Octreotide and Pasireotide Combination Treatment in Somatotroph Tumor Cells: Predominant Role of SST2 in Mediating Ligand Effects
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Patients and Tumors
2.3. Immunohistochemistry (IHC)
2.4. Cell Cultures
2.4.1. Primary Cell Cultures of Somatotroph Tumors
2.4.2. GH4C1 Cell Line
2.5. In Vitro GH Secretion
2.6. Cell Proliferation
2.7. Quantification of cAMP Levels
2.8. Intracellular [Ca2+] Measurement
2.9. Immunocytofluorescence (IF)
2.10. RNA Isolation and Quantitative Real Time (qRT)-PCR
2.11. Western Blotting
2.12. Combination Index Calculation
2.13. Statistical Analysis
3. Results
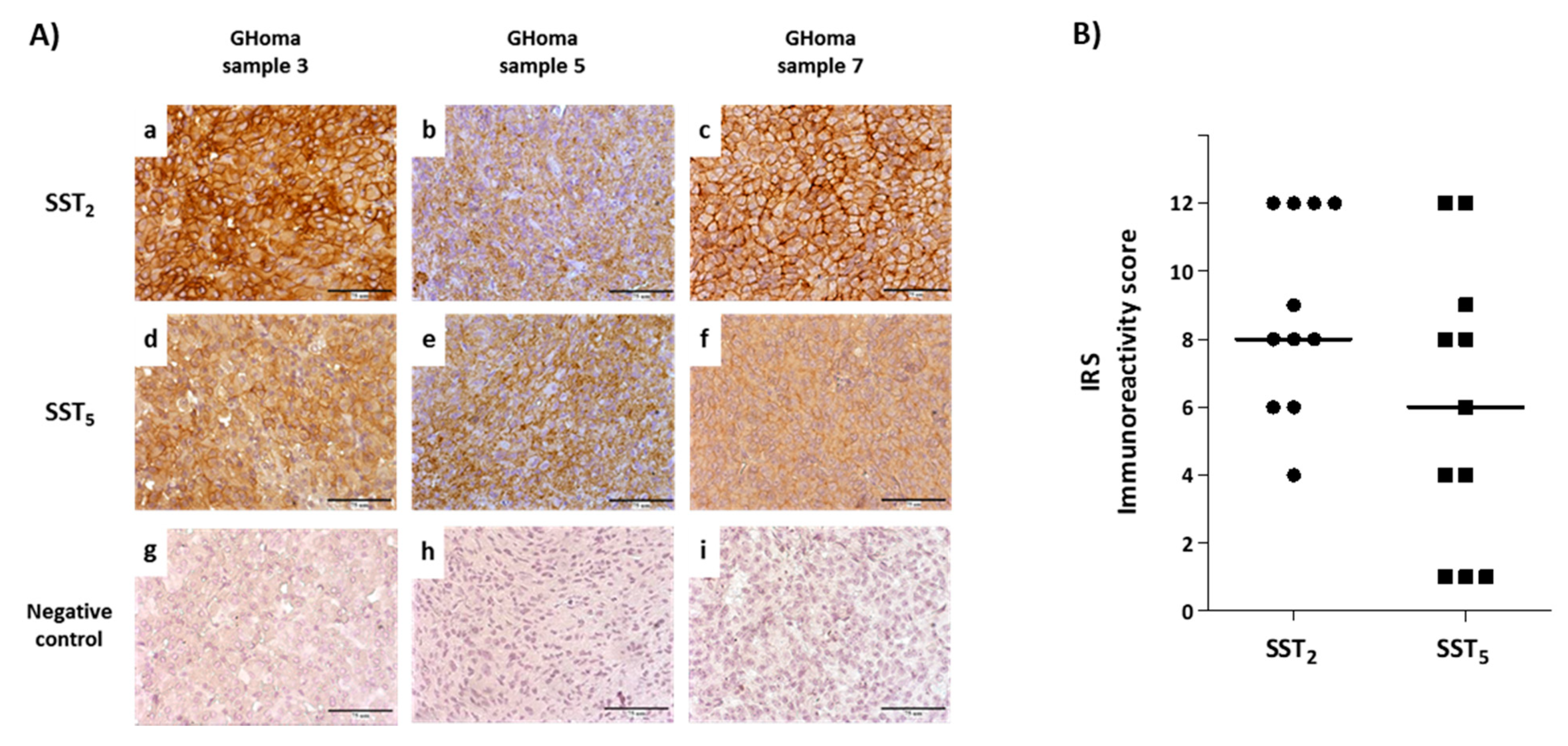
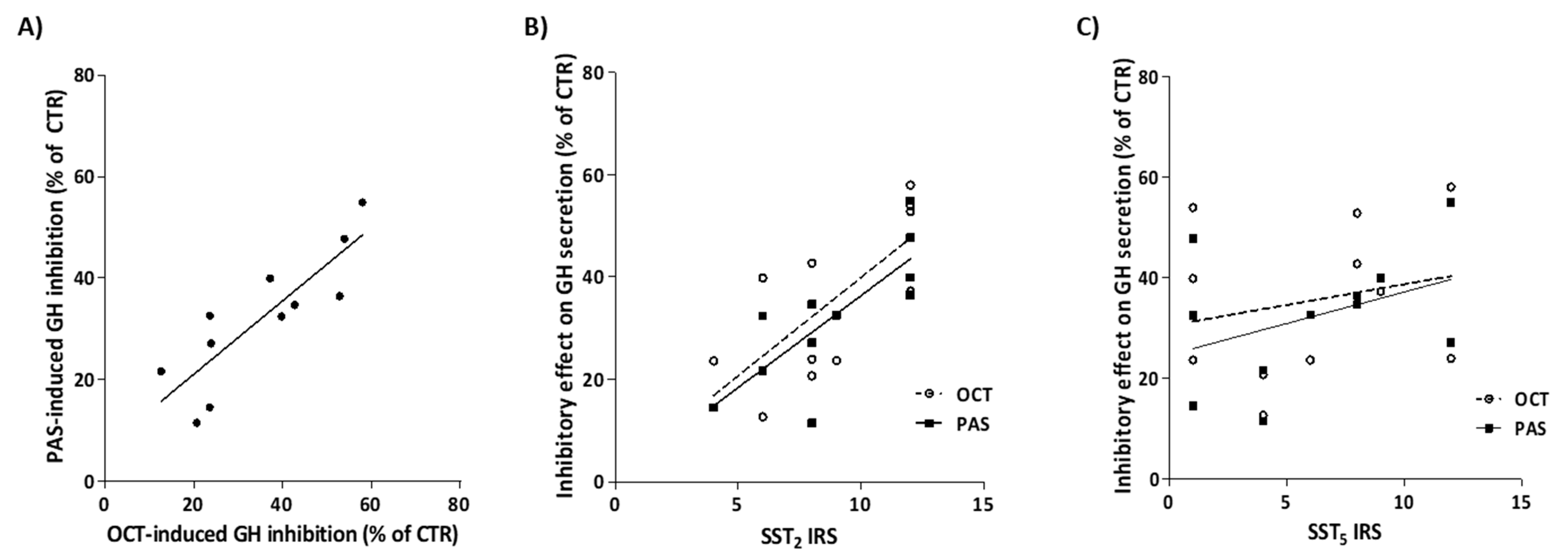
3.1. SST Protein Expression in Pituitary Tumor Samples
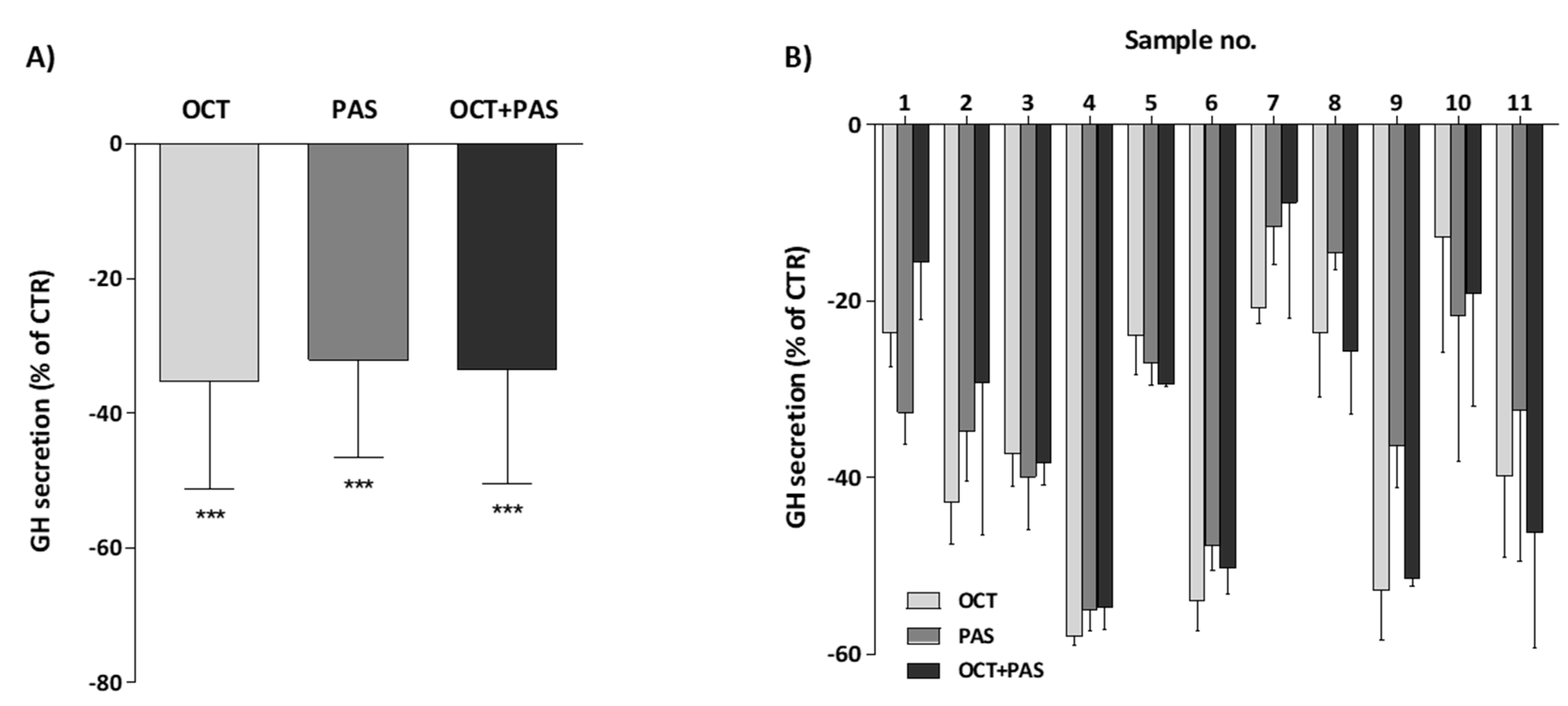
3.2. Effect of OCT and PAS on GH Secretion in Human Somatotroph Cells
3.3. SST mRNA and Protein Expression in GH4C1 Cells
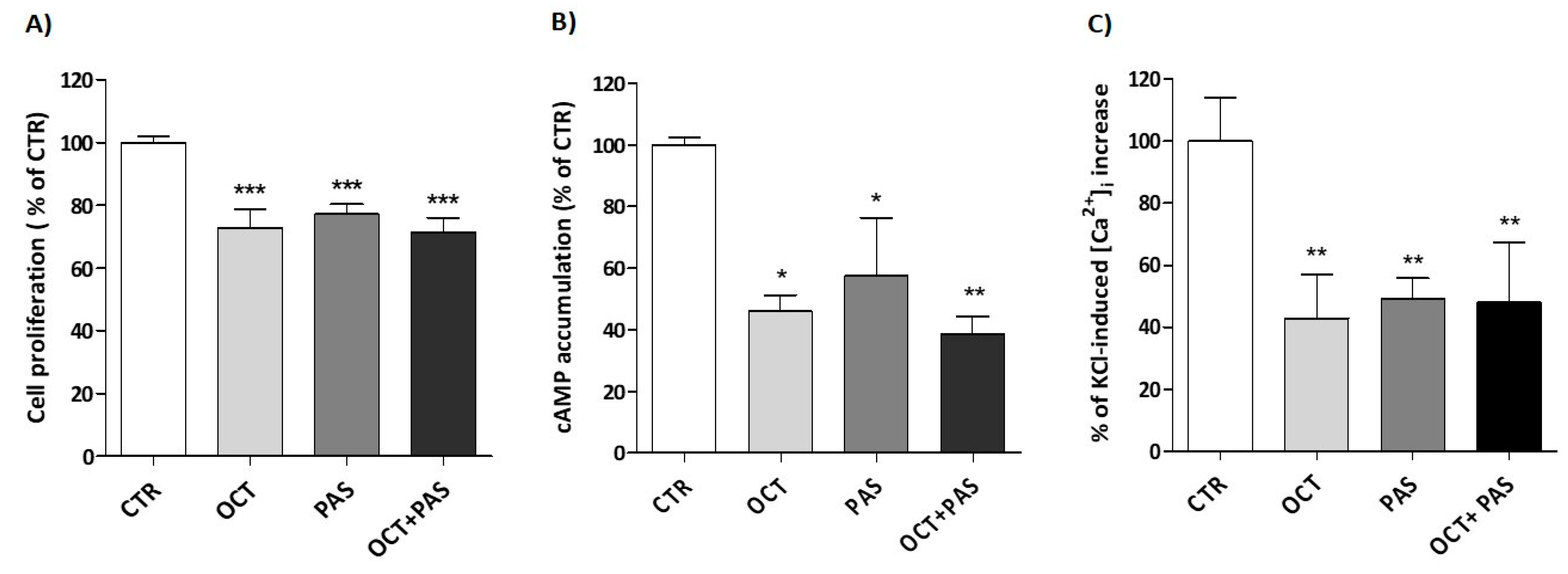
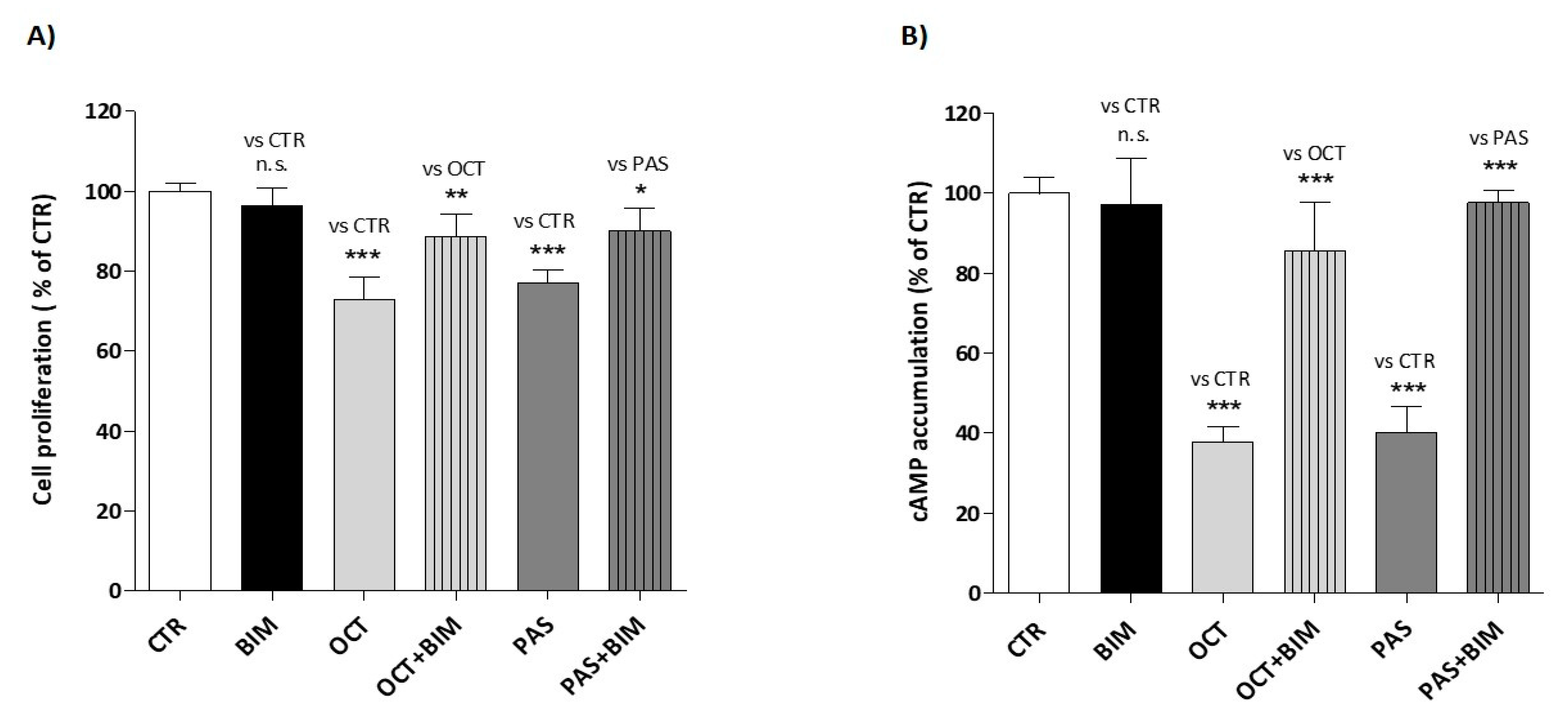
3.4. Inhibitory Effect of SRLs on Cell Proliferation, cAMP and Ca2+ Levels in GH4C1 Cells
3.5. Effect of BIM-23627 on SRL-Induced Inhibition of Cell Proliferation and cAMP Accumulation in GH4C1 Cells
3.6. OCT- and PAS-Induced Internalization of SST2 and SST5 in GH4C1 Cells
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melmed, S. Pituitary-Tumor Endocrinopathies. N. Engl. J. Med. 2020, 382, 937–950. [Google Scholar] [CrossRef]
- Gunther, T.; Tulipano, G.; Dournaud, P.; Bousquet, C.; Csaba, Z.; Kreienkamp, H.J.; Lupp, A.; Korbonits, M.; Castano, J.P.; Wester, H.J.; et al. International Union of Basic and Clinical Pharmacology. CV. Somatostatin Receptors: Structure, Function, Ligands, and New Nomenclature. Pharmacol. Rev. 2018, 70, 763–835. [Google Scholar] [CrossRef]
- Campana, C.; Cocchiara, F.; Corica, G.; Nista, F.; Arvigo, M.; Amaru, J.; Rossi, D.C.; Zona, G.; Ferone, D.; Gatto, F. Discordant GH and IGF-1 results in treated acromegaly: Impact of GH cut-offs and mean values assessment. J. Clin. Endocrinol. Metab. 2020. [Google Scholar] [CrossRef]
- Katznelson, L.; Laws, E.R., Jr.; Melmed, S.; Molitch, M.E.; Murad, M.H.; Utz, A.; Wass, J.A.; Endocrine, S. Acromegaly: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014, 99, 3933–3951. [Google Scholar] [CrossRef]
- Giustina, A.; Chanson, P.; Kleinberg, D.; Bronstein, M.D.; Clemmons, D.R.; Klibanski, A.; van der Lely, A.J.; Strasburger, C.J.; Lamberts, S.W.; Ho, K.K.; et al. Expert consensus document: A consensus on the medical treatment of acromegaly. Nat. Rev. Endocrinol. 2014, 10, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Corica, G.; Ceraudo, M.; Campana, C.; Nista, F.; Cocchiara, F.; Boschetti, M.; Zona, G.; Criminelli, D.; Ferone, D.; Gatto, F. Octreotide-Resistant Acromegaly: Challenges and Solutions. Ther. Clin. Risk Manag. 2020, 16, 379–391. [Google Scholar] [CrossRef]
