Epstein–Barr Virus in Inborn Immunodeficiency—More Than Infection
Abstract
:Simple Summary
Abstract
1. Introduction
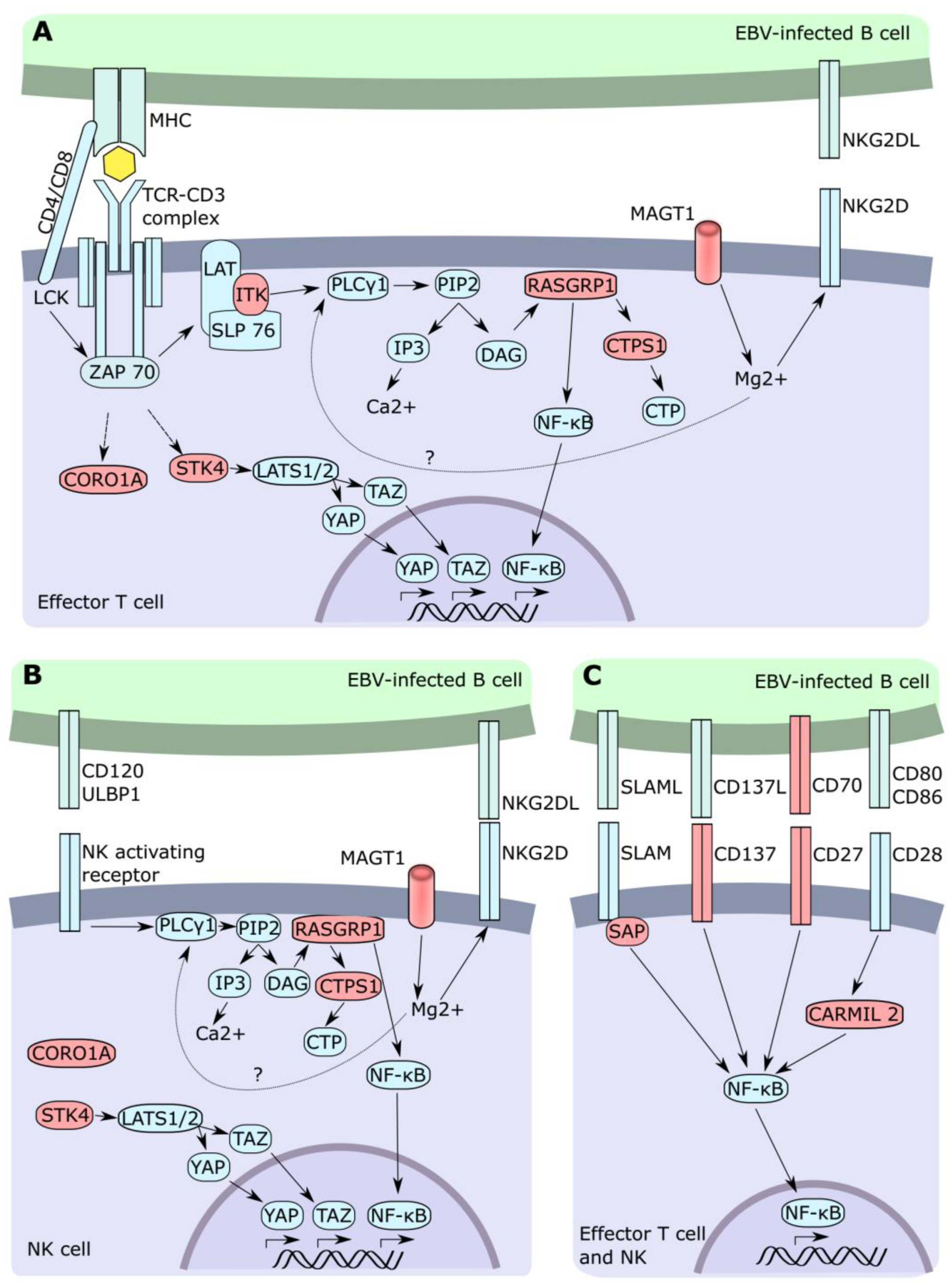
2. Inborn Errors of Immunity (IEI)
3. CD27-CD70 Deficiency
4. CD137 (TNFRSF9, 4-1BB) Deficiency
5. ITK Deficiency
6. RASGRP1 Deficiency
7. CTPS1 Deficiency
8. MAGT1 Deficiency (XMEN Syndrome)
9. Coronin 1A Deficiency
10. STK4 (MST1) Deficiency
11. CARMIL2 (RLTPR) Deficiency
12. SH2D1A (XLP1 Syndrome) and XIAP Deficiency (XLP2 Syndrome)
13. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pereira, M.S.; Blake, J.M.; Macrae, A.D. EB Virus Antibody at Different Ages. BMJ 1969, 4, 526–527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, C.D.; Swerdlow, A.J.; Macsween, K.F.; Harrison, N.; Williams, H.; McAulay, K.; Thomas, R.; Reid, S.; Conacher, M.; Britton, K.; et al. A Study of Risk Factors for Acquisition of Epstein-Barr Virus and Its Subtypes. J. Infect. Dis. 2007, 195, 474–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de-Thé, G.; Geser, A.; Day, N.E.; Tukei, P.M.; Williams, E.H.; Beri, D.P.; Smith, P.G.; Dean, A.G.; Bornkamm, G.W.; Feorino, P.; et al. Epidemiological Evidence for Causal Relationship between Epstein-Barr Virus and Burkitt’s Lymphoma from Ugandan Prospective Study. Nature 1978, 274, 756–761. [Google Scholar] [CrossRef]
- Dunmire, S.K.; Hogquist, K.A.; Balfour, H.H. Infectious Mononucleosis. In Current Topics in Microbiology and Immunology; Springer: Berlin/Heidelberg, Germany, 2015; Volume 390, pp. 211–240. [Google Scholar]
- Dunnet, W.N. Infectious Mononucleosis. BMJ 1963, 1, 1187–1191. [Google Scholar] [CrossRef] [PubMed]
- Temple, R.M.; Zhu, J.; Budgeon, L.; Christensen, N.D.; Meyers, C.; Sample, C.E. Efficient Replication of Epstein–Barr Virus in Stratified Epithelium In Vitro. Proc. Natl. Acad. Sci. USA 2014, 111, 16544–16549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, L.S.; Yap, L.F.; Murray, P.G. Epstein–Barr Virus: More than 50 Years Old and Still Providing Surprises. Nat. Rev. Cancer 2016, 16, 789–802. [Google Scholar] [CrossRef]
- Rezk, S.A.; Zhao, X.; Weiss, L.M. Epstein-Barr Virus (EBV)–Associated Lymphoid Proliferations, a 2018 Update. Hum. Pathol. 2018, 79, 18–41. [Google Scholar] [CrossRef]
- Kang, M.-S.; Kieff, E. Epstein–Barr Virus Latent Genes. Exp. Mol. Med. 2015, 47, e131. [Google Scholar] [CrossRef] [Green Version]
- Babcock, G.J.; Hochberg, D.; Thorley-Lawson, D.A. The Expression Pattern of Epstein-Barr Virus Latent Genes In Vivo Is Dependent upon the Differentiation Stage of the Infected B Cell. Immunity 2000, 13, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Murray, R.J.; Kurilla, M.G.; Brooks, J.M.; Thomas, W.A.; Rowe, M.; Kieff, E.; Rickinson, A.B. Identification of Target Antigens for the Human Cytotoxic T Cell Response to Epstein-Barr Virus (EBV): Implications for the Immune Control of EBV-Positive Malignancies. J. Exp. Med. 1992, 176, 157–168. [Google Scholar] [CrossRef] [Green Version]
- Blake, N.; Haigh, T.; Shaka’a, G.; Croom-Carter, D.; Rickinson, A. The Importance of Exogenous Antigen in Priming the Human CD8+ T Cell Response: Lessons from the EBV Nuclear Antigen EBNA1. J. Immunol. 2000, 165, 7078–7087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khanna, R.; Burrows, S.R.; Kurilla, M.G.; Jacob, C.A.; Misko, I.S.; Sculley, T.B.; Kieff, E.; Moss, D.J. Localization of Epstein-Barr Virus Cytotoxic T Cell Epitopes Using Recombinant Vaccinia: Implications for Vaccine Development. J. Exp. Med. 1992, 176, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Pappworth, I.Y.; Wang, E.C.; Rowe, M. The Switch from Latent to Productive Infection in Epstein-Barr Virus-Infected B Cells Is Associated with Sensitization to NK Cell Killing. J. Virol. 2007, 81, 474–482. [Google Scholar] [CrossRef] [Green Version]
- Chijioke, O.; Müller, A.; Feederle, R.; Barros, M.H.M.; Krieg, C.; Emmel, V.; Marcenaro, E.; Leung, C.S.; Antsiferova, O.; Landtwing, V.; et al. Human Natural Killer Cells Prevent Infectious Mononucleosis Features by Targeting Lytic Epstein-Barr Virus Infection. Cell Rep. 2013, 5, 1489–1498. [Google Scholar] [CrossRef] [Green Version]
- Azzi, T.; Lünemann, A.; Murer, A.; Ueda, S.; Béziat, V.; Malmberg, K.-J.; Staubli, G.; Gysin, C.; Berger, C.; Münz, C.; et al. Role for Early-Differentiated Natural Killer Cells in Infectious Mononucleosis. Blood 2014, 124, 2533–2543. [Google Scholar] [CrossRef] [Green Version]
- Latour, S.; Fischer, A. Signaling Pathways Involved in the T-cell-mediated Immunity against Epstein-Barr Virus: Lessons from Genetic Diseases. Immunol. Rev. 2019, 291, 174–189. [Google Scholar] [CrossRef]
- Taylor, G.S.; Long, H.M.; Brooks, J.M.; Rickinson, A.B.; Hislop, A.D. The Immunology of Epstein-Barr Virus–Induced Disease. Annu. Rev. Immunol. 2015, 33, 787–821. [Google Scholar] [CrossRef]
- Hislop, A.D. Tonsillar Homing of Epstein-Barr Virus-Specific CD8+ T Cells and the Virus-Host Balance. J. Clin. Investig. 2005, 115, 2546–2555. [Google Scholar] [CrossRef] [Green Version]
- Long, H.M.; Chagoury, O.L.; Leese, A.M.; Ryan, G.B.; James, E.; Morton, L.T.; Abbott, R.J.M.; Sabbah, S.; Kwok, W.; Rickinson, A.B. MHC II Tetramers Visualize Human CD4+ T Cell Responses to Epstein–Barr Virus Infection and Demonstrate Atypical Kinetics of the Nuclear Antigen EBNA1 Response. J. Exp. Med. 2013, 210, 933–949. [Google Scholar] [CrossRef]
