Socioeconomic Inequalities and Ethnicity Are Associated with a Positive COVID-19 Test among Cancer Patients in the UK Biobank Cohort
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
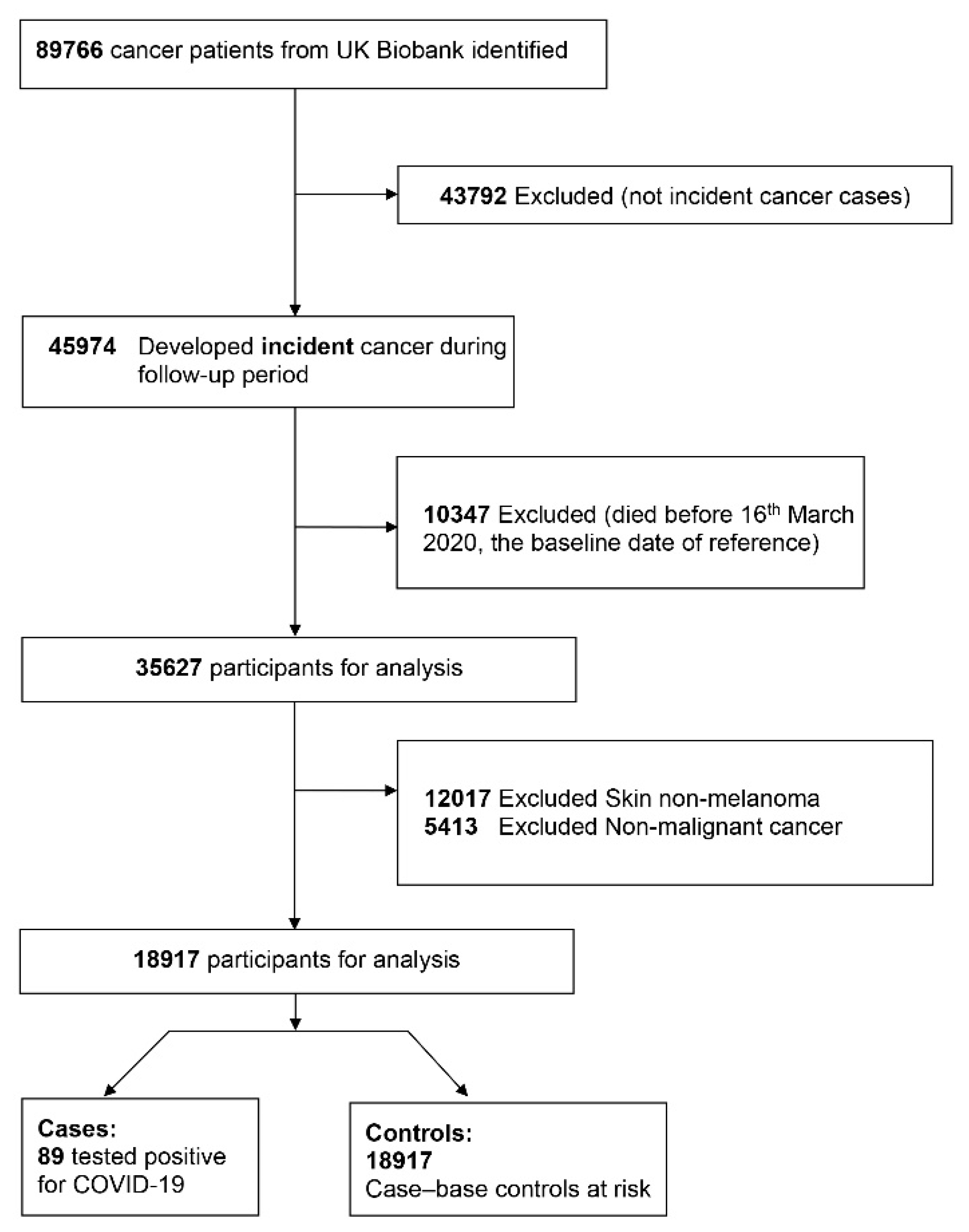
2.1. Study Design and Study Participants
2.2. Case-Base Constitution and Case-Control Definition
2.3. Sociodemographic Characteristics and Risk Factors at Baseline
2.4. Statistical Analyses
