Simple Summary
NTRK fusion genes are important but not well studied molecular markers in thyroid cancer. Their identification could help improve diagnosis and prognosis, and determine appropriate treatment. The aims of this study were to identify NTRK fusion-positive thyroid tumors in a large cohort of different thyroid tumors, to characterize these tumors by molecular, clinical and pathological features and to evaluate the impact of NTRK-rearranged tumors on prognosis of the disease. A suitable approach for selective NTRK fusion gene testing in thyroid cancer samples was created and utilized. In a cohort of 59 NTRK-rearranged carcinomas, characteristic features were described and recommendations for surgery and prognostic factors were determined thanks to the long-term follow-up of patients.
Abstract
Chromosomal rearrangements of NTRK genes are oncogenic driver mutations in thyroid cancer (TC). This study aimed to identify NTRK fusion-positive thyroid tumors and to correlate them with clinical and pathological data and determine their prognostic significance. The cohort consisted of 989 different TC samples. Based on the detected mutation, samples were triaged, and those that were positive for a BRAF, HRAS, KRAS, NRAS, RET, RET/PTC or PAX8/PPARγ mutation were excluded from further analyses. NTRK fusion gene testing was performed in 259 cases, including 126 cases using next-generation sequencing. NTRK fusion genes were detected in 57 of 846 (6.7%) papillary thyroid carcinomas and in 2 of 10 (20.0%) poorly differentiated thyroid carcinomas. A total of eight types of NTRK fusions were found, including ETV6/NTRK3, EML4/NTRK3, RBPMS/NTRK3, SQSTM1/NTRK3, TPM3/NTRK1, IRF2BP2/NTRK1, SQSTM1/NTRK1 and TPR/NTRK1. NTRK fusion-positive carcinomas were associated with the follicular growth pattern, chronic lymphocytic thyroiditis and lymph node metastases. NTRK1-rearranged carcinomas showed a higher frequency of multifocality and aggressivity than NTRK3-rearranged carcinomas. Tumor size, presence of metastases, positivity for the NTRK3 or NTRK1 fusion gene and a late mutation event (TERT or TP53 mutation) were determined as factors affecting patient prognosis. NTRK fusion genes are valuable diagnostic and prognostic markers.
1. Introduction
Thyroid cancer (TC) is the most common endocrine malignancy with a still increasing incidence. The prognosis of TC varies primarily depending on the type and stage of the tumor. In the case of papillary thyroid carcinoma (PTC), the prognosis is very favorable and the 10-year overall survival rate is 97% [1]. On the other hand, poorly differentiated thyroid carcinoma (PDTC) carries a worse prognosis, and anaplastic thyroid carcinoma (ATC) has a median survival of 6 months [2]. The clinical outcome of the disease is associated with various mutations occurring in TC. The most common mutation in TC is the BRAF V600E mutation, which has appeared to be associated with a higher risk of cancer recurrence [3]. However, this association has recently been disputed [4]. TERT promoter mutations are associated with distant metastases and a higher risk of mortality in advanced cases of TC [5]. Differentiated thyroid tumors harboring RAS mutations without any co-alterations have excellent prognosis [6]. Other genetic alterations occurring in TC are rearrangements of NTRK, RET, ALK, BRAF, MET, FGFR, PPARγ or ROS1 genes whose associations with the outcome of the disease are not yet well known.
A rearrangement involving one of the neurotrophic-tropomyosin receptor kinase (NTRK) genes belonging to the NTRK family represents a significant oncogenic event in TC. The NTRK family includes three genes, NTRK1, NTRK2 and NTRK3, encoding tropomyosin receptor kinases A, B and C, respectively. Fusions involving a kinase domain of NTRK gene lead to uncontrolled activation of the tyrosine receptor kinase (TRK) and subsequently the MAPK, PI3K/AKT and PLCγ pathways [7].
In TC, NTRK fusions have been reported in PTC, Hürthle cell carcinoma (HCC), PDTC and ATC [8,9]. The presence of NTRK fusions in TC is rare and the frequency ranges from 2.3 to 3.4% in predominantly adult cohorts [8,10,11,12]. In pediatric TC, NTRK fusions are approximately eight times more common than in adults; the frequency is between 18.3% and 25.9% [13,14,15]. Clinicopathological characteristics and long-term disease development are not well understood due to limited NTRK fusion-positive cohorts. Recently, there has been a growing interest in testing and characterizing NTRK fusion genes because they are therapeutically targetable. NTRK fusion-positive tumors are sensitive to TRK inhibitors, such as larotrectinib, which appears to be well tolerated and effective [16].
This study aimed to determine clinical and pathological features of a large cohort of NTRK fusion-positive thyroid tumors, to compare these characteristics between NTRK3 and NTRK1 fusion-positive tumors and to determine the prognostic significance of NTRK fusion genes based on long-term follow-up of patients with TC harboring this mutation.
2. Materials and Methods
2.1. The Cohort
A total of 989 (851 PTCs, 86 medullary thyroid carcinomas (MTCs), 19 follicular thyroid carcinomas (FTCs), 13 ATCs, 10 PDTCs and 10 HCCs) thyroid cancer tissues, 30 borderline thyroid tumor tissues (17 follicular tumors of uncertain malignant potential (FT-UMPs), 13 non-invasive follicular tumors with papillary-like nuclear features (NIFTPs)) and 194 benign thyroid tissues were collected from patients who underwent thyroid surgery at the Motol University Hospital (between years 2003 and 2020), the University Hospital Kralovske Vinohrady (between years 2016 and 2020) and the Military University Hospital (between years 2019 and 2020) in Prague. All samples except 65 formalin-fixed paraffin-embedded (FFPE) were fresh frozen thyroid tissues. Detailed clinical and pathological data were collected from all patients whose tumors were positive for the NTRK fusion gene.
2.2. Nucleic Acid Extraction
DNA and RNA were extracted from fresh frozen thyroid tissues using the AllPrep DNA/RNA/Protein Mini Kit (Qiagen, Venlo, Netherlands) or the AllPrep DNA/RNA/miRNA Universal Kit (Qiagen) and from FFPE thyroid tissues using the AllPrep DNA/RNA FFPE Kit (Qiagen) according to the instructions in the manuals. The concentrations and purity of samples were measured using a fluorometer (Qubit 2.0, Invitrogen, Carlsbad, CA, USA) and a spectrophotometer (QIAxpert, Qiagen), respectively.
2.3. NTRK Fusion Genes in Pediatric Samples
Analyses of NTRK fusion genes in pediatric PTC specimens (n = 93) using the QIASeq Targeted RNAscan panel (Qiagen) or the FusionPlex Comprehensive Thyroid and Lung (CTL) panel (ArcherDx, Boulder, CO, USA) were described previously [13]. New pediatric PTC samples collected during year 2020 (n = 11) were analyzed by the same procedure as the adult TC samples described below.
