Timing of the Pubertal Growth Spurt and Prostate Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
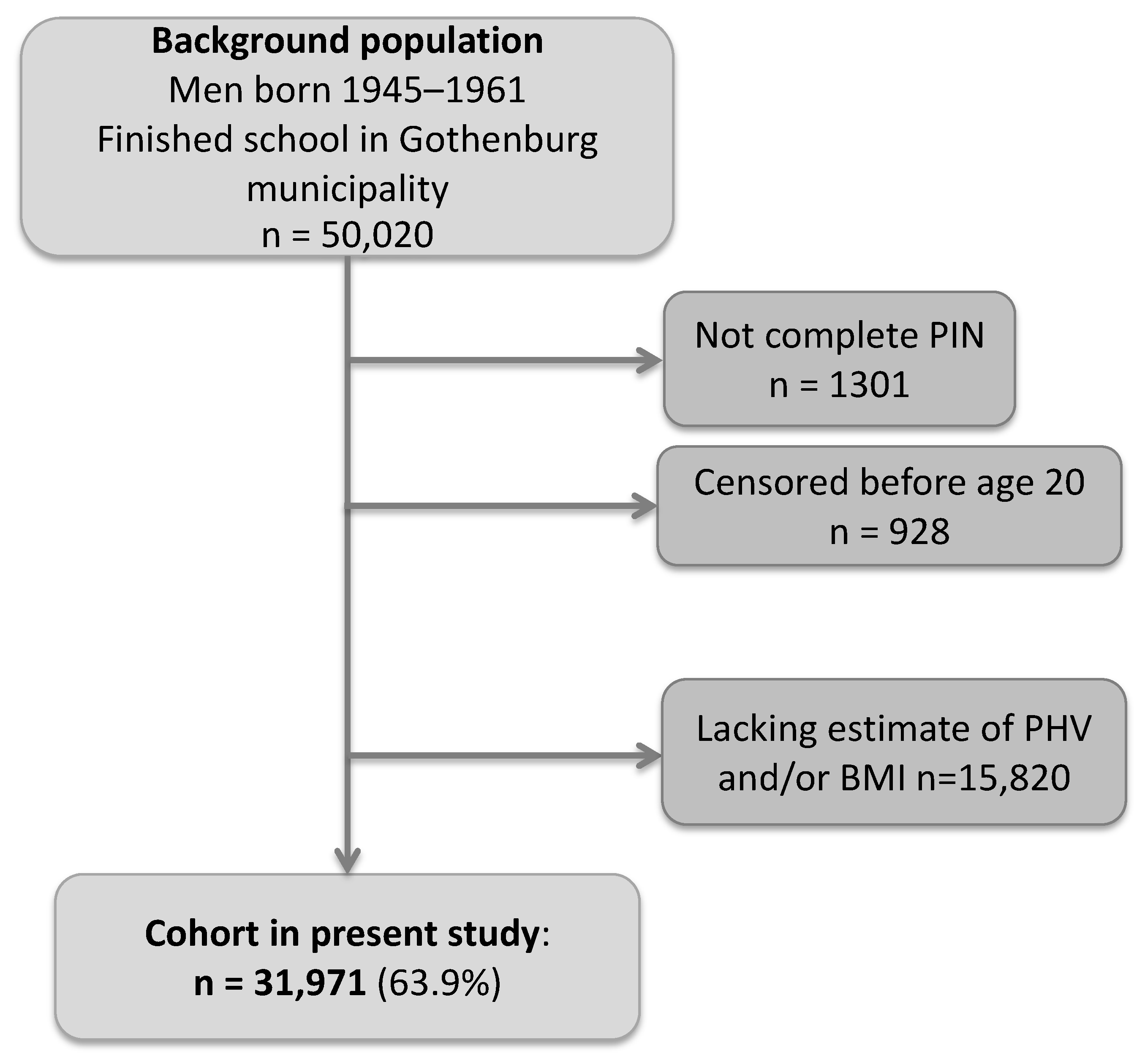
2.1. Study Population
2.2. Exposures
2.3. Outcomes
2.4. Statistical Analyses
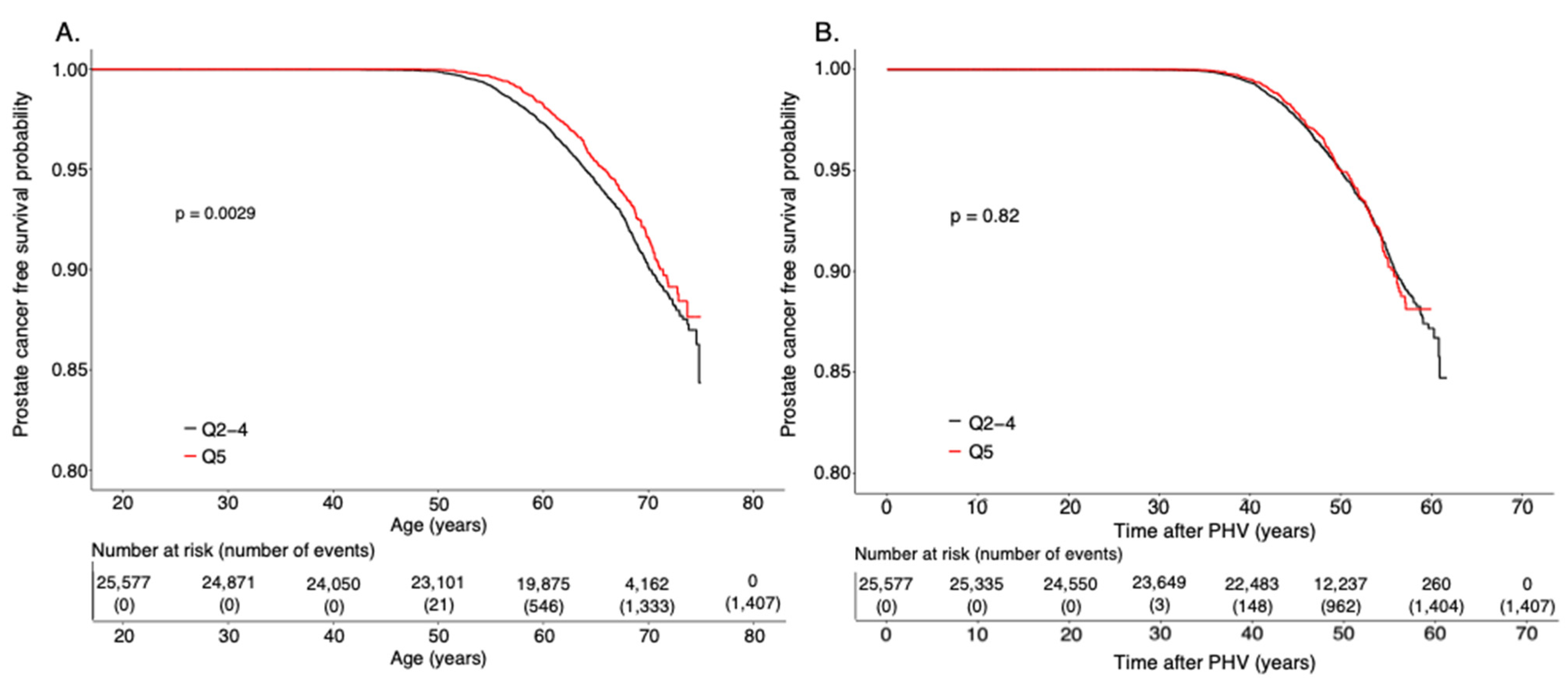
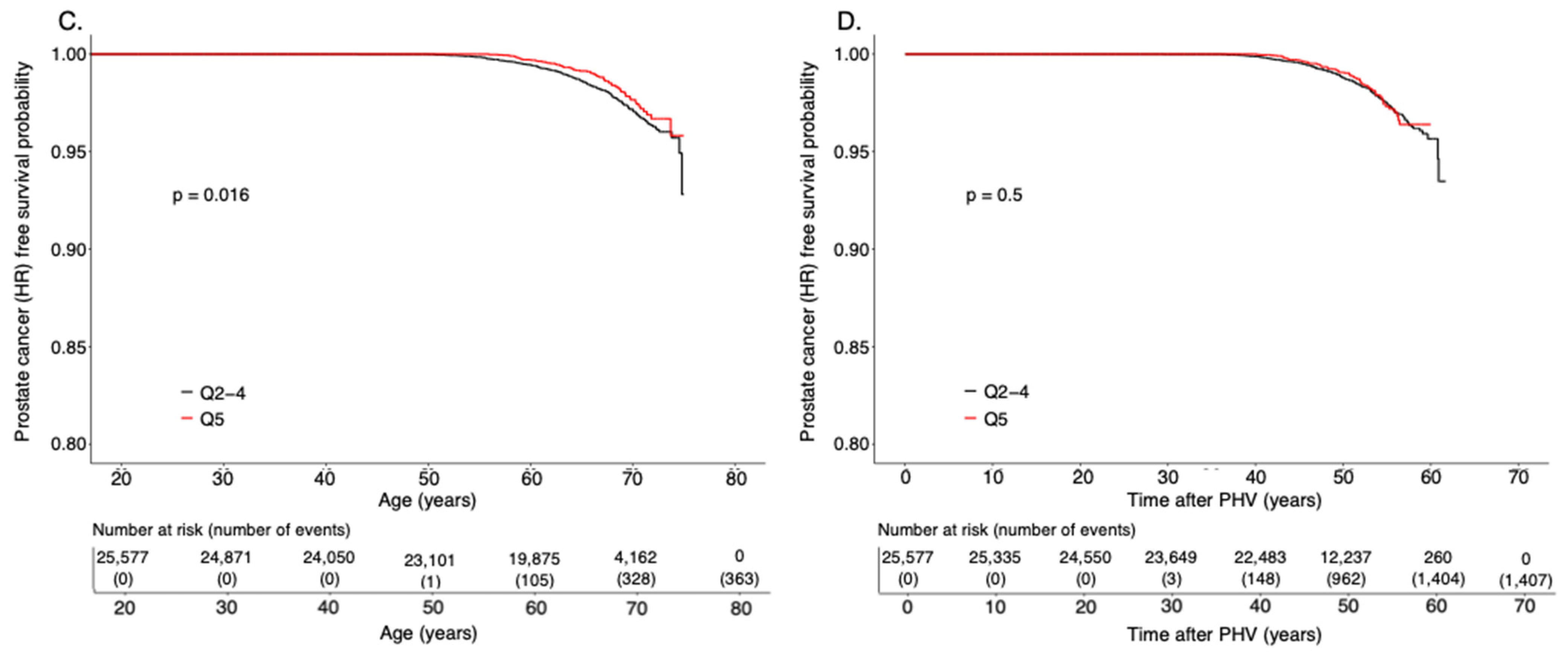
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crocetti, E. Epidemiology of Prostate Cancer in Europe; Centre for Parliamentary Studies (CfPS): London, UK, 2015. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- The Global Cancer Observatory; WHO; The International Agency for Research on Cancer. Globocan 2020. Prostate Cancer Fact Sheet. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/27-Prostate-fact-sheet.pdf (accessed on 19 April 2021).
- Haggstrom, C.; Stocks, T.; Ulmert, D.; Bjorge, T.; Ulmer, H.; Hallmans, G.; Manjer, J.; Engeland, A.; Nagel, G.; Almqvist, M.; et al. Prospective study on metabolic factors and risk of prostate cancer. Cancer 2012, 118, 6199–6206. [Google Scholar] [CrossRef] [PubMed]
- Mandair, D.; Rossi, R.E.; Pericleous, M.; Whyand, T.; Caplin, M.E. Prostate cancer and the influence of dietary factors and supplements: A systematic review. Nutr. Metab. 2014, 11, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allott, E.H.; Masko, E.M.; Freedland, S.J. Obesity and prostate cancer: Weighing the evidence. Eur. Urol. 2013, 63, 800–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heidegger, I. PSA screening—A matter of debate? Mag. Eur. Med. Urol. 2019, 12, 244–248. [Google Scholar] [CrossRef] [Green Version]
