Validation of the 8th Edition American Joint Commission on Cancer (AJCC) Gallbladder Cancer Staging System: Prognostic Discrimination and Identification of Key Predictive Factors
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
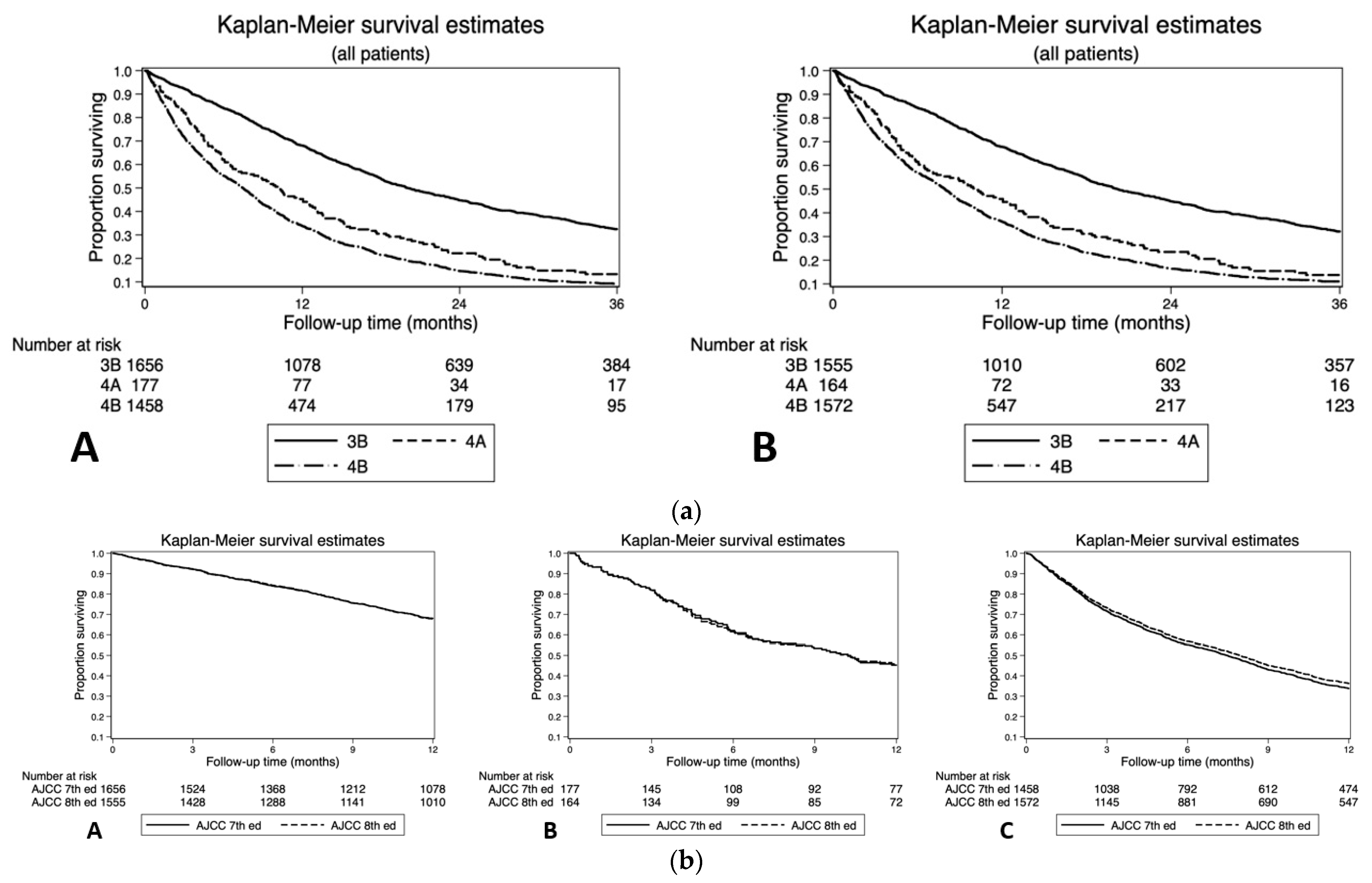
2.1. NCDB Cohort AJCC 8th and 7th Classification and Comparison (Overall Survival c-Index)
2.2. Impact of Nodal Disease on Survival of GBC Patients after AJCC 8th T-Stage Reclassification
2.3. Factors Associated with Risk of Death in GBC Patients Stratified by AJCC 8th T-Stage Classification
2.3.1. T1 Stage
2.3.2. T2 Stage
2.3.3. T3 Stage
2.3.4. T4 Stage
2.4. Factors Associated with Risk of Death in GBC Patients with Stage ≥ IIIB Classified by AJCC 8th Edition
3. Discussion
4. Materials and Methods
4.1. Data Sources and Samples
4.2. Statistical Analysis and Outcomes of Interest
4.3. Data Availability Statement
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lazcano-Ponce, E.C.; Miquel, J.F.; Munoz, N.; Herrero, R.; Ferrecio, C.; Wistuba, I.I.; Alonso de Ruiz, P.; Aristi Urista, G.; Nervi, F. Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J. Clin. 2001, 51, 349–364. [Google Scholar] [CrossRef] [PubMed]
- Hundal, R.; Shaffer, E.A. Gallbladder cancer: Epidemiology and outcome. Clin. Epidemiol. 2014, 6, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Font, C.; Gómez-Rio, M.; Rodríguez-Fernández, A.; Jiménez-Heffernan, A.; Sánchez, R.S.; Llamas-Elvira, J.M. Ability of FDG-PET/CT in the detection of gallbladder cancer. J. Surg. Oncol. 2014, 109, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Perpetuo, M.D.; Valdivieso, M.; Heilbrun, L.K.; Nelson, R.S.; Connor, T.; Bodey, G.P. Natural history study of gallbladder cancer: A review of 36 Years experience at M. D. Anderson Hospital and Tumor Institute. Cancer 1978, 42, 330–335. [Google Scholar] [CrossRef]
- Dutta, U.; Bush, N.; Kalsi, D.; Popli, P.; Kapoor, V.K. Epidemiology of gallbladder cancer in India. Chin. Clin. Oncol. 2019, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Tsilimigras, D.I.; Hyer, J.M.; Paredes, A.Z.; Moris, D.; Beal, E.W.; Merath, K.; Mehta, R.; Ejaz, A.; Cloyd, J.M.; Pawlik, T.M. The optimal number of lymph nodes to evaluate among patients undergoing surgery for gallbladder cancer: Correlating the number of nodes removed with survival in 6531 patients. J. Surg. Oncol. 2019, 119, 1099–1107. [Google Scholar] [CrossRef]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef] [Green Version]
