Assessment and Prediction of Response to Neoadjuvant Chemotherapy in Breast Cancer: A Comparison of Imaging Modalities and Future Perspectives
Abstract
Simple Summary
Abstract
1. Introduction
2. Evaluation of Residual Tumor after NAC
2.1. Conventional Imaging Techniques
2.1.1. Digital Mammography and Digital Breast Tomosynthesis
2.1.2. Ultrasound
2.2. Advanced Imaging Techniques
2.2.1. Magnetic Resonance Imaging
2.2.2. Contrast-Enhanced Spectral Mammography
2.3. Nuclear Medicine Techniques
2.4. Artificial Intelligence
3. Prediction of Response to NAC
3.1. Magnetic Resonance Imaging
3.2. Hybrid Imaging Techniques
3.3. Artificial Intelligence
3.3.1. Ultrasound
3.3.2. Magnetic Resonance Imaging
3.3.3. Positron Emission Tomography
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Huber, S.; Wagner, M.; Zuna, I.; Medl, M.; Czembirek, H.; Delorme, S. Locally advanced breast carcinoma: Evaluation of mammography in the prediction of residual disease after induction chemotherapy. Anticancer. Res. 2000, 20, 553–558. [Google Scholar] [PubMed]
- Rastogi, P.; Anderson, S.; Bear, H.D.; Geyer, C.E.; Kahlenberg, M.S.; Robidoux, A.; Margolese, R.G.; Hoehn, J.L.; Vogel, V.G.; Dakhil, S.R.; et al. Preoperative Chemotherapy: Updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J. Clin. Oncol. 2008, 26, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Diéras, V.; Fumoleau, P.; Romieu, G.; Tubiana-Hulin, M.; Namer, M.; Mauriac, L.; Guastalla, J.-P.; Pujade-Lauraine, E.; Kerbrat, P.; Maillart, P.; et al. Randomized Parallel Study of Doxorubicin Plus Paclitaxel and Doxorubicin Plus Cyclophosphamide As Neoadjuvant Treatment of Patients With Breast Cancer. J. Clin. Oncol. 2004, 22, 4958–4965. [Google Scholar] [CrossRef] [PubMed]
- Smith, I.C.; Heys, S.D.; Hutcheon, A.W.; Miller, I.D.; Payne, S.; Gilbert, F.J.; Ah-See, A.K.; Eremin, O.; Walker, L.G.; Sarkar, T.K.; et al. Neoadjuvant chemotherapy in breast cancer: Significantly enhanced response with docetaxel. J. Clin. Oncol. 2002, 20, 1456–1466. [Google Scholar] [CrossRef]
- Cuppone, F.; Bria, E.; Carlini, P.; Milella, M.; Felici, A.; Sperduti, I.; Nisticò, C.; Terzoli, E.; Cognetti, F.; Giannarelli, D. Taxanes as primary chemotherapy for early breast cancer: Meta-analysis of randomized trials. Cancer 2008, 113, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; Loibl, S.; Noske, A.; Roller, M.; Müller, B.M.; Komor, M.; Budczies, J.; Darb-Esfahani, S.; Kronenwett, R.; Hanusch, C.; et al. Tumor-Associated Lymphocytes As an Independent Predictor of Response to Neoadjuvant Chemotherapy in Breast Cancer. J. Clin. Oncol. 2010, 28, 105–113. [Google Scholar] [CrossRef]
- Mieog, J.S.D.; van der Hage, J.A.; van de Velde, C.J.H. Neoadjuvant chemotherapy for operable breast cancer. BJS 2007, 94, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Chagpar, A.B.; Middleton, L.P.; Sahin, A.A.; Dempsey, P.; Buzdar, A.U.; Mirza, A.N.; Ames, F.C.; Babiera, G.V.; Feig, B.W.; Hunt, K.K.; et al. Accuracy of Physical Examination, Ultrasonography, and Mammography in Predicting Residual Pathologic Tumor Size in Patients Treated with Neoadjuvant Chemotherapy. Ann. Surg. 2006, 243, 257–264. [Google Scholar] [CrossRef]
- Campanile, F.; Maurea, S.; Mainenti, P.P.; Corvino, A.; Imbriaco, M. Duodenal Involvement by Breast Cancer. Breast J. 2012, 18, 615–616. [Google Scholar] [CrossRef]
- Gradishar, W.J.; Moran, M.S.; Abraham, J.; Aft, R.; Agnese, D.; Allison, K.H.; Blair, S.L.; Burstein, H.J.; Dang, C.; Elias, A.D.; et al. NCCN Guidelines® Insights: Breast Cancer, Version 4.2021. J. Natl. Compr. Cancer Netw. 2021, 19, 484–493. [Google Scholar] [CrossRef]
