Fecal Immunochemical Tests Detect Screening Participants with Multiple Advanced Adenomas Better than T1 Colorectal Cancers
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Sample and Data Collection
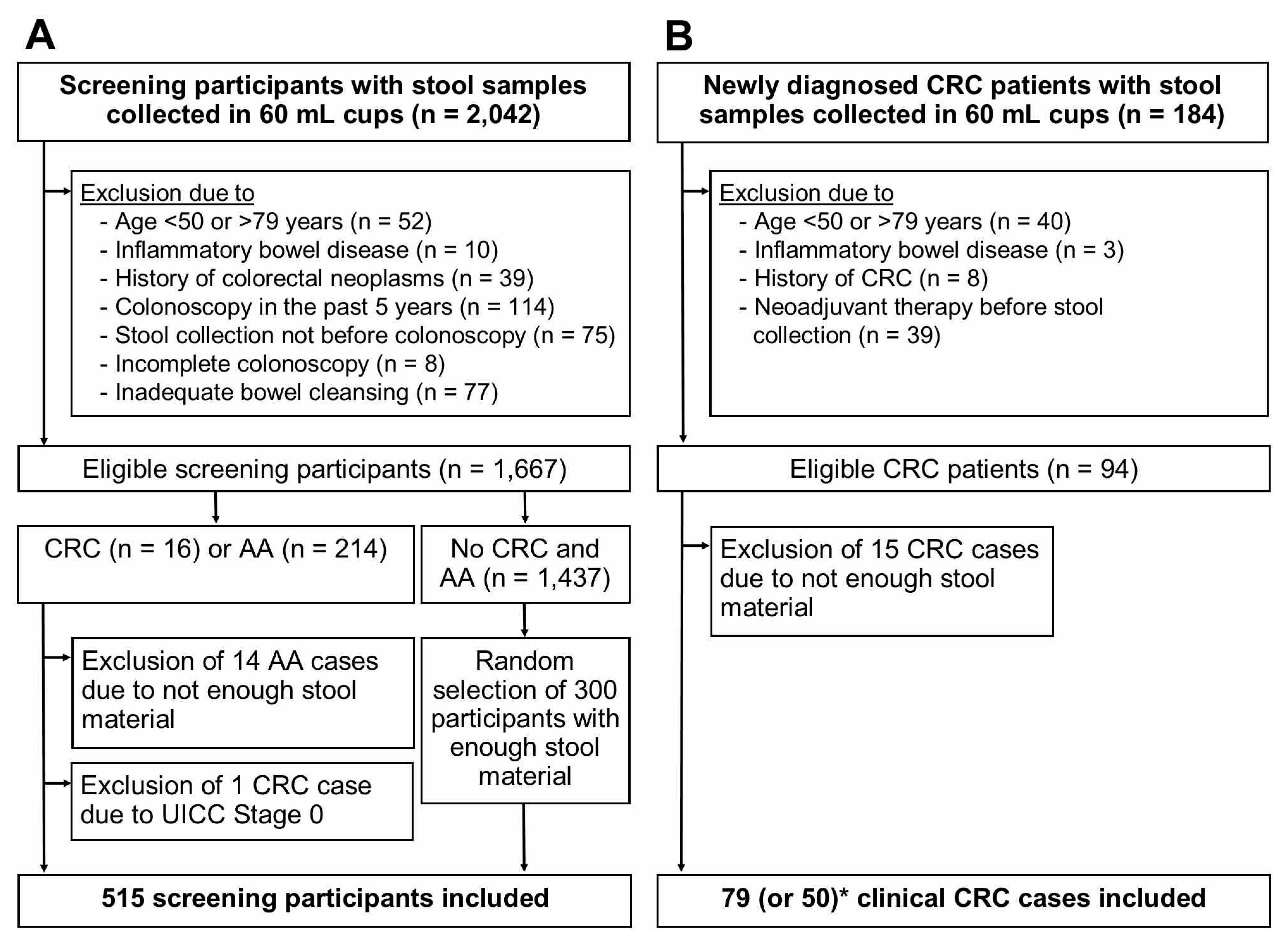
2.3. Selection of Study Participants
2.4. Laboratory Analysis
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Sensitivities at Original Cutoffs
3.3. Sensitivities at Cutoffs Yielding 93% Overall Specificity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schreuders, E.H.; Ruco, A.; Rabeneck, L.; Schoen, R.E.; Sung, J.J.; Young, G.P.; Kuipers, E.J. Colorectal cancer screening: A global overview of existing programmes. Gut 2015, 64, 1637–1649. [Google Scholar] [CrossRef] [PubMed]
- Navarro, M.; Nicolas, A.; Ferrandez, A.; Lanas, A. Colorectal cancer population screening programs worldwide in 2016: An update. World J. Gastroenterol. 2017, 23, 3632–3642. [Google Scholar] [CrossRef] [PubMed]
- Senore, C.; Basu, P.; Anttila, A.; Ponti, A.; Tomatis, M.; Vale, D.B.; Ronco, G.; Soerjomataram, I.; Primic-Zakelj, M.; Riggi, E.; et al. Performance of colorectal cancer screening in the european union member states: Data from the second european screening report. Gut 2019, 68, 1232–1244. [Google Scholar] [CrossRef]
- Gies, A.; Bhardwaj, M.; Stock, C.; Schrotz-King, P.; Brenner, H. Quantitative fecal immunochemical tests for colorectal cancer screening. Int. J. Cancer 2018, 143, 234–244. [Google Scholar] [CrossRef] [Green Version]
- Selby, K.; Levine, E.H.; Doan, C.; Gies, A.; Brenner, H.; Quesenberry, C.P.; Lee, J.K.; Corley, D.A. Effect of sex, age and positivity threshold on fecal immunochemical test accuracy: A systematic review and meta-analysis. Gastroenterology 2019, 157, 1494–1505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imperiale, T.F.; Gruber, R.N.; Stump, T.E.; Emmett, T.W.; Monahan, P.O. Performance characteristics of fecal immunochemical tests for colorectal cancer and advanced adenomatous polyps: A systematic review and meta-analysis. Ann. Intern. Med. 2019, 170, 319–329. [Google Scholar] [CrossRef] [Green Version]
- Miller, K.D.; Nogueira, L.; Mariotto, A.B.; Rowland, J.H.; Yabroff, K.R.; Alfano, C.M.; Jemal, A.; Kramer, J.L.; Siegel, R.L. Cancer treatment and survivorship statistics, 2019. CA Cancer J. Clin. 2019, 69, 363–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaukat, A.; Mongin, S.J.; Geisser, M.S.; Lederle, F.A.; Bond, J.H.; Mandel, J.S.; Church, T.R. Long-term mortality after screening for colorectal cancer. N. Engl. J. Med. 2013, 369, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Niedermaier, T.; Balavarca, Y.; Brenner, H. Stage-specific sensitivity of fecal immunochemical tests for detecting colorectal cancer: Systematic review and meta-analysis. Am. J. Gastroenterol. 2020, 115, 56–69. [Google Scholar] [CrossRef] [Green Version]
- Niedermaier, T.; Tikk, K.; Gies, A.; Bieck, S.; Brenner, H. Sensitivity of fecal immunochemical test for colorectal cancer detection differs according to stage and location. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.; et al. Stard 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, h5527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraser, C.G.; Allison, J.E.; Young, G.P.; Halloran, S.P.; Seaman, H.E. Improving the reporting of evaluations of faecal immunochemical tests for haemoglobin: The fitter standard and checklist. Eur. J. Cancer Prev. 2015, 24, 24–26. [Google Scholar] [CrossRef] [PubMed]
- Hundt, S.; Haug, U.; Brenner, H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann. Intern. Med. 2009, 150, 162–169. [Google Scholar] [CrossRef]
- Haug, U.; Kuntz, K.M.; Knudsen, A.B.; Hundt, S.; Brenner, H. Sensitivity of immunochemical faecal occult blood testing for detecting left- vs right-sided colorectal neoplasia. Br. J. Cancer 2011, 104, 1779–1785. [Google Scholar] [CrossRef] [Green Version]
