Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More Than 10 Years Post-Diagnosis and in Comparison to a Control Cohort
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Data Source and Study Population
2.2. Health-Related Quality of Life Measurement
2.3. Statistical Analysis
3. Results
3.1. Longitudinal Analysis of HRQoL in Breast Cancer Survivors and Comparison with Controls
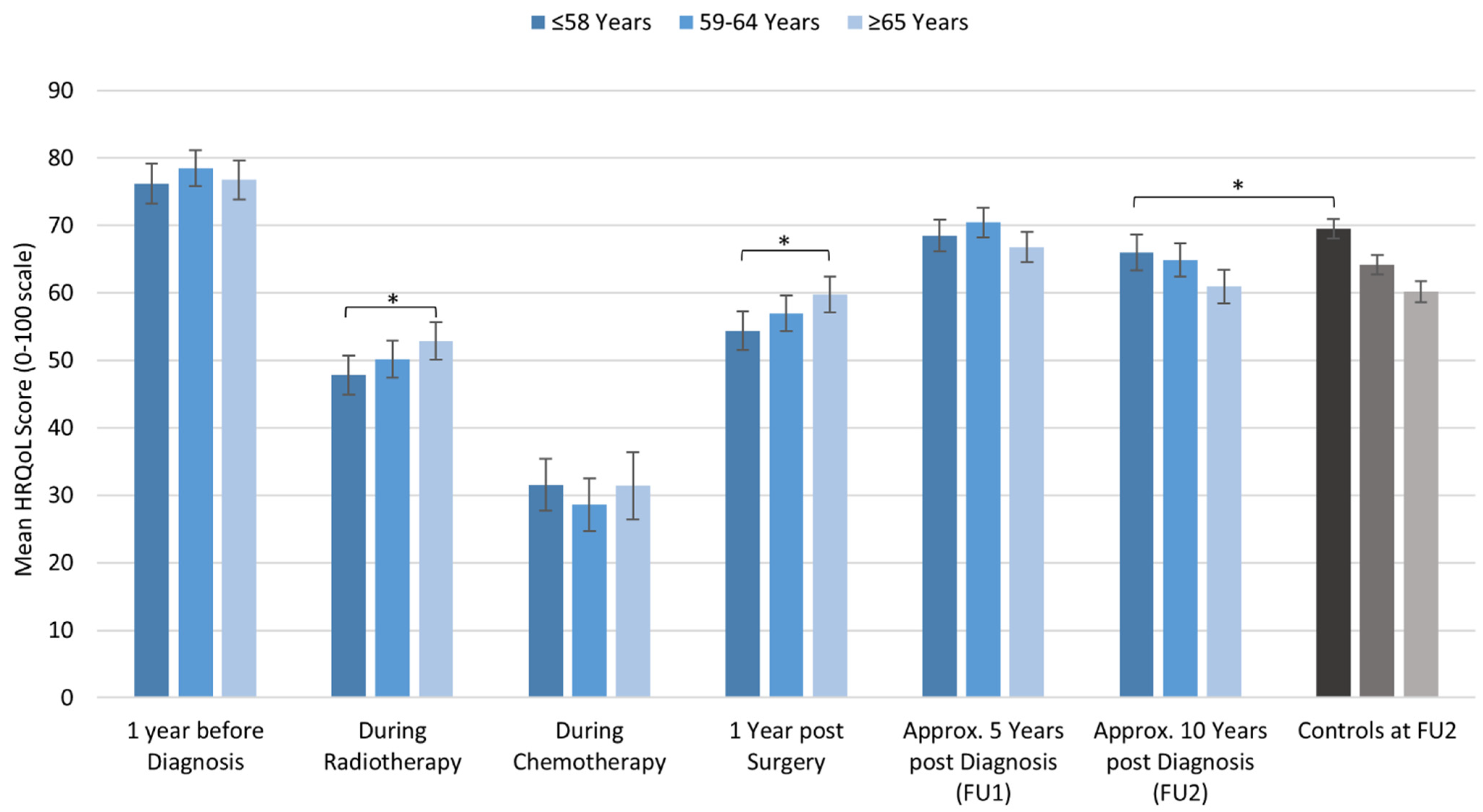
3.1.1. General HRQoL
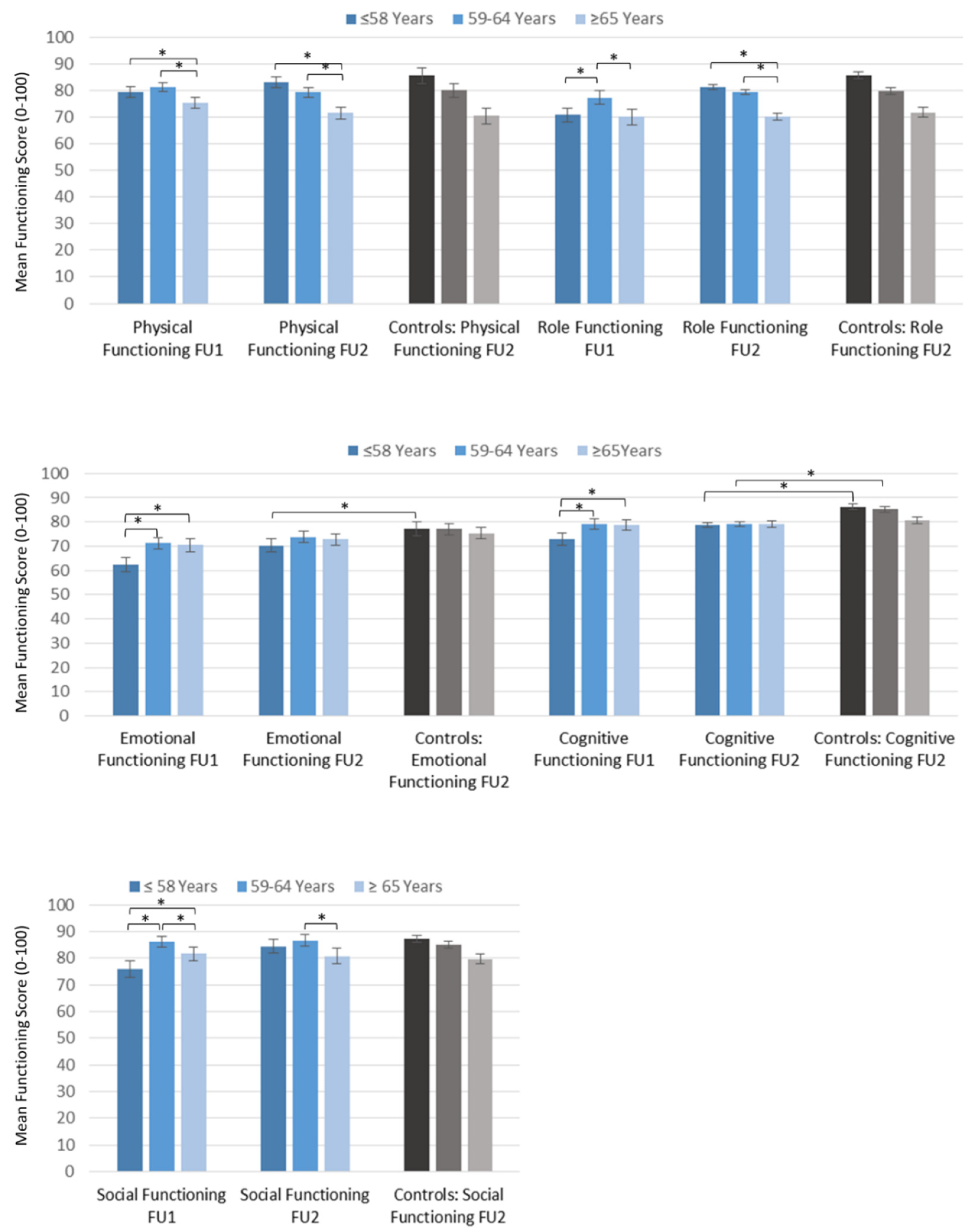
3.1.2. Cases’ Long-Term Course of Functioning Scales Stratified by Age and Compared to Healthy Controls
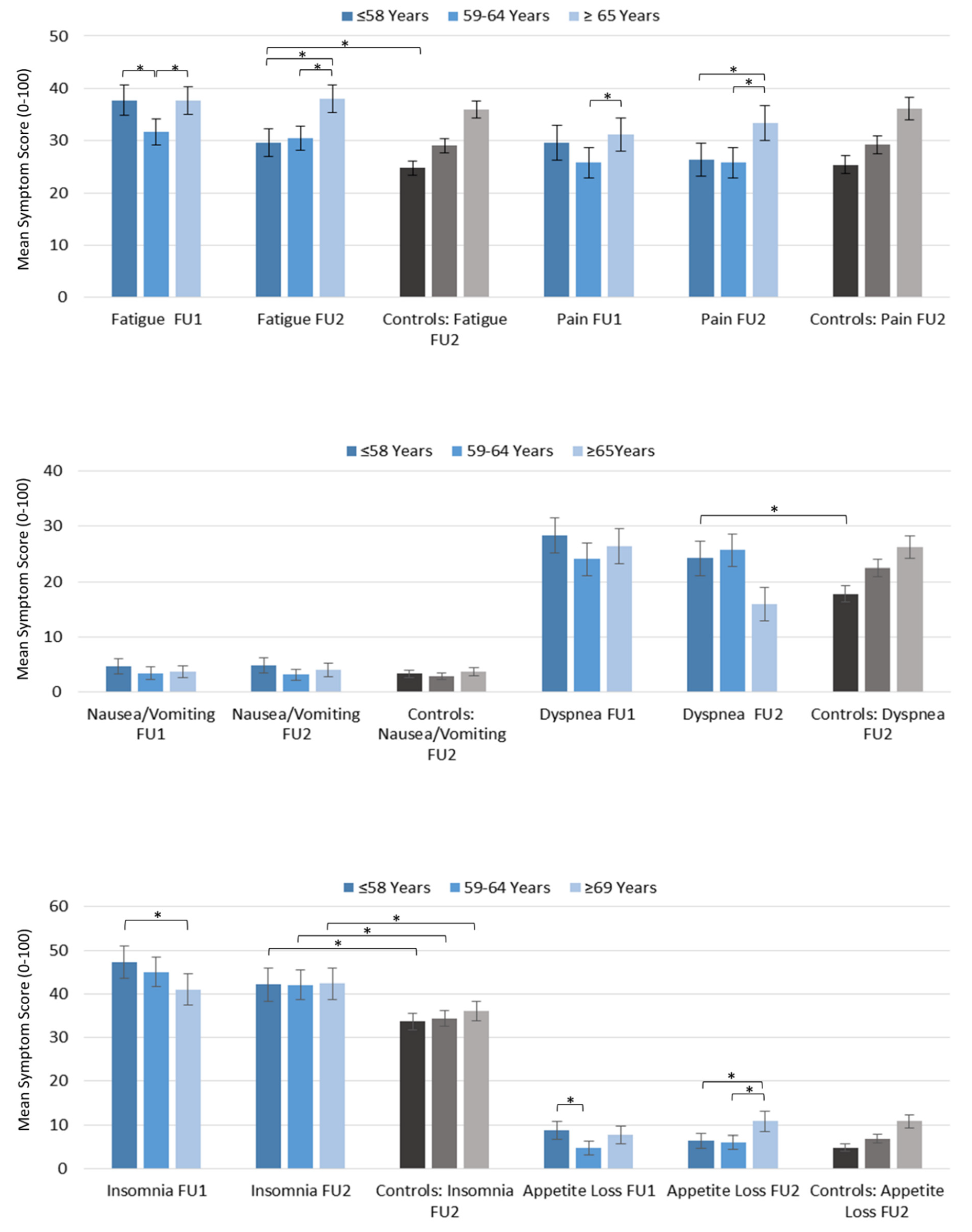
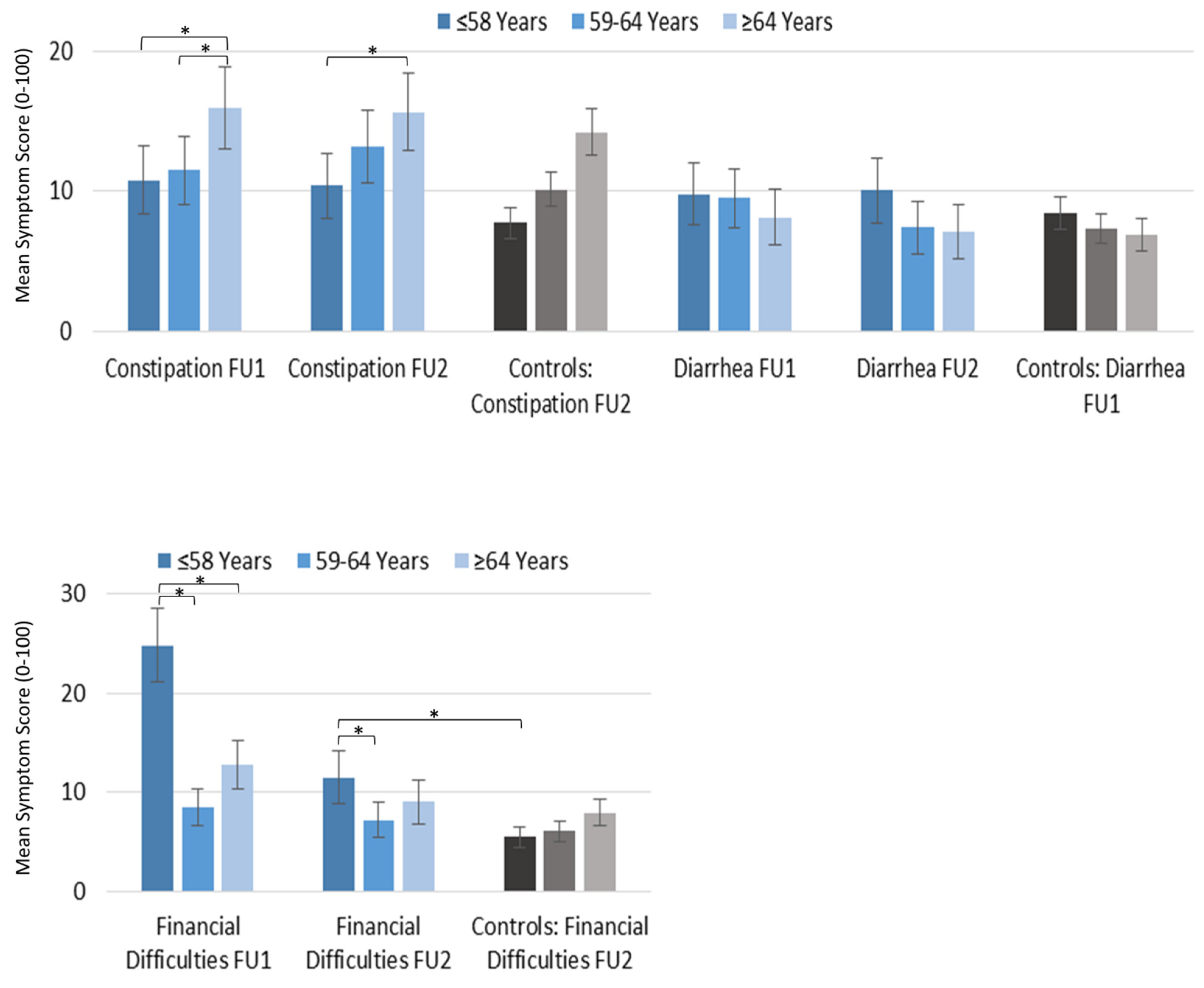
3.1.3. Survivors’ Long-Term Course of Symptom Scales Stratified by Age and Compared to Healthy Controls
4. Discussion
4.1. Longitudinal Development of HRQoL in Long-Term Breast Cancer Survivors
4.2. Long-Term HRQoL in Breast Cancer Survivors Compared to Healthy Controls
4.3. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robert Koch-Institut. Krebs in Deutschland 2015/2016. 2019. Available online: https://edoc.rki.de/handle/176904/6012 (accessed on 7 March 2021).
