Primary Endoscopic Endonasal Management of Giant Pituitary Adenomas: Outcome and Pitfalls from a Large Prospective Multicenter Experience
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Data Collection
2.3. Endocrinological Evaluation
2.4. Ophtalmological Evaluation
2.5. Ethics
2.6. Statistical analysis
2.7. Surgical Technique
3. Results
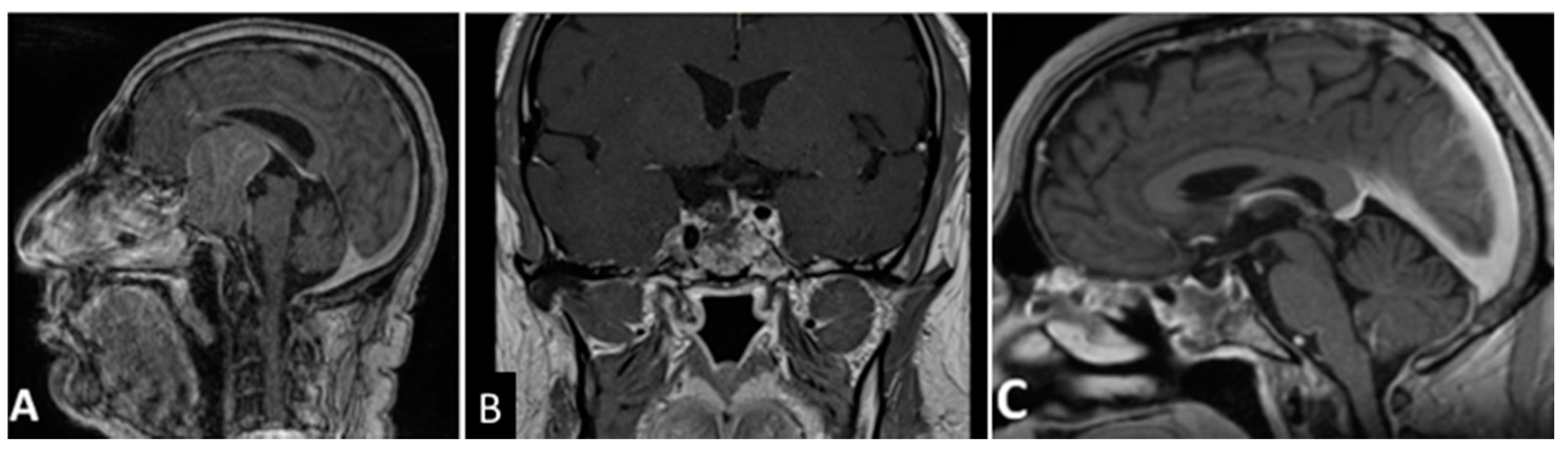
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melmed, S. Pathogenesis of pituitary tumors. Nat. Rev. Endocrinol. 2011, 7, 257–266. [Google Scholar] [CrossRef]
- Melmed, S. Mechanisms for pituitary tumorigenesis: The plastic pituitary. J. Clin. Investig. 2003, 112, 1603–1618. [Google Scholar] [CrossRef]
- Liu, J.K.; Couldwell, W.T. Contemporary management of prolactinomas. Neurosurg. Focus 2004, 16, E2. [Google Scholar] [CrossRef]
- Lopes, M.B.S. Growth hormone-secreting adenomas: Pathology and cell biology. Neurosurg. Focus 2010, 29, E2. [Google Scholar] [CrossRef] [PubMed]
- Tritos, N.A.; Biller, B.M.K.; Swearingen, B. Management of Cushing disease. Nat. Rev. Endocrinol. 2011, 7, 279–289. [Google Scholar] [CrossRef]
- Agrawal, A.; Cincu, R.; Goel, A. Current concepts and controversies in the management of non-functioning giant pituitary macroadenomas. Clin. Neurol. Neurosurg. 2007, 109, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, T.H.; Fraser, J.F.; Brown, S.; Tabaee, A.; Kacker, A.; Anand, V.K. Endoscopic Cranial Base Surgery: Classification of Operative Approaches. Neurosurgery 2008, 62, 991–1002, discussion 1002–1005. [Google Scholar] [CrossRef]
- Knosp, E.; Steiner, E.; Kitz, K.; Matula, C. Pituitary Adenomas with Invasion of the Cavernous Sinus Space. Neurosurgery 1993, 33, 610–617, discussion 617–618. [Google Scholar] [CrossRef] [PubMed]
- Chibbaro, S.; Cebula, H.; Todeschi, J.; Fricia, M.; Vigouroux, D.; Abid, H.; Kourbanhoussen, H.; Pop, R.; Nannavecchia, B.; Gubian, A.; et al. Evolution of Prophylaxis Protocols for Venous Thromboembolism in Neurosurgery: Results from a Prospective Comparative Study on Low-Molecular-Weight Heparin, Elastic Stockings, and Intermittent Pneumatic Compression Devices. World Neurosurg. 2018, 109, e510–e516. [Google Scholar] [CrossRef]
- Ganau, M.; Prisco, L.; Cebula, H.; Todeschi, J.; Abid, H.; Ligarotti, G.; Pop, R.; Proust, F.; Chibbaro, S. Risk of Deep vein thrombosis in neurosurgery: State of the art on prophylaxis protocols and best clinical practices. J. Clin. Neurosci. 2017, 45, 60–66. [Google Scholar] [CrossRef]