2.4. Analyses of Point Mutations, RET/PTC and PAX8/PPARγ Rearrangements
First, detection of mutations in the BRAF, HRAS, KRAS, NRAS, TERT, and TP53 genes, and RET/PTC1, RET/PTC3, and PAX8/PPARγ rearrangements in PTC, ATC, PDTC, FTC and HCC samples was performed. Mutations in the RET, HRAS and KRAS genes were analyzed in MTC samples. Libraries were prepared from purified PCR products of genes BRAF (exon 15), HRAS (exons 2 and 3), KRAS (exons 2 and 3), NRAS (exons 2 and 3), TP53 (exons 4, 5, 6, 7, 8 and 9) and RET (exons 8, 10, 11, 13, 14, 15 and 16) using the Nextera XT DNA Library Prep Kit (Illumina, San Diego, CA, USA) and subsequently sequenced on the MiSeq sequencer (Illumina). The promoter of the TERT gene was screened for the C228T and C250T mutations using capillary sequencing on the CEQ 8000 instrument (Beckman Coulter, Brea, CA, USA). A more detailed procedure was described in our previous study [17].
For RET/PTC and PAX8/PPARγ rearrangements detection, total RNA was reverse transcribed into cDNA by the same procedure as reported previously [13]. Subsequently, cDNA was diluted five times and amplified using the TaqMan Fast Advanced Master Mix (Applied Biosystems, Foster City, CA, USA), gene-specific primers and hydrolysis probes designed using the Primer3Plus software tool. Primer and probe sequences are summarized in Supplementary Table S1. Amplification of the ACTB gene was used as a cDNA quality control. Each experiment included a negative control where RNase-free water was used instead of template cDNA. Real-time PCR was performed as follows by the Light Cycler® 480 (Roche, Penzberg, Germany): 50 °C for 2 min, 95 °C for 20 s, followed by 40 cycles of 95 °C for 3 s and 60 °C for 30 s. The evaluation was performed by the Light Cycler® 480 SW 1.5.1. (Roche).
2.5. NTRK Fusion Genes Detection
Based on the previously detected mutations, specimens were selected for analyses of the NTRK fusion genes. Samples positive for the BRAF, HRAS, KRAS, NRAS, RET, RET/PTC or PAX8/PPARγ mutation were excluded from the further analyses. In contrast, samples in which the TERT or TP53 mutation was identified were included in further testing.
A total of 259 (205 PTCs, 16 sporadic MTCs, 13 FTCs, 9 ATCs, 6 PDTCs, and 10 HCCs) thyroid tissue samples were retrospectively analyzed using the NTRK Gene Fusions Detection Kit (AmoyDx, Xiamen, China) according to the manufacturer’s instructions. This Real-Time PCR kit allows to detect 109 different NTRK1, NTRK2 or NTRK3 fusions. Real-time PCR was performed using the Light Cycler® 480 (Roche) and the results were evaluated by the Light Cycler® 480 SW 1.5.1. (Roche).
An extended analysis of next-generation sequencing was performed for a total of 126/259 thyroid tissue samples (93 PTCs, 16 sporadic MTCs, 2 FTCs, 9 ATCs, and 6 PDTCs) using the FusionPlex CTL panel (ArcherDx) allowing to detect novel fusion genes as well. The manufacturer’s instructions were followed. Briefly, RNA was reverse transcribed using random primers into cDNA. The adapters containing unique molecular tags and sample indexes (i5) were ligated to modified ends of cDNA. Then, two rounds of PCR followed. Other sample indexes (i7) were added during the second PCR. Purified and quantified libraries were paired-end sequenced on the MiSeq sequencer (Illumina). Bioinformatic analysis was performed using the Archer Analysis software version 6.0.4. (ArcherDx). For a gene fusion to be considered as valid, at least five high-quality unique reads had to span the breakpoint and a minimum of three reads had to have a unique start site.
The gene-specific primers and hydrolysis probes were designed for all identified NTRK fusion genes using the Primer3Plus software tool. Primer and probe sequences are summarized in Supplementary Table S1. All NTRK fusion-positive samples were verified using these primers and probes by real-time PCR. PCR conditions were the same as for RET/PTC or PAX8/PPARγ rearrangements detection. A total of 30 borderline thyroid samples and 194 benign thyroid samples were screened by this procedure for all these identified NTRK fusion genes.
2.6. Statistical Analysis
Categorical variables were compared by use of the Fisher’s exact test, and continuous variables were compared by use of the t-test. Statistical analyses were performed using the Simple Interactive Statistical Analysis (SISA, https://www.quantitativeskills.com/sisa/) and GraphPad tools (GraphPad Software, San Diego, CA, USA). A p value < 0.05 was considered as statistically significant.
3. Results
3.1. Clinical and Pathological Features
The analyses revealed NTRK fusion gene in 59 patients with TC, in 57 of 846 (6.7%) patients with PTC in 2 of 10 (20.0%) patients with PDTC. No NTRK fusion gene was detected in 16 MTCs, 13 FTCs, 9 ATCs, 10 HCCs, 30 borderline thyroid tumors or 190 benign thyroid tissues subjected to NTRK fusion analyses. cDNA from five FFPE PTCs and four benign fresh frozen thyroid tissues were not of sufficient quality for analyses.
Clinical and pathological data of patients with TC harboring NTRK fusion are summarized in Table 1. In this cohort, the female to male ratio was 3.5:1 and the mean age of diagnosis was 32.8 ± 16.0 (range 6–77 years). The cohort consisted of 17 pediatric (˂20 years of age) and of 42 adult patients. Before the diagnosis of TC, only one patient suffered from a malignant disease (sigmoid colon cancer) and underwent radiation therapy. Four patients underwent hemithyroidectomy followed by total thyroidectomy, 55 patients underwent total thyroidectomy during one surgery and 37 patients also underwent lymph node (LN) dissection. The mean tumor size was 20.9 ± 11.9 mm (range 5–55 mm). A microcarcinoma (≤10 mm) was revealed in 13.6% of patients. A follicular growth pattern was shown to be present in 78.0% of cases, of which in 47.5% of cases it formed the whole tumor or was predominant, and in 30.5% of cases it was found mixed with a papillary growth pattern (approximately in a similar proportion). Only 13.6% of cases had predominantly papillary architecture. Both cases of PDTC had coexisting PTC component with a mixed papillary and follicular growth pattern. Multifocality, extrathyroidal extension and intravascular invasion were identified in 44.1%, 40.7% and 23.5% of cases, respectively. LN metastases were found in 54.2% of patients and distant metastases in 6.8% of patients, in all cases affecting lungs. Chronic lymphocytic thyroiditis (CLT) was identified in 65.5% of cases. Detailed data on individual cases are described in Supplementary Table S2.