- Gesellschaft der Epidemiologischen Krebsregister in Deutschland e.V. Atlas der Krebsinzidenz und –mortalität in Deutschland (GEKID-Atlas). Datenlieferung: Oktober 2019, Lübeck, 2020. Available online: http://www.gekid.de (accessed on 7 March 2021).
- Quante, A.S.; Ming, C.; Rottmann, M.; Engel, J.; Boeck, S.; Heinemann, V.; Westphalen, C.B.; Strauch, K. Projections of cancer incidence and cancer-related deaths in Germany by 2020 and 2030. Cancer Med. 2016, 5, 2649–2656. [Google Scholar] [CrossRef]
- Khan, N.F.; Mant, D.; Carpenter, L.; Forman, D.; Rose, P.W. Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: A database study. Br. J. Cancer 2011, 105, S29–S37. [Google Scholar] [CrossRef]
- Leach, C.R.; Weaver, K.E.; Aziz, N.M.; Alfano, C.M.; Bellizzi, K.M.; Kent, E.E.; Forsythe, L.P.; Rowland, J.H. The complex health profile of long-term cancer survivors: Prevalence and predictors of comorbid conditions. J. Cancer Surviv. Res. Pract. 2014, 9, 239–251. [Google Scholar] [CrossRef]
- Wu, H.-S.; Harden, J.K. Symptom Burden and Quality of Life in Survivorship: A review of the literature. Cancer Nurs. 2015, 38, E29–E54. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; De Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality-of-Life Instrument for Use in International Clinical Trials in Oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, A.; Pritzkuleit, R.; Raspe, H.; Katalinic, A. The OVIS study: Health related quality of life measured by the EORTC QLQ-C30 and -BR23 in German female patients with breast cancer from Schleswig-Holstein. Qual. Life Res. 2007, 16, 767–776. [Google Scholar] [CrossRef]
- Arndt, V.; Merx, H.; Stürmer, T.; Stegmaier, C.; Ziegler, H.; Brenner, H. Age-specific detriments to quality of life among breast cancer patients one year after diagnosis. Eur. J. Cancer 2004, 40, 673–680. [Google Scholar] [CrossRef]
- Arndt, V.; Merx, H.; Stegmaier, C.; Ziegler, H.; Brenner, H. Restrictions in quality of life in colorectal cancer patients over three years after diagnosis: A population based study. Eur. J. Cancer 2006, 42, 1848–1857. [Google Scholar] [CrossRef] [PubMed]
- Bantemajoppe, E.J.; De Bock, G.H.; Iersel, M.W.-V.; Busz, D.M.; Ranchor, A.V.; Langendijk, J.A.; Maduro, J.H.; Heuvel, E.E.V.D. The impact of age on changes in quality of life among breast cancer survivors treated with breast-conserving surgery and radiotherapy. Br. J. Cancer 2015, 112, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.E.; Wiskemann, J.; Steindorf, K. Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual. Life Res. 2018, 27, 2077–2086. [Google Scholar] [CrossRef]
- Koch, L.; Jansen, L.; Herrmann, A.; Stegmaier, C.; Holleczek, B.; Singer, S.; Brenner, H.; Arndt, V. Quality of life in long-term breast cancer survivors—A 10-year longitudinal population-based study. Acta Oncol. 2012, 52, 1119–1128. [Google Scholar] [CrossRef]
- Doege, D.; Thong, M.S.-Y.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Pritzkuleit, R.; Waldeyer-Sauerland, M.; Waldmann, A.; Zeissig, S.R.; et al. Health-related quality of life in long-term disease-free breast cancer survivors versus female population controls in Germany. Breast Cancer Res. Treat. 2019, 175, 499–510. [Google Scholar] [CrossRef]