- Brenner, H.; Tao, S. Superior diagnostic performance of faecal immunochemical tests for haemoglobin in a head-to-head comparison with guaiac based faecal occult blood test among 2235 participants of screening colonoscopy. Eur. J. Cancer 2013, 49, 3049–3054. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; Seiler, C.M.; Ronellenfitsch, U.; Brenner, H. Comparative evaluation of nine faecal immunochemical tests for the detection of colorectal cancer. Acta Oncol. 2013, 52, 1667–1675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gies, A.; Cuk, K.; Schrotz-King, P.; Brenner, H. Direct comparison of diagnostic performance of 9 quantitative fecal immunochemical tests for colorectal cancer screening. Gastroenterology 2018, 154, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Gies, A.; Gruner, L.F.; Schrotz-King, P.; Brenner, H. Effect of imperfect compliance with instructions for fecal sample collection on diagnostic performance of 9 fecal immunochemical tests. Clin. Gastroenterol. Hepatol. 2019, 17, 1829–1839. [Google Scholar] [CrossRef]
- Fraser, C.G.; Allison, J.E.; Halloran, S.P.; Young, G.P.; on behalf of the Expert Working Group on Fecal Immunochemical Tests for Hemoglobin Colorectal Cancer Screening Committee; World Endoscopy Organization. A proposal to standardize reporting units for fecal immunochemical tests for hemoglobin. J. Natl. Cancer Inst. 2012, 104, 810–814. [Google Scholar] [CrossRef] [Green Version]
- Tao, S.; Haug, U.; Kuhn, K.; Brenner, H. Comparison and combination of blood-based inflammatory markers with faecal occult blood tests for non-invasive colorectal cancer screening. Br. J. Cancer 2012, 106, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Elsafi, S.H.; Alqahtani, N.I.; Zakary, N.Y.; Al Zahrani, E.M. The sensitivity, specificity, predictive values, and likelihood ratios of fecal occult blood test for the detection of colorectal cancer in hospital settings. Clin. Exp. Gastroenterol. 2015, 8, 279–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirata, I.; Hoshimoto, M.; Saito, O.; Kayazawa, M.; Nishikawa, T.; Murano, M.; Toshina, K.; Wang, F.Y.; Matsuse, R. Usefulness of fecal lactoferrin and hemoglobin in diagnosis of colorectal diseases. World J. Gastroenterol. 2007, 13, 1569–1574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, B.C.; Joo, J.; Chang, H.J.; Yeo, H.Y.; Yoo, B.C.; Park, B.; Park, J.W.; Sohn, D.K.; Hong, C.W.; Han, K.S. A predictive model combining fecal calgranulin b and fecal occult blood tests can improve the diagnosis of colorectal cancer. PLoS ONE 2014, 9, e106182. [Google Scholar] [CrossRef]
- Niedermaier, T.; Weigl, K.; Hoffmeister, M.; Brenner, H. Diagnostic performance of flexible sigmoidoscopy combined with fecal immunochemical test in colorectal cancer screening: Meta-analysis and modeling. Eur. J. Epidemiol. 2017, 32, 481–493. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Haug, U.; Hundt, S. Sex differences in performance of fecal occult blood testing. Am. J. Gastroenterol. 2010, 105, 2457–2464. [Google Scholar] [CrossRef]
- Khalid-de Bakker, C.A.; Jonkers, D.M.; Sanduleanu, S.; de Bruine, A.P.; Meijer, G.A.; Janssen, J.B.; van Engeland, M.; Stockbrugger, R.W.; Masclee, A.A. Test performance of immunologic fecal occult blood testing and sigmoidoscopy compared with primary colonoscopy screening for colorectal advanced adenomas. Cancer Prev. Res. Phila. 2011, 4, 1563–1571. [Google Scholar] [CrossRef] [Green Version]
- Grobbee, E.J.; Wieten, E.; Hansen, B.E.; Stoop, E.M.; de Wijkerslooth, T.R.; Lansdorp-Vogelaar, I.; Bossuyt, P.M.; Dekker, E.; Kuipers, E.J.; Spaander, M.C. Fecal immunochemical test-based colorectal cancer screening: The gender dilemma. United Eur. Gastroenterol. J. 2017, 5, 448–454. [Google Scholar] [CrossRef] [Green Version]