Table 1.
Clinicopathological features of NTRK fusion-positive carcinomas.
3.2. NTRK Fusion Genes
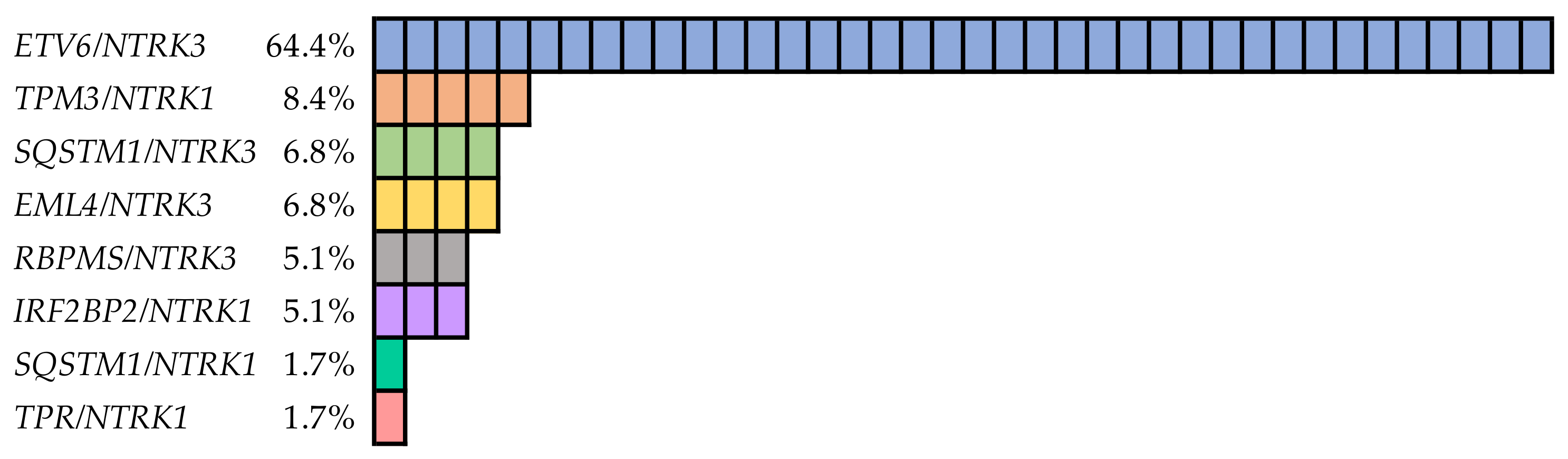
A total of eight types of NTRK fusions were found, including ETV6/NTRK3 (four isoforms), EML4/NTRK3, RBPMS/NTRK3, SQSTM1/NTRK3, TPM3/NTRK1, IRF2BP2/NTRK1 (two isoforms), SQSTM1/NTRK1 and TPR/NTRK1 (Figure 1). All fusion genes were in-frame. Transcripts of genes involved are listed in Supplementary Table S3. The ETV6/NTRK3 fusion gene represented the majority (38/59) of positive cases. The most common isoform was the ETV6 (exon 4)/NTRK3 (exon 14), which was detected in one case together with the ETV6 (exon 5)/NTRK3 (exon 14) isoform. Furthermore, in one PDTC case, two rare isoforms ETV6 (exon 2)/NTRK3 (exon 14) and ETV6 (exon 5)/NTRK3 (exon 15) were identified. The TPM3/NTRK1 fusion gene was detected in a significantly smaller group of samples (5/59), similarly to the SQSTM1/NTRK3 (4/59), EML4/NTRK3 (4/59), RBPMS/NTRK3 (3/59) and IRF2BP2/NTRK1 (3/59) fusion genes. Two isoforms of the IRF2BP2/NTRK1 fusion gene, IRF2BP2 (exon 1)/NTRK1 (exon 10) in two cases and IRF2BP2 (exon 2)/NTRK1 (exon 10) in one case were identified. The SQSTM1/NTRK1 was identified in the second PDTC case and the TPR/NTRK1 was found in one PTC.

Figure 1.
Frequencies of different types of NTRK fusion genes detected in thyroid cancer.
Co-alterations were identified in two samples and in both cases with TPM3/NTRK1. In the first case, the co-alteration was the TERT C228T mutation and in the second case, the TP53 K320* nonsense mutation. In one patient with multifocal PTC, the ETV6/NTRK3 rearrangement was identified in a nodule in the right thyroid lobe and the BRAF V600E mutation in a nodule in the left thyroid lobe.
The carcinomas harboring NTRK3 fusions (n = 49) were compared to the carcinomas with NTRK1 fusions (n = 10) (Table 2). NTRK3 fusion genes were almost 5 times more common than NTRK1 fusions. The carcinomas positive for NTRK1 fusions had a significantly more common mixture of papillary and follicular growth patterns (p = 0.006) than the carcinomas positive for NTRK3 fusions, which had mostly predominant follicular growth patterns. Other differences were the significantly higher frequencies of multifocality (p = 0.015), extrathyroidal extension (p = 0.008), intravascular invasion (p = 0.024) and distant metastases (p = 0.013) of NTRK1 fusion-positive carcinomas. The patients with carcinomas harboring NTRK1 fusions had LN metastases 80% of the time compared to 49% of time for NTRK3 fusion-positive carcinomas. However, the difference only approached the limit of statistical significance (p = 0.072).

Table 2.
Comparison of clinical and pathological features between NTRK3 and NTRK1 fusion-positive carcinomas.
Clinicopathological features of NTRK fusion-positive carcinomas were also compared between pediatric and adult patients (Supplementary Table S4). No statistically significant difference was observed between these cohorts.
3.3. Treatment and Follow-Up
The median follow-up was 63 months (range: 2–203 months). Fifty-one (86.4%) patients received radioactive iodine (RAI) treatment; eight patients (13.6%) received no RAI treatment due to microcarcinoma without aggressive features. The median cumulative dose of RAI per patient was 6.3 GBq (range: 1.9–28.0 GBq). Most patients (84.3%) were RAI responsive and accumulated RAI in thyroid remnants or in metastases. In addition to RAI therapy, both PDTC cases were also treated with external beam radiotherapy. The first patient with PDTC harboring two rare isoforms of ETV6/NTRK3 fusions discontinued radiation treatment due to intolerance and subsequently died. The second patient with PDTC harboring SQSTM1/NTRK1 was still alive (12 months after surgery). One patient with PTC and other two malignancies (sigmoid colon cancer diagnosed before TC and breast cancer diagnosed after TC), harboring TPM3/NTRK1 and TERT C228T mutations in PTC, underwent chemotherapy treatment and subsequently died.