- Gatto, F.; Barbieri, F.; Arvigo, M.; Thellung, S.; Amaru, J.; Albertelli, M.; Ferone, D.; Florio, T. Biological and Biochemical Basis of the Differential Efficacy of First and Second Generation Somatostatin Receptor Ligands in Neuroendocrine Neoplasms. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, A.; Melmed, S. Somatostatin agonists for treatment of acromegaly. Mol. Cell Endocrinol. 2008, 286, 192–198. [Google Scholar] [CrossRef]
- Jaquet, P.; Saveanu, A.; Gunz, G.; Fina, F.; Zamora, A.J.; Grino, M.; Culler, M.D.; Moreau, J.P.; Enjalbert, A.; Ouafik, L.H. Human somatostatin receptor subtypes in acromegaly: Distinct patterns of messenger ribonucleic acid expression and hormone suppression identify different tumoral phenotypes. J. Clin. Endocrinol. Metab. 2000, 85, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Hofland, L.J.; van der Hoek, J.; van Koetsveld, P.M.; de Herder, W.W.; Waaijers, M.; Sprij-Mooij, D.; Bruns, C.; Weckbecker, G.; Feelders, R.; van der Lely, A.J.; et al. The novel somatostatin analog SOM230 is a potent inhibitor of hormone release by growth hormone- and prolactin-secreting pituitary adenomas in vitro. J. Clin. Endocrinol. Metab. 2004, 89, 1577–1585. [Google Scholar] [CrossRef]
- Taboada, G.F.; Luque, R.M.; Neto, L.V.; Machado Ede, O.; Sbaffi, B.C.; Domingues, R.C.; Marcondes, J.B.; Chimelli, L.M.; Fontes, R.; Niemeyer, P.; et al. Quantitative analysis of somatostatin receptor subtypes (1–5) gene expression levels in somatotropinomas and correlation to in vivo hormonal and tumor volume responses to treatment with octreotide LAR. Eur. J. Endocrinol. 2008, 158, 295–303. [Google Scholar] [CrossRef]
- Plockinger, U.; Albrecht, S.; Mawrin, C.; Saeger, W.; Buchfelder, M.; Petersenn, S.; Schulz, S. Selective loss of somatostatin receptor 2 in octreotide-resistant growth hormone-secreting adenomas. J. Clin. Endocrinol. Metab. 2008, 93, 1203–1210. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Feelders, R.A.; van der Pas, R.; Kros, J.M.; Waaijers, M.; Sprij-Mooij, D.; Neggers, S.J.; van der Lelij, A.J.; Minuto, F.; Lamberts, S.W.; et al. Immunoreactivity score using an anti-sst2A receptor monoclonal antibody strongly predicts the biochemical response to adjuvant treatment with somatostatin analogs in acromegaly. J. Clin. Endocrinol. Metab. 2013, 98, E66–E71. [Google Scholar] [CrossRef] [PubMed]
- Casar-Borota, O.; Heck, A.; Schulz, S.; Nesland, J.M.; Ramm-Pettersen, J.; Lekva, T.; Alafuzoff, I.; Bollerslev, J. Expression of SSTR2a, but not of SSTRs 1, 3, or 5 in somatotroph adenomas assessed by monoclonal antibodies was reduced by octreotide and correlated with the acute and long-term effects of octreotide. J. Clin. Endocrinol. Metab. 2013, 98, E1730–E1739. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, J.D.; Bonert, V.S.; Nuno, M.; Ly, D.; Melmed, S. Acromegaly clinical trial methodology impact on reported biochemical efficacy rates of somatostatin receptor ligand treatments: A meta-analysis. J. Clin. Endocrinol. Metab. 2014, 99, 1825–1833. [Google Scholar] [CrossRef]