- Hsu, T.; Ennis, M.; Hood, N.; Graham, M.; Goodwin, P.J. Quality of Life in Long-Term Breast Cancer Survivors. J. Clin. Oncol. 2013, 31, 3540–3548. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L.; Wagner, L.I.; Monahan, P.O.; Daggy, J.; Smith, L.; Cohee, A.; Ziner, K.W.; Haase, J.E.; Miller, K.D.; Pradhan, K.; et al. Comparison of younger and older breast cancer survivors and age-matched controls on specific and overall quality of life domains. Cancer 2014, 120, 2237–2246. [Google Scholar] [CrossRef]
- Ganz, P.A.; Desmond, K.A.; Leedham, B.; Rowland, J.H.; Meyerowitz, B.E.; Belin, T.R. Quality of Life in Long-Term, Disease-Free Survivors of Breast Cancer: A Follow-up Study. J. Natl. Cancer Inst. 2002, 94, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Flesch-Janys, D.; Slanger, T.; Mutschelknauss, E.; Kropp, S.; Obi, N.; Vettorazzi, E.; Braendle, W.; Bastert, G.; Hentschel, S.; Berger, J.; et al. Risk of different histological types of postmenopausal breast cancer by type and regimen of menopausal hormone therapy. Int. J. Cancer 2008, 123, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Nolte, S.; Liegl, G.; Petersen, M.; Aaronson, N.; Costantini, A.; Fayers, P.; Groenvold, M.; Holzner, B.; Johnson, C.; Kemmler, G.; et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur. J. Cancer 2019, 107, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Cocks, K.; King, M.; Velikova, G.; De Castro, G.; St-James, M.M.; Fayers, P.; Brown, J. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur. J. Cancer 2012, 48, 1713–1721. [Google Scholar] [CrossRef]
- Schroevers, M.; Ranchor, A.V.; Sanderman, R. Adjustment to cancer in the 8 years following diagnosis: A longitudinal study comparing cancer survivors with healthy individuals. Soc. Sci. Med. 2006, 63, 598–610. [Google Scholar] [CrossRef]
- Sagen, Å.; Kåresen, R.; Sandvik, L.; Risberg, M.A. Changes in arm morbidities and health-related quality of life after breast cancer surgery—A five-year follow-up study. Acta Oncol. 2009, 48, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Mols, F.; Vingerhoets, A.J.; Coebergh, J.W.; Van De Poll-Franse, L.V. Quality of life among long-term breast cancer survivors: A systematic review. Eur. J. Cancer 2005, 41, 2613–2619. [Google Scholar] [CrossRef] [PubMed]
- Bloom, J.R.; Stewart, S.L.; Banks, P.J.; Shema, S.; Oakley-Girvan, I. Quality of life of younger breast cancer survivors: Persistence of problems and sense of well-being. Psycho-Oncology 2011, 21, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Bloom, J.R.; Stewart, S.L.; Chang, S.; Banks, P.J. Then and now: Quality of life of young breast cancer survivors. Psycho-Oncology 2004, 13, 147–160. [Google Scholar] [CrossRef]
- Howard-Anderson, J.; Ganz, P.A.; Bower, J.E.; Stanton, A.L. Quality of Life, Fertility Concerns, and Behavioral Health Outcomes in Younger Breast Cancer Survivors: A Systematic Review. J. Natl. Cancer Inst. 2012, 104, 386–405. [Google Scholar] [CrossRef] [PubMed]
- Morrow, P.K.; Broxson, A.C.; Munsell, M.F.; Basen-Enquist, K.; Rosenblum, C.K.; Schover, L.R.; Nguyen, L.H.; Hsu, L.; Castillo, L.; Hahn, K.M.; et al. Effect of Age and Race On Quality of Life in Young Breast Cancer Survivors. Clin. Breast Cancer 2014, 14, e21–e31. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arndt, V.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Pritzkuleit, R.; Waldeyer-Sauerland, M.; Waldmann, A.; Zeissig, S.R.; Doege, D.; et al. Return to work after cancer. A multi-regional population-based study from Germany. Acta Oncol. 2019, 58, 811–818. [Google Scholar] [CrossRef]