- Wood, R.; Fraser, L.A.; Brewster, D.H.; Garden, O.J. Epidemiology of gallbladder cancer and trends in cholecystectomy rates in Scotland, 1968–1998. Eur. J. Cancer 2003, 39, 2080–2086. [Google Scholar] [CrossRef]
- Hariharan, D.; Saied, A.; Kocher, H.M. Analysis of mortality rates for gallbladder cancer across the world. Off. J. Int. Hepato Pancreato Biliary Assoc. 2008, 10, 327–331. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.-H.; Gao, Y.-T.; Huang, Y.-H.; McGee, E.E.; Lam, T.; Wang, B.; Shen, M.-C.; Rashid, A.; Pfeiffer, R.M.; Hsing, A.W.; et al. A metallomic approach to assess associations of serum metal levels with gallstones and gallbladder cancer. Hepatology 2020, 71, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, N.; Bambino, K.; Boffetta, P.; Labgaa, I. Exploring the potential carcinogenic role of arsenic in gallbladder cancer. Eur. J. Cancer Prev. 2020, 29, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Barahona Ponce, C.; Scherer, D.; Brinster, R.; Boekstegers, F.; Marcelain, K.; Gárate, V.; Müller, B.; de Toro, G.; Retamales, J.; Barajas, O.; et al. Gallstones, body mass index, C-reactive protein and gallbladder cancer—Mendelian randomization analysis of chilean and European genotype data. Hepatology 2020. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.S.; Van Dyke, A.L.; Zhu, B.; Pfeiffer, R.M.; Petrick, J.L.; Adami, H.-O.; Albanes, D.; Andreotti, G.; Beane Freeman, L.E.; Berrington de González, A.; et al. Anthropometric risk factors for cancers of the biliary tract in the biliary tract cancers pooling project. Cancer Res. 2019, 79, 3973–3982. [Google Scholar] [CrossRef]
- Duffy, A.; Capanu, M.; Abou-Alfa, G.K.; Huitzil, D.; Jarnagin, W.; Fong, Y.; D’Angelica, M.; DeMatteo, R.P.; Blumgart, L.H.; O’Reilly, E.M. Gallbladder Cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC). J. Surg. Oncol. 2008, 98, 485–489. [Google Scholar] [CrossRef]
- Dwivedi, A.N.D.; Jain, S.; Dixit, R. Gall bladder carcinoma: Aggressive malignancy with protean loco-regional and distant spread. World J. Clin. Cases 2015, 3, 231–244. [Google Scholar] [CrossRef]