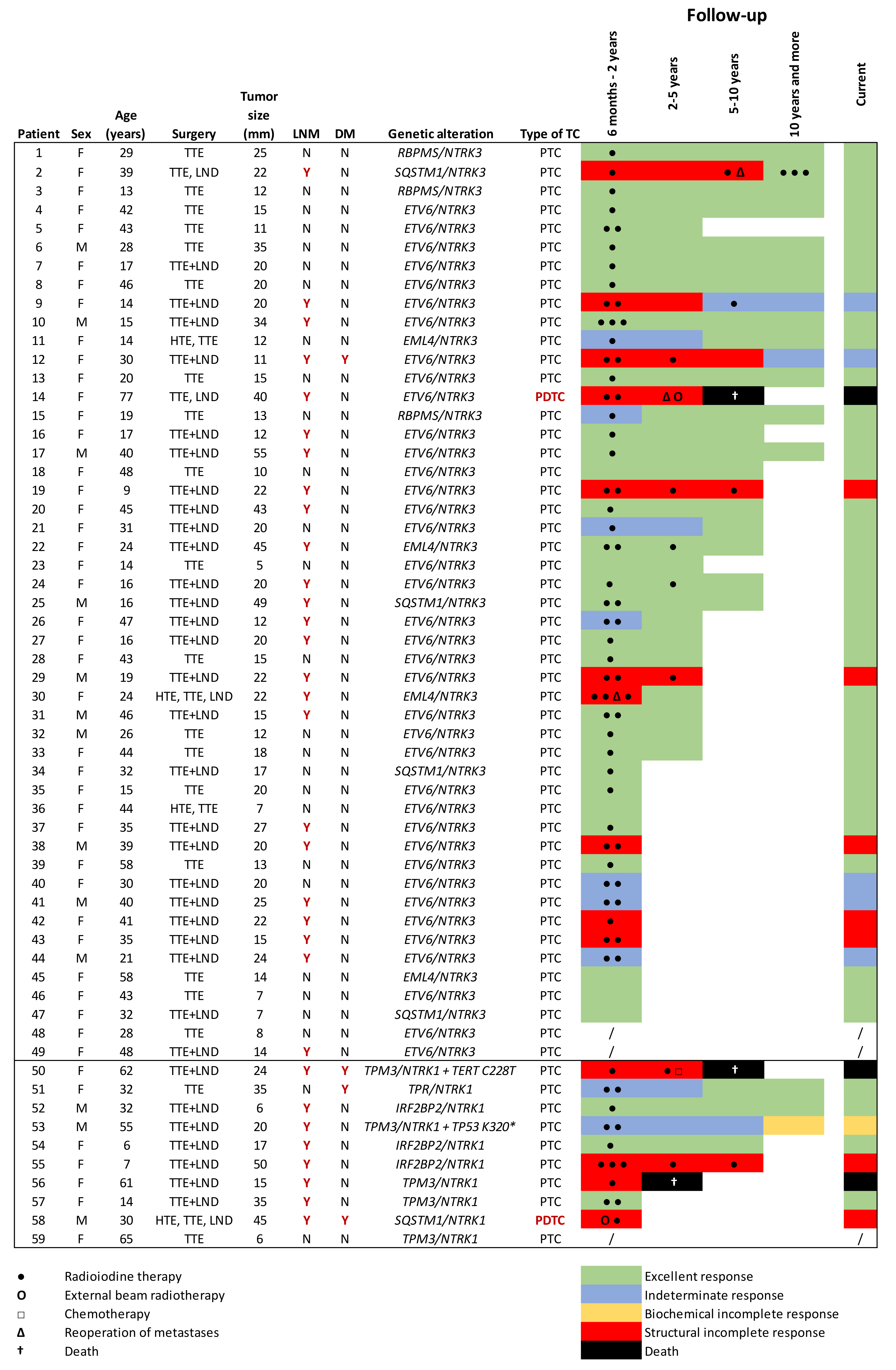
Each responses to treatment was determined using definitions and criteria in the 2015 American Thyroid Association Guidelines as an excellent response (ER), an indeterminate response (IR), a biochemical incomplete response (BIR), a structural incomplete response (SIR), [18] or death. The response to treatment was assessed in the following time periods after surgery: 6 months to 2 years, 2–5 years, 5–10 years, 10 years or more and current response. Detailed follow-ups describing the courses of treatment in individual patients are displayed in Figure 2. Follow-up data of one patient were unknown and two patients were not evaluated due to short-term follow-up (less than six months after surgery).

Figure 2.
Detailed follow-ups and the outcomes of patients harboring NTRK fusion-positive carcinomas. F, female; M, male; the, hemithyroidectomy; TTE, total thyroidectomy; LND, lymph node dissection; LNM, lymph node metastases; DM, distant metastases; TC, thyroid cancer; Y, yes; N, no; PTC, papillary thyroid carcinoma; PDTC, poorly differentiated thyroid carcinoma.
