carcinomatosis. Clin. Exp. Metastasis 2015, 32, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Melisko, M.E.; Magbanua, M.J.; Kablanian, A.T.; Scott, J.H.; Rugo, H.S.; Park, J.W. Detection of cerebrospinal fluid tumor cells and its clinical relevance in leptomeningeal metastasis of breast cancer. Breast Cancer Res. Treat. 2015, 154, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Tu, Q.; Wu, X.; Le Rhun, E.; Blonski, M.; Wittwer, B.; Taillandier, L.; De Carvalho Bittencourt, M.; Faure, G.C. CellSearch technology applied to the detection and quantification of tumor cells in CSF of patients with lung cancer leptomeningeal metastasis. Lung Cancer 2015, 90, 352–357. [Google Scholar] [CrossRef]
- Milojkovic Kerklaan, B.; Pluim, D.; Bol, M.; Hofland, I.; Westerga, J.; van Tinteren, H.; Beijnen, J.H.; Boogerd, W.; Schellens, J.H.; Brandsma, D. EpCAM-based flow cytometry in cerebrospinal fluid greatly improves diagnostic accuracy of leptomeningeal metastases from epithelial tumors. Neuro Oncol. 2016, 18, 855–862. [Google Scholar] [CrossRef]
- Glantz, M.J.; Cole, B.F.; Glantz, L.K.; Cobb, J.; Mills, P.; Lekos, A.; Walters, B.C.; Recht, L.D. Cerebrospinal fluid cytology in patients with cancer: Minimizing false-negative results. Cancer 1998, 82, 733–739. [Google Scholar] [CrossRef]
- van Bussel, M.T.J.; Pluim, D.; Bol, M.; Beijnen, J.H.; Schellens, J.H.M.; Brandsma, D. EpCAM-based assays for epithelial tumor cell detection in cerebrospinal fluid. J. Neurooncol. 2018, 137, 1–10. [Google Scholar] [CrossRef]
- Campoli, M.R.; Chang, C.C.; Kageshita, T.; Wang, X.; McCarthy, J.B.; Ferrone, S. Human high molecular weight-melanoma-associated antigen (HMW-MAA): A melanoma cell surface chondroitin sulfate proteoglycan (MSCP) with biological and clinical significance. Crit. Rev. Immunol. 2004, 24, 267–296. [Google Scholar] [CrossRef]
- Le Rhun, E.; Tu, Q.; De Carvalho Bittencourt, M.; Farre, I.; Mortier, L.; Cai, H.; Kohler, C.; Faure, G.C. Detection and quantification of CSF malignant cells by the CellSearch technology in patients with melanoma leptomeningeal metastasis. Med. Oncol. 2013, 30, 538. [Google Scholar] [CrossRef] [PubMed]
- Hyun, K.A.; Koo, G.B.; Han, H.; Sohn, J.; Choi, W.; Kim, S.I.; Jung, H.I.; Kim, Y.S. Epithelial-to-mesenchymal transition leads to loss of EpCAM and different physical properties in circulating tumor cells from metastatic breast cancer. Oncotarget 2016, 7, 24677–24687. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.S.; Allen, J.E.; Dicker, D.T.; Peters, K.L.; Sheehan, J.M.; Glantz, M.J.; El-Deiry, W.S. Identification and enumeration of circulating tumor cells in the cerebrospinal fluid of breast cancer patients with central nervous system metastases. Oncotarget 2011, 2, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Nevel, K.S.; DiStefano, N.; Lin, X.; Skakodub, A.; Ogilvie, S.Q.; Reiner, A.S.; Pentsova, E.; Boire, A. A retrospective, quantitative assessment of disease burden in patients with leptomeningeal metastases from non-small-cell lung cancer. Neuro Oncol. 2020, 22, 675–683. [Google Scholar] [CrossRef]
- Jiang, B.Y.; Li, Y.S.; Guo, W.B.; Zhang, X.C.; Chen, Z.H.; Su, J.; Zhong, W.Z.; Yang, X.N.; Yang, J.J.; Shao, Y.; et al. Detection of Driver and Resistance Mutations in Leptomeningeal Metastases of NSCLC by Next-Generation Sequencing of Cerebrospinal Fluid Circulating Tumor Cells. Clin. Cancer Res. 2017, 23, 5480–5488. [Google Scholar] [CrossRef] [PubMed]
- Magbanua, M.J.; Melisko, M.; Roy, R.; Sosa, E.V.; Hauranieh, L.; Kablanian, A.; Eisenbud, L.E.; Ryazantsev, A.; Au, A.; Scott, J.H.; et al. Molecular profiling of tumor cells in cerebrospinal fluid and matched primary tumors from metastatic breast cancer patients with leptomeningeal carcinomatosis. Cancer Res. 2013, 73, 7134–7143. [Google Scholar] [CrossRef]
- Li, X.; Zhang, Y.; Ding, J.; Wang, M.; Li, N.; Yang, H.; Wang, K.; Wang, D.; Ping Lin, P.; Li, M.; et al. Clinical significance of detecting CSF-derived tumor cells in breast cancer patients with leptomeningeal metastasis. Oncotarget 2018, 9, 2705–2714. [Google Scholar] [CrossRef]
- Cordone, I.; Masi, S.; Summa, V.; Carosi, M.; Vidiri, A.; Fabi, A.; Pasquale, A.; Conti, L.; Rosito, I.; Carapella, C.M.; et al. Overexpression of syndecan-1, MUC-1, and putative stem cell markers in breast cancer leptomeningeal metastasis: A cerebrospinal fluid flow cytometry study. Breast Cancer Res. 2017, 19, 46. [Google Scholar] [CrossRef]
- Le Rhun, E.; Massin, F.; Tu, Q.; Bonneterre, J.; Bittencourt Mde, C.; Faure, G.C. Development of a new method for identification and quantification in cerebrospinal fluid of malignant cells from breast carcinoma leptomeningeal metastasis. BMC Clin. Pathol. 2012, 12, 21. [Google Scholar] [CrossRef]
- Acosta, M.; Pereira, J.; Arroz, M. Screening of carcinoma metastasis by flow cytometry: A study of 238 cases. Cytom. B Clin. Cytom. 2016, 90, 289–294. [Google Scholar] [CrossRef]
- Ma, C.; Lv, Y.; Jiang, R.; Li, J.; Wang, B.; Sun, L. Novel method for the detection and quantification of malignant cells in the CSF of patients with leptomeningeal metastasis of lung cancer. Oncol. Lett. 2016, 11, 619–623. [Google Scholar] [CrossRef]
- Lin, X.; Fleisher, M.; Rosenblum, M.; Lin, O.; Boire, A.; Briggs, S.; Bensman, Y.; Hurtado, B.; Shagabayeva, L.; DeAngelis, L.M.; et al. Cerebrospinal fluid circulating tumor cells: A novel tool to diagnose leptomeningeal metastases from epithelial tumors. Neuro Oncol. 2017, 19, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- van Bussel, M.T.J.; Pluim, D.; Milojkovic Kerklaan, B.; Bol, M.; Sikorska, K.; Linders, D.T.C.; van den Broek, D.; Beijnen, J.H.; Schellens, J.H.M.; Brandsma, D. Circulating epithelial tumor cell analysis in CSF in patients with leptomeningeal metastases. Neurology 2020, 94, e521–e528. [Google Scholar] [CrossRef]
- Malani, R.; Fleisher, M.; Kumthekar, P.; Lin, X.; Omuro, A.; Groves, M.D.; Lin, N.U.; Melisko, M.; Lassman, A.B.; Jeyapalan, S.; et al. Cerebrospinal fluid circulating tumor cells as a quantifiable measurement of leptomeningeal metastases in patients with HER2 positive cancer. J. Neurooncol. 2020, 148, 599–606. [Google Scholar] [CrossRef] [PubMed]
- De Mattos-Arruda, L.; Mayor, R.; Ng, C.K.Y.; Weigelt, B.; Martínez-Ricarte, F.; Torrejon, D.; Oliveira, M.; Arias, A.; Raventos, C.; Tang, J.; et al. Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat. Commun. 2015, 6, 8839. [Google Scholar] [CrossRef] [PubMed]
- Momtaz, P.; Pentsova, E.; Abdel-Wahab, O.; Diamond, E.; Hyman, D.; Merghoub, T.; You, D.; Gasmi, B.; Viale, A.; Chapman, P.B. Quantification of tumor-derived cell free DNA(cfDNA) by digital PCR (DigPCR) in cerebrospinal fluid of patients with BRAFV600 mutated malignancies. Oncotarget 2016, 7, 85430–85436. [Google Scholar] [CrossRef] [PubMed]
- Pentsova, E.I.; Shah, R.H.; Tang, J.; Boire, A.; You, D.; Briggs, S.; Omuro, A.; Lin, X.; Fleisher, M.; Grommes, C.; et al. Evaluating Cancer of the Central Nervous System Through Next-Generation Sequencing of Cerebrospinal Fluid. J. Clin. Oncol. 2016, 34, 2404–2415. [Google Scholar] [CrossRef]
- Marchiò, C.; Mariani, S.; Bertero, L.; Di Bello, C.; Francia Di Celle, P.; Papotti, M.; Rudà, R.; Soffietti, R.; Cassoni, P. Liquoral liquid biopsy in neoplastic meningitis enables molecular diagnosis and mutation tracking: A proof of concept. Neuro Oncol. 2017, 19, 451–453. [Google Scholar] [CrossRef][Green Version]
- Swinkels, D.W.; de Kok, J.B.; Hanselaar, A.; Lamers, K.; Boerman, R.H. Early detection of leptomeningeal metastasis by PCR examination of tumor-derived K-ras DNA in cerebrospinal fluid. Clin. Chem. 2000, 46, 132–133. [Google Scholar] [CrossRef]