- Long, H.M.; Haigh, T.A.; Gudgeon, N.H.; Leen, A.M.; Tsang, C.-W.; Brooks, J.; Landais, E.; Houssaint, E.; Lee, S.P.; Rickinson, A.B.; et al. CD4+ T-Cell Responses to Epstein-Barr Virus (EBV) Latent-Cycle Antigens and the Recognition of EBV-Transformed Lymphoblastoid Cell Lines. J. Virol. 2005, 79, 4896–4907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, J.K.P.; Hui, K.F.; Ning, R.J.; Xu, X.Q.; Chan, K.H.; Chiang, A.K.S. Emergence of CD4+ and CD8+ Polyfunctional T Cell Responses against Immunodominant Lytic and Latent EBV Antigens in Children with Primary EBV Infection. Front. Microbiol. 2018, 9, 416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meckiff, B.J.; Ladell, K.; McLaren, J.E.; Ryan, G.B.; Leese, A.M.; James, E.A.; Price, D.A.; Long, H.M. Primary EBV Infection Induces an Acute Wave of Activated Antigen-Specific Cytotoxic CD4+ T Cells. J. Immunol. 2019, 203, 1276–1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, H.M.; Leese, A.M.; Chagoury, O.L.; Connerty, S.R.; Quarcoopome, J.; Quinn, L.L.; Shannon-Lowe, C.; Rickinson, A.B. Cytotoxic CD4+ T Cell Responses to EBV Contrast with CD8 Responses in Breadth of Lytic Cycle Antigen Choice and in Lytic Cycle Recognition. J. Immunol. 2011, 187, 92–101. [Google Scholar] [CrossRef] [Green Version]
- Long, H.M.; Meckiff, B.J.; Taylor, G.S. The T-Cell Response to Epstein-Barr Virus–New Tricks from an Old Dog. Front. Immunol. 2019, 10, 2193. [Google Scholar] [CrossRef]
- Ru, Y.; Chen, J.; Wu, D. Epstein-Barr Virus Post-Transplant Lymphoproliferative Disease (PTLD) after Hematopoietic Stem Cell Transplantation. Eur. J. Haematol. 2018, 101, 283–290. [Google Scholar] [CrossRef] [Green Version]
- Shindiapina, P.; Ahmed, E.H.; Mozhenkova, A.; Abebe, T.; Baiocchi, R.A. Immunology of EBV-Related Lymphoproliferative Disease in HIV-Positive Individuals. Front. Oncol. 2020, 10, 1723. [Google Scholar] [CrossRef]
- Castillo, J.J.; Beltran, B.E.; Miranda, R.N.; Young, K.H.; Chavez, J.C.; Sotomayor, E.M. EBV-Positive Diffuse Large B-Cell Lymphoma of the Elderly: 2016 Update on Diagnosis, Risk-Stratification, and Management. Am. J. Hematol. 2016, 91, 529–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tangye, S.G. Genetic Susceptibility to EBV Infection: Insights from Inborn Errors of Immunity. Hum. Genet. 2020, 139, 885–901. [Google Scholar] [CrossRef]
- Tangye, S.G.; Al-Herz, W.; Bousfiha, A.; Chatila, T.; Cunningham-Rundles, C.; Etzioni, A.; Franco, J.L.; Holland, S.M.; Klein, C.; Morio, T.; et al. Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee. J. Clin. Immunol. 2020, 40, 24–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Frange, P.; Blanche, S.; Casanova, J.L. Pathogenesis of Infections in HIV-Infected Individuals: Insights from Primary Immunodeficiencies. Curr. Opin. Immunol. 2017, 48, 122–133. [Google Scholar] [CrossRef]
- Luo, Y.; Liu, Y.; Wang, C.; Gan, R. Signaling Pathways of EBV-Induced Oncogenesis. Cancer Cell Int. 2021, 21, 93. [Google Scholar] [CrossRef]
- Yin, H.; Qu, J.; Peng, Q.; Gan, R. Molecular Mechanisms of EBV-Driven Cell Cycle Progression and Oncogenesis. Med. Microbiol. Immunol. 2019, 208, 573–583. [Google Scholar] [CrossRef] [Green Version]
- Leong, M.M.L.; Lung, M.L. The Impact of Epstein-Barr Virus Infection on Epigenetic Regulation of Host Cell Gene Expression in Epithelial and Lymphocytic Malignancies. Front. Oncol. 2021, 11, 201. [Google Scholar] [CrossRef]
- Cohen, J.I.; Kimura, H.; Nakamura, S.; Ko, Y.-H.; Jaffe, E.S. Epstein–Barr Virus-Associated Lymphoproliferative Disease in Non-Immunocompromised Hosts: A Status Report and Summary of an International Meeting, 8–9 September 2008. Ann. Oncol. 2009, 20, 1472–1482. [Google Scholar] [CrossRef]
- Kebudi, R.; Kiykim, A.; Sahin, M.K. Primary Immunodeficiency and Cancer in Children; A Review of the Literature. Curr. Pediatr. Rev. 2019, 15, 245–250. [Google Scholar] [CrossRef]
- Grant, E.J.; Nüssing, S.; Sant, S.; Clemens, E.B.; Kedzierska, K. The Role of CD27 in Anti-Viral T-Cell Immunity. Curr. Opin. Virol. 2017, 22, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Akiba, H.; Nakano, H.; Nishinaka, S.; Shindo, M.; Kobata, T.; Atsuta, M.; Morimoto, C.; Ware, C.F.; Malinin, N.L.; Wallach, D.; et al. CD27, a Member of the Tumor Necrosis Factor Receptor Superfamily, Activates NF-ΚB and Stress-Activated Protein Kinase/c-Jun N-Terminal Kinase via TRAF2, TRAF5, and NF-ΚB-Inducing Kinase. J. Biol. Chem. 1998, 273, 13353–13358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hintzen, R.Q.; Lens, S.M.; Beckmann, M.P.; Goodwin, R.G.; Lynch, D.; van Lier, R.A. Characterization of the Human CD27 Ligand, a Novel Member of the TNF Gene Family. J. Immunol. 1994, 152, 1762–1773. [Google Scholar]
- Orengo, A.M.; Cantoni, C.; Neglia, F.; Biassoni, R.; Ferrini, S. Reciprocal Expression of CD70 and of Its Receptor, CD27, in Human Long Term-Activated T and Natural Killer (NK) Cells: Inverse Regulation by Cytokines and Role in Induction of Cytotoxicity. Clin. Exp. Immunol. 1997, 107, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Tesselaar, K.; Xiao, Y.; Arens, R.; van Schijndel, G.M.W.; Schuurhuis, D.H.; Mebius, R.E.; Borst, J.; van Lier, R.A.W. Expression of the Murine CD27 Ligand CD70 In Vitro and In Vivo. J. Immunol. 2003, 170, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Nolte, M.A.; van Olffen, R.W.; van Gisbergen, K.P.J.M.; van Lier, R.A.W. Timing and Tuning of CD27-CD70 Interactions: The Impact of Signal Strength in Setting the Balance between Adaptive Responses and Immunopathology. Immunol. Rev. 2009, 229, 216–231. [Google Scholar] [CrossRef] [PubMed]
- Izawa, K.; Martin, E.; Soudais, C.; Bruneau, J.; Boutboul, D.; Rodriguez, R.; Lenoir, C.; Hislop, A.D.; Besson, C.; Touzot, F.; et al. Inherited CD70 Deficiency in Humans Reveals a Critical Role for the CD70-CD27 Pathway in Immunity to Epstein-Barr Virus Infection. J. Exp. Med. 2017, 214, 73–89. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.; Deschoolmeester, V.; Zwaenepoel, K.; Rolfo, C.; Silence, K.; Rottey, S.; Lardon, F.; Smits, E.; Pauwels, P. CD70: An Emerging Target in Cancer Immunotherapy. Pharmacol. Ther. 2015, 155, 1–10. [Google Scholar] [CrossRef]