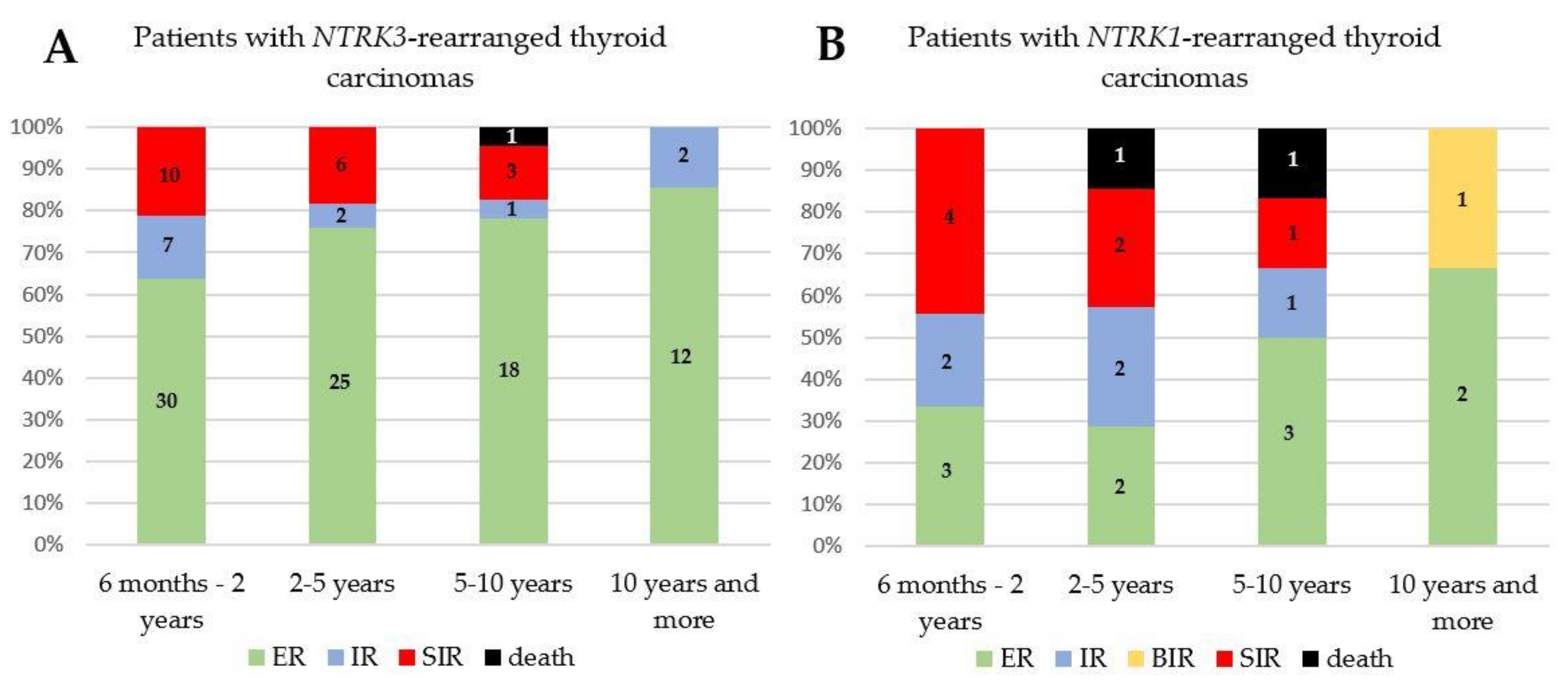
Initially, during two years of treatment, 58.9% of NTRK fusion-positive patients had ER, 16.1% had IR and 25.0% had SIR. When patients were grouped according to the NTRK3 or NTRK1 mutation, 63.8% of NTRK3 fusion-positive patients had ER and 21.3% had SIR. In the case of NTRK1 mutation, more patients had SIR (44.4%) than ER (33.3%). During follow-up, three patients from the cohort who until then had SIR, died. One patient succumbed to PDTC; another two PTC patients were polymorbid. In NTRK fusion-positive cohort, the 2, 5 and 10-year overall survival rates were 100.0% (40/40), 96.7% (29/30) and 85.0% (17/20), respectively. However, during follow-up, response to treatment had an improving tendency in NTRK3 as well as in NTRK1 fusion-positive patients (Figure 3). After 10 years of follow-up, 82.3% of patients had ER, 11.8% had IR, 5.9% had BIR and no patient had an SIR. No case of recurrence was reported during follow-up when the ER to the patient’s treatment changed to BIR, SIR, IR or death. The patients without metastases had predominantly ER, and 16.7% of them had IR. Only one patient from the cohort who had SIR improved to ER. The reason for the improvement of the patient’s condition was the resection of LN metastases seven years after the initial surgery and subsequent RAI therapy.
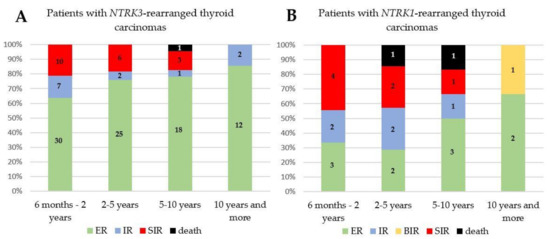
Figure 3.
A graphical representation of the responses to treatment of the patients harboring NTRK3 (A) and NTRK1 (B) fusion-positive carcinomas after surgery. ER, excellent response; IR, indeterminate response; BIR, biochemical incomplete response; SIR, structural incomplete response.
The prognosis of the disease also depended on the size of the tumor. All patients with a microcarcinoma (≤10 mm) had ER to treatment. However, it should be mentioned that one patient with an 11 mm carcinoma had metastases in 25 LN and also in the lungs. After 12 years of follow-up, the patient still had a high level of thyroglobulin antibodies. The patients with the tumor size ≤20 mm (n = 38) had LN metastases 36.8% of the time; and during the initial 2 years of treatment, 68.6% had ER, 17.1% had IR and 14.3% had SIR. The patients with tumors larger than 20 mm (n = 21) had LN metastases 85.7% of the time; and during the initial 2 years of treatment, 42.9% had an ER, 14.3% had IR and 42.9% had SIR. Both patients with PDTC had a tumor larger than 40 mm.
4. Discussion
Molecular testing of genetic alterations in TC can be beneficial in several ways. It can help to establish preoperative diagnosis, the extent of surgery that is possible, estimate prognosis and determine appropriate treatment. Molecular markers, such as the BRAF V600E mutation or the TERT mutation, have been well studied in large cohorts, and the management of thyroid nodules harboring these mutations has also been recommended in the American and the European Thyroid Association Guidelines [18,19]. However, data on NTRK fusion genes in TC are very limited due to their rare occurrence, and therefore there are only small cohorts of NTRK fusion-positive samples that are described and characterized [10,11,12,15,20,21,22,23,24]. Another reason is their more expensive and challenging accurate testing requiring RNA of suitable quality.
In this study, we retrospectively screened a large cohort of different thyroid tissue samples, including PTCs, PDTCs, ATCs, HCCs, FTCs, sporadic MTCs, NIFTPs, FT-UMPs and benign thyroid tissues, for NTRK fusion genes. NTRK fusion genes were detected in 59 TC samples, which to the best of our knowledge represents the largest cohort of NTRK fusion-positive samples in TC worldwide. The prevalence was 6.0% in all tested types of TC and 6.7% in PTCs, which was slightly higher than the prevalence around of 3% reported in PTCs in the literature [8,10,11,12]. One of the reasons for this result was a higher proportion of pediatric PTCs (n = 104) in our cohort, which are known to harbor NTRK fusions with a higher frequency (around 20%) [13,14,15]. After dividing the subjects into pediatric and adult patients, the prevalences of NTRK fusion genes in PTCs were 16.3% and 5.7%, respectively. No NTRK fusion gene was detected in any benign tissue sample (benign tumors, CLT). Thus, all eight tested types of NTRK fusions seem to be associated with a 100% probability of malignancy.
The low detection rate of NTRK fusions in adult PTC samples could discourage routine testing. However, as reported in another study, after elimination of samples harboring the BRAF V600E mutation, the detection rate of NTRK fusion genes increased up to 20% [11]. NTRK fusions are typically mutually exclusive with the BRAF, HRAS, KRAS, NRAS and other driver mutations [8,10,12,13,22]. Therefore, in our study, the samples positive for mutations in the BRAF, HRAS, KRAS and NRAS genes, and for RET/PTC or PAX8/PPARγ were excluded from the NTRK fusion gene analyses, and then the detection rate of NTRK fusions was 22.8%. The co-occurrence of NTRK fusions with the BRAF V600E mutation has been described, but is very rare [21,23]. In contrast, the co-occurrence with late mutation events such as TERT or TP53 mutations has been reported in several studies [9,25,26] and was also confirmed in this study. In one multifocal PTC in our study, the NTRK fusion gene was found in one thyroid nodule and the BRAF V600E mutation in another. Thus, it is important to point out the need to test all nodules in a case of multifocal TC due to the possibility of detection of different mutations, which could affect the patient’s treatment.
