Adherence to Treatment Guidelines and Associated Survival in Older Patients with Prostate Cancer: A Prospective Multicentre Cohort Study
Abstract
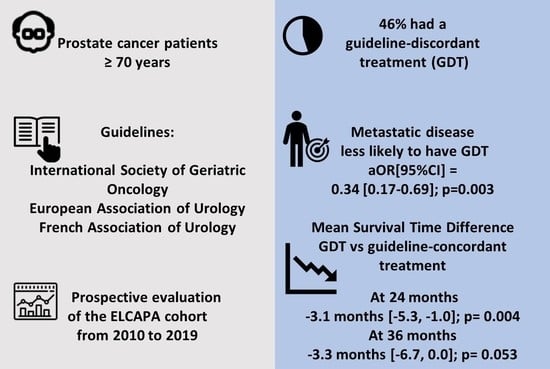
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Patients
2.2. Outcomes
2.3. Follow-Up
2.4. Covariates
2.5. Statistical Analysis
2.5.1. Evaluation of GDT
2.5.2. Survival Analysis
2.5.3. Estimation of the Propensity Score and Stabilized Weights
2.6. Sensitivity Analysis
3. Results
3.1. Study Population
3.2. Evaluation of GDT
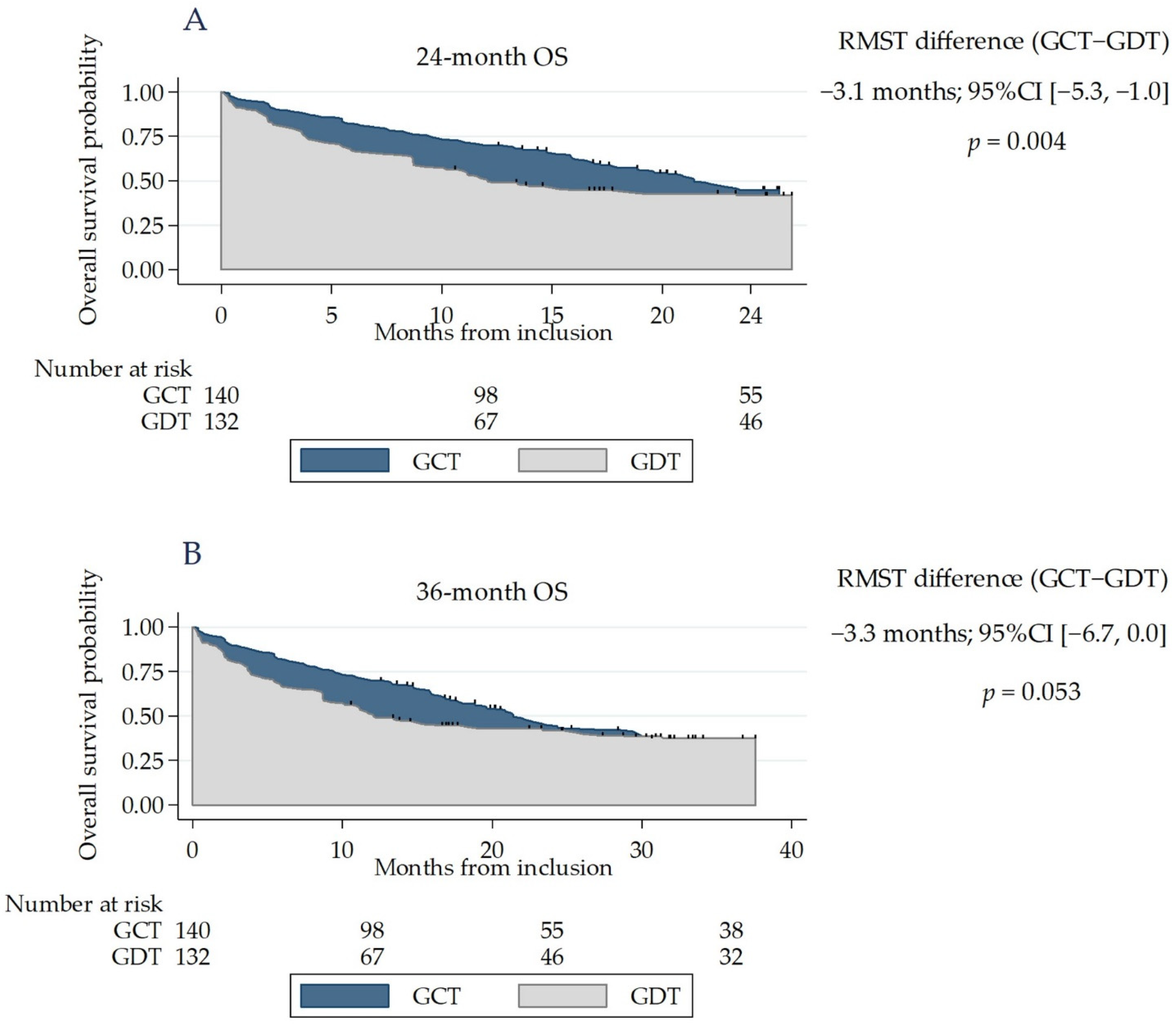
3.3. Survival
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Estimated Number of New Cases in 2018, Worldwide, Males, Ages 70+. Available online: http://gco.iarc.fr/today/home (accessed on 20 November 2020).
- World Health Organization Estimated Number of Incident Cases from 2018 to 2030, Prostate, Males, Ages 70+. Available online: http://gco.iarc.fr/tomorrow/home (accessed on 22 June 2020).
- Ferrat, E.; Audureau, E.; Paillaud, E.; Liuu, E.; Tournigand, C.; Lagrange, J.-L.; Canoui-Poitrine, F.; Caillet, P.; Bastuji-Garin, S. ELCAPA Study Group Four Distinct Health Profiles in Older Patients with Cancer: Latent Class Analysis of the Prospective ELCAPA Cohort. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2016, 71, 1653–1660. [Google Scholar] [CrossRef] [Green Version]
- Ferrat, E.; Paillaud, E.; Caillet, P.; Laurent, M.; Tournigand, C.; Lagrange, J.-L.; Droz, J.-P.; Balducci, L.; Audureau, E.; Canoui-Poitrine, F.; et al. Performance of Four Frailty Classifications in Older Patients with Cancer: Prospective Elderly Cancer Patients Cohort Study. J. Clin. Oncol. 2017, 35, 766–777. [Google Scholar] [CrossRef] [PubMed]
- Caillet, P.; Canoui-Poitrine, F.; Vouriot, J.; Berle, M.; Reinald, N.; Krypciak, S.; Bastuji-Garin, S.; Culine, S.; Paillaud, E. Comprehensive Geriatric Assessment in the Decision-Making Process in Elderly Patients with Cancer: ELCAPA Study. J. Clin. Oncol. 2011, 29, 3636–3642. [Google Scholar] [CrossRef] [PubMed]