- Park, J.; Chae, E.Y.; Cha, J.H.; Shin, H.J.; Choi, W.J.; Choi, Y.-W.; Kim, H.H. Comparison of mammography, digital breast tomosynthesis, automated breast ultrasound, magnetic resonance imaging in evaluation of residual tumor after neoadjuvant chemotherapy. Eur. J. Radiol. 2018, 108, 261–268. [Google Scholar] [CrossRef]
- Kim, E.; Do, S.-I.; Yun, J.-S.; Park, Y.; Park, C.; Moon, J.; Youn, I.; Choi, Y.; Ham, S.-Y.; Kook, S. Preoperative evaluation of mammographic microcalcifications after neoadjuvant chemotherapy for breast cancer. Clin. Radiol. 2020, 75, 641.e19–641.e27. [Google Scholar] [CrossRef] [PubMed]
- Um, E.; Kang, J.-W.; Lee, S.; Kim, H.J.; Yoon, T.I.; Sohn, G.; Chung, I.Y.; Kim, J.; Lee, J.W.; Son, B.H.; et al. Comparing Accuracy of Mammography and Magnetic Resonance Imaging for Residual Calcified Lesions in Breast Cancer Patients Undergoing Neoadjuvant Systemic Therapy. Clin. Breast Cancer 2018, 18, e1087–e1091. [Google Scholar] [CrossRef]
- Adrada, B.E.; Huo, L.; Lane, D.L.; Arribas, E.M.; Resetkova, E.; Yang, W. Histopathologic Correlation of Residual Mammographic Microcalcifications After Neoadjuvant Chemotherapy for Locally Advanced Breast Cancer. Ann. Surg. Oncol. 2014, 22, 1111–1117. [Google Scholar] [CrossRef]
- Vinnicombe, S.J.; MacVicar, A.D.; Guy, R.L.; Sloane, J.P.; Powles, T.J.; Knee, G.; Husband, J.E. Primary breast cancer: Mammographic changes after neoadjuvant chemotherapy, with pathologic correlation. Radiology 1996, 198, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Mun, H.; Kim, H.; Shin, H.; Cha, J.; Ruppel, P.; Oh, H.; Chae, E. Assessment of extent of breast cancer: Comparison between digital breast tomosynthesis and full-field digital mammography. Clin. Radiol. 2013, 68, 1254–1259. [Google Scholar] [CrossRef] [PubMed]
- Arasaki, A.; Uchiyama, N.; Kinoshita, T. Usefulness of digital breast tomosynthesis (DBT) in evaluation of pathological response after neoadjuvant chemotherapy (NAC) for breast cancer. J. Clin. Oncol. 2015, 33, 119. [Google Scholar] [CrossRef]
- Uchiyama, N.; Kinoshita, T.; Hojo, T.; Asaga, S.; Suzuki, J.; Kawawa, Y.; Otsuka, K. Usefulness of adjunction of digital breast tomosynthesis (DBT) to full-field digital mammography (FFDM) in evaluation of pathological response after neoadjuvant chemotherapy (NAC) for breast cancer. In Proceedings of the International Workshop on Digital Mammography, Philadelphia, PA, USA, 8–11 July 2012; pp. 354–361. [Google Scholar] [CrossRef]
- Dialani, V.; Chadashvili, T.; Slanetz, P.J. Role of Imaging in Neoadjuvant Therapy for Breast Cancer. Ann. Surg. Oncol. 2015, 22, 1416–1424. [Google Scholar] [CrossRef] [PubMed]
- Dobruch-Sobczak, K.; Piotrzkowska-Wroblewska, H.; Klimonda, Z.; Roszkowska-Purska, K.; Litniewski, J. Ultrasound echogenicity reveals the response of breast cancer to chemotherapy. Clin. Imaging 2019, 55, 41–46. [Google Scholar] [CrossRef]
- Evans, A.; Whelehan, P.; Thompson, A.; Purdie, C.; Jordan, L.; Macaskill, J.; Waugh, S.; Fuller-Pace, F.; Brauer, K.; Vinnicombe, S. Prediction of Pathological Complete Response to Neoadjuvant Chemotherapy for Primary Breast Cancer Comparing Interim Ultrasound, Shear Wave Elastography and MRI. Senol. Z. Mammadiagnostik Ther. 2018, 15, 229–237. [Google Scholar]