- Brenner, H.; Qian, J.; Werner, S. Variation of diagnostic performance of fecal immunochemical testing for hemoglobin by sex and age: Results from a large screening cohort. Clin. Epidemiol. 2018, 10, 381–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, C.M.; Wei, C.; Ensor, J.E.; Smolenski, D.J.; Amos, C.I.; Levin, B.; Berry, D.A. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control 2013, 24, 1207–1222. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Stock, C.; Hoffmeister, M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014, 348, g2467. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Werner, S.; Brenner, H. Fresh vs frozen samples and ambient temperature have little effect on detection of colorectal cancer or adenomas by a fecal immunochemical test in a colorectal cancer screening cohort in germany. Clin. Gastroenterol. Hepatol. 2017, 15, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Gies, A.; Niedermaier, T.; Weigl, K.; Schrotz-King, P.; Hoffmeister, M.; Brenner, H. Effect of long-term frozen storage and thawing of stool samples on faecal haemoglobin concentration and diagnostic performance of faecal immunochemical tests. Clin. Chem. Lab. Med. 2019, 58, 390–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| FIT Brand | Manufacturer, City, Country | Fecal Sampling Tube (Fecal Mass/Buffer Volume) | Analytical Instrument | Analytical Reading Technique | Analytical Working Range (µg Hb/g Feces) |
|---|---|---|---|---|---|
| IDK Hb ELISA | Immundiagnostik, Bensheim, Germany | IDK Extract (15 mg/1.5 mL) | DSX by Dynex Technologies | Enzyme-linked immunosorbent assay (ELISA) | 0.086 to 50 |
| QuantOn Hem | Immundiagnostik, Bensheim, Germany | QuantOn Hem TUBE (15 mg/1.5 mL) | QuantOn Hem test cassette and Smartphone * | Immunoaffinity chromatography and Photometry | 0.3 to 100 |
| immoCARE-C | CARE diagnostica, Möllersdorf, Austria | Sample Collection Tube (20 mg/2.5 mL) | immoCARE-C test cassette and CAREcube | Immunoaffinity chromatography and Photometry | 3.75 to 250 |
| RIDASCREEN Hb | R-Biopharm, Darmstadt, Germany | RIDA TUBE Hb (10 mg/2.5 mL) | DSX by Dynex Technologies | Enzyme-linked immunosorbent assay (ELISA) | 0.65 to 50 |
| CAREprime | Alfresa Pharma, Osaka, Japan | Specimen Collection Container A (9.5 mg/1.9 mL) | CAREprime | Immunoturbidimetry | 1.6 to 240 |
| SENTiFIT-FOB Gold | Sentinel Diagnostics, Milan, Italy | SENTiFIT pierceTube (10 mg/1.7 mL) | SENTiFIT 270 analyzer | Immunoturbidimetry | 1.7 to 129.88 |
| QuikRead go iFOBT | Orion Diagnostica, Espoo, Finland | QuikRead go iFOBT Sampling Set (10 mg/2.0 mL) | QuikRead go | Immunoturbidimetry | 15 to 200 |
| Eurolyser FOB test | Eurolyser Diagnostica, Salzburg, Austria | Eurolyser FOB Sample Collector (19.9 mg/1.6 mL) | Eurolyser CUBE | Immunoturbidimetry | 2.01 to 80.4 |
| OC-Sensor | Eiken Chemical, Tokyo, Japan | OC Auto-Sampling Bottle 3 (10 mg/2.0 mL) | OC Sensor io | Immunoturbidimetry | 10 to 200 |
| Screening and Clinical CRC Cases Combined (n (%)) | Screening AA Cases (n (%)) | Screening Participants Free of CRC and AA (n (%)) | ||||
|---|---|---|---|---|---|---|
| Total | 94 (100) | 65 (100) * | Total | 200 (100) | Total | 300 (100) |
| Sex | Sex | Sex | ||||
| Women | 38 (40.4) | 26 (40.0) | Women | 68 (34.0) | Women | 155 (51.7) |
| Men | 56 (59.6) | 39 (60.0) | Men | 132 (66.0) | Men | 145 (48.3) |
| Age (years) | Age (years) | Age (years) | ||||
| 50–59 | 15 (16.0) | 13 (20.0) | 50–59 | 67 (33.5) | 50–59 | 119 (39.7) |
| 60–69 | 42 (44.7) | 28 (43.1) | 60–69 | 88 (44.9) | 60–69 | 140 (46.7) |
| 70–79 | 37 (39.4) | 24 (36.9) | 70–79 | 45 (22.5) | 70–79 | 41 (13.7) |
| BMI (kg/m2) | BMI (kg/m2) | BMI (kg/m2) | ||||
| <18.5 (underweight) | 1 (1.1) | - | <18.5 (underweight) | 2 (1.0) | <18.5 (underweight) | 1 (0.3) |
| 18.5 to <25 (normal) | 31 (33.0) | 21 (32.3) | 18.5 to <25 (normal) | 54 (27.0) | 18.5 to <25 (normal) | 105 (35.0) |
| 25 to <30 (overweight) | 42 (44.7) | 31 (47.7) | 25 to <30 (overweight) | 89 (44.5) | 25 to <30 (overweight) | 124 (41.3) |
| ≥30 (obesity) | 18 (19.2) | 11 (16.9) | ≥30 (obesity) | 51 (25.5) | ≥30 (obesity) | 64 (21.3) |
| Missing | 2 (2.1) | 2 (3.1) | Missing | 4 (2.0) | Missing | 6 (2.0) |
| Location | Location | |||||
| Proximal colon | 32 (34.0) | 22 (33.9) | Proximal colon | 52 (26.0) | ||
| Distal colon | 30 (31.9) | 22 (33.9) | Distal colon | 70 (35.0) | ||