- Gravestein, L.A.; van Ewijk, W.; Ossendorp, F.; Borst, J. CD27 Cooperates with the Pre-T Cell Receptor in the Regulation of Murine T Cell Development. J. Exp. Med. 1996, 184, 675–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willoughby, J.E.; Kerr, J.P.; Rogel, A.; Taraban, V.Y.; Buchan, S.L.; Johnson, P.W.M.; Al-Shamkhani, A. Differential Impact of CD27 and 4-1BB Costimulation on Effector and Memory CD8 T Cell Generation Following Peptide Immunization. J. Immunol. 2014, 193, 244–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Croft, M. The Role of TNF Superfamily Members in T-Cell Function and Diseases. Nat. Rev. Immunol. 2009, 9, 271–285. [Google Scholar] [CrossRef] [Green Version]
- Rowley, T.F.; Al-Shamkhani, A. Stimulation by Soluble CD70 Promotes Strong Primary and Secondary CD8+ Cytotoxic T Cell Responses In Vivo. J. Immunol. 2004, 172, 6039–6046. [Google Scholar] [CrossRef] [Green Version]
- Hendriks, J.; Gravestein, L.A.; Tesselaar, K.; van Lier, R.A.W.; Schumacher, T.N.M.; Borst, J. CD27 Is Required for Generation and Long-Term Maintenance of T Cell Immunity. Nat. Immunol. 2000, 1, 433–440. [Google Scholar] [CrossRef]
- Ghosh, S.; Köstel Bal, S.; Edwards, E.S.J.; Pillay, B.; Jiménez Heredia, R.; Erol Cipe, F.; Rao, G.; Salzer, E.; Zoghi, S.; Abolhassani, H.; et al. Extended Clinical and Immunological Phenotype and Transplant Outcome in CD27 and CD70 Deficiency. Blood 2020, 136, 2638–2655. [Google Scholar] [CrossRef]
- Khodzhaev, K.; Bay, S.B.; Kebudi, R.; Altindirek, D.; Kaya, A.; Erbilgin, Y.; Ng, O.H.; Kiykim, A.; Erol, F.C.; Zengin, F.S.; et al. Lymphoma Predisposing Gene in an Extended Family: CD70 Signaling Defect. J. Clin. Immunol. 2020, 40, 883–892. [Google Scholar] [CrossRef]
- Abolhassani, H.; Edwards, E.S.J.; Ikinciogullari, A.; Jing, H.; Borte, S.; Buggert, M.; Du, L.; Matsuda-Lennikov, M.; Romano, R.; Caridha, R.; et al. Combined Immunodeficiency and Epstein-Barr Virus–Induced B Cell Malignancy in Humans with Inherited CD70 Deficiency. J. Exp. Med. 2017, 214, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Wajant, H. Therapeutic Targeting of CD70 and CD27. Expert Opin. Ther. Targets 2016, 20, 959–973. [Google Scholar] [CrossRef]
- Eken, A.; Cansever, M.; Somekh, I.; Mizoguchi, Y.; Zietara, N.; Okus, F.Z.; Erdem, S.; Canatan, H.; Akyol, S.; Ozcan, A.; et al. Genetic Deficiency and Biochemical Inhibition of ITK Affect Human Th17, Treg, and Innate Lymphoid Cells. J. Clin. Immunol. 2019, 39, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Howe, M.K.; Dowdell, K.; Roy, A.; Niemela, J.E.; Wilson, W.; McElwee, J.J.; Hughes, J.D.; Cohen, J.I. Magnesium Restores Activity to Peripheral Blood Cells in a Patient with Functionally Impaired Interleukin-2-Inducible T Cell Kinase. Front. Immunol. 2019, 10, 2000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youssefian, L.; Vahidnezhad, H.; Yousefi, M.; Saeidian, A.H.; Azizpour, A.; Touati, A.; Nikbakht, N.; Hesari, K.K.; Adib-Sereshki, M.M.; Zeinali, S.; et al. Inherited Interleukin 2–Inducible T-Cell (ITK) Kinase Deficiency in Siblings with Epidermodysplasia Verruciformis and Hodgkin Lymphoma. Clin. Infect. Dis. 2019, 68, 1938–1941. [Google Scholar] [CrossRef]
- Ghosh, S.; Drexler, I.; Bhatia, S.; Gennery, A.R.; Borkhardt, A. Interleukin-2-Inducible T-Cell Kinase Deficiency-New Patients, New Insight? Front. Immunol. 2018, 9, 979. [Google Scholar] [CrossRef]
- Fang, M.; Abolhassani, H.; Pan-Hammarström, Q.; Sandholm, E.; Liu, X.; Hammarström, L. Compound Heterozygous Mutations of IL2-Inducible T Cell Kinase in a Swedish Patient: The Importance of Early Genetic Diagnosis. J. Clin. Immunol. 2019, 39, 131–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravell, J.C.; Matsuda-Lennikov, M.; Chauvin, S.D.; Zou, J.; Biancalana, M.; Deeb, S.J.; Price, S.; Su, H.C.; Notarangelo, G.; Jiang, P.; et al. Defective Glycosylation and Multisystem Abnormalities Characterize the Primary Immunodeficiency XMEN Disease. J. Clin. Investig. 2020, 130, 507–522. [Google Scholar] [CrossRef] [Green Version]
- Ravell, J.C.; Chauvin, S.D.; He, T.; Lenardo, M. An Update on XMEN Disease. J. Clin. Immunol. 2020, 40, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, R.; Fournier, B.; Cordeiro, D.J.; Winter, S.; Izawa, K.; Martin, E.; Boutboul, D.; Lenoir, C.; Fraitag, S.; Kracker, S.; et al. Concomitant PIK3CD and TNFRSF9 Deficiencies Cause Chronic Active Epstein-Barr Virus Infection of T Cells. J. Exp. Med. 2019, 216, 2800–2818. [Google Scholar] [CrossRef]
- Somekh, I.; Thian, M.; Medgyesi, D.; Gülez, N.; Magg, T.; Duque, A.G.; Stauber, T.; Lev, A.; Genel, F.; Unal, E.; et al. CD137 Deficiency Causes Immune Dysregulation with Predisposition to Lymphomagenesis. Blood 2019, 134, 1510–1516. [Google Scholar] [CrossRef] [PubMed]
- Alosaimi, M.F.; Hoenig, M.; Jaber, F.; Platt, C.D.; Jones, J.; Wallace, J.; Debatin, K.; Schulz, A.; Jacobsen, E.; Möller, P.; et al. Immunodeficiency and EBV-Induced Lymphoproliferation Caused by 4-1BB Deficiency. J. Allergy Clin. Immunol. 2019, 144, 574–583.e5. [Google Scholar] [CrossRef] [Green Version]
- Shiow, L.R.; Roadcap, D.W.; Paris, K.; Watson, S.R.; Grigorova, I.L.; Lebet, T.; An, J.; Xu, Y.; Jenne, C.N.; Föger, N.; et al. The Actin Regulator Coronin 1A Is Mutant in a Thymic Egress–Deficient Mouse Strain and in a Patient with Severe Combined Immunodeficiency. Nat. Immunol. 2008, 9, 1307–1315. [Google Scholar] [CrossRef]