- Fan, Y.; Zhu, X.; Xu, Y.; Lu, X.; Xu, Y.; Wang, M.; Xu, H.; Ding, J.; Ye, X.; Fang, L.; et al. Cell-Cycle and DNA-Damage Response Pathway Is Involved in Leptomeningeal Metastasis of Non-Small Cell Lung Cancer. Clin. Cancer Res. 2018, 24, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.S.; Jiang, B.Y.; Yang, J.J.; Zhang, X.C.; Zhang, Z.; Ye, J.Y.; Zhong, W.Z.; Tu, H.Y.; Chen, H.J.; Wang, Z.; et al. Unique genetic profiles from cerebrospinal fluid cell-free DNA in leptomeningeal metastases of EGFR-mutant non-small-cell lung cancer: A new medium of liquid biopsy. Ann. Oncol. 2018, 29, 945–952. [Google Scholar] [CrossRef]
- Boire, A.; Brandsma, D.; Brastianos, P.K.; Le Rhun, E.; Ahluwalia, M.; Junck, L.; Glantz, M.; Groves, M.D.; Lee, E.Q.; Lin, N.; et al. Liquid biopsy in central nervous system metastases: A RANO review and proposals for clinical applications. Neuro Oncol. 2019, 21, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Xu, X.; Li, D.; Chen, K.; Zhan, Q.; Ge, M.; Zhou, X.; Liang, X.; Guan, M. Digital PCR-Based Detection of EGFR Mutations in Paired Plasma and CSF Samples of Lung Adenocarcinoma Patients with Central Nervous System Metastases. Target. Oncol. 2019, 14, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Yang, X.; Xing, W.; Yu, H.; Si, T.; Guo, Z. Detection of circulating tumor DNA from non-small cell lung cancer brain metastasis in cerebrospinal fluid samples. Thorac. Cancer 2020, 11, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xie, Y.; Lin, Y.; Yu, T.; Yin, Z. Different Gene Mutation Spectrum of the Paired CSF and Plasma Samples in Lung Adenocarcinoma with Leptomeningeal Metastases: The Liquid Biopsy Based on Circulating Tumor DNA. Chin. J. Lung Cancer 2020, 23, 646–654. [Google Scholar] [CrossRef]
- Zheng, M.M.; Li, Y.S.; Tu, H.Y.; Jiang, B.Y.; Yang, J.J.; Zhou, Q.; Xu, C.R.; Yang, X.R.; Wu, Y.L. Genotyping of Cerebrospinal Fluid Associated With Osimertinib Response and Resistance for Leptomeningeal Metastases in EGFR-Mutated NSCLC. J. Thorac. Oncol. 2021, 16, 250–258. [Google Scholar] [CrossRef]
- Carausu, M.; Melaabi, S.; Pierga, J.Y.; Bidard, F.C.; Cabel, L. ESR1 Mutation Detection and Dynamics in Meningeal Carcinomatosis in Breast Cancer. J. Breast Cancer 2019, 23, 218–223. [Google Scholar] [CrossRef]
- Angus, L.; Deger, T.; Jager, A.; Martens, J.W.M.; de Weerd, V.; van Heuvel, I.; van den Bent, M.J.; Sillevis Smitt, P.A.; Kros, J.M.; Bindels, E.M.; et al. Detection of aneuploidy in cerebrospinal fluid from patients with breast cancer can improve diagnosis of leptomeningeal metastases. Clin. Cancer Res. 2021, 27, 2798–2806. [Google Scholar] [CrossRef]
- Ballester, L.Y.; Glitza Oliva, I.C.; Douse, D.Y.; Chen, M.M.; Lan, C.; Haydu, L.E.; Huse, J.T.; Roy-Chowdhuri, S.; Luthra, R.; Wistuba, I.I.; et al. Evaluating Circulating Tumor DNA From the Cerebrospinal Fluid of Patients With Melanoma and Leptomeningeal Disease. J. Neuropathol. Exp. Neurol. 2018, 77, 628–635. [Google Scholar] [CrossRef]
- Smalley, I.; Law, V.; Wyatt, C.; Evernden, B.; Fang, B.; Koomen, J.M.; Welsh, E.A.; Macaulay, R.J.B.; Forsyth, P.A.; Smalley, K.S.M. Proteomic Analysis of CSF from Patients with Leptomeningeal Melanoma Metastases Identifies Signatures Associated with Disease Progression and Therapeutic Resistance. Clin. Cancer Res. 2020, 26, 2163–2175. [Google Scholar] [CrossRef] [PubMed]
- Gani, C.; Müller, A.C.; Eckert, F.; Schroeder, C.; Bender, B.; Pantazis, G.; Bamberg, M.; Berger, B. Outcome after whole brain radiotherapy alone in intracranial leptomeningeal carcinomatosis from solid tumors. Strahlenther. Onkol. 2012, 188, 148–153. [Google Scholar] [CrossRef]
- Brower, J.V.; Saha, S.; Rosenberg, S.A.; Hullett, C.R.; Ian Robins, H. Management of leptomeningeal metastases: Prognostic factors and associated outcomes. J. Clin. Neurosci. 2016, 27, 130–137. [Google Scholar] [CrossRef] [PubMed]
- El Shafie, R.A.; Böhm, K.; Weber, D.; Lang, K.; Schlaich, F.; Adeberg, S.; Paul, A.; Haefner, M.F.; Katayama, S.; Sterzing, F.; et al. Outcome and prognostic factors following palliative craniospinal irradiation for leptomeningeal carcinomatosis. Cancer Manag. Res. 2019, 11, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Devecka, M.; Duma, M.N.; Wilkens, J.J.; Kampfer, S.; Borm, K.J.; Münch, S.; Straube, C.; Combs, S.E. Craniospinal irradiation (CSI) in patients with leptomeningeal metastases: Risk-benefit-profile and development of a prognostic score for decision making in the palliative setting. BMC Cancer 2020, 20, 501. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.J.; Wijetunga, N.A.; Yamada, J.; Wolden, S.; Mehallow, M.; Goldman, D.A.; Zhang, Z.; Young, R.J.; Kris, M.G.; Yu, H.A.; et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol. 2021, 23, 134–143. [Google Scholar] [CrossRef]
- Li, Y.S.; Jiang, B.Y.; Yang, J.J.; Tu, H.Y.; Zhou, Q.; Guo, W.B.; Yan, H.H.; Wu, Y.L. Leptomeningeal Metastases in Patients with NSCLC with EGFR Mutations. J. Thorac. Oncol. 2016, 11, 1962–1969. [Google Scholar] [CrossRef]
- Kuiper, J.L.; Hendriks, L.E.; van der Wekken, A.J.; de Langen, A.J.; Bahce, I.; Thunnissen, E.; Heideman, D.A.; Berk, Y.; Buijs, E.J.; Speel, E.J.; et al. Treatment and survival of patients with EGFR-mutated non-small cell lung cancer and leptomeningeal metastasis: A retrospective cohort analysis. Lung Cancer 2015, 89, 255–261. [Google Scholar] [CrossRef]
- Grommes, C.; Oxnard, G.R.; Kris, M.G.; Miller, V.A.; Pao, W.; Holodny, A.I.; Clarke, J.L.; Lassman, A.B. “Pulsatile” high-dose weekly erlotinib for CNS metastases from EGFR mutant non-small cell lung cancer. Neuro Oncol. 2011, 13, 1364–1369. [Google Scholar] [CrossRef]
- Lee, E.; Keam, B.; Kim, D.W.; Kim, T.M.; Lee, S.H.; Chung, D.H.; Heo, D.S. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer. J. Thorac. Oncol. 2013, 8, 1069–1074. [Google Scholar] [CrossRef]
- Yang, H.; Yang, X.; Zhang, Y.; Liu, X.; Deng, Q.; Zhao, M.; Xu, X.; He, J. Erlotinib in combination with pemetrexed/cisplatin for leptomeningeal metastases and cerebrospinal fluid drug concentrations in lung adenocarcinoma patients after gefitinib failure. Target. Oncol. 2015, 10, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, T.; Hata, A.; Takeshita, J.; Fujita, S.; Hayashi, M.; Tomii, K.; Katakami, N. High-dose erlotinib for refractory leptomeningeal metastases after failure of standard-dose EGFR-TKIs. Cancer Chemother. Pharmacol. 2015, 75, 1261–1266. [Google Scholar] [CrossRef] [PubMed]
- Jackman, D.M.; Cioffredi, L.A.; Jacobs, L.; Sharmeen, F.; Morse, L.K.; Lucca, J.; Plotkin, S.R.; Marcoux, P.J.; Rabin, M.S.; Lynch, T.J.; et al. A phase I trial of high dose gefitinib for patients with leptomeningeal metastases from non-small cell lung cancer. Oncotarget 2015, 6, 4527–4536. [Google Scholar] [CrossRef] [PubMed]
- Tamiya, A.; Tamiya, M.; Nishihara, T.; Shiroyama, T.; Nakao, K.; Tsuji, T.; Takeuchi, N.; Isa, S.I.; Omachi, N.; Okamoto, N.; et al. Cerebrospinal Fluid Penetration Rate and Efficacy of Afatinib in Patients with EGFR Mutation-positive Non-small Cell Lung Cancer with Leptomeningeal Carcinomatosis: A Multicenter Prospective Study. Anticancer. Res. 2017, 37, 4177–4182. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.C.; Cho, B.C.; Kim, D.; Kim, S.W.; Lee, J.S.; Su, W.C.; John, T.; Chuan-Hao Kao, S.; Natale, R.; Wadeet, T.; et al. Osimertinib for patients (pts) with leptomeningeal metastases (LM) from EGFR-mutant non-small cell lung cancer (NSCLC): Updated results from the BLOOM study. Proc. Am. Soc. Clin. Oncol. 2017, 35, 2020. [Google Scholar] [CrossRef]
- Nanjo, S.; Hata, A.; Okuda, C.; Kaji, R.; Okada, H.; Tamura, D.; Irie, K.; Okada, H.; Fukushima, S.; Katakami, N. Standard-dose osimertinib for refractory leptomeningeal metastases in T790M-positive EGFR-mutant non-small cell lung cancer. Br. J. Cancer 2018, 118, 32–37. [Google Scholar] [CrossRef]