| Rectum | 31 (33.0) | 20 (30.8) | Rectum | 45 (22.5) | ||
| Missing | 1 (1.1) | 1 (1.5) | Multiple AAs | 33 (16.5) | ||
| UICC Stage | Size ≥ 1 cm | |||||
| I | 29 (30.9) | 22 (33.9) | No | 56 (28.0) | ||
| II | 26 (27.7) | 16 (24.6) | Yes | 144 (72.0) | ||
| III | 27 (28.7) | 22 (33.9) | ||||
| IV | 11 (11.7) | 4 (6.2) | Tubulovillous/villous | |||
| Missing | 1 (1.1) | 1 (1.5) | No | 62 (31.0) | ||
| Yes | 138 (69.0) | |||||
| T status | ||||||
| T1 | 18 (19.2) | 14 (21.5) | High-grade dysplasia | |||
| T2 | 18 (19.2) | 14 (21.5) | No | 184 (92.0) | ||
| T3 | 47 (50.0) | 32 (49.2) | Yes | 16 (8.0) | ||
| T4 | 9 (9.6) | 5 (7.7) | ||||
| Missing | 2 (2.1) | - | Number of AAs | |||
| Single AA | 167 (83.5) | |||||
| Multiple AAs | 33 (16.5) | |||||
| Variable | IDK Hb ELISA | QuantOn Hem | immoCARE-C | RIDASCREEN Hb | CAREprime | SENTiFIT-FOB Gold | QuikRead go iFOBT | Eurolyser FOB test | OC-Sensor |
|---|---|---|---|---|---|---|---|---|---|
| Cutoff | 2.0 µg/g | 3.7 µg/g | 6.25 µg/g | 8.0 µg/g | 6.3 µg/g | 17.0 µg/g | 15.0 µg/g | 8.04 µg/g | 10 µg/g |
| Specificity | 85.7 (81.2–89.4) | 85.7 (81.2–89.4) | 90.0 (86.0–93.2) | 90.7 (86.8–93.7) | 91.3 (87.6–94.3) | 96.3 (94.2–98.2) | 96.7 (94.0–98.4) | 97.0 (94.4–98.6) | 97.7 (95.3–99.1) |
| Sensitivity for CRC detection | |||||||||
| Overall | 83.0 (73.8–90.0) | 83.0 (73.8–90.0) | 76.6 (66.7–84.7) | 74.5 (64.4–82.9) | 73.4 (63.3–82.0) | 70.2 (79.2–62.8) | 62.8 (52.2–72.5) | 66.2 (53.4–77.4) * | 69.2 (56.6–80.1) * |
| by UICC stage | |||||||||
| I | 72.4 (52.8–87.3) | 69.0 (49.2–84.7) | 65.5 (45.7–82.1) | 62.1 (42.3–79.3) | 62.1 (42.3–79.3) | 58.6 (38.9–76.5) | 51.7 (32.5–70.6) | 54.6 (32.2–75.6) | 59.1 (36.–79.3) |
| II | 84.6 (65.1–95.6) | 88.5 (69.9–97.6) | 80.8 (60.7–93.5) | 76.9 (56.4–91.0) | 76.9 (56.4–91.0) | 76.9 (56.4–91.0) | 76.9 (56.4–91.0) | 75.0 (47.6–92.7) | 75.0 (47.6–92.7) |
| III | 92.6 (75.7–99.1) | 92.6 (75.7–99.1) | 81.5 (61.9–93.7) | 85.2 (66.3–95.8) | 81.5 (61.9–93.7) | 74.1 (53.7–88.9) | 59.3 (38.8–77.6) | 68.2 (45.1–86.1) | 72.7 (49.8–89.3) |
| IV | 81.8 (48.2–97.7) | 81.8 (48.2–97.7) | 81.8 (48.2–97.7) | 72.7 (39.0–94.0) | 72.7 (39.0–94.0) | 72.7 (39.0–94.0) | 63.6 (30.8–89.1) | 75.0 (19.4–99.4) | 75.0 (19.4–99.4) |
| p (trend) | 0.1785 | 0.1054 | 0.1897 | 0.1649 | 0.2526 | 0.2716 | 0.6030 | 0.3438 | 0.4048 |
| by T stage | |||||||||
| T1 | 55.6 (30.8–78.5) | 55.6 (30.8–78.5) | 38.9 (17.3–64.3) | 44.4 (21.5–69.2) | 44.4 (21.5–69.2) | 44.4 (21.5–69.2) | 44.4 (21.5–69.2) | 50.0 (23.0–77.0) | 50.0 (23.0–77.0) |
| T2 | 94.4 (72.7–99.9) | 83.3 (58.6–96.4) | 88.9 (65.3–98.6) | 83.3 (58.6–96.4) | 77.8 (52.4–93.6) | 72.2 (46.5–90.3) | 61.1 (35.8–82.7) | 57.1 (28.9–82.3) | 64.3 (35.1–87.2) |
| T3 | 87.2 (74.3–95.2) | 91.5 (79.6–97.6) | 85.1 (71.7–93.8) | 78.7 (64.3–89.3) | 78.7 (64.3–89.3) | 76.6 (62.0–87.7) | 70.2 (55.1–82.7) | 75.0 (56.6–88.5) | 78.1 (60.0–90.7) |
| T4 | 100 (66.4–100) | 100 (66.4–100) | 88.9 (51.8–99.7) | 100 (66.4–100) | 100 (66.4–100) | 88.9 (51.8–99.7) | 77.8 (40.0–97.2) | 80.0 (28.4–99.5) | 80.0 (28.4–99.5) |
| p (trend) | 0.0033 | 0.0004 | 0.0006 | 0.0023 | 0.0017 | 0.0083 | 0.0437 | 0.0856 | 0.0573 |
| by location | |||||||||
| Proximal only | 81.3 (63.6–92.8) | 81.3 (63.6–92.8) | 75.0 (56.6–88.5) | 75.0 (56.6–88.5) | 71.9 (53.3–86.3) | 65.6 (46.8–81.4) | 56.3 (37.7–73.6) | 63.6 (40.7–82.8) | 63.6 (40.7–82.8) |
| Distal only | 76.7 (57.7–90.1) | 76.7 (57.7–90.1) | 66.7 (47.2–82.7) | 66.7 (47.2–82.7) | 70.0 (50.6–85.3) | 63.3 (43.9–80.1) | 56.7 (37.4–74.5) | 50.0 (28.2–71.8) | 54.6 (32.2–75.6) |
| Rectum only | 90.3 (74.3–98.0) | 90.3 (74.3–98.0) | 87.1 (70.2–96.4) | 80.7 (62.5–92.6) | 77.4 (58.9–90.4) | 80.7 (62.5–92.6) | 74.2 (55.4–88.1) | 85.0 (62.1–96.8) | 90.0 (68.3–98.8) |
| p (trend) | 0.4089 | 0.4089 | 0.3037 | 0.6692 | 0.6733 | 0.2204 | 0.1563 | 0.1973 | 0.0974 |
| by sex | |||||||||
| Women | 73.7 (56.9–86.6) | 79.0 (62.7–90.5) | 68.4 (51.4–82.5) | 65.8 (48.7–80.4) | 68.4 (51.4–82.5) | 63.2 (46.0–78.2) | 55.3 (38.3–71.4) | 57.7 (36.9–76.7) | 61.5 (40.6–79.8) |