- Baumgartner, A.; Tausch, C.; Hosch, S.; Papassotiropoulos, B.; Varga, Z.; Rageth, C.; Baege, A. Ultrasound-based prediction of pathologic response to neoadjuvant chemotherapy in breast cancer patients. Breast 2018, 39, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Waldrep, A.R.; Avery, E.J.; Rose, F.F.; Midathada, M.V.; Tilford, J.A.; Kolberg, H.-C.; Hutchins, M.R. Breast Cancer Subtype Influences the Accuracy of Predicting Pathologic Response by Imaging and Clinical Breast Exam after Neoadjuvant Chemotherapy. Anticancer. Res. 2016, 36, 5389–5396. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vriens, B.E.; de Vries, B.; Lobbes, M.B.; van Gastel, S.M.; Berkmortel, F.W.V.D.; Smilde, T.J.; van Warmerdam, L.J.; de Boer, M.; van Spronsen, D.J.; Smidt, M.L.; et al. Ultrasound is at least as good as magnetic resonance imaging in predicting tumour size post-neoadjuvant chemotherapy in breast cancer. Eur. J. Cancer 2016, 52, 67–76. [Google Scholar] [CrossRef]
- Stein, R.G.; Wollschläger, D.; Kreienberg, R.; Janni, W.; Wischnewsky, M.; Diessner, J.; Stüber, T.; Bartmann, C.; Krockenberger, M.; Wischhusen, J.; et al. The impact of breast cancer biological subtyping on tumor size assessment by ultrasound and mammography—A retrospective multicenter cohort study of 6543 primary breast cancer patients. BMC Cancer 2016, 16, 459. [Google Scholar] [CrossRef] [PubMed]
- Makanjuola, D.I.; AlKushi, A.; Al Anazi, K. Defining radiologic complete response using a correlation of presurgical ultrasound and mammographic localization findings with pathological complete response following neoadjuvant chemotherapy in breast cancer. Eur. J. Radiol. 2020, 130, 109146. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.J.; Kim, H.H.; Cha, J.H. Current status of automated breast ultrasonography. Ultrasonogarphy 2015, 34, 165–172. [Google Scholar] [CrossRef]
- Lizzi, F.L.; Ostromogilsky, M.; Feleppa, E.J.; Rorke, M.C.; Yaremko, M.M. Relationship of Ultrasonic Spectral Parameters to Features of Tissue Microstructure. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 1987, 34, 319–329. [Google Scholar] [CrossRef]
- Taggart, L.R.; Baddour, R.E.; Giles, A.; Czarnota, G.J.; Kolios, M.C. Ultrasonic Characterization of Whole Cells and Isolated Nuclei. Ultrasound Med. Biol. 2007, 33, 389–401. [Google Scholar] [CrossRef]
- Lin, C.; Cao, L.; Wang, J.; Zheng, W.; Chen, Y.; Feng, Z.; Li, A.; Zhou, J. Ultrasonic spectrum analysis for in vivo characterization of tumor microstructural changes in the evaluation of tumor response to chemotherapy using diagnostic ultrasound. BMC Cancer 2013, 13, 302. [Google Scholar] [CrossRef]
- Oelze, M.L.; O’Brien, W.D.; Blue, J.P.; Zachary, J.F. Differentiation and Characterization of Rat Mammary Fibroadenomas and 4T1 Mouse Carcinomas Using Quantitative Ultrasound Imaging. IEEE Trans. Med Imaging 2004, 23, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Naini, A.; Papanicolau, N.; Falou, O.; Zubovits, J.; Dent, R.; Verma, S.; Trudeau, M.; Boileau, J.F.; Spayne, J.; Iradji, S.; et al. Quantitative Ultrasound Evaluation of Tumor Cell Death Response in Locally Advanced Breast Cancer Patients Receiving Chemotherapy. Clin. Cancer Res. 2013, 19, 2163–2174. [Google Scholar] [CrossRef] [PubMed]
- Czarnota, G.J.; Kolios, M.C. Ultrasound detection of cell death. Imaging Med. 2010, 2, 17. [Google Scholar] [CrossRef]
- Klimonda, Z.; Karwat, P.; Dobruch-Sobczak, K.; Piotrzkowska-Wroblewska, H.; Litniewski, J. Breast-lesions characterization using Quantitative Ultrasound features of peritumoral tissue. Sci. Rep. 2019, 9, 7963. [Google Scholar] [CrossRef]
- Piotrzkowska-Wroblewska, H.; Dobruch-Sobczak, K.; Klimonda, Z.; Karwat, P.; Roszkowska-Purska, K.; Gumowska, M.; Litniewski, J. Monitoring breast cancer response to neoadjuvant chemotherapy with ultrasound signal statistics and integrated backscatter. PLoS ONE 2019, 14, e0213749. [Google Scholar] [CrossRef]