- Yang, J.C.H.; Kim, S.W.; Kim, D.W.; Lee, J.S.; Cho, B.C.; Ahn, J.S.; Lee, D.H.; Kim, T.M.; Goldman, J.W.; Natale, R.B.; et al. Osimertinib in Patients With Epidermal Growth Factor Receptor Mutation-Positive Non-Small-Cell Lung Cancer and Leptomeningeal Metastases: The BLOOM Study. J. Clin. Oncol. 2020, 38, 538–547. [Google Scholar] [CrossRef]
- Saboundji, K.; Auliac, J.B.; Pérol, M.; François, G.; Janicot, H.; Marcq, M.; Dubos-Arvis, C.; Renault, A.; Guisier, F.; Odier, L.; et al. Efficacy of Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer with Leptomeningeal Metastases Pretreated with EGFR-Tyrosine Kinase Inhibitors. Target. Oncol. 2018, 13, 501–507. [Google Scholar] [CrossRef]
- Ahn, M.J.; Chiu, C.H.; Cheng, Y.; Han, J.Y.; Goldberg, S.B.; Greystoke, A.; Crawford, J.; Zhao, Y.; Huang, X.; Johnson, M.; et al. Osimertinib for Patients With Leptomeningeal Metastases Associated With EGFR T790M-Positive Advanced NSCLC: The AURA Leptomeningeal Metastases Analysis. J. Thorac. Oncol. 2020, 15, 637–648. [Google Scholar] [CrossRef]
- Park, S.; Lee, M.H.; Seong, M.; Kim, S.T.; Kang, J.H.; Cho, B.C.; Lee, K.H.; Cho, E.K.; Sun, J.M.; Lee, S.H.; et al. A phase II, multicenter, two cohort study of 160 mg osimertinib in EGFR T790M-positive non-small-cell lung cancer patients with brain metastases or leptomeningeal disease who progressed on prior EGFR TKI therapy. Ann. Oncol. 2020, 31, 1397–1404. [Google Scholar] [CrossRef]
- Lee, J.; Choi, Y.; Han, J.; Park, S.; Jung, H.A.; Su, J.M.; Lee, S.H.; Ahn, J.S.; Park, K.; Ahn, M.J. Osimertinib Improves Overall Survival in Patients With EGFR-Mutated NSCLC With Leptomeningeal Metastases Regardless of T790M Mutational Status. J. Thorac. Oncol. 2020, 15, 1758–1766. [Google Scholar] [CrossRef] [PubMed]
- Okuno, T.; Arakawa, S.; Yoshida, T.; Ohe, Y. Efficacy of osimertinib in a patient with leptomeningeal metastasis and EGFR uncommon S768I mutation. Lung Cancer 2020, 143, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Yu, T.; Lin, Y.; Xie, Y.; Feng, J.; Huang, M.; Guo, A.; Liu, X.; Yin, Z. Three Novel EGFR Mutations (750_758del, I759S, T751_I759delinsS) in One Patient with Metastatic Non-Small Cell Lung Cancer Responding to Osimertinib: A Case Report. OncoTargets Ther. 2020, 13, 7941–7948. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.C.; Ohe, Y.; Vansteenkiste, J.; Reungwetwattana, T.; Chewaskulyong, B.; Lee, K.H.; Dechaphunkul, A.; Imamura, F.; Nogami, N.; Kurata, T.; et al. Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Keam, B.; Ock, C.Y.; Kim, M.; Kim, T.M.; Kim, D.W.; Heo, D.S. Pemetrexed in the Treatment of Leptomeningeal Metastasis in Patients With EGFR-mutant Lung Cancer. Clin. Lung Cancer 2019, 20, e442–e451. [Google Scholar] [CrossRef] [PubMed]
- Jänne, P.; Planchard, D.; Howarth, P.; Todd, A.; Kobayashidoi, K. OA07.01 Osimertinib Plus Platinum/Pemetrexed in Newly Diagnosed Advanced EGFRm-Positive NSCLC; The Phase 3 FLAURA2 Study. J. Thorac. Oncol. 2019, 14, S222–S223. [Google Scholar] [CrossRef]
- Jing, W.; Wang, H.; Kong, L.; Yu, J.; Zhu, H. Great efficacy of bevacizumab plus erlotinib for leptomeningeal metastases from non-small cell lung cancer with initially positive EGFR mutation: A case report. Cancer Biol. Ther. 2018, 19, 1073–1077. [Google Scholar] [CrossRef]
- Jiang, T.; Xu, X.; Chen, X.; Ding, N.; Hu, Q.; Zhou, C.; Hu, J. Osimertinib in combination with bevacizumab in EGFR-Mutated NSCLC with leptomeningeal metastases. Transl. Lung Cancer Res. 2020, 9, 2514–2517. [Google Scholar] [CrossRef]
- Liao, B.C.; Lee, J.H.; Lin, C.C.; Chen, Y.F.; Chang, C.H.; Ho, C.C.; Shih, J.Y.; Yu, C.J.; Yang, J.C. Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors for Non-Small-Cell Lung Cancer Patients with Leptomeningeal Carcinomatosis. J. Thorac. Oncol. 2015, 10, 1754–1761. [Google Scholar] [CrossRef]
- Ahn, M.J.; Kim, D.W.; Cho, B.C.; Kim, S.W.; Lee, J.S.; Ahn, J.S.; Kim, T.M.; Lin, C.C.; Kim, H.R.; John, T.; et al. Activity and safety of AZD3759 in EGFR-mutant non-small-cell lung cancer with CNS metastases (BLOOM): A phase 1, open-label, dose-escalation and dose-expansion study. Lancet Respir. Med. 2017, 5, 891–902. [Google Scholar] [CrossRef]
- Cho, B.C.; Ahn, M.; Lee, J.; Kim, D.W.; Kim, S.W.; John, T.; Kao, S.C.-H.; Goldman, J.W.; Su, W.-C.; Natale, R.B.; et al. Phase I study (BLOOM) of AZD3759, a BBB penetrable EGFR inhibitor, in EGFRm NSCLC patients with leptomeningeal metastasis (LM) who progressed after other anticancer therapy. J. Clin. Oncol. 2017, 35, 2069. [Google Scholar] [CrossRef]
- Xu, H.; Zhou, L.; Lu, Y.; Su, X.; Cheng, P.; Li, D.; Gao, H.; Li, H.; Yuan, W.; Zhang, L.; et al. Dual Targeting of the Epidermal Growth Factor Receptor Using Combination of Nimotuzumab and Erlotinib in Advanced Non-Small-Cell Lung Cancer with Leptomeningeal Metastases: A Report of Three Cases. OncoTargets Ther. 2020, 13, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.B.; Kobayashi, S.; Pandya, S.S.; Yeo, W.L.; Shen, Z.; Tan, W.; Wilner, K.D. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J. Clin. Oncol. 2011, 29, e443–e445. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.K.; Han, B.; Lee, S.J.; Lim, T.; Sun, J.M.; Ahn, J.S.; Ahn, M.J.; Park, K. ALK inhibitor crizotinib combined with intrathecal methotrexate treatment for non-small cell lung cancer with leptomeningeal carcinomatosis. Lung Cancer 2012, 76, 253–254. [Google Scholar] [CrossRef]
- Arrondeau, J.; Ammari, S.; Besse, B.; Soria, J.C. LDK378 compassionate use for treating carcinomatous meningitis in an ALK translocated non-small-cell lung cancer. J. Thorac. Oncol. 2014, 9, e62–e63. [Google Scholar] [CrossRef] [PubMed]
- Dudnik, E.; Siegal, T.; Zach, L.; Allen, A.M.; Flex, D.; Yust-Katz, S.; Limon, D.; Hirsch, F.R.; Peled, N. Durable brain response with pulse-dose crizotinib and ceritinib in ALK-positive non-small cell lung cancer compared with brain radiotherapy. J. Clin. Neurosci. 2016, 26, 46–49. [Google Scholar] [CrossRef]
- Gainor, J.F.; Sherman, C.A.; Willoughby, K.; Logan, J.; Kennedy, E.; Brastianos, P.K.; Chi, A.S.; Shaw, A.T. Alectinib salvages CNS relapses in ALK-positive lung cancer patients previously treated with crizotinib and ceritinib. J. Thorac. Oncol. 2015, 10, 232–236. [Google Scholar] [CrossRef]
- Ou, S.H.; Sommers, K.R.; Azada, M.C.; Garon, E.B. Alectinib induces a durable (>15 months) complete response in an ALK-positive non-small cell lung cancer patient who progressed on crizotinib with diffuse leptomeningeal carcinomatosis. Oncologist 2015, 20, 224–226. [Google Scholar] [CrossRef]
- Gainor, J.F.; Chi, A.S.; Logan, J.; Hu, R.; Oh, K.S.; Brastianos, P.K.; Shih, H.A.; Shaw, A.T. Alectinib Dose Escalation Reinduces Central Nervous System Responses in Patients with Anaplastic Lymphoma Kinase-Positive Non-Small Cell Lung Cancer Relapsing on Standard Dose Alectinib. J. Thorac. Oncol. 2016, 11, 256–260. [Google Scholar] [CrossRef]
- Gaye, E.; Geier, M.; Bore, P.; Guilloïque, M.; Lucia, F.; Quéré, G.; Gouva, S.; Robinet, G.; Descourt, R. Intra-cranial efficacy of brigatinib in an ALK-positive non-small cell lung cancer patient presenting leptomeningeal carcinomatosis. Lung Cancer 2019, 133, 1–3. [Google Scholar] [CrossRef]
- Pellerino, A.; Buffoni, L.; Rudà, R.; Soffietti, R. Complete response of spinal metastases from non-small cell lung cancer with ALK inhibitors. Neurology 2019, 93, 217–219. [Google Scholar] [CrossRef]
- Frost, N.; Christopoulos, P.; Kauffmann-Guerrero, D.; Stratmann, J.; Riedel, R.; Schaefer, M.; Alt, J.; Gütz, S.; Christoph, D.C.; Laack, E.; et al. Lorlatinib in pretreated ALK- or ROS1-positive lung cancer and impact of TP53 co-mutations: Results from the German early access program. Ther. Adv. Med. Oncol. 2021, 13, 1758835920980558. [Google Scholar] [CrossRef]