- Nemunaitis, J.M.; Brown-Glabeman, U.; Soares, H.; Belmonte, J.; Liem, B.; Nir, I.; Phuoc, V.; Gullapalli, R.R. Gallbladder cancer: Review of a rare orphan gastrointestinal cancer with a focus on populations of New Mexico. BMC Cancer 2018, 18, 665. [Google Scholar] [CrossRef]
- Puhalla, H.; Bareck, E.; Scheithauer, W.; Ploner, M.; Stiglbauer, W.; Depisch, D. Therapy of gallbladder carcinoma. Experience of a central hospital. Chirurg 2002, 73, 50–56. [Google Scholar] [CrossRef]
- Henson, D.E.; Albores-Saavedra, J.; Corle, D. Carcinoma of the gallbladder. Histologic types, stage of disease, grade, and survival rates. Cancer 1992, 70, 1493–1497. [Google Scholar] [CrossRef]
- Chen, C.; Geng, Z.; Shen, H.; Song, H.; Zhao, Y.; Zhang, G.; Li, W.; Ma, L.; Wang, L. Long-term outcomes and prognostic factors in advanced gallbladder cancer: Focus on the advanced T stage. PLoS ONE 2016, 11. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Dong, P.; Zhang, Y.; Yang, M.; Chen, Y.; Tian, B.-L. Prognostic validation of the updated 8th edition tumor-node-metastasis classification by the union for international cancer control: Survival analyses of 307 patients with surgically treated gallbladder carcinoma. Oncol. Lett. 2018, 16, 4427–4433. [Google Scholar] [CrossRef] [Green Version]
- Primrose, J.N.; Fox, R.P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): A randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019, 20, 663–673. [Google Scholar] [CrossRef] [Green Version]
- Benson, A.B.; D’Angelica, M.I.; Abbott, D.E.; Abrams, T.A.; Alberts, S.R.; Anaya, D.A.; Anders, R.; Are, C.; Brown, D.; Chang, D.T.; et al. Guidelines Insights: Hepatobiliary cancers, version 2.2019. J. Natl. Compr. Cancer Netw. 2019, 17, 302–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawkins, W.G.; DeMatteo, R.P.; Jarnagin, W.R.; Ben-Porat, L.; Blumgart, L.H.; Fong, Y. Jaundice predicts advanced disease and early mortality in patients with gallbladder cancer. Ann. Surg. Oncol. 2004, 11, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P.; et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 2010, 362, 1273–1281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Joint Committee on Cancer. SEER Training. Available online: https://training.seer.cancer.gov/staging/systems/ajcc/ (accessed on 16 November 2019).
