Optimal Monitoring Technology for Pediatric Thyroidectomy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Environment
2.3. Ethics
2.4. Eligibility Criteria for Young Participants
2.5. Schedule of Participants
2.6. Interventions
2.6.1. Intermittent IONM Technology
2.6.2. Continuous IONM Technology
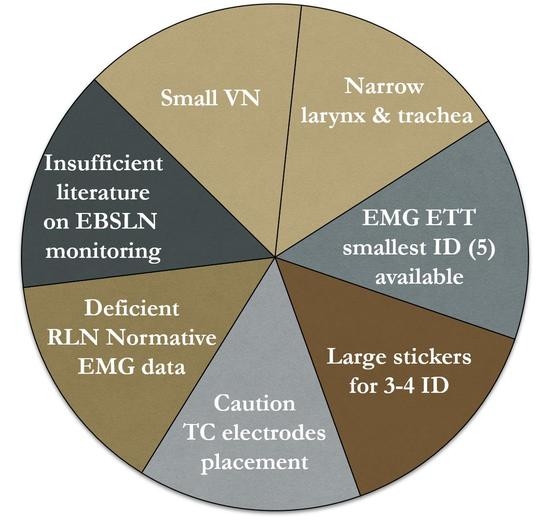
2.6.3. EMG Endotracheal Tube (ETT) Selection
2.6.4. Transcartilage (TC) Recording Electrodes
2.6.5. Troubleshooting Algorithm
2.7. Primary Objective
2.8. Secondary Outcome
2.9. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Procedures
3.3. Pathology
3.4. Morbidity
3.5. IONM and RLN Outcomes
3.5.1. NAR
3.5.2. EMG Profile
3.5.3. RLN Injury
3.5.4. IONM Technology
3.5.5. Troubleshooting Algorithm
4. Discussion
4.1. ETT & TC
4.2. C-IONM
4.3. EMG Profiles
4.4. RLN Morbidity
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Keane, A.; Bann, D.V.; Wilson, M.N.; Goldenberg, D. Pediatric Thyroid Cancer: To Whom Do You Send the Referral? Cancers 2021, 13, 4416. [Google Scholar] [CrossRef]
- Sosa, J.A.; Tuggle, C.T.; Wang, T.S.; Thomas, D.C.; Boudourakis, L.; Rivkees, S.; Roman, S.A. Clinical and economic outcomes of thyroid and parathyroid surgery in children. J. Clin. Endocrinol. Metab. 2008, 93, 3058–3065. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Park, S.; Jang, Y.E.; Kim, E.H.; Kim, H.S.; Kim, J.T. The distance between the glottis and the cuff of a tracheal tube placed through three supraglottic airway devices in children: A randomised controlled trial. Eur. J. Anaesthesiol. 2019, 36, 721–727. [Google Scholar] [CrossRef]
- O’Shea, J.E.; Loganathan, P.; Thio, M.; Kamlin, C.; Davis, P.G. Analysis of unsuccessful intubations in neonates using videolaryngoscopy recordings. Arch. Dis. Child Fetal Neonatal Ed. 2018, 103, F408–F412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, E.H.; Lee, J.H.; Song, I.K.; Kim, J.T.; Kim, B.R.; Kim, H.S. Effect of head position on laryngeal visualisation with the McGrath MAC videolaryngoscope in paediatric patients: A randomised controlled trial. Eur. J. Anaesthesiol. 2016, 33, 528–534. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, J.; Laschat, M.; Hellmich, M.; Wappler, F. A randomized controlled comparison of the Bonfils fiberscope and the GlideScope Cobalt AVL video laryngoscope for visualization of the larynx and intubation of the trachea in infants and small children with normal airways. Paediatr. Anaesth. 2013, 23, 913–919. [Google Scholar] [CrossRef]
- Dovas, A.; Lucchi, M.L.; Bortolami, R.; Grandis, A.; Palladino, A.R.; Banelli, E.; Carretta, M.; Magni, F.; Paolocci, N. Collaterals of recurrent laryngeal nerve fibres innervate the thymus: A fluorescent tracer and HRP investigation of efferent vagal neurons in the rat brainstem. Brain Res. 1998, 809, 141–148. [Google Scholar] [CrossRef]
- Prakash, M.; Johnny, J.C. Whats special in a child’s larynx? J. Pharm. Bioallied Sci. 2015, 7, S55–S58. [Google Scholar] [CrossRef]
- Fried, M.P.; Kelly, J.H.; Strome, M. Comparison of the adult and infant larynx. J. Fam. Pract. 1982, 15, 557–561. [Google Scholar]
- Motoyama, E.K. The shape of the pediatric larynx: Cylindrical or funnel shaped? Anesth. Analg. 2009, 108, 1379–1381. [Google Scholar] [CrossRef]
- Dalal, P.G.; Murray, D.; Messner, A.H.; Feng, A.; McAllister, J.; Molter, D. Pediatric laryngeal dimensions: An age-based analysis. Anesth. Analg. 2009, 108, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Wailoo, M.; Emery, J.L. Structure of the membranous trachea in children. Acta Anat. 1980, 106, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Hudgins, P.A.; Siegel, J.; Jacobs, I.; Abramowsky, C.R. The normal pediatric larynx on CT and MR. AJNR Am. J. Neuroradiol. 1997, 18, 239–245. [Google Scholar] [PubMed]