- Gainor, J.F.; Ou, S.H.; Logan, J.; Borges, L.F.; Shaw, A.T. The central nervous system as a sanctuary site in ALK-positive non-small-cell lung cancer. J. Thorac. Oncol. 2013, 8, 1570–1573. [Google Scholar] [CrossRef]
- Crinò, L.; Ahn, M.J.; De Marinis, F.; Groen, H.J.; Wakelee, H.; Hida, T.; Mok, T.; Spigel, D.; Felip, E.; Nishio, M.; et al. Multicenter Phase II Study of Whole-Body and Intracranial Activity With Ceritinib in Patients With ALK-Rearranged Non-Small-Cell Lung Cancer Previously Treated With Chemotherapy and Crizotinib: Results From ASCEND-2. J. Clin. Oncol. 2016, 34, 2866–2873. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Kim, T.M.; Crinò, L.; Gridelli, C.; Kiura, K.; Liu, G.; Novello, S.; Bearz, A.; Gautschi, O.; Mok, T.; et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017, 18, 874–886. [Google Scholar] [CrossRef]
- Chow, L.Q.; Barlesi, F.; Bertino, E.M.; van den Bent, M.J.; Wakelee, H.; Wen, P.Y.; Chiu, C.H.; Orlov, S.; Majem, M.; Chiari, R.; et al. Results of the ASCEND-7 phase II study evaluating ALK inhibitor ceritinib in patients with ALK+ non-small cell lung cancer metastatic to the brain. Ann. Oncol. 2019, 30, v602–v603. [Google Scholar] [CrossRef]
- Camidge, D.R.; Dziadziuszko, R.; Peters, S.; Mok, T.; Noe, J.; Nowicka, M.; Gadgeel, S.M.; Cheema, P.; Pavlakis, N.; de Marinis, F.; et al. Updated Efficacy and Safety Data and Impact of the EML4-ALK Fusion Variant on the Efficacy of Alectinib in Untreated ALK-Positive Advanced Non-Small Cell Lung Cancer in the Global Phase III ALEX Study. J. Thorac. Oncol. 2019, 14, 1233–1243. [Google Scholar] [CrossRef] [PubMed]
- Camidge, D.R.; Kim, H.R.; Ahn, M.J.; Yang, J.C.H.; Han, J.Y.; Hochmair, M.J.; Lee, K.H.; Delmonte, A.; García Campelo, M.R.; Kim, D.W.; et al. Brigatinib Versus Crizotinib in Advanced ALK Inhibitor-Naive ALK-Positive Non-Small Cell Lung Cancer: Second Interim Analysis of the Phase III ALTA-1L Trial. J. Clin. Oncol. 2020, 38, 3592–3603. [Google Scholar] [CrossRef] [PubMed]
- Ando, K.; Akimoto, K.; Sato, H.; Manabe, R.; Kishino, Y.; Homma, T.; Kusumoto, S.; Yamaoka, T.; Tanaka, A.; Ohmori, T.; et al. Brigatinib and Alectinib for ALK Rearrangement-Positive Advanced Non-Small Cell Lung Cancer With or Without Central Nervous System Metastasis: A Systematic Review and Network Meta-Analysis. Cancers 2020, 12, 942. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Solomon, B.J.; Chiari, R.; Riely, G.J.; Besse, B.; Soo, R.A.; Kao, S.; Lin, C.C.; Bauer, T.M.; Clancy, J.S.; et al. Lorlatinib in advanced ROS1-positive non-small-cell lung cancer: A multicentre, open-label, single-arm, phase 1-2 trial. Lancet Oncol. 2019, 20, 1691–1701. [Google Scholar] [CrossRef]
- Shaw, A.T.; Bauer, T.M.; de Marinis, F.; Felip, E.; Goto, Y.; Liu, G.; Mazieres, J.; Kim, D.W.; Mok, T.; Polli, A.; et al. First-Line Lorlatinib or Crizotinib in Advanced ALK-Positive Lung Cancer. N. Engl. J. Med. 2020, 383, 2018–2029. [Google Scholar] [CrossRef]
- Cardoso, F.; Paluch-Shimon, S.; Senkus, E.; Curigliano, G.; Aapro, M.S.; André, F.; Barrios, C.H.; Bergh, J.; Bhattacharyya, G.S.; Biganzoli, L.; et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann. Oncol. 2020, 31, 1623–1649. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Ahn, H.K.; Park, Y.H.; Nam, D.H.; Lee, J.I.; Park, W.; Choi, D.H.; Huh, S.J.; Park, K.T.; Ahn, J.S.; et al. Leptomeningeal metastases from breast cancer: Intrinsic subtypes may affect unique clinical manifestations. Breast Cancer Res. Treat. 2011, 129, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Lin, N.U.; Vanderplas, A.; Hughes, M.E.; Theriault, R.L.; Edge, S.B.; Wong, Y.N.; Blayney, D.W.; Niland, J.C.; Winer, E.P.; Weeks, J.C. Clinicopathologic features, patterns of recurrence, and survival among women with triple-negative breast cancer in the National Comprehensive Cancer Network. Cancer 2012, 118, 5463–5472. [Google Scholar] [CrossRef]
- Kennecke, H.; Yerushalmi, R.; Woods, R.; Cheang, M.C.; Voduc, D.; Speers, C.H.; Nielsen, T.O.; Gelmon, K. Metastatic behavior of breast cancer subtypes. J. Clin. Oncol. 2010, 28, 3271–3277. [Google Scholar] [CrossRef]
- Mehta, A.I.; Brufsky, A.M.; Sampson, J.H. Therapeutic approaches for HER2-positive brain metastases: Circumventing the blood-brain barrier. Cancer Treat. Rev. 2013, 39, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Stemmler, H.J.; Schmitt, M.; Willems, A.; Bernhard, H.; Harbeck, N.; Heinemann, V. Ratio of trastuzumab levels in serum and cerebrospinal fluid is altered in HER2-positive breast cancer patients with brain metastases and impairment of blood-brain barrier. Anticancer Drugs 2007, 18, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, E.C.; Oude Munnink, T.H.; Kosterink, J.G.; Brouwers, A.H.; Jager, P.L.; de Jong, J.R.; van Dongen, G.A.; Schröder, C.P.; Lub-de Hooge, M.N.; de Vries, E.G. Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer. Clin. Pharmacol. Ther. 2010, 87, 586–592. [Google Scholar] [CrossRef]
- Figura, N.B.; Rizk, V.T.; Mohammadi, H.; Evernden, B.; Mokhtari, S.; Yu, H.M.; Robinson, T.J.; Etame, A.B.; Tran, N.D.; Liu, J.; et al. Clinical outcomes of breast leptomeningeal disease treated with intrathecal trastuzumab, intrathecal chemotherapy, or whole brain radiation therapy. Breast Cancer Res. Treat. 2019, 175, 781–788. [Google Scholar] [CrossRef]
- Zagouri, F.; Zoumpourlis, P.; Le Rhun, E.; Bartsch, R.; Zografos, E.; Apostolidou, K.; Dimopoulos, M.A.; Preusser, M. Intrathecal administration of anti-HER2 treatment for the treatment of meningeal carcinomatosis in breast cancer: A metanalysis with meta-regression. Cancer Treat. Rev. 2020, 88, 102046. [Google Scholar] [CrossRef]
- Grossman, S.A.; Finkelstein, D.M.; Ruckdeschel, J.C.; Trump, D.L.; Moynihan, T.; Ettinger, D.S. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J. Clin. Oncol. 1993, 11, 561–569. [Google Scholar] [CrossRef]
- Hitchins, R.N.; Bell, D.R.; Woods, R.L.; Levi, J.A. A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J. Clin. Oncol. 1987, 5, 1655–1662. [Google Scholar] [CrossRef] [PubMed]
- Glantz, M.J.; Jaeckle, K.A.; Chamberlain, M.C.; Phuphanich, S.; Recht, L.; Swinnen, L.J.; Maria, B.; LaFollette, S.; Schumann, G.B.; Cole, B.F.; et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin. Cancer Res. 1999, 5, 3394–3402. [Google Scholar] [PubMed]
- Boogerd, W.; van den Bent, M.J.; Koehler, P.J.; Heimans, J.J.; van der Sande, J.J.; Aaronson, N.K.; Hart, A.A.; Benraadt, J.; Vecht, C.J. The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: A randomised study. Eur. J. Cancer 2004, 40, 2726–2733. [Google Scholar] [CrossRef] [PubMed]
- Le Rhun, E.; Mailliez, A.; Wallet, J.; Rodrigues, I.; Boulanger, T.; Desmoulins, I.; Barriere, J.; Fabbro, M.; Taillibert, S.; Andre, C.; et al. 371O. Intra-CSF liposomal cytarabine plus systemic therapy as initial treatment of breast cancer leptomeningeal metastasis: A randomised, open-label trial. Ann. Oncol. 2018, 29, viii122–viii132. [Google Scholar] [CrossRef]
- Swain, S.M.; Baselga, J.; Kim, S.B.; Ro, J.; Semiglazov, V.; Campone, M.; Ciruelos, E.; Ferrero, J.M.; Schneeweiss, A.; Heeson, S.; et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N. Engl. J. Med. 2015, 372, 724–734. [Google Scholar] [CrossRef]
- Jacot, W.; Pons, E.; Frenel, J.S.; Guiu, S.; Levy, C.; Heudel, P.E.; Bachelot, T.; D’Hondt, V.; Darlix, A.; Firmin, N.; et al. Efficacy and safety of trastuzumab emtansine (T-DM1) in patients with HER2-positive breast cancer with brain metastases. Breast Cancer Res. Treat. 2016, 157, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Diéras, V.; Miles, D.; Verma, S.; Pegram, M.; Welslau, M.; Baselga, J.; Krop, I.E.; Blackwell, K.; Hoersch, S.; Xu, J.; et al. Trastuzumab emtansine versus capecitabine plus lapatinib in patients with previously treated HER2-positive advanced breast cancer (EMILIA): A descriptive analysis of final overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2017, 18, 732–742. [Google Scholar] [CrossRef]