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The eighth edition AJCC cancer staging manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef]
- Amin, M.B.; Edge, S.; Greene, F.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. (Eds.) AJCC Cancer Staging Manual, 8th ed.; Springer International Publishing: New York, NY, USA, 2017; ISBN 978-3-319-40617-6. [Google Scholar]
- Shindoh, J.; de Aretxabala, X.; Aloia, T.A.; Roa, J.C.; Roa, I.; Zimmitti, G.; Javle, M.; Conrad, C.; Maru, D.M.; Aoki, T.; et al. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: An international multicenter study. Ann. Surg. 2015, 261, 733–739. [Google Scholar] [CrossRef] [Green Version]
- Oweira, H.; Mehrabi, A.; Giryes, A.; Tekbas, A.; Abdel-Rahman, O. External validation of the 8th American joint committee on cancer staging system for gall bladder carcinoma. J. Gastrointest. Oncol. 2018, 9, 1084–1090. [Google Scholar] [CrossRef]
- Jiang, W.; Zhao, B.; Li, Y.; Qi, D.; Wang, D. Modification of the 8th american joint committee on cancer staging system for gallbladder carcinoma to improve prognostic precision. BMC Cancer 2020, 20, 1129. [Google Scholar] [CrossRef]
- Lee, A.J.; Chiang, Y.-J.; Lee, J.E.; Conrad, C.; Chun, Y.-S.; Aloia, T.A.; Vauthey, J.-N.; Tzeng, C.-W.D. Validation of American joint committee on cancer eighth staging system for gallbladder cancer and its lymphadenectomy guidelines. J. Surg. Res. 2018, 230, 148–154. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Rein, L.; Clarke, C.; Mogal, H.; Tsai, S.; Christians, K.K.; Gamblin, T.C. Comparison of overall survival in gallbladder carcinoma at academic versus community cancer centers: An analysis of the national cancer data base. J. Surg. Oncol. 2020, 122, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Yang, J.; Xu, F.; Huang, Q.; Bai, L.; Wei, Y.-L.; Kaaya, R.E.; Wang, S.; Lyu, J. Prognostic Factors in patients with gallbladder adenocarcinoma identified using competing-risks analysis: A study of cases in the SEER database. Medicine 2020, 99, e21322. [Google Scholar] [CrossRef]
- Jaruvongvanich, V.; Assavapongpaiboon, B.; Wong, L. Racial/ethnic disparities in gallbladder cancer receipt of treatments. J. Gastrointest Oncol. 2018, 9, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Tran Cao, H.S.; Zhang, Q.; Sada, Y.H.; Chai, C.; Curley, S.A.; Massarweh, N.N. The role of surgery and adjuvant therapy in lymph node-positive cancers of the gallbladder and intrahepatic bile ducts. Cancer 2018, 124, 74–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.J.; Lemieux, A.; Kalpathy-Cramer, J.; Ord, C.B.; Walker, G.V.; Fuller, C.D.; Kim, J.-S.; Thomas, C.R. Nomogram for predicting the benefit of adjuvant chemoradiotherapy for resected gallbladder cancer. J Clin Oncol 2011, 29, 4627–4632. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.J.; Fuller, C.D.; Kim, J.-S.; Sittig, D.F.; Thomas, C.R.; Ravdin, P.M. Prediction model for estimating the survival benefit of adjuvant radiotherapy for gallbladder cancer. J. Clin. Oncol. 2008, 26, 2112–2117. [Google Scholar] [CrossRef]
- Geng, Z.-M.; Cai, Z.-Q.; Zhang, Z.; Tang, Z.-H.; Xue, F.; Chen, C.; Zhang, D.; Li, Q.; Zhang, R.; Li, W.-Z.; et al. Estimating survival benefit of adjuvant therapy based on a bayesian network prediction model in curatively resected advanced gallbladder adenocarcinoma. World J. Gastroenterol. 2019, 25, 5655–5666. [Google Scholar] [CrossRef]
- Kim, T.H.; Woo, S.M.; Lee, W.J.; Oh, E.S.; Youn, S.H.; Moon, S.H.; Kim, S.S.; Han, S.S.; Park, S.-J.; Kim, D.Y. Benefit of adjuvant chemoradiotherapy in resected gallbladder carcinoma. Sci. Rep. 2019, 9. [Google Scholar] [CrossRef] [Green Version]