- Rutland, J.W.; Loewenstern, J.; Ranti, D.; Tsankova, N.M.; Bellaire, C.P.; Bederson, J.B.; Delman, B.N.; Shrivastava, R.K.; Balchandani, P. Analysis of 7-tesla diffusion-weighted imaging in the prediction of pituitary macroadenoma consistency. J. Neurosurg. 2020, 134, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Cuocolo, R.; Ugga, L.; Solari, D.; Corvino, S.; D’Amico, A.; Russo, D.; Cappabianca, P.; Cavallo, L.M.; Elefante, A. Prediction of pituitary adenoma surgical consistency: Radiomic data mining and machine learning on T2-weighted MRI. Neuroradiology 2020, 62, 1649–1656. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cappabianca, P.; Cavallo, L.M.; Esposito, F.; De Divitiis, O.; Messina, A.; De Divitiis, E. Extended endoscopic endonasal approach to the midline skull base: The evolving role of transsphenoidal surgery. Pediatric Craniovertebral Junction Dis. 2008, 33, 151–199. [Google Scholar] [CrossRef]
- Kassam, A.; Snyderman, C.H.; Mintz, A.; Gardner, P.; Carrau, R.L. Expanded endonasal approach: The rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg. Focus 2005, 19, 1–7. [Google Scholar] [CrossRef]
- Chibbaro, S.; Ganau, M.; Gubian, A.; Scibilia, A.; Todeschi, J.; Riehm, S.; Moliere, S.; DeBry, C.; Goichot, B.; Proust, F.; et al. The Role of Endoscopic Endonasal Approach in the Multimodal Management of Giant Pituitary Adenoma: Case Report and Literature Review. Asian J. Neurosurg. 2018, 13, 888–892. [Google Scholar]
- Cebula, H.; Kurbanov, A.; Zimmer, L.A.; Poczos, P.; Leach, J.L.; De Battista, J.C.; Froelich, S.; Theodosopoulos, P.V.; Keller, J.T. Endoscopic, Endonasal Variability in the Anatomy of the Internal Carotid Artery. World Neurosurg. 2014, 82, e759–e764. [Google Scholar] [CrossRef] [PubMed]
- Cappabianca, P.; Frank, G.; Pasquini, E.; de Divitiis, O.; Calbucci, F. Extended approach to the suprasellar region and planum sphenoidale. In Endoscopic Endonasal Transsphenoidal Surgery; de Divitiis, E., Cappabianca, P., Eds.; Springer: New York, NY, USA; Wien, Austria, 2003; pp. 176–182. [Google Scholar]
- Hadad, G.; Bassagasteguy, L.; Carrau, R.L.; Mataza, J.C.; Kassam, A.; Snyderman, C.H.; Mintz, A. A Novel Reconstructive Technique after Endoscopic Expanded Endonasal Approaches: Vascular Pedicle Nasoseptal Flap. Laryngoscope 2006, 116, 1882–1886. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Nadkarni, T.; Muzumdar, D.; Desai, K.; Phalke, U.; Sharma, P. Giant pituitary tumors: A study based on surgical treatment of 118 cases. Surg. Neurol. 2004, 61, 436–445, discussion 445–446. [Google Scholar] [CrossRef]
- Mortini, P.; Barzaghi, R.; Losa, M.; Boari, N.; Giovanelli, M. Surgical Treatment of Giant Pituitary Adenomas: Strategies and Results in a Series of 95 Consecutive Patients. Neurosurgery 2007, 60, 993–1002, discussion 1003–1004. [Google Scholar] [CrossRef]
- Kasper, G.; Samuel, N.; Alkins, R.; Khan, O.H. Practice patterns in the management of recurrent and residual non-functioning pituitary adenomas: Results from a Canada-wide survey. eNeurologicalSci 2021, 22, 100317. [Google Scholar] [CrossRef]