2.5. Ethics Approval and Consent to Participate
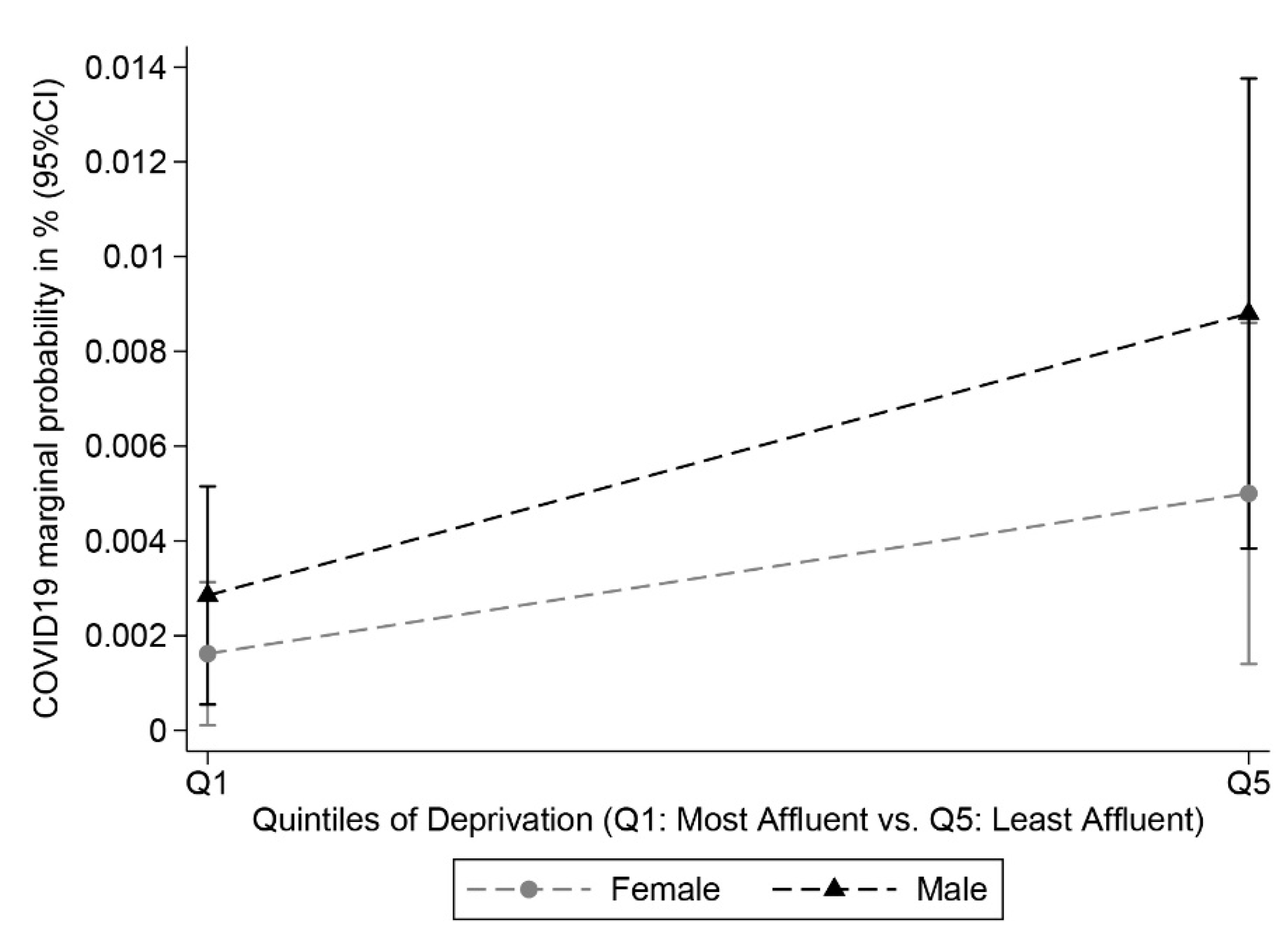
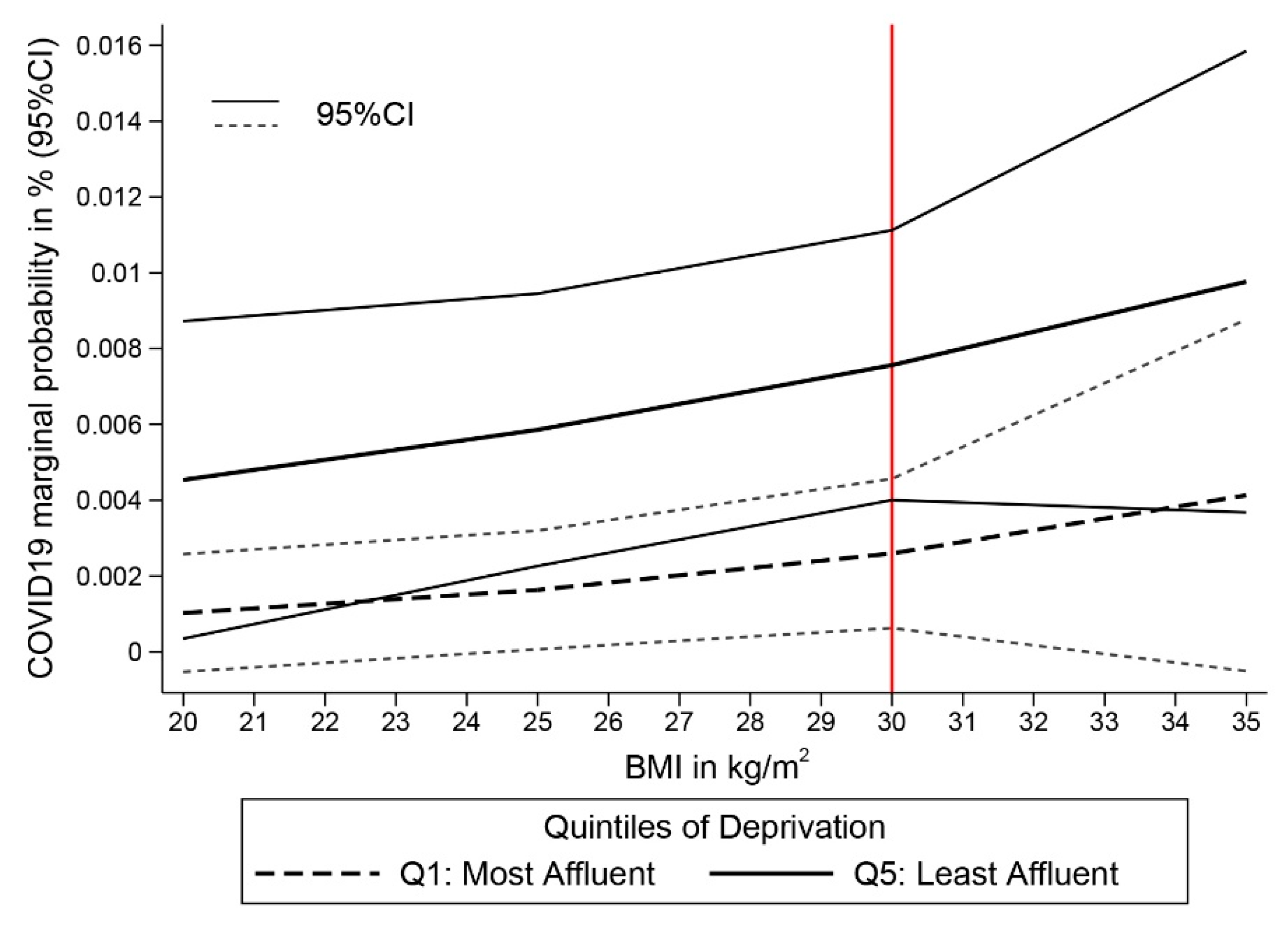
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 7 November 2020).