- Bruns, C.; Lewis, I.; Briner, U.; Meno-Tetang, G.; Weckbecker, G. SOM230: A novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profile. Eur. J. Endocrinol. 2002, 146, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Colao, A.; Bronstein, M.D.; Freda, P.; Gu, F.; Shen, C.C.; Gadelha, M.; Fleseriu, M.; van der Lely, A.J.; Farrall, A.J.; Hermosillo Resendiz, K.; et al. Pasireotide versus octreotide in acromegaly: A head-to-head superiority study. J. Clin. Endocrinol. Metab. 2014, 99, 791–799. [Google Scholar] [CrossRef]
- Ibanez-Costa, A.; Rivero-Cortes, E.; Vazquez-Borrego, M.C.; Gahete, M.D.; Jimenez-Reina, L.; Venegas-Moreno, E.; de la Riva, A.; Arraez, M.A.; Gonzalez-Molero, I.; Schmid, H.A.; et al. Octreotide and pasireotide (dis)similarly inhibit pituitary tumor cells in vitro. J. Endocrinol. 2016, 231, 135–145. [Google Scholar] [CrossRef]
- Gatto, F.; Feelders, R.A.; Franck, S.E.; van Koetsveld, P.M.; Dogan, F.; Kros, J.M.; Neggers, S.; van der Lely, A.J.; Lamberts, S.W.J.; Ferone, D.; et al. In Vitro Head-to-Head Comparison Between Octreotide and Pasireotide in GH-Secreting Pituitary Adenomas. J. Clin. Endocrinol. Metab. 2017, 102, 2009–2018. [Google Scholar] [CrossRef]
- Muhammad, A.; Coopmans, E.C.; Gatto, F.; Franck, S.E.; Janssen, J.; van der Lely, A.J.; Hofland, L.J.; Neggers, S. Pasireotide Responsiveness in Acromegaly Is Mainly Driven by Somatostatin Receptor Subtype 2 Expression. J. Clin. Endocrinol. Metab. 2019, 104, 915–924. [Google Scholar] [CrossRef]
- Iacovazzo, D.; Carlsen, E.; Lugli, F.; Chiloiro, S.; Piacentini, S.; Bianchi, A.; Giampietro, A.; Mormando, M.; Clear, A.J.; Doglietto, F.; et al. Factors predicting pasireotide responsiveness in somatotroph pituitary adenomas resistant to first-generation somatostatin analogues: An immunohistochemical study. Eur. J. Endocrinol. 2016, 174, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Chiloiro, S.; Bima, C.; Tartaglione, T.; Giampietro, A.; Gessi, M.; Lauretti, L.; Anile, C.; Colosimo, C.; Rindi, G.; Pontecorvi, A.; et al. Pasireotide and Pegvisomant Combination Treatment in Acromegaly Resistant to Second-Line Therapies: A Longitudinal Study. J. Clin. Endocrinol. Metab. 2019, 104, 5478–5482. [Google Scholar] [CrossRef]
- Cescato, R.; Loesch, K.A.; Waser, B.; Macke, H.R.; Rivier, J.E.; Reubi, J.C.; Schonbrunn, A. Agonist-biased signaling at the sst2A receptor: The multi-somatostatin analogs KE108 and SOM230 activate and antagonize distinct signaling pathways. Mol. Endocrinol. 2010, 24, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Lesche, S.; Lehmann, D.; Nagel, F.; Schmid, H.A.; Schulz, S. Differential effects of octreotide and pasireotide on somatostatin receptor internalization and trafficking in vitro. J. Clin. Endocrinol. Metab. 2009, 94, 654–661. [Google Scholar] [CrossRef]
- Kao, Y.J.; Ghosh, M.; Schonbrunn, A. Ligand-dependent mechanisms of sst2A receptor trafficking: Role of site-specific phosphorylation and receptor activation in the actions of biased somatostatin agonists. Mol. Endocrinol. 2011, 25, 1040–1054. [Google Scholar] [CrossRef] [PubMed]