- Zhao, K.; Liu, X.; Liu, D.; Li, Y.; Zhang, Z.; Lin, Y.; Zhang, Y.; Xu, D. Fractionated Gamma Knife surgery for giant pituitary adenomas. Clin. Neurol. Neurosurg. 2016, 150, 139–142. [Google Scholar] [CrossRef]
- Ganau, M.; Foroni, R.I.; Gerosa, M.; Zivelonghi, E.; Longhi, M.; Nicolato, A. Radiosurgical options in neuro-oncology: A review on current tenets and future opportunities. Part I: Therapeutic strategies. Tumori J. 2014, 100, 459–465. [Google Scholar] [CrossRef]
- Ganau, M.; Foroni, R.I.; Gerosa, M.; Ricciardi, G.K.; Longhi, M.; Nicolato, A. Radiosurgical Options in Neuro-oncology: A Review on Current Tenets and Future Opportunities. Part II: Adjuvant Radiobiological Tools. Tumori J. 2015, 101, 57–63. [Google Scholar] [CrossRef]
- Neto, M.A.D.P.; Vandergrift, A.; Fatemi, N.; Gorgulho, A.A.; DeSalles, A.A.; Cohan, P.; Wang, C.; Swerdloff, R.; Kelly, D.F. Endonasal transsphenoidal surgery and multimodality treatment for giant pituitary adenomas. Clin. Endocrinol. (Oxf.) 2010, 72, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Chacko, G.; Chacko, A.G.; Lombardero, M.; Mani, S.; Seshadri, M.; Kovacs, K.; Scheithauer, B.W. Clinicopathologic correlates of giant pituitary adenomas. J. Clin. Neurosci. 2009, 16, 660–665. [Google Scholar] [CrossRef]
- Jane, J.A.; Han, J.; Prevedello, D.M.; Jagannathan, J.; Dumont, A.S.; Laws, E.R. Perspectives on endoscopic transsphenoidal surgery. Neurosurg. Focus 2005, 19, E2. [Google Scholar] [CrossRef] [PubMed]
- Xue-Fei, S.; Yong-Fei, W.; Shi-Qi, L.; Jing-Song, W.; Yao, Z.; Ying, M.; Liang-Fu, Z. Microsurgical treatment for giant and irregular pituitary adenomas in a series of 54 consecutive patients. Br. J. Neurosurg. 2008, 22, 636–648. [Google Scholar] [CrossRef] [PubMed]
- Chibbaro, S.; Ganau, M.; Cebula, H.; Nannavecchia, B.; Todeschi, J.; Romano, A.; DeBry, C.; Proust, F.; Olivi, A.; Gaillard, S.; et al. The Endonasal Endoscopic Approach to Pathologies of the Anterior Craniocervical Junction: Analytical Review of Cases Treated at Four European Neurosurgical Centres. Neurosurg. Med Ethics 2019, 125, 187–195. [Google Scholar] [CrossRef]
- Chibbaro, S.; Cebula, H.; Aldea, S.; Baussart, B.; Tigan, L.; Todeschi, J.; Romano, A.; Ganau, M.; Debry, C.; Servadei, F.; et al. Endonasal Endoscopic Odontoidectomy in Ventral Diseases of the Craniocervical Junction: Results of a Multicenter Experience. World Neurosurg. 2017, 106, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Chibbaro, S.; Cornelius, J.F.; Froelich, S.; Tigan, L.; Kehrli, P.; DeBry, C.; Romano, A.; Herman, P.; George, B.; Bresson, D. Endoscopic endonasal approach in the management of skull base chordomas—Clinical experience on a large series, technique, outcome, and pitfalls. Neurosurg. Rev. 2013, 37, 217–224, discussion 224–225. [Google Scholar] [CrossRef] [PubMed]