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.K.; Hotte, S.J.; et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef]
- Yu, J.; Ouyang, W.; Chua, M.L.K.; Xie, C. SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020, 6, 1108–1110. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.-Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Lee, L.Y.W.; Cazier, J.-B.; Angelis, V.; Arnold, R.; Bisht, V.; Campton, N.A.; Chackathayil, J.; Cheng, V.W.T.; Curley, H.M.; Fittall, M.W.; et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: A prospective cohort study. Lancet 2020, 395, 1919–1926. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Chadeau-Hyam, M.; Bodinier, B.; Elliott, J.; Whitaker, M.D.; Tzoulaki, I.; Vermeulen, R.; Kelly-Irving, M.; Delpierre, C.; Elliott, P. Risk factors for positive and negative COVID-19 tests: A cautious and in-depth analysis of UK biobank data. Int. J. Epidemiol. 2020, 49, 1454–1467. [Google Scholar] [CrossRef] [PubMed]
- Khalatbari-Soltani, S.; Cumming, R.C.; Delpierre, C.; Kelly-Irving, M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J. Epidemiol. Community Health 2020, 74, 620–623. [Google Scholar] [CrossRef]
- Rothman, K.J.; Greenland, S.; Lash, T.L. Modern Epidemiology; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef]
- UK Biobank: Follow-up of Participants in very Large Prospective Cohorts. Available online: https://www.ukbiobank.ac.uk/wp-content/uploads/2019/06/R-Flaig.pdf (accessed on 6 September 2020).
- UK Biobank: Cancer Data: Linkage from National Cancer Registries. Available online: http://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/CancerLinkage.pdf (accessed on 6 September 2020).
- Møller, H.; Richards, S.; Hanchett, N.; Riaz, S.P.; Lüchtenborg, M.; Holmberg, L.; Robinson, D. Completeness of case ascertainment and survival time error in English cancer registries: Impact on 1-year survival estimates. Br. J. Cancer 2011, 105, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.; Rudkin, J.K.; Allen, N.; Crook, D.W.; Wilson, D.J.; Wyllie, D.H.; O’Connell, A.M. Dynamic linkage of COVID-19 test results between Public Health England’s Second Generation Surveillance System and UK Biobank. Microb. Genom. 2020, 6. [Google Scholar] [CrossRef]
- UK Biobank: Linkage of COVID-19 Tests with Public Health England’s SGSS. Available online: http://biobank.ndph.ox.ac.uk/showcase/refer.cgi?id=1758 (accessed on 6 September 2020).
- UK Biobank: COVID-19 Test Results Data. Available online: http://biobank.ctsu.ox.ac.uk/crystal/exinfo.cgi?src=COVID19_tests (accessed on 6 September 2020).
- Townsend, P.; Phillimore, P.; Beattie, A. Health and Deprivation: Inequality and the North; Croom Helm: London, UK, 1988. [Google Scholar]
- WHO. Body Mass Index-BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 15 November 2020).
- Zou, G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Borgan, O.; Langholz, B.; Samuelsen, S.O.; Goldstein, L.; Pogoda, J. Exposure Stratified Case-Cohort Designs. Lifetime Data Anal. 2000, 6, 39–58. [Google Scholar] [CrossRef]
- Rubin, D.B.; Schenker, N. Multiple imputation in health-care databases: An overview and some applications. Stat. Med. 1991, 10, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Updating Ethnic Contrasts in Deaths Involving the Coronavirus (COVID-19), England and Wales: Deaths occurring 2 March to 28 July 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/updatingethniccontrastsindeathsinvolvingthecoronaviruscovid19englandandwales/deathsoccurring2marchto28july2020 (accessed on 7 November 2020).
- Greater London Authority. Rapid Evidence Review: Inequalities in Relation to COVID-19 and Their Effects on London. Available online: https://data.london.gov.uk/dataset/rapid-evidence-review-inequalities-in-relation-to-covid-19-and-their-effects-on-london (accessed on 7 November 2020).
- Main figures. Office for National Statistics. Available online: https://www.ons.gov.uk/ (accessed on 5 March 2021).
- Cases in United Kingdom (Whole Pandemic). Coronavirus (COVID-19) in the UK. Available online: https://coronavirus.data.gov.uk/details/cases (accessed on 5 March 2021).