- Tashjian, A.H., Jr.; Yasumura, Y.; Levine, L.; Sato, G.H.; Parker, M.L. Establishment of clonal strains of rat pituitary tumor cells that secrete growth hormone. Endocrinology 1968, 82, 342–352. [Google Scholar] [CrossRef]
- Florio, T. Molecular mechanisms of the antiproliferative activity of somatostatin receptors (SSTRs) in neuroendocrine tumors. Front. Biosci. 2008, 13, 822–840. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rindi, G.; Wiedenmann, B. Neuroendocrine neoplasia of the gastrointestinal tract revisited: Towards precision medicine. Nat. Rev. Endocrinol. 2020, 16, 590–607. [Google Scholar] [CrossRef]
- Trouillas, J.; Roy, P.; Sturm, N.; Dantony, E.; Cortet-Rudelli, C.; Viennet, G.; Bonneville, J.F.; Assaker, R.; Auger, C.; Brue, T.; et al. A new prognostic clinicopathological classification of pituitary adenomas: A multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol. 2013, 126, 123–135. [Google Scholar] [CrossRef]
- Florio, T.; Casagrande, S.; Diana, F.; Bajetto, A.; Porcile, C.; Zona, G.; Thellung, S.; Arena, S.; Pattarozzi, A.; Corsaro, A.; et al. Chemokine stromal cell-derived factor 1alpha induces proliferation and growth hormone release in GH4C1 rat pituitary adenoma cell line through multiple intracellular signals. Mol. Pharmacol. 2006, 69, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, F.; Pattarozzi, A.; Gatti, M.; Porcile, C.; Bajetto, A.; Ferrari, A.; Culler, M.D.; Florio, T. Somatostatin receptors 1, 2, and 5 cooperate in the somatostatin inhibition of C6 glioma cell proliferation in vitro via a phosphotyrosine phosphatase-eta-dependent inhibition of extracellularly regulated kinase-1/2. Endocrinology 2008, 149, 4736–4746. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Florio, T.; Thellung, S.; Corsaro, A.; Bocca, L.; Arena, S.; Pattarozzi, A.; Villa, V.; Massa, A.; Diana, F.; Schettini, D.; et al. Characterization of the intracellular mechanisms mediating somatostatin and lanreotide inhibition of DNA synthesis and growth hormone release from dispersed human GH-secreting pituitary adenoma cells in vitro. Clin. Endocrinol. 2003, 59, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Gatti, M.; Solari, A.; Pattarozzi, A.; Campanella, C.; Thellung, S.; Maniscalco, L.; De Maria, R.; Wurth, R.; Corsaro, A.; Bajetto, A.; et al. In vitro and in vivo characterization of stem-like cells from canine osteosarcoma and assessment of drug sensitivity. Exp. Cell Res. 2018, 363, 48–64. [Google Scholar] [CrossRef]
- Wurth, R.; Barbieri, F.; Pattarozzi, A.; Gaudenzi, G.; Gatto, F.; Fiaschi, P.; Ravetti, J.L.; Zona, G.; Daga, A.; Persani, L.; et al. Phenotypical and Pharmacological Characterization of Stem-Like Cells in Human Pituitary Adenomas. Mol. Neurobiol. 2017, 54, 4879–4895. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsen, E.; Carlsson, C.; Tiensuu Janson, E.; Sandler, S.; Stridsberg, M. Somatostatin receptor 1–5; expression profiles during rat development. Ups J. Med. Sci. 2015, 120, 157–168. [Google Scholar] [CrossRef]