- Rawla, P. Epidemiology of Prostate Cancer. World J. Oncol. 2019, 10, 63–89. [Google Scholar] [CrossRef] [Green Version]
- Sarre, S.; Maattanen, L.; Tammela, T.L.; Auvinen, A.; Murtola, T.J. Postscreening follow-up of the Finnish Prostate Cancer Screening Trial on putative prostate cancer risk factors: Vitamin and mineral use, male pattern baldness, pubertal development and non-steroidal anti-inflammatory drug use. Scand. J. Urol. 2016, 50, 267–273. [Google Scholar] [CrossRef]
- Nair-Shalliker, V.; Yap, S.; Nunez, C.; Egger, S.; Rodger, J.; Patel, M.I.; O’Connell, D.L.; Sitas, F.; Armstrong, B.K.; Smith, D.P. Adult body size, sexual history and adolescent sexual development, may predict risk of developing prostate cancer: Results from the New South Wales Lifestyle and Evaluation of Risk Study (CLEAR). Int. J. Cancer 2017, 140, 565–574. [Google Scholar] [CrossRef]
- Lightfoot, N.; Conlon, M.; Kreiger, N.; Sass-Kortsak, A.; Purdham, J.; Darlington, G. Medical history, sexual, and maturational factors and prostate cancer risk. Ann. Epidemiol. 2004, 14, 655–662. [Google Scholar] [CrossRef]
- Giles, G.G.; Severi, G.; English, D.R.; McCredie, M.R.; MacInnis, R.; Boyle, P.; Hopper, J.L. Early growth, adult body size and prostate cancer risk. Int. J. Cancer 2003, 103, 241–245. [Google Scholar] [CrossRef]