- Honegger, J.; Ernemann, U.; Psaras, T.; Will, B. Objective criteria for successful transsphenoidal removal of suprasellar nonfunctioning pituitary adenomas. A prospective study. Acta Neurochir. 2006, 149, 21–29, discussion 29. [Google Scholar] [CrossRef] [PubMed]
- Takakura, K.; Teramoto, A. Management of Huge Pituitary Adenomas. Mod. Neurosurg. Meningiomas Pituit. Adenomas 1996, 65, 13–15. [Google Scholar] [CrossRef]
- Koutourousiou, M.; Gardner, P.A.; Fernandez-Miranda, J.C.; Paluzzi, A.; Wang, E.; Snyderman, C.H. Endoscopic endonasal surgery for giant pituitary adenomas: Advantages and limitations. J. Neurosurg. 2013, 118, 621–631. [Google Scholar] [CrossRef] [Green Version]
- Yano, S.; Hide, T.; Shinojima, N. Efficacy and Complications of Endoscopic Skull Base Surgery for Giant Pituitary Adenomas. World Neurosurg. 2017, 99, 533–542. [Google Scholar] [CrossRef]
- Elshazly, K.; Kshettry, V.R.; Farrell, C.J.; Nyquist, G.; Rosen, M.; Evans, J.J. Clinical Outcomes After Endoscopic Endonasal Resection of Giant Pituitary Adenomas. World Neurosurg. 2018, 114, e447–e456. [Google Scholar] [CrossRef]
- Nakao, N.; Itakura, T. Surgical outcome of the endoscopic endonasal approach for non-functioning giant pituitary adenoma. J. Clin. Neurosci. 2011, 18, 71–75. [Google Scholar] [CrossRef]
- Kuo, C.-H.; Yen, Y.-S.; Wu, J.-C.; Chang, P.-Y.; Chang, H.-K.; Tu, T.-H.; Huang, W.-C.; Cheng, H. Primary Endoscopic Transnasal Transsphenoidal Surgery for Giant Pituitary Adenoma. World Neurosurg. 2016, 91, 121–128. [Google Scholar] [CrossRef]
- Cavallo, L.M.; Solari, D.; Somma, T.; Cappabianca, P. The 3F (Fat, Flap, and Flash) Technique for Skull Base Reconstruction after Endoscopic Endonasal Suprasellar Approach. World Neurosurg. 2019, 126, 439–446. [Google Scholar] [CrossRef]
- Buchfelder, M.; Kreutzer, J. Transcranial surgery for pituitary adenomas. Pituitary 2008, 11, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, M.M.; Karekezi, C.; Almeida, J.P.; Kalyvas, A.; Castro, V.; Velásquez, C.; Gentili, F. Management of Giant Pituitary Adenomas. Neurosurg. Clin. N. Am. 2019, 30, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Gondim, J.A.; Almeida, J.P.C.; Albuquerque, L.A.F.; Gomes, E.F.; Schops, M. Giant Pituitary Adenomas: Surgical Outcomes of 50 Cases Operated on by the Endonasal Endoscopic Approach. World Neurosurg. 2014, 82, e281–e290. [Google Scholar] [CrossRef]
- Dolenc, V.V. Transcranial Epidural Approach to Pituitary Tumors Extending beyond the Sella. Neurosurg. 1997, 41, 542–550, discussion 551–552. [Google Scholar] [CrossRef]