- Zhu, X.; Zhang, X.; Hu, X.; Ren, H.; Wu, S.; Wu, J.; Wu, G.; Si, X.; Wang, B. Survival analysis of patients with primary gallbladder cancer from 2010 to 2015: A retrospective study based on SEER data. Medicine 2020, 99, e22292. [Google Scholar] [CrossRef]
- Chan, S.Y.; Poon, R.T.P.; Lo, C.M.; Ng, K.K.; Fan, S.T. Management of carcinoma of the gallbladder: A single-institution experience in 16 years. J. Surg. Oncol. 2008, 97, 156–164. [Google Scholar] [CrossRef]
- Ito, H.; Matros, E.; Brooks, D.C.; Osteen, R.T.; Zinner, M.J.; Swanson, R.S.; Ashley, S.W.; Whang, E.E. Treatment outcomes associated with surgery for gallbladder cancer: A 20-year experience. J. Gastrointest. Surg. 2004, 8, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.H.; Kwon, J.; Chie, E.K.; Kim, K.; Kim, Y.H.; Seo, D.W.; Narang, A.K.; Herman, J.M. Adjuvant chemoradiotherapy is associated with improved survival for patients with resected gallbladder carcinoma: A systematic review and Meta-analysis. Ann. Surg. Oncol. 2018, 25, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Hakeem, A.R.; Papoulas, M.; Menon, K.V. The role of neoadjuvant chemotherapy or chemoradiotherapy for advanced gallbladder cancer—A systematic review. Eur. J. Surg. Oncol. 2019, 45, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Moris, D.P.; Zhang, X.-F.; Bagante, F.; Spolverato, G.; Schmidt, C.; Dilhoff, M.; Pawlik, T.M. Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: A Surveillance, Epidemiology, and End Results (SEER) analysis. J. Surg. Oncol. 2017, 116, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Bo, X.; Shi, X.; Suo, T.; Xin, Y.; Nan, L.; Wang, C.; Ni, X.; Liu, H.; Pan, H.; et al. Modified staging classification of gallbladder carcinoma on the basis of the 8th edition of the American Joint Commission on Cancer (AJCC) staging system. Eur. J. Surg. Oncol. 2019, 46, 527–533. [Google Scholar] [CrossRef]
- Negi, S.S.; Singh, A.; Chaudhary, A. Lymph nodal involvement as prognostic factor in gallbladder cancer: Location, count or ratio? J. Gastrointest. Surg. 2011, 15, 1017–1025. [Google Scholar] [CrossRef]
- Liu, G.-J.; Li, X.-H.; Chen, Y.-X.; Sun, H.-D.; Zhao, G.-M.; Hu, S.-Y. Radical lymph node dissection and assessment: Impact on gallbladder cancer prognosis. World J. Gastroenterol. 2013, 19, 5150–5158. [Google Scholar] [CrossRef]
- Birnbaum, D.J.; Viganò, L.; Russolillo, N.; Langella, S.; Ferrero, A.; Capussotti, L. Lymph node metastases in patients undergoing surgery for a gallbladder cancer. Extension of the lymph node dissection and prognostic value of the lymph node ratio. Ann. Surg. Oncol. 2015, 22, 811–818. [Google Scholar] [CrossRef]
- Huang, X.-T.; Huang, C.-S.; Li, J.-H.; Chen, W.; Gan, T.-T.; Wang, X.-Y.; Liang, L.-J.; Yin, X.-Y. Evaluating the adequacy of nodal status in node-negative gallbladder cancer with T1b-T2 stages: Use of nodal staging score. HPB 2020. [Google Scholar] [CrossRef]
- Shirai, Y.; Sakata, J.; Wakai, T.; Ohashi, T.; Ajioka, Y.; Hatakeyama, K. Assessment of lymph node status in gallbladder cancer: Location, number, or ratio of positive nodes. World J. Surg. Oncol. 2012, 10, 87. [Google Scholar] [CrossRef] [Green Version]
- Uno, H.; Cai, T.; Pencina, M.J.; D’Agostino, R.B.; Wei, L.J. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat. Med. 2011, 30, 1105–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrell, F.E.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]

| AJCC 8th | AJCC 7th | TNM 8th | Changes between AJCC 8th and 7th Editions |
|---|---|---|---|
| I | I | T1N0M0 | Same criteria |