- Neal, R.D.; Nekhlyudov, L.; Wheatstone, P.; Koczwara, B. Cancer care during and after the pandemic. BMJ 2020, 370, m2622. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Neal, R.D.; Duffy, S.R.G.; Scott, S.E.; Whitaker, K.L.; Brain, K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: The view from primary care. Lancet Oncol. 2020, 21, 748–750. [Google Scholar] [CrossRef]
- NHS Digital. Health Survey for England-2004, Health of Ethnic Minorities, Main Report. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2004-health-of-ethnic-minorities-main-report (accessed on 7 November 2020).
- Hughes, A.; Kumari, M.; McMunn, A.; Bartley, M. Unemployment and inflammatory markers in England, Wales and Scotland, 1998-2012: Meta-analysis of results from 12 studies. Brain Behav. Immun. 2017, 64, 91–102. [Google Scholar] [CrossRef]
- Jose, R.J.; Manuel, A. COVID-19 cytokine storm: The interplay between inflammation and coagulation. Lancet Respir. Med. 2020, 8, e46–e47. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Churilla, T.M.; Egleston, B.L.; Fisher, S.G.; Ridge, J.A.; Horwitz, E.M.; Meyer, J.E. Causes of death among cancer patients. Ann. Oncol. 2017, 28, 400–407. [Google Scholar] [CrossRef]
- Shree, T.; Li, Q.; Glaser, S.L.; Brunson, A.; Maecker, H.T.; Haile, R.W.; Levy, R.; Keegan, T.H.M. Impaired Immune Health in Survivors of Diffuse Large B-Cell Lymphoma. J. Clin. Oncol. 2020, 38, 1664–1675. [Google Scholar] [CrossRef] [PubMed]
- Nazroo, J.; Becares, L. Evidence for ethnic inequalities in mortality related to COVID-19 infections: Findings from an ecological analysis of England and Wales. medRxiv 2020. [Google Scholar] [CrossRef]
- Office for National Statistics. Coronavirus (COVID-19) Related Deaths by Occupation, England and Wales: Deaths Registered between 9 March and 25 May 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregisteredbetween9marchand25may2020 (accessed on 7 November 2020).
- The Developer. England’s Sites Stayed open during Lockdown and Hundreds of Construction Workers Died. Available online: https://www.thedeveloper.live/places/places/englands-sites-stayed-open-during-lockdown-and-hundreds-of-construction-workers-died (accessed on 20 November 2020).
- Office for National Statistics. Coronavirus (COVID-19) Related Deaths by Occupation, England and Wales: Deaths Registered up to and Including 20 April 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregistereduptoandincluding20april2020 (accessed on 20 November 2020).
- Guardian. Oldham Takes Measures to Avoid Full Coronavirus Lockdown. Available online: https://www.theguardian.com/uk-news/2020/jul/28/oldham-greater-manchester-takes-measures-to-avoid-full-coronavirus-covid-19-lockdown (accessed on 20 November 2020).
- Haroon, S.; Chandan, J.S.; Middleton, J.; Cheng, K.K. Covid-19: Breaking the chain of household transmission. BMJ 2020, 370, m3181. [Google Scholar] [CrossRef] [PubMed]