- Youssef, A.S.; Agazzi, S.; Van Loveren, H.R. Transcranial Surgery for Pituitary Adenomas. Oper. Neurosurg. 2005, 57, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Nawar, R.N.; AbdelMannan, D.; Selman, W.R.; Arafah, B.M. Analytic Review: Pituitary Tumor Apoplexy: A Review. J. Intensiv. Care Med. 2008, 23, 75–90. [Google Scholar] [CrossRef]
- Kurwale, N.S.; Ahmad, F.; Suri, A.; Kale, S.S.; Sharma, B.S.; Mahapatra, A.K.; Suri, V.; Sharma, M.C. Post operative pituitary apoplexy: Preoperative considerations toward preventing nightmare. Br. J. Neurosurg. 2011, 26, 59–63. [Google Scholar] [CrossRef]
- Wang, S.; Lin, S.; Wei, L.; Zhao, L.; Huang, Y. Analysis of operative efficacy for giant pituitary adenoma. BMC Surg. 2014, 14, 59. [Google Scholar] [CrossRef] [Green Version]
- Fatemi, N.; Dusick, J.R.; Neto, M.A.D.P.; Kelly, D.F. The Endonasal Microscopic Approach for Pituitary Adenomas and Other Parasellar Tumors: A 10-year Experience. Oper. Neurosurg. 2008, 63 (Suppl. 4), 244–256, discussion 256. [Google Scholar] [CrossRef]
- Nomikos, P.; Ladar, C.; Fahlbusch, R.; Buchfelder, M. Impact of primary surgery on pituitary function in patients with non-functioning pituitary adenomas—A study on 721 patients. Acta Neurochir. 2004, 146, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Dusick, J.R.; Esposito, F.; Kelly, D.F.; Cohan, P.; DeSalles, A.; Becker, D.P.; Martin, N. The extended direct endonasal transsphenoidal approach for nonadenomatous suprasellar tumors. J. Neurosurg. 2005, 102, 832–841. [Google Scholar] [CrossRef] [Green Version]



| Demographics | N. | % |
|---|---|---|
| Male | 55 | 57.3 |
| Female | 41 | 42.7 |
| Mean Age (years) | 52.2 (26–81) | |
| Mean tumor diameter (mm) | 46.5 (41–61) | |
| KNOSP Classification | ||
| Grade 0 | 30 | 31.2 |
| Grade 1 | 24 | 25.0 |
| Grade 2 | 19 | 19.8 |
| Grade 3 | 9 | 9.4 |
| Grade 4 | 14 | 14.6 |
| Endocrinological status | ||
| Non-functioning | 96 | 100 |
| Preoperative Clinical symptoms and signs | ||
| Visual field defects | 78 | 81.2 |
| Anterior pituitary insufficiency | 53 | 55.2 |
| Headache | 12 | 12.5 |
| Visual acuity deficit | 9 | 9.4 |
| Drowsiness | 3 | 3.1 |
| Treatment | ||
| EEA-TTP 1 | 96 | 100 |
| GPA consistency | ||
| Soft | 50 | 52.1 |
| Firm/fibrous | 46 | 47.9 |
| GPA vascularization | ||
| Significant | 31 | 32.3 |
| Not significant | 65 | 67.7 |
| Extent of resection | ||
| GTR 2 (100%) | 34 | 35.4 |
| NTR 3 (96 to 99%) | 12 | 12.5 |
| STR 4 (75 to 95%) | 50 | 52.1 |
| Clinical outcome | ||
| Visual improvement | 77 | 98.7 |
| Recovery of pituitary function | 27 | 50.9 |
| Surgical complications | ||
| CSF 5 leak | 7 | 7.3 |
| Meningitis | 7 | 7.3 |
| Apoplexy of residual tumor | 2 | 2.1 |
| Hydrocephalus | 1 | 1.0 |
| Right eye Blindness | 1 | 1.0 |
| Transient DI | 37 | 37.5 |
| Transient delayed hyponatremia | 20 | 20.8 |
| Progression | ||
| Yes | 16 | 16.7 |
| No | 80 | 83.3 |
| Treatment of 16 recurrences | ||