| IIA | II | T2aN0M0 | IIA: Peritoneal side perimuscular connective tissue invasion |
| IIB | T2bN0M0 | IIB: Hepatic side perimuscular connective tissue invasion | |
| IIIA | IIIA | T3N0M0 | N staging changed from a location-based to a number-based approach: N1: 1–3 regional nodes N2: ≥4 regional nodes |
| IIB | IIIB | T1–3N1M0 | |
| IVA | IVA | T4N0-1M0 | |
| IVB | IVB | TxN2M0 TxNxM1 |
| (a) | ||||||||
| AJCC 7th | AJCC 8th | |||||||
| I | II | IIIA | IIIB | IVA | IVB | Total | ||
| I | 1058 | 0 | 0 | 0 | 0 | 0 | 1058 | |
| II | 0 | 2393 | 0 | 0 | 0 | 0 | 2393 | |
| IIIA | 0 | 0 | 1000 | 0 | 0 | 0 | 1000 | |
| IIIB | 0 | 0 | 0 | 1512 | 0 | 144 | 1656 | |
| IVA | 0 | 0 | 0 | 0 | 163 | 14 | 177 | |
| IVB | 0 | 0 | 0 | 43 | 1 | 1415 | 1459 | |
| Total | 1058 | 2393 | 1000 | 1555 | 164 | 1573 | 7743 | |
| (b) | ||||||||
| Same Stage | Reclassified | Total | ||||||
| Age | <55 years | 861 | 33 | 894 | ||||
| 55–69 years | 2631 | 76 | 2707 | |||||
| 70 and over | 4049 | 93 | 4142 | |||||
| Sex | Male | 2236 | 64 | 2300 | ||||
| Female | 5305 | 138 | 5443 | |||||
| Race | White | 5844 | 163 | 6007 | ||||
| Black | 1097 | 27 | 1124 | |||||
| Other | 600 | 12 | 612 | |||||
| Charlson–Deyo | 0 | 4980 | 132 | 5112 | ||||
| 1 | 1886 | 54 | 1940 | |||||
| 2+ | 675 | 16 | 691 | |||||
| Insurance | Private insurance | 2130 | 68 | 2198 | ||||
| Medicare/public, or uninsured | 5411 | 134 | 5545 | |||||
| CenterVolume | 5 or fewer cases/ 3 y period | 4881 | 93 | 4974 | ||||
| >5 cases/ 3 y period | 2660 | 109 | 2769 | |||||
| Facility | Community | 671 | 10 | 681 | ||||
| Comprehensive community | 2955 | 59 | 3014 | |||||
| Academic | 3915 | 133 | 4048 | |||||
| Year of diagnosis | 2004–2006 | 1093 | 16 | 1109 | ||||
| 2007–2009 | 1283 | 32 | 1315 | |||||
| 2010–2012 | 2398 | 73 | 2471 | |||||
| 2013–2015 | 2767 | 81 | 2848 | |||||
| Surgery | Simple resection | |||||||
| Radical resection | ||||||||
| Chemotherapy | No | 4830 | 82 | 4912 | ||||
| Yes | 2711 | 120 | 2831 | |||||
| Radiation | No | 6162 | 121 | 6283 | ||||
| Yes | 1379 | 81 | 1460 | |||||
| Grade | Well-differentiated | 1109 | 16 | 1125 | ||||
| Moderate/ intermediate differentiation | 3197 | 71 | 3268 | |||||
| Poorly differentiated or undifferentiated | 2745 | 99 | 2844 | |||||
| N/A, unknown, high-grade dysplasia | 490 | 16 | 506 | |||||
| N Stage | T1 | T2 | T3 | T4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| N1 | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| N2 | 2.258 | [1.656,3.079] | 1.607 | [1.455,1.778] | 1.306 | [1.178,1.449] | 0.857 | [0.603,1.218] |
| N+ | 1.928 | [0.618,6.016] | 1.643 | [1.239,2.180] | 1.393 | [1.124,1.726] | 1.062 | [0.638,1.769] |
| Nx | 1.281 | [1.008,1.627] | 2.221 | [1.983,2.487] | 2.194 | [1.946,2.473] | 0.991 | [0.650,1.511] |
| Factors | Variable | T1 | T2 | T3 | T4 | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | ||
| Age | <55 years | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 55–69 years | 1.327 | [0.861,2.044] | 1.163 | [0.967,1.398] | 1.034 | [0.888,1.203] | 0.955 | [0.598,1.525] | |
| 70 and over | 2.647 | [1.740,4.025] | 1.486 | [1.235,1.787] | 1.141 | [0.974,1.337] | 1.269 | [0.766,2.101] | |
| Sex | Male | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Female | 0.748 | [0.609,0.919] | 0.934 | [0.846,1.031] | 0.960 | [0.872,1.058] | 0.817 | [0.577,1.157] | |
| Race | White | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Black | 0.98 | [0.733,1.311] | 1.161 | [1.018,1.324] | 1.104 | [0.965,1.263] | 0.997 | [0.628,1.584] | |
| Other | 1.079 | [0.704,1.652] | 0.796 | [0.663,0.956] | 0.877 | [0.639,0.927] | 1.153 | [0.658,2.019] | |