- Bajetto, A.; Pattarozzi, A.; Corsaro, A.; Barbieri, F.; Daga, A.; Bosio, A.; Gatti, M.; Pisaturo, V.; Sirito, R.; Florio, T. Different Effects of Human Umbilical Cord Mesenchymal Stem Cells on Glioblastoma Stem Cells by Direct Cell Interaction or Via Released Soluble Factors. Front. Cell Neurosci. 2017, 11, 312. [Google Scholar] [CrossRef]
- Ruscica, M.; Magni, P.; Steffani, L.; Gatto, F.; Albertelli, M.; Rametta, R.; Valenti, L.; Ameri, P.; Magnaghi, V.; Culler, M.D.; et al. Characterization and sub-cellular localization of SS1R, SS2R, and SS5R in human late-stage prostate cancer cells: Effect of mono- and bi-specific somatostatin analogs on cell growth. Mol. Cell Endocrinol. 2014, 382, 860–870. [Google Scholar] [CrossRef]
- Chou, T.C.; Talalay, P. Quantitative analysis of dose-effect relationships: The combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 1984, 22, 27–55. [Google Scholar] [CrossRef]
- Topaly, J.; Zeller, W.J.; Fruehauf, S. Synergistic activity of the new ABL-specific tyrosine kinase inhibitor STI571 and chemotherapeutic drugs on BCR-ABL-positive chronic myelogenous leukemia cells. Leukemia 2001, 15, 342–347. [Google Scholar] [CrossRef]
- Chou, T.C. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res. 2010, 70, 440–446. [Google Scholar] [CrossRef]
- Murray, R.D.; Kim, K.; Ren, S.G.; Lewis, I.; Weckbecker, G.; Bruns, C.; Melmed, S. The novel somatostatin ligand (SOM230) regulates human and rat anterior pituitary hormone secretion. J. Clin. Endocrinol. Metab. 2004, 89, 3027–3032. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ren, S.G.; Taylor, J.; Dong, J.; Yu, R.; Culler, M.D.; Melmed, S. Functional association of somatostatin receptor subtypes 2 and 5 in inhibiting human growth hormone secretion. J. Clin. Endocrinol. Metab. 2003, 88, 4239–4245. [Google Scholar] [CrossRef]
- Ben-Shlomo, A.; Schmid, H.; Wawrowsky, K.; Pichurin, O.; Hubina, E.; Chesnokova, V.; Liu, N.A.; Culler, M.; Melmed, S. Differential ligand-mediated pituitary somatostatin receptor subtype signaling: Implications for corticotroph tumor therapy. J. Clin. Endocrinol. Metab. 2009, 94, 4342–4350. [Google Scholar] [CrossRef] [PubMed]
- Schmid, H.A.; Brueggen, J. Effects of somatostatin analogs on glucose homeostasis in rats. J. Endocrinol. 2012, 212, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Kugita, M.; Nishii, K.; Yamaguchi, T.; Suzuki, A.; Yuzawa, Y.; Horie, S.; Higashihara, E.; Nagao, S. Beneficial effect of combined treatment with octreotide and pasireotide in PCK rats, an orthologous model of human autosomal recessive polycystic kidney disease. PLoS ONE 2017, 12, e0177934. [Google Scholar] [CrossRef] [PubMed]
- Cuny, T.; Zeiller, C.; Bidlingmaier, M.; Defilles, C.; Roche, C.; Blanchard, M.P.; Theodoropoulou, M.; Graillon, T.; Pertuit, M.; Figarella-Branger, D.; et al. In vitro impact of pegvisomant on growth hormone-secreting pituitary adenoma cells. Endocr. Relat. Cancer 2016, 23, 509–519. [Google Scholar] [CrossRef]