- Leysen, L.; LaHousse, A.; Nijs, J.; Adriaenssens, N.; Mairesse, O.; Ivakhnov, S.; Bilterys, T.; Van Looveren, E.; Pas, R.; Beckwée, D. Prevalence and risk factors of sleep disturbances in breast cancersurvivors: Systematic review and meta-analyses. Support. Care Cancer 2019, 27, 4401–4433. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, M.A.; E Schwartz, C. Integrating response shift into health-related quality of life research: A theoretical model. Soc. Sci. Med. 1999, 48, 1507–1515. [Google Scholar] [CrossRef]

| Controls | Cases (Full-Responders *) | Cases (Partial Responders *) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age at Diagnosis/Recruitment | ≤58 | 1165 | (33.7) | 350 | (31.2) | 114 | (23.7) |
| 59–64 | 1288 | (37.3) | 395 | (35.2) | 171 | (35.6) | |
| ≥65 | 1000 | (29.0) | 378 | (33.7) | 196 | (40.7) | |
| Stage (S) | 1 | 619 | (55.1) | 266 | (55.3) | ||
| 2a/2b | 447 | (39.8) | 191 | (39.7) | |||
| 3a | 57 | (5.1) | 24 | (5.0) | |||
| Grading (G) | Low | 253 | (22.5) | 138 | (28.7) | ||
| Moderate | 621 | (55.3) | 252 | (52.4) | |||
| High | 245 | (21.8) | 90 | (18.7) | |||
| Nodal Status (N) | 0 | 314 | (67.4) | 378 | (78.6) | ||
| 1–3 | 104 | (22.3) | 86 | (17.9) | |||
| 4–9 | 48 | (10.3) | 17 | (3.5) | |||
| Tumor Size (T) | <2 cm | 86 | (18.5) | 305 | (63.4) | ||
| 2–4 cm | 102 | (21.9) | 165 | (34.3) | |||
| ≥5 cm | 172 | (36.9) | 11 | (2.3) | |||
| Education Status | Low | 1749 | (50.7) | 625 | (55.7) | 280 | (58.2) |
| Medium | 1075 | (31.1) | 308 | (27.4) | 136 | (28.3) | |
| High | 629 | (18.2) | 190 | (16.9) | 65 | (13.5) | |
| BMI at Diagnosis/Recruitment | <22.5 | 815 | (23.6) | 260 | (23.2) | 109 | (22.7) |
| 22.5–<25 | 894 | (25.9) | 326 | (29.0) | 121 | (25.2) | |
| 25–<30 | 1190 | (34.5) | 393 | (35.0) | 178 | (37.0) | |
| ≥30 | 549 | (15.9) | 144 | (12.8) | 73 | (15.2) | |
| Smoking status | Non-smoker | 1803 | (52.2) | 607 | (54.1) | 247 | (51.4) |
| Ex-Smoker | 1098 | (31.8) | 340 | (30.3) | 124 | (25.8) | |
| Current-smoker | 552 | (16.0) | 176 | (15.7) | 110 | (22.9) | |
| Alcohol Intake per Day (gram) | 0 | 581 | (16.8) | 207 | (18.4) | 112 | (23.3) |
| >0–<19 | 2311 | (66.9) | 739 | (65.8) | 298 | (62.0) | |
| ≥19 | 560 | (16.2) | 176 | (15.7) | 71 | (14.8) | |
| Physical Activity ** | 1 | 620 | (18.0) | 211 | (18.8) | 100 | (20.8) |
| 2 | 654 | (18.9) | 222 | (19.8) | 111 | (23.1) | |
| 3 | 706 | (20.4) | 221 | (19.7) | 86 | (17.9) | |
| 4 | 686 | (19.9) | 235 | (20.9) | 88 | (18.3) | |
| 5 | 766 | (22.2) | 227 | (20.2) | 87 | (18.1) | |
| Family Status | Married | 2420 | (70.1) | 787 | (70.1) | 307 | (63.8) |
| Single | 185 | (5.4) | 65 | (5.8) | 24 | (5.0) | |
| Separated | 52 | (1.5) | 13 | (1.2) | 7 | (1.5) | |
| Divorced | 383 | (11.1) | 125 | (11.1) | 64 | (13.3) | |
| Widowed | 413 | (12.0) | 132 | (11.8) | 79 | (16.4) | |
| Parous | Yes | 2932 | (84.9) | 932 | (83.0) | 409 | (85.0) |
| No | 521 | (15.1) | 191 | (17.0) | 72 | (15.0) | |
| Osteoporosis | Yes | 340 | (9.8) | 109 | (9.7) | 67 | (13.9) |
| No | 3012 | (87.2) | 993 | (88.4) | 396 | (82.3) | |
| Diabetes | Yes | 160 | (4.6) | 53 | (4.7) | 47 | (9.8) |
| No | 3288 | (95.2) | 1068 | (95.1) | 434 | (90.2) | |
| CVD | Yes | 1458 | (42.2) | 496 | (44.2) | 252 | (52.4) |
| No | 1995 | (57.8) | 627 | (55.8) | 229 | (47.6) | |
| Rheumatic Diseases | Yes | 1675 | (48.5 | 551 | (49.1) | 236 | (49.1) |
