A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery
Abstract
:Simple Summary
Abstract
1. Introduction
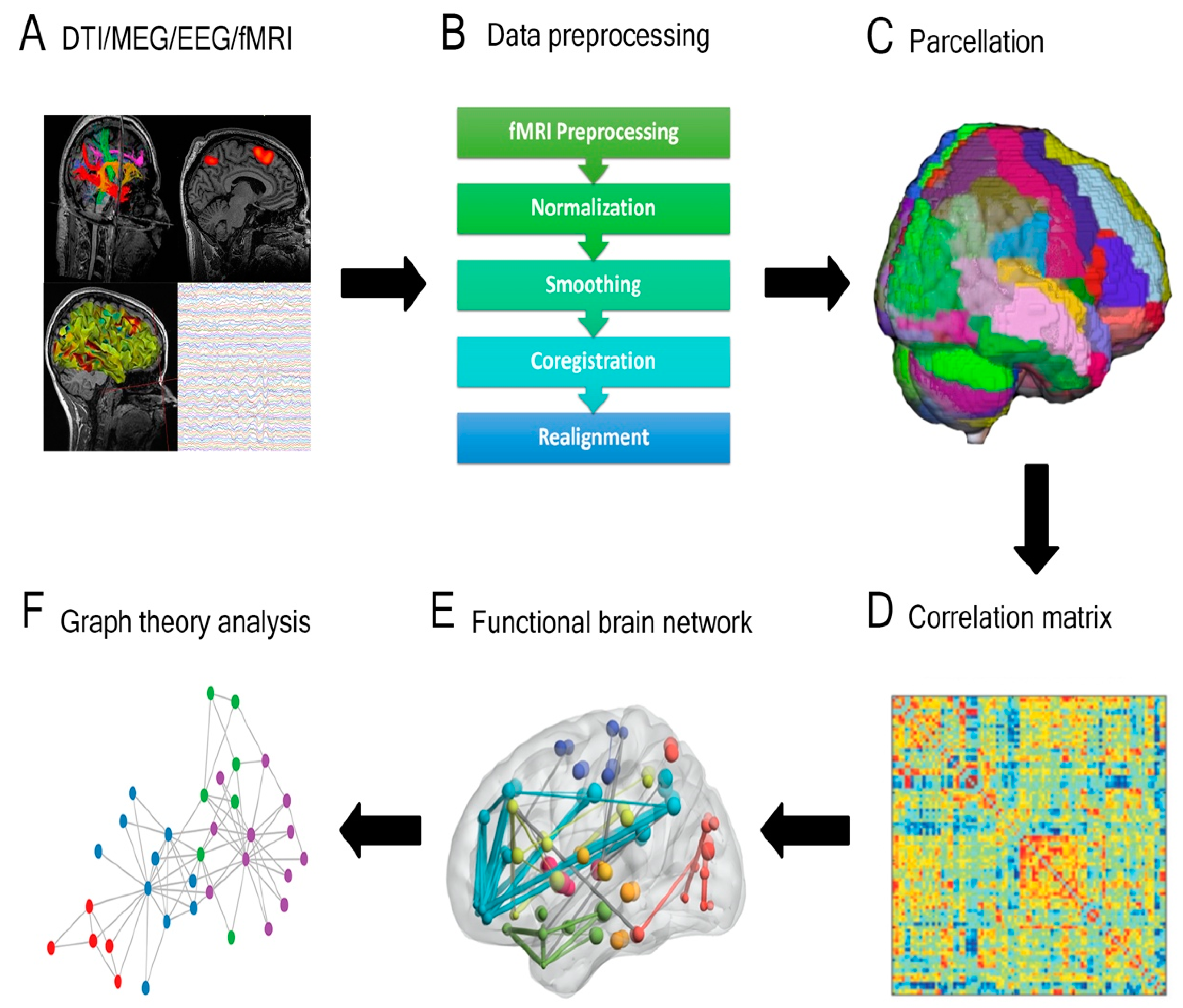
2. What Is Connectomics?
Overview of Connectomic Methodologies and Applications
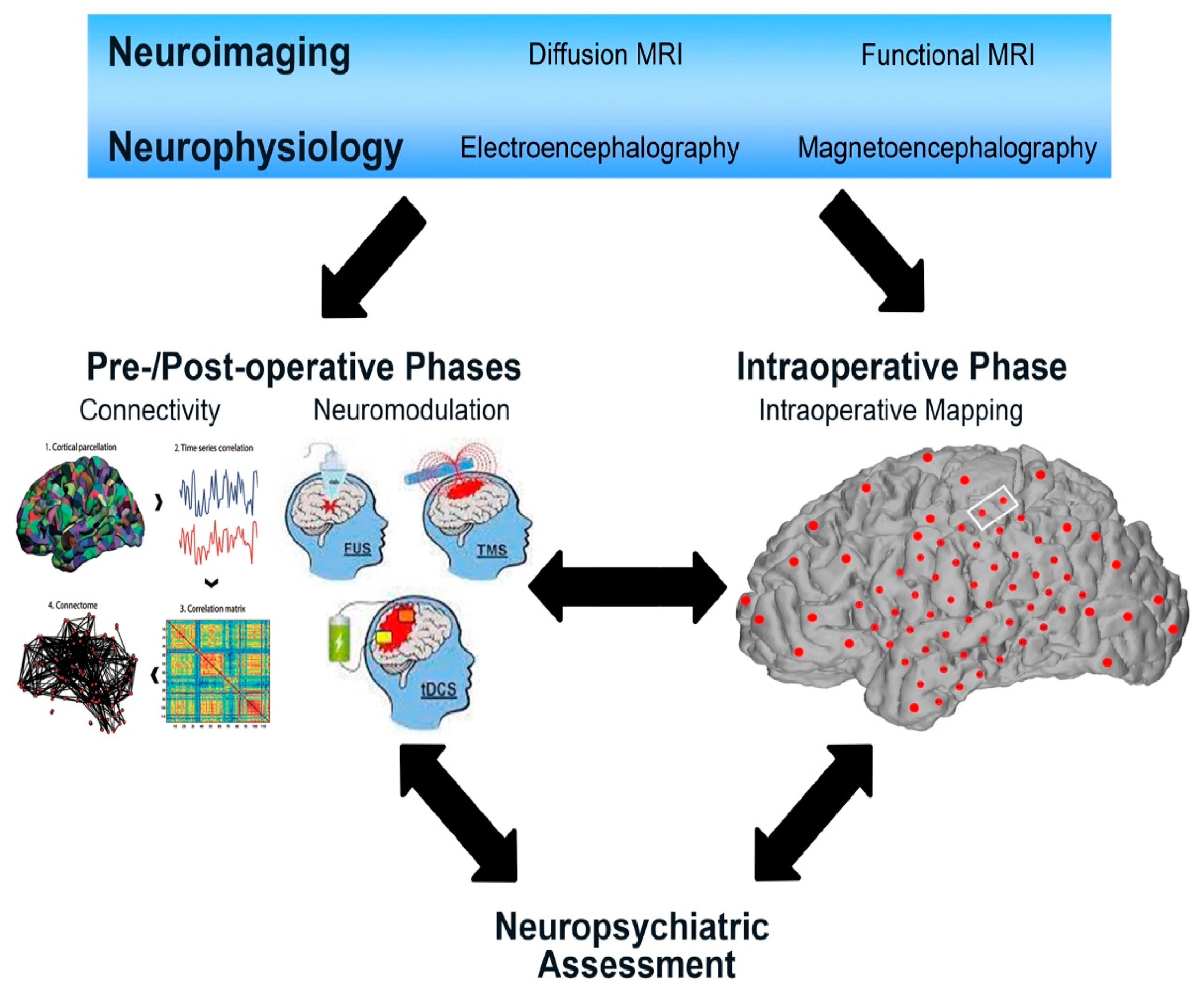
3. Integrating Connectomic Analysis into the Glioma Peri-Operative Pipeline: Lessons from Functional Neurosurgery
Demonstrated Utility of Connectomics within Functional Neurosurgery
4. Practical Applications of Connectivity for Glioma Surgery
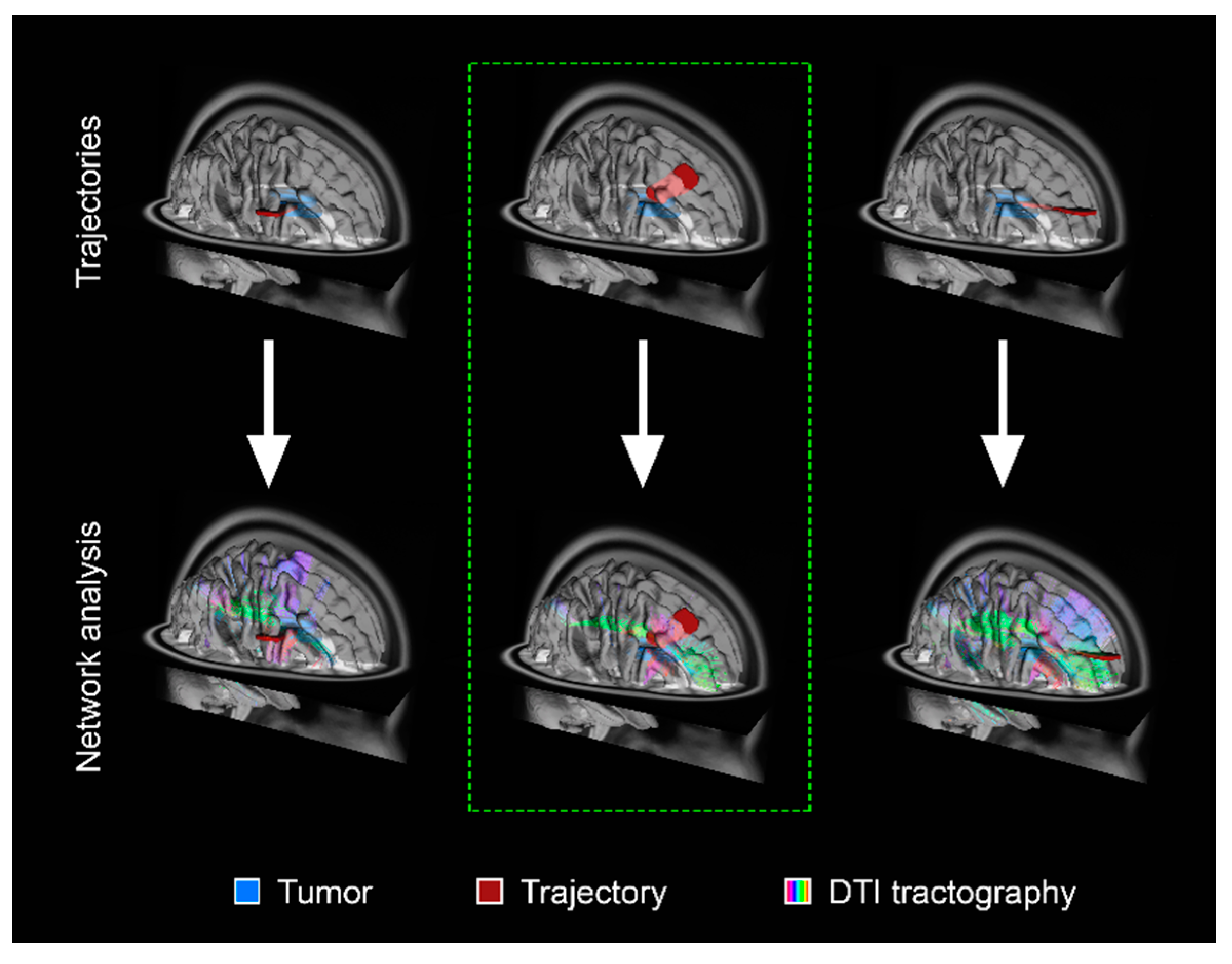
4.1. Conceptualizing Glioma Resection in Terms of Oncologic Disconnection
4.2. Preservation of Cognitive Eloquence, Higher-Order Behavioral and Social Functions
5. Employing Neuromodulation Strategies in Glioma Surgery to Influence Peri-Operative Functional Reorganization and Promote Post-Operative Neurorehabilitation
5.1. Harnessing the Neuroplastic Potential of the Brain to Modulate Function
5.2. Potential Neuromodulatory Strategies for Further Study
5.3. Metaplasticiy as a Marker of Plastic Potential
6. Limitations to Implementation
7. Future Directions
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Venkataramani, V.; Tanev, D.I.; Strahle, C.; Studier-Fischer, A.; Fankhauser, L.; Kessler, T.; Korber, C.; Kardorff, M.; Ratliff, M.; Xie, R.; et al. Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature 2019, 573, 532–538. [Google Scholar] [CrossRef]
- Venkatesh, H.S.; Morishita, W.; Geraghty, A.C.; Silverbush, D.; Gillespie, S.M.; Arzt, M.; Tam, L.T.; Espenel, C.; Ponnuswami, A.; Ni, L.; et al. Electrical and synaptic integration of glioma into neural circuits. Nature 2019, 573, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Dadario, N.B.; Brahimaj, B.; Yeung, J.; Sughrue, M.E. Reducing the Cognitive Footprint of Brain Tumor Surgery. Front. Neurol. 2021, 12, 711646. [Google Scholar] [CrossRef]
- Duffau, H. Functional Mapping before and after Low-Grade Glioma Surgery: A New Way to Decipher Various Spatiotemporal Patterns of Individual Neuroplastic Potential in Brain Tumor Patients. Cancers 2020, 12, 2611. [Google Scholar] [CrossRef] [PubMed]
- Mandonnet, E.; Duffau, H. An attempt to conceptualize the individual onco-functional balance: Why a standardized treatment is an illusion for diffuse low-grade glioma patients. Crit. Rev. Oncol. Hematol. 2018, 122, 83–91. [Google Scholar] [CrossRef]
