COVID-19 Vaccination in Patients with Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. Vaccination Status
4.2. Vaccination Timing
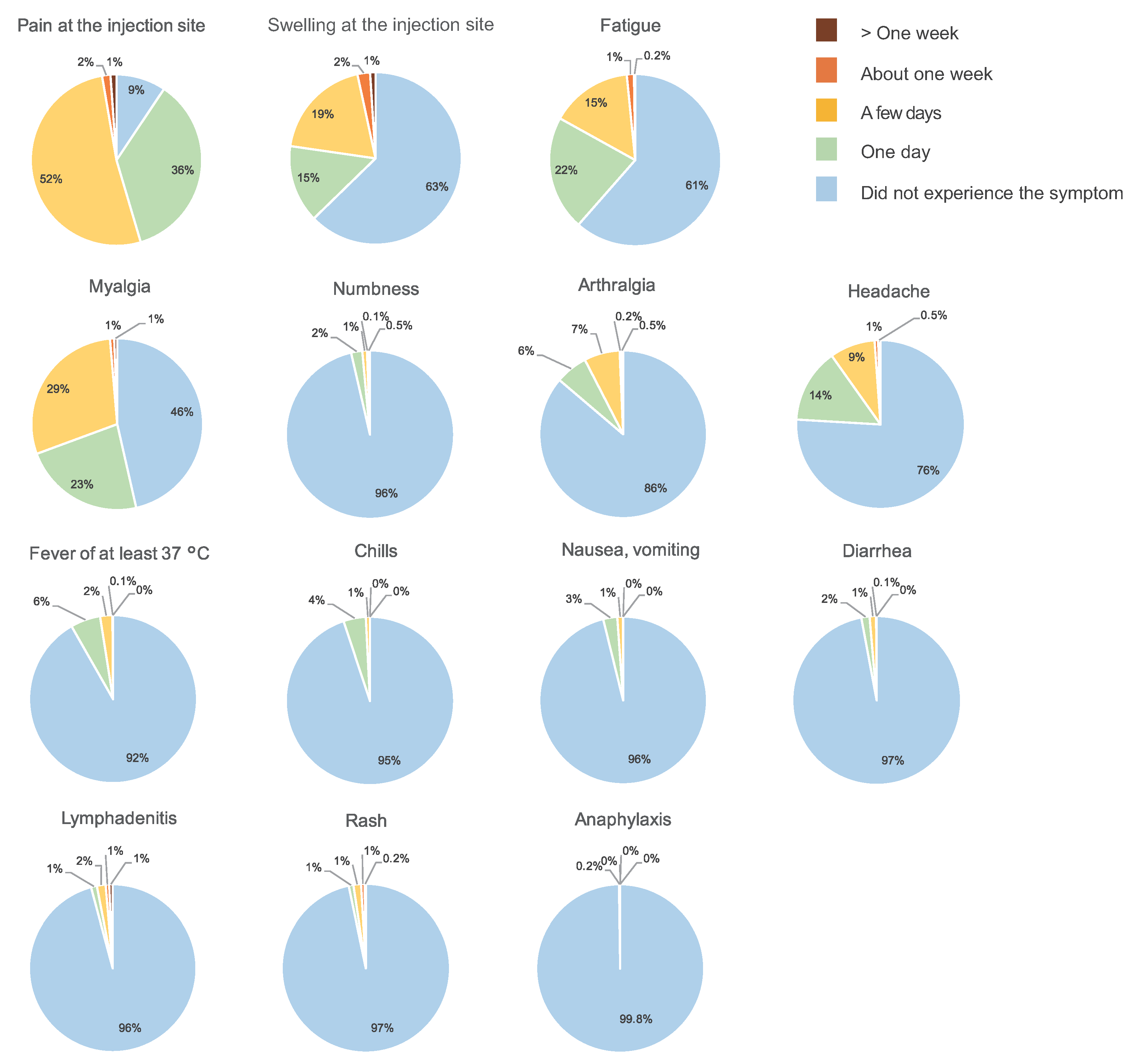
4.3. Side Effects
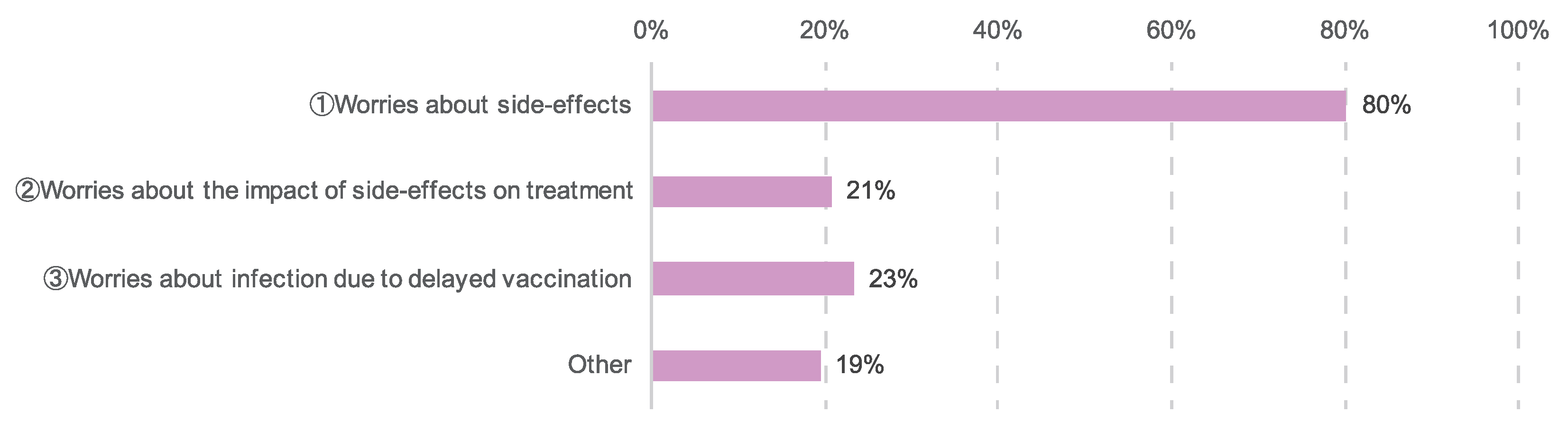
4.4. Vaccination Anxiety and Information Literacy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AACR | American Association for Cancer Research |
| ASCO | American Society of Clinical Oncology |
| COVID-19 | Coronavirus Disease 2019 |
| ESMO | European Society for Medical Oncology |
| NCCN | National Comprehensive Cancer Network |
| NCI | National Cancer Institute |
References
- Suzuki, H.; Mori, M.; Namiki, M.; Yamada, N.; Yoshikawa, T.; Tsutsumi, C.; Tozaki, S.; Iwamoto, H.; Torii, S.; Okubo, Y.; et al. Impact of COVID-19 on breast cancer patients. J. Jpn. Surg. Assoc. 2022, 83, 1–11. [Google Scholar]
- Kawate, T.; Yoshida, A.; Sugae, S.; Asaga, S.; Kaise, H.; Saji, S.; Yamauchi, C.; Miyoshi, Y.; Yamauchi, H.; Ishikawa, T. Recommendations for the management of breast cancer patients during the COVID-19 pandemic from the Japan Breast Cancer Society. Breast Cancer 2021, 28, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Lee, S.A.; Khil, E.K.; Byeon, S.J.; Kang, H.J.; Choi, J.A. COVID-19 vaccine-related axillary lymphadenopathy in breast cancer patients: Case series with a review of literature. Semin. Oncol. 2021, 48, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Wagner, T.; Nathan, M.; Szyszko, T. COVID-19 vaccine-related lymph node activation—Patterns of uptake on PET-CT. BJR Case Rep. 2021, 7, 20210040. [Google Scholar] [CrossRef]