- Schrading, S.; Kuhl, C.K. Breast Cancer: Influence of Taxanes on Response Assessment with Dynamic Contrast-enhanced MR Imaging. Radiology 2015, 277, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Rauch, G.M.; Adrada, B.E.; Kuerer, H.M.; Van La Parra, R.F.D.; Leung, J.W.T.; Yang, W.T. Multimodality Imaging for Evaluating Response to Neoadjuvant Chemotherapy in Breast Cancer. Am. J. Roentgenol. 2017, 208, 290–299. [Google Scholar] [CrossRef]
- Weber, J.J.; Jochelson, M.S.; Eaton, A.; Zabor, E.C.; Barrio, A.V.; Gemignani, M.L.; Pilewskie, M.; Van Zee, K.J.; Morrow, M.; El-Tamer, M. MRI and Prediction of Pathologic Complete Response in the Breast and Axilla after Neoadjuvant Chemotherapy for Breast Cancer. J. Am. Coll. Surg. 2017, 225, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Hu, J.; Gu, H.; Hua, J.; Chen, J.; Xu, J. Can diffusion-weighted MR imaging and contrast-enhanced MR imaging precisely evaluate and predict pathological response to neoadjuvant chemotherapy in patients with breast cancer? Breast Cancer Res. Treat. 2012, 135, 17–28. [Google Scholar] [CrossRef]
- Hahn, S.Y.; Ko, E.Y.; Han, B.-K.; Shin, J.H. Role of diffusion-weighted imaging as an adjunct to contrast-enhanced breast MRI in evaluating residual breast cancer following neoadjuvant chemotherapy. Eur. J. Radiol. 2014, 83, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.J.; Kim, H.H.; Cha, J.H.; Shin, H.J.; Chae, E.Y. Comparison of Pathologic Response Evaluation Systems after Neoadjuvant Chemotherapy in Breast Cancers: Correlation With Computer-Aided Diagnosis of MRI Features. Am. J. Roentgenol. 2019, 213, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Romeo, V.; Picariello, V.; Pignata, A.; Mancusi, V.; Stanzione, A.; Cuocolo, R.; Di Crescenzo, R.; Accurso, A.; Staibano, S.; Imbriaco, M. Influence of different post-contrast time points on dynamic contrast-enhanced (DCE) MRI T staging in breast cancer. Eur. J. Radiol. 2020, 124, 108819. [Google Scholar] [CrossRef] [PubMed]
- Pasquero, G.; Surace, A.; Ponti, A.; Bortolini, M.; Tota, D.; Mano, M.P.; Arisio, R.; Benedetto, C.; Baù, M.G. Role of Magnetic Resonance Imaging in the Evaluation of Breast Cancer Response to Neoadjuvant Chemotherapy. In Vivo 2020, 34, 909–915. [Google Scholar] [CrossRef]
- Fukuda, T.; Horii, R.; Gomi, N.; Miyagi, Y.; Takahashi, S.; Ito, Y.; Akiyama, F.; Ohno, S.; Iwase, T. Accuracy of magnetic resonance imaging for predicting pathological complete response of breast cancer after neoadjuvant chemotherapy: Association with breast cancer subtype. SpringerPlus 2016, 5, 152. [Google Scholar] [CrossRef]
- Kim, Y.; Sim, S.H.; Park, B.; Chae, I.H.; Han, J.H.; Jung, S.-Y.; Lee, S.; Kwon, Y.; Park, I.H.; Ko, K.; et al. Criteria for identifying residual tumours after neoadjuvant chemotherapy of breast cancers: A magnetic resonance imaging study. Sci. Rep. 2021, 11, 634. [Google Scholar] [CrossRef]
- Dromain, C.; Violi, N.V.; Meuwly, J. Angiomammography: A review of current evidences. Diagn. Interv. Imaging 2019, 100, 593–605. [Google Scholar] [CrossRef] [PubMed]
- Iotti, V.; Ravaioli, S.; Vacondio, R.; Coriani, C.; Caffarri, S.; Sghedoni, R.; Nitrosi, A.; Ragazzi, M.; Gasparini, E.; Masini, C.; et al. Contrast-enhanced spectral mammography in neoadjuvant chemotherapy monitoring: A comparison with breast magnetic resonance imaging. Breast Cancer Res. 2017, 19, 106. [Google Scholar] [CrossRef]
- Patel, B.K.; Hilal, T.; Covington, M.; Zhang, N.; Kosiorek, H.E.; Lobbes, M.; Northfelt, D.W.; Pockaj, B.A. Contrast-Enhanced Spectral Mammography is Comparable to MRI in the Assessment of Residual Breast Cancer Following Neoadjuvant Systemic Therapy. Ann. Surg. Oncol. 2018, 25, 1350–1356. [Google Scholar] [CrossRef]