- Duffau, H. The death of localizationism: The concepts of functional connectome and neuroplasticity deciphered by awake mapping, and their implications for best care of brain-damaged patients. Rev. Neurol. 2021, 177, 1093–1103. [Google Scholar] [CrossRef]
- Wong, J.K.; Middlebrooks, E.H.; Grewal, S.S.; Almeida, L.; Hess, C.W.; Okun, M.S. A Comprehensive Review of Brain Connectomics and Imaging to Improve Deep Brain Stimulation Outcomes. Mov. Disord. 2020, 35, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Baldermann, J.C.; Kibleur, A.; Treu, S.; Akram, H.; Elias, G.J.B.; Boutet, A.; Lozano, A.M.; Al-Fatly, B.; Strange, B.; et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat. Commun. 2020, 11, 3364. [Google Scholar] [CrossRef]
- Dostrovsky, J.O.; Lozano, A.M. Mechanisms of deep brain stimulation. Mov. Disord. 2002, 17 (Suppl. 3), S63–S68. [Google Scholar] [CrossRef]
- Hollunder, B.; Ganos, C.; Horn, A. Deep Brain Stimulation: From Sweet Spots to Sweet Networks? Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 939–941. [Google Scholar] [CrossRef]
- Sinha, N.; Dauwels, J.; Kaiser, M.; Cash, S.S.; Westover, M.B.; Wang, Y.; Taylor, P.N. Predicting neurosurgical outcomes in focal epilepsy patients using computational modelling. Brain 2017, 140, 319–332. [Google Scholar] [CrossRef] [Green Version]
- An, S.; Bartolomei, F.; Guye, M.; Jirsa, V. Optimization of surgical intervention outside the epileptogenic zone in the Virtual Epileptic Patient (VEP). PLoS Comput. Biol. 2019, 15, e1007051. [Google Scholar] [CrossRef] [Green Version]
- Duffau, H. Awake mapping of the brain connectome in glioma surgery: Concept is stronger than technology. Eur. J. Surg. Oncol. 2015, 41, 1261–1263. [Google Scholar] [CrossRef] [PubMed]
- Duffau, H. Can Non-invasive Brain Stimulation Be Considered to Facilitate Reoperation for Low-Grade Glioma Relapse by Eliciting Neuroplasticity? Front. Neurol. 2020, 11, 582489. [Google Scholar] [CrossRef] [PubMed]