- Ferrat, E.; Paillaud, E.; Laurent, M.; Le Thuaut, A.; Caillet, P.; Tournigand, C.; Lagrange, J.-L.; Canoui-Poitrine, F.; Bastuji-Garin, S. Predictors of 1-Year Mortality in a Prospective Cohort of Elderly Patients with Cancer. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2015, 70, 1148–1155. [Google Scholar] [CrossRef]
- Hurria, A.; Gupta, S.; Zauderer, M.; Zuckerman, E.L.; Cohen, H.J.; Muss, H.; Rodin, M.; Panageas, K.S.; Holland, J.C.; Saltz, L.; et al. Developing a cancer-specific geriatric assessment. Cancer 2005, 104, 1998–2005. [Google Scholar] [CrossRef]
- Paillaud, E.; Caillet, P.; Laurent, M.; Bastuji-Garin, S.; Liuu, E.; Lagrange, J.-L.; Culine, S.; Canoui-Poitrine, F. Optimal management of elderly cancer patients: Usefulness of the Comprehensive Geriatric Assessment. Clin. Interv. Aging 2014, 9, 1645–1660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balducci, L.; Extermann, M. Management of Cancer in the Older Person: A Practical Approach. Oncologist 2000, 5, 224–237. [Google Scholar] [CrossRef] [PubMed]
- Droz, J.-P.; Balducci, L.; Bolla, M.; Emberton, M.; Fitzpatrick, J.M.; Joniau, S.; Kattan, M.W.; Monfardini, S.; Moul, J.W.; Naeim, A.; et al. Management of Prostate Cancer in Older Men: Recommendations of a Working Group of the International Society of Geriatric Oncology. BJU Int. 2010, 106, 462–469. [Google Scholar] [CrossRef]
- Droz, J.-P.; Aapro, M.; Balducci, L.; Boyle, H.; Van den Broeck, T.; Cathcart, P.; Dickinson, L.; Efstathiou, E.; Emberton, M.; Fitzpatrick, J.M.; et al. Management of Prostate Cancer in Older Patients: Updated Recommendations of a Working Group of the International Society of Geriatric Oncology. Lancet Oncol. 2014, 15, e404–e414. [Google Scholar] [CrossRef]
- Droz, J.-P.; Albrand, G.; Gillessen, S.; Hughes, S.; Mottet, N.; Oudard, S.; Payne, H.; Puts, M.; Zulian, G.; Balducci, L.; et al. Management of Prostate Cancer in Elderly Patients: Recommendations of a Task Force of the International Society of Geriatric Oncology. Eur. Urol. 2017, 72, 521–531. [Google Scholar] [CrossRef]