| Men | 89.3 (78.1–96.0) | 85.7 (73.8–93.6) | 82.1 (69.6–91.1) | 80.4 (67.6–89.8) | 76.8 (63.6–87.0) | 75.0 (61.6–85.6) | 67.9 (54.0–79.7) | 71.8 (55.1–85.0) | 74.4 (57.9–87.0) |
| p-value | 0.0563 | 0.4146 | 0.1422 | 0.1488 | 0.4762 | 0.2547 | 0.2778 | 0.2898 | 0.2885 |
| by age (years) | |||||||||
| 50–59 | 86.7 (59.5–98.3) | 93.3 (68.1–99.8) | 86.7 (59.5–98.3) | 80.0 (51.9–95.7) | 73.3 (44.9–92.2) | 80.0 (51.9–95.7) | 73.3 (44.9–92.2) | 76.9 (46.2–95.0) | 76.9 (46.2–95.0) |
| 60–69 | 83.3 (68.6–93.0) | 81.0 (65.9–91.4) | 73.8 (58.0–86.1) | 73.8 (58.0–86.1) | 73.8 (58.0–86.1) | 69.1 (52.9–82.4) | 61.9 (45.6–76.4) | 57.1 (37.2–75.5) | 64.3 (44.1–81.4) |
| 70–79 | 81.1 (64.8–92.0) | 81.1 (64.8–92.0) | 75.7 (58.8–88.2) | 73.0 (55.9–86.2) | 73.0 (55.9–86.2) | 67.6 (50.2–82.0) | 59.5 (42.1–75.3) | 70.8 (48.9–87.4) | 70.8 (48.9–87.4) |
| p (trend) | 0.7022 | 0.4435 | 0.6084 | 0.7400 | 1.00 | 0.5260 | 0.4538 | 1.00 | 0.8582 |
| by BMI | |||||||||
| Normal | 80.7 (62.5–92.6) | 83.9 (66.3–94.6) | 74.2 (55.4–88.1) | 71.0 (52.0–85.8) | 71.0 (52.0–85.8) | 64.5 (45.4–80.8) | 54.8 (36.0–72.7) | 61.9 (38.4–81.9) | 66.7 (43.0–85.4) |
| Overweight | 88.1 (74.4–96.0) | 81.0 (65.9–91.4) | 81.0 (65.9–91.4) | 81.0 (65.9–91.4) | 78.6 (63.2–89.7) | 76.2 (60.6–88.0) | 69.1 (52.9–82.4) | 64.5 (45.4–80.8) | 67.7 (48.6–83.3) |
| Obesity | 83.3 (58.6–96.4) | 88.9 (65.3–98.6) | 77.8 (52.4–93.6) | 72.2 (46.5–90.3) | 72.2 (46.5–90.3) | 72.2 (46.5–90.3) | 66.7 (41.0–86.7) | 81.8 (48.2–97.7) | 81.8 (48.2–97.7) |
| p (trend) | 0.8417 | 0.8463 | 0.7298 | 0.8663 | 0.8688 | 0.5233 | 0.3675 | 0.3447 | 0.5576 |
| Sensitivity for AA detection | |||||||||
| Overall | 43.5 (36.5–50.7) | 41.5 (34.6–48.7) | 35.2 (28.6–42.2) ** | 36.0 (29.4–43.1) | 31.0 (24.7–37.9) | 18.0 (12.9–24.0) | 18.5 (13.4–24.6) | 19.5 (14.3–25.7) | 18.0 (12.9–24.0) |
| by size ≥ 1 cm | |||||||||
| No | 23.2 (13.0–36.4) | 26.8 (15.8–40.3) | 23.2 (13.0–36.4) | 17.9 (8.9–30.4) | 17.9 (8.9–30.4) | 8.9 (3.0–19.6) | 8.9 (3.0–19.6) | 5.4 (1.1–14.9) | 5.4 (1.1–14.9) |
| Yes | 51.4 (42.9–59.8) | 47.2 (38.9–55.7) | 39.9 (31.8–48.4) ** | 43.1 (34.8–51.6) | 36.1 (28.3–44.5) | 21.5 (15.1–29.1) | 22.2 (15.7–29.9) | 25.0 (18.2–32.9) | 22.9 (16.3–30.7) |
| p-value | 0.0004 | 0.0104 | 0.0319 | 0.0009 | 0.0165 | 0.0410 | 0.0411 | 0.0012 | 0.0035 |
| by tubulo/-villous histology | |||||||||
| No | 46.8 (34.0–59.9) | 43.6 (31.0–56.7) | 38.7 (26.6–51.9) | 40.3 (28.1–53.6) | 33.9 (22.3–47.0) | 19.4 (10.4–31.4) | 19.4 (10.4–31.4) | 24.2 (14.2–36.7) | 19.4 (10.4–31.4) |
| Yes | 42.0 (33.7–50.7) | 40.6 (32.3–49.3) | 33.6 (25.7–42.1) ** | 34.1 (26.2–42.6) | 29.7 (22.2–38.1) | 17.4 (11.5–24.8) | 18.1 (12.1–25.6) | 17.4 (11.5–24.8) | 17.4 (11.5–24.8) |
| p-value | 0.5414 | 0.7569 | 0.5231 | 0.4278 | 0.6206 | 0.8425 | 0.8455 | 0.3344 | 0.8425 |
| by high-grade dysplasia | |||||||||
| No | 42.9 (35.7–50.4) | 40.2 (33.1–47.7) | 34.4 (27.6–41.8) ** | 35.3 (28.4–42.7) | 29.9 (23.4–37.1) | 16.9 (11.7–23.1) | 17.4 (12.2–23.7) | 18.5 (13.2–24.9) | 16.9 (11.7–23.1) |
| Yes | 50.0 (24.7–75.4) | 56.3 (29.9–80.3) | 43.8 (19.8–70.1) | 43.8 (19.8–70.1) | 43.8 (19.8–70.1) | 31.3 (11.0–58.7) | 31.3 (11.0–58.7) | 31.3 (11.0–58.7) | 31.3 (11.0–58.7) |
| p-value | 0.6084 | 0.2903 | 0.5859 | 0.5892 | 0.2676 | 0.1732 | 0.1830 | 0.2053 | 0.1732 |
| by location | |||||||||
| Proximal only | 34.6 (22.0–49.1) | 30.8 (18.7–45.1) | 23.1 (12.5–36.8) | 25.0 (14.0–39.0) | 19.2 (9.6–32.5) | 7.7 (2.1–18.5) | 11.5 (4.4–23.4) | 11.5 (4.4–23.4) | 9.6 (3.2–21.0) |
| Distal only | 48.6 (36.4–60.8) | 44.3 (32.4–56.7) | 36.2 (25.0–48.7) ** | 37.1 (25.9–49.5) | 30.0 (19.6–42.1) | 14.3 (7.1–24.7) | 14.3 (7.1–24.7) | 14.3 (7.1–24.7) | 17.1 (9.2–28.0) |
| Rectum only | 28.9 (16.4–44.3) | 31.1 (18.2–46.7) | 26.7 (14.6–41.9) | 26.7 (14.6–41.9) | 22.2 (11.2–37.1) | 8.9 (2.5–21.2) | 8.9 (2.5–21.2) | 11.1 (3.7–24.1) | 8.9 (2.5–21.2) |
| p (trend) | 0.6781 | 0.9166 | 0.6584 | 0.8265 | 0.7247 | 0.8711 | 0.7572 | 1.00 | 1.00 |
| by number of AAs | |||||||||