- Hart, M.G.; Romero-Garcia, R.; Price, S.J.; Santarius, T.; Suckling, J. Connections, Tracts, Fractals, and the Rest: A Working Guide to Network and Connectivity Studies in Neurosurgery. World Neurosurg. 2020, 140, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Poologaindran, A.; Lowe, S.R.; Sughrue, M.E. The cortical organization of language: Distilling human connectome insights for supratentorial neurosurgery. J. Neurosurg. 2020, 134, 1959–1966. [Google Scholar] [CrossRef]
- Hagmann, P.; Kurant, M.; Gigandet, X.; Thiran, P.; Wedeen, V.J.; Meuli, R.; Thiran, J.P. Mapping human whole-brain structural networks with diffusion MRI. PLoS ONE 2007, 2, e597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, S.E.; Sporns, O. Brain Networks and Cognitive Architectures. Neuron 2015, 88, 207–219. [Google Scholar] [CrossRef] [Green Version]
- Bullmore, E.; Sporns, O. Complex brain networks: Graph theoretical analysis of structural and functional systems. Nat. Rev. Neurosci. 2009, 10, 186–198. [Google Scholar] [CrossRef]
- Hart, M.G.; Price, S.J.; Suckling, J. Connectome analysis for pre-operative brain mapping in neurosurgery. Br. J. Neurosurg. 2016, 30, 506–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, K.S.; Riva-Posse, P.; Gross, R.E.; Mayberg, H.S. Mapping the “Depression Switch” During Intraoperative Testing of Subcallosal Cingulate Deep Brain Stimulation. JAMA Neurol. 2015, 72, 1252–1260. [Google Scholar] [CrossRef] [Green Version]
- Riva-Posse, P.; Choi, K.S.; Holtzheimer, P.E.; Crowell, A.L.; Garlow, S.J.; Rajendra, J.K.; McIntyre, C.C.; Gross, R.E.; Mayberg, H.S. A connectomic approach for subcallosal cingulate deep brain stimulation surgery: Prospective targeting in treatment-resistant depression. Mol. Psychiatry 2018, 23, 843–849. [Google Scholar] [CrossRef] [Green Version]
- Lozano, A.M.; Lipsman, N. Probing and regulating dysfunctional circuits using deep brain stimulation. Neuron 2013, 77, 406–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mithani, K.; Mikhail, M.; Morgan, B.R.; Wong, S.; Weil, A.G.; Deschenes, S.; Wang, S.; Bernal, B.; Guillen, M.R.; Ochi, A. Connectomic Profiling Identifies Responders to Vagus Nerve Stimulation. Ann. Neurol. 2019, 86, 743–753. [Google Scholar] [CrossRef]
- Boutet, A.; Madhavan, R.; Elias, G.J.B.; Joel, S.E.; Gramer, R.; Ranjan, M.; Paramanandam, V.; Xu, D.; Germann, J.; Loh, A. Predicting optimal deep brain stimulation parameters for Parkinson’s disease using functional MRI and machine learning. Nat. Commun. 2021, 12, 3043. [Google Scholar] [CrossRef] [PubMed]