- Boyle, H.; Alibhai, S.; Decoster, L.; Efstathiou, E.; Fizazi, K.; Mottet, N.; Oudard, S.; Payne, H.; Prentice, M.; Puts, M.; et al. Updated recommendations of the International Society of Geriatric Oncology on prostate cancer management in older patients. Eur. J. Cancer 2019, 116, 116–136. [Google Scholar] [CrossRef] [PubMed]
- Nadpara, P.A.; Madhavan, S.S.; Tworek, C.; Sambamoorthi, U.; Hendryx, M.; Almubarak, M. Guideline-concordant lung cancer care and associated health outcomes among elderly patients in the United States. J. Geriatr. Oncol. 2015, 6, 101–110. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; Zhang, N.; Ho, V.; Ding, M.; He, W.; Niu, J.; Yang, M.; Du, X.L.; Zorzi, D.; Chavez-MacGregor, M.; et al. Adherence to treatment guidelines and survival for older patients with stage II or III colon cancer in Texas from 2001 through 2011. Cancer 2018, 124, 679–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mongiat-Artus, P.; Peyromaure, M.; Richaud, P.; Droz, J.-P.; Rainfray, M.; Jeandel, C.; Rebillard, X.; Moreau, J.-L.; Davin, J.-L.; Salomon, L.; et al. Recommandations pour la prise en charge du cancer de la prostate chez l’homme âgé: Un travail du comité de cancérologie de l’association française d’urologie. Progrès En Urol. 2009, 19, 810–817. [Google Scholar] [CrossRef]
- Fang, P.; He, W.; Gomez, D.R.; Hoffman, K.E.; Smith, B.D.; Giordano, S.H.; Jagsi, R.; Smith, G.L. Influence of Age on Guideline-Concordant Cancer Care for Elderly Patients in the United States. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, A.; Bastian, P.J.; Bellmunt, J.; Bolla, M.; Joniau, S.; Mason, M.D.; Matveev, V.; Mottet, N.; Van der Kwast, T.; Wiegel, T.; et al. Guidelines on Prostate Cancer 2012. Available online: https://uroweb.org/wp-content/uploads/08-Prostate-Cancer_LR-March-13th-20122.pdf (accessed on 9 November 2020).