- Peer Ring Association. 2022. Available online: http://site.peer-ring.com (accessed on 17 March 2022).
- Maringe, C.; Spicer, J.; Morris, M.; Purushotham, A.; Nolte, E.; Sullivan, R.; Rachet, B.; Aggarwal, A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol. 2020, 21, 1023–1034. [Google Scholar] [CrossRef]
- Tian, J.; Yuan, X.; Xiao, J.; Zhong, Q.; Yang, C.; Liu, B.; Cai, Y.; Lu, Z.; Wang, J.; Wang, Y.; et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: A multicentre, retrospective, cohort study. Lancet Oncol. 2020, 21, 893–903. [Google Scholar] [CrossRef]
- Hwang, J.K.; Zhang, T.; Wang, A.Z.; Li, Z. COVID-19 vaccines for patients with cancer: Benefits likely outweigh risks. J. Hematol. Oncol. 2021, 14, 38. [Google Scholar] [CrossRef]
- Corti, C.; Crimini, E.; Tarantino, P.; Pravettoni, G.; Eggermont, A.M.; Delaloge, S.; Curigliano, G. SARS-CoV-2 vaccines for cancer patients: A call to action. Eur. J. Cancer 2021, 148, 316–327. [Google Scholar] [CrossRef]
- Japanese Society of Medical Oncology. Q & A on COVID-19 Vaccination and Cancer Treatment. 2022. Available online: https://www.jsmo.or.jp/news/coronavirus-information/qa_vaccinel_3gakkai.html (accessed on 17 March 2022).