All eight identified NTRK fusion types have been previously described and are recurrent in TC [27]. One rare isoform, ETV6(exon 2)/NTRK3(exon 14), detected in the PDTC sample, is unlikely to be oncogenic due to the lack of the SAM domain of ETV6 necessary for the fusion protein oligomerization. The SAM domain is encoded by exons 3 and 4 of the ETV6 gene. The same PDTC sample also harbored another isoform, ETV6(exon 5)/NTRK3(exon 15), whose exons 3 and 4 of the ETV6 gene were preserved. Only NTRK1 and NTRK3 fusions were identified similarly to other studies [11,22,25]. NTRK2 fusions generally occur in other types of cancer, especially in gliomas. However, one case of the NTRK2 fusion (CRNDE/NTRK2) in ATC has been described in the literature [28].
In this study, we performed a detailed clinicopathological review to investigate characteristic features of NTRK fusion-positive tumors. NTRK fusions were associated with the follicular growth pattern, as was also observed previously [11,14,20,21,25]. The predominant follicular pattern was more common in NTRK3 than in NTRK1 fusion-positive carcinomas, in which the follicular architecture mostly co-occurred with foci of papillary formation. Additionally, in most (65.5%) patients with NTRK fusion-positive carcinomas, the CLT was identified. The same findings were concluded in other studies, in which, surprisingly, similar frequencies of CLT were found (66.7% and 69.2%) [20,22].
Regarding the aggressiveness of NTRK fusion-positive carcinomas, data from the publications differed. Chu et al. suggested that NTRK fusion-positive carcinomas are associated with clinically aggressive disease with a high metastatic rate. In their first publication including ten NTRK fusion-positive PTCs, the mean tumor size was 54.2 ± 23.0 mm; 100% of patients had lymphovascular invasion and LN metastases; and 60% of patients had distant metastases [25]. Their following publication included additional NTRK fusion-positive patients with a total of 18 patients. Extrathyroidal extension and LN metastases were then identified in 61.1% and 77.8% of patients, respectively [27]. Fazeli et al. identified distant metastases in 77% of PTC/PDTC patients [23]. All these studies were biased due to case selection, in the case of Chu et al., the authors selected cases based on unusual morphology and advanced presentation. Fazeli et al. chose patients with advanced or RAI refractory cancer [23,27].
In our study, there was no case selection based on the aggressivity of disease. The mean tumor size was 20.9 ± 11.9 and extrathyroidal extension was identified in 40.7%, multifocality in 44.1%, vascular invasion in 23.5%, LN metastases in 54.2% and distant metastases in 6.8%. These findings are in accordance with data found in studies of small cohorts, in which also no selection based on aggressivity of disease was applied: mean tumor size 19.1–33.0 mm [11,12,15,20,22], extrathyroidal invasion in 0–33.3% [11,15,20,22], multifocality in 23.1–66.7% [15,20,22], vascular invasion 16.7–71.4% [15,20], LN metastases in 41.7–72.7% [11,12,15,20,22] and distant metastases in 8% [11,20].
Furthermore, based on our data, NTRK1 fusion-positive carcinomas were significantly associated with a higher frequency of tumor multifocality and distant metastases, and were more invasive than the carcinomas harboring a NTRK3 fusion. There are no records of comparison between NTRK1 and NTRK3 fusion-positive carcinomas in the literature. In addition, in two of our NTRK1 fusion-positive cases, we identified a late mutation event (TERT and TP53 mutation), known to correlate with progressive disease behavior [29]. In contrast, in the literature, late mutation events were detected more frequently along with NTRK3 fusions than with NTRK1 fusions, in four and two cases, respectively [9,26,27,30].
In this study, we identified two cases of PDTC harboring a NTRK fusion gene. Both carcinomas also had a PTC component of a mixed papillary and follicular growth pattern. Thus, we hypothesize that both PTCs harboring a NTRK fusion dedifferentiated to PDTCs. In both PDTCs, only NTRK fusion was detected without further mutations, so we assume that it was a NTRK fusion-driven progression. This finding was also supported by two studies, in which PDTCs with a PTC component were observed [28,31]. The same feature for both PDTCs was the tumor size larger than 40 mm, indicating the importance of early surgery due to a risk of dedifferentiation of large carcinomas harboring a NTRK fusion gene.
Tumor size was also one of the factors affecting the outcome that were identified during follow-up of patients. We demonstrated that the size of the NTRK fusion-positive carcinoma was directly related to the frequency of metastases. The patients with the tumor size ≤20 mm had LN metastases in 36.8% of the time, and those with a tumor larger than 20 mm had LN metastases 85.7% of the time. All patients with microcarcinomas had excellent prognosis and almost all patients without metastases achieved a favorable outcome. On the other hand, more than half of patients with metastases suffered from persistent disease and three patients died. Other indicators of worse outcome were TERT or TP53 co-mutations and the presence of NTRK1 fusion. However, it seems that recurrence risk is very low. No case was observed in which the patient had structural disease after remission. It is important to note that most patients underwent relatively radical surgery and received RAI treatment.
Follow-up data of patients with NTRK fusion-positive TC are very scarce in the literature. Two studies reported that most patients had no evidence of disease [11,20]. Different data were observed in a study biased with case selection based on the aggressivity of disease. Chu et al. reported that from 11 patients with evaluable follow-up, only two patients (18.2%) achieved remission, and the remaining nine patients (81.8%) had recurrence or persistence of the disease. Interestingly, both patients with no evidence of disease had a tumor of the smallest size (21 and 35 mm) from the cohort, harbored a NTRK3 fusion gene and lacked any late mutation event [27].
Carcinomas of most patients in our study were RAI-avid. Therefore, RAI treatment seems to be a “gold standard” therapy for most NTRK fusion-positive carcinomas. In our study, to none of the patients had a TRK inhibitor been administrated. However, in the case of advanced or RAI-refractory carcinomas, patients may benefit from this kind of treatment. For the TRK inhibitor larotrectinib, a response rate of more than 75% was observed regardless of cancer type and was well tolerated by patients [32].