- Peverelli, E.; Giardino, E.; Mangili, F.; Treppiedi, D.; Catalano, R.; Ferrante, E.; Sala, E.; Locatelli, M.; Lania, A.G.; Arosio, M.; et al. cAMP/PKA-induced filamin A (FLNA) phosphorylation inhibits SST2 signal transduction in GH-secreting pituitary tumor cells. Cancer Lett. 2018, 435, 101–109. [Google Scholar] [CrossRef]
- Hubina, E.; Nanzer, A.M.; Hanson, M.R.; Ciccarelli, E.; Losa, M.; Gaia, D.; Papotti, M.; Terreni, M.R.; Khalaf, S.; Jordan, S.; et al. Somatostatin analogues stimulate p27 expression and inhibit the MAP kinase pathway in pituitary tumours. Eur. J. Endocrinol. 2006, 155, 371–379. [Google Scholar] [CrossRef]
- Peverelli, E.; Giardino, E.; Treppiedi, D.; Catalano, R.; Mangili, F.; Locatelli, M.; Lania, A.G.; Arosio, M.; Spada, A.; Mantovani, G. A novel pathway activated by somatostatin receptor type 2 (SST2): Inhibition of pituitary tumor cell migration and invasion through cytoskeleton protein recruitment. Int. J. Cancer 2018, 142, 1842–1852. [Google Scholar] [CrossRef]
- Tulipano, G.; Soldi, D.; Bagnasco, M.; Culler, M.D.; Taylor, J.E.; Cocchi, D.; Giustina, A. Characterization of new selective somatostatin receptor subtype-2 (sst2) antagonists, BIM-23627 and BIM-23454. Effects of BIM-23627 on GH release in anesthetized male rats after short-term high-dose dexamethasone treatment. Endocrinology 2002, 143, 1218–1224. [Google Scholar] [CrossRef] [PubMed]
- Zatelli, M.C.; Tagliati, F.; Taylor, J.E.; Rossi, R.; Culler, M.D.; degli Uberti, E.C. Somatostatin receptor subtypes 2 and 5 differentially affect proliferation in vitro of the human medullary thyroid carcinoma cell line tt. J. Clin. Endocrinol. Metab. 2001, 86, 2161–2169. [Google Scholar] [CrossRef]
- Ruscica, M.; Arvigo, M.; Gatto, F.; Dozio, E.; Feltrin, D.; Culler, M.D.; Minuto, F.; Motta, M.; Ferone, D.; Magni, P. Regulation of prostate cancer cell proliferation by somatostatin receptor activation. Mol. Cell Endocrinol. 2010, 315, 254–262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Poll, F.; Lehmann, D.; Illing, S.; Ginj, M.; Jacobs, S.; Lupp, A.; Stumm, R.; Schulz, S. Pasireotide and octreotide stimulate distinct patterns of sst2A somatostatin receptor phosphorylation. Mol. Endocrinol. 2010, 24, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Zatelli, M.C.; Piccin, D.; Vignali, C.; Tagliati, F.; Ambrosio, M.R.; Bondanelli, M.; Cimino, V.; Bianchi, A.; Schmid, H.A.; Scanarini, M.; et al. Pasireotide, a multiple somatostatin receptor subtypes ligand, reduces cell viability in non-functioning pituitary adenomas by inhibiting vascular endothelial growth factor secretion. Endocr. Relat. Cancer 2007, 14, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Zatelli, M.C.; Piccin, D.; Tagliati, F.; Ambrosio, M.R.; Margutti, A.; Padovani, R.; Scanarini, M.; Culler, M.D.; degli Uberti, E.C. Somatostatin receptor subtype 1 selective activation in human growth hormone (GH)- and prolactin (PRL)-secreting pituitary adenomas: Effects on cell viability, GH, and PRL secretion. J. Clin. Endocrinol. Metab. 2003, 88, 2797–2802. [Google Scholar] [CrossRef]