- National Comprehensive Cancer Network. COVID-19 Vaccination and Cancer Patients. 2022. Available online: https://www.nccn.org/covid-19 (accessed on 28 January 2022).
- The Royal College of Surgeons of England. Vaccinated Patients Guidance. 2022. Available online: https://www.rcseng.ac.uk/coronavirus/vaccinated-patients-guidance (accessed on 28 January 2022).
- Ko, G.; Hota, S.; Cil, T.D. COVID-19 vaccination and breast cancer surgery timing. Breast Cancer Res. Treat. 2021, 188, 825–826. [Google Scholar] [CrossRef]
- Japanese Society for Radiation Oncology. Suggestions on SARS-CoV-2 Vaccination. 2022. Available online: https://www.jastro.or.jp/medicalpersonnel/news/20210226.pdf (accessed on 28 January 2022).
- European Society for Medical Oncology. COVID-19 Vaccination in Cancer Patients: ESMO Statements. 2022. Available online: https://www.esmo.org/covid-19-and-cancer/covid-19-vaccination?hit=ehp (accessed on 28 January 2022).
- American Society of Clinical Oncology. COVID-19 Vaccines & Patients with Cancer. 2022. Available online: https://www.asco.org/covid-resources/vaccines-patients-cancer (accessed on 28 January 2022).
- Ribas, A.; Sengupta, R.; Locke, T.; Zaidi, S.K.; Campbell, K.M.; Carethers, J.M.; Jaffee, E.M.; Wherry, E.J.; Soria, J.C.; D’Souza, G.; et al. Priority COVID-19 Vaccination for Patients with Cancer while Vaccine Supply Is Limited. Cancer Discov. 2021, 11, 233–236. [Google Scholar] [CrossRef]
- National Cancer Institute. COVID-19: What People with Cancer Should Know. 2022. Available online: https://www.cancer.gov/about-cancer/coronavirus/coronavirus-cancer-patient-information (accessed on 28 January 2022).
- Waissengrin, B.; Agbarya, A.; Safadi, E.; Padova, H.; Wolf, I. Short-term safety of the BNT162b2 mRNA COVID-19 vaccine in patients with cancer treated with immune checkpoint inhibitors. Lancet Oncol. 2021, 22, 581–583. [Google Scholar] [CrossRef]
- Chapin-Bardales, J.; Gee, J.; Myers, T. Reactogenicity Following Receipt of mRNA-Based COVID-19 Vaccines. JAMA 2021, 325, 2201–2202. [Google Scholar] [CrossRef] [PubMed]
- Barda, N.; Dagan, N.; Ben-Shlomo, Y.; Kepten, E.; Waxman, J.; Ohana, R.; Hernán, M.A.; Lipsitch, M.; Kohane, I.; Netzer, D.; et al. Safety of the BNT162b2 mRNA COVID-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2021, 385, 1078–1090. [Google Scholar] [CrossRef] [PubMed]
- Goshen-Lago, T.; Waldhorn, I.; Holland, R.; Szwarcwort-Cohen, M.; Reiner-Benaim, A.; Shachor-Meyouhas, Y.; Hussein, K.; Fahoum, L.; Baruch, M.; Peer, A.; et al. Serologic Status and Toxic Effects of the SARS-CoV-2 BNT162b2 Vaccine in Patients Undergoing Treatment for Cancer. JAMA Oncol. 2021, 7, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Menni, C.; Klaser, K.; May, A.; Polidori, L.; Capdevila, J.; Louca, P.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Merino, J.; et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet Infect. Dis. 2021, 21, 939–949. [Google Scholar] [CrossRef]
- Pharmaceuticals and Medical Devices Agency. COMIRNATY Intramuscular Injection. 2022. Available online: https://www.info.pmda.go.jp/go/pdf/672212_631341DA1025_1_10 (accessed on 28 January 2022).