- Stray-Pedersen, A.; Jouanguy, E.; Crequer, A.; Bertuch, A.A.; Brown, B.S.; Jhangiani, S.N.; Muzny, D.M.; Gambin, T.; Sorte, H.; Sasa, G.; et al. Compound Heterozygous CORO1A Mutations in Siblings with a Mucocutaneous-Immunodeficiency Syndrome of Epidermodysplasia Verruciformis-HPV, Molluscum Contagiosum and Granulomatous Tuberculoid Leprosy. J. Clin. Immunol. 2014, 34, 871–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yee, C.S.; Massaad, M.J.; Bainter, W.; Ohsumi, T.K.; Föger, N.; Chan, A.C.; Akarsu, N.A.; Aytekin, C.; Ayvaz, D.Ç.; Tezcan, I.; et al. Recurrent Viral Infections Associated with a Homozygous CORO1A Mutation That Disrupts Oligomerization and Cytoskeletal Association. J. Allergy Clin. Immunol. 2016, 137, 879–888.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Punwani, D.; Pelz, B.; Yu, J.; Arva, N.C.; Schafernak, K.; Kondratowicz, K.; Makhija, M.; Puck, J.M. Coronin-1A: Immune Deficiency in Humans and Mice. J. Clin. Immunol. 2015, 35, 100–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moshous, D.; Martin, E.; Carpentier, W.; Lim, A.; Callebaut, I.; Canioni, D.; Hauck, F.; Majewski, J.; Schwartzentruber, J.; Nitschke, P.; et al. Whole-Exome Sequencing Identifies Coronin-1A Deficiency in 3 Siblings with Immunodeficiency and EBV-Associated B-Cell Lymphoproliferation. J. Allergy Clin. Immunol. 2013, 131, 1594–1603.e9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vignesh, P.; Rawat, A.; Kumrah, R.; Singh, A.; Gummadi, A.; Sharma, M.; Kaur, A.; Nameirakpam, J.; Jindal, A.; Suri, D.; et al. Clinical, Immunological, and Molecular Features of Severe Combined Immune Deficiency: A Multi-Institutional Experience from India. Front. Immunol. 2021, 11, 3747. [Google Scholar] [CrossRef] [PubMed]
- Abdollahpour, H.; Appaswamy, G.; Kotlarz, D.; Diestelhorst, J.; Beier, R.; Schäffer, A.A.; Gertz, E.M.; Schambach, A.; Kreipe, H.H.; Pfeifer, D.; et al. The Phenotype of Human STK4 Deficiency. Blood 2012, 119, 3450–3457. [Google Scholar] [CrossRef] [PubMed]
- Al-Saud, B.; Alajlan, H.; Sabar, H.; Anwar, S.; Alruwaili, H.; Al-Hussain, T.; Alamri, N.; Alazami, A.M. STK4 Deficiency in a Patient with Immune Complex Glomerulonephritis, Salt-Losing Tubulopathy, and Castleman’s-Like Disease. J. Clin. Immunol. 2019, 39, 823–826. [Google Scholar] [CrossRef] [PubMed]
- Ashrafi, F.; Klein, C.; Poorpooneh, M.; Sherkat, R.; Khoshnevisan, R. A Case Report of Sinusoidal Diffuse Large B-Cell Lymphoma in a STK4 Deficient Patient. Medicine 2020, 99, e18601. [Google Scholar] [CrossRef]
- Crequer, A.; Picard, C.; Patin, E.; D’Amico, A.; Abhyankar, A.; Munzer, M.; Debré, M.; Zhang, S.-Y.; de Saint-Basile, G.; Fischer, A.; et al. Inherited MST1 Deficiency Underlies Susceptibility to EV-HPV Infections. PLoS ONE 2012, 7, e44010. [Google Scholar] [CrossRef]
- Dang, T.S.; Willet, J.D.; Griffin, H.R.; Morgan, N.V.; O’Boyle, G.; Arkwright, P.D.; Hughes, S.M.; Abinun, M.; Tee, L.J.; Barge, D.; et al. Defective Leukocyte Adhesion and Chemotaxis Contributes to Combined Immunodeficiency in Humans with Autosomal Recessive MST1 Deficiency. J. Clin. Immunol. 2016, 36, 117–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halacli, S.O.; Ayvaz, D.C.; Sun-Tan, C.; Erman, B.; Uz, E.; Yilmaz, D.Y.; Ozgul, K.; Tezcan, İ.; Sanal, O. STK4 (MST1) Deficiency in Two Siblings with Autoimmune Cytopenias: A Novel Mutation. Clin. Immunol. 2015, 161, 316–323. [Google Scholar] [CrossRef]
- Jørgensen, S.E.; Al-Mousawi, A.; Assing, K.; Hartling, U.; Grosen, D.; Fisker, N.; Nielsen, C.; Jakobsen, M.A.; Mogensen, T.H. STK4 Deficiency Impairs Innate Immunity and Interferon Production through Negative Regulation of TBK1-IRF3 Signaling. J. Clin. Immunol. 2021, 41, 109–124. [Google Scholar] [CrossRef]
- Moran, I.; Avery, D.T.; Payne, K.; Lenthall, H.; Davies, E.G.; Burns, S.; Ip, W.; Oleastro, M.M.; Reisli, I.; Guner, S.; et al. B Cell–Intrinsic Requirement for STK4 in Humoral Immunity in Mice and Human Subjects. J. Allergy Clin. Immunol. 2019, 143, 2302–2305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nehme, N.T.; Schmid, J.P.; Debeurme, F.; André-Schmutz, I.; Lim, A.; Nitschke, P.; Rieux-Laucat, F.; Lutz, P.; Picard, C.; Mahlaoui, N.; et al. MST1 Mutations in Autosomal Recessive Primary Immunodeficiency Characterized by Defective Naive T-Cell Survival. Blood 2012, 119, 3458–3468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radwan, N.; El-Owaidy, R.; El-Sayed, Z.A.; Abdel-Baky, A.; El-Haddad, A.; Rashad, H.; Khorshed, E.N.; Platt, C.D.; Wallace, J.G.; Chou, J.; et al. A Case of STK4 Deficiency with Complications Evoking Mycobacterial Infection. J. Clin. Immunol. 2020, 40, 665–669. [Google Scholar] [CrossRef]
- Schipp, C.; Schlütermann, D.; Hönscheid, A.; Nabhani, S.; Höll, J.; Oommen, P.T.; Ginzel, S.; Fleckenstein, B.; Stork, B.; Borkhardt, A.; et al. EBV Negative Lymphoma and Autoimmune Lymphoproliferative Syndrome Like Phenotype Extend the Clinical Spectrum of Primary Immunodeficiency Caused by STK4 Deficiency. Front. Immunol. 2018, 9, 2400. [Google Scholar] [CrossRef] [Green Version]
- Sherkat, R.; Sabri, M.R.; Dehghan, B.; Bigdelian, H.; Reisi, N.; Afsharmoghadam, N.; Rahimi, H.; Rahmanian, N.; Klein, C. EBV Lymphoproliferative-Associated Disease and Primary Cardiac T-Cell Lymphoma in a STK4 Deficient Patient. Medicine 2017, 96, e8852. [Google Scholar] [CrossRef] [PubMed]
- Marangi, G.; Garcovich, S.; Sante, G.; Orteschi, D.; Frangella, S.; Scaldaferri, F.; Genuardi, M.; Peris, K.; Gurrieri, F.; Zollino, M. Complex Muco-Cutaneous Manifestations of CARMIL2-Associated Combined Immunodeficiency: A Novel Presentation of Dysfunctional Epithelial Barriers. Acta Derm. Venereol. 2020, 100, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosa, L.; Batura, V.; Colavito, D.; Fiedler, K.; Gaio, P.; Guo, C.; Li, Q.; Marzollo, A.; Mescoli, C.; Nambu, R.; et al. Novel CARMIL2 Loss-of-Function Variants Are Associated with Pediatric Inflammatory Bowel Disease. Sci. Rep. 2021, 11, 5945. [Google Scholar] [CrossRef] [PubMed]
- Maccari, M.E.; Speckmann, C.; Heeg, M.; Reimer, A.; Casetti, F.; Has, C.; Ehl, S.; Castro, C.N. Profound Immunodeficiency with Severe Skin Disease Explained by Concomitant Novel CARMIL2 and PLEC1 Loss-of-Function Mutations. Clin. Immunol. 2019, 208, 108228. [Google Scholar] [CrossRef]