- Zatelli, M.C.; Piccin, D.; Bottoni, A.; Ambrosio, M.R.; Margutti, A.; Padovani, R.; Scanarini, M.; Taylor, J.E.; Culler, M.D.; Cavazzini, L.; et al. Evidence for differential effects of selective somatostatin receptor subtype agonists on alpha-subunit and chromogranin a secretion and on cell viability in human nonfunctioning pituitary adenomas in vitro. J. Clin. Endocrinol. Metab. 2004, 89, 5181–5188. [Google Scholar] [CrossRef]
- Theodoropoulou, M.; Stalla, G.K. Somatostatin receptors: From signaling to clinical practice. Front. Neuroendocrinol. 2013, 34, 228–252. [Google Scholar] [CrossRef]
- Vazquez-Borrego, M.C.; Gupta, V.; Ibanez-Costa, A.; Gahete, M.D.; Venegas-Moreno, E.; Toledano-Delgado, A.; Cano, D.A.; Blanco-Acevedo, C.; Ortega-Salas, R.; Japon, M.A.; et al. A Somatostatin Receptor Subtype-3 (SST3) Peptide Agonist Shows Antitumor Effects in Experimental Models of Nonfunctioning Pituitary Tumors. Clin. Cancer Res. 2020, 26, 957–969. [Google Scholar] [CrossRef]
- Florio, T.; Rim, C.; Hershberger, R.E.; Loda, M.; Stork, P.J. The somatostatin receptor SSTR1 is coupled to phosphotyrosine phosphatase activity in CHO-K1 cells. Mol. Endocrinol. 1994, 8, 1289–1297. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marques, P.; Barry, S.; Carlsen, E.; Collier, D.; Ronaldson, A.; Awad, S.; Dorward, N.; Grieve, J.; Mendoza, N.; Muquit, S.; et al. Pituitary tumour fibroblast-derived cytokines influence tumour aggressiveness. Endocr. Relat. Cancer 2019, 26, 853–865. [Google Scholar] [CrossRef]
- Florio, T.; Morini, M.; Villa, V.; Arena, S.; Corsaro, A.; Thellung, S.; Culler, M.D.; Pfeffer, U.; Noonan, D.M.; Schettini, G.; et al. Somatostatin inhibits tumor angiogenesis and growth via somatostatin receptor-3-mediated regulation of endothelial nitric oxide synthase and mitogen-activated protein kinase activities. Endocrinology 2003, 144, 1574–1584. [Google Scholar] [CrossRef]
- Cuevas-Ramos, D.; Fleseriu, M. Somatostatin receptor ligands and resistance to treatment in pituitary adenomas. J. Mol. Endocrinol. 2014, 52, R223–R240. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, A.; Melmed, S. Pituitary somatostatin receptor signaling. Trends Endocrinol. Metab. 2010, 21, 123–133. [Google Scholar] [CrossRef]
- Nagel, F.; Doll, C.; Poll, F.; Kliewer, A.; Schroder, H.; Schulz, S. Structural determinants of agonist-selective signaling at the sst(2A) somatostatin receptor. Mol. Endocrinol. 2011, 25, 859–866. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, Q.; Bee, M.S.; Schonbrunn, A. Site specificity of agonist and second messenger-activated kinases for somatostatin receptor subtype 2A (Sst2A) phosphorylation. Mol. Pharmacol. 