- Centers for Disease Control and Prevention. Moderna COVID-19 Vaccine: What Healthcare Professionals Need to Know. 2022. Available online: https://www2.cdc.gov/vaccines/ed/covid19/moderna/40140.asp (accessed on 28 January 2022).
- Bernstine, H.; Priss, M.; Anati, T.; Turko, O.; Gorenberg, M.; Steinmetz, A.P.; Groshar, D. Axillary Lymph Nodes Hypermetabolism after BNT162b2 mRNA COVID-19 Vaccination in Cancer Patients Undergoing 18F-FDG PET/CT: A Cohort Study. Clin. Nucl. Med. 2021, 46, 396–401. [Google Scholar] [CrossRef]
- Eifer, M.; Tau, N.; Alhoubani, Y.; Kanana, N.; Domachevsky, L.; Shams, J.; Keret, N.; Gorfine, M.; Eshet, Y. COVID-19 mRNA Vaccination: Age and Immune Status and Its Association with Axillary Lymph Node PET/CT Uptake. J. Nucl. Med. 2022, 63, 134–139. [Google Scholar] [CrossRef]
- Schiaffino, S.; Pinker, K.; Magni, V.; Cozzi, A.; Athanasiou, A.; Baltzer, P.A.T.; Camps Herrero, J.; Clauser, P.; Fallenberg, E.M.; Forrai, G.; et al. Axillary lymphadenopathy at the time of COVID-19 vaccination: Ten recommendations from the European Society of Breast Imaging (EUSOBI). Insights Imaging 2021, 12, 119. [Google Scholar] [CrossRef]
- Faermann, R.; Nissan, N.; Halshtok-Neiman, O.; Shalmon, A.; Gotlieb, M.; Yagil, Y.; Samoocha, D.; Friedman, E.; Sklair-Levy, M. COVID-19 Vaccination Induced Lymphadenopathy in a Specialized Breast Imaging Clinic in Israel: Analysis of 163 cases. Acad. Radiol. 2021, 28, 1191–1197. [Google Scholar] [CrossRef]
- Society of Breast Imaging Patient Care and Delivery Committee. SBI Recommendations for the Management of Axillary Adenopathy in Patients with Recent COVID-19 Vaccination. 2022. Available online: https://www.sbi-online.org/Portals/0/Position%20Statements/2021/SBI-recommendations-for-managing-axillary-adenopathy-post-COVID-vaccination.pdf (accessed on 28 January 2022).
- Becker, A.S.; Perez-Johnston, R.; Chikarmane, S.A.; Chen, M.M.; El Homsi, M.; Feigin, K.N.; Gallagher, K.M.; Hanna, E.Y.; Hicks, M.; Ilica, A.T.; et al. Multidisciplinary Recommendations Regarding Post-Vaccine Adenopathy and Radiologic Imaging: Radiology Scientific Expert Panel. Radiology 2021, 300, E323–E327. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Rathore, F.A.; Farooq, F. Information Overload and Infodemic in the COVID-19 Pandemic. J. Pak. Med. Assoc. 2020, 70 (Suppl. 3), S162–S165. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.P.; Kung, P.T.; Wang, Y.H.; Tsai, W.C. Effect of time interval from diagnosis to treatment for cervical cancer on survival: A nationwide cohort study. PLoS ONE 2019, 14, e0221946. [Google Scholar] [CrossRef]
- Raphael, M.J.; Biagi, J.J.; Kong, W.; Mates, M.; Booth, C.M.; Mackillop, W.J. The relationship between time to initiation of adjuvant chemotherapy and survival in breast cancer: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2016, 160, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Polverini, A.C.; Nelson, R.A.; Marcinkowski, E.; Jones, V.C.; Lai, L.; Mortimer, J.E.; Taylor, L.; Vito, C.; Yim, J.; Kruper, L. Time to Treatment: Measuring Quality Breast Cancer Care. Ann. Surg. Oncol. 2016, 23, 3392–3402. [Google Scholar] [CrossRef] [PubMed]
- Olivotto, I.A.; Lesperance, M.L.; Truong, P.T.; Nichol, A.; Berrang, T.; Tyldesley, S.; Germain, F.; Speers, C.; Wai, E.; Holloway, C.; et al. Intervals Longer Than 20 Weeks From Breast-Conserving Surgery to Radiation Therapy Are Associated with Inferior Outcome for Women with Early-Stage Breast Cancer Who Are Not Receiving Chemotherapy. J. Clin. Oncol. 2009, 27, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Bleicher, R.J.; Ruth, K.; Sigurdson, E.R.; Beck, J.R.; Ross, E.; Wong, Y.N.; Patel, S.A.; Boraas, M.; Chang, E.I.; Topham, N.S.; et al. Time to Surgery and Breast Cancer Survival in the United States. JAMA Oncol. 2016, 2, 330–339. [Google Scholar] [CrossRef]









| No. of Patients (%) | ||
|---|---|---|
| Age (years) | 20s | 4 (0.3) |
| 30s | 94 (8) | |
| 40s | 467 (40) | |
| 50s | 520 (44) | |
| 60s | 86 (7) | |
| 70s | 6 (1) | |
| No response | 5 (0.4) | |
| Households | Single-person | 154 (13) |
| Two or more | 1028 (87) | |
| Type of cancer | Breast cancer | 944 (80) |
| Cervical cancer | 41 (3) | |