| Single | 38.9 (31.5–46.8) | 36.5 (29.2–44.3) | 29.5 (22.7–37.1) ** | 30.5 (23.7–38.1) | 24.6 (18.2–31.8) | 10.8 (6.5–16.5) | 12.0 (7.5–17.9) | 14.4 (9.4–20.6) | 12.6 (8.0–18.6) |
| Multiple | 66.7 (48.2–82.0) | 66.7 (48.2–82.0) | 63.6 (45.1–79.6) | 63.6 (45.1–79.6) | 63.6 (45.1–79.6) | 54.6 (36.4–71.9) | 51.5 (33.5–69.2) | 45.5 (28.1–63.7) | 45.5 (28.1–63.7) |
| p-value | 0.0040 | 0.0018 | 0.0003 | 0.0006 | <0.0001 | <0.0001 | <0.0001 | 0.0002 | <0.0001 |
| by sex | |||||||||
| Women | 36.8 (25.4–49.3) | 30.9 (20.2–43.3) | 29.4 (19.0–41.7) | 28.0 (17.7–40.2) | 23.5 (14.1–35.4) | 13.2 (6.2–23.6) | 11.8 (5.2–21.9) | 14.7 (7.3–25.4) | 13.2 (6.2–23.6) |
| Men | 47.0 (38.2–55.9) | 47.0 (38.2–55.9) | 38.2 (29.8–47.1) ** | 40.2 (31.7–49.0) | 34.9 (26.8–43.6) | 20.5 (13.9–28.4) | 22.0 (15.2–30.0) | 22.0 (15.2–30.0) | 20.5 (13.9–28.4) |
| p-value | 0.1788 | 0.0341 | 0.2735 | 0.1196 | 0.1094 | 0.2468 | 0.0865 | 0.2609 | 0.2468 |
| by age (years) | |||||||||
| 50–59 | 34.3 (23.2–46.9) | 35.8 (24.5–48.5) | 28.8 (18.3–41.3) ** | 28.4 (18.0–40.7) | 28.4 (18.0–40.7) | 13.4 (6.3–24.0) | 14.9 (7.4–25.7) | 13.4 (6.3–24.0) | 11.9 (5.3–22.2) |
| 60–69 | 48.9 (38.1–59.8) | 42.1 (31.6–53.1) | 34.1 (24.3–45.0) | 35.2 (25.3–46.1) | 27.3 (18.3–37.8) | 18.2 (10.8–27.8) | 19.3 (11.7–29.1) | 20.5 (12.6–30.4) | 18.2 (10.8–27.8) |
| 70–79 | 46.7 (31.7–62.1) | 48.9 (33.7–64.2) | 46.7 (31.7–62.1) | 48.9 (33.7–64.2) | 42.2 (27.7–57.9) | 24.4 (12.9–39.5) | 22.2 (11.2–37.1) | 26.7 (14.6–41.9) | 26.7 (14.6–41.9) |
| p (trend) | 0.1505 | 0.1766 | 0.0710 | 0.0366 | 0.1805 | 0.1721 | 0.3288 | 0.0919 | 0.0620 |
| by BMI | |||||||||
| Normal | 37.0 (24.3–51.3) | 35.2 (22.7–49.4) | 33.3 (21.1–47.5) | 29.6 (18.0–43.6) | 31.5 (19.5–45.6) | 16.7 (7.9–29.3) | 16.7 (7.9–29.3) | 16.7 (7.9–29.3) | 16.7 (7.9–29.3) |
| Overweight | 41.6 (31.2–52.5) | 37.1 (27.1–48.0) | 34.8 (25.0–45.7) | 37.1 (27.1–48.0) | 31.5 (22.0–42.2) | 14.6 (8.0–23.7) | 15.7 (8.9–25.0) | 19.1 (11.5–28.8) | 16.9 (9.8–26.3) |
| Obesity | 54.9 (40.3–68.9) | 58.8 (44.2–72.4) | 40.0 (26.4–54.8) ** | 43.1 (29.4–57.8) | 33.3 (20.8–47.9) | 27.5 (15.9–41.7) | 27.5 (15.9–41.7) | 25.5 (14.3–39.6) | 23.5 (12.8–37.5) |
| p (trend) | 0.0771 | 0.0177 | 0.5405 | 0.1581 | 0.9169 | 0.1706 | 0.1749 | 0.2765 | 0.3839 |
| Variable | IDK Hb ELISA | QuantOn Hem | immoCARE-C | RIDASCREEN Hb | CAREprime | SENTiFIT-FOB Gold | Eurolyser FOB Test | OC-Sensor |
|---|---|---|---|---|---|---|---|---|
| Cutoff | 4.8 µg/g | 9.59 µg/g | 9.2 µg/g | 12.27 µg/g | 6.65 µg/g | 1.7 µg/g | 2.01 µg/g | 3.6 µg/g |
| Specificity | 93.0 (89.5–95.6) | 93.0 (89.5–95.6) | 93.0 (89.5–95.6) | 93.0 (89.5–95.6) | 93.0 (89.5–95.6) | 93.3 (89.9–95.9) | 93.0 (89.5–95.6) | 93.0 (89.5–95.6) |
| Sensitivity for CRC detection | ||||||||
| Overall | 76.6 (66.7–84.7) | 78.7 (69.1–86.5) | 73.4 (63.3–82.0) | 73.4 (63.3–82.0) | 73.4 (63.3–82.0) | 75.5 (65.6–83.8) | 75.4 (63.1–85.2) * | 73.9 (61.5–84.0) * |
| by UICC stage | ||||||||
| I | 62.1 (42.3–79.3) | 65.5 (45.7–82.1) | 62.1 (42.3–79.3) | 62.1 (42.3–79.3) | 62.1 (42.3–79.3) | 62.1 (42.3–79.3) | 68.2 (45.1–86.1) | 63.6 (40.7–82.8) |
| II | 76.9 (56.4–91.0) | 84.6 (65.1–95.6) | 80.8 (60.7–93.5) | 76.9 (56.4–91.0) | 76.9 (56.4–91.0) | 76.9 (56.4–91.0) | 81.3 (54.4–96.0) | 81.3 (54.4–96.0) |
| III | 88.9 (70.8–97.7) | 85.2 (66.3–95.8) | 77.8 (57.7–91.4) | 81.5 (61.9–93.7) | 81.3 (54.4–96.0) | 85.2 (66.3–95.8) | 77.3 (54.6–92.2) | 77.3 (54.6–92.2) |
| IV | 81.8 (48.2–97.7) | 81.8 (48.2–97.7) | 72.7 (39.0–94.0) | 72.7 (39.0–94.0) | 72.7 (39.0–94.0) | 81.8 (48.2–97.7) | 75.0 (19.4–99.4) | 75.0 (19.4–99.4) |
| p (trend) | 0.0412 | 0.1380 | 0.3607 | 0.2526 | 0.2526 | 0.0764 | 0.6565 | 0.3854 |
| by T status | ||||||||
| T1 | 44.4 (21.5–69.2) | 50.0 (26.0–74.0) | 38.9 (17.3–64.3) | 38.9 (17.3–64.3) | 44.4 (21.5–69.2) | 50.0 (26.0–74.0) | 57.1 (28.9–82.3) | 50.0 (23.0–77.0) |
| T2 | 83.3 (58.6–96.4) | 77.8 (52.4–93.6) | 83.3 (58.6–96.4) | 83.3 (58.6–96.4) | 77.8 (52.4–93.6) | 72.2 (46.5–90.3) | 71.4 (41.9–91.6) | 71.4 (41.9–91.6) |