- Yonkof, J.R.; Gupta, A.; Rueda, C.M.; Mangray, S.; Prince, B.T.; Rangarajan, H.G.; Alshahrani, M.; Varga, E.; Cripe, T.P.; Abraham, R.S. A Novel Pathogenic Variant in CARMIL2 (RLTPR) Causing CARMIL2 Deficiency and EBV-Associated Smooth Muscle Tumors. Front. Immunol. 2020, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Uner, A.; Saglam, A.; Chadburn, A.; Crane, G.M. Peripheral Eosinophilia in Primary Immunodeficiencies of Actin Dysregulation: A Case Series of Wiskott-Aldrich Syndrome, CARMIL2 and DOCK8 Deficiency and Review of the Literature. Ann. Diagn. Pathol. 2019, 43, 151413. [Google Scholar] [CrossRef]
- Wang, Y.; Ma, C.S.; Ling, Y.; Bousfiha, A.; Camcioglu, Y.; Jacquot, S.; Payne, K.; Crestani, E.; Roncagalli, R.; Belkadi, A.; et al. Dual T Cell- and B Cell-Intrinsic Deficiency in Humans with Biallelic RLTPR Mutations. J. Exp. Med. 2016, 213, 2413–2435. [Google Scholar] [CrossRef] [PubMed]
- Alazami, A.M.; Al-Helale, M.; Alhissi, S.; Al-Saud, B.; Alajlan, H.; Monies, D.; Shah, Z.; Abouelhoda, M.; Arnaout, R.; Al-Dhekri, H.; et al. Novel CARMIL2 Mutations in Patients with Variable Clinical Dermatitis, Infections, and Combined Immunodeficiency. Front. Immunol. 2018, 9, 203. [Google Scholar] [CrossRef] [Green Version]
- Schober, T.; Magg, T.; Laschinger, M.; Rohlfs, M.; Linhares, N.D.; Puchalka, J.; Weisser, T.; Fehlner, K.; Mautner, J.; Walz, C.; et al. A Human Immunodeficiency Syndrome Caused by Mutations in CARMIL2. Nat. Commun. 2017, 8, 14209. [Google Scholar] [CrossRef] [Green Version]
- Sorte, H.S.; Osnes, L.T.; Fevang, B.; Aukrust, P.; Erichsen, H.C.; Backe, P.H.; Abrahamsen, T.G.; Kittang, O.B.; Øverland, T.; Jhangiani, S.N.; et al. A Potential Founder Variant in CARMIL2/RLTPR in Three Norwegian Families with Warts, Molluscum Contagiosum, and T-Cell Dysfunction. Mol. Genet. Genom. Med. 2016, 4, 604–616. [Google Scholar] [CrossRef]
- Atschekzei, F.; Jacobs, R.; Wetzke, M.; Sogkas, G.; Schröder, C.; Ahrenstorf, G.; Dhingra, A.; Ott, H.; Baumann, U.; Schmidt, R.E. A Novel CARMIL2 Mutation Resulting in Combined Immunodeficiency Manifesting with Dermatitis, Fungal, and Viral Skin Infections as Well as Selective Antibody Deficiency. J. Clin. Immunol. 2019, 39, 274–276. [Google Scholar] [CrossRef]
- Shamriz, O.; Simon, A.J.; Lev, A.; Megged, O.; Ledder, O.; Picard, E.; Joseph, L.; Molho-Pessach, V.; Tal, Y.; Millman, P.; et al. Exogenous Interleukin-2 Can Rescue In-Vitro T Cell Activation and Proliferation in Patients with a Novel Capping Protein Regulator and Myosin 1 Linker 2 Mutation. Clin. Exp. Immunol. 2020, 200, 215–227. [Google Scholar] [CrossRef]
- Magg, T.; Shcherbina, A.; Arslan, D.; Desai, M.M.; Wall, S.; Mitsialis, V.; Conca, R.; Unal, E.; Karacabey, N.; Mukhina, A.; et al. CARMIL2 Deficiency Presenting as Very Early Onset Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2019, 25, 1788–1795. [Google Scholar] [CrossRef]
- Kurolap, A.; Eshach Adiv, O.; Konnikova, L.; Werner, L.; Gonzaga-Jauregui, C.; Steinberg, M.; Mitsialis, V.; Mory, A.; Nunberg, M.Y.; Wall, S.; et al. A Unique Presentation of Infantile-Onset Colitis and Eosinophilic Disease without Recurrent Infections Resulting from a Novel Homozygous CARMIL2 Variant. J. Clin. Immunol. 2019, 39, 430–439. [Google Scholar] [CrossRef]
- Shayegan, L.H.; Garzon, M.C.; Morel, K.D.; Borlack, R.; Vuguin, P.M.; Margolis, K.G.; Demirdag, Y.Y.; Pereira, E.M.; Lauren, C.T. CARMIL2-related Immunodeficiency Manifesting with Photosensitivity. Pediatr. Dermatol. 2020, 37, 695–697. [Google Scholar] [CrossRef] [PubMed]
- Trück, J.; Kelly, D.F.; Taylor, J.M.; Kienzler, A.K.; Lester, T.; Seller, A.; Pollard, A.J.; Patel, S.Y. Variable Phenotype and Discrete Alterations of Immune Phenotypes in CTP Synthase 1 Deficiency: Report of 2 Siblings. J. Allergy Clin. Immunol. 2016, 138, 1722–1725.e6. [Google Scholar] [CrossRef] [Green Version]
- Kucuk, Z.Y.; Zhang, K.; Filipovich, L.; Bleesing, J.J.H. CTP Synthase 1 Deficiency in Successfully Transplanted Siblings with Combined Immune Deficiency and Chronic Active EBV Infection. J. Clin. Immunol. 2016, 36, 750–753. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Palmic, N.; Sanquer, S.; Lenoir, C.; Hauck, F.; Mongellaz, C.; Fabrega, S.; Nitschké, P.; Esposti, M.D.; Schwartzentruber, J.; et al. CTP Synthase 1 Deficiency in Humans Reveals Its Central Role in Lymphocyte Proliferation. Nature 2014, 510, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Minet, N.; Boschat, A.-C.; Sanquer, S.; Sobrino, S.; Lenoir, C.; de Villartay, J.P.; Leites-de-Moraes, M.; Picard, C.; Soudais, C.; et al. Impaired Lymphocyte Function and Differentiation in CTPS1-Deficient Patients Result from a Hypomorphic Homozygous Mutation. JCI Insight 2020, 5, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Nademi, Z.; Wynn, R.F.; Slatter, M.; Hughes, S.M.; Bonney, D.; Qasim, W.; Latour, S.; Trück, J.; Patel, S.; Abinun, M.; et al. Hematopoietic Stem Cell Transplantation for Cytidine Triphosphate Synthase 1 (CTPS1) Deficiency. Bone Marrow Transplant. 2019, 54, 130–133. [Google Scholar] [CrossRef]
- Somekh, I.; Marquardt, B.; Liu, Y.; Rohlfs, M.; Hollizeck, S.; Karakukcu, M.; Unal, E.; Yilmaz, E.; Patiroglu, T.; Cansever, M.; et al. Novel Mutations in RASGRP1 Are Associated with Immunodeficiency, Immune Dysregulation, and EBV-Induced Lymphoma. J. Clin. Immunol. 2018, 38, 699–710. [Google Scholar] [CrossRef]