- Heidenreich, A.; Bastian, P.J.; Bellmunt, J.; Bolla, M.; Joniau, S.; Mason, M.; Matveev, V.; Mottet, N.; Van der Kwast, T.; Wiegel, T.; et al. Guidelines on Prostate Cancer 2013. Available online: https://uroweb.org/wp-content/uploads/09_Prostate_Cancer_LR.pdf (accessed on 13 November 2020).
- Mottet, N.; Bastian, P.J.; Bellmunt, J.; van der Bergh, R.; Bolla, M.; van Casteren, N.; Cornford, P.; Joniau, S.; Mason, M.; Matveev, V.; et al. Guidelines on Prostate Cancer 2014. Available online: https://uroweb.org/wp-content/uploads/1607-Prostate-Cancer_LRV3.pdf (accessed on 9 November 2020).
- Mottet, N.; Bellmunt, J.; Briers, E.; van der Bergh, R.; Bolla, M.; van Casteren, N.; Cornford, P.; Culine, S.; Joniau, S.; Lam, T.; et al. Guidelines on Prostate Cancer 2015. Available online: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Prostate-Cancer-2015-v2.pdf (accessed on 13 November 2020).
- Mottet, N.; Bellmunt, J.; Briers, E.; Bolla, M.; Cornford, P.; De Santis, M.; Henry, A.; Joniau, S.; Lam, T.; Mason, M.; et al. Guidelines on Prostate Cancer 2016. Available online: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Prostate-Cancer-2016-1.pdf (accessed on 13 November 2020).
- Mottet, N.; Bellmunt, J.; Briers, E.; Bolla, M.; Bourke, L.; Cornford, P.; De Santis, M.; Henry, A.; Joniau, S.; Lam, T.; et al. Guidelines on Prostate Cancer 2017. Available online: https://uroweb.org/wp-content/uploads/09-Prostate-Cancer_2017_web.pdf (accessed on 13 November 2020).
- Mottet, N.; van der Bergh, R.; Briers, E.; Bourke, L.; Cornford, P.; De Santis, M.; Gillessen, S.; Govorov, A.; Grummet, J.; Henry, A.; et al. Guidelines on Prostate Cancer 2018. Available online: https://uroweb.org/wp-content/uploads/EAU-ESUR-ESTRO-SIOG-Guidelines-on-Prostate-Cancer-large-text-V2.pdf (accessed on 13 November 2020).
- Salomon, L.; Azria, D.; Bastide, C.; Beuzeboc, P.; Cormier, L.; Cornud, F.; Eiss, D.; Eschwège, P.; Gaschignard, N.; Hennequin, C.; et al. Recommandations en Onco-Urologie 2010: Cancer de la prostate. Progrès En Urol. 2010, 20, S217–S251. [Google Scholar] [CrossRef]
- Salomon, L.; Bastide, C.; Beuzeboc, P.; Cormier, L.; Fromont, G.; Hennequin, C.; Mongiat-Artus, P.; Peyromaure, M.; Ploussard, G.; Renard-Penna, R.; et al. Recommandations en onco-urologie 2013 du CCAFU: Cancer de la prostate. Progrès En Urol. 2013, 23, S69–S101. [Google Scholar] [CrossRef]
- Rozet, F.; Hennequin, C.; Beauval, J.-B.; Beuzeboc, P.; Cormier, L.; Fromont, G.; Mongiat-Artus, P.; Ouzzane, A.; Ploussard, G.; Azria, D.; et al. Recommandations en onco-urologie 2016-2018 du CCAFU: Cancer de la prostate. Progrès En Urol. 2016, 27, S95–S143. [Google Scholar] [CrossRef]
- Sohlberg, E.M.; Thomas, I.-C.; Yang, J.; Kapphahn, K.; Daskivich, T.J.; Skolarus, T.A.; Shelton, J.B.; Makarov, D.V.; Bergman, J.; Bang, C.K.; et al. Life expectancy estimates for patients diagnosed with prostate cancer in the Veterans Health Administration. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 734.e1–734.e10. [Google Scholar] [CrossRef]