- Barra, F.R.; Sobrinho, A.B.; Barra, R.R.; Magalhães, M.T.; Aguiar, L.R.; De Albuquerque, G.F.L.; Costa, R.P.; Farage, L.; Pratesi, R. Contrast-Enhanced Mammography (CEM) for Detecting Residual Disease after Neoadjuvant Chemotherapy: A Comparison with Breast Magnetic Resonance Imaging (MRI). BioMed. Res. Int. 2018, 2018, 8531916. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Xiang, C.; Yang, Q. The diagnostic performance of CESM and CE-MRI in evaluating the pathological response to neoadjuvant therapy in breast cancer: A systematic review and meta-analysis. Br. J. Radiol. 2020, 93, 20200301. [Google Scholar] [CrossRef]
- Kitajima, K.; Nakatani, K.; Yamaguchi, K.; Nakajo, M.; Tani, A.; Ishibashi, M.; Hosoya, K.; Morita, T.; Kinoshita, T.; Kaida, H.; et al. Response to neoadjuvant chemotherapy for breast cancer judged by PERCIST—multicenter study in Japan. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1661–1671. [Google Scholar] [CrossRef]
- Noritake, M.; Narui, K.; Kaneta, T.; Sugae, S.; Sakamaki, K.; Inoue, T.; Ishikawa, T. Evaluation of the Response to Breast Cancer Neoadjuvant Chemotherapy Using 18 F-FDG Positron Emission Mammography Compared with Whole-Body 18 F-FDG PET: A Prospective Observational Study. Clin. Nucl. Med. 2017, 42, 169–175. [Google Scholar] [CrossRef]
- Sasada, S.; Masumoto, N.; Goda, N.; Kajitani, K.; Emi, A.; Kadoya, T.; Okada, M. Dedicated breast PET for detecting residual disease after neoadjuvant chemotherapy in operable breast cancer: A prospective cohort study. Eur. J. Surg. Oncol. 2018, 44, 444–448. [Google Scholar] [CrossRef]
- Koyasu, H.; Goshima, S.; Noda, Y.; Nishibori, H.; Takeuchi, M.; Matsunaga, K.; Yamada, T.; Matsuo, M. The feasibility of dedicated breast PET for the assessment of residual tumor after neoadjuvant chemotherapy. Jpn. J. Radiol. 2018, 37, 81–87. [Google Scholar] [CrossRef]
- Jarrett, A.M.; Hormuth, D.A.; Adhikarla, V.; Sahoo, P.; Abler, D.; Tumyan, L.; Schmolze, D.; Mortimer, J.; Rockne, R.C.; Yankeelov, T.E. Towards integration of 64Cu-DOTA-trastuzumab PET-CT and MRI with mathematical modeling to predict response to neoadjuvant therapy in HER2 + breast cancer. Sci. Rep. 2020, 10, 20518. [Google Scholar] [CrossRef]
- Gong, C.; Yang, Z.; Sun, Y.; Zhang, J.; Zheng, C.; Wang, L.; Zhang, Y.; Xue, J.; Yao, Z.; Pan, H.; et al. A preliminary study of 18F-FES PET/CT in predicting metastatic breast cancer in patients receiving docetaxel or fulvestrant with docetaxel. Sci. Rep. 2017, 7, 6584. [Google Scholar] [CrossRef] [PubMed]
- Ming, Y.; Wu, N.; Qian, T.; Li, X.; Wan, D.Q.; Li, C.; Li, Y.; Wu, Z.; Wang, X.; Liu, J.; et al. Progress and Future Trends in PET/CT and PET/MRI Molecular Imaging Approaches for Breast Cancer. Front. Oncol. 2020, 10, 1301. [Google Scholar] [CrossRef] [PubMed]
- Huppe, A.I.; Mehta, A.K.; Brem, R.F. Molecular Breast Imaging: A Comprehensive Review. Semin. Ultrasound CT MRI 2018, 39, 60–69. [Google Scholar] [CrossRef]
- Hunt, K.N.; Conners, A.L.; Goetz, M.P.; O’Connor, M.K.; Suman, V.; Kalari, K.; Weinshilboum, R.; Wang, L.; Carter, J.; McLaughlin, S.; et al. Comparison of 99mTc-sestamibi molecular breast imaging and breast MRI in patients with invasive breast cancer receiving neoadjuvant chemotherapy. Am. J. Roentgenol. 2019, 213, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Sutton, E.J.; Onishi, N.; Fehr, D.A.; Dashevsky, B.Z.; Sadinski, M.; Pinker, K.; Martinez, D.; Brogi, E.; Braunstein, L.; Razavi, P.; et al. A machine learning model that classifies breast cancer pathologic complete response on MRI post-neoadjuvant chemotherapy. Breast Cancer Res. 2020, 22, 57. [Google Scholar] [CrossRef]
- Taourel, P.; Pages, E.; Millet, I.; Bourgier, C.; Rouanet, P.; Jacot, W.; Crochet, P.; Azria, D. Magnetic resonance imaging in breast cancer management in the context of neo-adjuvant chemotherapy. Crit. Rev. Oncol. 2018, 132, 51–65. [Google Scholar] [CrossRef] [PubMed]