- Barlow, W.E.; Ichikawa, L.; Rosner, D.; Izumi, S. Analysis of Case-Cohort Designs. J. Clin. Epidemiol. 1999, 52, 1165–1172. [Google Scholar] [CrossRef]
- McNutt, L.-A.; Wu, C.; Xue, X.; Hafner, J.P. Estimating the Relative Risk in Cohort Studies and Clinical Trials of Common Outcomes. Am. J. Epidemiol. 2003, 157, 940–943. [Google Scholar] [CrossRef] [PubMed]
- Fry, A.; Littlejohns, T.J.; Sudlow, C.; Doherty, N.; Adamska, L.; Sprosen, T.; Collins, R.; Allen, N.E. Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants With Those of the General Population. Am. J. Epidemiol. 2017, 186, 1026–1034. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Coomes, E.A.; Aldhaheri, K.; Alrawi, S. Serial Screening for COVID-19 in Asymptomatic Patients Receiving Anticancer Therapy in the United Arab Emirates. JAMA Oncol. 2021, 7, 129–131. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Tested Positive (Cases) N (%) | Entire Cohort (Controls) N (%) | p-Values |
|---|---|---|---|
| Age, years | 0.177 * | ||
| Median (interquartile range) | 74 (68–78) | 73 (67–77) | |
| Quintiles of Deprivation | 0.013 | ||
| 1st quintile (most affluent) | 8 (9.0) | 3604 (19.1) | |
| 2nd quintile | 16 (18.0) | 3682 (19.5) | |
| 3rd quintile | 18 (20.2) | 3659 (19.3) | |
| 4th quintile | 15 (16.9) | 3863 (20.4) | |
| 5th quintile (most deprived) | 31 (34.8) | 4090 (21.6) | |
| Sex | 0.518 | ||
| Female | 42 (47.2) | 9577 50.6) | |
| Male | 47 (52.8) | 9340 (49.4) | |
| Ethnicity | 0.031 | ||
| White | 81 (91.0) | 18,075 (95.6) | |
| Asian | 2 (2.3) | 284 (1.5) | |
| Black | 4 (4.5) | 234 (1.2) | |
| Others | 2 (2.3) | 220 (1.2) | |
| Marital status | 0.726 | ||
| With a partner | 68 (76.4) | 14,048 (74.3) | |
| Without a partner | 5 (5.6) | 1215 (6.4) | |
| Employment | 0.031 | ||
| Employed or self-employed | 33 (37.1) | 9240 (48.8) | |
| Retired | 42 (47.2) | 8197 (43.3) | |
| Unemployed/unpaid | 11 (12.4) | 1283 (6.8) | |
| Smoking status | 0.022 | ||
| Current smoker | 12 (13.5) | 1767 (9.3) | |
| Ex-smoker | 43 (48.3) | 7251 (38.3) | |
| Non-smoker | 33 (37.1) | 9772 (51.7) | |
| BMI (kg/m2) | 0.001 * | ||
| Median (interquartile range) | 28.6 (26.1–31.9) | 27.0 (24.5–30.1) | |
| Categorical BMI | 0.026 | ||
| <18.5 | 0 (0.0) | 64 (0.3) | |
| 18.5–24.9 | 16 (18.0) | 5557 (29.4) | |
| 25.0–29.9 | 38 (42.7) | 8412 (44.5) | |
| ≥30 | 33 (37.1) | 4795 (25.4) | |
| Malignancy types | 0.069 | ||
| Haematological cancers | 12 (0.8) | 1518 (99.2) | |
| Non-haematological cancers | 74 (0.5) | 15,975 (99.5) | |
| Skin melanoma and others | 3 (0.2) | 1424 (99.8) | |
| Years of cancer diagnosis | 0.052 | ||
| Within 5 years of diagnosis | 21 (23.6) | 3027 (16.0) | |
| Beyond 5 years of diagnosis | 68 (76.4) | 15,883 (84.0) | |
| Total numbers | 89 (0.5) | 18,917 (100.0) | |
| Missing values | |||
| Quintiles of deprivation | 1 (1.1) | 19 (0.1) | |
| Ethnicity | 0 (0.0) | 104 (0.6) | |
| Marital status | 16 (18.0) | 3654 (19.3) | |
| Employment | 3 (3.4) | 197 (1.0) | |
