3.1. Patient Characteristics
Among 249 patients (65 male patients), 46 (10 male patients; sex ratio 1:3.6) underwent HT and 203 (55 male; sex ratio 1:2.7) underwent BTT, with no significant between-group difference noted in the proportion of female patients (
p = 0.455). The mean age and history of hypothyroidism were similar between the HT and BTT groups (
p = 0.195 and
p = 0.282, respectively). Incidentaloma was the most common reason for patient visits in both the HT and BTT groups, with a significant between-group difference noted in the rates of incidentaloma (93.5% vs. 74.9%,
p = 0.006). Patients in the HT group were mostly diagnosed with cancer due to an incidentaloma (93.5%). Meanwhile, patients in the BTT group presented with many symptoms in the advanced stage, such as anterior neck mass (18.7%), lateral neck mass (3.0%), hoarseness (2.5%), and others (dyspnea, weight loss) (1.0%), in addition to incidentaloma (74.9%). There were significant differences in the family history related to thyroid disease (thyroid cancer, other organ cancers, and hypothyroidism) between the HT and BTT groups (26.1% vs. 13.3%,
p = 0.031). No patient had a history of radiation exposure in both the groups. The patient characteristics by group are presented in
Table 1.
Table 2 shows the between-group comparison of preoperative imaging findings (US and CT) for clinical TNM and US-guided detection of tumor aggressiveness. Most patients in the HT group had a T1 stage (67.4%) and N0 stage (89.1%) disease. Meanwhile, the BTT group had significantly more advanced T and N stage compared with the HT group (
p < 0.001 and
p < 0.001, respectively). The majority of patients in the BTT group had T3 stage (61.1%) and N1b stage (67.0%) tumors. Moreover, the rate of metastasis at the time of diagnosis was higher in the BTT group than in the HT group [ (0%) vs. 7 (3.4%),
p = 0.201]. The FNA cytology results for the nodule were 2 (4.3%), 1 (2.2%), 5 (10.9%), 21 (45.7%), and 17 (37.0%) for nondiagnostic, benign, atypia/follicular lesions of undetermined significance, suspicious for malignancy, and malignant, respectively, in the HT group. However, in the BTT group, there were only 15 (7.4%), 142 (70.0%), and 46 (22.7%) for atypia/follicular lesions of undetermined significance, suspicious for malignancy, and malignant, respectively, by significant difference (
p < 0.001). Aggressive variants were found on US in 4.3% and 37.4% of the patients in the HT and BTT groups, respectively, with a significant difference (
p < 0.001).
3.2. Pathological Findings and Surgical Outcomes
The pathological findings along with gene mutations are shown in
Table 3. All intermediate-risk pathological subtypes of PTC were identified in the study population, with a significant difference in their distribution between the HT and BTT groups (
p < 0.001). In the HT group, 19 (41.3%), 19 (41.3%), 6 (13.0%), 1 (2.2%), and 1 (2.2%) patient had DSV, SV, TCV, HV, and CCV, respectively. In the BTT group, 163 (80.3%), 23 (11.3%), 13 (6.4%), 3 (1.5%), and 1 (0.5%) patient had DSV, SV, TCV, HV, and CCV, respectively. The mean tumor size was 1.2 ± 0.8 cm (range, 0.4–3.5 cm) and 1.9 ± 1.2 cm (range, 0.3–7.0 cm) in the HT and BTT groups, respectively, with no significant difference (
p = 0.226). Meanwhile, there were significant between-group differences in multiplicity and bilaterality of thyroid cancer between the groups. The multiplicity of thyroid cancer was higher in the BTT group than in the HT group (55.7% vs. 23.9%,
p < 0.001). In total, 123 patients (60.0%) in the BTT group had bilateral thyroid cancer; of them, 36.0% had bilateral AVPTCs and 24.6% had cPTC and AVPTC. In the HT group, a clinically benign nodule on the lateral side of the thyroid cancer was identified as cPTC in 3 (6.5%) patients who underwent HT with partial thyroidectomy.