- Trinquart, L.; Bill-Axelson, A.; Rider, J.R. Restricted Mean Survival Times to Improve Communication of Evidence from Cancer Randomized Trials and Observational Studies. Eur. Urol. 2019, 76, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Marshall, A.; Altman, D.G.; Holder, R.L.; Royston, P. Combining estimates of interest in prognostic modelling studies after multiple imputation: Current practice and guidelines. BMC Med. Res. Methodol. 2009, 9, 57. [Google Scholar] [CrossRef] [Green Version]
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015, 34, 3661–3679. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern Med. 2017, 167, 268. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.C.; Carpenter, W.R.; Hendrix, L.H.; Bainbridge, J.; Wang, A.Z.; Nielsen, M.E.; Godley, P.A. Receipt of Guideline-Concordant Treatment in Elderly Prostate Cancer Patients. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, A.S.; Fleming, S.T.; Wang, D.; Goodman, M.; Wu, X.-C.; Owen, J.B.; Lo, M.; Ho, A.; Anderson, R.T.; Thompson, T. Clinical and Demographic Factors Associated with Receipt of Non Guideline-concordant Initial Therapy for Nonmetastatic Prostate Cancer. Am. J. Clin. Oncol. 2016, 39, 55–63. [Google Scholar] [CrossRef] [Green Version]
- Ellis, S.D.; Blackard, B.; Carpenter, W.R.; Mishel, M.; Chen, R.C.; Godley, P.A.; Mohler, J.L.; Bensen, J.T. Receipt of National Comprehensive Cancer Network guideline-concordant prostate cancer care among African American and Caucasian American men in North Carolina. Cancer 2013, 119, 2282–2290. [Google Scholar] [CrossRef]
- Schwam, Z.; Sosa, J.; Roman, S.; Judson, B. Receipt of Care Discordant with Practice Guidelines is Associated with Compromised Overall Survival in Nasopharyngeal Carcinoma. Clin. Oncol. 2016, 28, 402–409. [Google Scholar] [CrossRef]
- Kenis, C.; Bron, D.; Libert, Y.; Decoster, L.; Van Puyvelde, K.; Scalliet, P.; Cornette, P.; Pepersack, T.; Luce, S.; Langenaeken, C.; et al. Relevance of a systematic geriatric screening and assessment in older patients with cancer: Results of a prospective multicentric study. Ann. Oncol. 2013, 24, 1306–1312. [Google Scholar] [CrossRef] [PubMed]
- Bolenz, C.; Ho, R.; Nuss, G.R.; Ortiz, N.; Raj, G.V.; Sagalowsky, A.I.; Lotan, Y. Management of elderly patients with urothelial carcinoma of the bladder: Guideline concordance and predictors of overall survival. BJU Int. 2010, 106, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Dumontier, C.; Loh, K.P.; Bain, P.A.; Silliman, R.A.; Hshieh, T.; Abel, G.A.; Djulbegovic, B.; Driver, J.A.; Dale, W. Defining Undertreatment and Overtreatment in Older Adults with Cancer: A Scoping Literature Review. J. Clin. Oncol. 2020, 38, 2558–2569. [Google Scholar] [CrossRef] [PubMed]