| No | 1752 | (50.7) | 564 | (50.2) | 252 | (52.4) | |
| During Radiation | During Chemotherapy | 1 Year Post OP | 5 Years Post OP | 10 Years Post Diagnosis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Groups | Mean ∆ (95%CI) | p | Mean ∆ (95%CI) | p | Mean ∆ (95%CI) | p | Mean ∆ (95%CI) | p | Mean ∆ (95%CI) | p |
| 1 vs. 2 | –2.34 (−7.15, 2.47) | 0.49 | 2.94 (−3.71, 9.59) | 0.55 | −2.59 (−7.20, 2.03) | 0.39 | −1.91 (−576, 1.93) | 0.83 | 1.06 (−3.22, 5.35) | 0.83 |
| 1 vs. 3 | −5.05 (−9.87, −0.22) | 0.04 | 0.14 (−7.23, 7.51) | 1.00 | −5.42 (−10.07, −0.78) | 0.02 | 1.75 (−2.13, 5.63) | 0.18 | 5.04 (0.69, 9.38) | 0.02 |
| 2 vs. 3 | −2.70 (−7.36, 1.95) | 0.36 | −2.80 (−10.36, 4.75) | 0.66 | −2.84 (−7.36, 1.69) | 0.30 | 3.66 (−0.11, 5.76) | 0.69 | 3.98 (−0.24, 8.19) | 0.07 |
| 1 vs. controls | −3.52 (−6.51, 0.52) | 0.02 | ||||||||
| 2 vs. controls | −0.76 (−3.70, 2.18) | 0.60 | ||||||||
| 3 vs. controls | −0.77 (−3.73, 2.20) | 0.62 | ||||||||
| Age | FU1 | FU2 | Controls FU2 | Cases FU1 vs. Cases FU2 | Cases FU2 vs. Controls FU2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | Mean | Mean | Mean | Mean ∆ (95%CI) | p | CR * | Mean ∆ (95%CI) | p | CR | |
| Physical | ≤58 | 79.28 | 83.10 | 85.54 | 3.82 (2.18, 5.47) | <0.0001 | t | −2.44 (−4.53, −0.36) | 0.33 | |
| 59–64 | 81.49 | 79.27 | 80.12 | −2.22 (−3.69, −0.74) | 0.004 | −0.80 (−3.00, 1.41) | 0.98 | |||
| ≥64 | 75.19 | 71.59 | 70.65 | −3.59 (−5.39, −1.79) | <0.0001 | t | 0.5 (−3.52, 1.83) | 0.98 | ||
| Role | ≤58 | 70.70 | 81.27 | 85.73 | 10.57 (7.66, 13.48) | <0.0001 | s | −4.47 (−7.31, −1.63) | 0.071 | |
| 59–64 | 77.31 | 79.42 | 79.90 | 2.10 (−0.47, 4.67) | 0.07 | −0.51 (−3.52, 2.49) | 0.1 | |||
| ≥64 | 70.27 | 69.98 | 72.24 | −0.29 (−3.05, 2.47) | 0.69 | −2.19 (−5.78, 1.40) | 0.76 | |||
| Emotional | ≤58 | 62.33 | 70.35 | 77.30 | 8.00 (5.54, 10.48) | <0.0001 | s | −6.95 (−9.72, −4.17) | <0.0001 | s |
| 59–64 | 71.29 | 73.78 | 77.15 | 2.49 (0.28, 4.71) | 0.03 | −3.37 (−5.95, −0.78) | 0.12 | |||
| ≥64 | 70.44 | 72.76 | 75.77 | 2.33 (0.12, 4.54) | 0.03 | −3.00 (−5.83, −0.17) | 0.27 | |||
| Cognitive | ≤58 | 72.96 | 78.67 | 86.33 | 5.71 (3.30, 8.13) | <0.0001 | s | −7.66 (−10.10, −5.22) | <0.0001 | m |
| 59–64 | 79.25 | 79.12 | 85.39 | 0.13 (−2.08, 1.82) | 0.86 | −6.27 (−8.56, −3.97) | <0.0001 | s | ||
| ≥64 | 78.68 | 79.41 | 81.09 | 0.74 (−1.43, 2.90) | 0.33 | −1.86 (−4.44, 0.71) | 0.67 | |||
| Social | ≤58 | 75.84 | 84.54 | 87.51 | 8.70 (6.06, 11.33) | <0.0001 | m | −2.99 (−5.83, −0.13) | 0.40 | |
| 59–64 | 86.31 | 86.56 | 85.19 | 0.26 (−1.97, 2.48) | 0.82 | 1.40 (1.38, −1.40) | 0.94 | |||
| ≥64 | 81.81 | 80.73 | 80.05 | −1.08 (−3.84, −1.69) | 0.74 | 0.78 (−2.66, 4.22) | 0.1 | |||
| Age | FU1 | FU2 | Controls FU2 | Cases FU1 vs. Cases FU2 | Cases FU2 vs. Controls FU2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | Mean | Mean | Mean | Mean ∆ (95%CI) | p | CR * | Mean ∆ (95%CI) | p | CR | |
| Fatigue | ≤58 | 37.67 | 29.64 | 24.74 | −8.03 (−10.43, −5.62) | <0.0001 | s | 4.90 (2.09, 7.71) | 0.01 | s |
| 59–64 | 31.53 | 30.46 | 29.02 | −1.07 (−3.15, 1.02) | 0.34 | 1.44 (−1.34, 4.22) | 0.91 | |||
| ≥64 | 37.64 | 38.01 | 35.92 | 0.37 (−1.86, 2.60) | 0.65 | 2.09 (−5.15, 0.98) | 0.72 | |||
| Pain | ≤58 | 29.61 | 26.32 | 25.38 | −3.29 (−6.33, −0.25) | 0.013 | s | 0.94 (−2.63, 4.51) | 1 | |
| 59–64 | 25.62 | 25.72 | 29.2 | 0.11 (−2.72, 2.94) | 0.83 | −3.37 (−6.90, 0.16) | 0.43 | |||