- Habel, L.A.; Van Den Eeden, S.K.; Friedman, G.D. Body size, age at shaving initiation, and prostate cancer in a large, multiracial cohort. Prostate 2000, 43, 136–143. [Google Scholar] [CrossRef]
- Parent, A.S.; Teilmann, G.; Juul, A.; Skakkebaek, N.E.; Toppari, J.; Bourguignon, J.P. The timing of normal puberty and the age limits of sexual precocity: Variations around the world, secular trends, and changes after migration. Endocr. Rev. 2003, 24, 668–693. [Google Scholar] [CrossRef] [Green Version]
- Karlberg, J. On the modelling of human growth. Stat. Med. 1987, 6, 185–192. [Google Scholar] [CrossRef]
- Tanner, J.M. Growth of the human at the time of adolescence. Lect. Sci. Basis Med. 1953, 1, 308–363. [Google Scholar]
- Cole, T.J.; Pan, H.; Butler, G.E. A mixed effects model to estimate timing and intensity of pubertal growth from height and secondary sexual characteristics. Ann. Hum. Biol. 2014, 41, 76–83. [Google Scholar] [CrossRef]
- Ohlsson, C.; Bygdell, M.; Sonden, A.; Rosengren, A.; Kindblom, J.M. Association between excessive BMI increase during puberty and risk of cardiovascular mortality in adult men: A population-based cohort study. Lancet Diabetes Endocrinol. 2016, 4, 1017–1024. [Google Scholar] [CrossRef]
- Ohlsson, C.; Bygdell, M.; Celind, J.; Sonden, A.; Tidblad, A.; Savendahl, L.; Kindblom, J.M. Secular Trends in Pubertal Growth Acceleration in Swedish Boys Born From 1947 to 1996. JAMA Pediatr. 2019, 173, 860–865. [Google Scholar] [CrossRef] [Green Version]