- Jun, W.; Cong, W.; Xianxin, X.; Daqing, J. Meta-Analysis of Quantitative Dynamic Contrast-Enhanced MRI for the Assessment of Neoadjuvant Chemotherapy in Breast Cancer. Am. Surg. 2019, 85, 645–653. [Google Scholar] [CrossRef]
- Tudorica, A.; Oh, K.Y.; Chui, S.Y.-C.; Roy, N.; Troxell, M.L.; Naik, A.; Kemmer, K.A.; Chen, Y.; Holtorf, M.L.; Afzal, A.; et al. Early Prediction and Evaluation of Breast Cancer Response to Neoadjuvant Chemotherapy Using Quantitative DCE-MRI. Transl. Oncol. 2016, 9, 8–17. [Google Scholar] [CrossRef]
- Romeo, V.; Cavaliere, C.; Imbriaco, M.; Verde, F.; Petretta, M.; Franzese, M.; Stanzione, A.; Cuocolo, R.; Aiello, M.; Basso, L.; et al. Tumor segmentation analysis at different post-contrast time points: A possible source of variability of quantitative DCE-MRI parameters in locally advanced breast cancer. Eur. J. Radiol. 2020, 126, 108907. [Google Scholar] [CrossRef]
- Garcia-Vicente, A.; Pérez-Beteta, J.; Amo-Salas, M.; Molina, D.; Jimenez-Londoño, G.; Soriano-Castrejón, A.; Pardo, F.P.; Martínez-González, A. Predictive and prognostic potential of volume-based metabolic variables obtained by a baseline 18 F-FDG PET/CT in breast cancer with neoadjuvant chemotherapy indication. Rev. Esp. Med. Nucl. Imagen Mol. 2018, 37, 73–79. [Google Scholar] [CrossRef]
- Soldevilla-Gallardo, I.; Villaseñor-Navarro, Y.; Medina-Ornelas, S.S.; Villarreal-Garza, C.; Bargalló-Rocha, E.; Caro-Sánchez, C.H.; Gallardo-Alvarado, L.N.; Hernández-Ramírez, R.; Arela-Quispe, L.M.; García-Pérez, F.O. Positron emission mammography in the evaluation of interim response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Cancer Treat. Res. Commun. 2018, 16, 24–31. [Google Scholar] [CrossRef]
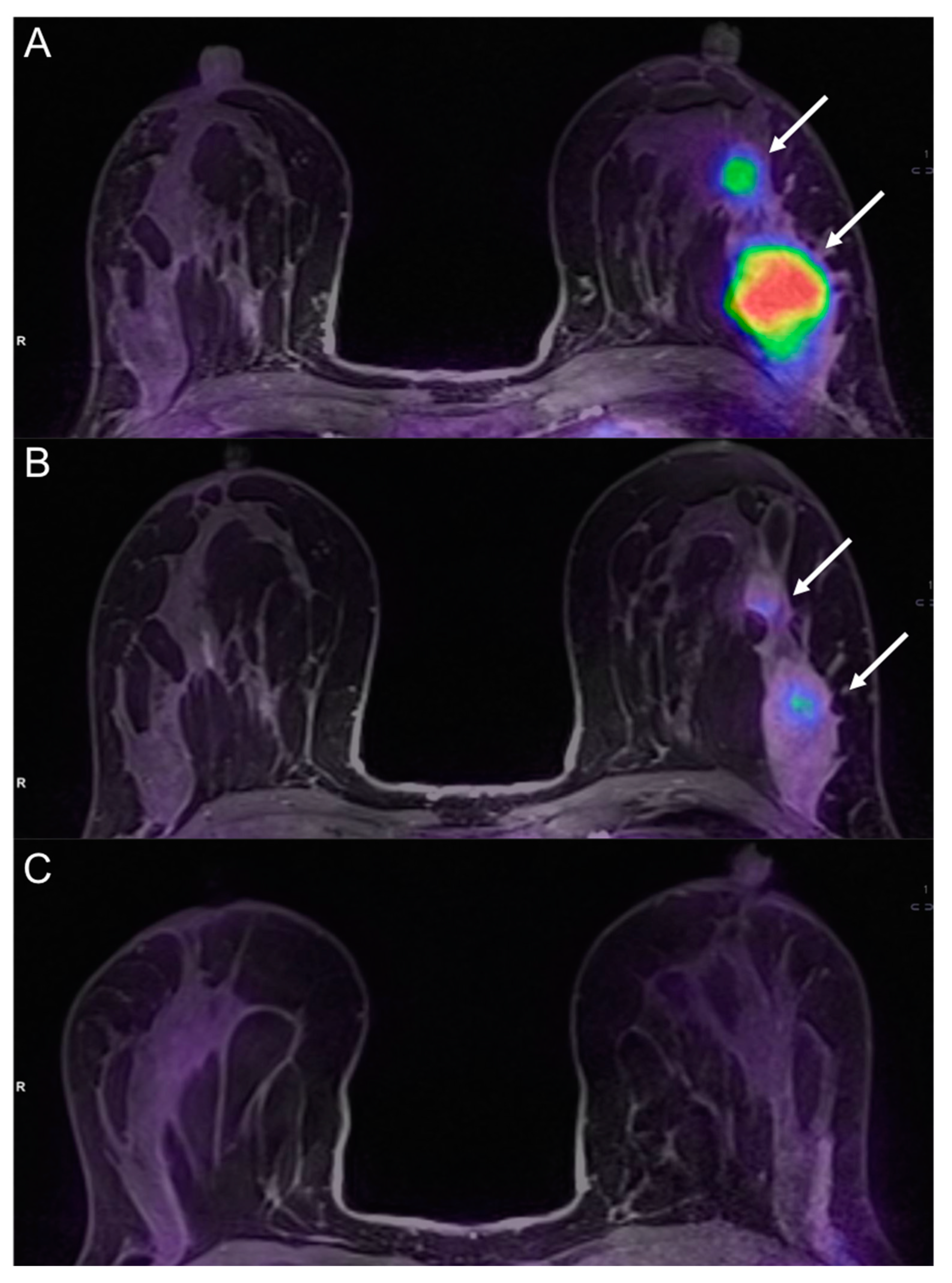
- Romeo, V.; D’Aiuto, M.; Frasci, G.; Imbriaco, M.; Nicolai, E. Simultaneous PET/MRI assessment of response to cytotoxic and hormone neo-adjuvant chemotherapy in breast cancer: A preliminary report. Med Oncol. 2016, 34, 18. [Google Scholar] [CrossRef]
- Cho, N.; Im, S.-A.; Cheon, G.J.; Park, I.-A.; Lee, K.-H.; Kim, T.-Y.; Kim, Y.S.; Kwon, B.R.; Lee, J.M.; Suh, H.Y.; et al. Integrated 18F-FDG PET/MRI in breast cancer: Early prediction of response to neoadjuvant chemotherapy. Eur. J. Nucl. Med. Mol. Imaging 2017, 45, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Shih, T.T.-F.; Yen, R.-F. Multiparametric Evaluation of Treatment Response to Neoadjuvant Chemotherapy in Breast Cancer Using Integrated PET/MR. Clin. Nucl. Med. 2017, 42, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Pengel, K.E.; Koolen, B.B.; Loo, C.E.; Vogel, W.V.; Wesseling, J.; Lips, E.H.; Rutgers, E.J.T.; Olmos, R.A.V.; Peeters, M.J.T.F.D.V.; Rodenhuis, S.; et al. Combined use of 18F-FDG PET/CT and MRI for response monitoring of breast cancer during neoadjuvant chemotherapy. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 1515–1524. [Google Scholar] [CrossRef] [PubMed]
- An, Y.Y.; Kim, S.H.; Kang, B.J.; Lee, A.W. Treatment Response Evaluation of Breast Cancer after Neoadjuvant Chemotherapy and Usefulness of the Imaging Parameters of MRI and PET/CT. J. Korean Med. Sci. 2015, 30, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Falou, O.; Soliman, H.; Sadeghi-Naini, A.; Iradji, S.; Lemon-Wong, S.; Zubovits, J.; Spayne, J.; Dent, R.; Trudeau, M.; Boileau, J.F.; et al. Diffuse Optical Spectroscopy Evaluation of Treatment Response in Women with Locally Advanced Breast Cancer Receiving Neoadjuvant Chemotherapy. Transl. Oncol. 2012, 5, 238–246. [Google Scholar] [CrossRef]