- Sapienza, C.M.; Ruddy, B.H.; Baker, S. Laryngeal structure and function in the pediatric larynx: Clinical applications. Lang. Speech Hear. Serv. Sch. 2004, 35, 299–307. [Google Scholar] [CrossRef]
- Holzki, J.; Brown, K.A.; Carroll, R.G.; Coté, C.J. The anatomy of the pediatric airway: Has our knowledge changed in 120 years? A review of historic and recent investigations of the anatomy of the pediatric larynx. Paediatr. Anaesth. 2018, 28, 13–22. [Google Scholar] [CrossRef]
- Brauckhoff, M.; Gimm, O.; Thanh, P.N.; Brauckhoff, K.; Ukkat, J.; Thomusch, O.; Dralle, H. First experiences in intraoperative neurostimulation of the recurrent laryngeal nerve during thyroid surgery of children and adolescents. J. Pediatr. Surg. 2002, 37, 1414–1418. [Google Scholar] [CrossRef]
- Legré, M.; Bois, E.; Bernard, S.; Teissier, N.; Van Den Abbeele, T. Recurrent laryngeal nerve monitoring during thyroidectomy and parathyroidectomy in children. Int. J. Pediatr. Otorhinolaryngol. 2020, 131, 109846. [Google Scholar] [CrossRef]
- Diercks, G.R.; Rastatter, J.C.; Kazahaya, K.; Kamani, D.; Quintanilla-Dieck, L.; Shindo, M.L.; Hartnick, C.; Shin, J.J.; Singer, M.C.; Stack, B.C.; et al. Pediatric intraoperative nerve monitoring during thyroid surgery: A review from the American Head and Neck Society Endocrine Surgery Section and the International Neural Monitoring Study Group. Head Neck 2022, 44, 1468–1480. [Google Scholar] [CrossRef]
- Schneider, R.; Machens, A.; Sekulla, C.; Lorenz, K.; Dralle, H. Recurrent Laryngeal Nerve Preservation Strategies in Pediatric Thyroid Oncology: Continuous vs. Intermittent Nerve Monitoring. Cancers 2021, 13, 4333. [Google Scholar] [CrossRef]
- Schneider, R.; Machens, A.; Sekulla, C.; Lorenz, K.; Weber, F.; Dralle, H. Twenty-year experience of paediatric thyroid surgery using intraoperative nerve monitoring. Br. J. Surg. 2018, 105, 996–1005. [Google Scholar] [CrossRef]
- Wu, C.W.; Huang, T.Y.; Randolph, G.W.; Barczyński, M.; Schneider, R.; Chiang, F.Y.; Silver Karcioglu, A.; Wojtczak, B.; Frattini, F.; Gualniera, P.; et al. Informed Consent for Intraoperative Neural Monitoring in Thyroid and Parathyroid Surgery-Consensus Statement of the International Neural Monitoring Study Group. Front. Endocrinol. 2021, 12, 795281. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawlor, C.M.; Zendejas, B.; Baird, C.; Munoz-San Julian, C.; Jennings, R.W.; Choi, S.S. Intraoperative Recurrent Laryngeal Nerve Monitoring During Pediatric Cardiac and Thoracic Surgery: A Mini Review. Front. Pediatr. 2020, 8, 587177. [Google Scholar] [CrossRef] [PubMed]
- Randolph, G.W.; Dralle, H.; International Intraoperative Monitoring Study Group; Abdullah, H.; Barczynski, M.; Bellantone, R.; Brauckhoff, M.; Carnaille, B.; Cherenko, S.; Chiang, F.Y.; et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: International standards guideline statement. Laryngoscope 2011, 121, S1–S16. [Google Scholar] [CrossRef]
- Chiang, F.Y.; Lee, K.W.; Chen, H.C.; Chen, H.Y.; Lu, I.C.; Kuo, W.R.; Hsieh, M.C.; Wu, C.W. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J. Surg. 2010, 34, 223–229. [Google Scholar] [CrossRef]
- Dionigi, G.; Chiang, F.Y.; Rausei, S.; Wu, C.W.; Boni, L.; Lee, K.W.; Rovera, F.; Cantone, G.; Bacuzzi, A. Surgical anatomy and neurophysiology of the vagus nerve (VN) for standardised intraoperative neuromonitoring (IONM) of the inferior laryngeal nerve (ILN) during thyroidectomy. Langenbecks Arch. Surg. 2010, 395, 893–899. [Google Scholar] [CrossRef]