- Horn, A.; Reich, M.; Vorwerk, J.; Li, N.; Wenzel, G.; Fang, Q.; Schmitz-Hubsch, T.; Nickl, R.; Kupsch, A.; Volkmann, J. Connectivity Predicts deep brain stimulation outcome in Parkinson disease. Ann. Neurol. 2017, 82, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, E.B., Jr.; Gale, J.T. Mechanisms of action of deep brain stimulation (DBS). Neurosci. Biobehav. Rev. 2008, 32, 388–407. [Google Scholar] [CrossRef] [PubMed]
- Khambhati, A.N.; Shafi, A.; Rao, V.R.; Chang, E.F. Long-term brain network reorganization predicts responsive neurostimulation outcomes for focal epilepsy. Sci. Transl. Med. 2021, 13, eabf6588. [Google Scholar] [CrossRef]
- Jakobs, M.; Fomenko, A.; Lozano, A.M.; Kiening, K.L. Cellular, molecular, and clinical mechanisms of action of deep brain stimulation—A systematic review on established indications and outlook on future developments. EMBO Mol. Med. 2019, 11, e9575. [Google Scholar] [CrossRef]
- Germann, J.; Elias, G.J.B.; Boutet, A.; Narang, K.; Neudorger, C.; Horn, A.; Loh, A.; Deeb, W.; Salvato, B.; Almeida, L. Brain structures and networks responsible for stimulation-induced memory flashbacks during forniceal deep brain stimulation for Alzheimer’s disease. Alzheimers Dement. 2021, 17, 777–787. [Google Scholar] [CrossRef]
- Elias, G.J.B.; Giacobbe, P.; Boutet, A.; Germann, J.; Beyn, M.E.; Gramer, R.M.; Pancholi, A.; Joel, S.E.; Lozano, A.M. Probing the circuitry of panic with deep brain stimulation: Connectomic analysis and review of the literature. Brain Stimul. 2020, 13, 10–14. [Google Scholar] [CrossRef] [Green Version]
- Boutet, A.; Jain, M.; Elias, G.J.B.; Gramer, R.; Germann, J.; Davidson, B.; Coblentz, A.; Giacobbe, P.; Kucharczyk, W.; Wennberg, R.A. Network Basis of Seizures Induced by Deep Brain Stimulation: Literature Review and Connectivity Analysis. World Neurosurg. 2019, 132, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Elias, G.J.B.; De Vloo, P.; Germann, J.; Boutet, A.; Gramer, R.M.; Joel, S.E.; Morlion, B.; Nuttin, B.; Lozano, A.M. Mapping the network underpinnings of central poststroke pain and analgesic neuromodulation. Pain 2020, 161, 2805–2819. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, A.; Boutet, A.; Elias, G.; Germann, J.; Yan, H.; Babu, H.; Lozano, A.M.; Valiante, T.A. Lesion Network Mapping Analysis Identifies Potential Cause of Postoperative Depression in a Case of Cingulate Low-Grade Glioma. World Neurosurg. 2020, 133, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Lang, S. Cognitive eloquence in neurosurgery: Insight from graph theoretical analysis of complex brain networks. Med. Hypotheses. 2017, 98, 49–56. [Google Scholar] [CrossRef]
- Kocher, M.; Jockwitz, C.; Lohmann, P.; Stoffels, G.; Filss, C.; Mottaghy, F.M.; Ruge, M.I.; Lucas, C.W.; Goldbrunner, R.; Shah, N.J. Lesion-Function Analysis from Multimodal Imaging and Normative Brain Atlases for Prediction of Cognitive Deficits in Glioma Patients. Cancers 2021, 13, 2373. [Google Scholar] [CrossRef] [PubMed]
- Wen, P.Y.; Kesari, S. Malignant gliomas in adults. N. Engl. J. Med. 2008, 359, 492–507. [Google Scholar] [CrossRef] [Green Version]
- Van den Heuvel, M.; Sporns, O. An anatomical substrate for integration among functional networks in human cortex. J. Neurosci. 2013, 33, 14489–14500. [Google Scholar] [CrossRef] [PubMed]
- Buckner, R.L.; DiNicola, L.M. The brain’s default network: Updated anatomy, physiology and evolving insights. Nat. Rev. Neurosci. 2019, 20, 593–608. [Google Scholar] [CrossRef]
- Cole, M.W.; Pathak, S.; Schneider, W. Identifying the brain’s most globally connected regions. Neuroimage 2010, 49, 3132–3148. [Google Scholar] [CrossRef]
- Duffau, H. The huge plastic potential of adult brain and the role of connectomics: New insights provided by serial mappings in glioma surgery. Cortex 2014, 58, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Horn, A.; Fox, M.D. Opportunities of connectomic neuromodulation. Neuroimage 2020, 221, 117180. [Google Scholar] [CrossRef]
- Feldman, D.E. Synaptic mechanisms for plasticity in neocortex. Annu. Rev. Neurosci. 2009, 32, 33–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abraham, W.C.; Bear, M.F. Metaplasticity: The plasticity of synaptic plasticity. Trends Neurosci. 1996, 19, 126–130. [Google Scholar] [CrossRef]