| T3 | 83.0 (69.2–92.4) | 87.2 (74.3–95.2) | 80.9 (66.7–90.9) | 78.7 (64.3–89.3) | 78.7 (64.3–89.3) | 83.0 (69.2–92.4) | 84.4 (67.2–94.7) | 84.4 (67.2–94.7) |
| T4 | 100 (66.4–100) | 100 (66.4–100) | 88.9 (51.8–99.7) | 100 (66.4–100) | 100 (66.4–100) | 100 (66.4–100) | 80.0 (28.4–99.5) | 80.0 (28.4–99.5) |
| p (trend) | 0.0006 | 0.0004 | 0.0017 | 0.0006 | 0.0017 | 0.0012 | 0.0833 | 0.0300 |
| by location | ||||||||
| Proximal only | 78.1 (60.0–90.7) | 78.1 (60.0–90.7) | 68.8 (50.0–83.9) | 71.9 (53.3–86.3) | 71.9 (53.3–86.3) | 71.9 (53.3–86.3) | 63.6 (40.7–82.8) | 68.2 (45.1–86.1) |
| Distal only | 66.7 (47.2–82.7) | 70.0 (50.6–85.3) | 66.7 (47.2–82.7) | 66.7 (47.2–82.7) | 70.0 (50.6–85.3) | 66.7 (47.2–82.7) | 72.7 (49.8–89.3) | 63.6 (40.7–82.8) |
| Rectum only | 83.9 (66.3–94.6) | 87.1 (70.2–96.4) | 83.9 (66.3–94.6) | 80.7 (62.5–92.6) | 77.4 (58.9–90.4) | 87.1 (70.2–96.4) | 90.0 (68.3–98.8) | 90.0 (68.3–98.8) |
| p (trend) | 0.6600 | 0.4479 | 0.2045 | 0.4819 | 0.6733 | 0.1921 | 0.0752 | 0.1646 |
| by sex | ||||||||
| Women | 68.4 (51.4–82.5) | 76.3 (59.8–88.6) | 65.8 (48.7–80.4) | 65.8 (48.7–80.4) | 68.4 (51.4–82.5) | 71.1 (54.1–84.6) | 69.2 (48.2–85.7) | 69.2 (48.2–85.7) |
| Men | 82.1 (69.6–91.1) | 80.4 (67.6–89.8) | 78.6 (65.6–88.4) | 78.6 (65.6–88.4) | 76.8 (63.6–87.0) | 78.6 (65.6–88.4) | 79.5 (63.5–90.7) | 76.9 (60.7–88.9) |
| p-value | 0.1422 | 0.7979 | 0.2343 | 0.2343 | 0.4762 | 0.4673 | 0.3889 | 0.5695 |
| by age (years) | ||||||||
| 50–59 | 80.0 (51.9–95.7) | 86.7 (59.5–98.3) | 80.0 (51.9–95.7) | 80.0 (51.9–95.7) | 73.3 (44.9–92.2) | 80.0 (51.9–95.7) | 76.9 (46.2–95.0) | 76.9 (46.2–95.0) |
| 60–69 | 73.8 (58.0–86.1) | 73.8 (58.0–86.1) | 73.8 (58.0–86.1) | 71.4 (55.4–84.3) | 73.8 (58.0–86.1) | 73.8 (58.0–86.1) | 75.0 (55.1–89.3) | 71.4 (51.3–86.8) |
| 70–79 | 78.4 (61.8–90.2) | 81.1 (64.8–92.0) | 70.3 (53.0–84.1) | 73.0 (55.9–86.2) | 73.0 (55.9–86.2) | 75.7 (58.8–88.2) | 75.0 (53.3–90.2) | 75.0 (53.3–90.2) |
| p (trend) | 1.00 | 1.00 | 0.5151 | 0.7451 | 1.00 | 0.8677 | 1.00 | 1.00 |
| by BMI | ||||||||
| Normal | 74.2 (55.4–88.1) | 80.7 (62.5–92.6) | 67.7 (48.6–83.3) | 71.0 (52.0–85.8) | 71.0 (52.0–85.8) | 74.2 (55.4–88.1) | 66.7 (43.0–85.4) | 71.4 (47.8–88.7) |
| Overweight | 81.0 (65.9–91.4) | 78.6 (63.2–89.7) | 81.0 (65.9–91.4) | 78.6 (63.2–89.7) | 78.6 (63.2–89.7) | 78.6 (63.2–89.7) | 80.7 (62.5–92.6) | 74.2 (55.4–88.1) |
| Obesity | 77.8 (52.4–93.6) | 83.3 (58.6–96.4) | 72.2 (46.5–90.3) | 72.2 (46.5–90.3) | 72.2 (46.5–90.3) | 77.8 (52.4–93.6) | 81.8 (48.2–97.7) | 81.8 (48.2–97.7) |
| p (trend) | 0.7298 | 1.00 | 0.6199 | 0.8688 | 0.8688 | 0.8639 | 0.2981 | 0.6806 |
| Sensitivity for AA detection | ||||||||
| Overall | 31.5 (25.1–38.4) | 28.0 (21.9–34.8) | 29.7 (23.4–36.5) ** | 31.0 (24.7–37.9) | 29.5 (23.3–36.3) | 28.5 (22.4–35.3) | 31.0 (24.7–37.9) | 26.5 (20.5–33.2) |
| by size ≥ 1 cm | ||||||||
| No | 17.9 (8.9–30.4) | 12.5 (5.2–24.1) | 19.6 (10.2–32.4) | 16.1 (7.6–28.3) | 16.1 (7.6–28.3) | 17.9 (8.9–30.4) | 19.6 (10.2–32.4) | 14.3 (6.4–26.2) |
| Yes | 36.8 (28.9–45.2) | 34.0 (26.4–42.4) | 33.6 (25.9–41.9) ** | 36.8 (28.9–45.2) | 34.7 (27.0–43.1) | 32.6 (25.1–40.9) | 35.4 (27.6–43.8) | 31.3 (23.8–39.5) |
| p-value | 0.0108 | 0.0026 | 0.0589 | 0.0040 | 0.0096 | 0.0383 | 0.0404 | 0.0196 |
| by tubulo/-villous histology | ||||||||
| No | 32.3 (20.9–45.3) | 24.2 (14.2–36.7) | 32.3 (20.9–45.3) | 37.1 (25.2–50.3) | 32.3 (20.9–45.3) | 29.0 (18.2–42.0) | 33.9 (22.3–47.0) | 27.4 (16.9–40.2) |
| Yes | 31.2 (23.6–39.6) | 29.7 (22.2–38.1) | 28.5 (21.1–36.8) ** | 28.3 (20.9–36.6) | 28.3 (20.9–36.6) | 28.3 (20.9–36.6) | 29.7 (22.2–38.1) | 26.1 (19.0–34.2) |
| p-value | 0.8709 | 0.4971 | 0.6173 | 0.2478 | 0.6162 | 1.00 | 0.6206 | 0.8635 |
| by high-grade dysplasia | ||||||||
| No | 30.4 (23.9–37.6) | 26.6 (20.4–33.6) | 29.0 (22.5–36.1) ** | 29.9 (23.4–37.1) | 28.3 (21.9–35.4) | 27.2 (20.9–34.2) | 30.4 (23.9–37.6) | 25.5 (19.4–32.5) |
| Yes | 43.8 (19.8–70.1) | 43.8 (19.8–70.1) | 37.5 (15.2–64.6) | 43.8 (19.8–70.1) | 43.8 (19.8–70.1) | 43.8 (19.8–70.1) | 37.5 (15.2–64.6) | 37.5 (15.2–64.6) |