Due to the high risk of multifocality and 100% probability of malignancy, total thyroidectomy may be recommended as a minimal surgical procedure in the case of preoperative detection of the oncogenic NTRK fusion gene in the thyroid nodule. Cervical ultrasonography with LN mapping of central and lateral compartments should be preoperatively performed. In the case of a nodule larger than 20 mm or the presence of late mutation event (TERT or TP53 mutation), prophylactic central LN dissection should be considered.
This study had a few limitations. First, as already mentioned, no patient received TRK inhibitor therapy. Second, 133 samples were only analyzed by real-time PCR, so that novel NTRK fusion genes could not be identified in these samples.
5. Conclusions
In conclusion, we detected the NTRK fusion gene in 59 (6.0%) TC samples. These samples were associated with the follicular growth pattern of TC, chronic lymphocytic thyroiditis and a high rate of LN metastases, especially in larger carcinomas. Furthermore, NTRK1 fusion-positive carcinomas differed from carcinomas harboring the NTRK3 fusion gene by higher frequencies of tumor multifocality, distant metastases and carcinoma invasiveness. Additionally, we reported that the size of the tumor, positivity for NTRK3 or NTRK1 fusion, the presence of metastases and late mutation events may provide prognostic information for patient outcomes. Based on all these findings, testing of NTRK fusions could help to establish diagnosis, advise on extent of surgery, specify prognosis and set up personalized treatments.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13081932/s1. Supplementary Table S1: Sequences of primers and hydrolysis probes designed for the ACTB gene and the detection of NTRK fusion genes using real-time PCR. Supplementary Table S2: Comprehensive clinicopathological data on NTRK fusion-positive carcinomas. Supplementary Table S3: Transcripts of genes involved in NTRK rearrangements Supplementary Table S4: Comparison of clinical and pathological features between pediatric and adult NTRK fusion-positive carcinomas.
Author Contributions
Conceptualization, B.P., V.S. and B.B.; sample and data collection, P.L., M.T., R.K., P.B., M.C. and J.A.; pathological assessment, D.K., J.D. and P.H.; clinical data evaluation, P.V.; methodology, B.P.; experimental investigation, B.P., V.S., K.M., J.M. and E.V.; software, J.V.; writing—original draft preparation, B.P.; writing—review and editing, B.B., V.S. and E.V.; supervision, J.V. and B.B.; funding acquisition, B.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministry of Health of the Czech Republic AZV (NU21-01-00448) and MH CZ—DRO (Institute of Endocrinology—EÚ, 00023761) grants.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Institute of Endocrinology in Prague (approval number F192).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ito, Y.; Miyauchi, A.; Kihara, M.; Fukushima, M.; Higashiyama, T.; Miya, A. Overall Survival of Papillary Thyroid Carcinoma Patients: A Single-Institution Long-Term Follow-Up of 5897 Patients. World J. Surg. 2018, 42, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Nachalon, Y.; Stern-Shavit, S.; Bachar, G.; Shvero, J.; Limon, D.; Popovtzer, A. Aggressive Palliation and Survival in Anaplastic Thyroid Carcinoma. JAMA Otolaryngol. Neck Surg. 2015, 141, 1128–1132. [Google Scholar] [CrossRef]
- Enumah, S.; Fingeret, A.; Parangi, S.; Dias-Santagata, D.; Sadow, P.M.; Lubitz, C.C. BRAFV600E Mutation is Associated with an Increased Risk of Papillary Thyroid Cancer Recurrence. World J. Surg. 2020, 44, 2685–2691. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Kwon, H. The Impact of BRAF Mutation on the Recurrence of Papillary Thyroid Carcinoma: A Meta-Analysis. Cancers 2020, 12, 2056. [Google Scholar] [CrossRef]
- Yang, J.; Gong, Y.; Yan, S.; Chen, H.; Qin, S.; Gong, R. Association between TERT promoter mutations and clinical behaviors in differentiated thyroid carcinoma: A systematic review and meta-analysis. Endocrine 2019, 67, 44–57. [Google Scholar] [CrossRef]
- Xing, M. Clinical utility of RAS mutations in thyroid cancer: A blurred picture now emerging clearer. BMC Med. 2016, 14, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Vaishnavi, A.; Le, A.T.; Doebele, R.C. TRKing Down an Old Oncogene in a New Era of Targeted Therapy. Cancer Discov. 2014, 5, 25–34. [Google Scholar] [CrossRef]
- Solomon, J.P.; Linkov, I.; Rosado, A.; Mullaney, K.; Rosen, E.Y.; Frosina, D.; Jungbluth, A.A.; Zehir, A.; Benayed, R.; Drilon, A.; et al. NTRK fusion detection across multiple assays and 33,997 cases: Diagnostic implications and pitfalls. Mod. Pathol. 2020, 33, 38–46. [Google Scholar] [CrossRef]
- Van Der Tuin, K.; Garcia, M.V.; Corver, W.E.; Khalifa, M.N.; Neto, D.R.; Corssmit, E.P.M.; Hes, F.J.; Links, T.P.; Smit, J.W.A.; Plantinga, T.S.; et al. Targetable gene fusions identified in radioactive iodine refractory advanced thyroid carcinoma. Eur. J. Endocrinol. 2019, 180, 235–241. [Google Scholar] [CrossRef]
- Agrawal, N.; Akbani, R.; Aksoy, B.A.; Ally, A.; Arachchi, H.; Asa, S.L.; Auman, J.T.; Balasundaram, M.; Balu, S.; Baylin, S.B.; et al. Integrated Genomic Characterization of Papillary Thyroid Carcinoma. Cell 2014, 159, 676–690. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Chen, J.-Y.; Huang, C.-J.; Chen, H.-S.; Yang, A.-H.; Hang, J.-F. Detection of NTRK1/3 Rearrangements in Papillary Thyroid Carcinoma Using Immunohistochemistry, Fluorescent In Situ Hybridization, and Next-Generation Sequencing. Endocr. Pathol. 2020, 31, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Cai, W.; Feng, D.; Teng, H.; Mao, F.; Jiang, Y.; Huajing, T.; Li, X.; Zhang, Y.; Liu, B.; et al. Genetic landscape of papillary thyroid carcinoma in the Chinese population. J. Pathol. 2018, 244, 215–226. [Google Scholar] [CrossRef]