| ≥64 | 31.11 | 33.33 | 36.08 | 2.23 (−0.77, 5.23) | 0.16 | −2.70 (−6.70, 1.31) | 0.72 | |||
| Nausea/Vomiting | ≤58 | 4.72 | 4.82 | 3.3 | 0.10 (−1.36, 1.55) | 0.97 | 1.52 (0.10, 2.93) | 0.24 | ||
| 59–64 | 3.38 | 3.15 | 2.91 | −0.23 (−1.61, 1.14) | 0.88 | 0.23 (−0.94, 1.41) | 1 | |||
| ≥64 | 3.67 | 4.09 | 3.65 | 0.42 (−1.07, 1.91) | 0.84 | 0.42 (−0.99, 1.83) | 0.99 | |||
| Dyspnoe | ≤58 | 28.2 | 24.18 | 17.76 | 4.07 (−7.09, −1.05) | 0.005 | s | 6.42 (3.26, 9.59) | 0.004 | s |
| 59–64 | 23.7 | 25.65 | 22.43 | 1.94 (−1.07, 4.96) | 0.29 | 3.25 (−0.06, 6.56) | 0.37 | |||
| ≥64 | 26.41 | 26.72 | 26.22 | 0.31 (−2.59, 3.22) | 0.93 | 0.55 (−3.16, 4.26) | 1 | |||
| Insomnia | ≤58 | 47.12 | 41.91 | 33.68 | −5.21 (−8.72, −1.71) | 0.0074 | s | 8.45 (4.40, 12.49) | 0.0008 | s |
| 59–64 | 44.96 | 41.97 | 34.38 | 2.99 (−6.39, 0.41) | 0.0297 | t | 7.72 (3.87, 11.56) | 0.001 | s | |
| ≥64 | 40.56 | 42.46 | 36.01 | 1.90 (−1.40, 5.20) | 0.234 | 6.32 (2.16, 10.48) | 0.03 | s | ||
| Appetite Loss | ≤58 | 8.89 | 6.38 | 4.77 | −2.51 (−4.72, −0.31) | 0.02 | s | 1.61 (−0.23, 3.44) | 0.73 | |
| 59–64 | 4.69 | 6.05 | 6.9 | 1.36 (−0.65, 3.37) | 0.3027 | −0.85 (−2.99, 1.19) | 0.97 | |||
| ≥64 | 7.66 | 10.7 | 10.82 | 3.03 (0.40, 5.66) | 0.04 | s | −0.03 (−2.77, 2.71) | 1 | ||
| Constipation | ≤58 | 10.69 | 10.4 | 7.76 | −0.29 (−2.74, 2.16) | 0.81 | 2.62 (0.24, 5.00) | 0.44 | ||
| 59–64 | 11.55 | 13.21 | 10.11 | 1.66 (−0.67, 4.00) | 0.15 | 3.07 (0.42, 5.71) | 0.2 | |||
| ≥64 | 15.72 | 15.63 | 14.21 | −0.09 (−2.84, 2.66) | 0.74 | 1.43 (−1.73, 4.59) | 0.91 | |||
| Diarrhea | ≤58 | 9.84 | 10.08 | 8.39 | 0.24 (−2.11, 2.60) | 0.9 | 1.66 (−0.82, 4.13) | 0.73 | ||
| 59–64 | 9.52 | 7.32 | 7.3 | −2.20 (−4.31, −0.08) | 0.071 | 0.11 (−2.04, 2.26) | 1 | |||
| ≥64 | 8.2 | 7.21 | 6.84 | −0.99 (−3.25, 1.27) | 0.41 | 0.25 (−2.47, 1.97) | 1 | |||
| Financial Difficulties | ≤58 | 24.98 | 11.53 | 5.5 | −13.45 (−16.52 −10.38) | <0.0001 | l | 6.02 (3.95, − 8.45) | <0.0001 | s |
| 59–64 | 8.29 | 7.23 | 6.06 | −1.06 (−2.83, 0.71) | 0.1862 | 1.17 (−0.89, 3.23) | 0.91 | |||
| ≥64 | 12.74 | 8.82 | 7.94 | −3.92 (−6.29, −1.55) | 0.0053 | s | 1.10 (−1.41, 3.61) | 0.94 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maurer, T.; Thöne, K.; Obi, N.; Jung, A.Y.; Behrens, S.; Becher, H.; Chang-Claude, J. Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More Than 10 Years Post-Diagnosis and in Comparison to a Control Cohort. Cancers 2021, 13, 1854. https://doi.org/10.3390/cancers13081854
Maurer T, Thöne K, Obi N, Jung AY, Behrens S, Becher H, Chang-Claude J. Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More Than 10 Years Post-Diagnosis and in Comparison to a Control Cohort. Cancers. 2021; 13(8):1854. https://doi.org/10.3390/cancers13081854
Chicago/Turabian StyleMaurer, Tabea, Kathrin Thöne, Nadia Obi, Audrey Y. Jung, Sabine Behrens, Heiko Becher, and Jenny Chang-Claude. 2021. "Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More Than 10 Years Post-Diagnosis and in Comparison to a Control Cohort" Cancers 13, no. 8: 1854. https://doi.org/10.3390/cancers13081854
APA StyleMaurer, T., Thöne, K., Obi, N., Jung, A. Y., Behrens, S., Becher, H., & Chang-Claude, J. (2021). Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More Than 10 Years Post-Diagnosis and in Comparison to a Control Cohort. Cancers, 13(8), 1854. https://doi.org/10.3390/cancers13081854