| p-value | 0.2746 | 0.1545 | 0.5688 | 0.2676 | 0.2516 | 0.1618 | 0.5792 | 0.3746 |
| by location | ||||||||
| Proximal only | 15.4 (6.9–28.1) | 15.4 (6.9–28.1) | 15.4 (6.9–28.1) | 17.3 (8.2–30.3) | 17.3 (8.2–30.3) | 17.3 (8.2–30.3) | 19.2 (9.6–32.5) | 13.5 (5.6–25.8) |
| Distal only | 32.9 (22.1–45.1) | 31.4 (20.9–43.6) | 30.4 (19.9–42.7) ** | 31.4 (20.9–43.6) | 28.6 (18.4–40.6) | 28.6 (18.4–40.6) | 32.9 (22.1–45.1) | 25.7 (16.0–37.6) |
| Rectum only | 26.7 (14.6–41.9) | 17.8 (8.0–32.1) | 24.4 (12.9–39.5) | 22.2 (11.2–37.1) | 20.0 (9.6–34.6) | 20.0 (9.6–34.6) | 24.4 (12.9–39.5) | 17.8 (8.0–32.1) |
| p (trend) | 0.2024 | 0.7185 | 0.2874 | 0.5572 | 0.7185 | 0.7185 | 0.5657 | 0.6113 |
| by number of AAs | ||||||||
| Single | 25.8 (19.3–33.1) | 22.8 (16.6–29.9) | 24.1 (17.8–31.3) ** | 24.6 (18.2–31.8) | 22.8 (16.6–29.9) | 22.8 (16.6–29.9) | 26.4 (19.8–33.7) | 19.8 (14.0–26.6) |
| Multiple | 60.6 (42.1–77.1) | 54.6 (36.4–71.9) | 57.6 (39.2–74.5) | 63.6 (45.1–79.6) | 63.6 (45.1–79.6) | 57.6 (39.2–74.5) | 54.6 (36.4–71.9) | 60.6 (42.1–77.1) |
| p-value | 0.0002 | 0.0005 | 0.0003 | <0.0001 | <0.0001 | 0.0002 | 0.0033 | <0.0001 |
| by sex | ||||||||
| Women | 22.1 (12.9–33.8) | 25.0 (15.3–37.0) | 26.5 (16.5–38.6) | 22.1 (12.9–33.8) | 20.6 (11.7–32.1) | 20.6 (11.7–32.1) | 22.1 (12.9–33.8) | 20.6 (11.7–32.1) |
| Men | 36.4 (28.2–45.2) | 29.6 (21.9–38.1) | 31.3 (23.5–40.0) ** | 35.6 (27.5–44.4) | 34.1 (26.1–42.8) | 32.6 (24.7–41.3) | 35.6 (27.5–44.4) | 29.6 (21.9–38.1) |
| p-value | 0.0533 | 0.6182 | 0.5164 | 0.0542 | 0.0511 | 0.0979 | 0.0542 | 0.2362 |
| by age (years) | ||||||||
| 50–59 | 25.4 (15.5–37.5) | 22.4 (13.1–34.2) | 21.2 (12.1–33.0) ** | 25.4 (15.5–37.5) | 25.4 (15.5–37.5) | 20.9 (11.9–32.6) | 25.4 (15.5–37.5) | 20.9 (11.9–32.6) |
| 60–69 | 31.8 (22.3–42.6) | 28.4 (19.3–39.0) | 30.7 (21.3–41.4) | 28.4 (19.3–39.0) | 27.3 (18.3–37.8) | 27.3 (18.3–37.8) | 31.8 (22.3–42.6) | 23.9 (15.4–34.1) |
| 70–79 | 40.0 (25.7–55.7) | 35.6 (21.9–51.2) | 40.0 (25.7–55.7) | 44.4 (29.6–60.0) | 40.0 (25.7–55.7) | 42.2 (27.7–57.9) | 37.8 (23.8–53.5) | 40.0 (25.7–55.7) |
| p (trend) | 0.1235 | 0.1379 | 0.0360 | 0.0499 | 0.1432 | 0.0199 | 0.1805 | 0.0398 |
| by BMI | ||||||||
| Normal | 27.8 (16.5–41.6) | 25.9 (15.0–39.7) | 29.6 (18.0–43.6) | 27.8 (16.5–41.6) | 27.8 (16.5–41.6) | 27.8 (16.5–41.6) | 27.8 (16.5–41.6) | 25.9 (15.0–39.7) |
| Overweight | 31.5 (22.0–42.2) | 23.6 (15.2–33.8) | 28.1 (19.1–38.6) | 33.7 (24.0–44.5) | 30.3 (21.0–41.0) | 28.1 (19.1–38.6) | 33.7 (24.0–44.5) | 27.0 (18.1–37.4) |
| Obesity | 37.3 (24.1–52.0) | 39.2 (25.8–53.9) | 34.0 (21.2–48.8) ** | 33.3 (20.8–47.9) | 33.3 (20.8–47.9) | 31.4 (19.1–45.9) | 31.4 (19.1–45.9) | 29.4 (17.5–43.8) |
| p (trend) | 0.3476 | 0.1601 | 0.6704 | 0.6020 | 0.5971 | 0.7476 | 0.7534 | 0.7436 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gies, A.; Niedermaier, T.; Gruner, L.F.; Heisser, T.; Schrotz-King, P.; Brenner, H. Fecal Immunochemical Tests Detect Screening Participants with Multiple Advanced Adenomas Better than T1 Colorectal Cancers. Cancers 2021, 13, 644. https://doi.org/10.3390/cancers13040644
Gies A, Niedermaier T, Gruner LF, Heisser T, Schrotz-King P, Brenner H. Fecal Immunochemical Tests Detect Screening Participants with Multiple Advanced Adenomas Better than T1 Colorectal Cancers. Cancers. 2021; 13(4):644. https://doi.org/10.3390/cancers13040644
Chicago/Turabian StyleGies, Anton, Tobias Niedermaier, Laura Fiona Gruner, Thomas Heisser, Petra Schrotz-King, and Hermann Brenner. 2021. "Fecal Immunochemical Tests Detect Screening Participants with Multiple Advanced Adenomas Better than T1 Colorectal Cancers" Cancers 13, no. 4: 644. https://doi.org/10.3390/cancers13040644
APA StyleGies, A., Niedermaier, T., Gruner, L. F., Heisser, T., Schrotz-King, P., & Brenner, H. (2021). Fecal Immunochemical Tests Detect Screening Participants with Multiple Advanced Adenomas Better than T1 Colorectal Cancers. Cancers, 13(4), 644. https://doi.org/10.3390/cancers13040644