- Liddy, W.; Wu, C.W.; Dionigi, G.; Donatini, G.; Giles Senyurek, Y.; Kamani, D.; Iwata, A.; Wang, B.; Okose, O.; Cheung, A.; et al. Varied Recurrent Laryngeal Nerve Course Is Associated with Increased Risk of Nerve Dysfunction During Thyroidectomy: Results of the Surgical Anatomy of the Recurrent Laryngeal Nerve in Thyroid Surgery Study, an International Multicenter Prospective Anatomic and Electrophysiologic Study of 1000 Monitored Nerves at Risk from the International Neural Monitoring Study Group. Thyroid 2021, 31, 1730–1740. [Google Scholar]
- Wu, C.W.; Randolph, G.W.; Barczyński, M.; Schneider, R.; Chiang, F.Y.; Huang, T.Y.; Karcioglu, A.S.; Konturek, A.; Frattini, F.; Weber, F.; et al. Training Courses in Laryngeal Nerve Monitoring in Thyroid and Parathyroid Surgery- The INMSG Consensus Statement. Front. Endocrinol. 2021, 12, 705346. [Google Scholar] [CrossRef]
- Wu, C.W.; Dionigi, G.; Barczynski, M.; Chiang, F.Y.; Dralle, H.; Schneider, R.; Al-Quaryshi, Z.; Angelos, P.; Brauckhoff, K.; Brooks, J.A.; et al. International neuromonitoring study group guidelines 2018: Part II: Optimal recurrent laryngeal nerve management for invasive thyroid cancer-incorporation of surgical, laryngeal, and neural electrophysiologic data. Laryngoscope 2018, 128, S18–S27. [Google Scholar] [CrossRef] [Green Version]
- Schneider, R.; Randolph, G.W.; Dionigi, G.; Wu, C.W.; Barczynski, M.; Chiang, F.Y.; Al-Quaryshi, Z.; Angelos, P.; Brauckhoff, K.; Cernea, C.R.; et al. International neural monitoring study group guideline 2018 part I: Staging bilateral thyroid surgery with monitoring loss of signal. Laryngoscope 2018, 128, S1–S17. [Google Scholar] [CrossRef] [Green Version]
- Dionigi, G.; Boni, L.; Rovera, F.; Rausei, S.; Castelnuovo, P.; Dionigi, R. Postoperative laryngoscopy in thyroid surgery: Proper timing to detect recurrent laryngeal nerve injury. Langenbecks Arch. Surg. 2010, 395, 327–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, T.Y.; Kim, H.Y.; Dionigi, G.; Lu, I.C.; Chang, P.Y.; Chiang, F.Y.; Lin, Y.C.; Tseng, H.Y.; Liu, C.H.; Wu, C.W. Laryngeal Neural Monitoring during Pediatric Thyroid Cancer Surgery-Is Transcartilage Recording a Preferable Method? Cancers 2021, 13, 4051. [Google Scholar] [CrossRef] [PubMed]




| Anatomical Peculiarities of the Neck in Children |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Concern | Adverse Event |
|---|---|
| EMG tube |
|
| Carotid sheet pocket creation & C-IONM electrode implantation |
|
| VN stimulation |
|
| C-IONM electrode displacement/replacement | |
| Hematoma | |
| Infection | |
| Allergies | |
| Surgical IONM break/malfunction | |
| Surgical C-IONM fracture/malfunction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, D.; Sun, H.; Kim, H.Y.; Pino, A.; Patroniti, S.; Frattini, F.; Impellizzeri, P.; Romeo, C.; Randolph, G.W.; Wu, C.-W.; et al. Optimal Monitoring Technology for Pediatric Thyroidectomy. Cancers 2022, 14, 2586. https://doi.org/10.3390/cancers14112586
Zhang D, Sun H, Kim HY, Pino A, Patroniti S, Frattini F, Impellizzeri P, Romeo C, Randolph GW, Wu C-W, et al. Optimal Monitoring Technology for Pediatric Thyroidectomy. Cancers. 2022; 14(11):2586. https://doi.org/10.3390/cancers14112586
Chicago/Turabian StyleZhang, Daqi, Hui Sun, Hoon Yub Kim, Antonella Pino, Serena Patroniti, Francesco Frattini, Pietro Impellizzeri, Carmelo Romeo, Gregory William Randolph, Che-Wei Wu, and et al. 2022. "Optimal Monitoring Technology for Pediatric Thyroidectomy" Cancers 14, no. 11: 2586. https://doi.org/10.3390/cancers14112586
APA StyleZhang, D., Sun, H., Kim, H. Y., Pino, A., Patroniti, S., Frattini, F., Impellizzeri, P., Romeo, C., Randolph, G. W., Wu, C.-W., Dionigi, G., & Fama’, F. (2022). Optimal Monitoring Technology for Pediatric Thyroidectomy. Cancers, 14(11), 2586. https://doi.org/10.3390/cancers14112586