| Endometrial cancer | 82 (7) | |
| Ovarian cancer | 93 (8) | |
| Others | 22 (2) | |
| Stage of cancer | 0 (DCIS) | 71 (6) |
| I | 458 (39) | |
| II | 403 (34) | |
| III | 153 (13) | |
| IV | 69 (6) | |
| Unknown | 28 (2) | |
| Stage of treatment | Before treatment | 13 (1) |
| Neoadjuvant chemotherapy | 27 (2) | |
| Adjuvant chemotherapy | 126 (11) | |
| Radiation therapy | 20 (2) | |
| Endocrine therapy | 625 (53) | |
| Inserting expander in breast | 35 (3) | |
| Follow-up | 370 (31) |
| Type of Adjustment | Details |
|---|---|
| Arranged to be vaccinated during the interval between administration of anticancer drugs | Received the vaccine right around the midpoint of the interval between the days of anti-cancer drug administration Attending physician scheduled the vaccination to be a week after anti-cancer drug administration After anti-cancer drug administration, avoiding the following week, received the vaccine the week after that, then anti-cancer drugs were administered the following week Chose the 3rd week after anti-cancer drug; selected the Pfizer vaccine to match the anti-cancer drug course |
| Changed the treatment schedule of chemotherapy because of vaccination | Spread out the interval of chemotherapy to 4 weeks, allowing at least one week before and after vaccination |
| Avoided being vaccinated when white blood cell count was lowered from anticancer drugs | Arranged to be vaccinated when immune function returned after anti-cancer drug administration Avoided overlapping with the period of myelosuppression |
| Avoided vaccination on the same day as molecular targeted drugs were administered | Allowed at least one week after the administration of molecular targeted therapy Was advised by chemotherapy doctors/nurses to avoid the three days before and after molecular targeted drug administration, and to arrange to be vaccinated early the next week after drug administration (administration every three weeks) Avoided the day of herceptin monotherapy, but received the vaccine (both 1st and 2nd doses) two days after treatment |
| Avoided administering anti-cancer drugs during the week of vaccination | Avoided administering anti-cancer drugs on the week of vaccination Allowed about one week after chemotherapy before vaccination |
| Since chemotherapy could not be paused, received the vaccine on a Friday, so it would work out even if there were side-effects | Since it was during radiation therapy, decided to be vaccinated on Friday, fearing a fever Received the vaccine after irradiation on Friday in order to be able to rest well for two days after vaccination |
| Received the vaccine on a different day from family | Taking anti-cancer drugs orally. Allowed one week from the next hospital visit (avoiding the possibility of becoming unable to see a doctor due to fever) and chose a different vaccination from family |
| Type of Worry | Responses from the Participants |
|---|---|
| Onset or worsening of lymphedema | Despite having already undergone lymph node dissection for breast cancer and receiving the first dose of the vaccine in the left arm, opposite the cancer side, I got lymphedema in my right arm, on the cancer side, two days later. I’m having a difficult time. I received the vaccine on the healthy side, but the lymphedema on the cancer side got worse. The swelling of the lymphedema that had been stable for the past few years got worse by the day, becoming numb the following week, and I suffered from a heavy feeling and pain. I had no choice but to receive conservative treatment. I currently sleep on my side, keeping the cancer side up, but since the pain after receiving the injection was strong I unintentionally ended up sleeping on the other side, causing the lymphedema to worsen. |
| Impediments to daily life and housework | Being unable to raise my arm up disrupted my daily activities. Since I had a 38.8 °C fever, I was unable to go out shopping, etc. After the second dose, I was bedridden and unable to do housework because of side-effects of muscle pain and chills. |