- Fishman, P.S.; Frenkel, V. Focused Ultrasound: An Emerging Therapeutic Modality for Neurologic Disease. Neurotherapeutics 2017, 14, 393–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conway, N.; Wildschuetz, N.; Moser, T.; Bulubas, L.; Sollmann, N.; Tanigawa, N.; Meyer, B.; Krieg, S.M. Cortical plasticity of motor-eloquent areas measured by navigated transcranial magnetic stimulation in patients with glioma. J. Neurosurg. 2017, 127, 981–991. [Google Scholar] [CrossRef]
- Deverdun, J.; van Dokkum, L.E.H.; Le Bars, E.; Herbet, G.; Mura, T.; D’agata, B.; Picot, M.; Menjot, N.; Molino, F.; Duffau, H. Language reorganization after resection of low-grade gliomas: An fMRI task based connectivity study. Brain Imaging Behav. 2020, 14, 1779–1791. [Google Scholar] [CrossRef]
- Vassal, M.; Charroud, C.; Deverdun, J.; Le Bars, E.; Molino, F.; Bonnetblanc, F.; Boyer, A.; Dutta, A.; Herbet, G.; Moritz-Gasser, S. Recovery of functional connectivity of the sensorimotor network after surgery for diffuse low-grade gliomas involving the supplementary motor area. J. Neurosurg. 2017, 126, 1181–1190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izutsu, N.; Kinoshita, M.; Yanagisawa, T.; Nakanishi, K.; Sakai, M.; Kishima, H. Preservation of Motor Function after Resection of Lower-Grade Glioma at the Precentral Gyrus and Prediction by Presurgical Functional Magnetic Resonance Imaging and Magnetoencephalography. World Neurosurg. 2017, 107, 1045e5–1045e8. [Google Scholar] [CrossRef] [PubMed]
- Duffau, H. Intraoperative cortico-subcortical stimulations in surgery of low-grade gliomas. Expert Rev. Neurother. 2005, 5, 473–485. [Google Scholar] [CrossRef]
- Louppe, E.; Moritz-Gasser, S.; Duffau, H. Language recovery through a two-stage awake surgery in an aphasic patient with a voluminous left fronto-temporo-insular glioma: Case report. Acta Neurochir. 2021, 163, 3115–3119. [Google Scholar] [CrossRef]
- Duffau, H.; Capelle, L.; Denvil, D.; Sichez, N.; Gatignol, P.; Lopes, M.; Mitchell, M.-C.; Sichez, J.-P.; Van Effenterre, R. Functional recovery after surgical resection of low grade gliomas in eloquent brain: Hypothesis of brain compensation. J. Neurol. Neurosurg. Psychiatry 2003, 74, 901–907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.J.; Udupa, K.; Ni, Z.; Moro, E.; Gunraj, C.; Mazzella, F.; Lozano, A.M.; Hodaie, M.; Lang, A.E.; Chen, R. Effects of subthalamic nucleus stimulation on motor cortex plasticity in Parkinson disease. Neurology 2015, 85, 425–432. [Google Scholar] [CrossRef] [Green Version]