- Mao, H.; Yang, W.; Latour, S.; Yang, J.; Winter, S.; Zheng, J.; Ni, K.; Lv, M.; Liu, C.; Huang, H.; et al. RASGRP1 Mutation in Autoimmune Lymphoproliferative Syndrome-like Disease. J. Allergy Clin. Immunol. 2018, 142, 595–604.e16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Platt, C.D.; Fried, A.J.; Hoyos-Bachiloglu, R.; Usmani, G.N.; Schmidt, B.; Whangbo, J.; Chiarle, R.; Chou, J.; Geha, R.S. Combined Immunodeficiency with EBV Positive B Cell Lymphoma and Epidermodysplasia Verruciformis Due to a Novel Homozygous Mutation in RASGRP1. Clin. Immunol. 2017, 183, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Winter, S.; Martin, E.; Boutboul, D.; Lenoir, C.; Boudjemaa, S.; Petit, A.; Picard, C.; Fischer, A.; Leverger, G.; Latour, S. Loss of RASGRP 1 in Humans Impairs T-cell Expansion Leading to Epstein-Barr Virus Susceptibility. EMBO Mol. Med. 2018, 10, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Salzer, E.; Cagdas, D.; Hons, M.; MacE, E.M.; Garncarz, W.; Petronczki, Ö.Y.; Platzer, R.; Pfajfer, L.; Bilic, I.; Ban, S.A.; et al. RASGRP1 Deficiency Causes Immunodeficiency with Impaired Cytoskeletal Dynamics. Nat. Immunol. 2016, 17, 1352–1360. [Google Scholar] [CrossRef] [PubMed]
- Tangye, S.G. XLP: Clinical Features and Molecular Etiology Due to Mutations in SH2D1A Encoding SAP. J. Clin. Immunol. 2014, 34, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Latour, S.; Winter, S. Inherited Immunodeficiencies with High Predisposition to Epstein–Barr Virus-Driven Lymphoproliferative Diseases. Front. Immunol. 2018, 9, 1103. [Google Scholar] [CrossRef]
- Wortzman, M.E.; Clouthier, D.L.; McPherson, A.J.; Lin, G.H.Y.; Watts, T.H. The Contextual Role of TNFR Family Members in CD8+ T-Cell Control of Viral Infections. Immunol. Rev. 2013, 255, 125–148. [Google Scholar] [CrossRef]
- Andreotti, A.H.; Schwartzberg, P.L.; Joseph, R.E.; Berg, L.J. T-Cell Signaling Regulated by the Tec Family Kinase, Itk. Cold Spring Harb. Perspect. Biol. 2010, 2, a002287. [Google Scholar] [CrossRef] [Green Version]
- Andreotti, A.H.; Joseph, R.E.; Conley, J.M.; Iwasa, J.; Berg, L.J.; Carver, R.J. Annual Review of Immunology Multidomain Control over TEC Kinase Activation State Tunes the T Cell Response. Ann. Rev. Immunol. 2018, 36, 549–578. [Google Scholar] [CrossRef]
- Mamontov, P.; Eberwine, R.A.; Perrigoue, J.; Das, A.; Friedman, J.R.; Mora, J.R. A Negative Role for the Interleukin-2-Inducible T-Cell Kinase (ITK) in Human Foxp3+ T REG Differentiation. PLoS ONE 2019, 14, e0215963. [Google Scholar] [CrossRef] [Green Version]
- Huang, W.; Jeong, A.-R.; Kannan, A.K.; Huang, L.; August, A. IL-2–Inducible T Cell Kinase Tunes T Regulatory Cell Development and Is Required for Suppressive Function. J. Immunol. 2014, 193, 2267–2272. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Rodriguez, J.; Wohlfert, E.A.; Handon, R.; Meylan, F.; Wu, J.Z.; Anderson, S.M.; Kirby, M.R.; Belkaid, Y.; Schwartzberg, P.L. Itk-mediated integration of T cell receptor and cytokine signaling regulates the balance between Th17 and regulatory T cells. J. Exp. Med. 2014, 211, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Dubovsky, J.A.; Beckwith, K.A.; Natarajan, G.; Woyach, J.A.; Jaglowski, S.; Zhong, Y.; Hessler, J.D.; Liu, T.-M.; Chang, B.Y.; Larkin, K.M.; et al. Ibrutinib is an irreversible molecular inhibitor of ITK driving a Th1-selective pressure in T lymphocytes. Blood 2013, 122, 2539–2549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broussard, C.; Fleischecker, C.; Horai, R.; Chetana, M.; Venegas, A.M.; Sharp, L.L.; Hedrick, S.M.; Fowlkes, B.J.; Schwartzberg, P.L. Altered Development of CD8+ T Cell Lineages in Mice Deficient for the Tec Kinases Itk and Rlk. Immunity 2006, 25, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Huck, K.; Feyen, O.; Niehues, T.; Rüschendorf, F.; Hübner, N.; Laws, H.J.; Telieps, T.; Knapp, S.; Wacker, H.H.; Meindl, A.; et al. Girls Homozygous for an IL-2–Inducible T Cell Kinase Mutation That Leads to Protein Deficiency Develop Fatal EBV-Associated Lymphoproliferation. J. Clin. Investig. 2009, 119, 1350–1358. [Google Scholar] [CrossRef]
- Kapnick, S.M.; Stinchcombe, J.C.; Griffiths, G.M.; Schwartzberg, P.L. Inducible T Cell Kinase Regulates the Acquisition of Cytolytic Capacity and Degranulation in CD8+ CTLs. J. Immunol. 2017, 198, 2699–2711. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-S.; Ha, S.; Shin, H.M.; Reboldi, A.; Hall, J.A.; Huh, J.R.; Usherwood, E.J.; Berg, L.J. CD8+ T Cells Require ITK-Mediated TCR Signaling for Migration to the Intestine. Immunohorizons 2020, 4, 57–71. [Google Scholar] [CrossRef] [Green Version]
- Linka, R.M.; Risse, S.L.; Bienemann, K.; Werner, M.; Linka, Y.; Krux, F.; Synaeve, C.; Deenen, R.; Ginzel, S.; Dvorsky, R.; et al. Loss-of-Function Mutations within the IL-2 Inducible Kinase ITK in Patients with EBV-Associated Lymphoproliferative Diseases. Leukemia 2012, 26, 963–971. [Google Scholar] [CrossRef]
- Bienemann, K.; Borkhardt, A.; Klapper, W.; Oschlies, I. High Incidence of Epstein-Barr Virus (EBV)-Positive Hodgkin Lymphoma and Hodgkin Lymphoma-like B-Cell Lymphoproliferations with EBV Latency Profile 2 in Children with Interleukin-2-Inducible T-Cell Kinase Deficiency. Histopathology 2015, 67, 607–616. [Google Scholar] [CrossRef]
- Huang, W.; Lei, X.; Ridder, G.; John Strauss, Y.Z. MTOR and Other Effector Kinase Signals That Impact T Cell Function and Activity Darienne. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef]
- Traut, T.W. Physiological Concentrations of Purines and Pyrimidines. Mol. Cell. Biochem. 1994, 140, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Fairbanks, L.D.; Bofill, M.; Ruckemann, K.; Simmonds, H.A. Importance of Ribonucleotide Availability to Proliferating T-Lymphocytes from Healthy Humans. J. Biol. Chem. 1995, 270, 29682–29689. [Google Scholar] [CrossRef] [Green Version]
- Li, F.-Y.; Lenardo, M.J.; Chaigne-Delalande, B. Loss of MAGT1 Abrogates the Mg2+ Flux Required for T Cell Signaling and Leads to a Novel Human Primary Immunodeficiency. Magnes. Res. 2011, 24, 109–114. [Google Scholar] [CrossRef]