- Pekova, B.; Sykorova, V.; Dvorakova, S.; Vaclavikova, E.; Moravcova, J.; Katra, R.; Astl, J.; Vlcek, P.; Kodetova, D.; Vcelak, J.; et al. RET, NTRK, ALK, BRAF, and MET Fusions in a Large Cohort of Pediatric Papillary Thyroid Carcinomas. Thyroid 2020, 30, 1771–1780. [Google Scholar] [CrossRef]
- Picarsic, J.L.; Buryk, M.A.; Ozolek, J.A.; Ranganathan, S.; Monaco, S.E.; Simons, J.P.; Witchel, S.F.; Gurtunca, N.; Joyce, J.; Zhong, S.; et al. Molecular Characterization of Sporadic Pediatric Thyroid Carcinoma with the DNA/RNA ThyroSeq v2 Next-Generation Sequencing Assay. Pediatr. Dev. Pathol. 2016, 19, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Prasad, M.L.; Vyas, M.; Horne, M.J.; Virk, R.K.; Morotti, R.; Liu, Z.; Tallini, G.; Nikiforova, M.N.; Christison-Lagay, E.R.; Udelsman, R.; et al. NTRKfusion oncogenes in pediatric papillary thyroid carcinoma in northeast United States. Cancer 2016, 122, 1097–1107. [Google Scholar] [CrossRef]
- Hong, D.S.; DuBois, S.G.; Kummar, S.; Farago, A.F.; Albert, C.M.; Rohrberg, K.S.; van Tilburg, C.M.; Nagasubramanian, R.; Berlin, J.D.; Federman, N.; et al. Larotrectinib in patients with TRK fusion-positive solid tumours: A pooled analysis of three phase 1/2 clinical trials. Lancet Oncol. 2020, 21, 531–540. [Google Scholar] [CrossRef]
- Pekova, B.; Dvorakova, S.; Sykorova, V.; Vacinova, G.; Vaclavikova, E.; Moravcova, J.; Katra, R.; Vlcek, P.; Sykorova, P.; Kodetova, D.; et al. Somatic genetic alterations in a large cohort of pediatric thyroid nodules. Endocr. Connect. 2019, 8, 796–805. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Paschke, R.; Cantara, S.; Crescenzi, A.; Jarzab, B.; Musholt, T.J.; Simoes, M.S. European Thyroid Association Guidelines regarding Thyroid Nodule Molecular Fine-Needle Aspiration Cytology Diagnostics. Eur. Thyroid J. 2017, 6, 115–129. [Google Scholar] [CrossRef]
- Seethala, R.R.; Chiosea, S.I.; Liu, C.Z.; Nikiforova, M.; Nikiforov, Y.E. Clinical and Morphologic Features of ETV6-NTRK3 Translocated Papillary Thyroid Carcinoma in an Adult Population Without Radiation Exposure. Am. J. Surg. Pathol. 2017, 41, 446–457. [Google Scholar] [CrossRef]
- Leeman-Neill, R.J.; Bs, L.M.K.; Liu, P.; Brenner, A.V.; Leeman-Neill, R.J.; Bogdanova, T.I.; Evdokimova, V.N.; Hatch, M.; Zurnadzy, L.Y.; Nikiforova, M.N.; et al. ETV6-NTRK3 is a common chromosomal rearrangement in radiation-associated thyroid cancer. Cancer 2014, 120, 799–807. [Google Scholar] [CrossRef]
- Abi-Raad, R.; Prasad, M.L.; Adeniran, A.J.; Cai, G. Fine-needle aspiration cytomorphology of papillary thyroid carcinoma withNTRKgene rearrangement from a case series with predominantly indeterminate cytology. Cancer Cytopathol. 2020, 128, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Fazeli, S.; Dadu, R.; Waguespack, S.G.; Sherman, S.I.; Busaidy, N.L.; Hu, M.I.; Jimenez, C.; Habra, M.A.; Williams, M.; Altameemi, L.; et al. MON-491 TRK-Fusion Thyroid Cancer: A Clinical Overview in a Large Population at a Single Cancer Center. J. Endocr. Soc. 2020, 4. [Google Scholar] [CrossRef]
- Pfeifer, A.; Rusinek, D.; Żebracka-Gala, J.; Czarniecka, A.; Chmielik, E.; Zembala-Nożyńska, E.; Wojtaś, B.; Gielniewski, B.; Szpak-Ulczok, S.; Oczko-Wojciechowska, M.; et al. NovelTG-FGFR1andTRIM33-NTRK1transcript fusions in papillary thyroid carcinoma. Genes Chromosom. Cancer 2019, 58, 558–566. [Google Scholar] [CrossRef]
- Chu, Y.-H.; Dias-Santagata, D.; Farahani, A.A.; Boyraz, B.; Faquin, W.C.; Nosé, V.; Sadow, P.M. Clinicopathologic and molecular characterization of NTRK-rearranged thyroid carcinoma (NRTC). Mod. Pathol. 2020, 33, 2186–2197. [Google Scholar] [CrossRef] [PubMed]
- Gatalica, Z.; Xiu, J.; Swensen, J.; Vranic, S. Molecular characterization of cancers with NTRK gene fusions. Mod. Pathol. 2019, 32, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.-H.; Wirth, L.J.; Farahani, A.A.; Nosé, V.; Faquin, W.C.; Dias-Santagata, D.; Sadow, P.M. Clinicopathologic features of kinase fusion-related thyroid carcinomas: An integrative analysis with molecular characterization. Mod. Pathol. 2020, 33, 2458–2472. [Google Scholar] [CrossRef]
- Xu, B.; Fuchs, T.L.; Dogan, S.; Landa, I.; Katabi, N.; Fagin, J.A.; TuttleMD, R.M.; Sherman, E.J.; Gill, A.J.; GhosseinMD, R. Dissecting Anaplastic Thyroid Carcinoma: A Comprehensive Clinical, Histologic, Immunophenotypic, and Molecular Study of 360 Cases. Thyroid 2020, 30, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
- Tavares, C.; Melo, M.; Teijeiro, J.M.C.; Soares, P.; Sobrinho-Simões, M. ENDOCRINE TUMOURS: Genetic predictors of thyroid cancer outcome. Eur. J. Endocrinol. 2016, 174, R117–R126. [Google Scholar] [CrossRef]
- Borre, P.V.; Schrock, A.B.; Anderson, P.M.; Morris, J.C.; Heilmann, A.M.; Holmes, O.; Wang, K.; Johnson, A.; Waguespack, S.G.; Ou, S.I.; et al. Pediatric, Adolescent, and Young Adult Thyroid Carcinoma Harbors Frequent and Diverse Targetable Genomic Alterations, Including Kinase Fusions. Oncologist 2017, 22, 255–263. [Google Scholar] [CrossRef]
- Duan, H.; Li, Y.; Hu, P.; Gao, J.; Ying, J.; Xu, W.; Zhao, D.; Wang, Z.; Ye, J.; Lizaso, A.; et al. Mutational profiling of poorly differentiated and anaplastic thyroid carcinoma by the use of targeted next-generation sequencing. Histopathology 2019, 75, 890–899. [Google Scholar] [CrossRef] [PubMed]
- Kummar, S.; Lassen, U.N. TRK Inhibition: A New Tumor-Agnostic Treatment Strategy. Target. Oncol. 2018, 13, 545–556. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).