2009, 76, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Arvigo, M.; Amaru, J.; Campana, C.; Cocchiara, F.; Graziani, G.; Bruzzone, E.; Giusti, M.; Boschetti, M.; Ferone, D. Cell specific interaction of pasireotide: Review of preclinical studies in somatotroph and corticotroph pituitary cells. Pituitary 2019, 22, 89–99. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | Tumor Characteristics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Sex, Age (Years) | GH (µg/L) | IGF-1 (µg/L) | IGF-1 (xULN) | Pre-SurgerySRLs | Tumor Size | Ki-67 | Mitoses (n/10 HPF) | p53 (+Nuclei/10 HPF) | Proliferation Index a | SST2 Protein (IRS) | SST5 Protein (IRS) |
| 1 | M, 54 | 2.7 | 454 | 2.02 | Yes | micro | <3% | 0/10 | 6/10 | 0 | 9 | 6 |
| 2 | F, 54 | 8.4 | 453 | 1.90 | Yes | macro | <3% | 0/10 | 2/10 | 0 | 8 | 8 |
| 3 | M, 49 | 10.9 | 394 | 1.53 | No | micro | <3% | 0/10 | 13/10 | 1 | 12 | 9 |
| 4 | M, 54 | 13.9 | 509 | 2.50 | No | macro | <3% | 1/10 | 0/10 | 0 | 12 | 12 |
| 5 | M, 39 | 62.0 | 989 | 4.10 | No | macro | <3% | 0/10 | 0/10 | 0 | 8 | 12 |
| 6 | F, 52 | 15.2 | 833 | 3.30 | No | macro | <3% | 0/10 | 5/10 | 0 | 12 | 1 |
| 7 | F, 21 | 51.1 | 858 | 2.30 | No | macro | <3% | 0/10 | 2/10 | 0 | 8 | 4 |
| 8 | M, 16 | 11.8 | 562 | 0.93 | Yes | macro | ≥3% | 3/10 | 13/10 | 3 | 4 | 1 |
| 9 | M, 50 | 8.0 | 469 | 1.89 | No | macro | <3% | 0/10 | 4/10 | 0 | 12 | 8 |
| 10 | M, 57 | 14.0 | 571 | 2.86 | No | macro | ≥3% | 8/10 | >10/10 | 3 | 6 | 4 |
| 11 | F, 39 | 7.9 | 436 | 1.80 | No | macro | <3% | 2/10 | 9/10 | 0 | 6 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amarù, J.; Barbieri, F.; Arvigo, M.; Solari, A.; Bajetto, A.; Nista, F.; Campana, C.; Gaggero, G.; Prior, A.; Criminelli Rossi, D.; et al. Octreotide and Pasireotide Combination Treatment in Somatotroph Tumor Cells: Predominant Role of SST2 in Mediating Ligand Effects. Cancers 2021, 13, 1816. https://doi.org/10.3390/cancers13081816
Amarù J, Barbieri F, Arvigo M, Solari A, Bajetto A, Nista F, Campana C, Gaggero G, Prior A, Criminelli Rossi D, et al. Octreotide and Pasireotide Combination Treatment in Somatotroph Tumor Cells: Predominant Role of SST2 in Mediating Ligand Effects. Cancers. 2021; 13(8):1816. https://doi.org/10.3390/cancers13081816
Chicago/Turabian StyleAmarù, Jessica, Federica Barbieri, Marica Arvigo, Agnese Solari, Adriana Bajetto, Federica Nista, Claudia Campana, Gabriele Gaggero, Alessandro Prior, Diego Criminelli Rossi, and et al. 2021. "Octreotide and Pasireotide Combination Treatment in Somatotroph Tumor Cells: Predominant Role of SST2 in Mediating Ligand Effects" Cancers 13, no. 8: 1816. https://doi.org/10.3390/cancers13081816
APA StyleAmarù, J., Barbieri, F., Arvigo, M., Solari, A., Bajetto, A., Nista, F., Campana, C., Gaggero, G., Prior, A., Criminelli Rossi, D., Zona, G., Ferone, D., Florio, T., & Gatto, F. (2021). Octreotide and Pasireotide Combination Treatment in Somatotroph Tumor Cells: Predominant Role of SST2 in Mediating Ligand Effects. Cancers, 13(8), 1816. https://doi.org/10.3390/cancers13081816