- Li, F.-Y.; Chaigne-Delalande, B.; Kanellopoulou, C.; Davis, J.C.; Matthews, H.F.; Douek, D.C.; Cohen, J.I.; Uzel, G.; Su, H.C.; Lenardo, M.J. Second Messenger Role for Mg2+ Revealed by Human T-Cell Immunodeficiency. Nature 2011, 475, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Li, F.Y.; Chaigne-Delalande, B.; Su, H.; Uzel, G.; Matthews, H.; Lenardo, M.J. XMEN Disease: A New Primary Immunodeficiency Affecting Mg2+ Regulation of Immunity against Epstein-Barr Virus. Blood 2014, 123, 2148–2152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karimi, M.; Cao, T.M.; Baker, J.A.; Verneris, M.R.; Soares, L.; Negrin, R.S. Silencing Human NKG2D, DAP10, and DAP12 Reduces Cytotoxicity of Activated CD8+ T Cells and NK Cells. J. Immunol. 2005, 175, 7819–7828. [Google Scholar] [CrossRef] [Green Version]
- Chaigne-Delalande, B.; Li, F.Y.; O’Connor, G.M.; Lukacs, M.J.; Jiang, P.; Zheng, L.; Shatzer, A.; Biancalana, M.; Pittaluga, S.; Matthews, H.F.; et al. Mg2+ Regulates Cytotoxic Functions of NK and CD8 T Cells in Chronic EBV Infection through NKG2D. Science 2013, 341, 186–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanier, L.L. NKG2D Receptor and Its Ligands in Host Defense. Cancer Immunol. Res. 2015, 3, 575–582. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.S.; Qi, Y.; Im, W. Effects of N-Glycosylation on Protein Conformation and Dynamics: Protein Data Bank Analysis and Molecular Dynamics Simulation Study. Sci. Rep. 2015, 5, 8926. [Google Scholar] [CrossRef]
- Pieters, J.; Müller, P.; Jayachandran, R. On Guard: Coronin Proteins in Innate and Adaptive Immunity. Nat. Rev. Immunol. 2013, 13, 510–518. [Google Scholar] [CrossRef]
- Foger, N. Requirement for Coronin 1 in T Lymphocyte Trafficking and Cellular Homeostasis. Science 2006, 313, 839–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mueller, P.; Massner, J.; Jayachandran, R.; Combaluzier, B.; Albrecht, I.; Gatfield, J.; Blum, C.; Ceredig, R.; Rodewald, H.-R.; Rolink, A.G.; et al. Regulation of T Cell Survival through Coronin-1–Mediated Generation of Inositol-1,4,5-Trisphosphate and Calcium Mobilization after T Cell Receptor Triggering. Nat. Immunol. 2008, 9, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Mueller, P.; Liu, X.; Pieters, J. Migration and Homeostasis of Naive T Cells Depends on Coronin 1-Mediated Prosurvival Signals and Not on Coronin 1-Dependent Filamentous Actin Modulation. J. Immunol. 2011, 186, 4039–4050. [Google Scholar] [CrossRef] [Green Version]
- Mace, E.M.; Orange, J.S. Lytic Immune Synapse Function Requires Filamentous Actin Deconstruction by Coronin 1A. Proc. Natl. Acad. Sci. USA 2014, 111, 6708–6713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, F.-X.; Zhao, B.; Guan, K.-L. Hippo Pathway in Organ Size Control, Tissue Homeostasis, and Cancer. Cell 2015, 163, 811–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurz, A.R.M.; Pruenster, M.; Rohwedder, I.; Ramadass, M.; Schäfer, K.; Harrison, U.; Gouveia, G.; Nussbaum, C.; Immler, R.; Wiessner, J.R.; et al. MST1-Dependent Vesicle Trafficking Regulates Neutrophil Transmigration through the Vascular Basement Membrane. J. Clin. Investig. 2016, 126, 4125–4139. [Google Scholar] [CrossRef]
- Kurz, A.R.M.; Catz, S.D.; Sperandio, M. Noncanonical Hippo Signalling in the Regulation of Leukocyte Function. Trends Immunol. 2018, 39, 656–669. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Du, X.; Shi, H.; Deng, K.; Chi, H.; Tao, W. Mammalian Sterile 20-like Kinase 1 (Mst1) Enhances the Stability of Forkhead Box P3 (Foxp3) and the Function of Regulatory T Cells by Modulating Foxp3 Acetylation. J. Biol. Chem. 2015, 290, 30762–30770. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.-S.; Lee, D.-H.; Kim, S.K.; Shin, S.Y.; Seo, E.-J.; Lim, D.-S. Mammalian Sterile 20–like Kinase 1 Suppresses Lymphoma Development by Promoting Faithful Chromosome Segregation. Cancer Res. 2012, 72, 5386–5395. [Google Scholar] [CrossRef] [Green Version]
- Stark, B.C.; Lanier, M.H.; Cooper, J.A. CARMIL Family Proteins as Multidomain Regulators of Actin-Based Motility. Mol. Biol. Cell 2017, 28, 1713–1723. [Google Scholar] [CrossRef]
- Sayos, J.; Wu, C.; Morra, M.; Wang, N.; Zhang, X.; Allen, D.; van Schaik, S.; Notarangelo, L.; Geha, R.; Roncarolo, M.G.; et al. The X-Linked Lymphoproliferative-Disease Gene Product SAP Regulates Signals Induced through the Co-Receptor SLAM. Nature 1998, 395, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Coffey, A.J.; Brooksbank, R.A.; Brandau, O.; Oohashi, T.; Howell, G.R.; Bye, J.M.; Cahn, A.P.; Durham, J.; Heath, P.; Wray, P.; et al. Host Response to EBV Infection in X-Linked Lymphoproliferative Disease Results from Mutations in an SH2-Domain Encoding Gene. Nat. Genet. 1998, 20, 129–135. [Google Scholar] [CrossRef]
- Nichols, K.E.; Harkin, D.P.; Levitz, S.; Krainer, M.; Kolquist, K.A.; Genovese, C.; Bernard, A.; Ferguson, M.; Zuo, L.; Snyder, E.; et al. Inactivating Mutations in an SH2 Domain-Encoding Gene in X-Linked Lymphoproliferative Syndrome. Proc. Natl. Acad. Sci. USA 1998, 95, 13765–13770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, C.S.; Nichols, K.E.; Tangye, S.G. Regulation of Cellular and Humoral Immune Responses by the SLAM and SAP Families of Molecules. Annu. Rev. Immunol. 2007, 25, 337–379. [Google Scholar] [CrossRef] [PubMed]
- Cannons, J.L.; Tangye, S.G.; Schwartzberg, P.L. SLAM Family Receptors and SAP Adaptors in Immunity. Annu. Rev. Immunol. 2011, 29, 665–705. [Google Scholar] [CrossRef] [PubMed]
- Palendira, U.; Low, C.; Chan, A.; Hislop, A.D.; Ho, E.; Phan, T.G.; Deenick, E.; Cook, M.C.; Riminton, D.S.; Choo, S.; et al. Molecular Pathogenesis of EBV Susceptibility in XLP as Revealed by Analysis of Female Carriers with Heterozygous Expression of SAP. PLoS Biol. 2011, 9, e1001187. [Google Scholar] [CrossRef] [PubMed]
- Parolini, S.; Bottino, C.; Falco, M.; Augugliaro, R.; Giliani, S.; Franceschini, R.; Ochs, H.D.; Wolf, H.; Bonnefoy, J.-Y.; Biassoni, R.; et al. X-Linked Lymphoproliferative Disease. J. Exp. Med. 2000, 192, 337–346. [Google Scholar] [CrossRef]