| Smoking | 1 (1.1) | 127 (0.7) | |
| BMI | 2 (2.2) | 89 (0.5) | |
| Years of cancer diagnosis | 0 (0.0) | 7 (0.0) |
| Characteristics | Crude RR (95% CI) | p-Value |
|---|---|---|
| Age | ||
| per ten-year increase | 1.17 (0.83–1.64) | 0.353 |
| Sex | ||
| Male vs. Female | 1.15 (0.76–1.74) | 0.518 |
| Ethnicity | ||
| Asian vs. White | 1.57 (0.39–6.34) | 0.529 |
| Black vs. White | 3.77 (1.39–10.20) | 0.009 |
| Others vs. White | 2.02 (0.50–8.16) | 0.324 |
| Marital status | ||
| With a partner vs. Without partner | 1.18 (0.47–2.91) | 0.727 |
| Quintiles of Townsend deprivation index | ||
| 2nd quintile vs. 1st quintile | 1.95 (0.84–4.56) | 0.121 |
| 3rd quintile vs. 1st quintile | 2.21 (0.96–5.08) | 0.062 |
| 4th quintile vs. 1st quintile | 1.75 (0.74–4.11) | 0.202 |
| 5th quintile vs. 1st quintile | 3.40 (1.56–7.38) | 0.002 |
| Employment status | ||
| Retired vs. employed | 1.43 (0.91–2.26) | 0.122 |
| Unemployed/unpaid vs. employed | 2.39 (1.21–4.71) | 0.012 |
| Smoking status | ||
| Current smoker vs. non-smoker | 2.00 (1.04–3.87) | 0.039 |
| Ex-smoker vs. non-smoker | 1.75 (1.11–2.75) | 0.015 |
| BMI | ||
| (per five kg/m2 increase) | 1.30 (1.08–1.56) | 0.006 |
| Categorical BMI in kg/m2 | ||
| Obesity (≥30) vs. Normal/overweight (<30) | 1.78 (1.16–2.75) | 0.009 |
| Malignancy types | ||
| Hematological cancer vs. Skin melanoma/others | 3.73 (1.05–13.19) | 0.041 |
| Non-hematological cancer vs. Skin melanoma/others | 2.19 (0.69–6.95) | 0.182 |
| Years of cancer diagnosis | ||
| Within 5 years vs. Beyond 5 years of diagnosis | 1.62 (0.99–2.63) | 0.054 |
| Variables | Model 1 aRR (95% CI) | Model 2 aRR (95% CI) | Model 3 aRR (95% CI) | Model 4 aRR (95% CI) | Model 5 aRR (95% CI) | Model 6 aRR (95% CI) | Model 7 aRR (95% CI) | * Model 8 aRR (95% CI) | Model 9 aRR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Townsend Deprivation Index | |||||||||
| 2nd vs. 1st | 1.96 (0.84–4.58) | 1.96 (0.84–4.58) | 1.84 (0.78–4.34) | 1.81 (0.77–4.28) | 1.79 (0.76–4.23) | 1.80 (0.76–4.25) | 1.79 (0.76–4.24) | 2.09 (0.85–5.13) | 1.90 (0.82–4.46) |
| 3rd vs. 1st | 2.22 (0.97–5.11) | 2.21 (0.96–5.09) | 2.21 (0.96–5.08) | 2.18 (0.95–5.01) | 2.01 (0.86–4.68) | 2.02 (0.87–4.69) | 2.00 (0.86–4.65) | 2.02 (0.81–5.04) | 1.98 (0.85–4.61) |
| 4th vs. 1st | 1.78 (0.75–4.19) | 1.74 (0.74–4.07) | 1.74 (0.74–4.07) | 1.56 (0.65–3.72) | 1.49 (0.63–3.54) | 1.49 (0.63–3.53) | 1.49 (0.63–3.54) | 1.78 (0.72–4.42) | 1.60 (0.68–3.76) |
| 5th vs. 1st | 3.46 (1.59–7.53) | 3.20 (1.45–7.06) | 2.86 (1.27–6.41) | 2.69 (1.21–6.00) | 2.41 (1.05–5.55) | 2.38 (1.04–5.48) | 2.37 (1.03–5.44) | 2.52 (1.00–6.33) | 2.57 (1.13–5.85) |
| Sex | |||||||||
| male vs. female | 1.13 (0.74–1.74) | 1.11 (0.72–1.72) | 1.16 (0.74–1.83) | 1.12 (0.72–1.75) | 1.16 (0.73–1.85) | 1.16 (0.73–1.85) | 1.16 (0.73–1.83) | 1.20 (0.71–2.02) | 1.08 (0.69–1.70) |
| Age | |||||||||
| per ten-year increase | 1.17 (0.83–1.73) | 1.21 (0.86–1.70) | 1.15 (0.73–1.81) | 1.12 (0.70–1.80) | 1.10 (0.68–1.78) | 1.08 (0.67–1.76) | 1.10 (0.68–1.78) | 1.10 (0.66–1.84) | 1.12 (0.70–1.80) |