- Montemurro, F.; Delaloge, S.; Barrios, C.H.; Wuerstlein, R.; Anton, A.; Brain, E.; Hatschek, T.; Kelly, C.M.; Peña-Murillo, C.; Yilmaz, M.; et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: Exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial☆. Ann. Oncol. 2020, 31, 1350–1358. [Google Scholar] [CrossRef]
- Ricciardi, G.R.R.; Russo, A.; Franchina, T.; Schifano, S.; Mastroeni, G.; Santacaterina, A.; Adamo, V. Efficacy of T-DM1 for leptomeningeal and brain metastases in a HER2 positive metastatic breast cancer patient: New directions for systemic therapy-a case report and literature review. BMC Cancer 2018, 18, 97. [Google Scholar] [CrossRef]
- Freedman, R.A.; Gelman, R.S.; Anders, C.K.; Melisko, M.E.; Parsons, H.A.; Cropp, A.M.; Silvestri, K.; Cotter, C.M.; Componeschi, K.P.; Marte, J.M.; et al. Translational Breast Cancer Research Consortium. TBCRC 022: A Phase II Trial of Neratinib and Capecitabine for Patients With Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer and Brain Metastases. J. Clin. Oncol. 2019, 37, 1081–1089. [Google Scholar] [CrossRef]
- Saura, C.; Oliveira, M.; Feng, Y.H.; Dai, M.S.; Chen, S.W.; Hurvitz, S.A.; Kim, S.B.; Moy, B.; Delaloge, S.; Gradishar, W.; et al. NALA Investigators. Neratinib Plus Capecitabine Versus Lapatinib Plus Capecitabine in HER2-Positive Metastatic Breast Cancer Previously Treated With ≥ 2 HER2-Directed Regimens: Phase III NALA Trial. J. Clin. Oncol. 2020, 38, 3138–3149. [Google Scholar] [CrossRef]
- Murthy, R.K.; Loi, S.; Okines, A.; Paplomata, E.; Hamilton, E.; Hurvitz, S.A.; Lin, N.U.; Borges, V.; Abramson, V.; Anders, C.; et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2020, 382, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Pellerino, A.; Palmiero, R.; Mo, F.; Bruno, F.; Muscolino, E.; Franchino, F.; Rudà, R.; Soffietti, R. Neratinib for treatment of leptomeningeal metastases from HER2-positive breast cancer in extended access program: Preliminary results. Neurol. Sci. 2020, 41, S264. [Google Scholar]
- Chen, T.W.; Jan, I.S.; Chang, D.Y.; Lin, C.H.; Chen, I.C.; Chen, H.M.; Cheng, A.L.; Lu, Y.S. Systemic treatment of breast cancer with leptomeningeal metastases using bevacizumab, etoposide and cisplatin (BEEP regimen) significantly improves overall survival. J. Neurooncol. 2020, 148, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Boogerd, W.; Dorresteijn, L.D.; van Der Sande, J.J.; de Gast, G.C.; Bruning, P.F. Response of leptomeningeal metastases from breast cancer to hormonal therapy. Neurology 2000, 55, 117–119. [Google Scholar] [CrossRef]
- Ozdogan, M.; Samur, M.; Bozcuk, H.S.; Sagtas, E.; Yildiz, M.; Artac, M.; Savas, B. Durable remission of leptomeningeal metastasis of breast cancer with letrozole: A case report and implications of biomarkers on treatment selection. Jpn. J. Clin. Oncol. 2003, 33, 229–231. [Google Scholar] [CrossRef]
- Navarro Martín, L.M.; Ocaña Fernández, A.; Rodríguez Sánchez, C.A.; Ruiz Martín, I.; Cruz Hernández, J.J. Durable clinical benefit with exemestane in leptomeningeal metastasis of breast cancer. Clin. Transl. Oncol. 2005, 7, 358–360. [Google Scholar] [CrossRef]
- Zoghi, B.; Elledge, R. Endocrine Therapy for Leptomeningeal Metastases from ER-Positive Breast Cancer: Case Report and a Review of the Literature. Breast J. 2016, 22, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.V.; Searle, K.; Jerzak, K.J. Central nervous system-specific efficacy of CDK4/6 inhibitors in randomized controlled trials for metastatic breast cancer. Oncotarget 2019, 10, 6317–6322. [Google Scholar] [CrossRef]
- Tolaney, S.M.; Sahebjam, S.; Le Rhun, E.; Bachelot, T.; Kabos, P.; Awada, A.; Yardley, D.; Chan, A.; Conte, P.; Diéras, V.; et al. A Phase II Study of Abemaciclib in Patients with Brain Metastases Secondary to Hormone Receptor-Positive Breast Cancer. Clin. Cancer Res. 2020, 26, 5310–5319. [Google Scholar] [CrossRef]
- Brastianos, P.K.; Kim, A.E.; Wang, N.; Lee, E.Q.; Ligibel, J.; Cohen, J.V.; Chukwueke, U.N.; Mahar, M.; Oh, K.; White, M.D.; et al. Palbociclib demonstrates intracranial activity in progressive brain metastases harboring cyclin-dependent kinase pathway alterations. Nat. Cancer 2021, 2, 498–502. [Google Scholar] [CrossRef]
- Anders, C.; Deal, A.M.; Abramson, V.; Liu, M.C.; Storniolo, A.M.; Carpenter, J.T.; Puhalla, S.; Nanda, R.; Melhem-Bertrandt, A.; Lin, N.U.; et al. TBCRC 018: Phase II study of iniparib in combination with irinotecan to treat progressive triple negative breast cancer brain metastases. Breast Cancer Res. Treat. 2014, 146, 557–566. [Google Scholar] [CrossRef]
- Litton, J.K.; Hurvitz, S.A.; Mina, L.A.; Rugo, H.S.; Lee, K.H.; Gonçalves, A.; Diab, S.; Woodward, N.; Goodwin, A.; Yerushalmi, R.; et al. Talazoparib versus chemotherapy in patients with germline BRCA1/2-mutated HER2-negative advanced breast cancer: Final overall survival results from the EMBRACA trial. Ann. Oncol. 2020, 31, 1526–1535. [Google Scholar] [CrossRef]
- Bangham, M.; Goldstein, R.; Walton, H.; Ledermann, J.A. Olaparib treatment for BRCA-mutant ovarian cancer with leptomeningeal disease. Gynecol. Oncol. Rep. 2016, 18, 22–24. [Google Scholar] [CrossRef]
- Exman, P.; Mallery, R.M.; Lin, N.U.; Parsons, H.A. Response to Olaparib in a Patient with Germline BRCA2 Mutation and Breast Cancer Leptomeningeal Carcinomatosis. NPJ Breast Cancer 2019, 5, 46. [Google Scholar] [CrossRef]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.A.; Shaw Wright, G.; et al. IMpassion130 Trial Investigators. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef]
- Brastianos, P.K.; Lee, E.Q.; Cohen, J.V.; Tolaney, S.M.; Lin, N.U.; Wang, N.; Chukwueke, U.; White, M.D.; Nayyar, N.; Kim, A.; et al. Single-arm, open-label phase 2 trial of pembrolizumab in patients with leptomeningeal carcinomatosis. Nat. Med. 2020, 26, 1280–1284. [Google Scholar] [CrossRef]
- Kumthekar, P.; Tang, S.C.; Brenner, A.J.; Kesari, S.; Piccioni, D.E.; Anders, C.; Carrillo, J.; Chalasani, P.; Kabos, P.; Puhalla, S.; et al. ANG1005, a Brain-Penetrating Peptide-Drug Conjugate, Shows Activity in Patients with Breast Cancer with Leptomeningeal Carcinomatosis and Recurrent Brain Metastases. Clin. Cancer Res. 2020, 26, 2789–2799. [Google Scholar] [CrossRef]
- Arasaratnam, M.; Hong, A.; Shivalingam, B.; Wheeler, H.; Guminksi, A.D.; Long, G.V.; Menzies, A.M. Leptomeningeal melanoma-A case series in the era of modern systemic therapy. Pigment Cell Melanoma Res. 2018, 31, 120–124. [Google Scholar] [CrossRef]
- Sakji-Dupré, L.; Le Rhun, E.; Templier, C.; Desmedt, E.; Blanchet, B.; Mortier, L. Cerebrospinal fluid concentrations of vemurafenib in patients treated for brain metastatic BRAF-V600 mutated melanoma. Melanoma Res. 2015, 25, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Floudas, C.S.; Chandra, A.B.; Xu, Y. Vemurafenib in leptomeningeal carcinomatosis from melanoma: A case report of near-complete response and prolonged survival. Melanoma Res. 2016, 26, 312–315. [Google Scholar] [CrossRef]
- Lee, J.M.; Mehta, U.N.; Dsouza, L.H.; Guadagnolo, B.A.; Sanders, D.L.; Kim, K.B. Long-term stabilization of leptomeningeal disease with whole-brain radiation therapy in a patient with metastatic melanoma treated with vemurafenib: A case report. Melanoma Res. 2013, 23, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, N.; Scheffler, B.; Stuplich, M.; Schaub, C.; Kebir, S.; Rehkämper, C.; Mack, F.; Niehusmann, P.; Simon, M.; Greschus, S.; et al. Vemurafenib for leptomeningeal melanomatosis. J. Clin. Oncol. 2013, 31, e173–e174. [Google Scholar] [CrossRef]