| Charlson–Deyo | 0 | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 1 | 0.995 | [0.788,1.256] | 1.149 | [1.035,1.275] | 1.136 | [1.024,1.261] | 0.965 | [0.661,1.409] | |
| 2+ | 1.510 | [1.129,2.020] | 1.573 | [1.366,1.812] | 1.126 | [0.950,1.335] | 0.691 | [0.340,1.404] | |
| Insurance | Private insurance | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Medicare/public, or uninsured | 1.288 | [0.966,1.717] | 1.154 | [1.027,1.296] | 1.138 | [1.018,1.272] | 1.260 | [0.895,1.772] | |
| Center Volume | 5 or fewer cases/ 3 y period | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| >5 cases/ 3 y period | 0.937 | [0.738,1.188] | 0.890 | [0.801,0.988] | 0.963 | [0.871,1.065] | 0.745 | [0.538,1.031] | |
| Facility | Community | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Comprehensive community | 0.848 | [0.614,1.171] | 0.905 | [0.772,1.060] | 0.997 | [0.843,1.179] | 1.347 | [0.674,2.695] | |
| Academic | 0.780 | [0.557,1.090] | 0.792 | [0.672,0.933] | 0.760 | [0.641,0.902] | 1.132 | [0.553,2.315] | |
| Year of diagnosis | 2004–2006 | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 2007–2009 | 0.954 | [0.707,1.286] | 1.061 | [0.905,1.243] | 1.007 | [0.922,1.152] | 1.639 | [1.039,2.586] | |
| 2010–2012 | 0.750 | [0.572,0.982] | 0.783 | [0.678,0.904] | 0.760 | [0.661,0.873] | 1.493 | [0.939,2.374] | |
| 2013–2015 | 0.489 | [0.364,0.657] | 0.745 | [0.645,0.861] | 0.728 | [0.634,0.836] | 1.044 | [0.636,1.713] | |
| Surgery | Simple resection | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Radical resection | 0.923 | [0.728,1.172] | 0.957 | [0.855,1.070] | 0.915 | [0.816,1.026] | 0.836 | [0.554,1.261] | |
| Chemotherapy | No | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Yes | 1.043 | [0.693,1.569] | 1.003 | [0.894,1.127] | 0.69 | [0.622,0.764] | 0.637 | [0.446,0.910] | |
| Radiation | No | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Yes | 0.832 | [0.503,1.377] | 0.638 | [0.553,0.735] | 0.619 | [0.546,0.702] | 0.515 | [0.337,0.787] | |
| Grade | Well- differentiated | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Moderate/ intermediate differentiation | 1.218 | [0.951,1.560] | 1.535 | [1.313,1.795] | 1.176 | [0.970,1.426] | 1.610 | [0.807,3.212] | |
| Poorly differentiated or undifferentiated | 1.968 | [1.460,2.654] | 2.434 | [2.080,2.849] | 1.765 | [1.460,2.133] | 1.822 | [0.926,3.583] | |
| N/A, unknown, high-grade dysplasia | 1.264 | [0.909,1.757] | 1.730 | [1.348,2.221] | 1.550 | [1.202,2.000] | 1.504 | [0.670,3.380] | |
| N stage | N0 | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| N1 | 2.416 | [1.683,3.467] | 1.74 | [1.554,1.947] | 1.450 | [1.304,1.612] | 1.095 | [0.729,1.645] | |
| N2 | 2.243 | [0.665,7.566] | 1.775 | [1.331,2.369] | 1.527 | [1.228,1.898] | 1.693 | [0.949,3.021] | |
| Nx | 1.256 | [0.978,1.612] | 2.097 | [1.866,2.356] | 2.010 | [1.777,2.274] | 1.100 | [0.680,1.780] |
| Factors | Variable | AJCC 7th Edition | AJCC 8th Edition | ||
|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | ||
| Stage | Stage IIIB | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Stage IVA | 1.968 | [1.638,2.365] | 1.688 | [1.481,1.923] | |
| Stage IVB | 2.379 | [2.120,2.670] | 2.008 | [1.878,2.148] | |
| Age | <55 years | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 55–69 years | 0.994 | [0.867,1.139] | 0.982 | [0.857,1.126] | |
| 70 and over | 1.139 | [0.986,1.316] | 1.111 | [0.963,1.283] | |
| Sex | Male | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Female | 0.899 | [0.821,0.985] | 0.917 | [0.838,1.003] | |
| Race | White | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Black | 0.997 | [0.885,1.123] | 1.005 | [0.893,1.131] | |