For positive metastatic LNs, the rate of LN involvement was higher in the BTT group than in the HT group (86.2% vs. 41.3%, p < 0.001). Further, although there was no significant between-group difference in the average number of harvested LNs (p = 0.091), the number of harvested metastatic LNs was significantly higher in the BTT group (6.7 ± 5.9 vs. 1.6 ± 2.4, p < 0.001). Additionally, more patients in the BTT group showed positive findings for perinodal soft tissue extension (53.2% vs. 2.2%, p < 0.001), microscopic ETE (76.8% vs. 39.1%, p < 0.001), and gross ETE (23.2% vs. 0.0%, p < 0.001). Meanwhile, there was no significant between-group difference in lymphovascular invasion (LVI) (p = 0.074) and positive BRAF mutation (p = 0.605). For positive TERT promoter mutation, all 46 patients in the HT group showed negative results, whereas 4 (16.0%) of the 25 patients in the BTT group had a TERT promoter mutation (p = 0.005). All patients in the HT group underwent genetic testing, but some patients in the BTT group were unable to undergo testing because of old age or loss of specimen. The BRAF and TERT promoter mutation rates were 38.9% and 8.1% for DSV, 36.4% and 0.0% for SV, 94.1% and 9.1% for TCV, 50% for HV, and 0.0% and 0.0% for CCV, respectively. In the final pathologic results, patients in the HT group had T1 (84.8%) or T2 (15.2%) stage disease and 58.7% and 41.3% had N0 and N1a stage disease, respectively. Meanwhile, for patients in the BTT group, 69.5% had T1–T2 stage disease, 30.5% had T3–T4 stage disease, and 18.7% and 67.0% had N1a and N1b stage disease, respectively.
Among patients in the BTT group, 94.6% underwent postoperative adjuvant RAI treatment. During the average follow-up period of 14.9 years, 2 patients (4.3%) in the HT group and 22 patients (10.8%) in the BTT group developed recurrence (
p = 0.178). The two patients in the HT group had locoregional recurrence in the lateral neck node 5 years and 3.3 years after the first surgery. Meanwhile, among these 22 patients in the BTT group, 11 (5.4%) patients had locoregional recurrence, 7 (3.4%) had distant recurrence, and 4 (2.0%) had both locoregional and distant recurrence. Among the 22 patients (10.8%) in the BTT group who developed recurrence within an average of 3.4 years after the first surgery, 17 (8.4%) patients were diagnosed with DSV; 3 (1.5%) patients, SV; and 2 (1.0%) patients, TCV. Among the 17 patients diagnosed with DSV who showed recurrence, 6 (35.3%) had distant metastasis, 4 (23.5%) had lateral neck node metastasis, 4 (23.5%) had operative bed and lateral neck node metastasis, 2 (11.8%) had distant and lateral neck node metastasis, and 1 (5.9%) had operative bed metastasis. Among the three SV patients, one patient each had lateral neck node metastasis, distant metastasis, and distant and lateral neck node metastasis. Among the two TCV patients, one patient had lateral neck node metastasis and the other had distant and lateral neck node metastasis. There was no significant difference in the distribution of recurrence sites between the two groups (