- Dupré, L.; Andolfi, G.; Tangye, S.G.; Clementi, R.; Locatelli, F.; Aricò, M.; Aiuti, A.; Roncarolo, M.-G. SAP Controls the Cytolytic Activity of CD8+ T Cells against EBV-Infected Cells. Blood 2005, 105, 4383–4389. [Google Scholar] [CrossRef] [PubMed]
- Hislop, A.D.; Palendira, U.; Leese, A.M.; Arkwright, P.D.; Rohrlich, P.S.; Tangye, S.G.; Gaspar, H.B.; Lankester, A.C.; Moretta, A.; Rickinson, A.B. Impaired Epstein-Barr Virus-Specific CD8+ T-Cell Function in X-Linked Lymphoproliferative Disease Is Restricted to SLAM Family-Positive B-Cell Targets. Blood 2010, 116, 3249–3257. [Google Scholar] [CrossRef] [Green Version]
- Yin, L.; Al-Alem, U.; Liang, J.; Tong, W.-M.; Li, C.; Badiali, M.; Médard, J.J.; Sumegi, J.; Wang, Z.-Q.; Romeo, G. Mice Deficient in the X-Linked Lymphoproliferative Disease Gene Sap Exhibit Increased Susceptibility to Murine Gammaherpesvirus-68 and Hypo-Gammaglobulinemia. J. Med. Virol. 2003, 71, 446–455. [Google Scholar] [CrossRef]
- Chen, G.; Tai, A.K.; Lin, M.; Chang, F.; Terhorst, C.; Huber, B.T. Signaling Lymphocyte Activation Molecule-Associated Protein Is a Negative Regulator of the CD8 T Cell Response in Mice. J. Immunol. 2005, 175, 2212–2218. [Google Scholar] [CrossRef] [Green Version]
- Rigaud, S.; Fondanèche, M.C.; Lambert, N.; Pasquier, B.; Mateo, V.; Soulas, P.; Galicier, L.; le Deist, F.; Rieux-Laucat, F.; Revy, P.; et al. XIAP Deficiency in Humans Causes an X-Linked Lymphoproliferative Syndrome. Nature 2006, 444, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Schmid, J.P.; Canioni, D.; Moshous, D.; Touzot, F.; Mahlaoui, N.; Hauck, F.; Kanegane, H.; Lopez-Granados, E.; Mejstrikova, E.; Pellier, I.; et al. Clinical Similarities and Differences of Patients with X-Linked Lymphoproliferative Syndrome Type 1 (XLP-1/SAP Deficiency) versus Type 2 (XLP-2/XIAP Deficiency). Blood 2011, 117, 1522–1529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Speckmann, C.; Lehmberg, K.; Albert, M.H.; Damgaard, R.B.; Fritsch, M.; Gyrd-Hansen, M.; Rensing-Ehl, A.; Vraetz, T.; Grimbacher, B.; Salzer, U.; et al. X-Linked Inhibitor of Apoptosis (XIAP) Deficiency: The Spectrum of Presenting Manifestations beyond Hemophagocytic Lymphohistiocytosis. Clin. Immunol. 2013, 149, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Epstein, M.A.; Achong, B.G.; Barr, Y.M. Virus Particles in Cultured Lymphoblasts from Burkitt’s Lymphoma. Lancet 1964, 283, 702–703. [Google Scholar] [CrossRef]
- Fujiwara, S.; Nakamura, H. Chronic Active Epstein–Barr Virus Infection: Is It Immunodeficiency, Malignancy, or Both? Cancers 2020, 12, 3202. [Google Scholar] [CrossRef]
- Meyts, I.; Bosch, B.; Bolze, A.; Boisson, B.; Itan, Y.; Belkadi, A.; Pedergnana, V.; Moens, L.; Picard, C.; Cobat, A.; et al. Exome and Genome Sequencing for Inborn Errors of Immunity. J. Allergy Clin. Immunol. 2016, 138, 957–969. [Google Scholar] [CrossRef] [Green Version]
| Gene | Common Clinical Features | Number of Reported Cases | Types and Number of Malignancies in Reported IEI Patients |
|---|---|---|---|
| CD27 | EBV viremia, LPD, HLH Recurrent infections Autoimmunity Lymphadenopathy Hypogammaglobulinemia | 33 [50] | HL (9/33) [50] BL (1/33) [50] NHL (1/33) [50] DLBCL (3/33) [50] |
| CD70 | EBV viremia, LPD, HLH Recurrent infections Autoimmunity Lymphadenopathy Hypogammaglobulinemia | 21 [50,51] | HL (9/21) [50,51] BL (1/21) [50] NHL (1/21) [51] |
| ITK | EBV viremia, LPD Recurrent infections CD4+ T cell lymphopenia ↓ iNKT Hypogammaglobulinemia | 21 [54,55,56,57,58] | HL (8/21) [56,57] HL-like (2/21) [57] DLBCL (2/21) [57,58] DLBCL-like (1/21) [57] BL (1/21) [57] NHL (1/21) [57] SMT (1/21) [57] |
| MAGT1 | Chronic EBV viremia, LPD Recurrent infections ↓ NKG2D Inverted CD4+:CD8+ ratio Hypogammaglobulinemia Autoimmunity | 37 [59,60] | HL (7/37) [59,60] BL (2/37) [59,60] Unclassified lymphoma (1/37) [59,60] Liposarcoma (1/37) [59,60] DLBCL (1/37) [59,60] EMZL (1/37) [59,60] Kaposi sarcoma (1/37) [59,60] |
| TNFRSF9 (4-1BB/CD137) | EBV viremia, LPD Recurrent infections Lymphadenopathy Hypogammaglobulinemia | 8 [61,62,63] | HL (2/8) [62,63] DLBCL (1/8) [63] BL (1/8) [62] |
| CORO1A | EBV viremia, LPD Recurrent infections Lymphopenia | 10 [64,65,66,67,68,69] | DLBCL (3/10) [67,68] Unclassified lymphoma (1/10) [65] Intracranial B cell lymphoma (1/10) [69] |
| STK4 | EBV viremia, LPD Recurrent infections | 29 [69,70,71,72,73,74,75,76,77,78,79,80] | HL (2/29) [78,80] DLBCL (1/29) [72] BL (1/29) [79] NHL (1/29) [80] PCTL (1/29) [81] |
| CARMIL2 | EBV viremia, LPD Recurrent infections Inflammatory bowel disease | 44 [82,83,84,85,86,87,88,89,90,91,92,93,94,95] | SMT (8/44) [84,85,86,89] |
| CTPS1 | EBV viremia, LPD Recurrent infections Hypogammaglobulinemia | 28 [96,97,98,99,100] | B-NHL (2/28) [98] CNSL (12/28) [100] |
| RASGRP1 | EBV viremia, LPD Recurrent infections CD4+ T cell lymphopenia Lymphadenopathy Autoimmunity | 9 [101,102,103,104,105] | DLBCL (2/9) [101] HL (2/9) [104] low grade unclassified lymphoma (1/9) [105] PBCL (1/9) [103] SMT (1/9) [104] |
| SH2D1A (XLP1) | EBV viremia, LPD, HLH Hypogammaglobulinemia | >100 [106,107] | Total lymphomas (25–30%) [106,107] DLBCL 30–40% [106,107] BL 40–60% [106,107] NHL 20–30% [106,107] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lino, C.N.R.; Ghosh, S. Epstein–Barr Virus in Inborn Immunodeficiency—More Than Infection. Cancers 2021, 13, 4752. https://doi.org/10.3390/cancers13194752
Lino CNR, Ghosh S. Epstein–Barr Virus in Inborn Immunodeficiency—More Than Infection. Cancers. 2021; 13(19):4752. https://doi.org/10.3390/cancers13194752
Chicago/Turabian StyleLino, Ciro Novaes Rosa, and Sujal Ghosh. 2021. "Epstein–Barr Virus in Inborn Immunodeficiency—More Than Infection" Cancers 13, no. 19: 4752. https://doi.org/10.3390/cancers13194752
APA StyleLino, C. N. R., & Ghosh, S. (2021). Epstein–Barr Virus in Inborn Immunodeficiency—More Than Infection. Cancers, 13(19), 4752. https://doi.org/10.3390/cancers13194752