- Tomic, K.; Sandin, F.; Wigertz, A.; Robinson, D.; Lambe, M.; Stattin, P. Evaluation of data quality in the National Prostate Cancer Register of Sweden. Eur. J. Cancer 2015, 51, 101–111. [Google Scholar] [CrossRef]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A.; Grading, C. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.V.; Whittington, R.; Malkowicz, S.B.; Schultz, D.; Blank, K.; Broderick, G.A.; Tomaszewski, J.E.; Renshaw, A.A.; Kaplan, I.; Beard, C.J.; et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998, 280, 969–974. [Google Scholar] [CrossRef]
- Dess, R.T.; Suresh, K.; Zelefsky, M.J.; Freedland, S.J.; Mahal, B.A.; Cooperberg, M.R.; Davis, B.J.; Horwitz, E.M.; Terris, M.K.; Amling, C.L.; et al. Development and Validation of a Clinical Prognostic Stage Group System for Nonmetastatic Prostate Cancer Using Disease-Specific Mortality Results From the International Staging Collaboration for Cancer of the Prostate. JAMA Oncol. 2020, 6, 1912–1920. [Google Scholar] [CrossRef]
- Regionala Cancercentrum i samverkan. Prostatacancer. In Nationellt Vårdprogram, 5.0 ed.; Regionala Cancercentrum i samverkan, Sveriges Kommuner och Regioner: Stockholm, Sweden, 2021; Available online: https://kunskapsbanken.cancercentrum.se/diagnoser/prostatacancer/ (accessed on 4 October 2021).