| Re-do EEA-TTP | 3 | 3.1 |
| GKRS 6 | 4 | 4.2 |
| SRT 7 | 9 | 9.4 |
| Surgical Approaches | EEA 1 | Microscopic Transsphenoidal | Transcranial | |
|---|---|---|---|---|
| Indications [20,21,22,23,24] | Medial wall cavernous invasion | Retro-chiasmatic extension of the tumor and expansion into the ventricular system | Temporal lobe invasion | |
| Tumor extending into planum sphenoidale amenable for transplanum EEA approach | Very large or dumbbellshaped tumors (usually more than 50 mm) extending into the planum sphenoidale, middle fossa or retro-chiasmatic region, especially in case of a shallow sella and/or narrow inter-carotid space | |||
| Contraindications [9,10,21,22] | Absolute | Tumor extension laterally to the supra-clinoidal part of the ICA 2 | N/A 3 | Cavernous invasion |
| Relative | N/A 3 | Cavernous invasion | N/A 3 | |
| Complications [19,31,41,42,46] | Visual deterioration | + | ++ | +++ |
| Postoperative cranial nerve dysfunction | + | ++ | +++ | |
| Pituitary function amelioration | ++ | + | + | |
| Diabetes Insipidus | + | ++ | +++ | |
| CSF leak | +++ | ++ | + | |
| Meningitis | + | ++ | ++ | |
| Mortality | + | + | + | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chibbaro, S.; Signorelli, F.; Milani, D.; Cebula, H.; Scibilia, A.; Bozzi, M.T.; Messina, R.; Zaed, I.; Todeschi, J.; Ollivier, I.; et al. Primary Endoscopic Endonasal Management of Giant Pituitary Adenomas: Outcome and Pitfalls from a Large Prospective Multicenter Experience. Cancers 2021, 13, 3603. https://doi.org/10.3390/cancers13143603
Chibbaro S, Signorelli F, Milani D, Cebula H, Scibilia A, Bozzi MT, Messina R, Zaed I, Todeschi J, Ollivier I, et al. Primary Endoscopic Endonasal Management of Giant Pituitary Adenomas: Outcome and Pitfalls from a Large Prospective Multicenter Experience. Cancers. 2021; 13(14):3603. https://doi.org/10.3390/cancers13143603
Chicago/Turabian StyleChibbaro, Salvatore, Francesco Signorelli, Davide Milani, Helene Cebula, Antonino Scibilia, Maria Teresa Bozzi, Raffaella Messina, Ismail Zaed, Julien Todeschi, Irene Ollivier, and et al. 2021. "Primary Endoscopic Endonasal Management of Giant Pituitary Adenomas: Outcome and Pitfalls from a Large Prospective Multicenter Experience" Cancers 13, no. 14: 3603. https://doi.org/10.3390/cancers13143603
APA StyleChibbaro, S., Signorelli, F., Milani, D., Cebula, H., Scibilia, A., Bozzi, M. T., Messina, R., Zaed, I., Todeschi, J., Ollivier, I., Mallereau, C. H., Dannhoff, G., Romano, A., Cammarota, F., Servadei, F., Pop, R., Baloglu, S., Lasio, G. B., Luca, F., ... Ganau, M. (2021). Primary Endoscopic Endonasal Management of Giant Pituitary Adenomas: Outcome and Pitfalls from a Large Prospective Multicenter Experience. Cancers, 13(14), 3603. https://doi.org/10.3390/cancers13143603