- Schelling, M.; Avril, N.; Nährig, J.; Kuhn, W.; Römer, W.; Sattler, D.; Werner, M.; Dose, J.; Jänicke, F.; Graeff, H.; et al. Positron Emission Tomography Using [18F]Fluorodeoxyglucose for Monitoring Primary Chemotherapy in Breast Cancer. J. Clin. Oncol. 2000, 18, 1689–1695. [Google Scholar] [CrossRef]
- Sharma, U.; Danishad, K.K.A.; Seenu, V.; Jagannathan, N.R. Longitudinal study of the assessment by MRI and diffusion-weighted imaging of tumor response in patients with locally advanced breast cancer undergoing neoadjuvant chemotherapy. NMR Biomed. 2009, 22, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Gullo, R.L.; Eskreis-Winkler, S.; Morris, E.A.; Pinker, K. Machine learning with multiparametric magnetic resonance imaging of the breast for early prediction of response to neoadjuvant chemotherapy. Breast 2020, 49, 115–122. [Google Scholar] [CrossRef]
- Fernandes, J.; Sannachi, L.; Tran, W.T.; Koven, A.; Watkins, E.; Hadizad, F.; Gandhi, S.; Wright, F.; Curpen, B.; El Kaffas, A.; et al. Monitoring Breast Cancer Response to Neoadjuvant Chemotherapy Using Ultrasound Strain Elastography. Transl. Oncol. 2019, 12, 1177–1184. [Google Scholar] [CrossRef]
- Ma, Y.; Zhang, S.; Zang, L.; Li, J.; Li, J.; Kang, Y.; Ren, W. Combination of shear wave elastography and Ki-67 index as a novel predictive modality for the pathological response to neoadjuvant chemotherapy in patients with invasive breast cancer. Eur. J. Cancer 2016, 69, 86–101. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.M.; Park, I.A.; Lee, S.H.; Kim, W.H.; Bae, M.S.; Koo, H.R.; Yi, A.; Kim, S.J.; Cho, N.; Moon, W.K. Stiffness of tumours measured by shear-wave elastography correlated with subtypes of breast cancer. Eur. Radiol. 2013, 23, 2450–2458. [Google Scholar] [CrossRef] [PubMed]
- Tadayyon, H.; Sannachi, L.; Gangeh, M.; Sadeghi-Naini, A.; Tran, W.; Trudeau, M.E.; Pritchard, K.; Ghandi, S.; Verma, S.; Czarnota, G.J. Quantitative ultrasound assessment of breast tumor response to chemotherapy using a multi-parameter approach. Oncotarget 2016, 7, 45094. [Google Scholar] [CrossRef]
- Tahmassebi, A.; Wengert, G.J.; Helbich, T.H.; Bago-Horvath, Z.; Alaei, S.; Bartsch, R.; Dubsky, P.; Baltzer, P.; Clauser, P.; Kapetas, P.; et al. Impact of Machine Learning With Multiparametric Magnetic Resonance Imaging of the Breast for Early Prediction of Response to Neoadjuvant Chemotherapy and Survival Outcomes in Breast Cancer Patients. Investig. Radiol. 2019, 54, 110–117. [Google Scholar] [CrossRef]
- Cain, E.H.; Saha, A.; Harowicz, M.R.; Marks, J.R.; Marcom, P.K.; Mazurowski, M.A. Multivariate machine learning models for prediction of pathologic response to neoadjuvant therapy in breast cancer using MRI features: A study using an independent validation set. Breast Cancer Res. Treat. 2019, 173, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Braman, N.M.; Etesami, M.; Prasanna, P.; Dubchuk, C.; Gilmore, H.; Tiwari, P.; Plecha, D.; Madabhushi, A. Intratumoral and peritumoral radiomics for the pretreatment prediction of pathological complete response to neoadjuvant chemotherapy based on breast DCE-MRI. Breast Cancer Res. 2017, 19, 1–14. [Google Scholar] [CrossRef]
- Braman, N.; Prasanna, P.; Whitney, J.; Singh, S.; Beig, N.; Etesami, M.; Bates, D.; Gallagher, K.; Bloch, B.N.; Vulchi, M.; et al. Association of Peritumoral Radiomics With Tumor Biology and Pathologic Response to Preoperative Targeted Therapy for HER2 (ERBB2)–Positive Breast Cancer. JAMA Netw. Open 2019, 2, e192561. [Google Scholar] [CrossRef]
- Chamming’S, F.; Ueno, Y.; Ferré, R.; Kao, E.; Jannot, A.-S.; Chong, J.; Omeroglu, A.; Mesurolle, B.; Reinhold, C.; Gallix, B. Features from Computerized Texture Analysis of Breast Cancers at Pretreatment MR Imaging Are Associated with Response to Neoadjuvant Chemotherapy. Radioloy 2018, 286, 412–420. [Google Scholar] [CrossRef]