p = 0.397). The most common treatment for recurrence was reoperation with postoperative high-dose RAI in both the HT and BTT groups (
Table 4).
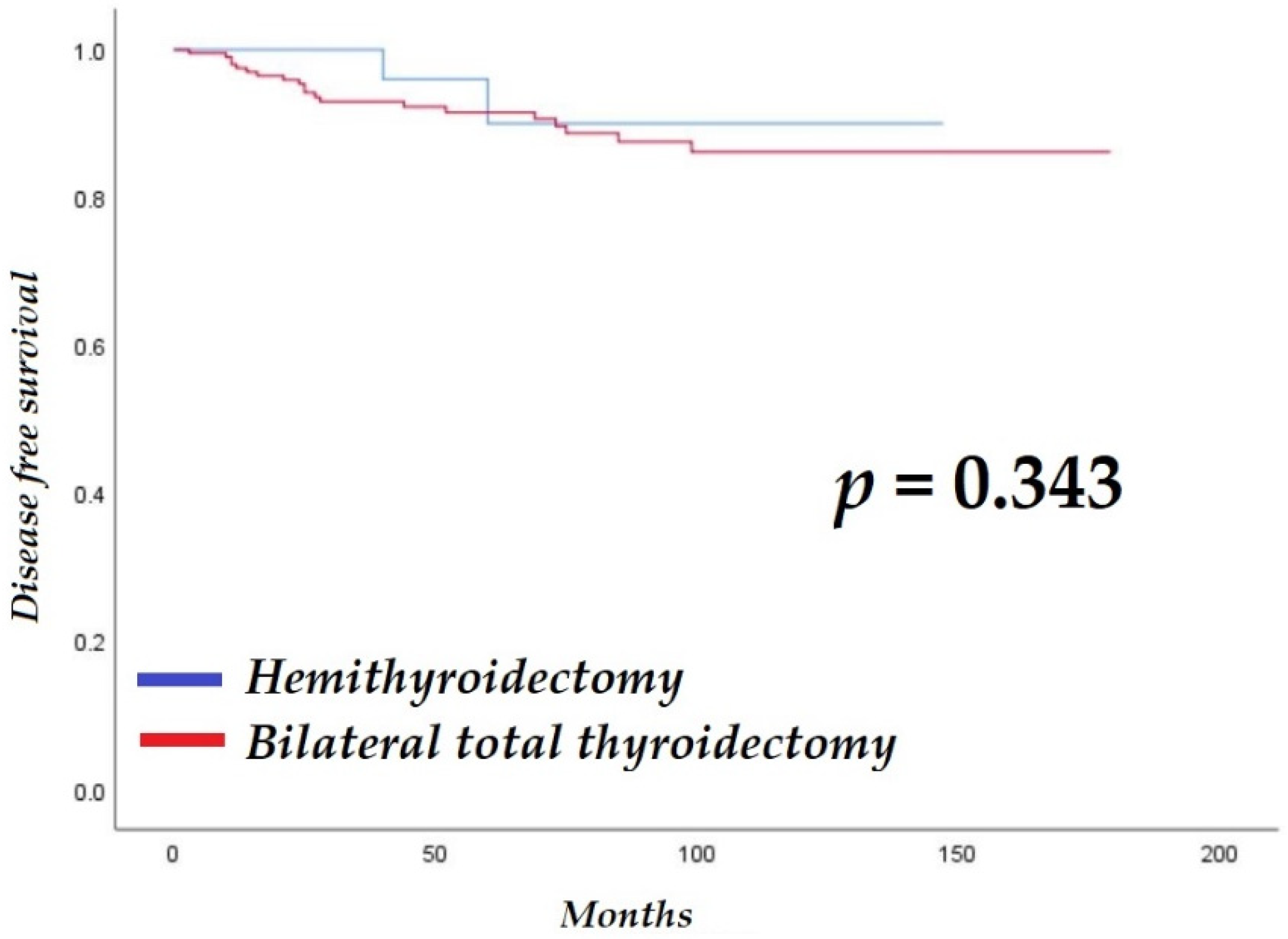
The average, median, and interquartile ranges of follow-up for the HT and BTT groups were 55.1 ± 39.0 months (range, 12–147 months), 42.5 months, and 54 months, and 77.0 ± 44.9 months (range, 11–179 months), 73.0 months, and 79 months, respectively. There was no significant difference in disease-free survival between the groups (HT: 137.5 ± 6.4 months vs. BTT: 158.4 ± 4.1 months; log-rank
p = 0.343;
Figure 1). One patient in the BTT group died during the follow-up period because of an underlying condition.
3.3. Predictive Risk Factors of Recurrence
Table 5 presents the results of the univariate and multivariate Cox regression analyses of predictive risk factors of recurrence. The risk of recurrence was 0.4 times lower for incidentalomas [hazard ratio (HR), 0.4; 95% confidence interval (CI), 0.2–0.9;
p = 0.033] and 2.7 times higher when cancer was diagnosed after a palpable neck mass was found (HR, 2.7; 95% CI, 1.1–6.4;
p = 0.025). The risk of recurrence was 8.3 times higher in patients with clinical N1b stage on preoperative US (HR, 8.3; 95% CI, 1.1–63.4;
p = 0.041). In addition, tumor size (HR, 1.3; 95% CI, 1.1–1.7;
p = 0.036), gross ETE positivity (HR, 3.1; 95% CI, 1.4–7.0;
p = 0.007), and pathology stage T3b (HR, 3.4; 95% CI, 1.0–11.4;
p = 0.045) or T4a (HR, 6.0; 95% CI, 1.9–18.8;
p = 0.002) increased the risk of recurrence. Conversely, age, sex, family history, clinical T stage, US-guided detection of aggressiveness, operation type, subtypes of AVPTC, perinodal soft tissue extension, microscopic ETE, multiplicity, bilaterality, LVI, LN metastasis, pathologic N stage, and postoperative adjuvant treatment methods did not have a significant impact on the risk of recurrence (
Table 5).
Patients in the HT group had none or one to two risk factors, including microscopic ETE, LVI, ≥4 LNs with extranodal extension, and ≥6 LNs. The patients were further divided into two groups: with no/low-risk factor and with intermediate or high-risk factor according to revised ATA guidelines [
3]. There were no significant differences in sex (
p = 0.190), age (
p = 0.480), family history (
p = 0.153), extranodal extension (
p = 0.089), bilaterality (
p = 0.768), tumor size (
p = 0.251), pathologic T stage (
p = 0.088), maximum diameter of LN (
p = 0.502), and BRAF mutation (
p = 0.129). Meanwhile, significant differences were noted in subtypes (
p = 0.002), multiplicity (
p < 0.001), and clinical N1a (
p < 0.001). For the subgroup with no risk factors, DSV was noted in 8 patients, SV in 18 patients, TCV in 6 patients, CCV in 1 patient, and HV in 1 patient. Meanwhile, for the subgroup with one to two risk factors, DSV was noted in 11 patients and SV in 1 patient.
The optimal cut-off point for tumor size predictive of recurrence was 1.4 cm (95% CI, 1.1–1.8,
p = 0.006) [
22]. The risk of recurrence was 3.3 times higher if tumor size was ≥1.4 cm (Harrell’s c-index, 0.666;
Table 6) [
23].