- Kim, D.W.; Barcena, E.; Mehta, U.N.; Rohlfs, M.L.; Kumar, A.J.; Penas-Prado, M.; Kim, K.B. Prolonged survival of a patient with metastatic leptomeningeal melanoma treated with BRAF inhibition-based therapy: A case report. BMC Cancer 2015, 15, 400. [Google Scholar] [CrossRef] [PubMed]
- Wilgenhof, S.; Neyns, B. Complete Cytologic Remission of V600E BRAF-Mutant Melanoma-Associated Leptomeningeal Carcinomatosis Upon Treatment With Dabrafenib. J. Clin. Oncol. 2015, 33, e109–e111. [Google Scholar] [CrossRef] [PubMed]
- Glitza, I.C.; Ferguson, S.D.; Guha-Thakurta, N. Rapid resolution of leptomeningeal disease with targeted therapy in a metastatic melanoma patient. J. Neurooncol. 2017, 133, 663–665. [Google Scholar] [CrossRef]
- Davies, M.A.; Saiag, P.; Robert, C.; Grob, J.J.; Flaherty, K.T.; Arance, A.; Chiarion-Sileni, V.; Thomas, L.; Lesimple, T.; Mortier, L.; et al. Dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma brain metastases (COMBI-MB): A multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017, 18, 863–873. [Google Scholar] [CrossRef]
- Tétu, P.; Sirven-Villaros, L.; Cuzzubbo, S.; Ursu, R.; Baroudjian, B.; Delyon, J.; Nataf, F.; De Margerie-Mellon, C.; Allayous, C.; Lefevre, W.; et al. Impact of New Systemic Treatment and Radiotherapy in Melanoma Patients with Leptomeningeal Metastases. Cancers 2020, 12, 2635. [Google Scholar] [CrossRef]
- Smalley, K.S.; Fedorenko, I.V.; Kenchappa, R.S.; Sahebjam, S.; Forsyth, P.A. Managing leptomeningeal melanoma metastases in the era of immune and targeted therapy. Int. J. Cancer 2016, 139, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- Long, G.V.; Atkinson, V.; Lo, S.; Sandhu, S.; Guminski, A.D.; Brown, M.P.; Wilmott, J.S.; Edwards, J.; Gonzalez, M.; Scolyer, R.A.; et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: A multicentre randomised phase 2 study. Lancet Oncol. 2018, 19, 672–681. [Google Scholar] [CrossRef]
- Glitza, I.C.; Rohlfs, M.; Bassett, R.L.; Ida, J.; Richard, J.; Iqbal, M.; Bernzen, T.; Gerber, D.; Lacey, C.; Diab, A.; et al. ICMT-07 Therapeutic outcomes of intrathecal IL-2 in metastatic melanoma patients with leptomeningeal disease. Soc. Neuro Oncol. 2015, 17, v108. [Google Scholar]
- Clemons-Miller, A.R.; Chatta, G.S.; Hutchins, L.; Angtuaco, E.J.; Ravaggi, A.; Santin, A.D.; Cannon, M.J. Intrathecal cytotoxic T-cell immunotherapy for metastatic leptomeningeal melanoma. Clin. Cancer Res. 2001, 7, 917s–924s. [Google Scholar]
- Glitza, I.C.; Haymaker, C.; Bernatchez, C.; Vence, L.; Rohlfs, M.; Richard, J.; Lacey, C.; Mansaray, R.; Fulbright, O.J.; Ramachandran, R.; et al. Intrathecal Administration of Tumor-Infiltrating Lymphocytes Is Well Tolerated in a Patient with Leptomeningeal Disease from Metastatic Melanoma: A Case Report. Cancer Immunol. Res. 2015, 3, 1201–1206. [Google Scholar] [CrossRef]
- Glitza, I.C.; Phillips, S.; Brown, C.; Haymaker, C.L.; Bassett, R.L.; Lee, J.J.; Rohlfs, M.L.; Richard, J.; Iqbal, M.; John, I.; et al. Single-center phase I/Ib study of concurrent intrathecal (IT) and intravenous (IV) nivolumab (N) for metastatic melanoma (MM) patients (pts) with leptomeningeal disease (LMD). J. Clin. Oncol. 2020, 38, 10008. [Google Scholar] [CrossRef]
- Sonabend, A.M.; Stupp, R. Overcoming the Blood-Brain Barrier with an Implantable Ultrasound Device. Clin. Cancer Res. 2019, 25, 3750–3752. [Google Scholar] [CrossRef]
- Idbaih, A.; Canney, M.; Belin, L.; Desseaux, C.; Vignot, A.; Bouchoux, G.; Asquier, N.; Law-Ye, B.; Leclercq, D.; Bissery, A.; et al. Safety and Feasibility of Repeated and Transient Blood-Brain Barrier Disruption by Pulsed Ultrasound in Patients with Recurrent Glioblastoma. Clin. Cancer Res. 2019, 25, 3793–3801. [Google Scholar] [CrossRef]
- Rothwell, W.T.; Bell, P.; Richman, L.K.; Limberis, M.P.; Tretiakova, A.P.; Li, M.; Wilson, J.M. Intrathecal Viral Vector Delivery of Trastuzumab Prevents or Inhibits Tumor Growth of Human HER2-Positive Xenografts in Mice. Cancer Res. 2018, 78, 6171–6182. [Google Scholar] [CrossRef] [PubMed]
- Boire, A.; Brastianos, P.K.; Garzia, L.; Valiente, M. Brain metastasis. Nat. Rev. Cancer 2020, 20, 4–11. [Google Scholar] [CrossRef]


| Preclinical Models |
|---|
| NSCLC |
| BM models using the ALK-rearranged NSCLC cell line H3122 EML4-ALKL1196M showed that the PF-06463922 compound is a potent brain-permeable ALK/ROS1 inhibitor with an increased ability to cross the BBB/BTB and penetrate into non-permeable micrometastases and macrometastases [22] |
| Melanoma |
| An in vivo longitudinal MRI study using contrast-enhanced T1-weighted spin echo images was performed after the intracardiac injection of melanoma cell lines A2058 in mice, reporting the presence in BM of regions with intact BBB mixed with other areas with a disrupted BBB [23] |
| BM models from melanoma cells (MDA-MB-435 and A2058) show vessel cooperation between tumor cells and BTB, while models using NSCLC cells (PC14-PE6 and HTB177) enhance the neoangiogenesis to alter the BBB/BTB [24] |
| Breast Cancer (BC) |
| After the intracardiac injection of BC cell lines 231-BR-HER2 and 4T1-BRS, the BTB permeability differs between the two models: the 231-BR model showed a significant permeability to drugs because of the high expression of S1PR-3 [19] |
| The BBB is more permeable in cell models using SUM190-BR3 and JIMT-1-BR3 BC cells compared with the 231-BR-HER2 counterpart [25] |
| Desmin-positive pericytes correlate with areas of high permeability on BTB from BC [17] |
| Intracranial injection model using human BC cell line BT474 is permeable to chemotherapy and antibodies in physiological conditions, but the drug delivery significantly increases after the BBB/BTB disruption [26]. Such a preclinical model has been reproduced in a clinical setting demonstrating a comparable drug delivery of targeted therapy (lapatinib) in BM and primary site [27]. Furthermore, intracranial injection of BT474 cells creates a leakier BBB/BTB and an increased drug uptake compared with intravenously or intracardially injection models, displaying that the route of administration significantly impacts the drug delivery [28] |
| Miscellanea |
| Some patient-derived xenograft models of CNS recurrences from NSCLC, BC, melanoma, prostate and neuroendocrine tumors revealed a decreased expression of NLS1 on BBB compared with healthy brain tissue [18] |
| Clinical Data |
| Breast Cancer |
| BBB/BTB interface is different according to molecular subtypes of BC. HER2-enriched cells tend to preserve the integrity of the BBB, while TNBC or basal-type BC disrupt the BBB. Moreover, the ECs of BTB express higher levels of GLUT1 and BCRP compared with those ER-positive or TNBC [20] |
| Lapatinib achieves significant concentrations (1.0–6.5 microM) from HER2-positive BM when administered at a daily dose of 1250 mg (last dose 2–3 h before surgery) [29]. This evidence was confirmed by PET studies when comparing tumors with normal brain tissue [30]. Although HER2-positive BM preserve the integrity of BBB, trastuzumab alone or linked to emtansine (TDM-1) achieves a significant distribution due to the leakiness of the BTB [31,32] |
| Study | Number of Patients | Type of Primary Solid Tumor | Results |
|---|---|---|---|
| Patel et al., 2011 [74] | 5 | BC | CTCs detected using CellSearch technique showing that the number of CTCs are correlated with leptomeningeal burden and response to chemotherapy |
| LeRhun et al., 2012 [80] | 8 | BC | Detection of CTCs with adapted CellSearch technology displays a quantitative correlation with the response to therapy |
| Subirà et al., 2012 [63] | 72 | BC (44) NSCLC (23) GIC (4) Cavum (1) | Sensitivity of CTCs: 75.5% Sensitivity of CSF cytology: 65.3% Specificity of CTCs: 96.1% Specificity of CSF cytology: 100% Immunoflow cytometry |