- Liu, Z.; Li, Z.; Qu, J.; Zhang, R.; Zhou, X.; Li, L.; Sun, K.; Tang, Z.; Jiang, H.; Li, H.; et al. Radiomics of Multiparametric MRI for Pretreatment Prediction of Pathologic Complete Response to Neoadjuvant Chemotherapy in Breast Cancer: A Multicenter Study. Clin. Cancer Res. 2019, 25, 3538–3547. [Google Scholar] [CrossRef]
- Li, P.; Wang, X.; Xu, C.; Liu, C.; Zheng, C.; Fulham, M.; Feng, D.; Wang, L.; Song, S.; Huang, G. 18F-FDG PET/CT radiomic predictors of pathologic complete response (pCR) to neoadjuvant chemotherapy in breast cancer patients. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1116–1126. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Zhou, Z.; Yang, Z.; Chen, X.; Cheng, J.; Shao, Z.; Guo, X.; Tuan, J.; Fu, X.; Yu, X. The Value of 18F-FDG PET/CT Imaging Combined With Pretherapeutic Ki67 for Early Prediction of Pathologic Response After Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer. Medicine 2016, 95, e2914. [Google Scholar] [CrossRef] [PubMed]
- Antunovic, L.; De Sanctis, R.; Cozzi, L.; Kirienko, M.; Sagona, A.; Torrisi, R.; Tinterri, C.; Santoro, A.; Chiti, A.; Zelic, R.; et al. PET/CT radiomics in breast cancer: Promising tool for prediction of pathological response to neoadjuvant chemotherapy. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1468–1477. [Google Scholar] [CrossRef]





| Assessment of Residual Tumor after NAC | |
|---|---|
| Morphological imaging techniques | Ultrasound—US |
| Automated Breast Ultrasound—ABUS | |
| Quantitative ultrasound (QUS) methods | |
| Digital mammography—DM | |
| Digital breast tomosynthesis—DBT | |
| Advanced imaging techniques | Contrast-enhanced spectral mammography—CESM |
| Magnetic resonance imaging—MRI | |
| Dedicated breast positron emission tomography—DbPET | |
| Molecular Breast imaging—MBI | |
| Prediction of the Response to Treatment | |
| Advanced imaging techniques | MRI diffusion weighted imaging—DWI |
| MRI perfusion weighted imaging—PWI | |
| Hybrid imaging: PET/Computed Tomography (CT), PET/MRI | |
| Future Perspectives | |
| Radiomics and Artificial Intelligence | Texture analysis, Machine Learning, Deep learning |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romeo, V.; Accardo, G.; Perillo, T.; Basso, L.; Garbino, N.; Nicolai, E.; Maurea, S.; Salvatore, M. Assessment and Prediction of Response to Neoadjuvant Chemotherapy in Breast Cancer: A Comparison of Imaging Modalities and Future Perspectives. Cancers 2021, 13, 3521. https://doi.org/10.3390/cancers13143521
Romeo V, Accardo G, Perillo T, Basso L, Garbino N, Nicolai E, Maurea S, Salvatore M. Assessment and Prediction of Response to Neoadjuvant Chemotherapy in Breast Cancer: A Comparison of Imaging Modalities and Future Perspectives. Cancers. 2021; 13(14):3521. https://doi.org/10.3390/cancers13143521
Chicago/Turabian StyleRomeo, Valeria, Giuseppe Accardo, Teresa Perillo, Luca Basso, Nunzia Garbino, Emanuele Nicolai, Simone Maurea, and Marco Salvatore. 2021. "Assessment and Prediction of Response to Neoadjuvant Chemotherapy in Breast Cancer: A Comparison of Imaging Modalities and Future Perspectives" Cancers 13, no. 14: 3521. https://doi.org/10.3390/cancers13143521
APA StyleRomeo, V., Accardo, G., Perillo, T., Basso, L., Garbino, N., Nicolai, E., Maurea, S., & Salvatore, M. (2021). Assessment and Prediction of Response to Neoadjuvant Chemotherapy in Breast Cancer: A Comparison of Imaging Modalities and Future Perspectives. Cancers, 13(14), 3521. https://doi.org/10.3390/cancers13143521