| Other | 0.862 | [0.734,1.013] | 0.856 | [0.729,1.005] | |
| Charlson–Deyo | 0 | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 1 | 1.07 | [0.974,1.176] | 1.065 | [0.970,1.170] | |
| 2+ | 1.347 | [1.159,1.566] | 1.313 | [1.131,1.524] | |
| Insurance | Private insurance | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Medicare/public, or uninsured | 1.098 | [0.996,1.211] | 1.093 | [0.992,1.205] | |
| Facility type | Community | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Comprehensive community | 0.974 | [0.837,1.134] | 0.996 | [0.856,1.158] | |
| Academic | 0.759 | [0.650,0.886] | 0.768 | [0.658,0.897] | |
| Center Volume | 5 or fewer cases/3 y period | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| >5 cases/3 y period | 0.932 | [0.851,1.021] | 0.919 | [0.840,1.007] | |
| Year of diagnosis | 2004–2006 | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| 2007–2009 | 1.008 | [0.883,1.150] | 1.009 | [0.884,1.152] | |
| 2010–2012 | 0.956 | [0.842,1.085] | 0.949 | [0.836,1.076] | |
| 2013–2015 | 0.882 | [0.776,1.003] | 0.869 | [0.766,0.986] | |
| Surgery | Simple resection | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Radical resection | 0.938 | [0.846,1.040] | 0.931 | [0.840,1.032] | |
| Chemotherapy | No | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Yes | 0.579 | [0.529,0.634] | 0.57 | [0.521,0.624] | |
| Radiotherapy | No | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Yes | 0.756 | [0.676,0.846] | 0.74 | [0.661,0.827] | |
| Grade | Well-differentiated | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| Moderate/intermediate differentiation | 1.43 | [1.194,1.712] | 1.446 | [1.210,1.727] | |
| Poorly differentiated or undifferentiated | 1.953 | [1.636,2.332] | 1.958 | [1.644,2.334] | |
| N/A, unknown, high-grade dysplasia | 1.54 | [1.216,1.949] | 1.498 | [1.185,1.894] | |
| Nodal disease | N0 | 1 | [1.000,1.000] | 1 | [1.000,1.000] |
| N1 | 1.224 | [1.067,1.404] | 1.139 | [0.995,1.304] | |
| N2 | 0.853 | [0.682,1.066] | 0.861 | [0.713,1.039] | |
| NX | 1.578 | [1.371,1.816] | 1.535 | [1.336,1.764] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannis, D.; Cerullo, M.; Moris, D.; Shah, K.N.; Herbert, G.; Zani, S.; Blazer, D.G., 3rd; Allen, P.J.; Lidsky, M.E. Validation of the 8th Edition American Joint Commission on Cancer (AJCC) Gallbladder Cancer Staging System: Prognostic Discrimination and Identification of Key Predictive Factors. Cancers 2021, 13, 547. https://doi.org/10.3390/cancers13030547
Giannis D, Cerullo M, Moris D, Shah KN, Herbert G, Zani S, Blazer DG 3rd, Allen PJ, Lidsky ME. Validation of the 8th Edition American Joint Commission on Cancer (AJCC) Gallbladder Cancer Staging System: Prognostic Discrimination and Identification of Key Predictive Factors. Cancers. 2021; 13(3):547. https://doi.org/10.3390/cancers13030547
Chicago/Turabian StyleGiannis, Dimitrios, Marcelo Cerullo, Dimitrios Moris, Kevin N. Shah, Garth Herbert, Sabino Zani, Dan G. Blazer, 3rd, Peter J. Allen, and Michael E. Lidsky. 2021. "Validation of the 8th Edition American Joint Commission on Cancer (AJCC) Gallbladder Cancer Staging System: Prognostic Discrimination and Identification of Key Predictive Factors" Cancers 13, no. 3: 547. https://doi.org/10.3390/cancers13030547
APA StyleGiannis, D., Cerullo, M., Moris, D., Shah, K. N., Herbert, G., Zani, S., Blazer, D. G., 3rd, Allen, P. J., & Lidsky, M. E. (2021). Validation of the 8th Edition American Joint Commission on Cancer (AJCC) Gallbladder Cancer Staging System: Prognostic Discrimination and Identification of Key Predictive Factors. Cancers, 13(3), 547. https://doi.org/10.3390/cancers13030547