- Wood, M.E.; Chrysanthopoulou, S.; Nordeng, H.M.; Lapane, K.L. The Impact of Nondifferential Exposure Misclassification on the Performance of Propensity Scores for Continuous and Binary Outcomes: A Simulation Study. Med. Care 2018, 56, e46–e53. [Google Scholar] [CrossRef] [PubMed]
- Bierbaum, M.; Rapport, F.; Arnolda, G.; Easpaig, B.N.G.; Lamprell, K.; Hutchinson, K.; Delaney, G.P.; Liauw, W.; Kefford, R.; Olver, I.; et al. Clinicians’ attitudes and perceived barriers and facilitators to cancer treatment clinical practice guideline adherence: A systematic review of qualitative and quantitative literature. Implement. Sci. 2020, 15, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Fischer, F.; Lange, K.; Klose, K.; Greiner, W.; Kraemer, A. Barriers and Strategies in Guideline Implementation—A Scoping Review. Healthcare 2016, 4, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gillessen, S.; Attard, G.; Beer, T.M.; Beltran, H.; Bossi, A.; Bristow, R.; Carver, B.; Castellano, D.; Chung, B.H.; Clarke, N.; et al. Management of Patients with Advanced Prostate Cancer: The Report of the Advanced Prostate Cancer Consensus Conference APCCC 2017. Eur. Urol. 2017, 73, 178–211. [Google Scholar] [CrossRef] [Green Version]
- Gillessen, S.; Attard, G.; Beer, T.M.; Beltran, H.; Bjartell, A.; Bossi, A.; Briganti, A.; Bristow, R.; Chi, K.N.; Clarke, N.; et al. Management of Patients with Advanced Prostate Cancer: Report of the Advanced Prostate Cancer Consensus Conference 2019. Eur. Urol. 2020, 77, 508–547. [Google Scholar] [CrossRef]


| Variable | Category | Adjusted OR (95% CI) | |
|---|---|---|---|
| (n = 190) | p | ||
| Mobility (G8 score item) | Goes out | 1 | |
| Able to get out of bed/chair but does not go out | 1.79 (0.51–6.25) | 0.36 | |
| Bed- or chair-bound | 0.91 (0.37–2.26) | 0.84 | |
| Age | <80 | 1 | |
| 80–85 | 0.87 (0.35–2.15) | 0.76 | |
| >86 | 0.58 (0.28–1.18) | 0.13 | |
| Risk of Depression | No | 1 | |
| Yes | 0.55 (0.28–1.1) | 0.09 | |
| Cognitive Impairment | No | 1 | |
| Yes | 1.20 (0.56–2.53) | 0.64 | |
| Gleason Score | ≤6 | 1 | |
| 7 | 0.73 (0.26–2.03) | 0.55 | |
| 8 à 10 | 0.85 (0.32–2.25) | 0.74 | |
| Serum PSA Level | Log PSA | 0.96 (0.79–1.16) | 0.64 |
| Clinical Stage | Non-metastatic | 1 | |
| Metastatic | 0.34 (0.17–0.69) | 0.003 | |
| Characteristic | Original Cohort | Weighted Cohort * | ||||
|---|---|---|---|---|---|---|
| GCT (%) | GDT (%) | SMD | GCT (%) | GDT (%) | SMD | |
| n = 275 | n = 143 | n = 132 | ||||
| G8 score | ||||||
| ≤14 | 113 (80) | 100 (77) | −0.04 | 78 | 78 | −0.008 |
| Activities of Daily Living score | ||||||
| ≥1 abnormal item | 15 (10) | 18 (14) | 0.14 | 11 | 12 | 0.02 |
| Instrumental Activities of Daily Living score | ||||||
| ≥1 abnormal item | 55 (40) | 43 (35) | 0.2 | 40 | 39 | −0.03 |
| Mobility (G8 score item) | ||||||
| Goes out | 90 (66) | 93 (74) | −0.04 | 70 | 69 | −0.02 |