| Impact on work | I was told by my attending physician that I would be given the vaccine in the opposite arm from the operation, meaning that I was vaccinated in my dominant arm. Later, the pain in my shoulder was dreadful, severely impeding my ability to work. I left work early because of the side-effects, and my boss changed my shift for me. |
| Worries about impact on hospital visits or treatment | It means being imaged while the lymphedema is swollen. I’m worried that it will be mistaken for a relapse or metastasis. I had prolonged nausea and vomiting and was unable to take tamoxifen. Since I couldn’t take a break from the radiation therapy, even though I had a fever the day after receiving the vaccine, I still had to go to the hospital. It was quite difficult. |
| Impact on cancer treatment or surgery | Since I received the second dose about one week after the operation, it was scary because I didn’t know if the pain in my body and the fever were because of the operation or a side-effect of the vaccine. My neutrophil count decreased rapidly, so I had to suspend taking my medicine. It was difficult to tell the difference between the side-effects of the anti-cancer drugs and the vaccine. |
| Feeling worried | There was something like an odd feeling of worry, and I was unable to sleep. Since I took the vaccine on the same day as my family, I worried about how long the side-effects of my other family members would continue. |
| Worries about metastasis | I experienced extreme pain three days after the first dose in my left rib. Since the pain was like a broken bone, I was checked for bone metastasis, but there was nothing out of the ordinary. There is a lingering mild headache and nausea, and I worry about whether it is brain metastasis. |
| Organization | Summary of the Guideline |
|---|---|
| National Comprehensive Cancer Network (NCCN) [11] | Most people with cancer should get the vaccines as soon as they can. |
| European Society for Medical Oncology (ESMO) [15] | Considering the data for vaccines other than for COVID-19, vaccine effectiveness and safety is expected to be similar to nonpatients with cancer. Effectiveness varies depending on individual circumstances, but the benefits of vaccination are expected to significantly outweigh the risks. Ideally, the vaccine should be taken before cancer treatment, but it is also acceptable to take it during treatment if treatment has already begun. |
| American Society of Clinical Oncology (ASCO) [16] | Patients receiving cancer treatment may also be vaccinated. To avoid reducing the effectiveness of the vaccine, vaccination in the interval between administration of anticancer drugs may be considered. |
| American Association for Cancer Research (AACR) [17] | It is recommended that patients receiving cytotoxic anticancer drug treatment and immunotherapy be vaccinated preferentially. |
| National Cancer Institute (NCI) [18] | Patients with cancer may also be vaccinated. However, the possibility that vaccine effectiveness will be reduced for patients in an immunosuppressive state cannot be rejected, so patients should continue to take sufficient precautions against infection even after vaccination. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, H.; Akiyama, T.; Ueda, N.; Matsumura, S.; Mori, M.; Namiki, M.; Yamada, N.; Tsutsumi, C.; Tozaki, S.; Iwamoto, H.; et al. COVID-19 Vaccination in Patients with Cancer. Cancers 2022, 14, 2556. https://doi.org/10.3390/cancers14102556
Suzuki H, Akiyama T, Ueda N, Matsumura S, Mori M, Namiki M, Yamada N, Tsutsumi C, Tozaki S, Iwamoto H, et al. COVID-19 Vaccination in Patients with Cancer. Cancers. 2022; 14(10):2556. https://doi.org/10.3390/cancers14102556
Chicago/Turabian StyleSuzuki, Hitomi, Tomohiro Akiyama, Nobuko Ueda, Satoko Matsumura, Miki Mori, Masatoshi Namiki, Norikazu Yamada, Chika Tsutsumi, Satoshi Tozaki, Hisayuki Iwamoto, and et al. 2022. "COVID-19 Vaccination in Patients with Cancer" Cancers 14, no. 10: 2556. https://doi.org/10.3390/cancers14102556
APA StyleSuzuki, H., Akiyama, T., Ueda, N., Matsumura, S., Mori, M., Namiki, M., Yamada, N., Tsutsumi, C., Tozaki, S., Iwamoto, H., Torii, S., Okubo, Y., & Ishiguro, K. (2022). COVID-19 Vaccination in Patients with Cancer. Cancers, 14(10), 2556. https://doi.org/10.3390/cancers14102556