- Lee, E.J.; Fomenko, A.; Lozano, A. Magnetic Resonance-Guided Focused Ultrasound: Current Status and Future Perspectives in Thermal Abalation and Blood Brain Barrier Opening. J. Korean Neurosurg. Soc. 2019, 62, 10–26. [Google Scholar] [CrossRef] [Green Version]
- Meng, Y.; Reilly, R.M.; Pezo, R.C.; Trudeau, M.; Sahgal, A.; Singnurkar, A.; Perry, J.; Myrehaug, S.; Pople, C.B.; Davidson, B. MR guided focused ultrasound enhances delivery of trastuzumab to HER2-positive brain metastases. Sci. Transl. Med. 2021, 13, eabj4011. [Google Scholar] [CrossRef] [PubMed]
- Southwell, D.G.; Hervey-Jumper, S.L.; Perry, D.W.; Berger, M.S. Intraoperative mapping during repeat awake craniotomy reveals the functional plasticity of adult cortex. J. Neurosurg. 2016, 124, 1460–1469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, T.; Muragaki, Y.; Miura, I.; Tamura, M.; Maruyama, T.; Nitta, M.; Kurisu, K.; Iseki, H.; Okada, Y. Functional plasticity of language confirmed with intraoperative electrical stimulations and updated neuronavigation: Case report of low-grade glioma of the left inferior frontal gyrus. Neurol. Med. Chir. 2014, 54, 587–592. [Google Scholar] [CrossRef] [Green Version]
- Herbet, G.; Maheu, M.; Costi, E.; Lafargue, G.; Duffau, H. Mapping neuroplastic potential in brain-damaged patients. Brain 2016, 139 Pt 3, 829–844. [Google Scholar] [CrossRef]
- Rivera-Rivera, P.A.; Rios-Lago, M.; Sachez-Casarrubios, S.; Salazar, O.; Yus, M.; Gonzales-Hidalgo, M.; Sanz, A.; Avecillas-Chasin, J.; Alvarez-Linera, J.; Pascual-Leone, A. Cortical plasticity catalyzed by prehabilitation enables extensive resection of brain tumors in eloquent areas. J. Neurosurg. 2017, 126, 1323–1333. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.-Z.; Edwards, M.J.; Rounis, E.; Bhatia, K.P.; Rothwell, J.C. Theta burst stimulation of the human motor cortex. Neuron 2005, 45, 201–206. [Google Scholar] [CrossRef] [Green Version]
- Barcia, J.A.; Sanz, A.; Gonzales-Hidalgo, M.; de Las Heras, C.; Alonso-Lera, P.; Diaz, P.; Pascual-Leone, A.; Oliviero, A.; Ortiz, T. rTMS stimulation to induce plastic changes at the language motor area in a patient with a left recidivant brain tumor affecting Broca’s area. Neurocase 2012, 18, 132–138. [Google Scholar] [CrossRef]