| Ethnicity | |||||||||
| Asian vs. White | 1.49 (0.36–6.04) | 0.74 (0.10–5.41) | 0.91 (0.12–6.61) | 0.97 (0.13–7.39) | 0.93 (0.12–7.09) | 0.94 (0.13–6.89) | 1.16 (0.14–9.31) | 1.64 (0.39–6.89) | |
| Black vs. White | 2.92 (0.99–8.67) | 2.97 (1.00–8.85) | 3.43 (1.21–9.77) | 3.52 (1.19–10.45) | 3.39 (1.14–10.07) | 3.41 (1.15–10.11) | 5.79 (1.88–17.85) | 3.44 (1.13–10.46) | |
| Others vs. White | 1.86 (0.47–7.30) | 1.80 (0.46–7.05) | 1.89 (0.46–7.82) | 2.00 (0.51–7.83) | 1.94 (0.50–7.58) | 1.91 (0.49–7.46) | 2.83 (0.73–10.91) | 1.80 (0.46–7.06) | |
| Employment status | |||||||||
| Retired vs. employed | 1.29 (0.74–2.24) | 1.32 (0.76–2.31) | 1.28 (0.72–2.26) | 1.28 (0.72–2.27) | 1.28 (0.72–2.26) | 1.39 (0.79–2.46) | 1.22 (0.69–2.14) | ||
| Unemployed/unpaid vs. employed | 2.09 (1.03–4.24) | 2.11 (1.04–4.29) | 2.01 (0.99–4.09) | 2.00 (0.98–4.07) | 1.99 (0.98–4.04) | 2.35 (1.06–5.20) | 2.07 (1.02–4.20) | ||
| Smoking status | |||||||||
| Current smoker vs. non-smoker | 1.44 (0.71–2.96) | 1.51 (0.74–3.06) | 1.49 (0.73–3.02) | 1.49 (0.73–3.04) | 1.30 (0.54–3.16) | 1.77 (0.91–3.44) | |||
| Ex-smoker vs. non-smoker | 1.69 (1.07–2.68) | 1.57 (0.99–2.50) | 1.56 (0.98–2.49) | 1.56 (0.98–2.49) | 1.53 (0.93–2.52) | 1.56 (0.98–2.47) | |||
| BMI | |||||||||
| Per 5 kg/m2 increase | 1.28 (1.08–1.52) | 1.29 (1.09–1.52) | 1.28 (1.08–1.51) | 1.41 (1.20–1.67) | 1.27 (1.08–1.50) | ||||
| Malignancy type | |||||||||
| Haematological vs. skin melanoma and ** others | 4.21 (0.92–19.33) | 4.18 (0.91–19.18) | 3.94 (0.84–18.38) | 4.30 (0.94–19.70) | |||||
| Non-haematological vs. skin melanoma and ** others | 2.74 (0.67–11.22) | 2.74 (0.67–11.19) | 2.31 (0.56–9.53) | 2.80 (0.69–11.46) | |||||
| Years of cancer diagnosis | |||||||||
| Within 5 years vs. beyond 5 years of diagnosis | 1.55 (0.93–2.58) | 1.44 (0.81–2.56) | 1.67 (1.02–2.73) | ||||||
| Marital status | |||||||||
| With a partner vs. without a partner | 2.36 (0.66–8.35) | 1.36 (0.52–3.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.F.; Nikšić, M.; Rachet, B.; Sanchez, M.-J.; Luque-Fernandez, M.A. Socioeconomic Inequalities and Ethnicity Are Associated with a Positive COVID-19 Test among Cancer Patients in the UK Biobank Cohort. Cancers 2021, 13, 1514. https://doi.org/10.3390/cancers13071514
Lee SF, Nikšić M, Rachet B, Sanchez M-J, Luque-Fernandez MA. Socioeconomic Inequalities and Ethnicity Are Associated with a Positive COVID-19 Test among Cancer Patients in the UK Biobank Cohort. Cancers. 2021; 13(7):1514. https://doi.org/10.3390/cancers13071514
Chicago/Turabian StyleLee, Shing Fung, Maja Nikšić, Bernard Rachet, Maria-Jose Sanchez, and Miguel Angel Luque-Fernandez. 2021. "Socioeconomic Inequalities and Ethnicity Are Associated with a Positive COVID-19 Test among Cancer Patients in the UK Biobank Cohort" Cancers 13, no. 7: 1514. https://doi.org/10.3390/cancers13071514