| Nayak et al., 2013 [64] | 51 | NSCLC (21) BC (15) Melanoma (1) Ovarian cancer (2) Others (12) | Sensitivity of CTCs: 100% Sensitivity of CSF cytology: 66.7% Specificity of CTCs: 97.2% Specificity of CSF cytology: 100% Median CTCs: 20.7 cells/mL CellSearch technique |
| LeRhun et al., 2013 [72] | 2 | Melanoma | First study that used adapted CellSearch technology against HMW-MAA to detect melanoma CTCs |
| Lee et al., 2015 [66] | 38 | BC | Sensitivity of CTCs: 80.9% Sensitivity of CSF cytology: 66.7% Specificity of CTCs: 84.6% Specificity of CSF cytology: 100% CellSearch technique |
| Subirà et al., 2015 [65] | 144 | BC (39) NSCLC (35) GIC (6) Ovarian (4) Prostate (3) Others (5) | Sensitivity of CTCs: 79.8% Sensitivity of CSF cytology: 50.0% Specificity of CTCs: 84.0% Specificity of CSF cytology: 100% Immunoflow cytometry |
| Tu et al., 2015 [67] | 18 | NSCLC | Sensitivity of CTCs: 77.8% Sensitivity of CSF cytology: 44.4% Specificity of CTCs: 100% Specificity of CSF cytology: not reported CellSearch technique |
| Acosta et al., 2016 [81] | 6 | Epithelial cell tumors | Sensitivity of CTCs: 100.0% Specificity of CTCs: 100.0% Immunoflow cytometry |
| Milojkovic Kerklaan et al., 2016 [68] | 29 | Epithelial cell tumors | Sensitivity of CTCs: 100.0% Sensitivity of CSF cytology: 61.5% Specificity of CTCs: 100.0% Specificity of CSF cytology: 100% Immunoflow cytometry |
| Ma et al., 2016 [82] | 10 | NSCLC | Seven out of ten CSF samples where CTCs were found with a range from 3 to 1823 tumor cells TM-iFISH |
| Jiang et al., 2017 [76] | 21 | NSCLC | Sensitivity of CTCs: 95.2% Sensitivity of CSF cytology: 57.1% Specificity of CTCs: 100% Specificity of CSF cytology: not reported CellSearch technique |
| Lin et al., 2017 [83] | 95 | NSCLC (36) BC (31) Others (28) | Sensitivity of CTCs: 93.0% Sensitivity of CSF cytology: 29.0% Specificity of CTCs: 95.0% Specificity of CSF cytology: not reported CellSearch technique |
| van Bussel et al., 2020 [84] | 81 | NSCLC | Sensitivity of CTCs: 94.0% Specificity of CTCs: 100.0% Cut-off for CTCs positivity: 0.9 CTC/mL Immunoflow cytometry |
| Nevel et al., 2020 [75] | 16 | NSCLC | Patients with ≥50 CTCs/3 mL had an increased risk of death in comparison with that of those with <CTCs/3 mL CellSearch technique |
| Malani et al., 2020 [85] | 15 | HER2-positive BC | CSF CTCs were identified in 13 patients (87%) Median CSF CTCs was 22 CTCs/3 mL (range 0–200 +). HER2 expression analysis of CTCs was performed in 8 patients; 75% had confirmed expression of HER2 in CSF CellSearch technique |
| Study | Number of Patients | Type of Primary Solid Tumor | Results |
|---|---|---|---|
| Swinkels et al., 2000 [90] | 2 | NSCLC | KRAS mutation was found in CSF of 2/2 patients (100%) CSF Mutant-allele-specific amplification (PCR) |
| Momtaz et al., 2016 [87] | 11 | BRAF-mutated malignancies | BRAF mutations detected in CSF-ctDNA of 6/11 patients (54%) Droplet digital sequencing |
| Pentsova et al., 2016 [88] | 32 BM 9 LM | NSCLC (11) BC (11) Melanoma (6) Others (13) | Mutations were detected in CSF-ctDNA of 20/32 patients (63%) with BM and 3/4 patients (75%) with LM Targeted sequencing |
| Marchio et al., 2017 [89] | 2 | NSCLC | KRAS mutations detectable in CSF-ctDNA of 2/2 patients (100%) Targeted sequencing |
| Fan et al., 2018 [91] | 11 | EGFR-mutated NSCLC | EGFR mutations were found in CSF-ctDNA of 11/11 patients (100%). Mutations were not concordant in 1/11 (9%) Targeted sequencing |
| Li et al., 2018 [92] | 42 | EGFR-mutated NSCLC | Distinct EGFR mutations were found in CSF-ctDNA of 28 patients (92%) Targeted sequencing |
| Huang et al., 2019 [94] | 20 BM 15 LM | EGFR-mutated NSCLC | EGFR mutations were detected in 23/35 patients: BM: blood: 6/11 (54.5%); CSF: 5/10 (50%) LM: blood: 4/11 (36.4%); CSF: 9/12 (75%) T790 mutation was significantly higher in blood (9/23) than that of CSF (3/23) Sensitivity in CSF: 56%; in blood: 89% Specificity in CSF: 46%; in blood: 100% Twelve patients received a first-generation TKI after the detection of actionable mutation in CSF, while 5 patients switched to osimertinib after the detection of T790 mutation in CSF or blood Droplet digital PCR |
| Ma et al., 2020 [95] | 11 | NSCLC that progressed after 3rd generation TKIs | CSF-ctDNA was identified in 8/11 patients (72.7%) and in the blood of 6/11 (54.5%) EGFR C797 mutation and MET amplification were found in CSF of 4/11 patients (36.3%) and in the blood of 2/11 (18.2%) One patient only had C797 and T790 mutation concurrently Longitudinal assessment with CSF-ctDNA displayed that the level of C797 mutation decreased with radiological and neurological improvement, while the blood level of T790 mutation increased early before leptomeningeal progression Nanowire-based ctDNA assay |
| Li et al., 2020 [96] | 18 | NSCLC EGFR-mutated (11) ALK-rearranged (6) ROS1-mutated (1) | The MET mutational rate was higher in CSF (100%) than that of blood (66.7%) A higher number of SNVs and copy number variants were found in CSF in comparison with blood SNVs were higher in patients pretreated with ≥2 TKIs than that of those who received 1 TKI only NGS |
| Nevel et al., 2020 [75] | 21 | NSCLC | CSF-ctDNA concentrations ranged from 0.093 pg/microL to 0.562 ng/microL Median CSF-ctDNA concentration was 0.022 ng/microL An increased risk of death was observed when ctDNA concentrations were higher than the median cutpoint Targeted exome sequencing MSKCC IMPACT |
| Zheng et al., 2021 [97] | 80 | EGFR-mutated NSCLC Cohort 1: CSF and blood genotyping before the 1st administration of osimertinib (45) Cohort 2: CSF genotyping at the time of progression with LM during treatment with osimertinib (35) | Detection of actionable EGFR mutations in CSF-ctDNA: Cohort 1: 42/45 (93.3%) Cohort 2: 34/35 (97.1%) Median iPFS was higher in patients with EGFR exon 19 deletion (11.9 months) compared with that of patients harboring EGFR exon 21 L858 mutation (2.8 months) Median iPFS was higher in patients with EGFR T790-positive CSF genotyping (15.6 months) than that of those without T790 mutation (7.0 months) Concomitant presence of CD42 (2.8 months) and CDKN2a mutations (2.5 months) confers a shorter iPFS (11.6 and 9.6 months, respectively) than that of patients with CSF-ctDNA negative Cohort 2: EGFR C795 mutation, MET dysregulation, co-occurrence of TP53 and RB1 mutations as well as loss of T790 mutation in CSF-ctDNA were correlated with shorter survival NGS |
| Carausu et al., 2019 [98] | 1 | HR-positive/HER2-negative BC | First report of detection of CSF-ctDNA of ESR1 mutation after treatment with aromatase inhibitor Droplet digital PCR |
| Angust et al., 2021 [99] | 151 | BC | Thirty CSF samples were analyzed with NGS and 121 with mFAST-SeqS Sensitivity of NGS: 8/30 (26.7%) Sensitivity of mFAST-SeqS: 112/121 (92.6%) Aneuploidy was found in 24 patients using mFAST-SeqS only and was correlated with worse prognosis |
| Ballester et al., 2018 [100] | 7 | Melanoma | Thirty percent of patients with a negative CSF cytology showed a CSF-ctDNA positivity Droplet digital PCR |
| Study | Type of Study | No. of Patients | Treatment | Results |
|---|---|---|---|---|
| EGFR TKIs | ||||
| Grommes et al., 2011 [109] | Retrospective | 9 | Pulsatile high-dose erlotinib (1500 mg weekly) | Radiological response in 6/9 patients (66.7%) Median OS: 12 months |
| Lee et al., 2013 [110] | Retrospective | 25 | Arm 1: gefitinib 250 mg/day Arm 2: erlotinib 150 mg/day | Clearance of CSF cytology in 10/25 patients (40%) Erlotinib led to CSF cytology conversion in 64.3% of patients, while only in 9.1% following gefitinib |