| Able to get out of bed/chair but does not go out | 31 (23) | 17 (14) | 19 | 19 | ||
| Bed- or chair-bound | 15 (11) | 15 (12) | 11 | 12 | ||
| Age | ||||||
| <80 | 57 (40) | 76 (54) | −0.2 | 47 | 50 | −0.07 |
| 81–90 | 71 (50) | 57 (42) | 46 | 43 | ||
| >90 | 15 (10) | 5 (4) | 7 | 7 | ||
| Cumulative Illness Rating Scale for Geriatrics grade 3 or 4 comorbidities | ||||||
| At least one | 93 (68) | 92 (71) | 0.15 | 70 | 70 | −0.001 |
| Eastern Cooperative Oncology Group performance status | ||||||
| 0–1 | 69 (49) | 78 (59) | 0.09 | 55 | 53 | 0.03 |
| 2 | 37 (26) | 25 (19) | 22 | 23 | ||
| 3–4 | 36 (25) | 29 (22) | 23 | 24 | ||
| Risk of depression | ||||||
| Yes | 55 (41) | 40 (31) | −0.3 | 38 | 37 | −0.02 |
| Cognitive impairment | ||||||
| Yes | 52 (37) | 29 (23) | −0.12 | 32 | 31 | −0.02 |
| Weight loss | ||||||
| <5% | 88 (62) | 87 (66) | −0.08 | 65 | 67 | 0.04 |
| 5–10% | 29 (20) | 18 (14) | 20 | 12 | ||
| >10% | 25 (18) | 26 (20) | 15 | 21 | ||
| Gleason score | ||||||
| ≤6 | 9 (10) | 16 (16) | −0.2 | 11 | 9 | 0.06 |
| 7 | 31 (34) | 42 (42) | 35 | 36 | ||
| 8 to 10 | 51 (56) | 41 (41) | 54 | 55 | ||
| Serum PSA level (median (IQR)) | ||||||
| Log PSA | 3.7 (2.9–4.9) | 3.1 (2.2–4.8) | −0.2 | 3.7 (2.8–4.8) | 3.1 (2.2–4.6) | 0.01 |
| Clinical stage | ||||||
| Metastatic | 105 (73) | 62 (48) | −0.3 | 63 | 62 | −0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González Serrano, A.; Martínez Tapia, C.; de la Taille, A.; Mongiat-Artus, P.; Irani, J.; Bex, A.; Paillaud, E.; Audureau, E.; Barnay, T.; Laurent, M.; et al. Adherence to Treatment Guidelines and Associated Survival in Older Patients with Prostate Cancer: A Prospective Multicentre Cohort Study. Cancers 2021, 13, 4694. https://doi.org/10.3390/cancers13184694
González Serrano A, Martínez Tapia C, de la Taille A, Mongiat-Artus P, Irani J, Bex A, Paillaud E, Audureau E, Barnay T, Laurent M, et al. Adherence to Treatment Guidelines and Associated Survival in Older Patients with Prostate Cancer: A Prospective Multicentre Cohort Study. Cancers. 2021; 13(18):4694. https://doi.org/10.3390/cancers13184694
Chicago/Turabian StyleGonzález Serrano, Adolfo, Claudia Martínez Tapia, Alexandre de la Taille, Pierre Mongiat-Artus, Jacques Irani, Axel Bex, Elena Paillaud, Etienne Audureau, Thomas Barnay, Marie Laurent, and et al. 2021. "Adherence to Treatment Guidelines and Associated Survival in Older Patients with Prostate Cancer: A Prospective Multicentre Cohort Study" Cancers 13, no. 18: 4694. https://doi.org/10.3390/cancers13184694
APA StyleGonzález Serrano, A., Martínez Tapia, C., de la Taille, A., Mongiat-Artus, P., Irani, J., Bex, A., Paillaud, E., Audureau, E., Barnay, T., Laurent, M., & Canouï-Poitrine, F. (2021). Adherence to Treatment Guidelines and Associated Survival in Older Patients with Prostate Cancer: A Prospective Multicentre Cohort Study. Cancers, 13(18), 4694. https://doi.org/10.3390/cancers13184694