- Casey, V.A.; Dwyer, J.T.; Coleman, K.A.; Krall, E.A.; Gardner, J.; Valadian, I. Accuracy of recall by middle-aged participants in a longitudinal study of their body size and indices of maturation earlier in life. Ann. Hum. Biol. 1991, 18, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, C.; Lewis, S.J.; Martin, R.M.; Donovan, J.L.; Hamdy, F.C.; Neal, D.E.; Eeles, R.; Easton, D.; Kote-Jarai, Z.; Al Olama, A.A.; et al. Pubertal development and prostate cancer risk: Mendelian randomization study in a population-based cohort. BMC Med. 2016, 14, 66. [Google Scholar] [CrossRef] [Green Version]
- Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: Individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012, 13, 1141–1151. [Google Scholar] [CrossRef]
- Grossmann, M.; Cheung, A.S.; Zajac, J.D. Androgens and prostate cancer; pathogenesis and deprivation therapy. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 603–616. [Google Scholar] [CrossRef] [PubMed]
- Klap, J.; Schmid, M.; Loughlin, K.R. The relationship between total testosterone levels and prostate cancer: A review of the continuing controversy. J. Urol. 2015, 193, 403–413. [Google Scholar] [CrossRef]
- Ruth, K.S.; Day, F.R.; Tyrrell, J.; Thompson, D.J.; Wood, A.R.; Mahajan, A.; Beaumont, R.N.; Wittemans, L.; Martin, S.; Busch, A.S.; et al. Using human genetics to understand the disease impacts of testosterone in men and women. Nat. Med. 2020, 26, 252–258. [Google Scholar] [CrossRef]
- Watts, E.L.; Appleby, P.N.; Perez-Cornago, A.; Bueno-de-Mesquita, H.B.; Chan, J.M.; Chen, C.; Cohn, B.A.; Cook, M.B.; Flicker, L.; Freedman, N.D.; et al. Low Free Testosterone and Prostate Cancer Risk: A Collaborative Analysis of 20 Prospective Studies. Eur. Urol. 2018, 74, 585–594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rider, J.R.; Sandin, F.; Andren, O.; Wiklund, P.; Hugosson, J.; Stattin, P. Long-term outcomes among noncuratively treated men according to prostate cancer risk category in a nationwide, population-based study. Eur. Urol. 2013, 63, 88–96. [Google Scholar] [CrossRef]
- Brooke, H.L.; Talback, M.; Hornblad, J.; Johansson, L.A.; Ludvigsson, J.F.; Druid, H.; Feychting, M.; Ljung, R. The Swedish cause of death register. Eur. J. Epidemiol. 2017, 32, 765–773. [Google Scholar] [CrossRef]
- Ludvigsson, J.F.; Andersson, E.; Ekbom, A.; Feychting, M.; Kim, J.L.; Reuterwall, C.; Heurgren, M.; Olausson, P.O. External review and validation of the Swedish national inpatient register. BMC Public Health 2011, 11, 450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Hemelrijck, M.; Garmo, H.; Wigertz, A.; Nilsson, P.; Stattin, P. Cohort Profile Update: The National Prostate Cancer Register of Sweden and Prostate Cancer data Base—A refined prostate cancer trajectory. Int. J. Epidemiol. 2016, 45, 73–82. [Google Scholar] [CrossRef] [PubMed]
| Risk Classification at Diagnosis | Definition |
|---|---|
| High-risk or metastatic | Any of: PSA > 20 ng/mL Gleason score 4 + 3 = 7 or higher Tumor stage T3–4 Regional lymph node metastasis N1 Metastasis M1 |
| Low or intermediate risk | All prostate cancers not categorized as high-risk |
| HR (95% CI) for Age at PHV | |||
|---|---|---|---|
| Quintiles | Prostate cancer | High-risk or metastatic prostate cancer | Low or intermediate risk prostate cancer |
| Q1 | 0.94 (0.83–1.06) | 0.86 (0.67–1.09) | 0.97 (0.84–1.11) |
| Q2–4 | Ref | Ref | Ref |
| Q5 | 0.83 (0.73–0.94) | 0.73 (0.56–0.94) | 0.86 (0.74–0.99) |
| Quintiles of Age at PHV | Number of Cases of Prostate Cancer/100,000 Follow Up Years |
|---|---|
| Q2–4 | 92 |
| Q5 | 77 |
| Difference | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Célind, J.; Bygdell, M.; Martikainen, J.; Styrke, J.; Damber, J.-E.; Kindblom, J.M.; Ohlsson, C. Timing of the Pubertal Growth Spurt and Prostate Cancer. Cancers 2021, 13, 6238. https://doi.org/10.3390/cancers13246238
Célind J, Bygdell M, Martikainen J, Styrke J, Damber J-E, Kindblom JM, Ohlsson C. Timing of the Pubertal Growth Spurt and Prostate Cancer. Cancers. 2021; 13(24):6238. https://doi.org/10.3390/cancers13246238
Chicago/Turabian StyleCélind, Jimmy, Maria Bygdell, Jari Martikainen, Johan Styrke, Jan-Erik Damber, Jenny M. Kindblom, and Claes Ohlsson. 2021. "Timing of the Pubertal Growth Spurt and Prostate Cancer" Cancers 13, no. 24: 6238. https://doi.org/10.3390/cancers13246238