| Yang et al., 2015 [111] | Retrospective | 6 | Pemetrexed 500 mg/m2 day 1; cisplatin 30 mg day 1–2; erlotinib 150 mg day 3–21 | Response rate: CR 1/6 (16.6%); PR 2/6 (33.3%); SD 2/6 (33.3%) Median OS: 9 months |
| Kawamura et al., 2015 [112] | Retrospective | 35 | Arm 1: high-dose erlotinib (200–600 mg/day every 2–4 days) Arm 2: standard dose erlotinib (150 mg/day) | High-dose erlotinib: radiological response in 3/10 patients (30%), neurological improvement in 6/12 patients (50%) Median OS: high-dose group: 6.2 months Standard dose group: 5.9 months |
| Jackman et al., 2015 [113] | Phase I | 7 | 2 weeks of high-dose of gefitinib (750–1000 mg/day) and 2 weeks of 500 mg/day | Median OS: 3.5 months Median PFS: 2.3 months CSF cytology clearance in 1/7 patients (14.3%) Neurological improvement in 4/7 patients (57.1%) |
| Liao et al., 2015 [129] | Retrospective | 75 | Arm A: Gefitinib + CT Arm B: Erlotinib + CT Arm C: Afatinib + CT Regimen details not available | The association of TKI plus chemotherapy is correlated with prolonged survival in both univariate and multivariate analysis |
| Tamiya et al., 2017 [114] | Prospective | 11 | Afatinib 40 mg/m2 daily | Median CSF penetration: 2.45% Median CSF concentration: 1.4 ng/mL (2.9 nM) Radiological response: 27.3% Median PFS: 2 months Median OS: 3.8 months |
| Yang et al., 2017 [115] | Phase I | 32 | Osimertinib 160 mg daily | 20/23 patients (86.9%) had neurological improvement 23/32 (72%) had radiological response |
| Nanjo et al., 2018 [116] | Prospective | 13 (3 definitive LM and 8 possible LM) | Osimertinib 80 mg daily | CSF penetration: 2.5% Median PFS: 7.2 months |
| Yang et al., 2020 [117] | Prospective | 41 | Osimertinib 160 mg daily | ORR 62% Median OS 15.2 months |
| Saboundji et al., 2018 [118] | Retrospective | 20 | Osimertinib 80 mg daily | 100% of patients experienced neurological improvement Median PFS: 17.2 months Median OS: 18 months |
| Ahn et al., 2020 [119] | Retrospective | 22 | Osimertinib 80 mg daily | ORR 55% Median OS 18.8 months |
| Park et al., 2020 [120] | Phase 2 | 40 | Osimertinib 160 mg daily | ORR 55% Median PFS 7.6 months Median OS 16.9 months |
| Lee et al., 2020 [121] | Retrospective | 351 87 with T790 mutation | Osimertinib | No difference in median OS according to T790M mutational status (10.1 months (95% CI 4.3–15.8) versus 9.0 months (95% CI: 6.8–11.21)) Patients treated with osimertinib had a superior OS of 17.0 months (95% CI 15.1–18.9) compared with that of those not treated with osimertinib who had a median OS of 5.5 months (95% CI 4.3–6.6), regardless of T790M mutational status |
| Ahn et al., 2016 [130] | Prospective | 29 (4 with LM) | AZD3759 | 3/4 patients (75%) had a significant reduction of EGFR expression 1/4 patients (25%) had a CSF conversion in two consecutive samples |
| Cho et al., 2017 [131] | Prospective | 18 | Arm 1: AZD3759 200 mg daily Arm 2: AZD3759 300 mg daily | 5/18 patients (27.8%) had a radiological response, while 9/18 patients (50%) had a stable disease |
| Xu et al., 2020 [132] | Prospective | 3 | erlotinib (150 mg/day) plus nimotuzumab (200 mg/m2) weekly | Rapid clinical response within 6–8 weeks from the start of treatment 2/3 patients reported a radiological response |
| ALK inhibitors | ||||
| Costa et al., 2011 [133] | Case report | 1 | WBRT plus crizotinib 250 mg twice daily | PFS: 9 months |
| Ahn et al., 2012 [134] | Case series | 2 | Intrathecal MTX plus crizotinib 250 mg twice daily | PFS 5 and 10 months, respectively |
| Arrondeau et al., 2014 [135] | Case report | 1 | Ceritinib 750 mg daily | PFS: 5.5 months |
| Dudnik et al., 2015 [136] | Case series | 3 | WBRT plus ceritinib 500 mg/daily | PFS patient 1: 18 months; patient 2 and 3: 7 months |
| Gainor et al., 2015 [137] | Case series | 4 | Alectinib 600 mg twice daily | Radiological and neurological improvement in 4/4 patients (75%) |
| Ou et al., 2015 [138] | Case report | 1 | Alectinib 600–750 mg twice daily | Long-lasting complete response (15 months) |
| Gainor et al., 2016 [139] | Case series | 2 | Alectinib 900 mg twice daily | Radiological and neurological improvement for 3.5 and 6 months, respectively |
| Gaye et al., 2019 [140] | Case report | 1 | Brigatinib 180 mg once daily with a 7 day lead-in period at 90 mg | PFS 14 months |
| Pellerino et al., 2019 [141] | Case report | 1 | Lorlatinib 100 mg once daily | PFS 12 months Complete radiological response |
| Frost et al., 2020 [142] | Prospective | 36 BM 9 LM | Lorlatinib 100 mg daily | Median duration of treatment: 10.4 months PFS: 8.0 months Intracranial response rate: 54% Time to treatment failure: 13.0 months Calculated 12-, 18- and 24-month OS were 65, 54 and 47% TP53 mutations were associated with a shorter PFS (3.7 versus 10.8 months), suggesting a role as strong prognostic biomarker |
| Study | Number of Patients | Primary Solid Tumor | Treatment | Primary Outcome Measure |
|---|---|---|---|---|
| NCT04356118 Phase 4 | 30 | NSCLC | Recombinant human endostatin + intrathecal MTX + targeted therapy (EGFR TKIs or ALK inhibitors) | OS Neurological PFS Adverse events |
| NCT04356222 Phase 4 | 30 | NSCLC | Durvalumab + intrathecal MTX | OS Neurological PFS Adverse events |
| NCT04315246 Phase 1/2 | 63 | Ductal or lobular BC, NSCLC, melanoma | Intracerebroventricular administration of 177Lu-DTPA-omburtamab | Incidence of AEs and SAEs (time frame: 1 year) |
| NCT03661424 Phase I | 16 | HER2-positive BC | Anti-CD3 x Anti-HER2/Neu (HER2Bi) Armed Activated T Cells (BATs) | Type, frequency, severity, duration and timing of AEs Number of patients who achieved the 80% of the total administrations of BATs |
| NCT04192981 Phase 1 | 36 | Primary solid tumors harboring PIK3CA mutations | GDC-0084 with or without WBRT | Primary: MTD |
| NCT03974204 Phase: NA | 74 | BC | --- | Proteomic profiles from CSF at diagnosis CSF cytology positivity at diagnosis |
| NCT04729348 Phase 2 | 19 | Any solid tumors | Pembrolizumab plus Lenvatinib | Six-month OS |
| NCT04425681 Phase 2 | 20 | EGFR-mutated NSCLC | Osimertinib + bevacizumab | ORR PFS |
| NCT04148898 Phase 2 | 80 | EGFR-mutated NSCLC | Arm 1: Osimertinib alone Arm 2: Osimertinib + bevacizumab | Intracranial PFS ORR |
| NCT04233021 Phase 2 | 113 | EGFR-mutated NSCLC | Osimertinib alone | ORR |
| NCT03696030 Phase 1 | 39 | HER2-positive BC | Intraventricular administration of autologous HER2-CAR T Cells | DLT AEs |
| NCT03719768 Phase 1b | 23 | Any solid tumors | Avelumab + WBRT | Safety and DLT |
| NCT04588545 Phase 1/2 | 39 | HER2-positive BC | Focal RT or WBRT + intrathecal trastuzumab/pertuzumab | MTD OS |
| NCT02422641 Phase 2 | 16 | Any subtypes of BC | Intravenous high-dose MTX | 12-week OS |
| NCT03613181 Phase 3 | 150 | HER2-negative BC | ANG1005 versus Physician’s Best Choice | OS |
| NCT03501979 Phase 2 | 30 | HER2-positive BC | Tucatinib + Trastuzumab + Capecitabine | OS |
| NCT04420598 Phase 2 | 39 | Cohort 5: HER2-positive or HER2-low expressing BC with LM | Trastuzumab deruxtecan | OS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellerino, A.; Brastianos, P.K.; Rudà, R.; Soffietti, R. Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches. Cancers 2021, 13, 2888. https://doi.org/10.3390/cancers13122888
Pellerino A, Brastianos PK, Rudà R, Soffietti R. Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches. Cancers. 2021; 13(12):2888. https://doi.org/10.3390/cancers13122888
Chicago/Turabian StylePellerino, Alessia, Priscilla K. Brastianos, Roberta Rudà, and Riccardo Soffietti. 2021. "Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches" Cancers 13, no. 12: 2888. https://doi.org/10.3390/cancers13122888
APA StylePellerino, A., Brastianos, P. K., Rudà, R., & Soffietti, R. (2021). Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches. Cancers, 13(12), 2888. https://doi.org/10.3390/cancers13122888