- Fontaine, D.; Hamani, C.; Lozano, A. Efficacy and safety of motor cortex stimulation for chronic neuropathic pain: Critical review of the literature. J. Neurosurg. 2009, 110, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Sollmann, N.; Tanigawa, N.; Bulubas, L.; Sabih, J.; Zimmer, C.; Ringel, F.; Meyer, B.; Krieg, S.M. Clinical Factors Underlying the Inter-individual Variability of the Resting Motor Threshold in Navigated Transcranial Magnetic Stimulation Motor Mapping. Brain Topogr. 2017, 30, 98–121. [Google Scholar] [CrossRef] [PubMed]
- Herbet, G.; Duffau, H. Revisiting the Functional Anatomy of the Human Brain: Toward a Meta-Networking Theory of Cerebral Functions. Physiol. Rev. 2020, 100, 1181–1228. [Google Scholar] [CrossRef] [PubMed]
- Azad, T.D.; Duffau, H. Limitations of functional neuroimaging for patient selection and surgical planning in glioma surgery. Neurosurg. Focus 2020, 48, E12. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samuel, N.; Vetkas, A.; Pancholi, A.; Sarica, C.; Loh, A.; Germann, J.; Harmsen, I.E.; Tasserie, J.; Milano, V.; Yamamoto, K.; et al. A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery. Cancers 2021, 13, 6127. https://doi.org/10.3390/cancers13236127
Samuel N, Vetkas A, Pancholi A, Sarica C, Loh A, Germann J, Harmsen IE, Tasserie J, Milano V, Yamamoto K, et al. A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery. Cancers. 2021; 13(23):6127. https://doi.org/10.3390/cancers13236127
Chicago/Turabian StyleSamuel, Nardin, Artur Vetkas, Aditya Pancholi, Can Sarica, Aaron Loh, Jurgen Germann, Irene E. Harmsen, Jordy Tasserie, Vanessa Milano, Kazuaki Yamamoto, and et al. 2021. "A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery" Cancers 13, no. 23: 6127. https://doi.org/10.3390/cancers13236127
APA StyleSamuel, N., Vetkas, A., Pancholi, A., Sarica, C., Loh, A., Germann, J., Harmsen, I. E., Tasserie, J., Milano, V., Yamamoto, K., Kalia, S. K., Kongkham, P. N., & Lozano, A. M. (2021). A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery. Cancers, 13(23), 6127. https://doi.org/10.3390/cancers13236127





